Abstract
Cross-priming, the activation of naive CD8+ T cells by dendritic cells presenting Ags synthesized by other cells, is believed to play an important role in the generation of antiviral and antitumor responses. The molecular mechanism(s) underlying cross-priming remain poorly defined and highly controversial. GRP94 (gp96), an abundant endoplasmic reticulum chaperone with innate immune-activating capacity, has been widely reported to play a major role in cross-priming. In this study, we show that cells whose expression of GRP94 is silenced via transient or stable transfection with GRP94-directed small interfering RNAs demonstrate no reduction in their abilities to generate class I peptide complexes in cultured cells or to prime antiviral CD8+ T cell responses in vivo. In demonstrating the dispensability of GRP94, our finding points to the importance of alternative mechanisms for generation of class I peptide complexes from endogenous and exogenous Ags and immunogens.
Antiviral CD8+ T cells recognize viral oligopeptides bound to cell surface MHC class I molecules. CD8+ T cells can play critical roles in antiviral immunity, where they limit viral replication by either lysing infecting cells or releasing cytokines with direct or indirect antiviral activities. For a number of viruses where traditional vaccines that elicit neutralizing Abs are ineffective, there is great interest in developing vaccines that elicit effective antiviral CD8+ T cell responses.
The mechanism of naive CD8+ T cell activation is a critical issue for rationally designing CD8+ T cell-inducing vaccines. There is compelling evidence that naive CD8+ T cells are activated by dendritic cells (DCs)3 located in lymphatic tissues (lymph nodes and spleen) with access to active areas of viral infection (1). It is uncertain, however, to what extent CD8+ T cell activation follows DC presentation of peptides derived from de novo protein synthesis in the presenting DC itself (direct priming) vs peptides derived from extracellular sources, i.e., acquired from virions or infected cells (cross-priming) (2).
The origin of peptides derived from de novo protein synthesis is reasonably well established; a fraction of all protein synthesis is subject to rapid degradation and the resulting peptides provide the relevant Ag source for direct priming (3). Debate continues, however, over how Ags are transferred from infected cells (or tumor cells) to DCs during the process of cross-priming. Evidence from in vitro models supports two major cross-priming routes: 1) Ag internalization, transfer to the cytosol, degradation by proteasomes, and subsequent peptide transfer/loading on MHC class I molecules (4–7) and 2) receptor-mediated uptake of molecular chaperone-peptide complexes, in particular GRP94, and transfer of the peptide, by an as yet undetermined pathway, to MHC class I molecules in the endoplasmic reticulum (ER) (8, 9). Evidence for the post-ER transfer of GRP94-associated peptides to recycling MHC class I molecules has also been presented (10).
Glucose-regulated protein 94 (GRP94, also known as gp96), is a highly abundant ER chaperone that participates in the biogenesis of numerous cell surface and secreted proteins, including a subset of integrins and Toll-like receptors (11–14). A number of reports conclude that GRP94-associated peptides are efficiently acquired by DCs, with CD91, SRA, Lox-1, or CD36 serving as the relevant endocytic receptors (15, 16). GRP94 is also reported to exhibit adjuvant activity by inducing proinflammatory cytokines and chemokines that promote DC maturation (17, 18). The molecular origin and basis of the adjuvant activity attributed to GRP94 is uncertain. The capacity of GRP94 to tightly bind endotoxin in conjunction with the technical hurdle of preparing GRP94 with biologically insignificant levels of endotoxins and purification-derived contaminants (i.e., Con A, a lectin frequently used for GRP94 purification), has lent a significant element of uncertainty to this function (19–21). Also, it has not yet been demonstrated that GRP94 functions in vivo as a peptide-binding protein, and the biochemical basis for GRP94 function as a bona fide (i.e., specific, regulated, and reversible) peptide-binding protein has been questioned (19, 22–25).
None of these studies is conclusive, however, and GRP94 is being actively pursued as a CD8+ T cell vaccine in human clinical trials (26, 27). Since it is of obvious interest and importance to explore its role in cross-priming, we have examined the effect of GRP94 gene knockdown on the cross-priming capacity of cells infected with vaccinia virus (VV), influenza A virus (IAV), or vesicular stomatitis virus (VSV).
Materials and Methods
Mice
All experiments used 6- to 10-wk-old female C57BL/6J mice purchased from Taconic Farms. Mice were housed in the animal care facility at the National Institute of Allergy and Infectious Diseases (NIAID) under specific pathogen-free conditions, maintained on standard mouse chow and water provided ad libitum, and cared for with strict adherence to animal regulations and all studies were performed on an Institutional Animal Care and Use Committee-approved animal study proposal.
Peptides and Abs
Peptides were synthesized and characterized by the Biologic Resource Branch, National Institute of Allergy and Infectious Diseases. Peptides used in this article are described in Table I. For each synthetic peptide, mass spectrometric analysis indicated that the predicted mass form constituted >95% of the material analyzed. Peptides were dissolved in DMSO at 10 mM and stored at −20°C. Abs to GRP94 (rat IgG2a Ab 9G10) were from StressGen. Rabbit anti-peptide Abs were specific for ER resident proteins.
Table I.
