Abstract
Objective
Mental health disorders commonly co-occur in patients with chronic pain, but little is known about the role of chronic pain in mental health service use. In this study, we explored the role of chronic pain in mental health service use by adults according to age group.
Design
Cross-sectional analysis of survey data from the second wave of the Healthcare for Communities telephone survey, collected in 2000 to 2001.
Setting
Randomly selected U.S. households.
Participants
U.S. civilian adults (N=6629)
Measurements
Common mental disorders were assessed using the short-form versions of the World Health Organization's Composite International Diagnostic Interview (CIDI-SF). Chronic pain conditions and mental health services received were identified by self report. Physical and mental functioning were assessed using the Short Form-12.
Results
Adults older than age 60 had higher rates of chronic pain and lower rates of mental health service use compared to those age 18 to 60 years. In multiple logistic regression models, an interaction effect was found between age and chronic pain (OR 3.0 [1.1-8.0]), with chronic pain significantly increasing the odds of any mental health care in the past year in adults older than 60 years of age.
Conclusions
Chronic pain increases the likelihood of mental health service use among older adults. Chronic pain may facilitate the presentation of distress in medical settings for these adults.
Keywords: pain, mental health, health services, geriatrics
Mental health disorders commonly co-occur in patients with chronic pain. Reported 12-month prevalence rates in population-based samples range from 7-28% for depression, 4-17% for anxiety disorders and 0.8-5% for substance use disorders.1-5 In primary care clinic samples, rates of depression may be as high as 46% in individuals with pain conditions.2 Individuals with chronic pain conditions have high rate of primary care and emergency room visits,6-9 but little is known about mental health service use in individuals with chronic pain and co-morbid mental health disorders. In a survey of 409 adults with self-reported osteoarthritis or rheumatoid arthritis, 42% reported not receiving needed mental health services.10 A survey of veterans in the VA Connecticut Healthcare System found that pain was associated with a higher use of outpatient medical services but was not related to use of outpatient or inpatient psychiatric services.11
An analysis of the Healthcare for Communities survey data from 1997-1998 found the presence of a chronic pain condition in persons with depression to be associated with a 20% increase in number of medical visits and a 21% lower likelihood of receiving any mental health specialty care relative to individuals without chronic pain.12 A separate analysis of this same data, focusing on age effects, found that adults 65 years or older meeting criteria for a mental disorder were also less likely to receive specialty mental health care or counseling or referrals for specialty mental health care from primary care providers than those less than 65 years of age.13 The elderly are more likely to experience chronic pain, but some studies suggest that older persons with chronic pain are less likely to experience severe psychological distress or depressed mood than younger individuals with chronic pain.14-16
In this study, we sought to obtain a more in-depth look at the role of chronic pain conditions in mental health service use according to age group using data from the 2000-2001 Healthcare for Communities Survey. Specifically, we sought to answer the following questions:
Do the rates of co-morbidity between chronic pain and mental disorders differ for those over and under 60 years of age?
How does co-morbidity of chronic pain affect access to, utilization of, and satisfaction with mental health services for those over and under 60 years of age?
On the basis of these prior studies suggesting lower rates of mental health service use in the elderly and in patients with chronic pain, we hypothesized that rates of mental health service use would be lower in elderly with chronic pain relative to younger patients with chronic pain or individuals of any age without chronic pain.
METHODS
Data Source
Data are from the second wave of Healthcare for Communities (HCC2), a part of the Robert Wood Johnson Foundation's Health Tracking Initiative conducted in 2000-2001. HCC was a nationwide telephone survey designed to track the effects of the changing health care system on individuals at risk for alcohol, drug abuse, and mental health (ADM) disorders.17 The HCC respondents were a stratified probability sample of participants in the Community Tracking Study (CTS), a nationally representative study of the U.S. civilian population.18 Details of the sampling design are described elsewhere.17 HCC2 followed all individuals who responded to the initial HCC survey conducted in 1997-1998 (HCC1). Of the 14,985 respondents selected for HCC1, 9,585 complete interviews were obtained, yielding a response rate of 64%. A total of 6,659 of the 9,585 HCC1 respondents (70.9%, weighted) completed the HCC2 survey. Excluding cases with missing values for questions assessing the presence of a chronic pain condition left a total sample size of 6629 for this study. Informed consent was obtained verbally before the interview, and the study was approved by the institutional review boards at UCLA and RAND.
Variables
The presence of common mental disorders in the past 12 months (major depression, dysthymia, generalized anxiety disorder (GAD), and panic disorder) was assessed using short-form versions19 of the World Health Organization's Composite International Diagnostic Interview (CIDI-SF),20 based upon the Diagnostic and Statistical Manual Third Edition-revised (DSM-IIIR)21. Chronic pain conditions, other chronic conditions, and mental health service use were identified by self-report. The HCC survey asked about 17 different chronic conditions (“Here is a list of health problems some people have. Please indicate if you now have any of these problems.”), four of which were defined for this analysis as chronic pain conditions: arthritis, chronic back problems, migraine/chronic headaches, and `other' chronic pain condition. Rates reported in this study refer to current prevalence of chronic pain and other chronic medical conditions, and 12-month prevalence of mental health, problem drug or alcohol use, and mental health service use.
Problem alcohol use was defined as an Alcohol Use Disorders Identification Test (AUDIT) core total score of eight or higher.22 Problem drug use was defined as a positive answer to either of two questions, adapted from the CIDI, assessing tolerance or emotional or psychological problems as a result of drug use. The Physical Component Summary-12 (PCS-12) and Mental Health Summary-12 (MCS-12) from the Short Form-12 (SF-12)23 were used as aggregate measures of physical functioning and mental health functioning. Both PCS-12 and MCS-12 summary scores have a mean of 50 and a standard deviation of 10 in the general U.S. adult population, with a higher score indicating better functioning. Level of pain interference with the respondents' daily activities was derived from the SF-12 pain interference item (extremely/a lot versus moderately/a little bit versus not at all).
