Abstract
Nitric oxide (NO) is a unique and nearly ubiquitous molecule that is widely utilized as a signaling molecule in cells throughout the body. NO is highly diffusible, labile, and multiply reactive, suiting it well for its role as an important regulator of a number of diverse biologic processes, including vascular tone and permeability, platelet adhesion, neurotransmission, and mitochondrial respiration. NO can protect cells against antioxidant injury, can inhibit leukocyte adhesion, and can participate in antimicrobial defense, but can also have deleterious effects, including inhibition of enzyme function, promotion of DNA damage, and activation of inflammatory processes. This molecule's chemistry dictates its biologic activity, which can be both direct and indirect. In addition, NO has bimodal effects in a number of cells, maintaining homeostasis at low doses, and participating in pathophysiology in others. Perturbation of NO regulation is involved in the most important and prevalent disease processes in critical care units, including sepsis, acute lung injury, and multiple organ failure. Given that NO is ubiquitous, highly diffusible, and promiscuously reactive, its regulation is complex. The NO concentration, kinetics, and localization, both inside and outside the cell, are clearly crucial factors. In the present update we review a selection of studies that have yielded important information on these complex but important issues. Interpretation of these and other studies aimed at elucidating physiologic and pathophysiologic roles of NO must take this complexity into account. A full review of the role of NO in these diseases is beyond the scope of the current manuscript; the present article will focus on recent advances in understanding the complex role of NO in health and disease.
Introduction
Nitric oxide (NO) is a unique and nearly ubiquitous molecule that is widely utilized as a signaling molecule in cells throughout the body. NO is a highly diffusible, labile, and multiply reactive free radical gas, suiting it well for its role as an important regulator of a number of diverse biologic processes, including vascular tone and permeability, platelet adhesion, neurotransmission, and mitochondrial respiration. NO can protect cells against antioxidant injury, can inhibit leukocyte adhesion, and can participate in antimicrobial defense, but can also have deleterious effects, including inhibition of enzyme function, promotion of DNA damage, and activation of inflammatory processes.
The chemistry of NO dictates its biologic activity. NO has direct effects on metal complexes and alkyl radicals – including, most importantly, guanylate cyclase, cytochromes, and lipid radicals – but also has indirect effects through nitration to form nitrotyrosine, through nitrosation to form nitrosothiols and nitrosamines, and through combination with oxidative radicals, the most important of which is peroxynitrite (see Figure 1) [1,2]. NO acts as a second messenger by activating soluble guanylate cyclase and participating in signal transduction pathways involving cyclic GMP, but also operates independently of guanylate cyclase [2]. NO regulates the cytoplasmic redox balance and also signal transduction, either by regulating cytoplasmic and mitochondrial calcium signals or by post-translational modification of intracellular proteins. NO is a bifunctional modulator of cell death, capable of either stimulating or inhibiting apoptosis.
Figure 1.
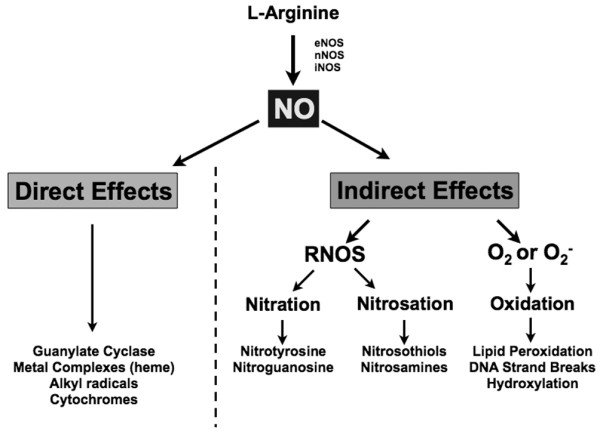
Direct and indirect actions of nitric oxide. Nitric oxide (NO) has direct effects on metal complexes and alkyl radicals, including guanylate cyclase, cytochromes, and lipid radicals. NO also has indirect actions through nitration to form nitrotyrosine, through nitrosation to form nitrosothiols and nitrosamines, and through combination with oxidative radicals, with the potential for subsequent peroxidation of lipids, DNA strand breaks, and hydroxylation. eNOS, endothelial NO synthase; iNOS, inducible NO synthase; nNOS, neuronal NO synthase; O2-, superoxide. Reprinted from Free Radical Biology and Medicine, 45(1), Douglas D. Thomas, Lisa A. Ridnour, Jeffrey S. Isenberg, Wilmarie Flores-Santana, Christopher H. Switzer, Sonia Donzelli, Perwez Hussain, Cecilia Vecoli, Nazareno Paolocci, Stefan Ambs, Carol A. Colton, Curtis C. Harris, David D. Roberts and David A. Wink, The chemical biology of nitric oxide: Implications in cellular signaling, 14 Pages, Copyright (2008), with permission from Elsevier.
Given that NO is ubiquitous, highly diffusible, and promiscuously reactive, one might well ask how it is regulated with precision. The answers are complex and remain to be fully elucidated, but the NO concentration, kinetics, and localization, both inside and outside the cell, are clearly crucial factors [2]. In the present update we shall review a selection of studies that have yielded important information on these complex but important issues. Interpretation of these and other studies aimed at elucidating physiologic and pathophysiologic roles of NO must take this complexity into account.
Perturbation of NO regulation is involved in the most important and prevalent disease processes in critical care units, including sepsis, acute lung injury, and multiple organ failure [3]. A full review of the role of NO in these diseases is beyond the scope of the current manuscript; the present article will focus on recent advances in understanding the complex role of NO in health and disease.
Nitric oxide synthases
NO is synthesized from L-arginine and oxygen by the enzyme nitric oxide synthase (NOS). At least three distinct isoforms of NOS are known, including neuronal nitric oxide synthase (nNOS, NOS1), inducible nitric oxide synthase (iNOS, NOS2), and endothelial nitric oxide synthase (eNOS, NOS3) enzymes. Whereas iNOS activity depends on transcription, eNOS and nNOS are constitutively expressed and are activated by elevated intracellular calcium; iNOS gene expression is modulated by inflammatory mediators, such as the cytokines TNFα, IFNγ, and lipopolysaccharide, which activate transcription factors such as NFκB or activator protein 1; and the iNOS isoform generates much larger quantities of NO (nanomolar range) than constitutive NOS isoforms (picomolar range) [4].
