Abstract
Glucose-6-phosphate dehydrogenase (G6PD) deficiency is the most common enzymatic disorder of red blood cells in humans. It is estimated that about 400 million people are affected by this deficiency.1 The G6PD enzyme catalyzes the first step in the pentose phosphate pathway, leading to antioxidants that protect cells against oxidative damage.2 A G6PD-deficient patient, therefore, lacks the ability to protect red blood cells against oxidative stresses from certain drugs, metabolic conditions, infections, and ingestion of fava beans.3 The following is a literature review, including disease background, pathophysiology, and clinical implications, to help guide the clinician in management of the G6PD-deficient patient. A literature search was conducted in the following databases: PubMed, The Cochrane Library, Web of Science, OMIM, and Google; this was supplemented by a search for selected authors. Keywords used were glucose-6-phosphate dehydrogenase (G6PD) deficiency, anesthesia, analgesia, anxiolysis, management, favism, hemolytic anemia, benzodiazepines, codeine, codeine derivatives, ketamine, barbiturates, propofol, opioids, fentanyl, and inhalation anesthetics. Based on titles and abstracts, 23 papers and 1 website were identified. The highest prevalence of G6PD is reported in Africa, southern Europe, the Middle East, Southeast Asia, and the central and southern Pacific islands; however, G6PD deficiency has now migrated to become a worldwide disease. Numerous drugs, infections, and metabolic conditions have been shown to cause acute hemolysis of red blood cells in the G6PD-deficient patient, with the rare need for blood transfusion. Benzodiazepines, codeine/codeine derivatives, propofol, fentanyl, and ketamine were not found to cause hemolytic crises in the G6PD-deficient patient. The most effective management strategy is to prevent hemolysis by avoiding oxidative stressors. Thus, management for pain and anxiety should include medications that are safe and have not been shown to cause hemolytic crises, such as benzodiazepines, codeine/codeine derviatives, propofol, fentanyl, and ketamine. The authors of this article make 5 particular recommendations: (1) Anyone suspected of G6PD deficiency should be screened; (2) exposure to oxidative stressors in these individuals should be avoided; (3) these patients should be informed of risks along with signs and symptoms of an acute hemolytic crisis; (4) the clinician should be able to identify both laboratory and clinical signs of hemolysis; and finally, (5) if an acute hemolytic crisis is identified, the patient should be admitted for close observation and care.
Keywords: Glucose-6-phosphate dehydrogenase, G6PD, Blood disease, Blood deficiency, G6PD deficiency, G6PD management, Favism, Hemolysis, Hemolytic crisis, Anemia
Glucose-6-phosphate dehydrogenase (G6PD) deficiency is the most common enzymatic disorder of red blood cells in humans. It is estimated that about 400 million people are affected by this deficiency.1 The G6PD enzyme catalyzes the first step in the pentose phosphate pathway, leading to antioxidants that protect cells against oxidative damage.2 A G6PD-deficient patient, therefore, lacks the ability to protect red blood cells against oxidative stresses from certain drugs, infections, metabolic conditions, and ingestion of fava beans.3 The following is a literature review, including disease background, pathophysiology, and clinical implications, to help guide the clinician in management of the G6PD-deficient patient.
METHODS
A literature search was conducted in the following databases: PubMed, The Cochrane Library, Web of Science, OMIM, and Google; this was supplemented by a search for selected authors. Keywords used were glucose-6-phosphate dehydrogenase (G6PD) deficiency, anesthesia, analgesia, anxiolysis, management, favism, hemolytic anemia, benzodiazepines, codeine, codeine derivatives, ketamine, barbiturates, propofol, opioids, fentanyl, and inhalation anesthetics. Based on titles and abstracts, 23 papers and 1 website were identified. Pertinent data were then extrapolated from these papers to meet the objectives of this literature review: (1) disease background, (2) pathophysiology, and (3) clinical implications to help guide the clinician in management of the G6PD-deficient patient.
BACKGROUND
It is estimated that about 400 million people are affected by glucose-6-phosphate dehydrogenase (G6PD) deficiency.1 The highest prevalence of G6PD is reported in Africa, southern Europe, the Middle East, southeast Asia, and the central and southern Pacific islands; however, because of migration, deficient alleles are quite prevalent in North and South America and in parts of northern Europe.4
The deficiency is an X-linked hereditary genetic defect caused by mutations in the G6PD gene. The inheritance of G6PD deficiency shows a typical X-linked pattern with higher incidence in males than in females.3
Over the past several decades, with advances in the field of genetics, testing for G6PD deficiency has become feasible. Screening for this disorder has become more important owing to its clinical implications.
