Abstract
Objective
To evaluate the primary care communications initiative, which introduced NHSnet to primary care in Scotland.
Design
Semi-structured telephone interviews, postal questionnaire.
Setting
All 15 Scottish health boards, random sample of 1 in 3 of all Scottish general practices.
Participants
Information management and technology managers of health boards, 355 practice managers in the general practices.
Main outcome measures
Variations between health boards in styles of project management, means of connection to NHSnet, costs to general practices, and training provided. Practices' levels of participation in initiative, initial use of NHSnet, and factors acting as incentives and disincentives to use of NHSnet.
Results
99% of Scottish general practices agreed to participate in initiative. Health boards varied significantly in project management styles (from minimal to total control), the nature of the networks they established (intranets or direct connections), costs to practices (from nothing to £125 per general practitioner per year), and training provided (from none to an extensive programme). In 56% of practices someone accessed NHSnet at least once a week. Practices varied considerably in amount of internet training received and staff groups targeted and in the intention to provide desktop access to NHSnet through a practice network.
Conclusion
The initiative has successfully introduced a network that links Scottish general practices, health boards, and hospital trusts. However local variation in this “national” initiative may affect its use in primary care. Health authorities and general practices in England and Wales may wish to note these findings in order to avoid unhelpful variation.
Introduction
NHSnet offers the prospect of an electronic network for primary care professionals across Britain. The new NHS Information Management and Technology Strategy, which is investing £1bn to improve patient care,1 and the plans for an electronic telecommunications infrastructure linking all UK general practices2,3 should make this prospect a reality. This will benefit patients by reducing paperwork and speeding up access to laboratory results, hospital appointments, and referral and discharge letters through use of email. Perhaps more importantly, it will redress the traditional problem of poor access to library resources in primary care4 by providing access to up to date information through NHSnet web pages and the internet.5,6 With the current emphasis on evidence based practice7–10 and clinical governance,11 and the increasing amount of information that doctors must sift through to keep up to date,12–14 rectifying this problem has become a priority.4,15
However, since the plans for the electronic infrastructure were announced, Scotland has moved ahead of England and Wales on this issue. The English white paper suggested that it would be 2002 before all general practices were connected to NHSnet.3 The Scottish Office, on the other hand, launched its primary care communications initiative in April 1997.16,17 This offered all Scottish general practices a free computer, installation of an ISDN line, registration to NHSnet, and one day's training.5 Practices could not receive the free computer without agreeing to connect to NHSnet.18
Because of the intense interest in this issue in Scottish primary care and the fact that the Scottish experience might provide useful lessons for England and Wales, we decided to evaluate the primary care communication initiative at the end of 1998, just over a year after it was launched and four months after it was considered complete. We explored the way in which it was implemented, identified initial levels of use of NHSnet, and assessed the impact of local variations.
Participants and methods
In our evaluation we conducted telephone interviews and a postal questionnaire. Both were piloted before use and minor changes made.
We conducted semi-structured telephone interviews with the individual (usually the information manager) in each of the 15 Scottish health boards who was responsible for local coordination of the initiative. These interviews were recorded, transcribed, and analysed based on categories that emerged from both the questions and responses. The interviews explored the level of health board involvement in implementing the initiative, the infrastructures put in place, costs to practices, and training provided.
We sent a questionnaire to the practice managers of a random sample of one in three of all Scottish general practices, stratified by health board (n=355). The questionnaire asked about the practices' participation in the initiative, access to and levels of use of NHSnet, training received, and problems encountered.
We analysed the results using SPSS.
Results
We achieved 100% participation in the interviews and an 87% (308/355) response to the questionnaire, reflecting the high level of interest in this issue.
Participation and initial use
The response to the primary care communication initiative surpassed expectations, with 1053 (99%) of the 1065 general practices in Scotland deciding to participate. The momentum generated by this initial enthusiasm seems to have led to promising initial levels of use of NHSnet: 203/299 (68%) of respondents said they were now accessing NHSnet, and 174/308 (56%) identified at least one member of the primary care team (a general practitioner in 47% of cases) who was using it at least once a week. This perhaps reflects the fact that 65/140 (46%) of practices listed access to information via NHSnet as one of the main advantages of the initiative (see table).
Coordination of the initiative
While initial levels of involvement and use were encouraging, reaching this stage was a complicated process. Although this was a national initiative with a central project management team to coordinate its implementation, a lack of coherence emanated from a decision to devolve a degree of coordinating responsibility to the 15 Scottish health boards; a policy which has also been recommended in England.19
The roots of the problem were twofold. Firstly, the level of responsibility given to each health board by the project management team varied, with two health boards having minimal input and five taking almost complete control of implementation. The remaining eight formed a spectrum in between, from those that simply facilitated communication with general practices to those that demanded more input into coordination, prioritisation, and means of connection. Secondly, the health boards were allowed to make local decisions about key issues such as costs to practices and networking arrangements. These two factors introduced considerable local variation.