Some of the diversity of cellular responses to NO can be explained by different actions of NO at different concentration levels [2]. For example, physiological actions due to cyclic-GMP-mediated processes predominate at NO concentrations ranging from 1 to 30 nM, tissue repair processes including AKT phosphorylation (30 to 100 nM) and hypoxia inducible factor-1 stabilization (100 to 300 nM) at somewhat higher concentrations, antipathogenic and tumoricidal responses from 300 to 800 nM, and nitrosative stress at concentrations >1 μM [2]. In general, lower concentrations promote cell survival and proliferation, and higher concentrations favor cell cycle arrest, apoptosis, and senescence. Interactions of NO with other reactive species can modulate its concentrations and thus change its cellular profile [2].
Another important factor contributing to the diversity of NO action is localization within the cell. For example, eNOS binding to the cell membrane anchoring protein caveolin decreases enzyme activity, whereas binding to heat shock protein 90 increases its activity [5]. In addition, different NOS enzymes localize to different portions of the cell, allowing for local action and regulation. In the heart, for example, nNOS is present in presynaptic nerves and the cardiomyocyte sarcoplasmic reticulum, eNOS is localized in caveolae of endothelial cells and in myocytes at the T-tube sarcoplasmic reticulum, and iNOS is induced in the myocyte cytoplasm [6]. NO localization allows for potential modulation of intracellular calcium concentrations through interaction with ryanodine receptors, which are also localized to T-tubules [6].
Another isoform, a mitochondrial variant of NOS, was described recently. Whether this is a distinct NOS isoform coded by mitochondrial DNA or whether it represents nNOS translocated to mitochondria with specific post-translational modifications is unclear [7]. This mitochondrial variant of NOS is bound to the mitochondrial PDZ domains of cytochrome oxidase and to complex I [5], and this localization allows the released NO to modulate mitochondrial respiration [7]. The source of mitochondrial NO also remains somewhat controversial; diffusion of cytosolic NO into the mitochondria may also contribute to mitochondrial NO concentrations. In any event, mitochondrial NO is an important regulator of mitochondrial respiration. In hypoxic conditions, mitochondrial NO could be maintained either by stimulation of NOS or from the reduction of nitrite by cytochrome oxidase [7]. In other pathologic conditions, such as sepsis, diffusion of NO produced by cytosolic iNOS may result in an increased mitochondrial NO concentration [7].
As nNOS has been increasingly studied, its importance in regulation of the circulatory system – not only by modulating neurotransmission, but also acting on its own – has become more apparent [8]. nNOS is present not only in sympathetic and parasympathetic nerve terminals, but also in cardiac myocytes, where it localizes to the sarcoplasmic reticulum and modulates calcium influx [6]. nNOS was recently shown to decrease endotoxin-induced TNF synthesis in cultured cardiac myocytes by inhibiting L-type calcium channel-dependent ERK signaling, suggesting nNOS might modulate inflammatory signaling [9]. On the other hand, nNOS appeared to play a role in mediating impaired microcirculatory responses in sepsis. In a rat cecal ligation and puncture (CLP) model, both inhibition and deletion of nNOS restored eNOS signaling and vasodilatory responses and increased downstream capillary red blood cell velocity [10]. Studies of the role of nNOS isoforms in the pathophysiology of disease are likely to proliferate as the importance of its role, both by producing NO and also by modulating other NOS isoforms, gains recognition.
Uncoupling of endothelial nitric oxide synthase
Although eNOS exists as a homodimer that produces NO from L-arginine, under certain conditions it can become uncoupled – to become a monomer that produces not NO, but the oxidative free radical superoxide (O2-) [11]. The most prominent of these conditions is a lack of availability of tetrahydrobiopterin (BH4), which usually results from its oxidation to dihydrobiopterin under conditions of oxidative stress. The resultant oxidative stress from O2-production can further promote NOS uncoupling, a forward feedback loop that can magnify the amount of oxidative stress within the cell. Other conditions that can uncouple eNOS include relative deficiency of its substrate, arginine and the presence of an endogenous competitive NOS inhibitor, asymmetric dimethyl-L-arginine (ADMA) [11].
The pathophysiology of eNOS uncoupling suggests several possible approaches to restore eNOS functionality in clinical situations, including administration of BH4, of folic acid to increase intracellular BH4 levels, or of exogenous arginine. In sepsis, there was concern that arginine treatment would provide a substrate for increased NO production from iNOS, but in fact arginine has been given to patients with sepsis without worsening hemodynamics, and arginine has been proposed as a component of immunomodulatory nutritional formulations [12]. More clinical trials are needed to evaluate the potential of these therapies.
Nitrosothiols
S-nitrosylation refers to the reaction of NO with sulfhydryl groups on critical protein cysteine residues, often the site of disulfide bonds. S-nitrosothiol species have been implicated in controlling oxygen delivery to tissues, and modulating both the function and activity of transcription factors, enzymes, and ion channels. S-nitrosylation may also be a mechanism for localizing NO activity within the cell. Recent evidence in cardiac myocytes suggests that S-nitrosylated proteins located in the vicinity of phosphatases regulate calcium sensitivity and reuptake, modulating both systolic and diastolic function [13]. Interestingly, NOS itself can be nitrated and nitrosylated; in the case of the nNOS isoform, this decreases enzyme activity [14].
Intravascular proteins such as albumin and also cysteine 93 on the β subunit of hemoglobin can be S-nitrosylated, and this may serve to buffer excess NO, ameliorating potential toxic effects of overabundant NO release. S-nitrosylation may also allow NO to exert distant effects, and also to transport NO bioactivity in response to vasoregulatory signals in areas that may require increased blood flow. In fact, S-nitrosylated human serum albumin has recently been tested as a means of NO supplementation, and has been shown to reduce lung injury and to prolong survival in a rat model of endotoxin infusion [15].
Nitrite
Nitrite has recently been shown to be a reservoir of NO in the circulation, and may in fact be the most important such reservoir. Nitrite is uniquely poised to behave as a carrier of NO bioactivity in the systemic circulation due to its relative stability and its ability to be reduced to NO. Nitrite converts to NO under acidemic and ischemic conditions, ensuring NO production in situations in which oxygen-dependent NOS enzyme activities may be compromised and in areas in which increased blood flow would be desirable [16]. Nitrite reduction to NO can therefore be an important regulator of regional blood flow.
A recent set of careful studies in normal volunteers has broadened our knowledge about the kinetics, potency, and mechanisms of action of nitrite; its vasodilatory effects do not appear to be susceptible to tolerance, which sets this anion apart from the organic nitrates [17]. Accumulating evidence has suggested that nitrite infusion may represent a therapeutic alternative for diseases associated with regional hypoxia and vasoconstriction, including sickle cell disease, pulmonary hypertension, and stroke, and clinical trials are currently underway.
