Abstract
INTRODUCTION
Postoperative hypocalaemia commonly occurs after extensive thyroid surgery and may require calcium and/or vitamin D supplements to alleviate or prevent the symptoms. In this study, we determined the risk factors for developing hypocalcaemia and whether early serum calcium levels can predict the development of or differentiate between temporary or permanent hypocalcaemia.
PATIENTS AND METHODS
A total of 162 patients who either had a completion or total thyroidectomy formed the basis of this prospective study. Serial serum calcium measurements were recorded as well as details of the operation, pathology, indications for surgery, number of parathyroids identified at operation and any complications.
RESULTS
Eighty-four (52%) patients did not develop hypocalcaemia but 69 (43%) were found to have temporary hypocalcaemia and 9 (5%) had permanent hypocalcaemia. Hypocalcaemia was more common after total than completion thyroidectomies and the identification of parathyroids at operation appears to have a significant adverse effect on outcome. The calcium levels measured on day 1 postoperatively and the slope (serum calcium levels of day 1 postoperative minus day of operation) were statistically significant in predicting the development of hypocalcaemia and possibly to differentiate between temporary or permanent hypocalcaemia.
DISCUSSION
Although almost half the patients having extensive thyroid surgery developed hypocalcaemia (as defined by any postoperative corrected serum calcium level of < 2.12 mmol/l) only 24% had a serum calcium of < 2.12 mmol/l associated with clinical symptoms of hypocalcaemia or a calcium level of < 2.0 mmol/l. Only 5% had persistent hypocalcaemia defined as requiring exogenous supplements at 6 months' postoperatively. Patients having a completion thyroidectomy appear to be less likely to develop hypocalcaemia perhaps as a result of any iatrogenic effects on the parathyroids at the first operation being reversed before the second operation. Identification and, therefore, exposure of parathyroids at operation may have an adverse effect on the blood supply to the glands affecting their function.
CONCLUSIONS
Serum calcium levels measured 6 hours' post-surgery and on day 1 postoperatively can be useful in predicting if the patient will develop hypocalcaemia and the slope may indicate whether the hypocalcaemia will be temporary or permanent. Patients with toxic goitres and those having a one-stage total thyroidectomy are most at risk of developing hypocalcaemia.
Keywords: Hypocalcaemia, Thyroid surgery
Hypocalcaemia is an important and common complication following thyroid surgery with reports varying from 0.5% to 75%.1–10 This wide variation is partly due to differences in defining hypocalcaemia and variance in laboratory ranges for normocalcaemia. Various causes for postoperative hypocalcaemia have been suggested including haemodilution or increased urinary calcium excretion secondary to surgical stress, calcitonin release secondary to thyroid gland manipulation, hungry bone syndrome (reversal of toxic thyroid osteodystrophy)1,6,11–18 and interference with the functioning of the parathyroid glands either through direct injury, removal or devascularisation.7,8,19 Although the development of postoperative hypocalcaemia is likely to be multifactorial in nature, thyroid lobectomy alone is hardly ever associated with this complication,1,16,20,21 which is most common following total thyroidectomy where there is a greater risk of parathyroid injury compared to other forms of thyroid surgery.
In most cases, post-thyroidectomy hypocalcaemia is temporary, but may take several months to resolve.10 A small percentage (0–12%)4,6,22,23 persist beyond this stage and are considered permanent, although the cut-off time between a temporary and permanent hypocalcaemia varies between 6 months24 and 1 year.3,6,23 Previous studies have looked at factors that may predict the development of hypocalcaemia after total thyroidectomy including the identification of parathyroids intra-operatively and different dissection techniques, though a general consensus of opinion is lacking.3,6,25
In this prospective study, we determined the incidence of temporary and permanent hypocalcaemia after either completion or total thyroidectomy and assessed the clinical and biochemical features that may be predictive based on statistical analysis.