Networking arrangements
Area networks
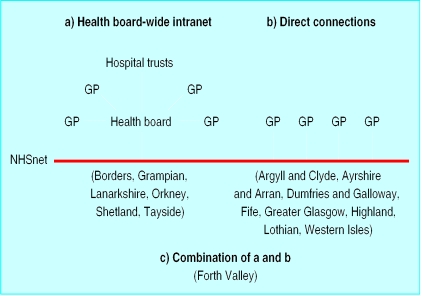
Health boards varied in the way that they connected practices to NHSnet. Some created local intranets through which all practices were connected to NHSnet via a single access point (fig 1a). These intranets also incorporated health boards and hospital trusts. Others, finding the costs of maintaining an intranet prohibitive, established direct connections to NHSnet from each individual practice (fig 1b). At the time of the evaluation Shetland and Orkney health boards had provided their practices with access to email only.
This lack of a coherent infrastructure across Scotland made problems harder to deal with. For example, there were ongoing difficulties with computer connections to NHSnet, with 25 (8%) of practices and 10 (67%) of the health boards complaining about the instability of email connections. Three health boards also reported that some practices had received huge bills from spurious calls generated by “a problem with the configuration of the software.” Practices affected by these problems reported that they were less inclined to use the computer. Unfortunately, the central project management team was disbanded before all difficulties were resolved.
Internal networks
Difficulty in gaining access to information resources has been a longstanding issue in primary care.4 To address this, the project management team had promoted desktop access to NHSnet and email throughout each general practice by linking the NHSnet computer to the practice's internal network.
However, the message from the health boards on this issue was inconsistent. Four health boards insisted on internal networking, 12 stated that they were in favour of it and generally encouraged it, but the remaining three (Greater Glasgow, Lanarkshire, and Lothian) decided not to permit practices to do this until their technical and security concerns were alleviated. This led to confusion among practices, only 37/299 (12%) of which connected their NHSnet computer to their internal network. Indeed, 133/299 (45%) said they had no intention of introducing this arrangement.
The impact of this lack of internal networking on access to NHSnet was exacerbated because most practices installed their NHSnet computer in a busy area—130/292 (45%) in the main office, 52 (18%) in reception, and 47 (16%) in the practice manager's office. Few were in a quiet and accessible location such as the practice library (9 (3%)), and eight were still in their boxes. Poor access discouraged people from using NHSnet in 57/308 (19%) of practices and caused 112/296 (38%) of practices to restrict its use. Of these, 35/64 (55%) stated that they did not give access to community nursing staff.
Costs to practices
Because the issue of costs to practices was devolved to health boards, the way in which recurring costs were dealt with varied considerably (see extra table on BMJ 's website). Thus, practices in three health boards (Dumfries and Galloway, Orkney, and Western Isles) paid nothing, whereas the rest were responsible for paying either the cost of calls or a set monthly charge from which all bills were paid.
Fortunately, though perhaps surprisingly, costs to practices did not seem to be a disincentive to use, and only nine (3%) of practices thought that this was a problem. However, this may be a spurious finding caused by the timing of the evaluation: levels of use at this early stage may not have generated sufficiently large bills to have a negative impact. As bills escalate, practices that have to pay for calls may start to restrict use.
Training
Education is an important element of managing change.20,21 This was taken into account on a superficial level during the implementation of the initiative by the provision of one day's training for one person from each practice (see box). This was provided at three main centres around Scotland, and representatives from about 790 practices attended. Unfortunately, this introduced further local variation as the distances involved meant that only half of the health boards were able to take full advantage of it. This arrangement discriminated against practices in the more remote areas despite recognition that rural areas need remote access to information more than most.22
Subjects covered by national training day on use of NHSnet
Windows NT
Client (such as NT environment, running programs, Explorer)
Administration (such as security, user rights, archiving)
Utilities (such as backup, printer management)
MS Exchange
Client (such as address book, messages, attachments)
Server (such as mailbox, profiles)
Internet Explorer
Anti-virus software
Of those who did attend the training only 55/142 (39%) found it useful. It focused on administration issues rather than use of the internet as an information resource. Thus, the opportunity to maximise use of the internet to support evidence based practice was missed. Indeed, only 15 minutes were spent on use of Internet Explorer. Because of the focus on administration issues, the 313 attendees were mainly practice managers (143 (46%)) and office staff (120 (38%)). Only 43 (14%) were general practitioners, and eight (3%) were practice nurses.
