Abstract
Purpose
In Zambia, where emergency medical services are very limited, the police are frequently called to the scene for unaccompanied people experiencing seizures or people who have exhibit disturbed behaviors during a seizure. Police officers receive no formal medical training to manage such encounters. We developed and administered a police-specific survey to assess their knowledge, attitudes, and practices (KAP) regarding epilepsy in Zambia.
Methods
In 2004, a 28-item KAP questionnaire that included queries specific to police encounters with seizures and epilepsy was developed and delivered to a random sample of 200 police officers stationed in Lusaka. Descriptive data were reviewed and open text questions post-coded and categorized.
Results
The response rate was 87.5% (n=175). Police were familiar with epilepsy with 85% having witnessed a seizure. Although 77.1% recognized epilepsy as a brain disorder, almost 20% blamed spirit possession, 13.9% associated epilepsy with witchcraft and over half the respondents believe epilepsy is contagious. When asked how they would treat someone brought in for peace disturbance during a seizures, most police provided supportive or neutral responses, but 8% reported taking harmful actions (arrest, detain, handcuff, restrain) and 14.3% indicated that people with epilepsy in police custody require quarantine.
Conclusions
A significant number of police officers in Zambia lack critical knowledge regarding epilepsy and self-report detrimental actions towards people with seizures. In regions of the developing world where the police provide emergency medical services, police officers need to be a target for educational and social intervention programs.
Keywords: stigma, police, tolerance, knowledge, epilepsy, law enforcement, prison
Introduction
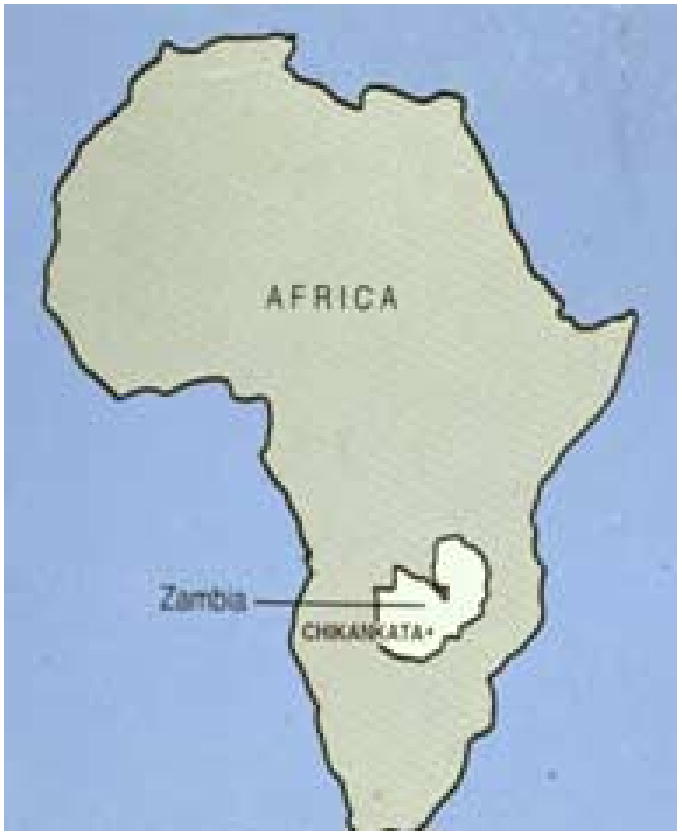
Zambia, a land-locked country located in southern Africa (Figure 1), has a population of ∼10 million people and epilepsy prevalence rates in Zambia appear to substantially exceed rates from more developed countries [1]. As with most other countries of sub-Saharan Africa (SSA), Zambia's major public health challenges include HIV/AIDS. Economic development in the region is slow and the World Bank ranks Zambia among the poorest of nations [2].
Figure 1.