Guideline-consistent counseling was defined as at least four visits with a mental health specialist or four visits with a primary care provider that included some counseling (five or more minutes per visit) for mental health problems, in the past 12 months. This criteria is more conservative than that used in the National Comorbidity Study (8 visits).24 A similar counseling definition to the one used in this study was used in the Medical Outcomes Study, where appropriate counseling or medication use was found to be associated with improved 2-year functional outcomes in depression.25 HCC respondents were asked about all prescribed medications which they had taken “at least several times a week for a month or more” in the past 12 months. Respondents were asked to read the names directly off of their pill bottles to the interviewers for all of their medications. These medications were later grouped into therapeutic categories by study staff. Guideline-consistent antidepressant therapy was defined as any antidepressant taken at an adequate dose for at least two months in the past 12 months. Appropriate pharmacotherapy was based upon Agency for Health Care Policy and Research and other published guidelines, and included parameters for the type of medication, dosage, and duration of treatment.26
Satisfaction with mental health treatment was assessed by a single item with five potential responses: Very satisfied, satisfied, neither satisfied nor dissatisfied, dissatisfied, very dissatisfied. Data are presented in this paper for percent reporting either satisfied or very satisfied (labeled as “Satisfied with mental health care”).
Data Analysis
Sample weights were used to weight the data to make them representative of the U.S. population and adjust for the probability of selection, non-response, and the number of households in the CTS survey that did not have a phone. Statistical differences were assessed with chi square statistic for categorical variables and t-statistic (comparison of age group differences) or F statistic (comparison of differences between the four chronic pain/age categories) for continuous variables. We opted to use age 60 as the dividing point for the two age categories rather than the traditional 65 in order to increase the sample size of older individuals. A comparison of socio-demographic and clinical variable frequencies using the two different cut points revealed no significant differences, other than a greater percentage of individuals 65 and older with Medicare as their main health insurance plan. Logistic regression analysis was used to estimate odds ratios for mental health care, based on risk factors while controlling for socio-demographic variables and mean physical and mental health functioning scores. Interaction terms concerning the presence of a chronic pain condition and age group, and presence of a mental health disorder and age group, were included to estimate the effect sizes for those older and younger than 60 years of age. All analyses were conducted using Software for the Statistical Analysis of Correlated Data (SUDAAN, version 9.01, Research Triangle Park, NC).
RESULTS
Demographics
Table 1 lists the socio-demographic characteristics of the 2000-2001 Healthcare for Communities (HCC2) population and for individuals with and without chronic pain, by age (18 to 60 years [N=4978] and older than 60 years of age [N=1651]). Data are consistent with that for the 1997-1998 survey presented elsewhere,12, 13 with the exception that the mean annual income was higher in the HCC2 population used for this analysis ($54,296 versus $39,765), likely due to a higher mean income in responders ($50,239) versus non-responders ($47,097) to the HCC2 survey.27 Individuals older than 60 years of age were less educated, had a lower mean income, were more likely to be White, were more likely to have Medicare or Medicaid and less likely to be uninsured, and were less likely to have an unmarried partner than individuals age 18 to 60 years of age.
Table 1.
Socio-Demographic Characteristics of Respondents with or without a Chronic Pain Condition, by Age Group
| With Chronic Pain (N=3135) |
Without Chronic Pain (N=3494) |
||||||
|---|---|---|---|---|---|---|---|
| Sample Characteristics N(%) | Overall (N=6629) |
18~60 (N=2074) |
Over 60 (N=1061) |
Chisq (df) P Value |
18~60 (N=2904) |
Over 60 (N=590) |
Chisq (df) P Value |
| Age | |||||||
| Under 30 | 852 (13.8%) | ||||||
| 31 to 45 | 2117 (33.2%) | ||||||
| 46 to 60 | 2009 (25.2%) | ||||||
| Over 60 | 1651 (27.8%) | ||||||
| Gender | |||||||
| Female | 4122 (52.2%) | 1396 (56.2%) | 746 (64.3%) | 211.01 (1) p<0.001 | 1654 (46.4%) | 326 (48.2%) | 0.51 (1) p=0.476 |
| Race | 24.05 (3) p<0.001 | 29.54 (3) p<0.001 | |||||
| White | 5289 (75.4%) | 1654 (74.7%) | 910 (83.7%) | 2227 (71.0%) | 498 (83.3%) | ||
| Black | 740 (11.8%) | 234 (12.1%) | 98 (10.1%) | 359 (13.2%) | 49 (8.2%) | ||
| Hispanic | 401 (9.7%) | 111 (10.0%) | 31 (3.4%) | 233 (12.9%) | 26 (4.7%) | ||
| Other | 199 (3.1%) | 75 (3.3%) | 22 (2.8%) | 85 (2.9%) | 17 (3.8%) | ||
| Marital Status | 57.76 (2) p<0.001 | 47.76 (2) p<0.001 | |||||
| Married | 3974 (62.1%) | 1252 (60.4%) | 545 (53.3%) | 1829 (66.4%) | 348 (61.5%) | ||
| Single | 2262 (32.5%) | 667 (31.4%) | 503 (45.8%) | 862 (27.0%) | 230 (37.9%) | ||
| Unmarried partner | 375 (5.4%) | 148 (8.2%) | 11 (0.8%) | 206 (6.7%) | 10 (0.7%) | ||
| Education, N(%) | 48.05 (2) p<0.001 | 33.95 (2) p<0.001 | |||||
| Less than high school | 732 (13.2%) | 205 (11.3%) | 257 (27.5%) | 166 (8.1%) | 104 (16.2%) | ||
| HS Grad or some college | 3973 (61.3%) | 1275 (64.3%) | 628 (57.0%) | 1719 (61.0%) | 351 (62.5%) | ||
| College or high | 1924 (25.5%) | 594 (24.4%) | 176 (15.6%) | 1019 (30.9%) | 135 (21.3%) | ||
| Total household income, Mean (SD) | $54297 (56257) | $55211 (47255) | $31831 (37364) | 125.32 (1) p<0.001 | $63521 (60342) | $48465 (71001) | 14.56 (1) p<0.001 |
| Health insurance coverage | 211.01 (4) p<0.001 | 177.31 (4) p<0.001 | |||||
| Medicare | 1094 (17.7%) | 134 (5.2%) | 614 (60.1%) | 49 (1.5%) | 297 (49.7%) | ||
| Medicaid | 152 (2.3%) | 77 (3.8%) | 16 (1.8%) | 57 (2.0%) | 2 (0.6%) | ||
| Private | 4468 (66.4%) | 1524 (74.1%) | 348 (31.1%) | 2355 (80.9%) | 241 (42.1%) | ||
| Other | 224 (3.5%) | 69 (3.5%) | 50 (4.3%) | 72 (2.6%) | 33 (6.0%) | ||
| Uninsured | 648 (10.1%) | 254 (13.4%) | 31 (2.7%) | 350 (12.9%) | 13 (1.6%) | ||
Clinical Characteristics
Table 2 lists clinical characteristics for the 2000-2001 HCC2 population, with or without chronic pain, by age (18 to 60 years, and older than 60 years of age).