Peptides used
| Name | Sequence | Protein/Virus |
|---|---|---|
| OVA257 | SIINFEKL | Chicken OVA |
| B8R | TSYKFESV | VV |
| K3L | YSLPNAGDVI | VV |
| B2R | YSQVNKRYI | VV |
| A3L | KSYNYMLL | VV |
| A42R | YAPVSPIVI | VV |
| L2R | VIYIFTVRL | VV |
| A23R | IGMFNLTFI | VV |
| J3R | SIFRFLNI | VV |
| A8R | ITYRFYLI | VSV |
| VSV-N52 | RGYVYQGL | IAV |
| PA224 | SSLENFRAYV | IAV |
| NP366 | ASNENMDAM | IAV |
| PB1-F2–62 | LSLRNPILV | IAV |
| NP55 | RLIQNSLTI | IAV |
| NS1–114 | RTFSFQLI | IAV |
Cell culture and transfections
L-Kb (L929 stably transfected with Kb molecule), HEK293–94KD, and HEL293-SCRM (HEK293 stably transfected with plasmids encoding a GRP94-directed or sequence scrambled siRNA were cultured in DMEM containing 10% FBS and DC-like DC2.4 cells (H-2b) were cultured in IMDM containing 10% FBS. NP-S-EGFP plasmid transient transfections were performed with Lipofectamine 1 day before injections. Transient siRNA transfections were conducted by transfecting 1–2 × 106 L-Kb cells in solution V using Amaxa nucleofector and the T-24 program. siRNA specific for GRP94 and neo (5′-pGGCUCAAGGACAGAUGAUGtt and pAAUGAACUGCAGGACGAGGCAtt, respectively) were used at 10 nM. As indicated, cells were infected 3 days after siRNA transfection. All siRNAs were purchased from Dharmacon. siRNA knockdown efficacy was determined by immunoblotting using GRP94-specific Ab.
Viral infections
rVVs or rVSVs containing the fusion protein mCherry-ub-OVA257, NP-SIINFEKL-EGFP, NP-S-mCherry, or OVA were used at a multiplicity of infection of 10. Cells were incubated with the viruses for 20 min at 37°C, with occasional mixing, in balanced salt solution containing 0.1% BSA. For the PR8-OVA infections (multiplicity of infection = 10), cells were washed and resuspended in autoclavable minimal essential medium with 0.1% BSA at pH 6.8 and incubated at 37°C for 1 h. Cells were then incubated at 37°C in growth medium for the remainder of the assay.
Flow cytometry
Kb-OVA257 levels were determined by incubating cells for 30 min on ice with 25-D.1.16 Ab conjugated with Alexa Fluor 647. Kb levels were determined by FITC-conjugated anti-Kb Ab (AF6-88.5; BD, Pharmingen). Cellular FITC and Alexa Fluor 647 levels were determined by an LSR II (BD Biosciences) using FACSDiva (BD Biosciences) software and data were analyzed using FlowJo (Tree Star) software.
Cross-priming experiments with intracellular cytokine staining
HEK293–94KD and HEL293-SCRM cells were infected with rVVs or rVSV at 10 PFU/cell, incubated for 6 h at 37°C to allow for viral gene expression, and then exposed to 254 nM light at 4 mW/cm2 for 1 h on ice. This treatment suffices to reduce the PFUs to below detection and abrogate the cross-priming capacity of cells infected with rVVs expressing short-lived minigene products (28). Alternatively, cells were infected for 5 h with A/Puerto Rico/8/34 influenza virus (PR8) with SIINFEKL inserted into the neuraminidase (29). To prevent infection with PR8, cells were coinjected with a sufficient amount of the neutralizing mAb H28-E23 to block the immunogenicity of a substantial dose of PR8 (30). For each condition, 1 × 107 cells were injected i.p. per mouse. Six days subsequent, for the vaccinia model, and 7 days subsequent, for the influenza model, splenic and peritoneal cells were harvested from primed animals, suspended in RPMI 1640 medium plus 10% FBS, and seeded at 2 × 106 cells/well in U-bottom 96-well plates. Peptides were added to wells to a final concentration of 0.5 μM. Cells were incubated initially for 2 h at 37°C and then for 3 h with brefeldin A (Sigma-Aldrich) at 10 μg/ml. Dead cells were first stained with EMA at 5 μg/ml in balanced salt solution/BSA for 15 min in the dark on ice followed by 15 min on ice in light. Cells were then stained with FITC anti-CD8α mAb on ice for 30 min, washed, and fixed with 1% paraformaldehyde in PBS at room temperature for 20 min, then further stained with Alexa Fluor 647-conjugated anti-IFN-γ in PBS containing 0.1% saponin (Sigma-Aldrich). Stained cells were analyzed on an LSR II flow cytometer with live-gate on the CD8+ cells. A total of 150,000 cells were normally acquired and analyzed with FlowJo software (Tree Star).
