Abstract
INTRODUCTION
Two week wait referral guidelines have been published by the UK Department of Health for suspected urological cancers. Concordance to these guidelines is variable. Our objectives were to assess the incidence of urological malignancy and the proportion of inappropriate referrals in the two-week wait pathway.
PATIENTS AND METHODS
Retrospective audit of all two-week wait referrals to the urology department over 6 months. Inappropriate referrals were those not satisfying the referral criteria, but referred under the two-week wait system. Detection rates were calculated for each referral criterion based on diagnosis obtained from histology, imaging reports and clinic letters.
RESULTS
Incidence of cancer was 90 of 400 two-week wait referrals (23%). The cancer-detection rate based on reasons for referral ranged from 50 of 122 (41%) for elevated prostate-specific antigen levels to 2 of 56 (4%) for scrotal lumps; 42 (11%) referrals were inappropriate.
CONCLUSIONS
The overall cancer-detection rate is acceptable. Most inappropriate referrals were for long-standing symptoms and non-specific testicular/scrotal symptoms. The testicular cancer detection rate raises questions about the two-week wait guidelines. Providing general practitioners with fast-track scrotal ultrasound and revising the guideline may reduce the disproportionately high number of patients referred with suspected testicular cancer. Other inappropriate referrals are a cause for concern as they add to the workload of the ‘urgent-referral’ pathway.
Urological cancers (those involving the prostate, testis, penis, urethra, bladder, ureters and kidneys) accounted for 15.4% of all new cancers in England,1 and 12.1% of deaths from cancer,2 in England and Wales, in 2004.
The two-week wait referral guidelines published by the UK Department of Health for suspected urological cancers3 are summarised in Table 1. NHS trusts and SHAs are encouraged to carry out clinical audits of suspected cancer referrals to generate further information.4 There is wide variation among various centres and regions in the concordance of general practitioner (GP) referrals based on these guidelines, and also the rate of cancers detected based on the two-week wait system.
Table 1.
Two-week wait referral guidelines for suspected urological cancers
|
The objectives of this audit were to calculate: (i) the rate of detection of cancers among the two-week wait referrals; (ii) the rate of detection of cancers based on the reason for referral; and (iii) the proportion of inappropriate referrals.
Keywords: Two-week wait, Urological cancer
Patients and Methods
This was a retrospective audit looking at all two-week wait referrals from primary care to the urology department at a 1200-bedded teaching hospital in England, during a 6-month period from April 2006 to September 2006. These data were obtained from the Cancer Network Office. The data were entered into a Microsoft Excel spreadsheet and tabulated based on several parameters including the date of referral, reason for referral, date of first urology out-patient appointment and the final diagnosis. The reason for referral was identified by accessing the letter from the urologist to the GP after the first appointment. All letters are available online from the patient management system on the Trust intranet.
The final diagnosis was identified from imaging and pathology reports, which are available on the Trust intranet. The cancer-detection rate was calculated as the percentage of patients who had confirmed urological cancer, among all the referrals.
Based on the symptoms and reasons for referral, the pick-up rate for cancers specific to a particular organ (prostate, testis, etc.) was identified. Inappropriate referrals were those which did not satisfy the recommended referral criteria, but were referred under the two-week wait system.
Results
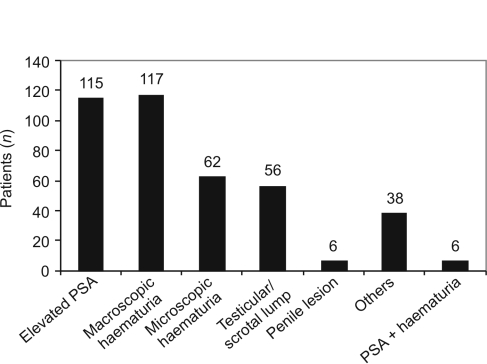
A total of 400 referrals were made for suspected urological cancer under the two-week wait system during the 6-month period. Of these, 326 patients (82%) were males and 74 were females. The age ranged from 16–91 years, with a mean age of 63.2 years. The majority of referrals were for elevated prostate-specific antigen and haematuria. A detailed analysis of the reasons for referral is given in Figure 1.