Table 2.
Clinical Characteristics of Individuals with or without a Chronic Pain Condition, by Age Group
| With Chronic Pain (N=3135) |
Without Chronic Pain (N=3494) |
||||||
|---|---|---|---|---|---|---|---|
| Clinical Characteristics N(%) | Overall (N=6629) |
18~60 (N=2074) |
Over 60 (N=1061) |
Chisq (df) P Value |
18~60 (N=2904) |
Over 60 (N=590) |
Chisq (df) P Value |
| Mental health disorders, N(%) | |||||||
| Major depressive disorder | 783 (9.1%) | 460 (19.4%) | 91 (6.9%) | 65.35 (1) p<0.001 | 221 (5.9%) | 11 (1.4%) | 20.92 (1) p<0.001 |
| Dysthymia | 333 (3.8%) | 185 (7.3%) | 65 (5.2%) | 2.65 (1) p=0.104 | 81 (2.2%) | 2 (0.04%) | 25.50 (1) p<0.001 |
| Panic | 286 (3.3%) | 179 (7.7%) | 37 (2.9%) | 20.24 (1) p<0.001 | 68 (1.7%) | 2 (0.06%) | 27.94 (1) p<0.001 |
| Generalized anxiety disorder | 299 (3.9%) | 184 (8.9%) | 42 (2.8%) | 11.04 (1) p<0.001 | 66 (2.0%) | 7 (1.6%) | 0.29 (1) p=0.592 |
| Number of mental health disorders, Mean (SD) | 0.2 (0.7) | 0.5 (1.0) | 0.2 (0.6) | 56.27 (1) p<0.001 | 0.1 (0.5) | 0.04 (0.2) | 29.64 (1) p<0.001 |
| Alcohol or drug problems (past year),N(%) | 455 (6.7%) | 176 (8.5%) | 28 (2.5%) | 33.66 (1) p<0.001 | 233 (8.l%) | 18 (2.8%) | 21.57 (1) p<0.001 |
| Chronic pain conditions, N(%) | |||||||
| Arthritis/rheumatism | 2019 (28.7%) | 1110 (53.1%) | 909 (86.1%) | 148.11 (1) p<0.001 | |||
| Mental health disorders, N(%) | |||||||
| Back problems | 1340 (17.6%) | 902 (41.8%) | 438 (39.3%) | 0.71 (1) p=0.340 | |||
| Chronic headaches | 860 (10.9%) | 748 (35.1%) | 112 (10.3%) | 116.19 (1) p<0.001 | |||
| Other chronic pain disorder | 724 (9.5%) | 541 (25.4%) | 183 (16.8%) | 14.03 (1) p<0.001 | |||
| Number of chronic pain conditions, Mean (SD) | 0.7 (0.9) | 1.6 (0.8) | 1.52 (0.7) | 056 (1) p=0.453 | |||
| Number of chronic conditions, excluding pain, Mean (SD) | 0.8 (1.2) | 1.0 (1.3) | 1.7 (1.5) | 108.18 (1) p<0.001 | 0.4 (0.7) | 1.0 (1.1) | 104.15 (1) p<0.001 |
| Level of pain interference, N(%) | 5.58 (2) p=0.062 | 15.40 (2) p<0.001 | |||||
| High pain | 752 (9.9%) | 442 (18.7%) | 233 (22.3%) | 62 (1.9%) | 15 (2.6%) | ||
| Moderate pain | 2580 (37.5%) | 1103 (54.1%) | 583 (55.5%) | 694 (22.3%) | 200 (34.2%) | ||
| No pain | 3297 (52.6%) | 529 (27.3%) | 245 (22.2%) | 2148 (75.8%) | 375 (63.3%) | ||
| PCS-12a, Mean (SD) | 46.4 (6.3) | 44.5 (6.7) | 42.1 (7.4) | 39.35 (1) p<0.001 | 48.9 (4.3) | 47.0 (5.7) | 39.54 (1) I p<0.001 |
| MCS-12a, Mean (SD) | 45.6 (5.6) | 44.4 (6.4) | 44.6 (6.3) | 0.64 (1) p=0.423 | 46.5 (4.8) | 46.6 (4.8) | 0.21 (1) p=0.649 |
Physical and mental health component summary scores from the Short Form-12 (SF-12)
Mental Health
Overall, individuals with chronic pain were more likely to have a mental health disorder than those without chronic pain. Individuals age 18 to 60 years with chronic pain were more likely to meet criteria for 12-month major depressive disorder, panic disorder, and generalized anxiety disorder than those older than age 60 with chronic pain (19.4%, 7.7% and 8.9% versus 6.9%, 2.9% and 2.8%, respectively). The prevalence of dysthymia did not differ between age groups with chronic pain. The mean number of mental health disorders was greatest in those age 18 to 60 years with a chronic pain condition and differed significantly by age group. The mean MCS-12 score did not differ significantly by age group.
Chronic pain Conditions and Physical Functioning
Among individuals with a chronic pain condition, arthritis was more common (86.1% versus 53.1%), and chronic headaches and other chronic pain condition were less common (10.3% versus 35.1%, and 16.8% versus 25.4%, respectively), in individuals older than 60 years of age relative to younger individuals. The prevalence of chronic back problems did not differ significantly by age group. Individuals older than 60 had a significantly greater mean number of chronic non-pain conditions than those age 18 to 60 years. Level of pain interference did not differ significantly by age group among those with a chronic pain condition, but was significantly higher in those older than 60 years of age, among those without a chronic pain condition. Physical functioning (as measured by mean PCS-12 score) was decreased in persons older than age 60 relative to younger individuals.
Mental Health Service Use
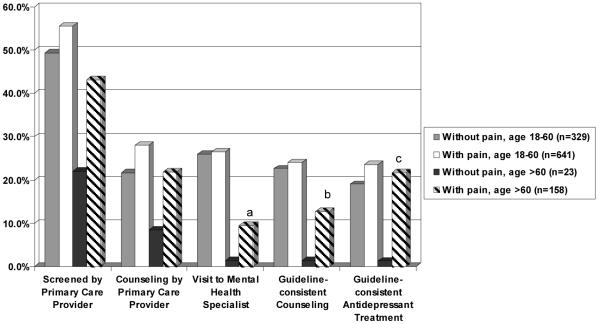
Table 3 describes mental health service use in the past 12 months among by individuals with and without chronic pain, by age group (18 to 60 years and older than 60 years), for the entire HCC2 sample (n=6629). Figure 1 illustrates differences in mental health service use in the past 12 months, ages 18 to 60 years versus older than 60 years, with and without a chronic pain condition, among those with a mental health disorder (n=1151).