Nitric oxide synthase inhibition
NO overproduction has been implicated in the pathogenesis of a number of diseases, and so therapeutic strategies aimed at blocking NOS have been tested both in preclinical models and in clinical trials. Interpretation of these studies, particularly those in animal models, has been complicated by a number of factors, several of which merit discussion. The first factor is isoform specificity. Many pharmacologic NOS inhibitors are arginine analogs, and these may inhibit more than one NOS isoform. Structurally distinct NOS isoform inhibitors can overcome this limitation, but may have effects unrelated to NO synthesis. More broadly, although the different localization and kinetics of different isoforms confer a degree of specificity of function, there is always some degree of overlap. In the setting of experiments with knockout animals, one isoform may potentially take over the functions of another – a difficulty that may be mitigated, but not eliminated, by use of tissue specific promoters, conditional knockouts, or multiple knockouts. This complicates not only interpretation of experiments, but also of disease pathophysiology.
A second factor is the reactivity of NO with other radicals, particularly reactive oxygen intermediates. Many of these reactions are concentration-dependent, which means that they can and do differ in different parts of the cell [5]. For example, when local NO levels exceed O2- concentrations, NO tends to reduce oxidative stress. When O2- levels exceed NO concentrations, O2- reduces the amount of bioavailable NO. When local NO and O2- levels are roughly equimolar, however, the highly reactive and toxic radical peroxynitrite is formed, with kinetics substantially faster than dismutation of O2- by superoxide dismutase (see Figure 2) [18]. Peroxynitrite can rapidly oxidize the active NOS cofactor BH4 to inactive dihydrobiopterin, uncoupling eNOS. The formation of peroxynitrite when concentrations of NO and O2- are similar may be the explanation for some settings, prominently those in which reperfusion injury plays a role, in which both NO inhibition and NO donors appear to have beneficial effects [18], as altering NO concentration in either direction would be expected to reduce peroxynitrite levels.
Figure 2.
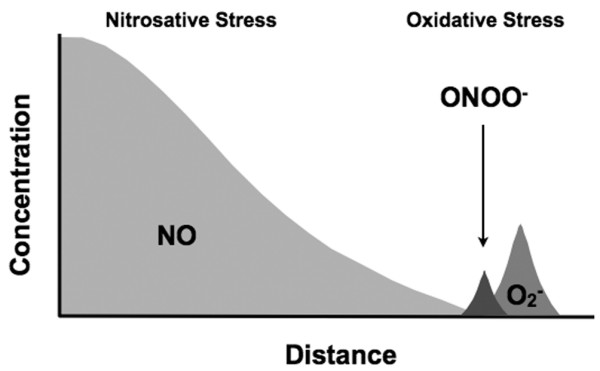
Reaction of nitric oxide with oxidative radicals is dependent on concentration and distance. When local nitric oxide (NO) levels exceed concentrations of reactant oxidant species, NO tends to reduce oxidative stress. When oxidant species exceed NO concentrations, they reduce the amount of bioavailable NO. When local NO and superoxide (O2-) levels are roughly equimolar, however, the highly reactive and toxic radical peroxynitrite (ONOO-) is formed.
A third, and to some extent related, factor is that NO action is often bimodal, depending on the concentration. In cardiac myocytes, for example, NO can have either positive or negative inotropic effects, depending on the concentration (see Figure 3) [19]. NO at low concentrations stimulates protein kinase A, increasing contractility by opening sarcolemmal calcium channels and stimulating ryanodine receptors. At high concentrations, however, actions of NO and cyclic GMP decrease contractility by hyperpolarizing the plasma membrane, decreasing calcium influx, and also by decreasing the sensitivity of troponin T to calcium [19].
Figure 3.
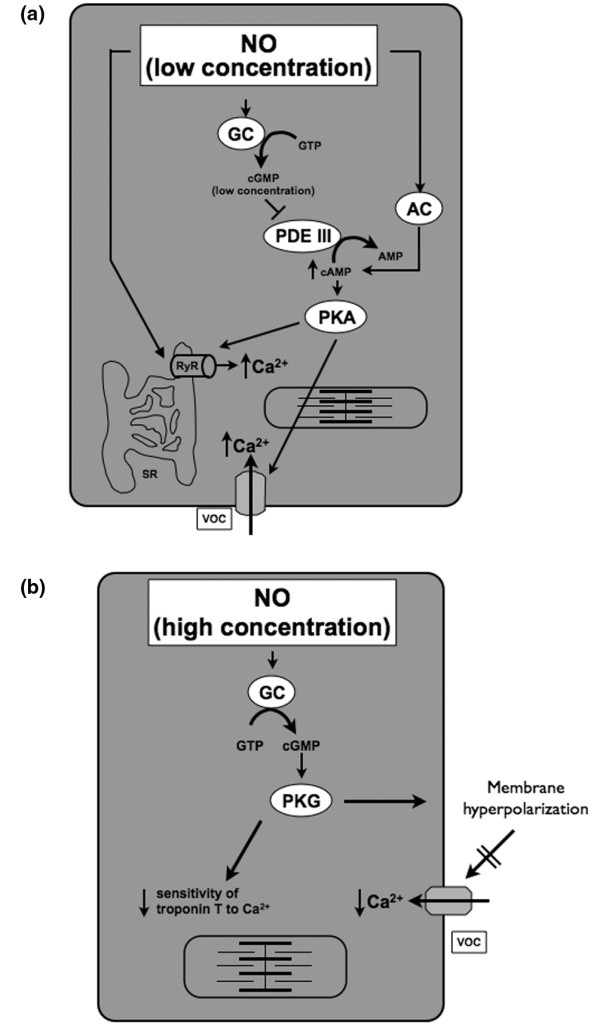
Bimodal actions of nitric oxide in cardiac myocytes. (a) At low concentrations, nitric oxide (NO) stimulates adenylate cyclase (AC) and acts through guanylate cyclase (GC) to inhibit phosphodiesterase (PDE), both of which increase cAMP levels, thus stimulating cAMP-dependent protein kinase A (PKA). PKA increases contractility by opening voltage-operated calcium channels (VOCs) on the plasma membrane and by stimulating ryanodine receptors (RyRs) on the sarcoplasmic reticulum (SR). (b) At high concentrations, however, NO produces much larger amounts of cyclic GMP (cGMP), which stimulates the cGMP-dependent protein kinase G (PKG). PKG decreases contractility by hyperpolarizing the plasma membrane, decreasing calcium influx through voltage-sensitive channels, and also by decreasing sensitivity of troponin T to calcium [19]. Reprinted from Life Sciences, 81(10), R. Rastaldo, P. Pagliaro, S. Cappello, C. Penna, D. Mancardi, N. Westerhof and G. Losano, Nitric oxide and cardiac function, 15 Pages, Copyright (2007), with permission from Elsevier.