Figure 1.
Reasons for referral. [PSA, prostate-specific antigen]
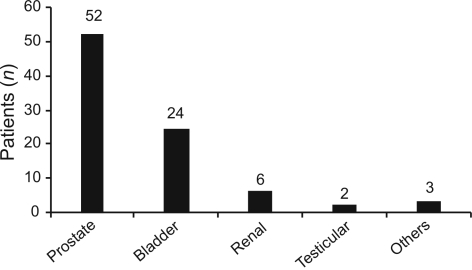
Of the 400 referrals, a final diagnosis of urological cancer was made in 90 patients. Thus, the cancer detection rate is 23%. A detailed analysis of the site of cancer is given in Figure 2.
Figure 2.
Site of origin of cancer.
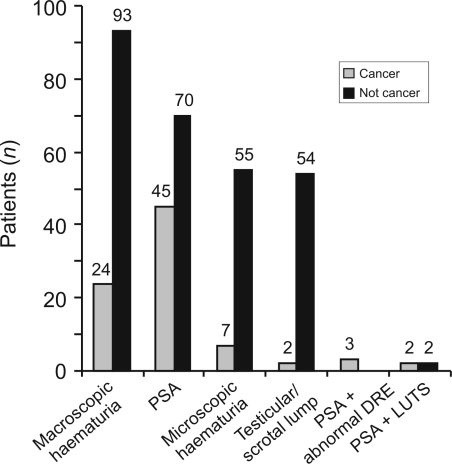
The rate of detection of cancer based on reasons for referral was extremely variable, ranging from 41% for elevated prostate-specific antigen to 4% for testicular/scrotal lumps (Fig. 3). The highest rate of detection based on the reason for referral was for a combination of elevated prostate-specific antigen and an abnormal prostate on digital examination. Three patients were referred with these findings, and all were diagnosed with prostate cancer. Suspected testicular cancer had a very low rate of detection at 4%, with only two of the 56 patients confirmed to have cancer.
Figure 3.
Rate of detection of cancer based on reasons for referral. DRE, digital rectal examination; LUTS, lower urinary tract symptoms.
At least 42 referrals (11% of the total) were considered inappropriate because they did not conform to the two-week wait guidelines. Examples of such referrals are given in Table 2.
Table 2.
Examples of inappropriate referrals
|
Discussion
A systematic review published by the Centre for Reviews and Dissemination, University of York, to assess the implementation and effectiveness of the NHS two-week wait policy identified 16 audits in urology, from which the following results emerged. The cancer detection rates varied from 13% to 40%, and the proportion of inappropriate referrals varied from 0% to 30%.5 The results from our centre fall well within these ranges.
Though the overall cancer-detection rate is acceptable, the rate based on the reason for referral is very variable. The testicular cancer detection rate, in particular, raises many questions about the two-week wait guidelines, and also about whether the guidelines are being misused.
Several studies have been published questioning the usefulness of the two-week wait guidelines. An audit of two-week wait referrals for head and neck cancer at Southmead Hospital in 2002 found a low yield of significant pathology.6 Similarly, an audit from Eastbourne reported that, prior to the implementation of the two-week wait directive, the detection rate of breast cancer was 22% and all cancers were seen within 1 week of referral letter. After the implementation of the two-week wait directive, a re-audit showed that the cancer detection rate had dropped to 19% and only 85% of patients were seen in 2 weeks.7 An audit by Cant et al.8 concluded that the waiting time for ‘urgent’ appointments for suspected breast cancer was unchanged following the two-week wait directive, but there was an increased wait for other patients, especially those assessed as having a lower probability of cancer. The findings of our audit, and of these previous studies, suggest that it may be time to re-visit the concept of the two-week wait system with a view to at least revising the current guidelines.
