Abstract
INTRODUCTION
Corrective surgery for Dupuytren's disease represents a significant proportion of a hand surgeon's workload. The decision to go ahead with surgery and the success of surgery requires measuring the degree of contracture of the diseased finger(s). This is performed in clinic with a goniometer, pre- and postoperatively. Monitoring the recurrence of the contracture can inform on surgical outcome, research and audit.
PATIENTS AND METHODS
We compared visual and computer software-aided estimation of Dupuytren's contractures to clinical goniometric measurements in 60 patients with Dupuytren's disease. Patients' hands were digitally photographed. There were 76 contracted finger joints – 70 proximal interphalangeal joints and six distal interphalangeal joints. The degrees of contracture of these images were visually assessed by six orthopaedic staff of differing seniority and re-assessed with computer software.
RESULTS
Across assessors, the Pearson correlation between the goniometric measurements and the visual estimations was 0.83 and this significantly improved to 0.88 with computer software. Reliability with intra-class correlations achieved 0.78 and 0.92 for the visual and computer-aided estimations, respectively, and with test–retest analysis, 0.92 for visual estimation and 0.95 for computer-aided measurements.
CONCLUSIONS
Visual estimations of Dupuytren's contractures correlate well with actual clinical goniometric measurements and improve further if measured with computer software. Digital images permit monitoring of contracture after surgery and may facilitate research into disease progression and auditing of surgical technique.
Keywords: Dupuytren's disease, Goniometer, Assessment, Deformity
Dupuytren's disease, a fibroproliferative disorder, represents a significant workload for the hand surgeon. Presenting more commonly in the elderly male population, it has a varying prevalence, between 2–42%, determined largely by familial predilection.1 An incomplete autosomal dominant inheritance has been proposed.2
Typical symptoms include palmar nodules, pitting and skin thickening. This can then progress to digital fixed flexion deformities, predominantly affecting the little and ring fingers.3 The worse the contracture, the more disabling the condition becomes for the patient.
Patients with Dupuytren's disease need treatment when the contracture progresses and becomes functionally disabling. In clinic, the history is reviewed and the deformity is measured with a goniometer. A decision about the need for surgical correction is then made taking into account the patient's wishes, function of the hand and the measured severity of contracture.
Some hand surgeons use a ‘table-top’ test for consideration to progress to surgery. If the patient is unable to flatten their hand fully, palm facing down, on a table surface, then the disease is deemed severe enough for surgical intervention.
After surgical correction, the patients are re-assessed in clinic to measure the deformity. Success of the operation is determined by the degree of correction and improved function. A variable rate of recurrence has been reported up to 71%.4–7
The assessment of Dupuytren's contracture before and after surgery consumes a significant proportion of the hand surgeon's clinic. Given the drive by the NHS to audit surgical outcome, an accurate and reliable method of assessing the effectiveness of Dupuytren's surgery without the need to attend hospital may seem desirable.
The aim of this study was to examine whether clinical goniometric measurements of Dupuytren's contractures correlate well with visual estimations of digital images and whether this is improved by computer-aided measurements. We also investigated whether orthopaedic experience of the doctor correlated with accuracy of estimation of Dupuytren's contractures and tried to determine what characteristics of a digital photograph generated best correlation with goniometric measurements.
Patients and Methods
Informed consent was obtained from 60 patients, with Dupuytren's contractures, to allow a photograph to be taken of their affected hand in clinic. Each patient had their affected hand photographed with a digital camera by a consultant orthopaedic surgeon, no specific instructions were given to the consultant about how to frame the hand in the photograph. The contractures were then measured by a single consultant using a finger goniometer.
Each digital image of the hand was then assessed for the degree of contracture by six orthopaedic staff of differing levels of experience. Two were foundation doctors, two specialist registrars and two orthopaedic consultant hand surgeons. Two methods for assessing the degree of contracture on the digital image were used:
The observer visually estimated the degree of contracture(s) of the affected finger(s) from the digital image.
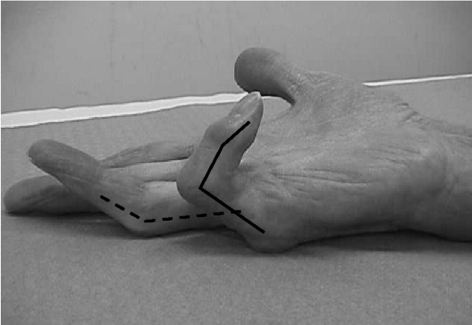
The observer used a computer program to measure the degree of contracture. The assessor was first instructed on how to use the package (Image J, v.1.36b; National Institutes of Health, Bethesda, MD, USA); this involved superimposing lines over the mid-axes of the relevant phalanges which best represented their position (Fig. 1). The computer then measured the angle of contracture between the lines.