Given this complexity, it becomes less surprising that NOS inhibition can have different effects in different settings, and that sometimes both NOS inhibition and NO donors can have similar effects in the same setting. Despite this complexity, NO inhibition can provide useful insights into disease pathophysiology, and may have therapeutic potential in some settings as well.
Sepsis
NO overproduction due to activation by cytokine-inducible NOS has been implicated in the pathophysiology of microcirculatory failure and organ dysfunction in sepsis, and NOS inhibition was shown to prevent vasodilation and hypotension in several experimental models [20-22]. The nonspecific NOS inhibitor NG-methyl-L-arginine (L-NMMA), however, did not improve mortality in a multicenter, randomized, double-blind, placebo-controlled trial of patients with septic shock, although hypotension was improved [23]. Precisely why this clinical trial failed is not entirely certain, but concerns have been expressed about the dosage, patient selection, titration to maintain blood pressure, as well as the nonspecific nature of the NOS inhibitor used. Despite the lack of benefit of NOS inhibition in this large clinical trial, studies of NO in sepsis continue to yield important pathophysiologic insights – and a role for manipulation of NO in the treatment of sepsis has not yet been ruled out definitively.
One recent study suggested that nNOS plays a more important role in sepsis than previously recognized. Mice deficient in nNOS had impaired bacterial clearance and decreased survival in a CLP model of sepsis; the results were similar when wild-type mice were treated with a selective nNOS inhibitor, suggesting that nNOS may have a protective role in sepsis [24].
The role of the other constitutive NOS isoform in sepsis is also being elucidated. Nonselective NOS inhibition is known to increase both leukocyte rolling and adhesion in a rat CLP model of sepsis [25], suggesting that eNOS may also have a protective role. In a recent study, mice with cardiomyocyte-specific overexpression of eNOS were protected from myocardial dysfunction associated with endotoxin infusion and also with polymicrobial bacterial challenge, an effect that appeared to be mediated by preserved myofilament sensitivity to calcium [26]. In an interesting clinical study, an eNOS polymorphism that is associated with decreased basal NO production and hypertension was associated with lower blood pressures in patients with Escherichia coli bacteremia, although this effect was not seen with Gram-positive bacteremia, and the eNOS polymorphism did not correlate with outcome in this relatively small study (147 patients) [27]. Genetic studies of this size are probably not robust enough to permit firm conclusions and the results require confirmation in other populations, but they do have the potential to generate provocative hypotheses.
Several recent studies have contributed to elucidating the role of iNOS in the pathophysiology of sepsis. In a rat model of CLP-induced sepsis, selective pharmacologic iNOS inhibition increased capillary red cell velocity and increased local skeletal muscle tissue oxygen consumption, although NOS inhibition did not decrease the number of capillaries with stopped flow [28]. In a murine CLP model, iNOS knockout mice and wild-type mice treated with a selective iNOS inhibitor showed a decrease in microvascular leakage without a significant decrease in abnormal leukocyte rolling and adhesion [29]. This discordance between adhesion of leukocytes and microvascular leakage suggested that these are regulated independently, and that increased vascular permeability in sepsis is dependent on iNOS induction, but that leukocyte activation occurs with or without iNOS. Studies such as these suggest that attenuation of the protective effects of constitutive NOS isoforms may help explain the failure of this therapy when applied in patients with septic shock, and that selective iNOS inhibition might have potential salutary effects, but the impact of such an approach remains to be elucidated by appropriately designed clinical trials.
Since NOS inhibition in septic shock is potentially a double-edged sword, scavenging excess NO has been proposed as another potential approach to counteract the effects of NO production in sepsis. This approach has the theoretical advantage of being most effective in the areas of largest NO overproduction. A chemically modified human-derived hemoglobin conjugate pyridoxalated hemoglobin polyoxyethylene selectively scavenges excessive NO without interfering with NOS expression or activity. Its potential to increase systemic blood pressure and to reduce vasopressor and ventilation needs without adversely affecting cardiac output, organ function, and survival provided the impetus for a multicenter, randomized, placebo-controlled clinical trial in patients with distributive shock. Although the overall 28-day mortality was similar, a rapid increase in blood pressure and rapid withdrawal of vasopressors were observed in these patients, and survivors treated with pyridoxalated hemoglobin polyoxyethylene spent less time on mechanical ventilation [30]. This new approach to NO modulation may be useful in distributive shock states, but larger trials with hard outcomes will be needed.
Other studies have suggested that NOS inhibition might be used in combination with other approaches. In a porcine model of continuous infusion of Pseudomonas aeruginosa, selective NOS inhibition in conjunction with oxygen free radical scavenging improved sepsis-induced microcirculatory dysfunction, hepatosplanchnic dysfunction, metabolic dysfunction, and renal dysfunction [31]. The level of production of reactive oxygen intermediates by cultured endothelial cells when exposed to sera from patients with severe sepsis was recently shown to correlate with mortality [32]. Also, as noted above, oxidative stress contributes to uncoupling of eNOS, increasing formation of reactive oxygen intermediates [11]. Addressing both oxidative and nitrosative stress, by reducing formation of peroxynitrite and other toxic intermediates, might have therapeutic promise.
Cardiogenic shock
The classic hemodynamic profile for patients with cardiogenic shock consists of low cardiac output and high systemic vascular resistance, but wide variations in left ventricular ejection fraction and systemic vascular resistance in patients with cardiogenic shock suggest that pathophysiologic mechanisms of cardiogenic shock may vary among patients. About one-fifth of patients with cardiogenic shock complicating myocardial infarction in the SHOCK trial had clinical evidence of a systemic inflammatory response syndrome, marked by fever, leukocytosis and low systemic vascular resistance [33]. This observation has led to an expansion of the classic paradigm to include the possibility of the contribution of inflammatory responses to vasodilation and myocardial stunning, leading clinically to persistence of shock [34]. Activation of iNOS with production of NO and peroxynitrite was proposed as one potential mechanism [34], and so NOS inhibition was proposed as a therapeutic strategy for patients with persistent shock despite an open infarct artery.