OT-1 proliferation experiments
OT-1 cells (TCR-transgenic CD8+ T cells specific for Kb-OVA257) were purified from spleen and lymph nodes of OT-1 mice by positive selection with magnetic beads (Miltenyi Biotec). Cells were labeled with CFSE (1.7 mM for 10 min) and injected via the tail vein (2.5 × 106/mouse) into CD45.1 C57BL/6 mice. One × 107 HEK-293 cells transfected with DNA or infected with different viruses as described above were injected i.p. 3 h after injection of OT-1 cells. Spleens were harvested ~72 h after OT-1 injection and OT-1 proliferation was determined by staining for CD8 and CD45.1 and gating for CFSE-labeled CD8+CD45.1+ cells by an LSR II flow cytometer. A total of 2 million events were normally acquired and analyzed with FlowJo software (Tree Star).
Results
Suppression of GRP94 expression does not diminish Ag processing and presentation
GRP94 has been proposed to play at least two critical roles in Ag processing and presentation: acceptor of peptides transported into the ER by the TAP and aminopeptidase functioning in the proteolytic trimming of TAP-transported peptides to a length optimal for class I binding (31). As peptide acceptor, GRP94 is thought to bind the antigenic peptide repertoire of the cell, thereby enabling it to serve as an ideal peptide vector in Ag cross-presentation (32).
To identify a role(s) for GRP94 in the cross-presentation of viral Ags, we first examined the Ag presentation capacity of viral protein-expressing cells using control and GRP94-siRNA knockdown cell lines. We silenced GRP94 expression by transfecting L-Kb cells with siRNA specific for either GRP94 or, as a negative control, aminoglycoside phosphotransferase (neo). GRP94-siRNA reduced GRP94 expression to near undetectable levels (>95% reduction, relative to untransfected, mock-transfected, or neo-siRNA transfected cells) as measured by immunoblotting (Fig. 1A). siRNA-transfected cells were subsequently infected with either a rVV expressing a reporter fusion protein, NP-S-mCherry, consisting of IAV nucleoprotein (NP) containing in-frame OVA257 peptide (SIINFEKL) followed by mCherry fluorescent protein, or a rVV expressing mCherry-Ub-S, consisting of mCherry fused to ubiquitin and terminating in the OVA257 peptide. Previous studies have demonstrated that ubiquitin hydrolases cleave the fusion protein from the ubiquitin COOH terminus, releasing the peptide for presentation on MHC molecules (33) Following rVV infection, cell aliquots were sampled every hour for 5.5 h, and cell surface Kb-SIINFEKL complex levels were quantitated via flow cytometry using the 25-D.1.16 TCR-like mAb (34).
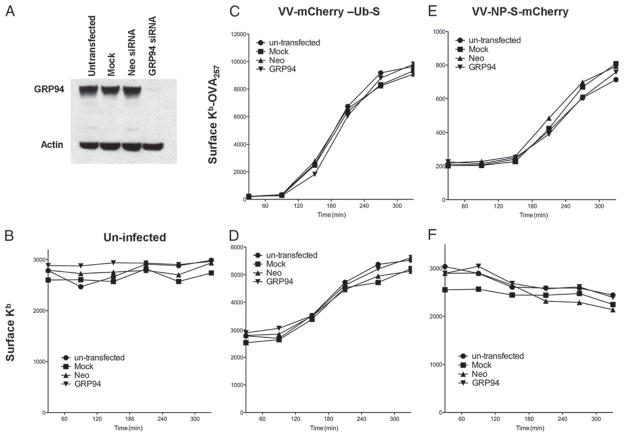
FIGURE 1.
GRP94 has no essential role in Ag processing and presentation. A, Knockdown of GRP94 was confirmed by Western blot analysis. L-Kb cells were untransfected (●), mock transfected (■), transfected with control Neo siRNA (▲), or transfected with GRP94 siRNA (▼). Cells were infected 4–5 days later with VV-mCherry-Ub- S (C and D) or VV-NP-S-mCherry (E and F) or uninfected as a control (B). Samples were taken every 1h up to 5.5 h after infection. Levels of surface Kb-OVA257 were then measured by staining with Alexa Fluor 647-labeled 25-D.1.16 (C and E), and levels of the surface Kb molecule (B, D, and F) were determined by staining with anti-Kb Ab (HB176) followed by a secondary FITC-conjugated anti-mouse Ab. The experiment was repeated two times.
As seen in Fig. 1, GRP94 knockdown had no discernible effect on the capacity of cells to generate Kb-SIINFEKL complexes from NP-S-mCherry (Fig. 1E) or mCherry-Ub-S (Fig. 1C), which is a >10-fold efficient source of Kb-SIINFEKL due to the direct liberation of SIINFEKL from the nascent gene. The four-cell populations examined expressed the indicator FP at nearly identical levels (data not shown). Silencing GRP94 expression did not diminish the total amount of conformed total cell surface Kb molecules in uninfected cells (Fig. 1B) or cells infected with either rVV (Fig. 1, D and F).
Together, these data indicate that GRP94 does not contribute to a rate-limiting step(s) in the generation of either viral or self-peptide-class I complexes or the biogenesis of MHC class I molecules.
In vivo analysis of GRP94 function in cross-priming
Next, we evaluated GRP94 function in cross-priming, by immunizing B6 mice with HEK-293 cells expressing NP-S-GFP from different vectors. Because they are of human origin, HEK-293 cells cannot directly present Ags to murine CD8+ T cells (or donate Kb-SIINFEKL complexes to DCs via “cross-dressing” (35)). Therefore, assuming cell- associated virus is completely inactivated, activation of naive CD8+ T cells by injected HEK-293 cells must occur via cross-priming.
