Abstract
This study compared the effectiveness of topical benzocaine 20% versus a combination of lidocaine, tetracaine, and phenylephrine in providing sufficient analgesia for the placement of orthodontic temporary anchorage devices (TADs). The 2 topical anesthetics were tested against each other bilaterally using a randomized, double-blind, crossover design. The agents were left in place for the amount of time prescribed by the manufacturer. The TAD was then placed, and each subject rated the degree of pain on a Heft-Parker visual analogue scale. A pulse oximeter was used to record the preoperative and postoperative pulse rates. Statistically significant differences in perceived pain (P < .05) and success rate (P < .01) between drugs were seen, but no significant difference in pulse rate change between the topical anesthetics was observed (P > .05). It was concluded that when the efficacy of topical benzocaine and of a combination product was compared as the sole anesthetic to facilitate acceptable pain control for placement of orthodontic temporary anchorage devices, the combination product was considerably more efficacious.
Keywords: Orthodontic temporary anchorage devices, Topical anesthesia, Topical anesthetics, Lidocaine, Tetracaine, Benzocaine, Phenylephrine
Anchorage control is fundamental to successful orthodontic treatment. Miniscrews, or orthodontic temporary anchorage devices (TADs), have recently emerged as an increasingly more common means of providing the orthodontist with intraoral absolute anchorage. TADs are able to be loaded immediately following placement, can be placed quickly and efficiently, do not require a mucoperiosteal flap for placement or removal, and can be placed by the orthodontist.1–4
Topical anesthesia has been shown to reduce the discomfort of local anesthetic injections5–13 and some intraoral operative procedures, including periodontal scaling and root planing,14,15 gingival manipulation,16,17 biopsy,18,19 dentinal/pulpal anesthesia,20 and dental extractions.21 Topical anesthetics have been shown not only to reduce the perception of pain, but to reduce patient anxiety22,23 and the possibility of needle-stick injuries. The potential of sufficient analgesia from topical anesthetics for orthodontic temporary anchorage placement has been suggested in the literature4,24 and would offer a major advantage to the clinician and the patient; however, no studies to date have been performed to compare topical anesthetic agents for this purpose.
The goal of this research project was to determine the comparative efficacy of 2 topical anesthetics for the placement of orthodontic TADs, thus giving the clinician an efficient, nonpainful technique for TAD placement, while providing minimal psychological and physiologic stress to the patient.
METHODS
Seventeen adolescent and adult subjects, 8 males and 9 females aged 12 to 76 years, who were patients of record at the University of Texas Health Science Center at Houston Dental Branch Orthodontic Clinic and required TAD placement bilaterally for space closure, space maintenance, or intrusion or extrusion of teeth were included in this double-blind, prospective study. Exclusion criteria included allergy or other contraindication to any study medication, inability to consent to participation in the study, use of analgesics prior to the procedure, history of cardiovascular disease, and any contraindication to the use of TADs. The University of Texas Health Science Center at Houston Human Subjects Committee approved this study as protocol HSC-DB-07-0006, and written informed consent was obtained from each subject and, if applicable, the subject's guardian.
A random number table was used to determine which topical anesthetic was to be used first on each subject for the open-label study. The second anchor was placed after a washout period of at least 5 days, and the comparator drug utilized at the second visit.
TADs used were the Quattro temporary anchorage devices from the Mondeal Orthodontic Anchorage System (GAC International Inc, Bohemia, NY). Quattro temporary anchorage devices are self-drilling, self-tapping, polished titanium screws with a tube and slot on the head, which allow for 3-dimensional edgewise control. The threaded portion of the TAD is 1.5 mm in diameter and 7 mm in length (Figure 1). Placement of the anchor is initiated in the mucosa by simply inserting the TAD through the gingival or alveolar mucosa to the periosteum, using a manual driver. All TADs were placed by the same, blinded orthodontist.
Figure 1.