Figure 1.
Computer software-aided measurements of Dupuytren's contracture. With the aid of computer-software, lines are super-imposed of the mid axes of the affected fingers as judged by the assessor. The computer then automatically calculates the angle between the lines for each affected joint.
Eleven of the 60 photographs were intentionally duplicated during both estimations to permit test–retest reliability analysis and, in order to avoid recall bias, the two assessments were performed 1 week apart. No assessor was aware of this.
Each photograph was also assessed by the study team to determine what characteristics of the photograph achieved the best correlations. The characteristics assessed were:
The degree to which the hand was pronated relative to the surface on which it was resting when being photographed was noted. Three categories were judged: flat (0–15°), slightly pronated (16–30°) or moderately pronated (31–45°).
We also recorded whether the hand was photographed from the side or whether an oblique view was obtained.
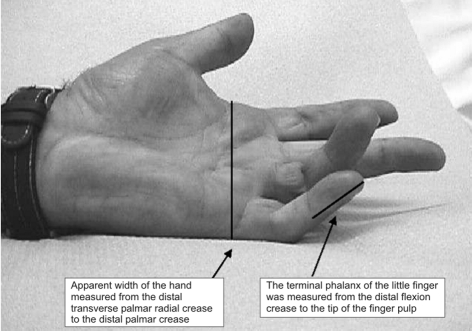
Finally, we visually documented whether the panning angle of the camera-hand view was low (0–25°), medium (26–50°) or high (51–75°). In order to determine the accuracy of this visual assessment of the panning angle, the width of the hand, as it appeared on the photograph, was measured by the same computer software. A low panning angle would generate an apparent narrow hand width whereas a higher panning angle would generate a broader hand width. The width was defined as the distance from distal transverse palmar radial crease to the distal palmar ulnar crease as seen on the photograph. To allow for different magnifications of the photograph, the palmar width was standardised according to the length of the terminal phalanx of the little finger, the distal flexion crease to the tip of the finger pulp (Fig. 2). This hand width to terminal phalanx ratio was then correlated with the visually assessed panning angle of the camera.
Figure 2.
Assessing the panning angle of the camera by measuring the apparent width of the hand. The apparent width of the hand was measured and divided by the length of the terminal phalanx; this allowed standardisation of magnification. Therefore, a relatively low ratio of apparent hand width to terminal phalanx would indicate a less pronated hand and a relatively high ratio of apparent hand width to terminal phalanx would indicate a more pronated hand. This hand also demonstrates what photographic features would facilitate accurate estimation of Dupuytren contractures. The image is taken on a flat surface, with the patient told to extend the fingers maximally; the hand is slightly pronated from flat, photographed from the ulnar side in a direct side-on view with a medium level camera panning angle view.
The goniometric measurements were correlated with the estimated visual and computer-aided measurements for all the assessors combined and at each level of assessor experience (foundation doctor, specialist registrar and consultant hand surgeon). Reliability was assessed using the intra-class correlation coefficient and test-retest correlation.
Pearson's correlations were also used to determine what features of the digital photograph (i.e. degree of pronation, view and panning angle) produced the best correlation between the actual goniometric measurements and the two separate measurements made by the assessors.
Results
Sixty patients were recruited with 76 unique Dupuytren's disease affected joints, as 16 patients had two joints affected on their diseased hand. In total, 87 photographs were assessed including 11 duplicates; all duplicates were of the PIPJ of the little finger. Measurements were performed on 81 PIPJs, (64 little fingers and 17 ring fingers) and six DIPJs (all little fingers). The metacarpophalangeal joint was excluded from this study and duplicate measurements were only included in the test–retest analysis.
For all assessors combined, for all joints affected the estimated visual measurements had a correlation of 0.83 (P < 0.01) with the goniometric measurements (Table 1). However, for the computer-aided measurements, the correlation with actual goniometric measurements significantly (P < 0.05) improved to 0.88, this correlation itself being significant (P < 0.01).
Table 1.
Correlations of goniometric measurements of finger joint contracture with visual and computer-aided measurements
| Average correlations | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| All | Foundation doctors | Specialist registrars | Consultants | ||||||
| n | VM | CAM | VM | CAM | VM | CAM | VM | CAM | |
| All joints | 76 | 0.83 | 0.88 | 0.84 | 0.88 | 0.81 | 0.87 | 0.86 | 0.88 |
| PIPJs | 70 | 0.84 | 0.88 | 0.84 | 0.88 | 0.82 | 0.88 | 0.86 | 0.89 |
| DIPJs | 6 | 0.78 | 0.93 | 0.92 | 0.95 | 0.77 | 0.94 | 0.67 | 0.90 |
| Little finger | 59 | 0.83 | 0.88 | 0.82 | 0.87 | 0.81 | 0.86 | 0.85 | 0.90 |
| Ring finger | 17 | 0.87 | 0.89 | 0.92 | 0.92 | 0.81 | 0.91 | 0.88 | 0.85 |
Pearson average correlations achieved when comparing actual clinical goniometric measurements with the estimated visual measurements (VM) and the computer-aided measurements (CAM). The results are tabulated by joint, finger and clinical experience of assessor.