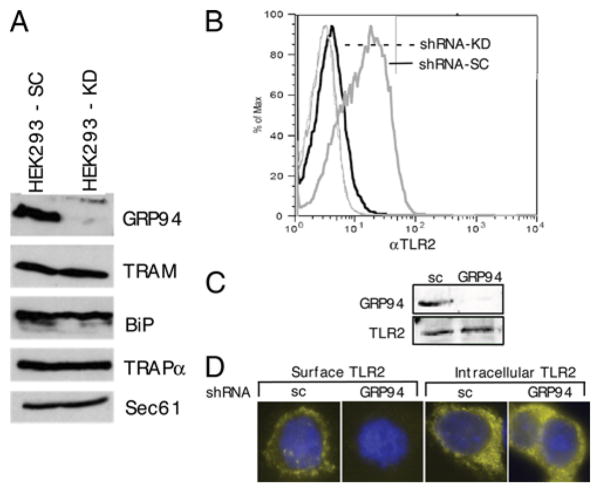
HEK293 cells were stably transfected with GRP94-targeting siRNA or siRNA encoding a scrambled version of the GRP94-targeting sequence. Via immunoblotting, GRP94 is undetectable in the knockdown cells, while the levels of TRAM, BiP, TRAPα, and Sec61 are similar between control and knockdown cells, indicating that ER resident chaperones and integral membrane proteins are expressed at normal levels in the absence of GRP94 expression (Fig. 2A). The lack of functional GRP94 was confirmed by the intracellular accumulation of TLR2 (Fig. 2, B–D), which requires GRP94 for export from the ER (36). In addition, silencing of GRP94 expression was not accompanied by discernible changes in cell doubling time or morphology (data not shown), consistent with previous studies where GRP94 expression was knocked out via chemical mutagenesis (37) (Fig. 2).
FIGURE 2.
Knockdown of GRP94 from HEK-293 cells. A, Western blot analysis of HEK-293 cells stably transfected with GRP94 or control scramble siRNA to determined expression levels of GRP94 and other ER proteins indicated. B–D, Stable HEK293 cell lines expressing short hairpin RNA (shRNA) directed against GRP94 (shRNA-GRP94) or scrambled shRNA control (shRNA-sc) were transfected with a plasmid encoding FLAG-tagged TLR2. Forty-eight hours posttransfection, TLR2 surface expression was examined by flow cytometry using FLAG epitope-specific mAb (B). Histograms for the shRNA-GRP94-expressing cells are represented by the dark line; the gray line represents the shRNA-sc-expressing cells. Immunoblot confirmed equal amounts of TLR2 expression in total cell extracts (C). The presence of TLR2 in the ER of GRP94 knockdown cells was shown by confocal microscopy of fixed, permeabilized cells (D). Examination of fixed, unpermeabilized cells confirmed the lack of surface expression in GRP knockdown cells.
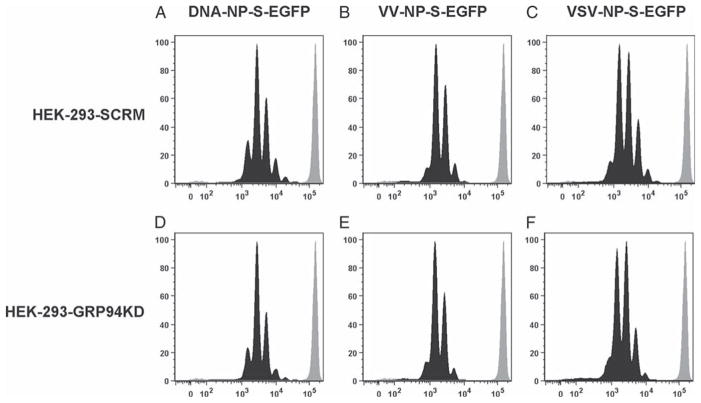
HEK-293 cells were infected with rVV or rVSV expressing NP-S-GFP or transfected with a plasmid expressing NP-S-GFP under the control of the CMV promoter and injected into B6 mice that had received OT-I TCR-transgenic CD8+ T cells. OT-I cells are specific for Kb-SIINFEKL complexes and their division (monitored by CFSE fluorescence) following adoptive transfer provides a sensitive measure of cross-priming (38). If GRP94 contributes significantly to cross-priming in an in vivo viral infection model, OT-1 division would be predicted to be lower in the knockdown vs the control cell injection animals. As seen in Fig. 3, OT-1 division was identical in all scenarios examined, indicating that suppression of GRP94 expression did not affect the cross-priming capacity of HEK-293 expressing NP-S-GFP via either infection or DNA transfection.
FIGURE 3.
GRP94 is not required for in vivo OVA257 cross-priming measured by OT-1 CD8+ T cell division. Donor HEK-293 cells expressing GRP94 (A–C) or knockdown of GRP94 (D–F) were transfected with NP-S-EGFP DNA (A and D) or infected with VV-NP-S-EGFP (B and E) or VSV-NP-S-EGFP (C and F) and injected into B6 mice. The proliferation of CFSE-labeled OT-1 CD8+ T cells was measured 3 days after adaptive transfer. In each graph, the black histogram represents the infected or transfected cells and the gray histogram represents control cells without infection or transfection. Each experiment was repeated two times.