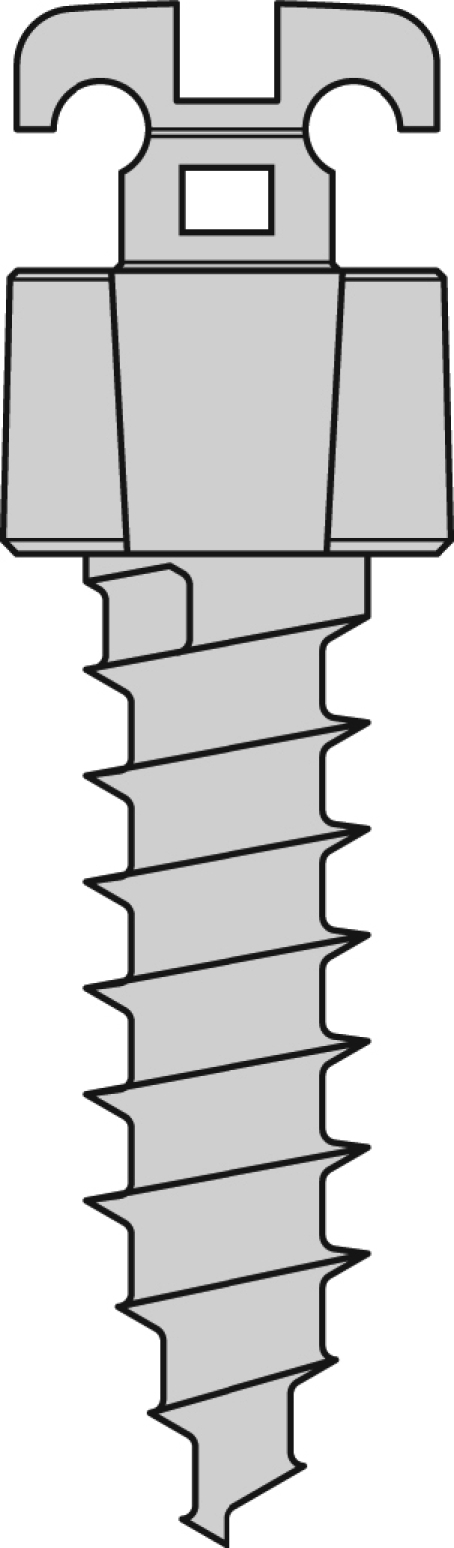
Diagram of Quattro temporary intraosseous orthodontic anchorage device (GAC International Inc) (enlargement approximately 13×).
Prior to placement of the TADs, a preoperative pulse rate was determined with a pulse oximeter (Comfort Cuff 506N3, Criticare Systems Inc, Waukesha, Wis) after the subject was allowed to sit in the dental chair for 10 minutes. Subjects were familiarized with the use of a Heft-Parker visual analogue scale25 (VAS) pain assessment instrument at the placement appointment. A baseline VAS score was taken preoperatively to quantitatively ensure that subjects were not in pain prior to the procedure, and to obtain information on the comparability/consistency of pain evaluations across the 2 groups. Pulse rate was continuously monitored for 30 minutes, because discomfort-related tachycardia will likely occur very early upon or shortly after beginning the TAD placement procedure.
The TAD placement site was marked with an intraoral dye marker. One of the 2 study drugs—20% benzocaine gel (HurriCaine Topical Anesthetic GEL, Beutlich LP Pharmaceuticals, Waukegan, Ill) or a combination product containing lidocaine 20%, tetracaine 4%, and phenylephrine 2% (TAC 20% Alternate Topical Anesthetic Gel Thick, Professional Arts Pharmacy, Lafayette, La)—was applied on the attached gingiva or alveolar mucosa overlying the intended anchorage site using a cotton-tipped applicator and was allowed to remain in contact with the tissue for the amount of time prescribed by the manufacturer (1.0 and 2.5 minutes, respectively). To blind the subject, goggles were placed over the patient's eyes while the anesthetic was applied. Placement of the TAD was then accomplished by a different orthodontist, who did not know which topical anesthetic preparation was utilized. All TADs were placed by the same, blinded orthodontist. The maximum postoperative pulse rate in beats per minute (BPM) observed within 30 minutes was recorded to be used in the experimental comparison with preoperative values. Subjects rated the pain of TAD placement on the postoperative VAS immediately after each placement procedure was completed. VAS and pulse rate data were analyzed by a blinded, independent evaluator.
In the event the subject did not tolerate placement of the orthodontic temporary anchorage device because of pain greater than mild at any time, the procedure was interrupted, the subject completed the VAS form, and the study drug was rated as a failure. A standard amide local anesthetic (2% lidocaine with 1 ∶ 100,000 epinephrine) was then injected by infiltration, and the TAD placed. Subjects were monitored in the postoperative period for 1 day for the occurrence of pain and/or other complications, and appropriate analgesics and/or other interventions were provided as necessary.