The results also indicate that, regardless of joint or finger, the computer-aided measurements improved the correlation. The most marked improvement occurred in the assessment of the little finger DIPJ. This was regardless of the experience of the assessor.
To assess reliability of measurements, for the estimated visual and computer-aided measurements, intra-class correlation coefficients were calculated. The intra-class correlation coefficient assesses measurement reliability by comparing the variability of different measurements of the same subject to the total variation across all measurements and all subjects.
For the estimated visual measurements, the intra-class correlation was 0.78 (95% CI, 0.68–0.86) and for the computer-aided measurements the intra-class correlation was 0.92 (95% CI, 0.88–0.94).
Further reliability was assessed by test–retest analysis. Given that there were 6 assessors and 11 duplicates, data were available for 66 images. Between duplicate photographs, a correlation of 0.92 was achieved for visual estimations and 0.95 for computer-aided measurements.
The following characteristics were determined based on the 60 digital images, accounting for 76 affected joints:
Thirty-six affected joints were from a hand photographed when flat, 28 images were of a slightly pronated hand and 12 images of a moderately pronated hand.
Seventy of the affected hands were photographed from a side-on perspective the other six had an oblique view.
Twenty-six affected joints were photographed from a low camera panning-angle, 43 from a medium panning-angle and 7 from a high panning-angle. The visually assessed panning angle had a 0.86 Pearson correlation with the hand width to terminal phalanx ratio.
The results (Table 2) demonstrate that, when visually estimating Dupuytren's contractures from a digital photograph, the hand should be flat, viewed from side-on and photographed from a moderately elevated camera panning-angle to generate the best correlation. Similar findings where also noted when the hand was assessed for computer-aided measurements, although a hand slightly pronated from flat had a marginally better, but not statistically significant, correlation.
Table 2.
Correlations of clinical goniometric measurements of joint contracture for both visual measurements and computer-aided measurements, as determined by the characteristics of the photographed hand
| Hand characteristic when photographed | Specific hand descriptor | n | Correlations | |
|---|---|---|---|---|
| Visual measurement | Computer-aided measurement | |||
| Flatness of hand | ||||
| Flat | 36 | 0.85 | 0.88 | |
| Slightly pronated | 28 | 0.82 | 0.89 | |
| Moderately pronated | 12 | 0.83 | 0.89 | |
| View of hand | ||||
| Side-on | 70 | 0.84 | 0.89 | |
| Oblique | 6 | 0.40 | 0.55 | |
| Panning-angle | ||||
| Low | 26 | 0.73 | 0.77 | |
| Moderate | 43 | 0.89 | 0.92 | |
| High | 7 | 0.86 | 0.86 | |
Of the 76 joints photographed 74 were photographed from the ulnar side and two affected finger joints were photographed from the radial side of the hand. No meaningful correlations could be computed given the small number of hands that were photographed from the radial side.
Although not a primary aim of the study, the mean degree of Dupuytren's contracture was calculated and compared to the estimated visual and computer-aided measurement means (Table 3). Although not statistically significant, both types of estimations tended to over-estimate the degree of contracture.
Table 3.
Actual mean goniometric finger joint contracture measurements compared with mean estimated visual measurements and mean estimated computer-assisted measurements as determined by the Dupuytren affected joint
| PIPJ little finger | DIPJ little finger | PIPJ ring finger | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Measurements | n | Mean | CI | n | Mean | CI | n | Mean | CI |
| Goniometric | 53 | 51 | 45–56 | 6 | 47 | 34–60 | 17 | 49 | 38–59 |
| Visual estimation | 318 | 56 | 54–59 | 36 | 48 | 41–55 | 102 | 55 | 50–60 |
| Computer-aided | 318 | 53 | 50–55 | 36 | 55 | 50–59 | 102 | 50 | 45–55 |
The number of measurements (n) and confidence interval (CI) are given; the measurements are in degrees.
Discussion
A publicly funded NHS must be efficient and cost-effective. Examples of initiatives to facilitate efficiency include: preventing unnecessary hospital admissions, treating patients in the community, decreasing length of hospital stays, following up patients only where absolutely necessary after surgery, and auditing surgical outcomes.
There is no cure for Dupuytren's disease and surgery may only offer respite. Recurrence of contractures does occur, especially in patients who are younger (less than 40 years of age), have both hands affected and have a positive family history.11 Careful judgement based on severity, the rate of contracture progression and functional disability allows a decision on whether and when to perform surgery. This decision is informed by goniometric measurements of the degree of contracture.