Variations in training were compounded by the fact that health boards were expected to provide more detailed training locally. All but two health boards (Highland and Western Isles) did so or planned to do so, but they differed in the range, amount, and type of training provided and in the staff groups they targeted (see extra table on BMJ 's website). Despite the fact that nine health boards invited all members of the primary heath care team to their training, again it was usually the practice managers (77/192 (40%)) and office staff (70 (37%)) who attended, whereas only 37 (19%) attendees were general practitioners and eight (4%) were practice nurses. This bias towards administrative staff meant that, although 10 health boards provided training on use of the internet, this was not targeted at healthcare professionals. Interestingly, the practices of health boards that did provide internet training seemed more likely to make regular use of NHSnet (see extra table on BMJ 's website), suggesting that targeting education at healthcare professionals might have a positive impact on use: at one extreme, only 20% of respondents in a health board that had provided no internet training were using NHSnet compared with 95% of respondents in a health board that had provided it.
These differences in national and local provision of training meant that some practices had less opportunity to develop their skills and knowledge than others. This is important since 88/178 (49%) of practices felt that lack of training was a disincentive to using NHSnet.
Discussion
The Scottish primary care communications initiative has been successful in implementing a national network that links all Scottish general practices as well as most health boards and hospital trusts. The level of participation is high, and initial levels of use of NHSnet, while not overwhelming, are at least encouraging. Yet, although this initiative is to be welcomed as an important step forward for primary care,2 its implementation has been less than satisfactory.
Unfortunately health boards were given different levels of responsibility for implementation and were allowed to make local decisions on what should have been core issues. As a result, a highly variable system has emerged with inequalities in levels of use, networking arrangements, access to NHSnet, costs to practices, and availability of training. There is a now need to examine the infrastructure that has been created and consider ways of improving coordination so that the variations described here do not affect the future use of NHSnet across Scotland.
The variation in costs to practices highlights the dangers of allowing local decision making within a national initiative. As well as leading to discontent among those who have to pay, it will disadvantage some practices and may inhibit their use of NHSnet, a potentially valuable source of evidence for a specialty that has traditionally had poor access to information.4 This issue should be rectified to achieve consistency and fairness across Scotland.
Access to sources of evidence via NHSnet has obvious advantages23,24 and may be important for the future development of evidence based practice in primary care.25 With clinical governance looming large, there is a need for progress in this area.11 Desk top access to the internet for all primary care professionals should be a priority, yet few general practices have provided this. The initial lack of internal networking we found may have been partly because of practices' lack of knowledge regarding the potential of NHSnet. This was undoubtedly compounded by the mixed messages from health boards as to whether internal networks were acceptable. This issue will probably resolve itself as concerns about security are reduced and understanding of the potential of desk top access to the internet increases.
Simply providing the necessary equipment to access to NHSnet is not enough; comprehensive, appropriate education targeted at the right individuals is also required to ensure that the potential of NHSnet to support evidence based practice is maximised.26 Health boards should take the opportunity now, while enthusiasm is still high, to redress imbalances in this area.
There are obvious lessons to be learnt from the implementation of the Scottish primary care communications initiative in relation to ensuring that future national projects avoid the introduction of local differences through effective central coordination. Moves are under way to make NHSnet available to general practices in England and Wales.5 Those coordinating the process should look to Scotland and learn from its experiences.
What is already known on this topic
Access to research evidence in primary care is traditionally poor, but the internet can address this by bringing up to date information into the consulting room
All general practices in Scotland have been offered access to NHSnet, but no evaluation had been made of its introduction or its impact on use of the internet
What this study adds
99% of Scottish general practices are connected to NHSnet, but problems may arise through local variations in infrastructure, costs to practices, and training provided
56% of practices use NHSnet at least once a week, but access can be difficult and training has not been targeted at healthcare professionals
There are organisational implications for those in England and Wales embarking on a similar exercise
Supplementary Material
Table.
Advantages of Scottish primary care communications initiative listed by 140 general practices
| Advantages | No (%) of practices listing this advantage |
|---|---|
| Email facility | 78 (56) |
| NHSnet and internet access | 65 (46) |
| Connection with hospital trusts | 28 (20) |
| Connection with health board | 24 (17) |
| Free computer | 23 (16) |
| Word processor | 21 (15) |
| Other | 26 (19) |
Figure.
Types of network adopted by Scottish health boards to link general practices with NHSnet
Acknowledgments
We thank Dr Malcolm McWhirter, director of public health, Forth Valley Health Board, for his support and encouragement. Invaluable assistance and advice was provided by Dave Simpson, information management and technology manager, and Mary Cameron, systems manager, Forth Valley Health Board. We also thank all those who participated in the evaluation.
