Abstract
Presented is a case of incarcerated paracaecal hernia mimicking acute appendicitis. The clinical scenario highlights the need for a high index of suspicion in the management of patients with localised peritonism even in the absence of obstructive symptoms and the presence of normal laboratory markers of inflammation.Whilst computed tomography might offer a pre-operative diagnosis, in such a low-risk patient laparoscopy offers the combined advantages of immediate diagnosis and definitive treatment of acute pathology.
Keywords: Ileal entrapment, Paracaecal hernia, Appendicitis
Case report
A32-year-old man presented with a 24-h history of sharp, localised right iliac fossa pain described as increasing in severity and without radiation. Colicky exacerbations were infrequent. The patient denied current or previous intestinal obstructive (distension, vomiting, constipation) or urinary symptoms. There was no prior medical or surgical history of note.
Clinical examination demonstrated an afebrile patient with a scaphoid abdomen and no visible or palpable abdominal wall hernias. Peritonismwas noted in the right iliac fossa. No masses or visceromegaly were evident. The bowel sounds were scanty but of normal pitch. Urinalysis confirmed the absence of blood, leukocytes and nitrites.
Plain radiographswere not performed.Laboratory investigations demonstrated the renal function, haematological profile and C-reactive protein to bewithin normal limits.
On the basis of a clinical diagnosis of probable obstructive appendicitis secondary to faecolith, the patient was taken to theatre. Prior to port insertion, examination under general anaesthesia demonstrated a tangerine-sized smooth mass in the lateral right iliac fossa which was not indentable. Three ports were inserted (10 mm infra-umbilical, 5 mm LIF and 10 mm suprapubic) using an open technique.
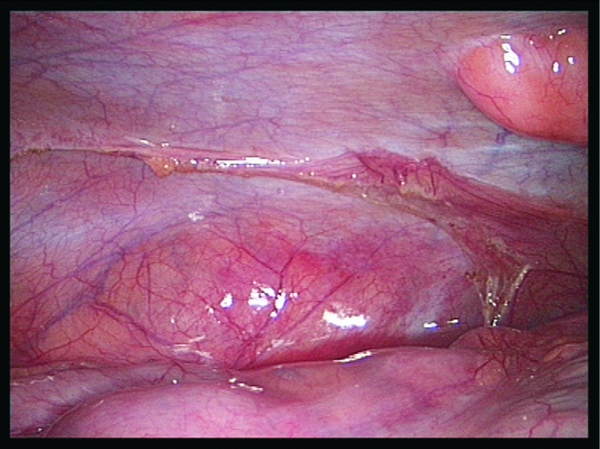
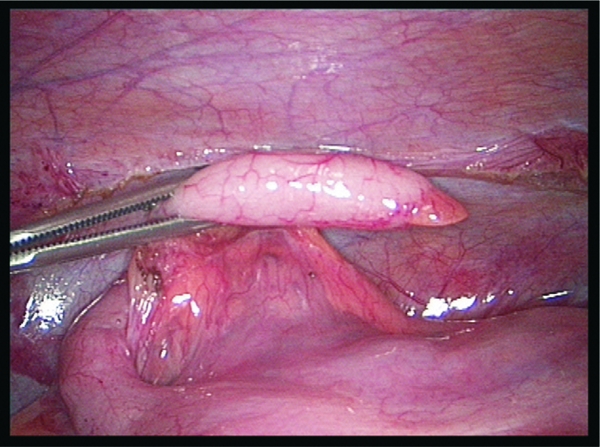
The initial finding was of ileum retained within a paracaecal hernia (Fig. 1). No significant proximal dilatation was noted. On reduction, the ileum was confirmed to be viable and without stricture (Fig. 2). The hernia neck was demonstrated (Fig. 3) and the appendix noted to be within the sac (Fig. 4). For the purpose of obliterating the sac (preventing further occurrences of intestinal incarceration) and appendicular mobilisation, the entire paracolic attachment was divided with diathermy (Fig. 5). Subsequent examination suggested possible appendicitis (a turgid, incompressible appendix; Fig. 6); routine laparoscopic appendicectomy was performed with an endoloop and retrieval via the suprapubic port. Following lavage and confirmed haemostasis, the ileumwas re-inspected and confirmed to be viable. Routine closure was performed.
Figure 1.