PATHOPHYSIOLOGY
Glucose-6-phosphate dehydrogenase (G6PD) deficiency is known to provide protection against malaria, particularly the form of malaria caused by Plasmodium falciparum, the deadliest form.2,3 Areas endemic to malaria usually have more individuals with the deficiency, possibly because of an evolutionary advantage.
Glucose-6-phosphate dehydrogenase (G6PD) is an enzyme that catalyzes the first step in the pentose phosphate pathway (Figure 1). The pentose phosphate pathway (PPP) includes converting glucose to ribose-5-phosphate, a precursor to RNA, DNA, ATP, CoA, NAD, and FAD. The pathway also includes the creation of NADPH, which provides the reducing energy of the cell by maintaining the reduced glutathione within the cell. Reduced glutathione functions as an antioxidant and protects cells against oxidative damage.2
Figure 1.

The hexose monophosphate shunt.
Most cells have a backup system of other metabolic pathways that can generate the intracellular NADPH necessary. On the other hand, red blood cells do not have the “other NADPH producers.” Therefore, G6PD deficiency becomes especially lethal in red blood cells, where any oxidative stress will result in hemolytic anemia. Oxidative stresses can arise from numerous things, such as consumption of fava beans, certain drugs, infections, and certain metabolic conditions like diabetic ketoacidosis.3
The oxidative denaturation of hemoglobin results in puddling of hemoglobin, and bite or hemiblister cells appear in the peripheral smear, as illustrated in Figure 2. In this figure, one is able to visualize denatured hemoglobin precipitates, also known as “Heinz bodies.” This can be differentiated from a normal peripheral blood smear, which depicts red blood cells that are uniform in size and shape (Figure 3).
Figure 2.
Peripheral smear from a patient with Heinz body hemolytic anemia. Heinz body preparation reveals the denatured hemoglobin precipitates. (© 2007 Rector and Visitors of the University of Virginia Charles E. Hess, M.D., and Lindsey Krstic, B.A.)
Figure 3.
High-power view of a normal peripheral blood smear. The red cells are of relatively uniform size and shape. A lymphocyte can also be seen. The diameter of the normal red cell should approximate that of the nucleus of the small lymphocyte. (© 2007 Rector and Visitors of the University of Virginia Charles E. Hess, M.D., and Lindsey Krstic, B.A.)
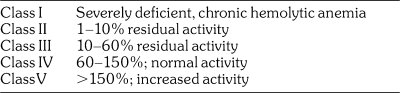
The World Health Organization has classified the different G6PD variants according to the magnitude of the enzyme deficiency and the severity of hemolysis (Table 1).3–5 Class I variants have severe enzyme deficiency (less than 10% of normal) and have chronic hemolytic anemia. Class II variants also have severe enzyme deficiency, but there is usually only intermittent hemolysis. Class III variants have moderate enzyme deficiency (10 to 60% of normal) with intermittent hemolysis, usually associated with infection or drugs. Class IV variants have no enzyme deficiency or hemolysis. Class V variants have increased enzyme activity. Classes IV and V are of no clinical significance.
Table 1.
Classes of G6PD Deficiency
CLINICAL IMPLICATIONS
Every health care provider has to be cautious in managing the G6PD-deficient patient. As was mentioned before, ingestion of fava beans, certain drugs, infections, and metabolic conditions can cause hemolysis. Inadequate management of those G6PD-deficient individuals who develop acute hemolytic anemia can lead to permanent neurologic damage or death.
First of all, a number of drugs, as listed in Table 2,3,5,6 can precipitate hemolysis in G6PD-deficient subjects. These drugs can interact with hemoglobin and oxygen, leading to the intracellular formation of hydrogen peroxide (H2O2) and other oxidizing radicals. As these oxidants accumulate within enzyme-deficient cells, hemoglobin and other proteins are oxidized, leading to loss of function and cell death.3,5–7
Table 2.
Drugs and Chemicals Associated With Hemolysis in G6PD Deficiency
Altikat et al.8 studied the effects of certain anesthetic agents such as halothane, isoflurane, ketamine, sevoflurane, prilocaine, diazepam, and midazolam on enzymatic activity of G6PD. They found that although isoflurane, sevoflurane, diazepam, and midazolam had an inhibitory effect on G6PD activity in vitro, halothane, ketamine, and prilocaine had none. On the other hand, no documented cases were found to show that benzodiazepines, codeine/codeine derivatives, propofol, fentanyl, or ketamine can cause hemolytic crisis in the G6PD-deficient patient in vivo.