Patients and Methods
In anticipation of this study, information was collected prospectively on all patients under the care of the senior author who either had a completion or total thyroidectomy from 1996 to 2007. Serum calcium was measured on the evening of surgery and on the first postoperative day, and on subsequent days when required. The presence or absence of any clinical signs or symptoms of hypocalcaemia was recorded. In our laboratory, the normal range for corrected serum calcium is 2.12–2.57 mmol/l. In this study, statistical analysis was performed defining hypocalcaemia as a corrected serum calcium of < 2.12 mmol/l although clinically significant hypocalcaemia may be considered when the corrected serum calcium is < 2.0 mmol/l if clinically asymptomatic or < 2.12 mmol/l in the presence of one or more signs or symptoms of hypocalcaemia. By including every patient with even a single serum calcium level below the reference range for our laboratory, we have ensured that no cases of hypocalcaemia have been excluded from the analysis for risk factors and predictive tests.
The surgical procedure (completion or total thyroidectomy), the number of parathyroid glands identified at operation, the pathology (toxic goitre, non-toxic goitre or malignant) and any complications were also recorded along with the patients' demographics. The type and length of calcium and vitamin D therapy received by the patients was also documented. Patients requiring calcium replacement therapy were initially prescribed this for 4 weeks; a week later serum calcium levels were measured and the following week they were re-assessed in the clinic. If the patient became clinically hypocalcaemic after stopping the exogenous calcium, they restarted their supplements. In these patients, the parathyroid hormone and calcium levels were repeated at 3 months' postoperatively. Permanent hypocalcaemia was defined by the requirement for calcium with or without vitamin D supplement for more than 6 months' postoperatively.
Statistical analysis
Information on categorical variables is presented as frequencies and percentages and continuous variables are described as median and interquartile range (IQR). Associations between categorical variables were tested with the chi-squared test whereas the median test was used for three group comparisons of continuous variables. Statistical significance was considered to be any test with a P < 0.05. Logistic regression models were fitted in order to examine whether serum calcium measurements would be useful in predicting the development of temporary and permanent hypocalcaemia. Finally, ROC curves were implemented in an attempt to explore calcium cut-off points that could be potentially useful in distinguishing between temporary and permanent hypocalcaemia patients during the first postoperative hours. All analysis was done with SPSS v.14.
Results
A total of 162 patients participated in this study. (All but 6 had their operation after 2000). The age range was 17–84 years and the majority (83.3%) were female.
In the study cohort, 125 patients had a one-stage total thyroidectomy and 37 patients had a completion thyroidectomy. Patients fell into three distinct groups of normocalcaemia (84, 51.9%), temporary hypocalcaemia (69, 42.6%) and permanent hypocalcaemia (9, 5.5%); the characteristics of all three groups are shown in Table 1. There was no statistically significant difference in age between the three groups (χ22 = 2.124; P = 0.346), though hypocalcaemia patients had a lower median age however a significant association was found between the type of operation and hypocalcaemia (χ22 = 9.079; P = 0.011 with significantly more patients having a one-stage total thyroidectomy developing either temporary (20.6%; 95% CI, 8.0–33.1%) or permanent (9.9%; 95% CI, –19.0 to 38.8%) hypocalcaemia compared to the normocalcaemia group. An association was observed between the pathology and the development of hypocalcaemia (χ24 = 14.665; P = 0.005). Patients with a toxic goitre developed temporary hypocalcaemia more frequently than those with malignancy. The variables of vocal cord palsy and other complications were not found to be significantly associated with the development of hypocalcaemia.
Table 1.