Table 3.
Mental Health Services Utilization in the Past 12 Months by Individuals with and without a Chronic Pain Condition, by Age Group
| With Chronic Pain (N=3135) |
Without Chronic Pain (N=3494) |
||||||
|---|---|---|---|---|---|---|---|
| Mental Health Service Utilization, N (%) | Overall (N=6629) |
18~60 (N=2074) |
Over 60 (N=1061) |
Chisq (df) P Value |
18~60 (N=2904) |
Over 60 (N=590) |
Chisq (df) P Value |
| Perceived the need for mental health care | 1005 (11.5%) | 530 (22.3%) | 96 (7.4%) | 42.88 (1) p<0.001 | 361 (9.1%) | 18 (2.0%) | 42.42 (1) p<0.001 |
| Screened by primary care for mental health/substance use problem | 2000 (27.7%) | 842 (37.8%) | 237 (22.0%) | 42.24 (1) p<0.001 | 824 (26.7%) | 97 (17.1%) | 11.68 (1) p=0.0006 |
| Received any mental health care | 658 (6.9%) | 347 (12.5%) | 61 (4.4%) | 50.06 (1) p<0.001 | 238 (6.1%) | 12 (1.0%) | 33.78 p<0.001 |
| Primary care provided mental health/substance abuse counseling | 530 (5.8%) | 291 (10.6%) | 48 (4.0%) | 37.94 (1) p<0.001 | 180 (4.7%) | 11 (1.5%) | 14.72 (1) p=0.0001 |
| Visited a mental health care specialist | 514 (5.2%) | 267 (9.3%) | 35 (2.0%) | 50.46 (1) p<0.001 | 202 (5.1%) | 10 (0.7%) | 37.50 (1) p<0.001 |
| Guideline-consistent mental health/substance abuse counseling | 424 (4.3%) | 230 (8.2%) | 32 (2.2%) | 35.46 (1) p<0.001 | 155 (3.7%) | 7 (0.6%) | 28.03 (1) p<0.001 |
| Took psychiatric medications | |||||||
| Antidepressants | 808 (9.2%) | 411 (15.1%) | 130 (10.8%) | 6.09 (1) p=0.014 | 237 (6.4%) | 30 (4.2%) | 2.77 (1) p=0.096 |
| Guideline-consistent antidepressants | 596 (6.1%) | 310 (10.7%) | 83 (5.8%) | 28.03 (1) p<0.001 | 184 (4.3%) | 19 (3.3%) | 0.66 (1) p=0.415 |
| Satisfied with mental health care | 3571 (53.1%) | 1114 (52.4%) | 573 (54.0%) | 0.33 (1) p=0.565 | 1590 (54.6%) | 294 (47.1%) | 8.26 (1) p=0.004 |
| Got less treatment than needed | 273 (3.2%) | 158 (7.2%) | 21 (1.4%) | 19.45 (1) p<0.001 | 92 (2.2%) | 2 (0.2%) | 29.67 (1) p<0.001 |
Figure 1. Percent of Those with a Mental Health Disorder Who Used Mental Health Services in the Past 12 Months, by Age and Presence of Chronic Pain.
ap<0.05 bp<0.01 cp<0.001 for difference between those with versus without chronic pain, age >60
Regardless of the presence of a chronic pain condition, individuals age 18 to 60 years were more likely than those older than age 60: to perceive the need for mental health care (22.3% versus 7.4% with chronic pain, 9.1% versus 2.0% without chronic pain), to have been screened by a primary care provider for a mental health or substance use disorder (37.8% versus 22.0% with chronic pain, 26.7% versus 17.1% without chronic pain), or to have received any mental health care in the past 12 months (12.5% versus 4.4% with chronic pain, 6.1% versus 1.0% without chronic pain), including mental health specialty care and guideline-consistent mental health/substance abuse counseling.
Logistic Regression Analyses
Table 4 lists the results of logistic regression analyses examining risk factors for mental health service use among the total HCC2 population (N=6629). The presence of a chronic pain condition did not significantly increase the odds of being screened by a primary care provider for mental health/substance abuse in the past year (odds ratio [OR] 1.2, 95% confidence interval [95% CI] 0.98-1.4). The fourth and fifth rows in the table list the interaction effects for age by pain and age by mental health disorder. A significant interaction effect existed between age and chronic pain for the variables `any mental health care in the past year,' `satisfaction with mental health care,' but not for `mental health specialty visits in the past year' or `received effective counseling or antidepressants in the past year.' A significant interaction effect was present between age and mental health disorder for the outcome `satisfaction with mental health care'. In analyses stratified by age group (data not shown), a statistically significant association between the presence of a chronic pain condition and use of mental health services existed in those older than age 60 (any mental health care: OR 3.9, 95% CI 1.4-11.0, p=0.009, T=2.61, degrees of freedom (df)=1; mental health specialty visits: OR 4.2, 95% CI 1.1-17.1, p=0.042, T=2.04, df=1) but not in those 18 to 60 years of age. In contrast, the number of chronic non-pain conditions was not significantly associated with mental health service use for the full sample or for either age group in stratified analyses. Number of non-pain chronic conditions was significantly associated with being screened by a primary care provider for mental health/substance abuse in the full sample (OR 1.2, 95% CI 1.1-1.4, Table 4); when age groups were examined separately in stratified analyses, however, this relationship held true only for those 18 to 60 years of age (OR 1.3, 95% CI 1.1-1.5, p=0.0002, T=3.77, df=1).
Table 4.