A substantial body of data supports that there is a disproportionate burden of epilepsy in SSA relative to more developed regions and that the social and economic burden of the disease in the region is substantial[1, 3-5]. Research in Kenya and Zambia found that neurologic impairment is quite common among both children and adults with epilepsy [4, 6]. Misperceptions regarding the nature of epilepsy may result in care-seeking through traditional healers or no care-seeking at all [7, 8]. A 2001 study of public health priorities in mental health funding identified epilepsy as one of the key conditions in need of greater support[9]. A community-based approach to epilepsy care is recognized as the most-likely method to decreasing the epilepsy treatment gap in SSA[10-14]
In urban Zambia, where public emergency medical services are very limited, the police are frequently called when someone who is unaccompanied experiences a seizure. This may be especially likely if the episode includes associated confusion with aggressive or psychotic features. In New York City, the frequency of police aid to persons experiencing seizures in public in 1977 was examined as an index of uncontrolled seizures, and to assess variations in seizure frequency by age, sex, and ethnicity[15]. This study involving 5500 people screened for history of violence during their seizures found only 7 who exhibited significant aggression during their seizures. Training for police in Zambia includes basic first aid medical training, but no specific information on the acute management or nature of seizures (Personal Communication, Superintendent Staff-Training Department, Police Headquarters, Lusaka). Zambia has a centralized police service and personnel and officers may be posted to any part of the country. The police are members of an organization intended to serve the public at large and take a leading role in law enforcement. In addition, the police are expected to provide a wider range of emergency and other services. Among the norms that are intended to guide Zambian police actions is an expectation that the police be equitable in their treatment of citizens (Zambian Bill of Rights Part III-articles 21 and 23).
In a series of 10 focus group discussions conducted by our research team involving both rural and urban populations and segregated into men, women, youths and parents of children with epilepsy as well as our own clinic experiences, Zambian police are also contacted for people who are unconscious or confused and those who are found wandering during partial seizures, indicating that police encounters with people with epilepsy in Zambia are not limited to aggressive or violent actions., Several focus group participants reported encounters with police, many of them negative in nature. For example, the father of a child with epilepsy whose seizures often manifested with “wandering” behaviors was threatened by the police with imprisonment if he couldn't manage to keep his child at home. Another man with epilepsy reported physical assault at the hands of police after being detained at police headquarters after a public seizure. Therefore, we developed and administered a survey for Zambian police officers to assess their knowledge, attitudes, behaviors and practices (KAP) regarding epilepsy. The survey included role-specific questions regarding professional behaviors. Although 72 languages are spoken in Zambia, English is the official language and the language used for higher education.
Methods
Instrument
To examine how the police in Zambia understand and deal with people with epilepsy, we developed a 28-item, self-administered KAP survey that included generic questions used in other studies of epilepsy-associated stigma [16-24]. The survey assessed demographic characteristics (6-items), the respondents' personal proximity/experience with epilepsy (4-items), knowledge of epilepsy (11-items), recommendations for care (1-item), social tolerance (4-items), and two open-ended text questions regarding how the police officers would respond to someone with a seizure and someone they know to have epilepsy (see Appendix A for the complete questionnaire). The survey was piloted in series with three urban Lusaka police officers who were then removed from the sampling frame. Questions were read to them and discussions undertaken to assure the intended concept of the questions was appreciated. Minor language edits were made to facilitate clarification By the third piloting no further queries or clarifications were necessary. No major structural changes in the original instrument were necessary.
Respondent Sample
Using the register of police officers from the Police Central Headquarters in Lusaka, a random sample of 200 was selected using a random number generating program and police officer's registration numbers which are assigned sequentially at the time of hire. Unfortunately, accurate demographic data for the overall sampling frame was not available. The senior police officer in charge of research distributed the questionnaires to the respective stations where sampled officers were on duty. Questionnaires were completed anonymously after duty hours and returned to the Central Police Headquarters to be collected by the local investigators. ZMK 10,000 equivalent value of ∼$2.00 was offered to potential participants for their time.
Analysis
Data were double-entered into Microsoft Access for accuracy before importation into EPI INFO version 3.2.2 for descriptive analysis. Investigators reviewed the two open-text, police-specific scenarios and post-coded responses. To facilitate post-coding, each of the co-investigators was asked to review the transcript and independently assigned the response into one of three categories: “supportive”, “harmful” or “neutral”. For the question “Someone is brought in to the police station who has had a convulsion. You do not know if they have epilepsy. What would you do?” answers were post-coded into one of these three ranked categories (supportive, harmful or neutral). For the question, “Someone with known epilepsy is arrested and brought in to the police station. What would you do?” frequent responses included ambiguous actions, so this question was post-coded into 6 descriptive categories(1-proceed with arrest, 2-bond them/post bail, 3-help, 4-neutral, 5-quarantine, 6-harmful) and the nature of the explicit answer is provided.