Age, gender, study drug, preoperative and postoperative VAS scores, preoperative pulse rate in BPM, and maximum postoperative pulse rate in BPM data were recorded, and descriptive statistics calculated for each variable. The difference between maximum postoperative and preoperative pulse rates was calculated, as was the difference divided by the preoperative pulse rate (percent pulse rate change). A paired t test was utilized to compare the 2 study drugs from the subjects (n = 17) in which 2 TADs were placed—1 with each study drug for both VAS and percent pulse rate change. A Pearson chi-square test was utilized to compare the success rates of the 2 study drugs. The statistical significance level was set at P < .05.
RESULTS
Seventeen subjects, 8 males and 9 females aged 12 to 76 years, had TADs placed bilaterally, 1 with each study drug for a total of 34 study drug applications, 17 for each study drug. Subject demographics are shown in Table 1.
Table 1.
Subject Demographics
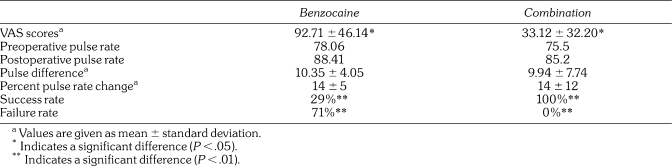
Table 2 shows the mean VAS, preoperative and postoperative pulse rates, pulse difference, percent pulse rate change, and percent success and failure for the benzocaine and combination topical groups.
Table 2.
Mean VAS Scores, Preoperative and Postoperative Pulse Rates, Pulse Difference and Percent Pulse Rate Change, and Success and Failure Rates of Benzocaine and a Combination of Lidocaine, Tetracaine, and Phenylephrine
A lower rating on the VAS score signifies less pain perception. The mean pain rating for the benzocaine group was 92.71 ± 46.14 SD. The mean pain rating for the TAC group was 33.12 ± 32.20 SD. The paired t test demonstrated a significant difference (P < .05) in perceived pain values between anesthetic groups. The combination topical group had significantly lower perceived pain values than the benzocaine group.
A smaller percent change signifies a smaller physiologic response to the experimental stimulus. The mean percent pulse rate change in the benzocaine group was 14 ± 5 SD, and for the combination topical group, the mean percent pulse rate change was 14 ± 12 SD. The paired t test did not indicate a significant difference (P > .05) between groups for percent pulse rate change. No adverse events were observed in either group.
The Pearson chi-square analysis demonstrated a significant difference (P < .01) between groups for success rate, with TAC exhibiting a significantly higher success rate than benzocaine.
The independent t test demonstrated no difference (P > .05) in pain rating or percent pulse rate change between genders. Pearson correlation demonstrated no correlation (P > .05) between age and pain rating or percent pulse rate change.
DISCUSSION
Results of this study indicate that the placement of orthodontic temporary anchorage devices is well tolerated when a combination topical anesthetic is used. The 100% success rate and the significantly (P < .05) lower pain rating for the TAC group, compared with only a 29% success rate and higher pain ratings for the benzocaine group, indicate that subjects experienced less pain when TAC was used instead of benzocaine. However, the lack of a significant difference (P > .05) in percent pulse rate change suggests that the difference in pain levels experienced was not dramatic enough to elicit a different physiologic response.
This apparent anomaly could be due to the fact that benzocaine was rated as a failure 71% of the time, and this occurred most often shortly after the procedure began. Therefore, as dictated by protocol, the procedure was interrupted, 2% lidocaine with 1 ∶ 100,000 epinephrine was infiltrated, and the TAD was placed. We suspect that if the procedure had been completed without the infiltration of anesthetic, a marked increase in pulse rate could have occurred, and a significant difference in pulse rate change between study drug groups might have been observed.
The difference in success rates and pain ratings between TAC and benzocaine could be anticipated owing to the presence of both an ester (tetracaine) and an amide (lidocaine) anesthetic as well as a vasoconstrictor (phenylephrine) in TAC. Several studies have been performed to compare mixtures of topical anesthetics, most commonly EMLA (2.5% lidocaine and 2.5% prilocaine), versus single anesthetic agents. Both McMillan et al.16 and Donaldson and Meechan17 found EMLA to be a more effective topical anesthetic agent than 5% lidocaine gel for minor manipulations of the gingiva. Tulga and Mutlu,7 on the other hand, found 20% benzocaine gel to be more effective than EMLA cream in reducing intraoral injection pain; although it was the authors' perception that the chocolate flavor of the benzocaine gel used impressed the patients, who were composed entirely of 120 children aged 10 to 15 years, compared with the unpleasant taste of the EMLA cream.7
Although generally regarded as equivalent in efficacy to 20% benzocaine, 5% lidocaine was not evaluated in the present study.