Patients' characteristics, operation, number of parathyroids identified, incidence of vocal cord palsies and other complications in patients with temporary, permanent or no hypocalcaemia postoperatively
| Hypocalcaemia | P-value | |||
|---|---|---|---|---|
| Temporary (n = 69) | Permanent (n = 9) | None (n = 84) | ||
| Age, median (IQR) | 38 (31, 51) | 34 (29, 41) | 42 (31, 61) | 0.346 |
| Sex, n (%) | ||||
| Male | 7 (10.1) | 2 (22.2) | 18 (21.4) | |
| Female | 62 (89.9) | 7 (77.8) | 66 (78.6) | 0.158 |
| Level 6, n (%) | ||||
| Yes | 4 (5.8) | 2 (22.2) | 5 (6.0) | |
| No | 65 (94.2) | 7 (77.8) | 79 (94.0) | 0.166 |
| Operation, n (%) | ||||
| Total | 61 (88.4) | 7 (77.8) | 57 (67.9) | |
| Completion | 8 (11.6) | 2 (22.2) | 27 (32.1) | 0.011 |
| Pathology, n (%) | ||||
| Toxic goitre | 51 (74.0) | 4 (44.4) | 39 (46.4) | |
| Non-toxic goitre | 6 (8.7) | 1 (11.1) | 9 (10.7) | |
| Malignancy | 11 (15.9) | 4 (44.4) | 36 (42.9) | 0.005 |
| Missing | 1 (1.4) | 0 (0.0) | 0 (0.0) | |
| Vocal cord palsy, n (%) | ||||
| Normal | 66 (95.7) | 9 (100.0) | 78 (92.8) | |
| Temporary | 2 (2.9) | 0 (0.0) | 3 (3.6) | 0.855 |
| Permanent | 1 (1.4) | 0 (0.0) | 3 (3.6) | |
| Complications, n (%) | ||||
| Yes | 5 (7.2) | 3 (33.3) | 11 (13.1) | |
| No | 64 (92.8) | 6 (66.7) | 72 (85.7) | 0.062 |
| Missing | 0 (0.0) | 0 (0.0) | 1 (1.2) | |
Identification of the parathyroids during surgery had an adverse effect on the development of postoperative hypocalcaemia. An association test between the number of parathyroid glands identified and the development of hypocalcaemia produced a significant result (χ24 = 11.427; P = 0.022): that is, the greater the number of parathyroids identified, the greater the incidence of hypocalcaemia following surgery. When no parathyroids were seen, normocalcaemia resulted in 70% of patients while 30% developed temporary hypocalcaemia. When all four parathyroids were identified, 90% of patients developed temporary and 10% permanent hypocalcaemia.
The main purpose of this study was to measure and identify the value of serial postoperative serum calcium levels which are shown for the three groups in Figure 1A–C. Calcium levels drop between the day of operation and day 1 postoperatively in the temporary group and even more dramatically in those with permanent hypocalcaemia whereas they remain virtually unchanged in patients in the normocalcaemic group. To quantify the reductions seen in the early postoperative period, the difference between serum calcium levels on day 1 postoperative minus day of the operation (slope 1) was derived for all patients. The median (IQR) slope 1 in the normocalcaemic group (n = 81) was 0.00 (–0.06, 0.05) whereas that in the permanent hypocalcaemic group (n = 9) was –0.30 (–0.38, –0.24). For those with temporary hypocalcaemia (n = 69), the respective values were –0.07 (–0.14, 0.01). An overall comparison showed that the median slope 1 values were significantly different (χ22 = 24.121; P < 0.0001) in the three groups. Logistic regression models were used and when comparing temporary with normocalcaemia all three variables of interest, i.e. calcium levels on the day of operation, at day 1 postoperatively and slope 1 were found to be associated with the outcome even adjusting for age, sex, type of operation and number of parathyroid glands identified (Table 2). In all cases, an increase in the calcium level was associated with reduced odds of having temporary hypocalcaemia. Thus a 1/100 unit increase in calcium day 1 results in a 26% (95% CI, 18–33%) decrease in the odds of having temporary hypocalcaemia. In the case of permanent hypocalcaemia, the calcium on the day of operation and slope 1 were also significantly associated with the outcome but, due to the small number of patients, only the unadjusted coefficients were derived here.
Figure 1.