After preliminary studies using the NOS inhibitor L-NMMA showed promising hemodynamic effects, with increased blood pressure and urine output [35], a phase III randomized trial to study L-NMMA in patients with cardiogenic shock – the Tilarginine Acetate Injection Randomized International Study in Unstable AMI Patients/Cardiogenic Shock (TRIUMPH) trial – was initiated. The results of this trial have recently been published [36]. Although L-NMMA increased blood pressure significantly at 2 hours, there was no effect on either the primary outcome, the 30-day mortality, or the secondary outcomes of shock resolution and duration and 6-month mortality [36]. Whether the failure of this clinical trial represents the failure of the strategy of NOS inhibition or whether factors such as dosing, timing, and NOS inhibitor selectivity were important is not yet entirely certain.
Acute lung injury
Acute lung injury is another area in which both oxidative stress and nitrosative stress play a role. As in other fields, different isoforms are involved and play different roles. In a sheep model of combined burn injury and Pseudomonas pneumonia in which selective iNOS inhibition had previously been shown to improve gas exchange, a new study showed that selective nNOS inhibition improved pulmonary gas exchange, lung compliance, and lung edema [37]. nNOS inhibition also decreased nitrotyrosine in lung tissue, a marker of peroxynitrite formation, and, interestingly, diminished levels of iNOS protein in the lung [37]. It was speculated that nNOS was a trigger for iNOS formation in this model, but direct evidence was not provided. Additional investigations in the same model examined early nNOS inhibition combined with delayed iNOS inhibition, and found a similar improvement in pulmonary gas exchange and injury score, along with decreased inflammation, although lung edema was not decreased in this study [38]. Support for the notion that peroxynitrite is a pivotal pathogenetic mediator in lung injury was provided when a metalloporphyrinic peroxynitrite decomposition catalyst was shown to prevent IL-2-induced vascular leakage in an ovine model [39].
Interestingly – despite the fact that pathophysiologic considerations, bolstered by clinical association studies, suggest that high levels of NO, either by themselves or in combination with reactive oxygen intermediates, mediate pulmonary damage in acute lung injury – when baseline levels of urinary NO metabolites were examined in 566 patients from the multicenter ARDSNET trial comparing low tidal volumes with high tidal volumes in acute lung injury, higher urine NO was associated with better clinical outcomes, including lower mortality and more organ-failure-free days [40]. There are a number of potential explanations for this surprising finding. Urine NO may not accurately reflect pulmonary NO levels, or higher baseline NO levels may have been a marker for less severe injury. An alternative explanation, however, is that NO has beneficial effects, either in the lung or in organs other than the lung. Potential mechanisms include NO scavenging of reactive oxygen species, microcirculatory vasodilation, and decreased platelet and leukocyte adhesion to the endothelium.
Nitric oxide and diabetes
Failure of NO signaling is an important component of the pathogenesis of endothelial dysfunction in patients with diabetes, leading to accelerated atherosclerosis and vascular events. Hyperglycemia can induce overproduction of O2-, can decrease NO production, and can damage endothelial cells, suggesting a mechanism by which glucose contributes to endothelial dysfunction in diabetes [41]. Insulin resistance also plays an important role [41]. Recent studies have shown that endothelial dysfunction in diabetes may also be related to production of ADMA, by competitive inhibition of arginine binding to NOS and by uncoupling of eNOS [42]. Studies have begun to explore the role of dimethylarginine dimethylaminohydrolase, an enzyme primarily responsible for ADMA degradation. Levels of dimethylarginine dimethylaminohydrolase are decreased in diabetes, particularly in the kidney [43]. Strategies to enhance dimethylarginine dimethylaminohydrolase activity may have therapeutic potential to modulate ADMA levels in this and other conditions.
Diabetes can also cause iNOS induction, with resultant nitrosative stress. A recent study in streptozotocin-induced diabetes in rats showed overexpression of iNOS in the diabetic liver and kidney, suggesting a potential role for iNOS in mediating organ dysfunction [44]. iNOS may also mediate insulin resistance in inflammatory processes, impairing insulin signaling and worsening hyperglycemia.
Nitric oxide and cellular energy metabolism
NO is known to modulate mitochondrial function, generally downregulating mitochondrial energy production by reversibly inhibiting cytochrome c oxidase, the terminal acceptor in the mitochondrial electron transport chain [45]. This can be advantageous in a phenomenon known as ischemic preconditioning, in which brief periods of ischemia are protective against subsequent episodes of sustained ischemia followed by reperfusion. A recent study showed that cardiomyocyte-specific NOS overexpression was protective against ischemia–reperfusion injury, thus bolstering the role of NO in preconditioning [46]. The mechanisms have not been completely characterized, but they appear to include NO-stimulated increases in protein kinase C, and perhaps opening of mitochondrial KATP channels. Very high levels of NO, such as those that can occur with inflammation after ischemia/reperfusion, however, can cause opening of the mitochondrial permeability transition pore, with uncoupling of oxidative phosphorylation, dissipation of membrane gradients, membrane swelling, and cell death. This is another example of a biphasic effect of NO, with beneficial effects at low doses and deleterious effects at high doses.
The initial phases of sepsis are characterized by impaired hemodynamics, but later organ failure can occur despite restoration of an adequate blood pressure and cardiac output. Oxygen delivery does not appear to be the limiting factor in multiple organ failure, suggesting a defect in cellular oxygen use, which in turn would point to mitochondrial dysfunction as a pathogenic mechanism in sepsis-induced organ failure [47]. This hypothesis is supported both by laboratory investigations showing progressive mitochondrial dysfunction with ATP depletion and respiratory chain complex I inhibition in animal models of sepsis [48] and by a study in patients with septic shock, in which skeletal muscle biopsies demonstrated similar ATP depletion and respiratory chain complex I inhibition [49]. In both settings, the degree of mitochondrial dysfunction correlated with the severity of illness and with eventual outcome [48,49].
NO contributes to mitochondrial dysfunction in sepsis, in part by nitrating regulatory proteins. Oxidative stress contributes as well, and in this dysfunction, as in other areas, an additive effect can occur in which NO-induced mitochondrial injury causes inefficient mitochondrial respiration, with increased production of oxidant species. In this context, a recent study demonstrated that ADMA-induced uncoupling of eNOS led to increased peroxynitrite formation and mitochondrial dysfunction in pulmonary endothelial cells [42].
On the contrary, it has been speculated that NO may play an adaptive role in some situations, modulating oxidative phosphorylation at a time when mitochondrial efficiency is compromised [50]. While this may potentially protect the cell by simultaneously decreasing mitochondrial oxygen utilization and promoting repair processes, it could also contribute to bioenergetic failure. The balance between beneficial and pathogenic effects may differ in different organs and at different times in the course of sepsis.