Efficient cross-priming of peptides derived from vaccinia and influenza viruses expressed in GRP94-silenced cells
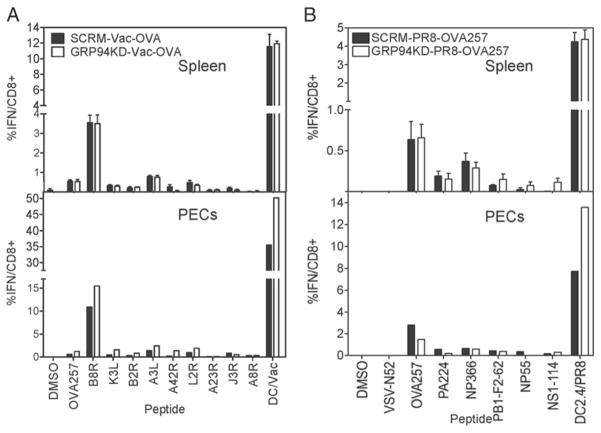
We next determined the GRP94 contribution to cross-priming by measuring the ability of HEK-293 cells to induce primary CD8+ T cell responses to peptides encoded by rVVs expressing full-length OVA or recombinant IAV expressing SIINFEKL in the stalk region of the neuraminidase (39). In these experiments, mice were immunized by i.p. injection of rVV-infected cells and CD8+ T cell responses were measured at day 6. Analyses were performed on both peritoneal exudate cells (PECs) and splenocytes by ex vivo intracellular cytokine staining using SIINFEKL or immunodominant viral peptides or DMSO as a negative control. Total antiviral responses were estimated using APCs infected with VV or IAV. As seen in Fig. 4, GRP94 knockdown cells were capable of eliciting responses to SIINFEKL, eight VV, and five IAV determinants. Consistent with the results reported above, the overall in vivo antiviral immunological responses to GRP94 knockdown cells were equal or even greater than the control cells.
FIGURE 4.
GRP94 show no effect on cross-priming of viral peptides measured by intracellular staining for INF-γ. Mice were immunized i.p. with infected HEK-293 cells expressing GRP94 or GRP94 knocked down. Six days later, splenocytes and PECs were tested for IFN-γ accumulation following restimulation with the indicated peptides or infected DC2.4. DMSO was used as a negative no-peptide control. A, Cross-priming of cells infected with rVV-OVA. B, Cross-priming of cells infected with PR8-OVA257. Values were subtracted from background obtained from wells receiving no peptides and are expressed as mean ± SE of three individual mice in each group for splenic responses. For peritoneal responses, PECs were pooled. Each experiment was repeated two times.
Discussion
Our findings demonstrate that for multiple Ags and viral systems, GRP94 is dispensable for the generation of both peptide class I complexes in cultured cells and immunogens in donor cells with cross-priming activity. In the latter case, although these findings do not address the possibility that other chaperones function in Ag presentation and cross-priming, they are consistent with previous studies that indicate that protein- based cross-priming is the rule rather than the exception (5–7, 40), and also from the original findings of Rammensee and colleagues (41), extended now to many systems, that naturally processed antigenic peptides are, with few exceptions (28), extremely short-lived in cells unless protected by binding to MHC class I molecules. We note that our
The view that chaperones and heat shock proteins could serve as universal immunogens, with application to human cancer immunotherapy, has generated tremendous interest among clinicians, immunologists, and chaperone biologists. In the case of GRP94, the available clinical trial data have not, however, convincingly demonstrated substantial utility for this application (42, 43).
Beyond the complexities that befall interpretation of clinical immunotherapy data, a key question remains unanswered, does GRP94 associate stably with antigenic peptides in vivo? Arguing against such a function are the findings of this study, the inability to detect a substantial and diverse population of associated peptides in biochemically purified GRP94 (18, 21–23) and, to a lesser degree, the kinetic/structural characteristics of the in vitro peptide complexation reaction, where associated synthetic peptides are stable to SDS (17, 44).
In contrast, in models using cells engineered to secrete GRP94, specific CD8+ T cell responses to cell-derived Ags have been clearly demonstrated (45–48). Some measure of caution, however, is necessary in concluding that such data identify an in vivo peptide-binding function for GRP94. Because GRP94 elicits substantial innate immune responses, it is possible that GRP94-secreting (tumor) cells are de facto high-priority immunosurveillance targets and as a result are efficiently processed for in vivo cell-based cross-priming reactions.
From a clinical standpoint, whether the efficacy of tumor cell-secreted GRP94 derives from GRP94-peptide complexes or APC-dependent processing of GRP94-secreting (tumor) cells is of somewhat limited significance. Defining an essential role for GRP94 in Ag processing and/or peptide cross-priming does require, however, an unequivocal demonstration that GRP94 can stably associate with a diverse peptide pool and that such an activity is an intrinsic function of the native protein. Nearly two decades after the initial proposal of such an intrinsic activity (49), such evidence does not exist.
Acknowledgments
We are grateful to Glennys Reynoso for outstanding technical assistance.