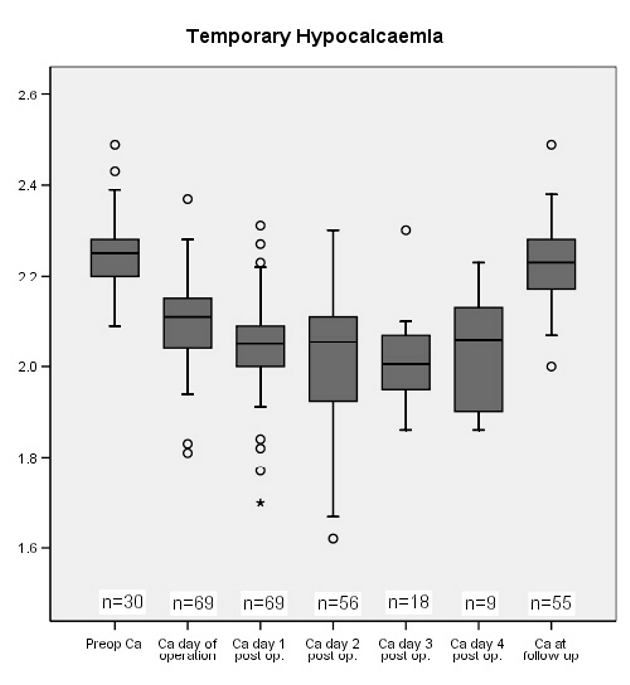
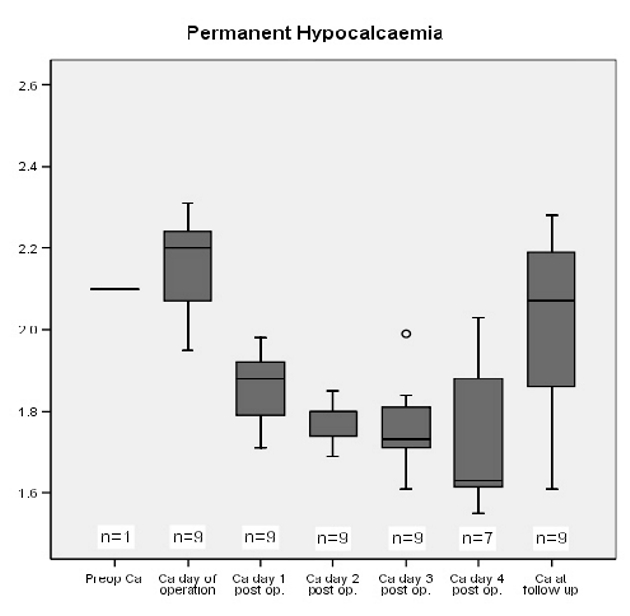
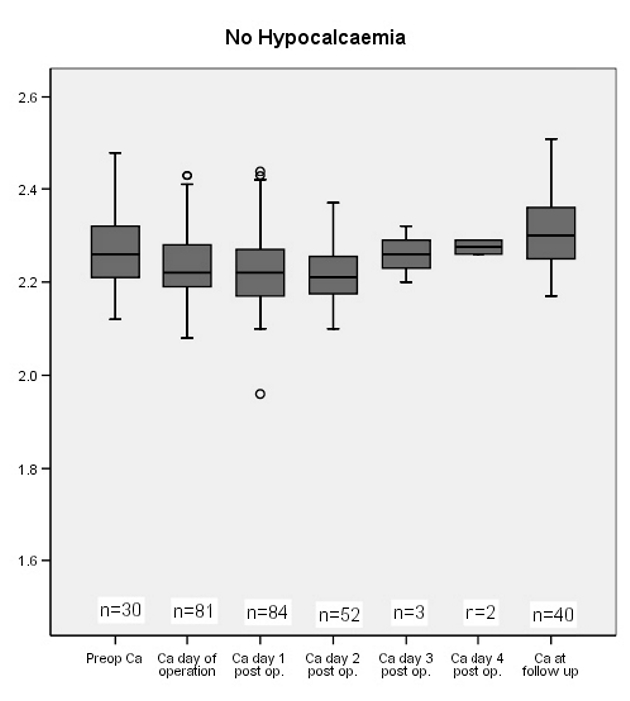
Calcium levels in patients with (A) temporary, (B) permanent, and (C) no hypocalcaemia pre- and postoperatively.
Table 2.
Logistic regression results of the outcomes of initial and permanent hypocalcaemia
| Hypocalcaemia | Unadjusted | Adjusted* | ||||||
|---|---|---|---|---|---|---|---|---|
| calcium | β | SE | Exp(β) (95% CI) | P-value | β | SE | Exp(β) (95% CI) | P-value |
| Temporary | ||||||||
| Operation day | –0.216 | 0.036 | 0.81 (0.75–0.87) | < 0.0001 | –0.251 | 0.045 | 0.78 (0.71–0.85) | < 0.0001 |
| Day 1 | –0.254 | 0.041 | 0.78 (0.72–0.84) | < 0.0001 | –0.299 | 0.051 | 0.74 (0.67–0.82) | < 0.0001 |
| Slope 1 | –0.049 | 0.017 | 0.95 (0.92–0.98) | 0.004 | –0.045 | 0.018 | 0.96 (0.92–0.99) | 0.012 |
| Permanent | ||||||||
| Operation day | –0.121 | 0.049 | 0.89 (0.81–0.98) | 0.014 | – | – | – | – |
| Slope 1 | –0.426 | 0.169 | 0.65 (0.47–0.91) | 0.011 | – | – | – | – |
Adjusted for the variables of age, sex, operation and number of parathyroids.