The low success rate of benzocaine could be due to the location of the TAD placement. Nakanishi et al.12 found that when topical anesthetic was applied in the mucobuccal fold of the anterior mandible, a reduction in pain from needle insertion resulted, although no difference from placebo was found when it was applied in the pterygotemporal depression. Nusstein and Beck13 similarly reported that 20% benzocaine lacked effectiveness in reducing pain from needle insertion in the pterygomandibular raphe for an inferior alveolar nerve block, as well as over the maxillary first molars, even though benzocaine was beneficial in reducing needle insertion pain over the maxillary lateral incisors.
Meechan6 emphasized that the importance of location in determining topical anesthetic efficacy related to factors such as tissue type (e.g., keratinized vs nonkeratinized mucosa) and the depth at which the noxious event occurs (e.g., superficial infiltration vs a deeper regional block). Therefore, benzocaine might have a higher success rate if used prior to TAD placement in areas of thin, nonkeratinized mucosa, or in the mucobuccal fold of the anterior mandible or maxilla.
For this study, all TADs were placed in the attached or unattached buccal mucosa of the maxilla or mandible, but information on mucosal type, thickness, and specific location was not collected. For this reason, future research is needed to determine whether the efficacy of topical anesthetic agents for TAD placement is related to tissue type, thickness, or location of placement.
Although anesthesia of the periosteum and cortical bone is not predictable with topical anesthetics, the brevity of the temporary anchorage device placement technique may have minimized discomfort resulting from stimulation of these tissues. Therefore, future research is needed to compare the use of TAC topical anesthetic versus traditional injection anesthesia for TAD placement. Safety issues related to combination topical anesthetics also require further investigation.26 The 100% success rate of TAC topical anesthetic may not be observed with a larger population owing to variations in TAD placement location, topical anesthetic application time, and interoperator variability.
The use of a topical anesthetic as the sole means of analgesia for placement of orthodontic temporary anchorage devices has been demonstrated, and TAC was shown to significantly (P < .05) decrease pain ratings when compared with 20% benzocaine, and to have a significantly (P < .01) higher success rate (100%) compared with benzocaine (29%). When the efficacy of topical benzocaine is compared with that of TAC as the sole anesthetic to facilitate acceptable pain control for placement of orthodontic temporary anchorage devices, TAC was found to be more efficacious.
Acknowledgments
The authors are grateful to Criticare Systems Inc, for the use of the pulse oximeter described in this study.
REFERENCES
- Costa A, Raffainl M, Melsen B. Miniscrews as orthodontic anchorage: a preliminary report. Int J Adult Orthodon Orthognath Surg. 1998;13:201–209. [PubMed] [Google Scholar]
- Kanomi R. Mini-implant for orthodontic anchorage. J Clin Orthod. 1997;31:763–767. [PubMed] [Google Scholar]
- Kuroda S, Sugawara Y, Deguchi T, Kyung H.M, Takano-Yamamoto T. Clinical use of miniscrew implants as orthodontic anchorage: success rates and postoperative discomfort. Am J Orthod Dentofacial Orthop. 2007;131:9–15. doi: 10.1016/j.ajodo.2005.02.032. [DOI] [PubMed] [Google Scholar]
- Kravit N.D, Kusnoto B. Placement of mini-implants with topical anesthetic. J Clin Orthod. 2006;40:602–604. [PubMed] [Google Scholar]
- Meechan J.G. Effective topical anesthetic agents and techniques. Dent Clin N Am. 2002;46:759–766. doi: 10.1016/s0011-8532(02)00035-6. [DOI] [PubMed] [Google Scholar]
- Meechan J.G. Intra-oral topical anaesthetics: a review. J Dent. 2000;28:3–14. doi: 10.1016/s0300-5712(99)00041-x. [DOI] [PubMed] [Google Scholar]