Footnotes
Abbreviations used in this paper: DC, dendritic cell; ER, endoplasmic reticulum; GRP94, glucose-regulated protein 94; IAV, influenza A virus; neo, aminoglycoside phosphotransferase; NP, nucleoprotein, VV, vaccinia virus; VSV, vesicular stomatitis virus; siRNA, small interfering RNA; PEC, peritoneal exudate cell; shRNA, short hairpin RNA.
Disclosures
The authors have no financial conflict of interest.
J.R.B. and J.W.Y. are supported by the Division of Intramural Research, National Institute of Allergy and Infectious Diseases. C.V.N. is supported by Grant CA104392 from the National Institutes of Health.
References
- 1.Steinman RM. Dendritic cells: understanding immunogenicity. Eur J Immunol. 2007;37(Suppl 1):S53–S60. doi: 10.1002/eji.200737400. [DOI] [PubMed] [Google Scholar]
- 2.Yewdell JW, Haeryfar SM. Understanding presentation of viral antigens to CD8+ T cells in vivo: the key to rational vaccine design. Annu Rev Immunol. 2005;23:651–682. doi: 10.1146/annurev.immunol.23.021704.115702. [DOI] [PubMed] [Google Scholar]
- 3.Yewdell JW. Plumbing the sources of endogenous MHC class I peptide ligands. Curr Opin Immunol. 2007;19:79–86. doi: 10.1016/j.coi.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 4.Shen L, Rock KL. Cellular protein is the source of cross-priming antigen in vivo. Proc Natl Acad Sci USA. 2004;101:3035–3040. doi: 10.1073/pnas.0308345101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Norbury CC, Basta S, Donohue KB, Tscharke DC, Princiotta MF, Berglund P, Gibbs J, Bennink JR, Yewdell JW. CD8+ T cell cross-priming via transfer of proteasome substrates. Science. 2004;304:1318–1321. doi: 10.1126/science.1096378. [DOI] [PubMed] [Google Scholar]
- 6.Wolkers MC, Brouwenstijn N, Bakker AH, Toebes M, Schumacher TN. Antigen bias in T cell cross-priming. Science. 2004;304:1314–1317. doi: 10.1126/science.1096268. [DOI] [PubMed] [Google Scholar]
- 7.Basta S, Stoessel R, Basler M, van den Broek M, Groettrup M. Cross-presentation of the long-lived lymphocytic choriomeningitis virus nucleoprotein does not require neosynthesis and is enhanced via heat shock proteins. J Immunol. 2005;175:796–805. doi: 10.4049/jimmunol.175.2.796. [DOI] [PubMed] [Google Scholar]
- 8.Binder RJ, Srivastava PK. Peptides chaperoned by heat-shock proteins are a necessary and sufficient source of antigen in the cross-priming of CD8+ T cells. Nat Immunol. 2005;6:593–599. doi: 10.1038/ni1201. [DOI] [PubMed] [Google Scholar]
- 9.Murshid A, Gong J, Calderwood SK. Heat-shock proteins in cancer vaccines: agents of antigen cross-presentation. Expert Rev Vaccines. 2008;7:1019–1030. doi: 10.1586/14760584.7.7.1019. [DOI] [PubMed] [Google Scholar]
- 10.Berwin B, Rosser MF, Brinker KG, Nicchitta CV. Transfer of GRP94(Gp96)-associated peptides onto endosomal MHC class I molecules. Traffic. 2002;3:358–366. doi: 10.1034/j.1600-0854.2002.30505.x. [DOI] [PubMed] [Google Scholar]
- 11.Randow F, Seed B. Endoplasmic reticulum chaperone gp96 is required for innate immunity but not cell viability. Nat Cell Biol. 2001;3:891–896. doi: 10.1038/ncb1001-891. [DOI] [PubMed] [Google Scholar]
- 12.Melnick J, Dul J, Argon Y. Sequential interaction of the chaperones BiP and GRP94 with immunoglobulin chains in the endoplasmic reticulum. Nature. 1994;370:373–375. doi: 10.1038/370373a0. [DOI] [PubMed] [Google Scholar]
- 13.Yang Y, Liu B, Dai J, Srivastava PK, Zammit DJ, Lefrançois L, Li Z. Heat shock protein gp96 is a master chaperone for Toll-like receptors and is important in the innate function of macrophages. Immunity. 2007;26:215–226. doi: 10.1016/j.immuni.2006.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dollins D, Warren J, Immormino R, Gewirth D. Structures of GRP94-nucleotide complexes reveal mechanistic differences between the hsp90 chaperones. Mol Cell. 2007;28:41–56. doi: 10.1016/j.molcel.2007.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berwin B, Hart J, Rice S, Gass S, Pizzo S, Post S, Nicchitta C. Scavenger receptor-A mediates gp96/GRP94 and calreticulin internalization by antigen-presenting cells. EMBO J. 2003;22:6127–6136. doi: 10.1093/emboj/cdg572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tewalt EF, Maynard JC, Walters JJ, Schell AM, Berwin BL, Nicchitta CV, Norbury CC. Redundancy renders the glycoprotein 96 receptor scavenger receptor A dispensable for cross priming in vivo. Immunology. 2008;125:480–491. doi: 10.1111/j.1365-2567.2008.02861.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Suto R, Srivastava PK. A mechanism for the specific immunogenicity of heat shock protein-chaperoned peptides. Science. 1995;269:1585–1588. doi: 10.1126/science.7545313. [DOI] [PubMed] [Google Scholar]