The secondary aim of this study was to determine whether examining the calcium levels would enable a distinction to be made between those patients with temporary and permanent hypocalcaemia. Normocalcaemic patients were excluded from this analysis. Adjustment for confounding variables could not be done at this stage due to the small number of permanent hypocalcaemia cases. The variables of calcium at day 1 postoperatively and slope 1 appeared to have the best discriminatory ability. These results suggest that both variables might potentially be useful markers in discriminating between permanent and temporary hypocalcaemia patients. Due to the small number of patients with permanent hypocalcaemia in this study, the estimations of sensitivity and specificity in Table 3 may not be very accurate and should, therefore, be applied with some caution. If, for example, we assume that all patients with a calcium level of equal or less than 1.94 on day 1 postoperatively will develop permanent hypocalcaemia, this has 88.9% sensitivity and 85.5% specificity, whereas for those with a level of 1.97 or less, the sensitivity is 100% but the specificity falls to 78.3%. Assuming that all patients with slope values of –0.24 or less have permanent hypocalcaemia, this has 66.7% sensitivity and 94.2% specificity whilst a slope of –0.20 or less has a 100% sensitivity and 92.8% specificity.
Table 3.
Combinations of sensitivity and specificity for various cut-off points of the day 1 calcium levels and slope levels (day 1-day of operation)
| Cut-off point | |||||||
|---|---|---|---|---|---|---|---|
| –0.30 | –0.25 | –0.24 | –0.23 | –0.20 | –0.15 | –0.10 | |
| Slope | |||||||
| Sensitivity (%) | 55.6 | 55.6 | 66.7 | 88.9 | 100 | 100 | 100 |
| 1-Specificity (%) | 1.4 | 4.3 | 5.8 | 5.8 | 7.2 | 20.3 | 44.9 |
| Calcium day 1 | |||||||
| Cut-off point | 1.90 | 1.92 | 1.94 | 1.97 | 2.00 | 2.02 | 2.04 |
| Sensitivity (%) | 55.6 | 66.7 | 88.9 | 100 | 100 | 100 | 100 |
| 1-Specificity (%) | 5.8 | 8.7 | 14.5 | 21.7 | 27.5 | 33.3 | 40.6 |
Discussion
The rates of temporary hypocalcaemia of 42.6% (even when defined as one measurement of a corrected serum calcium of < 2.12 mmol/l) and of permanent hypocalcaemia of 5.5% are comparable to published series.1,2,10 Interestingly, the rate of temporary hypocalcaemia falls to 24% when the criteria for defining hypocalcaemia are changed to a corrected serum calcium of < 2.12 mmol/l with one or more symptoms of hypocalcaemia or <2.0 mmol/l. Sturniolo et al.10 observed transient asymptomatic hypocalcaemia in 75% of their patients who had a total thyroidectomy and 62% having non-thyroid surgery indicating that surgical stress rather than abnormal parathyroid function may be responsible for postoperative hypocalcaemia though the mechanism remains unclear.
There was no statistical difference in the age and sex of the patients who had temporary hypocalcaemia, permanent hypocalcaemia or no hypocalcaemia. This supports the findings of Glinoer et al.3 but contrasts with the study by Prim et al.7 who found hypocalcaemia was statistically more common in females. This study also indicated that patients having a total thyroidectomy are more likely to develop hypocalcaemia than those patients having a completion thyroidectomy and this could be due to a number of factors. For example, the pathology was found to be highly associated with the type of surgery (χ22 = 95.883; P < 0.0001). In our experience, toxic goitres tend to be more bloody requiring more diathermy to be used for haemostasis which may compromise the vascular supply to the parathyroid glands. Completion thyroidectomy was performed in patients found to have a malignancy in the thyroid lobe previously removed. This two-stage procedure may have resulted in a lower incidence of hypocalcaemia since the parathyroids on the side of the previous lobectomy may have had time to recover their function prior to the completion surgery. The surgical planes in most intrathyroid malignancies (follicular, papillary) are preserved and the difficult dissection frequently associated with a vascular toxic goitre is not encountered. This series did not demonstrate level 6 neck dissections to be significant in the development of hypocalcaemia but Pisanu et al.26 cautioned against central neck dissections since they found this to be associated with permanent hypoparathyroidism.