Logistic Regression Models: Odds of Mental Health (MH) Care in the Past 12 Months
| Any MH Care in past year | MH specialty visits in past year | Screened by primary care for MH/substance abuse in past year | Perceived need for MH Care | Received effective counseling or antidepressants in past year | Satisfied with MH Care | |
|---|---|---|---|---|---|---|
| Risk Factors | Odds ratio (95% confidence interval) [P value, T test (df)] | |||||
| Presence of a chronic pain condition | 1.0 (0.7, 1.3) | 0.8 (0.6, 1.2) | 1.2 (0.98, 1.4) | 1.3 (1.0, 1.7) | 1.0 (0.8, 1.4) | 0.9 (0.7, 0.99) |
| [p=0.878, T(1)=-0.15] | [p=0.325, T(1)=-0.98] | [p=0.086, T(1)=1.72] | [p=0.025, T(1)=2.24] | [p=0.755, T(1)=0.31] | [p=0.037, T(1)=-2.09] | |
| Presence of a mental health disorder | 10.7 (7.9, 14.4) | 10.6 (7.3, 15.2) | 2.4 (1.9, 3.0) | 13.1 (10.4, 16.4) | 6.7 (5.0, 9.0) | 1.2 (1.0, 1.5) |
| [p<0.001, T(1)=15.52] | [p<0.001, T(1)=12.70] | [p<0.001, T(1)=7.84] | [p<0.001, T(1)=21.70] | [p<0.001, T(1)=12.47] | [p=0.048, T(1)=1.98] | |
| Age 60 years or older (reference 18-60) | 0.2 (0.1, 0.5) | 0.2 (0.1, 0.4) | 0.6 (0.5, 0.8) | 0.4 (0.3, 0.6) | 0.5 (0.4, 0.7) | 0.7 (0.5, 0.9) |
| [p=0.0006, T(1)=-3.43] | [p<0.001, T(1)=-5.05] | [p<0.001, T(1)=-4.11] | [p<0.001, T(1)=-4.46] | [p<0.001, T(1)=-4.61] | [p=0.0016, T(1)=-3.15] | |
| Interaction effect of age and pain | 3.0 (1.1, 8.0) | P=0.128a | P=0.553a | P=0.228a | P=0.913a | 1.4 (1.0, 1.8) |
| [p=0.030, T(1)=2.17] | [p=0.031, T(1)=2.16] | |||||
| Interaction effect of age and MH disorder | P=0.587a | P=0.761a | P=0.411a | P=0.183a | P=0.320a | 1.7 (1.0, 2.6) |
| [p=0.030, T(1)=2.18] | ||||||
| Number of chronic conditions, excluding pain | 1.0 (0.9, 1.1) | 0.9 (0.8, 1.1) | 1.2 (1.1, 1.4) | 1.0 (0.9, 1.1) | 1.0 (0.95, 1.2) | 1.0 (0.95, 1.1) |
| [p=0.633, T(1)=-0.48] | [p=0.372, T(1)=-0.89] | [p=0.0002, T(1)=3.80] | [p=0.678, T(1)=-0.41] | [p=0.324, T(1)=0.99] | [p=0.481, T(1)=0.71] | |
Interaction effects not significant at the p<0.05 level were excluded from the final models presented
CONCLUSIONS
This study confirms the high rates of chronic pain and low rates of mental health service use in those over 60 years of age that have been found in previous studies. Our results confirm previously documented findings of a high prevalence of common mental health disorders in individuals with chronic pain, increased disability among those with chronic pain and co-morbid mental health disorders, and a significant degree of unmet need for mental health services among older adults. Contrary to our hypothesis and previous studies in mixed age populations, it suggests that the presence of a chronic pain condition increases the likelihood of receiving mental health care in those over 60 years of age.
In our study, more than half of individuals older than age 60 had at least one chronic pain condition, most typically arthritis. The prevalence of arthritis increased with age, while the prevalence of chronic back pain remained stable and chronic headaches decreased. With increasing age, chronic pain is more common and less associated with mental disorders,28 possibly due to a lower association of depression and anxiety with arthritis relative to other chronic pain conditions. Prior studies14, 15 also suggest that chronic pain affects emotional functioning less in older individuals. We found that individuals older than 60 with a chronic pain condition were less likely to have a mental disorder than those younger than age 60 with a chronic pain condition, although mean mental functioning (MCS-12 score) did not differ significantly by age group. Because the presence of chronic pain and associated physical limitations increase with age, they may be expected and better accepted by older individuals.
The lower use of mental health services in older versus younger individuals is consistent with prior population-based studies.24, 29, 30 In an analysis of Medical Expenditure Panel Survey data, 70% of adults age 65 and older with self-reported depression received any treatment, whereas only 49% received an adequate course (medication and/or psychotherapy).31 Fifty-three percent of adults age 65 or older with mental disorders surveyed in the 1997-98 Healthcare for Communities (HCC) survey received any mental health care in the prior year.13 In our study of the 2000-01 HCC data, treatment rates for those older than age 60 remained low, with the presence of a chronic pain condition more than tripling the likelihood of receipt of any mental health care in the prior year. This finding, in combination with the high rates of chronic pain in older adults, underscores the importance of adequate education and training of mental health providers, particularly those working with geriatric populations, regarding the diagnosis and treatment of chronic pain conditions and their relationship with mental health disorders.
The presence of chronic medical conditions could be a potential deterrent to identifying mental health needs in individuals in medical settings due to “competing demands”32 or alternatively, could increase the likelihood of recognition via increased contact and thus opportunity for diagnosis. Prior studies have shown mixed results, some finding number of chronic conditions to be associated with mental health service use29, 30 and others finding some conditions but not others associated with mental health care31-33. In our study, the effect on mental health services was specific to chronic pain conditions.
Research on expectations of aging suggests a possible explanation for this finding. In a survey of community-residing adults aged 65 to 100 in the Los Angeles area,34 50% viewed depression as an expected development in aging, and those who attributed depression to aging were more likely to believe it was not important to discuss feeling depressed with a doctor35. The presence of chronic pain in elderly individuals may prompt discussion of distress with health care providers and increase the opportunity for recognition of mental disorders. Further study is needed to verify this hypothesis.
Strengths of this study are its population-based study design and detailed information on mental health service use as well as information on both DSM-IV mental health disorders and chronic medical conditions. Limitations include the self-report nature of information on medical conditions and chronic pain conditions, limited data on substance abuse disorders, and the cross-sectional nature of the information obtained. While specified as “chronic” (or in the case of arthritis, assumed to be chronic based on the nature of the condition), the data on chronic pain did not include information on other variables such as duration of pain and adequacy of treatment that may influence the relationship with mental health disorder and likelihood of receiving mental health services. Post-traumatic stress disorder (PTSD), simple phobia, and social phobia were found to be significantly associated with arthritis and chronic spinal pain in the National Co-morbidity Study (original and replication),3-5 but were not assessed by Healthcare for Communities. The high degree of co-morbidity of anxiety disorders among each other and with depression, however, likely limits the number of individuals with other anxiety disorders missed in this assessment. The absolute number of older individuals with a mental health disorder but no chronic pain condition was small (N=23), and may limit the generalizability of the results. In addition, while most of the significant effects noted in our findings were highly significant at the p<0.001 level, the interaction effect of age and pain was significant only at the p<0.05 level, likely a reflection of the additional power required to detect interaction effects. Hence, our results should be considered provisional, and analysis of other data sets is warranted to replicate our findings. Compared to the group with a chronic pain condition, older adults without a chronic pain condition had a lower mean number of chronic medical (non-pain) conditions and mental health disorders. It is possible that this group may not represent individuals who present for care in the outpatient setting. Further study would be required to confirm this hypothesis.