- 18.Binder RJ, Harris ML, Menoret A, Srivastava PK. Saturation, competition, and specificity in interaction of heat shock proteins (hsp) gp96, hsp90, and hsp70 with CD11b+ cells. J Immunol. 2000;165:2582–2587. doi: 10.4049/jimmunol.165.5.2582. [DOI] [PubMed] [Google Scholar]
- 19.Wallin RP, Lundqvist A, More SH, von Bonin A, Kiessling R, Ljunggren HG. Heat-shock proteins as activators of the innate immune system. Trends Immunol. 2002;23:130–135. doi: 10.1016/s1471-4906(01)02168-8. [DOI] [PubMed] [Google Scholar]
- 20.Demine R, Walden P. Testing the role of gp96 as peptide chaperone in antigen processing. J Biol Chem. 2005;280:17573–17578. doi: 10.1074/jbc.M501233200. [DOI] [PubMed] [Google Scholar]
- 21.Tsan MF, Gao B. Cytokine function of heat shock proteins. Am J Physiol. 2004;286:C739–C744. doi: 10.1152/ajpcell.00364.2003. [DOI] [PubMed] [Google Scholar]
- 22.Nicchitta CV, Carrick DM, Baker-Lepain JC. The messenger and the message: gp96 (GRP94)-peptide interactions in cellular immunity. Cell Stress Chaperones. 2004;9:325–331. doi: 10.1379/CSC-62.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ying M, Flatmark T. Binding of the viral immunogenic octapeptide VSV8 to native glucose-regulated protein Grp94 (gp96) and its inhibition by the physiological ligands ATP and Ca2+ FEBS J. 2006;273:513–522. doi: 10.1111/j.1742-4658.2005.05084.x. [DOI] [PubMed] [Google Scholar]
- 24.Javid B, MacAry PA, Lehner PJ. Structure and function: heat shock proteins and adaptive immunity. J Immunol. 2007;179:2035–2040. doi: 10.4049/jimmunol.179.4.2035. [DOI] [PubMed] [Google Scholar]
- 25.Demine R, Walden P. Testing the role of gp96 as peptide chaperone in antigen processing. J Biol Chem. 2005;280:17573–17578. doi: 10.1074/jbc.M501233200. [DOI] [PubMed] [Google Scholar]
- 26.Testori A, Richards J, Whitman E, Mann G, Lutzky J, Camacho L, Parmiani G, Tosti G, Kirkwood J, Hoos A, et al. Phase III comparison of vitespen, an autologous tumor-derived heat shock protein gp96 peptide complex vaccine, with physician’s choice of treatment for stage IV melanoma: the C-100-21 Study Group. J Clin Oncol. 2008;1:955–962. doi: 10.1200/JCO.2007.11.9941. [DOI] [PubMed] [Google Scholar]
- 27.Amato RJ. Heat-shock protein-peptide complex-96 for the treatment of cancer. Expert Opin Biol Ther. 2007;7:1267–1273. doi: 10.1517/14712598.7.8.1267. [DOI] [PubMed] [Google Scholar]
- 28.Lev A, Takeda K, Zanker D, Maynard JC, Dimberu P, Waffarn E, Gibbs J, Netzer N, Princiotta MF, Neckers L, et al. The exception that reinforces the rule: crosspriming by cytosolic peptides that escape degradation. Immunity. 2008;28:787–798. doi: 10.1016/j.immuni.2008.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jenkins MR, Webby R, Doherty PC, Turner SJ. Addition of a prominent epitope affects influenza A virus-specific CD8+ T cell immunodominance hierarchies when antigen is limiting. J Immunol. 2006;177:2917–2925. doi: 10.4049/jimmunol.177.5.2917. [DOI] [PubMed] [Google Scholar]
- 30.Chen W, Masterman KA, Basta S, Haeryfar SM, Dimopoulos N, Knowles B, Bennink JR, Yewdell JW. Cross-priming of CD8+ T cells by viral and tumor antigens is a robust phenomenon. Eur J Immunol. 2004;34:194–199. doi: 10.1002/eji.200324257. [DOI] [PubMed] [Google Scholar]
- 31.Menoret A, Li Z, Niswonger ML, Altmeyer A, Srivastava PK. An endoplasmic reticulum protein implicated in chaperoning peptides to major histocompatibility of class I is an aminopeptidase. J Biol Chem. 2001;276:33313–33318. doi: 10.1074/jbc.M103383200. [DOI] [PubMed] [Google Scholar]
- 32.Srivastava P. Interaction of heat shock proteins with peptides and antigen presenting cells: chaperoning of the innate and adaptive immune responses. Annu Rev Immunol. 2002;20:395–425. doi: 10.1146/annurev.immunol.20.100301.064801. [DOI] [PubMed] [Google Scholar]
- 33.Fruci D, Lauvau G, Saveanu L, Amicosante M, Butler RH, Polack A, Ginhoux F, Lemonnier F, Firat H, van Endert PM. Quantifying recruitment of cytosolic peptides for HLA class I presentation: impact of TAP transport. J Immunol. 2003;170:2977–2984. doi: 10.4049/jimmunol.170.6.2977. [DOI] [PubMed] [Google Scholar]