Goniometry is commonly used for measuring the range of movement of joints in hand and orthopaedic practice. Georgeu et al.12 compared the use of computer-aided goniometry with standard goniometry, and reported a high correlation (0.975) for finger joints. Motion analysis has also been compared to standard goniometric measurements for finger joints achieving results comparable with conventional goniometry.13 An extensive search of the Medline database found no study comparing clinical goniometric measurements of patients suffering with Dupuytren's contracture to visual or computer-aided estimates.
In this study, visual estimations of the degree of Dupuytren contractures on digital photographs correlate well with actual goniometric measurements. Further accuracy of these measurements can be obtained with computer-aided measurements. The photographed hands do not need to be assessed by a consultant hand surgeon to achieve good correlations with goniometric assessments.
The metacarpophalangeal joints are also commonly affected in Dupuytren's disease and, although not incorporated into this study, the authors believe that similar visual and computer-aided correlations would be achievable.
To permit the best assessment of the degree of contracture, the hand should be photographed on a flat surface, with the patient told to extend their fingers maximally. The hand should be slightly pronated from flat and photographed from the ulnar side to give a direct side-on view with a medium level panning angle (Fig. 2).
Such a photograph could be assessed by any member of the consultant hand surgeon's team. This will allow pre-operative assessment of severity as well as postoperative monitoring of disease progression and, therefore, surgical outcome. A decision can then be made whether primary or further revision surgery was a real option after taking into account the patient's functional disability.
These patients then need to be seen and their options carefully discussed. Such an approach could free up a significant amount of clinic time while still permitting satisfactory assessment of outcome after Dupuytren's contracture surgery and facilitating research into Dupuytren's surgery and audit.
References
- 1.Whalley DC, Elliot D. Dupuytren's disease: a legacy of the north? J Hand Surg Br. 1993;18:363–7. doi: 10.1016/0266-7681(93)90065-n. [DOI] [PubMed] [Google Scholar]
- 2.Elliot D. The early history of contracture of the palmar fascia (part I) J Hand Surg Br. 1988;13:246–55. doi: 10.1016/0266-7681_88_90078-2. [DOI] [PubMed] [Google Scholar]
- 3.Hueston J. Dupuytren's contracture. Edinburgh: E&S Livingstone; 1963. pp. 51–63. [Google Scholar]
- 4.Gordon S. Dupuytren's contracture: recurrence and extension following surgical treatment. Br J Plast Surg. 1957;51:286–8. doi: 10.1016/s0007-1226(56)80052-0. [DOI] [PubMed] [Google Scholar]
- 5.Hall PN, Fitzgerald A, Sterne GD, Logan AM. Skin replacement in Dupuytren's disease. J Hand Surg Br. 1997;22:193–7. doi: 10.1016/s0266-7681(97)80061-7. [DOI] [PubMed] [Google Scholar]
- 6.Norotte G, Apoil A, Travers V. A ten years' follow-up of the results of the results of surgery for Dupuytren's disease. A study of fifty-eight cases. Ann Chir Main. 1988;7:277–81. doi: 10.1016/s0753-9053(88)80024-3. [DOI] [PubMed] [Google Scholar]
- 7.Hueston JT. Digital Wolfe grafts in recurrent Dupuytren's contracture. Plast Reconstr Surg. 1962;29:342–4. doi: 10.1097/00006534-196204000-00005. [DOI] [PubMed] [Google Scholar]
- 8.National Audit Office. Out-patient services. London: NHS; 1991. [Google Scholar]
- 9.Department of Health. The Patient's Charter. London: DH; 1992. [Google Scholar]
- 10.McCormack TT, Collier JA, Abel PD, Collins CD, Ritchie WN. Attitudes to follow-up after uncomplicated surgery – hospital out-patients or general practitioner? Health Trends. 1984;16:46–7. [PubMed] [Google Scholar]
- 11.Hueston JT. State of the art: the management of recurrent Dupuytren's disease. Eur Med Bibliogr. 1991;1:7–16. [Google Scholar]
- 12.Georgeu GA, Mayfield S, Logan AM. Lateral digital photography with computer-aided goniometry versus standard goniometry for recording finger joint angles. J Hand Surg Br. 2002;27:184–6. doi: 10.1054/jhsb.2001.0692. [DOI] [PubMed] [Google Scholar]
- 13.Chiu HY, Su FC, Wang ST, Hsu HY. The motion analysis and goniometry of the finger joints. J Hand Surg Br. 1998;23:788–91. doi: 10.1016/s0266-7681(98)80098-3. [DOI] [PubMed] [Google Scholar]