Results
A total of 175 surveys were returned for a response rate of 87.5%. Descriptive data regarding demographics, personal proximity, knowledge and tolerance are provided in Table 1. Among completed questionnaires, missing data for individual questions was <5% for any single question. Local terms for epilepsy included the following: akakosh, cabana, chikonikoni, chikonya, chipumputu, chituwani, kaganyuka, kakoshi, kanono, kashita, kasuntu, kifwafwa, kikonyi, kishimo, kuganyuka, kunyu, kuwa, makwa, musamfu, nafwa, njilinjili. Njinjili, umusamfu, and vizilisi.
Police officers were asked “Someone is brought in to the police station who has had a convulsion. You do not know if the person has epilepsy. What would you do?” Investigators post-coded responses into three categories-supportive, neutral or harmful practices (Table 2). Although 77% reported that they would offer supportive care (seek or refer to medical services or provide first aid), 8% indicated that they would (1) detain and/or arrest the individual or (2) isolate them (i.e. place them in a closed cell without windows, access to other persons, or free atmosphere) or (3) restrain them with handcuffs or straps. Additional text provided by the respondents indicated that fear of catching epilepsy was apparently uppermost in the minds of officers doing this.
Table 2.
Responses to question, “Someone is brought in to the police station who has had a convulsion. You do not know if the person has epilepsy. What would you do?” (n=159)
| Post-coded category | N (%) respondents | Examples |
|---|---|---|
| Supportive | 115 (72.3) | Seek or refer to medical care |
| Provide first aid | ||
| Neutral | 32 (20.1) | Observe |
| Wait until recovery | ||
| Refer to superior | ||
| Pray for him | ||
| Harmful | 12 (7.5) | Isolate |
| Arrest | ||
| Detain | ||
| Handcuff and strap | ||
The second open-text, police-specific question was, “Someone with known epilepsy is arrested and brought in to the police station. What would you do?” Results are provided in Table 3. Although overtly harmful responses were rare (<1%), but 14% of respondents indicated that they would place such a person in quarantine.
Table 3.
Response to the question, “Someone with known epilepsy is arrested and brought in to the police station. What would you do?” (n=153)5
| Response | N (%) | Example |
|---|---|---|
| Proceed with arrest | 23 (15.0) | Charge him accordingly |
| Treat as any other criminal | ||
| Arrest as usual | ||
| Bond them/ Post bail | 54 (35.3) | Arrange bond |
| Arrange bond, if crime not dangerous | ||
| Arrange bond as quickly as possible | ||
| Help | 32 (20.9) | Refer to clinic |
| Take to hospital | ||
| Call doctor | ||
| Neutral | 22 (14.4) | Treat fairly |
| Pray for him | ||
| Seek advice from superior | ||
| Quarantine | 22 (14.4) | All respondents literally said “quarantine” |
| Harmful action | 1 (0.7) | Handcuff and strap down |
Answers were not mutually exclusive and respondent may have been coded for more than one type of response so total > 100%
Discussion
Limitations
Although we took a random sample of registered, employed Zambian police in Lusaka, we were not able to compare the demographic characteristics of our sample of 200 with the overall sampling frame. There are no formal records maintained to determine how frequently Zambian police encounter someone with a seizure or epilepsy. Our own potential biases in post-coding open-ended questions could potentially lead to a more negative perception of police self-proporaed actions. Therefore, when we felt responses were ambiguous, we provided details of the response rather than simple categories. Data presented here provide insight into police officers' understanding of epilepsy in urban Lusaka. Within Zambia, there are few police in the rural regions and extrapolation of this data to other African countries may not be appropriate, but there are few prior studies that have assessed the encounters that occur between people with epilepsy and police officers, and none of these have been conducted in developing countries where the police are the de facto emergency medical service providers. Although easier to analyze, the content of simple multiple choice questions is by its nature very limited, so we also asked open-ended questions. Interpretation of the text in such responses is fraught with the potential for misunderstanding but can offer some valuable insights not available when using closed or limited responses. Clearly, further qualitative work would offer more valuable insights into our understanding of how Zambian police conceptualize epilepsy and respond to people with the disorder.