Nitric oxide donors and the microcirculation
As we have seen, explorations of the complex role of NO in health and disease have continued to highlight bimodal actions of NO, generally with protective actions at low levels and deleterious actions at higher levels. The potential for NO to interact with other reactive species is also concentration-dependent – and, perhaps most importantly, localization of NO is a crucial determinant of its effects, both within cells and in tissues and organs. This is perhaps most strikingly observed in the microvasculature, where regional heterogeneity in flow may lead to pathologic events even if the global hemodynamic parameters remain normal. In sepsis, for example, microvascular heterogeneity documented by orthogonal polarization spectral imaging was recently shown to be abnormal in septic patients, and the abnormalities were more pronounced in nonsurvivors than in survivors [51].
The potential for NO to have beneficial effects has provided the rationale for trials of administration of NO donors in various diseases. Interest has been especially keen in sepsis, in which the microcirculatory pathology plays a crucial role and where local administration of vasodilators might be expected to augment microcirculatory flow. Two recent experimental studies demonstrate how NO donors have the potential to improve splanchnic microcirculation in sepsis. In a resuscitated porcine model of Pseudomonas administration, the NO donor sodium nitroprusside increased the ileal mucosal and hepatic microcirculatory blood flows [52]. Another NO donor, SIN-1, was tested in a porcine model of endotoxemia, with use of tonometry to measure splanchnic pCO2 along with porphyrin phosphorescence to assess microvascular oxygen pressures, which allowed for exploration of mechanisms of NO action [53]. The NO donor normalized mucosal oxygen tension, but improved serosal oxygen tension only when given along with fluids-suggesting that NO along with appropriate resuscitation can redistribute, and thereby improve, splanchnic microvascular perfusion [53].
In two clinical studies of sepsis patients utilizing orthogonal polarization spectral imaging, the sepsis-induced impairment of sublingual microcirculatory blood flow was reversed with topical administration of acetylcholine – suggesting that the endothelium was still NO responsive [54] – and with intravenous nitroglycerin [55]. Precisely how to deliver NO donors in the clinical setting remains an issue, as they have the potential to exacerbate hypotension in shock states. A study in a mouse model of cardiac ischemia and reperfusion showed that NO inhalation was protective, and produced an increase in the concentration of NO metabolites in the lung, the liver, the heart, and the brain [56], suggesting that inhaled NO can have a systemic effect, perhaps via nitrosothiols, nitrosamine, or increased generation of nitrite.
Novel agents to rescue the microcirculation may prove to be a cutting-edge strategy to optimize tissue perfusion in shock. NO is vital to microcirculatory homeostasis, and appears to protect microcirculatory patency when it sustains an insult. The hypothesis that inhaled NO administration will improve microcirculatory perfusion without significant impairment of systemic hemodynamics is supportable on the basis of current data, but will need to be tested in clinical trials. Our bias is that indices of microcirculatory perfusion may yield physiologic information that macrocirculatory indices cannot, and help to guide such therapy. Accordingly, we are initiating a randomized clinical trial to test the efficacy of inhaled NO in improving microcirculatory perfusion and organ failure in septic patients with persistent microcirculatory dysfunction (as assessed by sidestream darkfield imaging of the sublingual circulation) after early goal-directed resuscitation has been successfully accomplished [3]. Since it is possible that NO will improve microcirculatory perfusion without impacting organ failure, or will improve organ failure without an increase in perfusion, this trial may allow for inferences about the relative roles of microcirculatory perfusion and other potential mechanisms, such as inflammation and mitochondrial function, in the development of organ failure in sepsis. Regardless of the outcome of this trial, we look forward to further studies to translate mechanistic and therapeutic insights from animal studies into the clinical area.
Abbreviations
ADMA: asymmetric dimethyl-L-arginine; BH4: tetrahydrobiopterin; CLP: cecal ligation and puncture; eNOS: endothelial nitric oxide synthase (NOS3); IFN: interferon; IL: interleukin; iNOS: inducible nitric oxide synthase (NOS2); L-NMMA: NG-methyl-L-arginine; NF: nuclear factor; nNOS: neuronal nitric oxide synthase (NOS1); NO: nitric oxide; NOS: nitric oxide synthase; O2-: superoxide; TNF: tumor necrosis factor.
Competing interests
The authors declare that they have no competing interests.
Contributor Information
Steven M Hollenberg, Email: hollenberg-steven@cooperhealth.edu.
Ismail Cinel, Email: cinelismail@yahoo.com.
References
- Zimmet JM, Hare JM. Nitroso-redox interactions in the cardiovascular system. Circulation. 2006;114:1531–1544. doi: 10.1161/CIRCULATIONAHA.105.605519. [DOI] [PubMed] [Google Scholar]