The Healthcare for Communities survey asked about chronic pain conditions commonly seen in primary care and included an “other chronic pain disorder” category, but did not ask specifically about neuropathic pain. Reported prevalence rates in cross-sectional studies of neuropathic pain in diabetics have ranged from 5% to 19%.36-38 In HCC2, 583 people reported having diabetes; of these, 88 (weighted percent = 12.0%) reported having “other chronic pain disorder.” It is not possible to know from this data what specific conditions are accounted for by the category “other chronic pain disorder.” The percent of individuals with diabetes reporting “other chronic pain disorder,” however, is consistent with the expected frequency of painful diabetic neuropathy.
In summary, our study shows that while rates of mental health service use among older adults are low regardless of the presence of co-morbid medical conditions, the presence of chronic pain increases the likelihood of mental health care, and suggests that those with a mental health disorder but no chronic pain may be at greatest risk of not receiving needed mental health services. Further research is needed to identify reasons for these findings and how to best address this area of unmet need.
Appendix.
Odds of Mental Health (MH) Care in the Past 12 Months: Logistic Regression Model Covariates
| Any MH Care in past year |
MH specialty visits in past year |
Screened by primary care for MH/substance abuse in past year |
Perceived need for MH Care |
Received effective counseling or antidepressants in past year |
Satisfied with MH Care |
|
|---|---|---|---|---|---|---|
| Covariates | Odds ratio (95% confidence interval) [P value, T test (df)] | |||||
| Gender (reference male) | 1.5 (1.1, 2.0) | 1.4 (1.0, 2.0) | 1.3 (1.1, 1.6) | 1.8 (1.5, 2.3) | 1.7 (1.3, 2.3) | 1.0 (0.9, 1.2) |
| [p=0.008, T(1)=2.64] | [p=0.053, T(1)=1.94] | [p=0.0004, T(1)=3.54] | [p<0.001, T(1)=5.38] | [p=0.002, T(1)=3.72] | [p=0.836, T(1)=-0.21] | |
| Race | F(1,3)=2.96, p=0.031 | K(1,3)=0.97, p=0.405 | F(1;3)=4.85, p=0.002 | F(1;3)=4.53, p=0.004 | F(1,3)=7.42, p=0.0001 | F(1,3)=0.65, p=0.583 |
| White (reference) | -- | -- | -- | -- | -- | -- |
| Black/African American | 0.5 (0.3, 0.8) | 0.6 (0.4, 1.1) | 0.9 (0.7, 1.2) | 0.5 (0.4, 0.8) | 0.4 (0.3, 0.6) | 1.0 (0.8, 1.3) |
| [p=0.005, T(1)=-2.82] | [p=0.563, T(1)=-0.58] | [p=0.0004, T(1)=-3.52] | [p<0.001, T(1)= -4.61] | |||
| Hispanic | 0.6 (0.3, 1.3) | 0.9 (0.4, 2.0) | 1.7 (1.2, 2.3) | 1.0 (0.7, 1.5) | 0.7 (0.3, 1.3) | 0.8 (0.6, 1.1) |
| [p=0.207, T(1)=-1.26] | [p=0.003, T(1)=2.96] | [p=0.947, T(1)=0.07] | [p=0.239, T(1)=-1.18] | |||
| Other race | 0.8 (0.4, 1.5) | 1.1 (0.5, 2.2) | 0.5 (0.3, 0.9) | 0.7 (0.4, 1.2) | 0.6 (0.3, 1.1) | 1.0 (0.7, 1.5) |
| [p=0.475, T(1)=-0.71] | [p=0.025, T(1)=-2.24] | [p=0.203, T(1)=-1.27] | [p=0.099, T(1)=-1.65] | |||
| Marital status | F(1,3)=0.54, p=0.583 | F(1,3)=1.91, p=0.148 | F(1,3)=2.42, p=0.090 | F(1,3)=3.38, p=0.034 | F(1,3)=1.71, p=0.181 | F(1,3)=1.62, p=0.198 |
| Married (reference) | -- | -- | -- | -- | -- | -- |
| Single | 1.2 (0.9, 1.6) | 1.4 (1.0, 2.0) | 0.8 (0.7, 1.0) | 1.3 (0.98, 1.7) | 0.9 (0.7, 1.2) | 0.9 (0.7, 1.0) |
| [p=0.065, T(1)=1.85] | ||||||
| Unmarried partner | 0.9 (0.6, 1.5) | 1.2 (0.7, 2.0) | 0.9 (0.6, 1.3) | 1.5 (1.0, 2.2) | 0.6 (0.4, 1.0) | 0.9 (0.6, 1.2) |
| [p=0.026, T(1)=2.22] | ||||||
| Education | F(1,3)=10.6, p<.0001 | F(1,3)=18.4, p<.0001 | F(1,3)=2.76, p=0.064 | F(1,3)=7.91, p=0.0004 | F(1,3)=15.27, p<.0001 | F(1,3)=13.89, p<.0001 |
| Less than high school (reference) | -- | -- | -- | -- | -- | -- |
| High school graduate or some college | 2.0 (1.3, 3.1) | 2.5 (1.5, 4.0) | 1.0 (0.8, 1.3) | 1.2 (0.8, 1.8) | 2.5 (1.8, 3.6) | 0.6 (0.5, 0.8) |
| [p=0.003, T(1)=2.96] | [p=0.0002, T(1)=3.68] | [p=0.289, T(1)=1.06] | [p<0.001, T(1)=5.02] | [p<0.001, T(1)=-3.91] | ||
| College or higher | 3.2 (1.9, 5.4) | 4.9 (2.9, 8.4) | 1.3 (0.95, 1.7) | 2.0 (1.3, 3.0) | 3.0 (2.0, 4.5) | 0.5 (0.4, 0.7) |
| [p<0.001, T(1)=4.46] | [p<0.001, T(1)=5.94] | [p=0.003, T(1)=2.98] | [p<0.001, T(1)=5.34] | [p<0.001, T(1)=-5.25] | ||
| Family income (log-transformed) | 1.0 (0.96, 1.1) | 1.0 (0.9, 1.1) | 1.0 (0.97, 1.1) | 1.0 (0.9, 1.1) | 1.0 (0.98, 1.1) | 1.0 (0.97, 1.02) |
| [p=0.552, T(1)=0.59] | [p=0.866, T(1)=0.17] | [p=0.884, T(1)=0.15] | [p=0.196, T(1)=1.29] | [p=0.805, T(1)=-0.25] | ||
| Health insurance coverage | F(1,3)=0.90, p=0.461 | F(1,3)=0.87, p=0.482 | F(1,3)=3.22, p=0.012 | F(1,3)=2.98, p=0.018 | F(1,3)=3.08, p=0.015 | F(1,3)=3.30, p=0.0106 |
| Medicare | 0.9 (0.4, 1.8) | 1.5 (0.8, 3.0) | 0.8 (0.5, 1.3) | 0.4 (0.2, 0.7) | 1.7 (0.9, 3.2) | 1.4 (1.0, 1.9) |
| [p=0.396, T(1)=-0.85] | [p=0.002, T(1)=-3.08] | [p=0.112, T(1)=1.59] | [p=0.035, T(1)=2.11] | |||
| Medicaid | 1.5 (0.6, 3.8) | 2.1 (0.8, 5.1) | 1.0 (0.5, 1.8) | 0.6 (0.3, 1.1) | 2.6 (1.2, 5.6) | 1.5 (0.9, 2.4) |