- Tulga F, Mutlu Z. Four types of topical anesthetic agents: evaluation of clinical effectiveness. J Clin Pediatr Dent. 1999;23:217–220. [PubMed] [Google Scholar]
- Hersh E.V, Houpt M.I, Cooper S.A, Feldman R.S, Wolff M.S, Levin L.M. Analgesic efficacy and safety of an intra-oral lidocaine patch. J Am Dent Assoc. 1996;127:1626–1634. doi: 10.14219/jada.archive.1996.0098. [DOI] [PubMed] [Google Scholar]
- Rosivack R.G, Koenigsberg S.R, Maxwell K.C. An analysis of the effectiveness of two topical anesthetics. Anesth Prog. 1990;37:290–292. [PMC free article] [PubMed] [Google Scholar]
- Rosa A.L, Sverzut C.E, Xavier S.P, Lavrador M.A. Clinical effectiveness of lidocaine and benzocaine for topical anesthesia. Anesth Prog. 1999;46:97–99. [PMC free article] [PubMed] [Google Scholar]
- Hutchins H.S, Young F.A, Lackland D.T, Fishburne C.P. The effectiveness of topical anesthesia and vibration in alleviating the pain of oral injections. Anesth Prog. 1997;44:87–89. [PMC free article] [PubMed] [Google Scholar]
- Nakanishi O, Haas D, Ishikawa T, Kameyama S, Nishi M. Efficacy of mandibular topical anesthesia varies with the site of administration. Anesth Prog. 1996;43:14–19. [PMC free article] [PubMed] [Google Scholar]
- Nusstein J.M, Beck M. Effectiveness of 20% benzocaine as a topical anesthetic for intraoral injections. Anesth Prog. 2003;50:159–163. [PMC free article] [PubMed] [Google Scholar]
- Svensson P, Petersen J.K, Svensson H. Efficacy of a topical anesthetic on pain and unpleasantness during scaling of gingival pockets. Anesth Prog. 1994;41:35–39. [PMC free article] [PubMed] [Google Scholar]
- Van Steenberghe D, Bercy P, De Boever J, et al. Patient evaluation of a novel non-injectable anesthetic gel: a multicenter crossover study comparing the gel to infiltration anesthesia during scaling and root planing. J Periodontol. 2004;75:1471–1478. doi: 10.1902/jop.2004.75.11.1471. [DOI] [PubMed] [Google Scholar]
- McMillan A.S, Walshaw D, Meechan J.G. The efficacy of EMLA and 5% lignocaine gel for anaesthesia of human gingival mucosa. Br J Oral Maxillofac Surg. 2000;38:58–61. doi: 10.1054/bjom.1999.0143. [DOI] [PubMed] [Google Scholar]
- Donaldson D, Meechan J.G. A comparison of the effects of EMLA cream and topical 5% lidocaine on discomfort during gingival probing. Anesth Prog. 1995;42:7–10. [PMC free article] [PubMed] [Google Scholar]
- Roller N.W, Ship I.I. Lidocaine topical film strip for oral mucosal biopsies. J Oral Med. 1975;30:55–58. [PubMed] [Google Scholar]
- Meechan J.G. The use of EMLA for an intraoral soft-tissue biopsy in a needle phobic: a case report. Anesth Prog. 2001;48:32–34. [PMC free article] [PubMed] [Google Scholar]
- Vickers E.R, Marzbani N, Gerzina T.M, McLean C, Punnia-Moorthy A, Mather L. Pharmacokinetics of EMLA cream application to oral mucosa. Anesth Prog. 1997;44:32–37. [PMC free article] [PubMed] [Google Scholar]
- Taware C.P, Mazumdar S, Pendharkar M, Adani M.H, Devarajan P.V. A bioadhesive delivery system as an alternative to infiltration anaesthesia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:609–615. doi: 10.1016/s1079-2104(97)90360-7. [DOI] [PubMed] [Google Scholar]
- Kincheloe J.E, Mealiea W.L, Jr, Mattison G.D, Seib K. Psychophysical measurement of pain perception after administration of a topical anesthetic. Quintessence Int. 1991;22:311–315. [PubMed] [Google Scholar]
- Martin M.D, Ramsay D.S, Whitney C, Fiset L, Weinstein P. Topical anesthesia: differentiating the pharmacological and psychological contributions of efficacy. Anesth Prog. 1994;41:40–47. [PMC free article] [PubMed] [Google Scholar]
- Graham J.W. Profound, needle-free anesthesia in orthodontics. J Clin Orthod. 2006;40:723–724. [PubMed] [Google Scholar]
- Heft M.W, Parker S.R. An experimental basis for revising the graphic rating scale for pain. Pain. 1984;19:153–161. doi: 10.1016/0304-3959(84)90835-2. [DOI] [PubMed] [Google Scholar]
- Kravitz N.D. The use of compound topical anesthetics: a review. J Am Dent Assoc. 2007;138:1333–1339. doi: 10.14219/jada.archive.2007.0048. [DOI] [PubMed] [Google Scholar]