- 34.Porgador A, Yewdell JW, Deng Y, Bennink JR, Germain RN. Localization, quantitation, and in situ detection of specific peptide-MHC class I complexes using a monoclonal antibody. Immunity. 1997;6:715–726. doi: 10.1016/s1074-7613(00)80447-1. [DOI] [PubMed] [Google Scholar]
- 35.Yewdell JW, Haeryfar SM. Understanding presentation of viral antigens to CD8+ T cells in vivo: the key to rational vaccine design. Annu Rev Immunol. 2005;23:651–682. doi: 10.1146/annurev.immunol.23.021704.115702. [DOI] [PubMed] [Google Scholar]
- 36.Randow F, Seed B. Endoplasmic reticulum chaperone gp96 is required for innate immunity but not cell viability. Nat Cell Biol. 2001;3:891–896. doi: 10.1038/ncb1001-891. [DOI] [PubMed] [Google Scholar]
- 37.Randow F, Seed B. Endoplasmic reticulum chaperone gp96 is required for innate immunity but not cell viability. Nat Cell Biol. 2001;3:891–896. doi: 10.1038/ncb1001-891. [DOI] [PubMed] [Google Scholar]
- 38.Kurts C, Heath WR, Carbone FR, Allison J, Miller JF, Kosaka H. Constitutive class I-restricted exogenous presentation of self antigens in vivo. J Exp Med. 1996;184:923–930. doi: 10.1084/jem.184.3.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jenkins MR, Webby R, Doherty PC, Turner SJ. Addition of a prominent epitope affects influenza A virus-specific CD8+ T cell immunodominance hierarchies when antigen is limiting. J Immunol. 2006;177:2917–2925. doi: 10.4049/jimmunol.177.5.2917. [DOI] [PubMed] [Google Scholar]
- 40.Shen LJ, Rock KL. Cellular protein is the source of cross-priming antigen in vivo. Proc Natl Acad Sci USA. 2004;101:3035–3040. doi: 10.1073/pnas.0308345101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Falk K, Rötzschke O, Rammensee HG. Cellular peptide composition governed by major histocompatibility complex class I molecules. Nature. 1990;348:248–251. doi: 10.1038/348248a0. [DOI] [PubMed] [Google Scholar]
- 42.Wood C, Srivastava P, Bukowski R, Lacombe L, Gorelov AI, Gorelov S, Mulders P, Zielinski H, Hoos A, Teofilovici F, et al. An adjuvant autologous therapeutic vaccine (HSPPC-96; vitespen) versus observation alone for patients at high risk of recurrence after nephrectomy for renal cell carcinoma: a multicentre, open-label, randomised phase III trial. Lancet. 2008;372:145–154. doi: 10.1016/S0140-6736(08)60697-2. [DOI] [PubMed] [Google Scholar]
- 43.Testori A, Richards J, Whitman E, Mann GB, Lutzky J, Camacho L, Parmiani G, Tosti G, Kirkwood JM, Hoos A, et al. Phase III comparison of vitespen, an autologous tumor-derived heat shock protein gp96 peptide complex vaccine, with physician’s choice of treatment for stage IV melanoma: the C-100-21 Study Group. J Clin Oncol. 2008;26:955–962. doi: 10.1200/JCO.2007.11.9941. [DOI] [PubMed] [Google Scholar]
- 44.Gidalevitz T, Biswas C, Ding H, Schneidman-Duhovny D, Wolfson HJ, Stevens F, Radford S, Argon Y. Identification of the N-terminal peptide binding site of glucose-regulated protein 94. J Biol Chem. 2004;279:16543–16552. doi: 10.1074/jbc.M313060200. [DOI] [PubMed] [Google Scholar]
- 45.Schreiber TH, V, Deyev V, Rosenblatt JD, Podack ER. Tumor-induced suppression of CTL expansion and subjugation by gp96-Ig vaccination. Cancer Res. 2009;69:2026–2033. doi: 10.1158/0008-5472.CAN-08-3706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Oizumi S, Strbo N, Pahwa S, Deyev V, Podack ER. Molecular and cellular requirements for enhanced antigen cross-presentation to CD8 cytotoxic T lymphocytes. J Immunol. 2007;179:2310–2317. doi: 10.4049/jimmunol.179.4.2310. [DOI] [PubMed] [Google Scholar]
- 47.Dai J, Liu B, Caudill MM, Zheng H, Qiao Y, Podack ER, Li Z. Cell surface expression of heat shock protein gp96 enhances cross-presentation of cellular antigens and the generation of tumor-specific T cell memory. Cancer Immun. 2003;3:1. [PubMed] [Google Scholar]
- 48.Yamazaki K, Nguyen T, Podack ER. Cutting edge: tumor secreted heat shock-fusion protein elicits CD8 cells for rejection. J Immunol. 1999;163:5178–5182. [PubMed] [Google Scholar]
- 49.Srivastava PK, Heike M. Tumor-specific immunogenicity of stress-induced proteins: convergence of two evolutionary pathways of antigen presentation? Semin Immunol. 1991;3:57–64. [PubMed] [Google Scholar]