The role of identifying parathyroid glands in the prevention of hypocalcaemia has been debated in the literature. Rimpl and Wahl,27 however, advocated the identification of at least three parathyroid glands to avoid hypocalcaemia and, therefore, recommended location of the parathyroid glands routinely. Walsh et al.28 found no association with the number of parathyroids identified. Our study, on the other hand, suggested that the identification of the parathyroid glands was not a safeguard and, in fact, increased the risk of hypocalcaemia probably related to either direct trauma or disruption of the blood supply due to surgical manipulation. As a result, we would not recommend active identification of the parathyroids during total thyroidectomy.
Lee et al.29 reported 58% of parathyroid tissue was extracapsular, 20% intracapsular and 22% intrathyroidal. Like Pattou et al.,6 we support the idea of an intracapsular dissection to reduce further the inadvertent removal of parathyroid glands during thyroid surgery, although one exception to this would be in cases of obvious capsular involvement in patients with malignancy.
It is our practice to measure the corrected serum calcium levels on the evening of the operation, on day 1, and on subsequent days according to the clinical situation. Our results strongly suggest that the calcium levels on the day of the operation and on day 1 postoperatively as well as the slope 1 value are useful in predicting the development of hypocalcaemia. Additionally, the calcium values on day 1 postoperatively and slope 1 may be helpful to differentiate between temporary and permanent hypocalcaemia. The relationship between these values has been previously reported in the literature,25,30–32 but we have, in addition, been able to provide the sensitivity and specificity of these values (Table 3), allowing their more useful application to clinical practice.
It is important to predict the development of postoperative hypocalcaemia at the earliest opportunity to prevent potentially devastating clinical consequences and to optimise the length of hospital stay.1,18,25,30,31 It is equally important to identify whether the detected hypocalcaemia is temporary or permanent since this not only influences the type and duration of treatment, but can also affect the incidence of pharmacological side-effects including iatrogenic hypercalcaemia and vitamin D induced inhibition of residual parathyroid function which, in cases of temporary hypocalcaemia, may become permanent if vitamin D is continued for longer than is required.23,33
When hypocalcaemia does occur, the decision to prescribe calcium alone or with vitamin D has led to algorithms being published.1,34 Our patients with a corrected serum calcium of < 2.0 mmol/l received calcium with additional vitamin D prescribed for 4 weeks initially if the corrected serum calcium was < 1.8 mmol/l. Thirteen patients were discharged on calcium alone and 20 received calcium and vitamin D supplements with medication continued long-term in the 9 patients with permanent hypocalcaemia.
Conclusions
Serum calcium levels measured at 6-h post surgery and on day 1 postoperatively are useful in predicting whether the patient will develop hypocalcaemia and day 1 postoperative calcium level and the slope may differentiate whether the patient will have a temporary or permanent hypocalcaemia. Patients with toxic goitres and those having a one-stage total thyroidectomy are most at risk of developing hypocalcaemia.