- Thomas DD, Ridnour LA, Isenberg JS, Flores-Santana W, Switzer CH, Donzelli S, Hussain P, Vecoli C, Paolocci N, Ambs S, Colton CA, Harris CC, Roberts DD, Wink DA. The chemical biology of nitric oxide: implications in cellular signaling. Free Radic Biol Med. 2008;45:18–31. doi: 10.1016/j.freeradbiomed.2008.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trzeciak S, Cinel I, Phillip Dellinger R, Shapiro NI, Arnold RC, Parrillo JE, Hollenberg SM. Resuscitating the microcirculation in sepsis: the central role of nitric oxide, emerging concepts for novel therapies, and challenges for clinical trials. Acad Emerg Med. 2008;15:399–413. doi: 10.1111/j.1553-2712.2008.00109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alderton WK, Cooper CE, Knowles RG. Nitric oxide synthases: structure, function and inhibition. Biochem J. 2001;357(Pt 3):593–615. doi: 10.1042/0264-6021:3570593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kone BC, Kuncewicz T, Zhang W, Yu ZY. Protein interactions with nitric oxide synthases: controlling the right time, the right place, and the right amount of nitric oxide. Am J Physiol Renal Physiol. 2003;285:F178–F190. doi: 10.1152/ajprenal.00048.2003. [DOI] [PubMed] [Google Scholar]
- Schulz R, Rassaf T, Massion PB, Kelm M, Balligand JL. Recent advances in the understanding of the role of nitric oxide in cardiovascular homeostasis. Pharmacol Ther. 2005;108:225–256. doi: 10.1016/j.pharmthera.2005.04.005. [DOI] [PubMed] [Google Scholar]
- Carreras MC, Poderoso JJ. Mitochondrial nitric oxide in the signaling of cell integrated responses. Am J Physiol Cell Physiol. 2007;292:C1569–C1580. doi: 10.1152/ajpcell.00248.2006. [DOI] [PubMed] [Google Scholar]
- Seddon MD, Chowienczyk PJ, Brett SE, Casadei B, Shah AM. Neuronal nitric oxide synthase regulates basal microvascular tone in humans in vivo. Circulation. 2008;117:1991–1996. doi: 10.1161/CIRCULATIONAHA.107.744540. [DOI] [PubMed] [Google Scholar]
- Geoghegan-Morphet N, Burger D, Lu X, Sathish V, Peng T, Sims SM, Feng Q. Role of neuronal nitric oxide synthase in lipopolysaccharide-induced tumor necrosis factor-alpha expression in neonatal mouse cardiomyocytes. Cardiovasc Res. 2007;75:408–416. doi: 10.1016/j.cardiores.2007.03.020. [DOI] [PubMed] [Google Scholar]
- Lidington D, Li F, Tyml K. Deletion of neuronal NOS prevents impaired vasodilation in septic mouse skeletal muscle. Cardiovasc Res. 2007;74:151–158. doi: 10.1016/j.cardiores.2006.12.022. [DOI] [PubMed] [Google Scholar]
- Forstermann U, Munzel T. Endothelial nitric oxide synthase in vascular disease: from marvel to menace. Circulation. 2006;113:1708–1714. doi: 10.1161/CIRCULATIONAHA.105.602532. [DOI] [PubMed] [Google Scholar]
- Luiking YC, Deutz NE. Exogenous arginine in sepsis. Crit Care Med. 2007;35(9 Suppl):S557–S563. doi: 10.1097/01.CCM.0000279191.44730.A2. [DOI] [PubMed] [Google Scholar]
- Berkowitz DE. Myocyte nitroso-redox imbalance in sepsis: NO simple answer. Circ Res. 2007;100:1–4. doi: 10.1161/01.RES.0000255898.65901.9d. [DOI] [PubMed] [Google Scholar]
- Sun J, Druhan LJ, Zweier JL. Dose dependent effects of reactive oxygen and nitrogen species on the function of neuronal nitric oxide synthase. Arch Biochem Biophys. 2008;471:126–133. doi: 10.1016/j.abb.2008.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakubowski A, Maksimovich N, Olszanecki R, Gebska A, Gasser H, Podesser BK, Hallstrom S, Chlopicki S. S-nitroso human serum albumin given after LPS challenge reduces acute lung injury and prolongs survival in a rat model of endotoxemia. Naunyn Schmiedebergs Arch Pharmacol. 2008;379:281–290. doi: 10.1007/s00210-008-0351-2. [DOI] [PubMed] [Google Scholar]
- Lundberg JO, Weitzberg E, Gladwin MT. The nitrate–nitrite–nitric oxide pathway in physiology and therapeutics. Nat Rev Drug Discov. 2008;7:156–167. doi: 10.1038/nrd2466. [DOI] [PubMed] [Google Scholar]
- Dejam A, Hunter CJ, Tremonti C, Pluta RM, Hon YY, Grimes G, Partovi K, Pelletier MM, Oldfield EH, Cannon RO 3rd, Schechter AN, Gladwin MT. Nitrite infusion in humans and nonhuman primates: endocrine effects, pharmacokinetics, and tolerance formation. Circulation. 2007;116:1821–1831. doi: 10.1161/CIRCULATIONAHA.107.712133. [DOI] [PubMed] [Google Scholar]
- Pacher P, Beckman JS, Liaudet L. Nitric oxide and peroxynitrite in health and disease. Physiol Rev. 2007;87:315–424. doi: 10.1152/physrev.00029.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rastaldo R, Pagliaro P, Cappello S, Penna C, Mancardi D, Westerhof N, Losano G. Nitric oxide and cardiac function. Life Sci. 2007;81:779–793. doi: 10.1016/j.lfs.2007.07.019. [DOI] [PubMed] [Google Scholar]
- Broussard MD, Parrillo JE, Prancan AV, Hollenberg SM. Inducible nitric oxide synthase (iNOS) deficient septic mice show improved microvascular responsiveness to endothelin-1 [abstract] FASEB J. 2000;14:A404. [Google Scholar]
- Hollenberg SM, Broussard M, Osman J, Parrillo JE. Increased microvascular reactivity and improved mortality in septic mice lacking inducible nitric oxide synthase. Circ Res. 2000;86:774–778. doi: 10.1161/01.res.86.7.774. [DOI] [PubMed] [Google Scholar]
- Matejovic M, Krouzecky A, Martinkova V, Rokyta R Jr, Kralova H, Treska V, Radermacher P, Novak I. Selective inducible nitric oxide synthase inhibition during long-term hyperdynamic porcine bacteremia. Shock. 2004;21:458–465. doi: 10.1097/00024382-200405000-00010. [DOI] [PubMed] [Google Scholar]
- Lopez A, Lorente JA, Steingrub J, Bakker J, McLuckie A, Willatts S, Brockway M, Anzueto A, Holzapfel L, Breen D, Silberman MS, Takala J, Donalson J, Arneson C, Grove G, Grossman S, Grover R. Multiple-center, randomized, placebo-controlled, double-blind study of the nitric oxide synthase inhibitor 546C88: effect on survival in patients with septic shock. Crit Care Med. 2004;32:21–30. doi: 10.1097/01.CCM.0000105581.01815.C6. [DOI] [PubMed] [Google Scholar]
- Cui X, Besch V, Khaibullina A, Hergen A, Quezado M, Eichacker P, Quezado ZM. Neuronal nitric oxide synthase deficiency decreases survival in bacterial peritonitis and sepsis. Intensive Care Med. 2007;33:1993–2003. doi: 10.1007/s00134-007-0814-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundrani R, Easington CR, Mattoo A, Parrillo JE, Hollenberg SM. Nitric oxide synthase inhibition increases venular leukocyte rolling and adhesion in septic rats. Crit Care Med. 2000;28:2898–2903. doi: 10.1097/00003246-200008000-00035. [DOI] [PubMed] [Google Scholar]