Nevertheless, hemolytic crises induced by inhalational general anesthetic agents are still being studied, especially because some authors have vaguely related G6PD deficiency to malignant hyperthermia.9 Clearly, not enough research has been done to study the effects of inhalational anesthetic agents on the G6PD-deficient patient.
Of important note, methylene blue is ineffective in patients with G6PD deficiency who may require exchange or hyperbaric therapy, because these patients lack the ability to return hemoglobin to the ferrous form.10 Therefore, drugs such as benzocaine, lidocaine, articaine, prilocaine, and silver nitrate, which are known to induce methemoglobinemia, should also be avoided.11
Infection is probably the most common factor inciting hemolysis in G6PD-deficient subjects.12,13 In one study, for example, an abrupt fall in hemoglobin concentration occurred in approximately 20% of G6PD-deficient subjects with pneumonia.12 A variety of other infectious agents, including Escherichia coli,12 rickettsiae,14 viral hepatitis,15–21 dental caries,16 salmonella,17–19 and beta-hemolytic streptococci,20 have been implicated. Quereshy et al.16 describe a case of a G6PD-deficient patient who developed hemolytic anemia secondary to a maxillofacial infection due to a grossly carious tooth.
The factors responsible for accelerated destruction of G6PD-deficient red cells during infection are not known. One possible explanation is that the red cells are damaged by oxidants generated by phagocytosing macrophages—a mechanism similar to that seen with drug-induced hemolysis.20,21,22
Certain metabolic conditions, such as diabetic ketoacidosis, also appear to be capable of triggering destruction of G6PD-deficient red cells.6,13 Both acidosis and hyperglycemia are potential precipitating factors,23 and correction of the abnormalities is associated with reversal of the hemolytic process. In some diabetic patients, occult infection may be a common trigger for inducing both acute hemolysis and ketoacidosis.
Postoperatively, the G6PD-deficient patient can present certain clinical manifestations that may trigger the need for additional support or treatment. In general, hemolysis is seen 1 to 3 days after contact with triggering factors. Acute hemolysis is self-limited, but in rare instances it can be severe enough to warrant a blood transfusion.24 The patient may develop cyanosis, headache, fatigue, tachycardia, dyspnea, lethargy, lumbar/substernal pain, abdominal pain, splenomegaly, hemoglobinuria, and/or scleral icterus.3,23,25 Also, the breakdown products of hemoglobin will accumulate in the blood, causing jaundice, and they can be excreted in the urine, causing dark brown discoloration.3
Peripheral blood smear microscopy might include fragments of red blood cell “schistocytes” and reticulocytes. Denatured hemoglobin inclusions within the red blood cells are known as Heinz bodies. Lactate dehydrogenase (LDH) will be elevated in blood. Unconjugated bilirubin in the blood is elevated, leading to jaundice. Haptoglobin levels are decreased. The direct Coombs test is positive, if hemolysis is caused by an immune process. However, because hemolysis in G6PD deficiency is not an immune process, the direct Coombs result should be negative. Hemosiderin in the urine indicates chronic intravascular hemolysis. Urobilinogen is also present in the urine.
Grant E. Sklar described a case in which a G6PD-deficient patient experienced a decrease in hemoglobin concentration of almost 4 g/dL and an increase in unconjugated bilirubin consistent with the development of hemolysis secondary to acetaminophen overdose.24 On the contrary, according to a more recent article in Lancet, the association between acetaminophen and hemolysis in the G6PD-deficient patient is doubtful.3
General anesthesia typically masks the immediate signs of hemolysis, making it difficult to identify a hemolytic crisis while the patient is asleep. Even hypotension, which could be a result of hemolysis, may be attributed to other causes in an anesthetized patient. The appearance of free hemoglobin in plasma or urine is presumptive evidence of a hemolytic reaction. Treatment consists of discontinuation of the offending agent and maintenance of urine output by infusion of crystalloid solutions and diuretics such as mannitol and/or furesomide.25
Contrary to the difficulty in determining a hemolytic crisis while the patient is under general anesthesia, clinical signs and symptoms are a bit more obvious. Clinical signs and symptoms of hemolysis typically arise within 24 to 72 hours of drug dosing, and anemia worsens until about day 7.3 This makes it difficult for the health practitioner to identify a hemolytic crisis in patients who undergo outpatient or short hospital stay (less than 24 hour) procedures. Therefore, the practitioner should inform the high-risk patient and his or her caretaker to look for signs and symptoms of a hemolytic crisis (cyanosis, headache, dyspnea, fatigue, lumbar/substernal pain, jaundice, scleral icterus, dark urine). A simple postoperative phone call to check on the patient prior to the follow-up appointment could be important to his or her health. It is believed that after removal of the offending hemolytic agent, hemoglobin concentrations begin to recover after 8 to 10 days; thus, rarely (except in children) does acute hemolysis lead to severe anemia requiring a blood transfusion.3
The most important management strategy is to prevent a hemolytic crisis in the first place by avoiding the oxidative stressors.3 Fortunately, acute hemolysis in G6PD-deficient adults is short-lived and usually does not require specific treatment.3 However, in the event of a hemolytic crisis, the offending agent should be removed, and the patient should be monitored closely. Table 3 summarizes the laboratory test findings in patients with acute hemolysis.3,21 At minimum, a daily complete blood count should be followed to monitor the need for a blood transfusion.