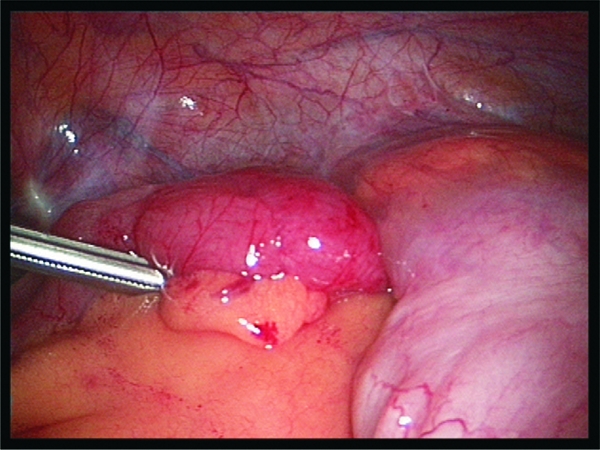
Ileum retained inferior to caecal pole.
Figure 2.
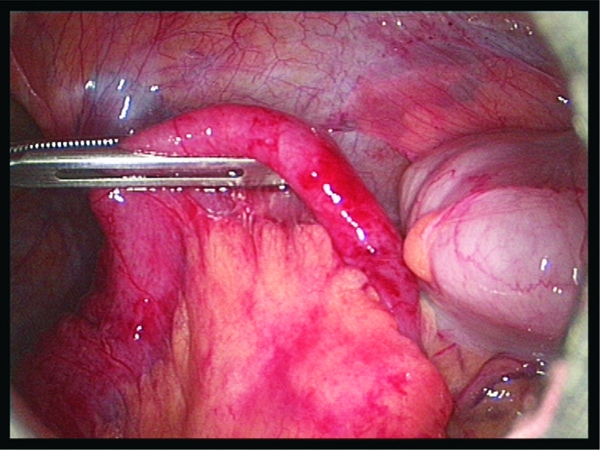
Ileum withdrawn and confirmed to be viable.Minimal proximal dilatation (left of picture).
Figure 3.
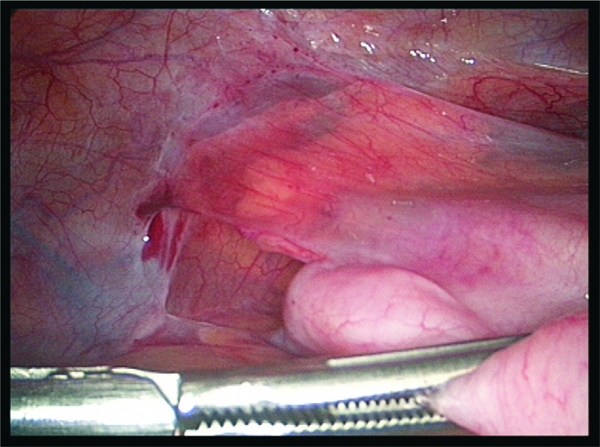
Demonstration of hernia neck.
Figure 4.
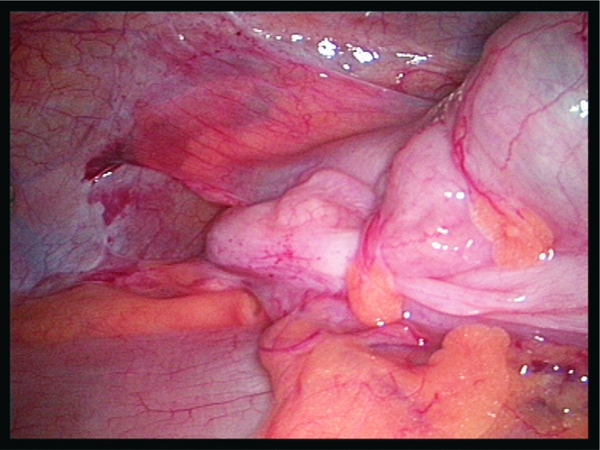
Appendix sited within hernia sac.
Figure 5.
Diathermy division of paracolic attachment deroofing sac.
Figure 6.
Macroscopic acute, uncomplicated appendicitis.
Subsequent histological examination demonstrated no evidence of acute appendicitis.
Postoperatively, the patient was asymptomatic and fit for discharge the following morning. Interestingly, in retrospect, he had been aware since childhood of intermittent colicky central abdominal pain but had never sought medical attention and had not thought it important at the initial consultation.
Relevant literature
The embryological development of the caecum through a process of budding, exteriorisation into the umbilicus and subsequent retraction onto the posterior abdominal wall predisposes to paracaecal fossae, of which four are typically described (superior and inferior ileocaecal, retrocaecal and paracolic).1,2 Relative to the caecal pole, five positions have been documented: retrocaecal (65%), descending, pelvic (31%), transverse retrocaecal (2.5%), ascending paracaecal preileal (1%) and ascending paracaecal postileal (0.5%).2 No record is made of the appendix lying within a paracaecal hernia.