Editorial by Kelly
Footnotes
Funding: Supported by the Directorate of Public Health, Forth Valley Health Board.
Competing interests: MW is employed by Forth Valley Health Board.
Extra tables giving further details of results appear on the BMJ's website. This article is part of the BMJ's trial of open peer review, and documentation relating to this also appears on the website
References
- 1.Wyatt J, Keen J. The NHS's new information strategy. BMJ. 1998;317:900. doi: 10.1136/bmj.317.7163.900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scottish Office Department of Health. The Scottish health service: ready for the future. Edinburgh: Scottish Office Department of Health; 1997. [Google Scholar]
- 3.Department of Health. The new NHS. London: HMSO; 1997. [Google Scholar]
- 4.Scottish Library and Information Council. Enabling access to the knowledge base of healthcare. Library and information provision for the NHS in Scotland. Edinburgh: Scottish Library and Information Council; 1998. [Google Scholar]
- 5.Scottish Health Care Supplies. National initiatives to promote primary care information management and technology. Information for health boards. Edinburgh: Scottish Health Care Supplies, 1997.
- 6.De Lusignan S, Brown A. Internet can be accessed from NHSnet. BMJ. 1998;317:1319. doi: 10.1136/bmj.317.7168.1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davidoff F, Haynes B, Sackett D, Smith R. Evidence based medicine. BMJ. 1995;310:1085–1086. doi: 10.1136/bmj.310.6987.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silagy C, Haines A, editors. Evidence based practice in primary care. London: BMJ Books; 1998. [Google Scholar]
- 9.Sackett DL, Rosenberg JA, Muir Gray JA, Haynes RB, Richardson WS. Evidence-based medicine: what it is and what it isn't. BMJ. 1996;312:71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.NHS in Scotland Management Executive. Primary care: the way ahead. A discussion paper. Edinburgh: Scottish Office Department of Health; 1996. [Google Scholar]
- 11.Scottish Office. Designed to care. Renewing the National Health Service in Scotland. Edinburgh: Scottish Office Department of Health; 1998. [Google Scholar]
- 12.Rosenberg W, Donald A. Evidence based medicine: an approach to clinical problem solving. BMJ. 1995;310:1122–1126. doi: 10.1136/bmj.310.6987.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weed LL. New connections between medical knowledge and patient care. BMJ. 1997;315:231–235. doi: 10.1136/bmj.315.7102.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Muir Gray JA. Where's the chief knowledge officer? BMJ. 1998;317:832–840. doi: 10.1136/bmj.317.7162.832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Glanville J, Haines M, Auston I. Getting research into practice. Finding information in clinical effectiveness. BMJ. 1998;317:200–203. doi: 10.1136/bmj.317.7152.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scottish Office Department of Health. Investment in primary care IM&T. Preliminary briefing for health boards. Edinburgh: Scottish Office Department of Health; 1997. [Google Scholar]
- 17.Dunmore T. Primary care computer equipment launch. Edinburgh: Scottish Office Department of Health; 1997. . (Letter to health boards.) [Google Scholar]
- 18.NHS Executive Information Management Group. NHS-wide networking. London: NHS Executive; 1995. [Google Scholar]
- 19.NHS Telecommunications Branch. GP Practices—technical requirements for connection to, and use of, NHSnet. Birmingham: NHS Telecommunications Branch, 1997.
- 20.Atkinson C, Hayden K. Change and teamwork in primary care. London: BMJ Books; 1993. Strategies for success; pp. 16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Broome A. Managing change. London: Macmillan; 1990. [Google Scholar]
- 22.Farmer J, Richardson A. Information for trained nurses in remote areas: do electronically networked resources provide an answer? Health Libraries Rev. 1997;14:97–103. [PubMed] [Google Scholar]
- 23.Steiner BD, Reid A, Smucker DR. Developments on the internet: a practical guide for primary care physicians. Fam Med. 1996;28:128–133. [PubMed] [Google Scholar]
- 24.Westberg EE, Miller RA. The basis for using the internet to support the information needs of primary care. J Am Med Informatics Assoc. 1999;6:6–25. doi: 10.1136/jamia.1999.0060006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kidd M, Purves I. Role of information technology. In: Silagy C, Haines A, editors. Evidence based practice in primary care. London: BMJ Books; 1998. pp. 123–128. [Google Scholar]
- 26.Klercker T, Zetraeus S. Dilemmas in introducing world wide web-based information technology in primary care: a focus group study. Fam Pract. 1998;15:205–210. doi: 10.1093/fampra/15.3.205. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.