Table 3.
Laboratory Evaluation in Patients With Acute Hemolysis
SUMMARY
The most effective management strategy is to prevent hemolysis by avoiding oxidative stressors. Therefore, management for pain and anxiety should include medications that are safe and have not been shown to cause hemolytic crises, such as benzodiazepines, codeine/codeine derviatives, propofol, fentanyl, and ketamine.
In conclusion, the authors of this article make 5 particular recommendations. First, anyone suspected of G6PD deficiency, with a family history of the disorder, a history of hemolysis, and/or of African, southern European, Middle Eastern, southeast Asian, or central and southern Pacific Island descent, should be screened for G6PD deficiency. Second, exposure to oxidative drugs and ingestion of fava beans in the G6PD-deficient patient should be avoided. Third, clinicians should inform high-risk patients of any risk for hemolysis, along with signs and symptoms of an acute hemolytic crisis. These signs and symptoms should include cyanosis, headache, dyspnea, fatigue, lumbar/substernal pain, jaundice, scleral icterus, and dark urine. Fourth, in the event of a hemolytic crisis, the clinician should be able to identify both laboratory and clinical signs. Laboratory signs include anemia on complete blood count, Heinz bodies on peripheral smear, decreased haptoglobin, elevated bilirubin, urobilinogen, and elevated lactate dehydrogenase. Clinical signs include headache, dyspnea, fatigue, lumbar/substernal pain, jaundice, scleral icterus, and dark urine. The health care provider should also know that laboratory signs may precede the clinical signs, which usually appear 24 to 72 hours after exposure to the offending agent. Fifth, if an acute hemolytic crisis is identified, the patient should be admitted for close observation to include, at minimum, a daily complete blood count to monitor the need for a blood transfusion.
REFERENCES
- Glader B.E. Wintrobe's Clinical Hematology. 10th ed. Baltimore: Williams & Wilkins; 2008. Glucose-6-phosphate dehydrogenase deficiency and related disorders of hexose monophosphate shunt and glutathione metabolism; pp. 1176–1190. [Google Scholar]
- Luzzatto L, Metha A, Vulliany T. Glucose-6-phosphate dehydrogenase deficiency. In: Scriver C.R, Beaudet A.L, Sly W.S, et al., editors. The Metabolic and Molecular Basis of Inherited Disease. 8th ed. Columbus: McGraw-Hill; 2001. pp. 4517–4553. [Google Scholar]
- Cappellini M.D, Fiorelli G. Glucose-6-phosphate dehydrogenase deficiency. Lancet. 2008;371:64–74. doi: 10.1016/S0140-6736(08)60073-2. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Working group glucose-6-phosphate dehydrogenase deficiency. Bull WHO. 1989;67:601–611. [PMC free article] [PubMed] [Google Scholar]
- Beutler E. The Molecular biology of enzymes of erythrocyte metabolism. In: Stamatoyannopoulos G, Nienhus A.W, Majerus P.W, et al., editors. The Molecular Basis of Blood Disease. Philadelphia: WB Saunders; 1993. [Google Scholar]
- Beutler E. G6PD deficiency. Blood. 1994;84:3613–3636. [PubMed] [Google Scholar]
- G6PD Deficiency Favism Association. Associazione Italiana Favismo. Unsafe to take. 2009. Available at: http://www.g6pd.org/favism/english/index.mv. Accessed March 7, 2009.