In the early 1990s, the police in Zambia underwent vigorous reforms, which included changing their title from “Police Force” to “Police Service”, and changing entry qualifications from grade seven to grade twelve (secondary school completion). In 2002, 26% of women and 14% of men in Zambia were reported to be illiterate [25]. In our sample of police, over 90% of respondents had completed secondary school illustrating that police officers in Zambia are substantially more educated than the general population they serve. In spite of their educational status, the Zambian police officers surveyed demonstrate intolerance for people with epilepsy and knowledge gaps regarding the biomedical nature of the disease with supernatural causes and contagion fears being common. Although the majority of police indicated that they would provide supportive assistance to people they encounter with seizures while on duty, a substantial minority (∼20%) report that they would undertake actions that could be harmful and/or stigmatizing to someone with epilepsy, including the belief that people with epilepsy require isolation or quarantine. In this survey, the police officers' commonly indicated a desire to bond/bail people with epilepsy who have been arrested. This is difficult to interpret as it could reflect either a desire to help the individual or contagion fears. This deserves further qualitative study.
Despite its limitations, to the best of our knowledge, this study represents the first systematic evaluation of police offers' attitudes towards seizures and people with epilepsy in a resource poor environment. Our findings indicated that Zambia police officers require further education regarding the non-contagious nature of epilepsy and acute seizure management as well as some social sensitization regarding the condition. In less developed regions where emergency medical services are extremely limited, law enforcement personnel should be an important target for educational programs aimed at decreasing epilepsy-associated morbidity, mortality, and stigma.
Table 1.
Descriptive Data (n=175)
| Variable | |
|---|---|
| Demographic | |
| Age (years) | Mean 31.8; SD 7.0; Range 19-53 |
| Males | 71.3 % |
| Number of years of formal education | Mean 12; SD 1.0; Range 9-13 |
| Marital status (married) | 72.3% |
| Urban residence | 95.4 % |
| Fluent in English1 | 90.0% |
| Personal proximity | |
| Has heard of epilepsy | 97.7% |
| Knows someone with epilepsy | 91.7% |
| Has witnessed a seizure | 85.0% |
| Has a family member with epilepsy2 | 35.5% |
| Not familiar with epilepsy3 | 2.3% |
| Knowledge | |
| Epilepsy is a form of … | |
| -Madness | 1.2% |
| -Mental retardation | 30.1% |
| -Spirit or demon possession | 19.3% |
| -Brain disease | 77.1% |
| Epilepsy is contagious | |
| -Always | 1.8% |
| -Sometimes | 52.1% |
| -Never | 46.1% |
| The cause of epilepsy is… | |
| -Brain injury | 67.2% |
| -Runs in families | 35.5% |
| -Birth injury | 21.1% |
| -Blood disorder | 31.3% |
| -Witchcraft | 13.9% |
| -Curse from God | 4.2% |
| -Spirit possession | 18.7% |
| -Excessive worry | 7.2% |
| 4 Would recommend treatment via… | |
| -Doctor | 85.6% |
| -Traditional healer | 24.6% |
| -Church healing session | 27.5% |
| Tolerance | |
| Would allow their child to play with a child with epilepsy | 83.6% |
| Would allow their son to marry a PWE | 56.2% |
| Would allow daughter to marry a PWE | 57.4% |
| Believes a child with epilepsy should never attend school | 4.8% |
Self-reported assessment
Within the Zambian context of family is more inclusive and this answer reflects both primary (parents, brothers, sisters) and secondary (aunts, uncles, cousins) degree relatives.
Data for these individuals was dropped from further KAP-related analysis
Health-care seeking patterns for many conditions in the region involve dual care from both a traditional healer and a physician
Acknowledgments
Funding for this work was provided by the US National Institute of Health (NINDS R21 NS48060). We appreciate the cooperation of the Zambian Police Service in supporting the conduct of this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Appendix A
KAP Survey-Police Version
-
Please provide the following information:
Age______(years) Sex □ Male □ Female
Highest grade attained__________ Other training_________________
-
Marital Status (please check one)
□ never married
□ currently married (monogamous)
□ currently married (polygamous)
□ divorced/separated/widow/widower (not remarried)
□ currently married (previously divorced)
Number of children ____
-
Residence
□ City
□ Rural
- Please check the boxes below indicating the languages you speak.
Fluent Some None English Nyanja Bemba Tonga Lozi Other (___________) What rank do you have as a police officer?_________________
-
Have you ever heard or read about the disease called “epilepsy”?
□ No
□ Yes--If yes, please give the local names for this disease.
-
Have you ever known anyone with epilepsy?