References
- 1.Fahmy FF, Gillet D, Lolen Y, Shotton JC. Management of serum calcium levels in post-thyroidectomy patients. Clin Otolaryngol. 2004;29:735–9. doi: 10.1111/j.1365-2273.2004.00895.x. [DOI] [PubMed] [Google Scholar]
- 2.Gac EP, Cabane TP, Amat VJ, Huidobro GF, Rossi FR, et al. Incidence of hypocalcaemia after total thyroidectomy [in Spanish] Rev Med Chil. 2007;135:26–30. doi: 10.4067/s0034-98872007000100004. [DOI] [PubMed] [Google Scholar]
- 3.Glinoer D, Andry G, Chantrain G, Samil N. Clinical aspects of early and late hypocalcaemia after thyroid surgery. Eur J Surg Oncol. 2000;26:571–7. doi: 10.1053/ejso.2000.0949. [DOI] [PubMed] [Google Scholar]
- 4.Jacobs JK, Aland JW, Jr, Ballinger JF. Total thyroidectomy: A review of 213 patients. Ann J Surg. 1983;197:542–9. doi: 10.1097/00000658-198305000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lo CY, Lam KY. Post-operative hypocalcaemia in patients who did or did not undergo parathyroid autotransplantation during thyroidectomy: a comparative study. Surgery. 1998;124:1081–6. doi: 10.1067/msy.1998.92560. [DOI] [PubMed] [Google Scholar]
- 6.Pattou FP, Combemale F, Fabre S, Carnaille B, Decoulx M, et al. Hypocalcaemia following thyroid surgery: incidence and prediction of outcome. World J Surg. 1998;22:718–24. doi: 10.1007/s002689900459. [DOI] [PubMed] [Google Scholar]
- 7.Prim MP, de Diego JI, Hardisson D, Madero R, Gavilan J. Factors related to nerve injury and hypocalcaemia in thyroid gland surgery. Otolaryngol Head Neck Surg. 2001;124:111–4. doi: 10.1067/mhn.2001.112305. [DOI] [PubMed] [Google Scholar]
- 8.Sasson AR, Pingpank JF, Jr, Wetherington W, Hanion AL, Ridge JA. Incidental parathyroidectomy during thyroid surgery does not cause symptomatic hypocalcaemia. Arch Otolaryngol Head Neck Surg. 2001;127:304–8. doi: 10.1001/archotol.127.3.304. [DOI] [PubMed] [Google Scholar]
- 9.Shindo ML, Sinha UK, Rice DH. Safety of thyroidectomy in residency: a review of 186 consecutive cases. Laryngoscope. 1995;105:1173–5. doi: 10.1288/00005537-199511000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Sturniolo G, Lo Schiavo MG, Tonante A, D'Alia C, Bonanno L. Hypocalcaemia and hypoparathyroidism after total thyroidectomy: a clinical biological study and surgical considerations. Int J Surg Invest. 2000;2:99–105. [PubMed] [Google Scholar]
- 11.Bourrel C, Uzzan B, Tison P, Despreaux G, Frachet B, et al. Transient hypocalcaemia after thyroidectomy. Ann Otol Rhinol Laryngol. 1993;102:496–501. doi: 10.1177/000348949310200702. [DOI] [PubMed] [Google Scholar]
- 12.Demeester-Mirkine N, Hooghe L, Van Geertruyden J, De Maertelaer V. Hypocalcemia after thyroidectomy. Arch Surg. 1992;127:854–8. doi: 10.1001/archsurg.1992.01420070118021. [DOI] [PubMed] [Google Scholar]
- 13.Falk AS, Birken EA, Baran DT. Temporary post thyroidectomy hypocalcaemia. Arch Otolaryngol Head Neck Surg. 1998;114:168–74. doi: 10.1001/archotol.1988.01860140066023. [DOI] [PubMed] [Google Scholar]
- 14.Headley CM. Hungry bone syndrome following parathyroidectomy. ANNA J. 1998;24:283–9. [PubMed] [Google Scholar]
- 15.Lindblom P, Westerdahl J, Bergenfelz A. Low parathyroid hormone levels after thyroid surgery: a feasible predictor of hypocalcaemia. Surgery. 2000;131:515–20. doi: 10.1067/msy.2002.123005. [DOI] [PubMed] [Google Scholar]
- 16.Miki H, Inoue H, Kitaichi M, Masuda E, Komaki K, Monden Y. Estimation of free calcium levels after thyroidectomy. J Med Invest. 1997;44:83–7. [PubMed] [Google Scholar]
- 17.Payne RJ, Hier MP, Tamilia M, Young J, MacNamara E, Black MJ. Postoperative parathyroid hormone level as a predictor of post-thyroidectomy hypocalcaemia. J Otolaryngol. 2003;32:362–7. doi: 10.2310/7070.2003.13985. [DOI] [PubMed] [Google Scholar]