- Altikat S, Ciftci M, Buyukokuroglu M.E. In vitro effects of some anesthetic drugs on enzymatic activity of human red blood cell glucose-6-phosphate dehydrogenase. Polish J Pharmacol. 2002;54:67–71. [PubMed] [Google Scholar]
- Basora M, Villaonga A, Ayuso M.A. Glucose-6-phosphate dehydrogenase deficiency: anesthetic implications. Rev Esp Anesthesiol Reanim. 1990;37:380. [PubMed] [Google Scholar]
- Srikanth M.S, Kahlstrom R, Oh K.H, et al. Topical benzocaine (hurricaine) induced methemoglobinemia during endoscopic procedures in gastric bypass patients. Obes Surg. 2005;15:584–590. doi: 10.1381/0960892053723376. [DOI] [PubMed] [Google Scholar]
- Hegedus F, Herb K. Benzocaine-induced methemoglobinemia. Anesth Prog. 2005;52:136–139. doi: 10.2344/0003-3006(2005)52[136:BM]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burka E.R, Weaver Z, III, Marks P.A. Clinical spectrum of hemolytic anemia associated with glucose-6-phosphate dehydrogenase deficiency. Ann Intern Med. 1966;64:817. doi: 10.7326/0003-4819-64-4-817. [DOI] [PubMed] [Google Scholar]
- Shannon K, Buchanan G.R. Severe hemolytic anemia in black children with glucose-6-phosphate dehydrogenase deficiency. Pediatrics. 1982;70:364–369. [PubMed] [Google Scholar]
- Whelton A, Donadio J.V, Jr, Elisberg B.L. Acute renal failure complicating rickettsial infections in glucose-6-phosphate dehydrogenase–deficient individuals. Ann Intern Med. 1968;69:323–328. doi: 10.7326/0003-4819-69-2-323. [DOI] [PubMed] [Google Scholar]
- Phillips S.M, Silvers N.P. Glucose-phosphate dehydrogenase deficiency, infectious hepatitis, acute hemolysis, and renal failure. Ann Intern Med. 1969;70:99–104. doi: 10.7326/0003-4819-70-1-99. [DOI] [PubMed] [Google Scholar]
- Quereshy F.A, Gold E.S, Powers M.P. Hemolytic anemia in a glucose-6-phosphate dehydrogenase–deficient patient triggered by a maxillofacial infection. J Oral Maxillofac Surg. 2000;58:805–807. doi: 10.1053/joms.2000.7273. [DOI] [PubMed] [Google Scholar]
- Chan T.K, Chesterman C.N, McFadzean A.J, et al. The survival of glucose-6-phosphate dehydrogenase–deficient erythrocytes in patients with typhoid fever on chloramphenicol therapy. J Lab Clin Med. 1971;77:177–184. [PubMed] [Google Scholar]
- Constantopoulos A, Economopoulos P, Kandylas J. Fulminant diarrhea and acute hemolysis due to G-6-PD deficiency in salmonellosis. Lancet. 1973;1:1522. doi: 10.1016/s0140-6736(73)91871-0. [DOI] [PubMed] [Google Scholar]
- Hersko C, Vardy P.A. Haemolysis in typhoid fever in children with G-6-PD deficiency. Br Med J. 1967;1:214–215. doi: 10.1136/bmj.1.5534.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mengel C.E, Metz E, Yancey W.S. Anemia during acute infections: role of glucose-6-phosphate dehydrogenase deficiency in Negroes. Arch Intern Med. 1967;119:287–290. doi: 10.1001/archinte.119.3.287. [DOI] [PubMed] [Google Scholar]
- Salen G, Goldstein F, Harrani F, et al. Acute hemolytic anemia complicating viral hepatitis in patients with glucose-6-phosphate dehydrogenase deficiency. Ann Intern Med. 1966;65:1210–1220. doi: 10.7326/0003-4819-65-6-1210. [DOI] [PubMed] [Google Scholar]
- Baehner R.L, Nathan D.G, Castle W.B. Oxidant injury of Caucasian glucose-6-phosphate dehydrogenase–deficient red blood cells by phagocytosing leukocytes during infection. J Clin Invest. 1971;50:2466–2473. doi: 10.1172/JCI106747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards C.Q. Anemia and the liver: hepatobiliary manifestations of anemia. Clin Liver Dis. 2002;6:891–907. doi: 10.1016/s1089-3261(02)00050-8. [DOI] [PubMed] [Google Scholar]
- Sklar G.E. Hemolysis as a potential complication of acetaminophen overdose in a patient with glucose-6-phosphate dehydrogenase deficiency. Pharmacotherapy. 2002;22:656–658. doi: 10.1592/phco.22.8.656.33216. [DOI] [PubMed] [Google Scholar]
- Stoelting R.K, Miller R.D. Basics of Anesthesia. 5th ed. Philadelphia: Churchill Livingstone; 2007. p. 361. [Google Scholar]