In 1976, Bass and Longley3 reported a paracaecal hernia and noted 145 previous documented cases. Over a period of 13 years, Newsom and Kukora4 described a single paracaecal hernia in a series of 14 congenital or postoperative internal hernias supporting the rarity of the condition. In a larger series, Rivkind et al.5 presented five patients from a 2-year series with incarcerated paracaecal hernia, none of which required resection at laparotomy. They outlined the accepted principles of prompt surgical intervention with sac obliteration or closure. Sciacca et al.6 re-iterated this approach in a series of three such hernias in a cohort of 533 operated cases of small bowel obstruction (incidence 0.6%). The clinical finding of a ‘large round bump localised in the right iliac fossa’ was noted. Images of the actual procedure were published in 2006 by Smith et al.7
Further developments have included a case report of incarcerated paracaecal hernia following colonoscopy requiring laparotomy8 and a description of laparoscopic paracaecal hernia repair utilising obliteration of the neck with PDS sutures.9
Most recently, Hirokawa et al.10 recorded the management of a 74-year-old man presenting with intestinal obstruction who required mini-laparotomy for the management of an incarcerated paracaecal hernia noted at laparoscopy.
Aside from a high index of suspicion, diagnosis has been aided by advances in radiological imaging with computed tomography appearing to be the modality of choice.9,11
Conclusions
Presented is an incarcerated paracaecal hernia mimicking acute appendicitis. The clinical scenario highlights the need for a high index of suspicion in the management of patients with localised peritonism even in the absence of obstructive symptoms and the presence of normal laboratory markers of inflammation. Whilst computed tomography might offer a pre-operative diagnosis, in such a low-risk patient laparoscopy offers the combined advantages of immediate diagnosis and definitive treatment of acute pathology.
References
- 1.Larson WJ. Human Embryology. 3rd edn. Philadelphia, PA: Churchill Livingstone; 2001. [Google Scholar]
- 2.Schumpelick V, Dreuw B, Ophoff K, Prescher A. Appendix and cecum. Embryology, anatomy, and surgical applications. Surg Clin North Am. 2000;80:295–318. doi: 10.1016/s0039-6109(05)70407-2. [DOI] [PubMed] [Google Scholar]
- 3.Bass J, Jr, Longley BJ. Paracecal hernia: case report and review of the literature. Am Surg. 1976;42:285–8. [PubMed] [Google Scholar]
- 4.Newsom BD, Kukora JS. Congenital and acquired internal hernias: unusual causes of small bowel obstruction. Am J Surg. 1986;152:279–85. doi: 10.1016/0002-9610(86)90258-8. [DOI] [PubMed] [Google Scholar]
- 5.Rivkind AI, Shiloni E, Muggia-Sullam M, Weiss Y, Lax E, Freund HR. Paracecal hernia: a cause of intestinal obstruction. Dis Colon Rectum. 1986;29:752–4. doi: 10.1007/BF02555327. [DOI] [PubMed] [Google Scholar]
- 6.Sciacca P, Bertolini R, Borrello M, Bargigli R, Marcarone Palmieri R. Intestinal obstruction caused by paracecal hernia. 3 case reports and review of the literature. Minerva Chir. 1997;52:983–8. [PubMed] [Google Scholar]
- 7.Smith GH, Skipworth RJ, Duff MD, Anderson DN. Red herring: a rare cause of small bowel obstruction. Surgeon. 2006;4:107–10. doi: 10.1016/s1479-666x(06)80040-5. [DOI] [PubMed] [Google Scholar]
- 8.Patterson R, Klassen G. Small bowel obstruction from internal hernia as a complication of colonoscopy. Can J Gastroenterol. 2000;14:959–60. doi: 10.1155/2000/893292. [DOI] [PubMed] [Google Scholar]
- 9.Omori H, Asahi H, Inoue Y, Irinoda T, Saito KJ. Laparoscopic paracecal hernia repair. Laparoendosc Adv Surg Tech A. 2003;13:55–7. doi: 10.1089/109264203321235494. [DOI] [PubMed] [Google Scholar]
- 10.Hirokawa T, Hayakawa T, Tanaka M, Okada Y, Sawai H, et al. Laparoscopic surgery for diagnosis and treatment of bowel obstruction: case report of paracecal hernia. Med Sci Monit. 2007;13:CS79–82. [PubMed] [Google Scholar]
- 11.Barbary C, Floquet M, Riebel N, Tissier S, Laurent V, Régent D. Small bowel obstruction caused by enteroliths and Meckel's diverticulitis associated with internal paracecal hernia in an adult. J Radiol. 2004;85:49–50. doi: 10.1016/s0221-0363(04)97546-4. [DOI] [PubMed] [Google Scholar]