- 18.Payne RJ, Hier M, Tamilia M, MacNamara E, Young J, Black MJ. Same-day discharge after total thyroidectomy: the value of 6-hour serum parathyroid hormone and calcium levels. Head Neck. 2005;27:1–7. doi: 10.1002/hed.20103. [DOI] [PubMed] [Google Scholar]
- 19.See AH, Soo KC. Hypocalcaemia following thyroidectomy for thyrotoxicosis. Br J Surg. 1996;84:95–7. [PubMed] [Google Scholar]
- 20.Pelizzo MR, Bernante P, Toniato A, Piotto A, Grigoletto R. Hypoparathyroidism after thyroidectomy. Analysis of a consecutive recent series [in Italian] Minerva Chir. 1998;53:239–44. [PubMed] [Google Scholar]
- 21.De Pasquale L, Schubert L, Bastagli A. Post-thyroidectomy hypocalcaemia and feasibility of short-stay thyroid surgery. Chir Ital. 2000;52:549–54. [PubMed] [Google Scholar]
- 22.Pedersen WC, Johnson CL, Gaskill HV, Aust JB, Cruz AB. Operative maagement of thyroid disease: technicl considerations in residency training program. Am J Surg. 1984;148:350. doi: 10.1016/0002-9610(84)90469-0. [DOI] [PubMed] [Google Scholar]
- 23.Proye C, Carnaille B, Maynou C, Bizard JP, Gilliot P, et al. The parathyroid risk in thyroid surgery. Argument against the early post-operative prescription of vitamin D. Experience with 729 thyroidectomies in 1988. Chirugie. 1990;116:493–500. [PubMed] [Google Scholar]
- 24.Tartaglia F, Sgueglia M, Muhaya A, Cresti R, Mulas MM, et al. Complications in total thyroidectomy: our experience and a number of considerations. Chir Ital. 2003;55:499–510. [PubMed] [Google Scholar]
- 25.Husein M, Hier MP, Al-Abdulhadi K, Black M. Predicting calcium status post thyroidectomy with early calcium levels. Otolaryngol Head Neck Surg. 2002;127:289–93. doi: 10.1067/mhn.2002.127891. [DOI] [PubMed] [Google Scholar]
- 26.Pisanu A, Cois A, Piu S, Altana ML, Uccheddu A. Factors predicting outcome of hypocalcaemia following total thyroidectomy. Chir Ital. 2003;55:35–40. [PubMed] [Google Scholar]
- 27.Rimpl I, Wahl RA. Surgery of nodular goiter: postoperative hypocalcaemia in relation to extent of resection and manipulation of the parathyroid glands [in German]. Langenbecks. Arch Chir Suppl Kongressbd. 1998;115:1063–6. [PubMed] [Google Scholar]
- 28.Walsh SR, Kumar B, Coveney EC. Serum calcium slope predicts hypocalcaemia following thyroid surgery. Int J Surg. 2007;5:41–4. doi: 10.1016/j.ijsu.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 29.Lee NJ, Blakey JD, Bhuta S, Calcaterra TC. Unintentional parathyroidectomy during thyroidectomy. Laryngoscope. 1999;109:1238–40. doi: 10.1097/00005537-199908000-00010. [DOI] [PubMed] [Google Scholar]
- 30.Adams J, Andersen P, Everts E, Cohen JI. Early postoperative calcium levels as predictors of hypocalcaemia. Laryngoscope. 1998;108:1829–31. doi: 10.1097/00005537-199812000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Luu Q, Andersen PE, Adams J, Wax MK, Cohen JI. The predictive value of perioperative calcium levels after thyroid/parathyroid surgery. Head Neck. 2002;24:63–67. doi: 10.1002/hed.10013. [DOI] [PubMed] [Google Scholar]
- 32.Moore C, Lampe H, Agrawal S. Predictability of hypocalcaemia using early post-operative serum calcium levels. J Otolaryngol. 2001;30:266–70. doi: 10.2310/7070.2001.19512. [DOI] [PubMed] [Google Scholar]
- 33.Proye C, Pattou F, Techer JE. Hypocalcaemie après thyroidectomie. Valeur predictive du dosage postoperatoire precoe de la parathormone. Atti XVII Congr. Naz SIEC; 1997; Firenze. [Google Scholar]
- 34.Gillett D, Fahmy F, Liew L, Massey S, Shotton JC. How we do it: implementing change- a multi-centre audit of an evidence-based protocol on post-thyroidectomy calcium maintenance. Clin Otolaryngol. 2006;31:216–32. doi: 10.1111/j.1749-4486.2006.01163.x. [DOI] [PubMed] [Google Scholar]