□ Yes
□ No
□ Not familiar with epilepsy
-
Have you ever witnessed a seizure?
□ No
□ Not familiar with seizure
-
□ Yes-If yes, please check all those things you observed
□ confusion
□ tongue biting
□ loss of urine or stool
□ loss of consciousness
□ stiffening
□ staring
Someone is brought in to the police station who has had a convulsion. You do not know if the person has epilepsy. What would you do?
Someone with known epilepsy is arrested and brought in to the police station. What would you do?
-
Would you allow your child to play with a child who has epilepsy?
□ Yes
□ No
□ Not familiar with epilepsy
-
“A child with epilepsy should never attend school.” This statement is—
□ True
□ False
□ Sometimes true
□ Not familiar with epilepsy
-
Would you allow your son to marry a person with epilepsy?
□ Yes
□ No
□ Not familiar with epilepsy
-
Would you allow your daughter to marry a person with epilepsy?
□ Yes
□ No
□ Not familiar with epilepsy
-
“Epilepsy is a form of…” (Please tick all that apply)
□ Madness
□ Spirit or demon possession
□ Mental retardation
□ Brain disease
□ Not familiar with epilepsy
-
Epilepsy is a contagious condition (Please tick one)
□ Always
□ Sometimes
□ Never
-
What do you think is the cause of epilepsy? (Please tick all that apply)
□ Brain injury
□ Runs in families
□ Birth injury
□ Excessive worry
□ Blood disorder
□ Witchcraft
□ Curse from God
□ Spirit possession
□ Not familiar with epilepsy
-
If you had a friend or relative with epilepsy, what kind of treatment would you suggest? (Tick all that apply)
□ See a doctor
□ See a traditional healer
□ Acupuncture
□ See a church healing session
□ Nothing-there is no treatment
□ I don't know what to recommend
□ Not familiar with epilepsy
-
Do you have a close family member with epilepsy?
□ Yes
□ No
Thank you for participating in this survey. We welcome any comments you have regarding this survey. Please place them below.
References
- 1.Birbeck GL, Kalichi EM. Epilepsy prevalence in rural Zambia: a door-to-door survey. Trop Med Int Health. 2004 Jan;9(1):92–5. doi: 10.1046/j.1365-3156.2003.01149.x. [DOI] [PubMed] [Google Scholar]
- 2.WorldBank. Zambia-Country Brief. [9 December 2006]; Available from: http://web.worldbank.org/WBSITE/EXTERNAL/COUNTRIES/AFRICAEXT/ZAMBIA.
- 3.Snow RW, Williams RE, Rogers JE, Mung'ala VO, Peshu N. The prevalence of epilepsy among a rural Kenyan population. It's association with premature mortality. Trop Geogr Med. 1994;46(3):175–9. [PubMed] [Google Scholar]
- 4.Birbeck G, Kalichi E. The functional status of people with epilepsy in rural sub-Saharan Africa. J Neurol Sci. 2002 doi: 10.1016/s0022-510x(02)00467-7. Submitted. 9-5-02. [DOI] [PubMed] [Google Scholar]
- 5.Birbeck GL, Kalichi EM. Famine-associated AED toxicity in rural Zambia. Epilepsia. 2003 Aug;44(8):1127. doi: 10.1046/j.1528-1157.2003.22403.x. [DOI] [PubMed] [Google Scholar]
- 6.Mung'ala-Odera V, Meehan R, Njuguna P, Mturi N, Alcock KJ, Newton CR. Prevalence and risk factors of neurological disability and impairment in children living in rural Kenya. Int J Epidemiol. 2006 Jun;35(3):683–8. doi: 10.1093/ije/dyl023. [DOI] [PubMed] [Google Scholar]
- 7.Baskind R, Birbeck GL. Epilepsy-associated stigma in sub-Saharan Africa: the social landscape of a disease. Epilepsy Behav. 2005 Aug;7(1):68–73. doi: 10.1016/j.yebeh.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 8.El Sharkawy G, Newton C, Hartley S. Attitudes and practices of families and health care personnel toward children with epilepsy in Kilifi, Kenya. Epilepsy Behav. 2006 Feb;8(1):201–12. doi: 10.1016/j.yebeh.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 9.Modiba P, Schneider H, Porteus K, Gunnarson V. Profile of Community Mental Health Service Needs in the Moretele District (North-West Province) in South Africa. J Ment Health Policy Econ. 2001 Dec 1;4(4):189–96. [PubMed] [Google Scholar]