In the meantime, it is imperative that fresh guidance is issued into the overuse or, in some cases, even abuse of the guidelines, deliberate or not. It is said that, on average, a GP will see one or two testicular cancers during his career. One possible explanation for the apparent over-referral may be to relieve patient anxiety given the constant media publicity on testicular cancer. Second, GPs may not feel confident about their ability to distinguish, reliably, testicular from extra testicular swellings or where the symptoms are simply those of vague scrotal/testicular discomfort with little or nothing to find on examination. The two-week wait route, therefore, not infrequently, is used to get around these diagnostic uncertainties, which from the hospital's point can very easily be resolved with a scrotal ultrasound. In contrast to criteria relating to other cancers, guidelines from the National Institute for Health and Clinical Excellence (NICE) on testicular swellings are much less easy to implement in clinical practice. One way forward would be to provide GPs with a fast-track access to scrotal ultrasound but, even then, some patients may not be satisfied till they have seen a hospital specialist.
Most of the inappropriate referrals were for long-standing symptoms like haematuria with a known benign cause and for non-specific testicular/scrotal symptoms, as discussed above. Three referrals for haematuria and two for elevated prostate-specific antigen were in patients with known prostate cancer. Other reasons (Table 2) included traumatic haematuria, abnormal prostate, chronically elevated prostate-specific antigen and ‘bleeding’ (which turned out to be vaginal from a uterine polyp). This is a cause for concern because these patients can overburden an already stretched two-week wait service, thus compromising the care of those patients who do need to be seen urgently and cannot because of limited resources. A total of 71,593 patients were referred under the two-week wait system with suspected urological cancer in England in the year 2006–2007.10 One way to address this issue would be to ensure stricter implementation of the two-week wait guidelines. Consultants should have the choice to refuse to see inappropriate referrals within 2 weeks, and to act on such referrals as routine, making sure that the care of the patient is not compromised.
References
- 1.Office for National Statistics. Cancer statistics registrations: registrations of cancer diagnosed in 2004, England. London: Office for National Statistics; Series MB1 no. 35. [Google Scholar]
- 2.Office for National Statistics. Mortality statistics: review of the Registrar General on deaths by cause, sex and age, in England and Wales. London: Office for National Statistics; 2004. Series DH2 no. 31. [Google Scholar]
- 3.Department of Health. Referral Guidelines for Suspected Cancer. < http://www.doh.gov.uk/cancer>.
- 4.NHS Executive. Cancer information strategy. London: Department of Health; 2000. [Google Scholar]
- 5.Lewis R, Collins R, Flynn A, Dean ME, Myers L, et al. A systematic review of cancer waiting time audits. Qual Saf Health Care. 2005;14:62–6. doi: 10.1136/qshc.2004.013359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams RW, Hughes W, Felmingham S, Irvine GH. An audit of two week wait referrals for head and neck cancer. Ann R Coll Surg Engl (Suppl) 2002;84:304–6. [Google Scholar]
- 7.Khawaja AR, Allan SM. Has the breast cancer two week wait guarantee for assessment made any difference? Eur J Surg Oncol. 2000;26:536–9. doi: 10.1053/ejso.2000.0942. [DOI] [PubMed] [Google Scholar]
- 8.Cant PJ, Yu DSL. Impact of the two week wait directive for suspected cancer on service provision in a symptomatic breast clinic. Br J Surg. 2000;87:6–1082. doi: 10.1046/j.1365-2168.2000.01551.x. [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Health and Clinical Excellence. Referral guidelines for suspected cancer. London: NICE; 2005. Clinical Guideline 27; p. 30. [Google Scholar]
- 10. < http://www.performance.doh.gov.uk/cancerwaits/index.htm>.