| [p=0.919, T(1)=-0.10] | [p=0.091, T(1)=-1.69] | [p=0.015, T(1)=2.44] | [p=0.127, T(1)=1.53] | |||
| Private | 1.2 (0.7, 2.0) | 1.3 (0.8, 2.4) | 1.3 (0.9, 1.8) | 0.7 (0.4, 0.96) | 1.5 (0.9, 2.6) | 1.5 (1.2, 1.9) |
| [p=0.196, T(1)=1.29] | [p=0.030, T(1)=-2.17] | [p=0.101, T(1)=1.64] | [p=0.0005, T(1)=3.50] | |||
| Other | 1.3 (0.7, 2.6) | 1.8 (0.8, 4.1) | 1.0 (0.6, 1.7) | 1.0 (0.6, 1.7) | 2.4 (1.4, 4.2) | 1.7 (1.1, 2.7) |
| [p=0.951, T=0.06] | [p=0.892, T(1)=-0.14] | [p=0.002, T(1)=3.13] | [p=0.0125, T(1)=2.50] | |||
| Uninsured (reference) | -- | -- | -- | -- | -- | -- |
| PCS-12a | 0.97 (0.95, 0.99) | 0.96 (0.94, 0.98)b | 0.99 (0.97, 1.01) | 0.96 (0.94, 0.99) | 0.95 (0.93, 0.97)c | 0.99 (0.98, 1.01) |
| [p=0.003, T(1)=-3.00] | [p=0.002, T(1)=-3.14] | [p=0.311, T(1)=-1.01] | [p=0.002, T(1)=-3.13] | [p<0.001, T(1)=-4.93] | [p=0.373, T(1)=-0.89] | |
| MCS-12 a | 0.97 (0.95, 0.99) | 0.97 (0.94, 0.99) | 0.98 (0.96, 0.99) | 0.95 (0.93, 0.97) | 0.96 (0.94, 0.98)c | 1.0 (0.99, 1.02) |
| [p=0.005, T(1)=-2.84] | [p=0.012, T(1)=-2.53] | [p=0.007, T(1)=-2.69] | [p<0.001, T(1)=-5.17] | [p<0.001, T(1)=-4.17] | [p=0.229, T(1)=1.20] | |
Physical and mental health component summary scores from the Short Form-12 (SF-12)
Acknowledgment
The first author of this paper is supported by a Ruth L. Kirschstein National Research Service Award (NRSA) Institutional Research Training Grant (T32).
Sponsor's Role: The sponsor of this research had no role in the design, methodology, analysis of data or preparation of the manuscript.
Further Acknowledgement: We would like to thank Kenneth B. Wells, MD, MPH for access to the HCC data.
REFERENCES
- 1.McWilliams LA, Goodwin RD, Cox BJ. Depression and anxiety associated with three pain conditions: results from a nationally representative sample. Pain. 2004;111(12):77–83. doi: 10.1016/j.pain.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 2.Bair MJ, Robinson RL, Katon W, et al. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163(20):2433–2445. doi: 10.1001/archinte.163.20.2433. [DOI] [PubMed] [Google Scholar]
- 3.Stang PE, Brandenburg NA, Lane MC, et al. Mental and physical comorbid conditions and days in role among persons with arthritis. Psychosom Med. 2006;68(1):152–158. doi: 10.1097/01.psy.0000195821.25811.b4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McWilliams LA, Cox BJ, Enns MW. Mood and anxiety disorders associated with chronic pain: an examination in a nationally representative sample. Pain. 2003;106(12):127–133. doi: 10.1016/s0304-3959(03)00301-4. [DOI] [PubMed] [Google Scholar]
- 5.Von Korff M, Crane P, Lane M, et al. Chronic spinal pain and physical-mental comorbidity in the United States: results from the national comorbidity survey replication. Pain. 2005;113(3):331–339. doi: 10.1016/j.pain.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 6.Blyth FM, March LM, Brnabic AJ, et al. Chronic pain in Australia: a prevalence study. Pain. 2001;89(23):127–134. doi: 10.1016/s0304-3959(00)00355-9. [DOI] [PubMed] [Google Scholar]
- 7.Andersson HI, Ejlertsson G, Leden I, et al. Impact of chronic pain on health care seeking, self care, and medication. Results from a population-based Swedish study. J Epidemiol Community Health. 1999;53(8):503–509. doi: 10.1136/jech.53.8.503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bernard AM, Wright SW. Chronic pain in the ED. Am J Emerg Med. 2004;22(6):444–447. doi: 10.1016/j.ajem.2004.07.026. [DOI] [PubMed] [Google Scholar]
- 9.Von Korff M, Wagner EH, Dworkin SF, et al. Chronic pain and use of ambulatory health care. Psychosom Med. 1991;53(1):61–79. doi: 10.1097/00006842-199101000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Hagglund KJ, Clark MJ, Hilton SA, et al. Access to healthcare services among persons with osteoarthritis and rheumatoid arthritis. Am J Phys Med Rehabil. 2005;84(9):702–711. doi: 10.1097/01.phm.0000167618.84726.33. [DOI] [PubMed] [Google Scholar]
- 11.Kerns RD, Otis J, Rosenberg R, et al. Veterans' reports of pain and associations with ratings of health, health-risk behaviors, affective distress, and use of the healthcare system. J Rehabil Res Dev. 2003;40(5):371–379. doi: 10.1682/jrrd.2003.09.0371. [DOI] [PubMed] [Google Scholar]
- 12.Bao Y, Sturm R, Croghan TW. A national study of the effect of chronic pain on the use of health care by depressed persons. Psychiatr Serv. 2003;54(5):693–697. doi: 10.1176/appi.ps.54.5.693. [DOI] [PubMed] [Google Scholar]
- 13.Klap R, Unroe KT, Unutzer J. Caring for mental illness in the United States: a focus on older adults. Am J Geriatr Psychiatry. 2003;11(5):517–524. [PubMed] [Google Scholar]
- 14.Wittink HM, Rogers WH, Lipman AG, et al. Older and younger adults in pain management programs in the United States: differences and similarities. Pain Med. 2006;7(2):151–163. doi: 10.1111/j.1526-4637.2006.00113.x. [DOI] [PubMed] [Google Scholar]