- 10.Danesi MA. Patient perspectives on epilepsy in a developing country. Epilepsia. 1984;25(2):184–90. doi: 10.1111/j.1528-1157.1984.tb04175.x. [DOI] [PubMed] [Google Scholar]
- 11.de Boer HM, Engel J, Jr, Prilipko LL. “Out of the shadows”: a partnership that brings progress! Epilepsia. 2005;46 1:61–2. doi: 10.1111/j.0013-9580.2005.461020.x. [DOI] [PubMed] [Google Scholar]
- 12.Diop AG, de Boer HM, Mandlhate C, Prilipko L, Meinardi H. The global campaign against epilepsy in Africa. Acta Trop. 2003 Jun;87(1):149–59. doi: 10.1016/s0001-706x(03)00038-x. [DOI] [PubMed] [Google Scholar]
- 13.IOM. Neurological, Psychiatric, and Developmental Disorders: Meeting the challenge in the developing world. 1. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 14.Leonardi M, Ustun TB. The global burden of epilepsy. Epilepsia. 2002;43(Suppl 6):21–5. doi: 10.1046/j.1528-1157.43.s.6.11.x. [DOI] [PubMed] [Google Scholar]
- 15.Neugebauer R, Oppenehimer G, Susser M. Seizures in public places in New York City. American Journal of Public Health. 1986;76(9):1115–9. doi: 10.2105/ajph.76.9.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jacoby A, Gorry J, Gamble C, Baker GA. Public knowledge, private grief: a study of public attitudes to epilepsy in the United Kingdom and implications for stigma. Epilepsia. 2004 Nov;45(11):1405–15. doi: 10.1111/j.0013-9580.2004.02904.x. [DOI] [PubMed] [Google Scholar]
- 17.Prpic I, Korotaj Z, Vlasic-Cicvaric I, Paucic-Kirincic E, Valerjev A, Tomac V. Teachers' opinions about capabilities and behavior of children with epilepsy. Epilepsy Behav. 2003 Apr;4(2):142–5. doi: 10.1016/s1525-5050(03)00025-8. [DOI] [PubMed] [Google Scholar]
- 18.Hills MD, MacKenzie HC. New Zealand community attitudes toward people with epilepsy. Epilepsia. 2002 Dec;43(12):1583–9. doi: 10.1046/j.1528-1157.2002.32002.x. [DOI] [PubMed] [Google Scholar]
- 19.Desai P, Padma MV, Jain S, Maheshwari MC. Knowledge, attitudes and practice of epilepsy: experience at a comprehensive rural health services project. Seizure. 1998 Apr;7(2):133–8. [PubMed] [Google Scholar]
- 20.Fong CY, Hung A. Public awareness, attitude, and understanding of epilepsy in Hong Kong Special Administrative Region, China. Epilepsia. 2002;43(3):311–6. doi: 10.1046/j.1528-1157.2002.31901.x. [DOI] [PubMed] [Google Scholar]
- 21.Dent W, Helbok R, Matuja WB, Scheunemann S, Schmutzhard E. Prevalence of active epilepsy in a rural area in South Tanzania: a door-to-door survey. Epilepsia. 2005 Dec;46(12):1963–9. doi: 10.1111/j.1528-1167.2005.00338.x. [DOI] [PubMed] [Google Scholar]
- 22.Novotna II, Rektor I. The trend in public attitudes in the Czech Republic towards persons with epilepsy. Eur J Neurol. 2002;9(5):535–40. doi: 10.1046/j.1468-1331.2002.00466.x. [DOI] [PubMed] [Google Scholar]
- 23.Atadzhanov M, Chomba E, Haworth A, Mwewe E, Birbeck G. Knowledge, attitudes, behaviors and practices (KABP) regarding epilepsy among Zambian clerics. Epilepsy & Behavior. 2006;9(1):83–8. doi: 10.1016/j.yebeh.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 24.Birbeck G, Chomba E, Atadzhanov M, Mbewe E, Haworth A. Zambian teachers-What do they know about epilepsy and how can we work with them to decrease stigma? Epilepsy & Behavior. 2006;9(2):275–280. doi: 10.1016/j.yebeh.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 25.Earthtrends. [9 December 2006]; earthtrends.wri.org/pdf_library/country_profile/pop_cou)894.pdf. Last.