- 15.Rustoen T, Wahl AK, Hanestad BR, et al. Age and the experience of chronic pain: differences in health and quality of life among younger, middle-aged, and older adults. Clin J Pain. 2005;21(6):513–523. doi: 10.1097/01.ajp.0000146217.31780.ef. [DOI] [PubMed] [Google Scholar]
- 16.Wijeratne C, Shome S, Hickie I, et al. An age-based comparison of chronic pain clinic patients. Int J Geriatr Psychiatry. 2001;16(5):477–483. doi: 10.1002/gps.366. [DOI] [PubMed] [Google Scholar]
- 17.Sturm R, Gresenz C, Sherbourne C, et al. The design of Healthcare for Communities: a study of health care delivery for alcohol, drug abuse, and mental health conditions. Inquiry. 1999;36(2):221–233. [PubMed] [Google Scholar]
- 18.Kemper P, Blumenthal D, Corrigan JM, et al. The design of the community tracking study: a longitudinal study of health system change and its effects on people. Inquiry. 1996;33(2):195–206. [PubMed] [Google Scholar]
- 19.Kessler R, Andrews G, Mroczek D, et al. The World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF) Int J Methods Psychiatr Res. 1998;7:171–185. [Google Scholar]
- 20.Composite International Diagnostic Interview (CIDI) Version 2.1 World Health Organization; Geneva, Switzerland: 1995. [Google Scholar]
- 21.American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM-III-R. American Psychiatric Association; Washington, DC: 1987. [Google Scholar]
- 22.The Alcohol Use Disorders Identification Test (AUDIT) Guidelines for use in primary health care. World Health Organization; Geneva, Switzerland: 1992. [Google Scholar]
- 23.Ware J, Jr., Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Wang PS, Lane M, Olfson M, et al. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 25.Sturm R, Wells KB. How can care for depression become more cost-effective? Jama. 1995;273(1):51–58. [PubMed] [Google Scholar]
- 26.Young AS, Klap R, Sherbourne CD, et al. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry. 2001;58(1):55–61. doi: 10.1001/archpsyc.58.1.55. [DOI] [PubMed] [Google Scholar]
- 27.Stockdale SE, Klap R, Belin TR, et al. Longitudinal patterns of alcohol, drug, and mental health need and care in a national sample of U.S. adults. Psychiatr Serv. 2006;57(1):93–99. doi: 10.1176/appi.ps.57.1.93. [DOI] [PubMed] [Google Scholar]
- 28.Arnow BA, Hunkeler EM, Blasey CM, et al. Comorbid depression, chronic pain, and disability in primary care. Psychosom Med. 2006;68(2):262–268. doi: 10.1097/01.psy.0000204851.15499.fc. [DOI] [PubMed] [Google Scholar]
- 29.Hewitt M, Rowland JH. Mental health service use among adult cancer survivors: analyses of the National Health Interview Survey. J Clin Oncol. 2002;20(23):4581–4590. doi: 10.1200/JCO.2002.03.077. [DOI] [PubMed] [Google Scholar]
- 30.Crabb R, Hunsley J. Utilization of mental health care services among older adults with depression. J Clin Psychol. 2006;62(3):299–312. doi: 10.1002/jclp.20231. [DOI] [PubMed] [Google Scholar]
- 31.Harman JS, Edlund MJ, Fortney JC, et al. The influence of comorbid chronic medical conditions on the adequacy of depression care for older Americans. J Am Geriatr Soc. 2005;53(12):2178–2183. doi: 10.1111/j.1532-5415.2005.00511.x. [DOI] [PubMed] [Google Scholar]
- 32.Klinkman MS. Competing demands in psychosocial care. A model for the identification and treatment of depressive disorders in primary care. Gen Hosp Psychiatry. 1997;19(2):98–111. doi: 10.1016/s0163-8343(96)00145-4. [DOI] [PubMed] [Google Scholar]
- 33.Borowsky SJ, Rubenstein LV, Meredith LS, et al. Who is at risk of nondetection of mental health problems in primary care? J Gen Intern Med. 2000;15(6):381–388. doi: 10.1046/j.1525-1497.2000.12088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sarkisian CA, Hays RD, Mangione CM. Do older adults expect to age successfully? The association between expectations regarding aging and beliefs regarding healthcare seeking among older adults. J Am Geriatr Soc. 2002;50(11):1837–1843. doi: 10.1046/j.1532-5415.2002.50513.x. [DOI] [PubMed] [Google Scholar]
- 35.Sarkisian CA, Lee-Henderson MH, Mangione CM. Do depressed older adults who attribute depression to “old age” believe it is important to seek care? J Gen Intern Med. 2003;18(12):1001–1005. doi: 10.1111/j.1525-1497.2003.30215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Daousi C, MacFarlane IA, Woodward A, et al. Chronic painful peripheral neuropathy in an urban community: a controlled comparison of people with and without diabetes. Diabet Med. 2004;21(9):976–982. doi: 10.1111/j.1464-5491.2004.01271.x. [DOI] [PubMed] [Google Scholar]
- 37.Davies M, Brophy S, Williams R, et al. The prevalence, severity, and impact of painful diabetic peripheral neuropathy in type 2 diabetes. Diabetes Care. 2006;29(7):1518–1522. doi: 10.2337/dc05-2228. [DOI] [PubMed] [Google Scholar]
- 38.Argoff CE, Cole BE, Fishbain DA, et al. Diabetic peripheral neuropathic pain: clinical and quality-of-life issues. Mayo Clin Proc. 2006;81(4 Suppl):S3–11. doi: 10.1016/s0025-6196(11)61474-2. [DOI] [PubMed] [Google Scholar]