- Ichinose F, Buys ES, Neilan TG, Furutani EM, Morgan JG, Jassal DS, Graveline AR, Searles RJ, Lim CC, Kaneki M, Picard MH, Scherrer-Crosbie M, Janssens S, Liao R, Bloch KD. Cardiomyocyte-specific overexpression of nitric oxide synthase 3 prevents myocardial dysfunction in murine models of septic shock. Circ Res. 2007;100:130–139. doi: 10.1161/01.RES.0000253888.09574.7a. [DOI] [PubMed] [Google Scholar]
- Huttunen R, Hurme M, Laine J, Eklund C, Vuento R, Aittoniemi J, Huhtala H, Syrjanen J. Endothelial nitric oxide synthase G894T (GLU298ASP) polymorphism is associated with hypotension in patients with E. coli bacteremia but not in bacteremia caused by a Gram-positive organism. Shock. 2008;31:448–453. doi: 10.1097/SHK.0b013e318188e58e. [DOI] [PubMed] [Google Scholar]
- Bateman RM, Sharpe MD, Goldman D, Lidington D, Ellis CG. Inhibiting nitric oxide overproduction during hypotensive sepsis increases local oxygen consumption in rat skeletal muscle. Crit Care Med. 2008;36:225–231. doi: 10.1097/01.CCM.0000295307.92027.2F. [DOI] [PubMed] [Google Scholar]
- Hollenberg SM, Guglielmi M, Parrillo JE. Discordance between microvascular permeability and leukocyte dynamics in septic iNOS-deficient mice. Crit Care. 2007;11:R125. doi: 10.1186/cc6190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinasewitz GT, Privalle CT, Imm A, Steingrub JS, Malcynski JT, Balk RA, DeAngelo J. Multicenter, randomized, placebo-controlled study of the nitric oxide scavenger pyridoxalated hemoglobin polyoxyethylene in distributive shock. Crit Care Med. 2008;36:1999–2007. doi: 10.1097/CCM.0b013e31817bfe84. [DOI] [PubMed] [Google Scholar]
- Matejovic M, Krouzecky A, Rokyta R Jr, Radej J, Kralova H, Treska V, Radermacher P, Novak I. Effects of combining inducible nitric oxide synthase inhibitor and radical scavenger during porcine bacteremia. Shock. 2007;27:61–68. doi: 10.1097/01.shk.0000235088.53421.6f. [DOI] [PubMed] [Google Scholar]
- Huet O, Obata R, Aubron C, Spraul-Davit A, Charpentier J, Laplace C, Nguyen-Khoa T, Conti M, Vicaut E, Mira JP, Duranteau J. Plasma-induced endothelial oxidative stress is related to the severity of septic shock. Crit Care Med. 2007;35:821–826. doi: 10.1097/01.CCM.0000257464.79067.AF. [DOI] [PubMed] [Google Scholar]
- Kohsaka S, Menon V, Lowe AM, Lange M, Dzavik V, Sleeper LA, Hochman JS. Systemic inflammatory response syndrome after acute myocardial infarction complicated by cardiogenic shock. Arch Intern Med. 2005;165:1643–1650. doi: 10.1001/archinte.165.14.1643. [DOI] [PubMed] [Google Scholar]
- Hochman JS. Cardiogenic shock complicating acute myocardial infarction: expanding the paradigm. Circulation. 2003;107:2998–3002. doi: 10.1161/01.CIR.0000075927.67673.F2. [DOI] [PubMed] [Google Scholar]
- Dzavik V, Cotter G, Reynolds HR, Alexander JH, Ramanathan K, Stebbins AL, Hathaway D, Farkouh ME, Ohman EM, Baran DA, Prondzinsky R, Panza JA, Cantor WJ, vered Z, Buller CE, Kleiman NS, Webb JG, Holmes DR, Parrillo JE, Hazen SL, Gross SS, Harrington RA, Hochman JS. Effect of nitric oxide synthase inhibition on haemodynamics and outcome of patients with persistent cardiogenic shock complicating acute myocardial infarction: a phase II dose-ranging study. Eur Heart J. 2007;28:1109–1116. doi: 10.1093/eurheartj/ehm075. [DOI] [PubMed] [Google Scholar]
- Alexander JH, Reynolds HR, Stebbins AL, Dzavik V, Harrington RA, Werf F Van de, Hochman JS. Effect of tilarginine acetate in patients with acute myocardial infarction and cardiogenic shock: the TRIUMPH randomized controlled trial. JAMA. 2007;297:1657–1666. doi: 10.1001/jama.297.15.joc70035. [DOI] [PubMed] [Google Scholar]
- Enkhbaatar P, Connelly R, Wang J, Nakano Y, Lange M, Hamahata A, Horvath E, Szabo C, Jaroch S, Holscher P, Hillmann M, Traber LD, Schmalstieg FC, Herndon DN, Traber DL. Inhibition of neuronal nitric oxide synthase in ovine model of acute lung injury. Crit Care Med. 2009;37:208–214. doi: 10.1097/CCM.0b013e318193226a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange M, Hamahata A, Enkhbaatar P, Esechie A, Connelly R, Nakano Y, Jonkam C, Cox RA, Traber LD, Herndon DN, Traber DL. Assessment of vascular permeability in an ovine model of acute lung injury and pneumonia-induced Pseudomonas aeruginosa sepsis. Crit Care Med. 2008;36:1284–1289. doi: 10.1097/CCM.0b013e318169ef74. [DOI] [PubMed] [Google Scholar]
- Maybauer DM, Maybauer MO, Szabo C, Westphal M, Traber LD, Enkhbaatar P, Murthy KG, Nakano Y, Salzman AL, Herndon DN, Traber DL. Lung-protective effects of the metalloporphyrinic peroxynitrite decomposition catalyst WW-85 in interleukin-2 induced toxicity. Biochem Biophys Res Commun. 2008;377:786–791. doi: 10.1016/j.bbrc.2008.10.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClintock DE, Ware LB, Eisner MD, Wickersham N, Thompson BT, Matthay MA. Higher urine nitric oxide is associated with improved outcomes in patients with acute lung injury. Am J Respir Crit Care Med. 2007;175:256–262. doi: 10.1164/rccm.200607-947OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bermudez V, Bermudez F, Acosta G, Acosta A, Anez J, Andara C, Leal E, Cano C, Manuel V, Hernandez R, Israili Z. Molecular mechanisms of endothelial dysfunction: from nitric oxide synthesis to ADMA inhibition. Am J Ther. 2008;15:326–333. doi: 10.1097/MJT.0b013e318160beda. [DOI] [PubMed] [Google Scholar]
- Sud N, Wells SM, Sharma S, Wiseman DA, Wilham J, Black SM. Asymmetric dimethylarginine inhibits HSP90 activity in pulmonary arterial endothelial cells: role of mitochondrial dysfunction. Am J Physiol Cell Physiol. 2008;294:C1407–C1418. doi: 10.1152/ajpcell.00384.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palm F, Onozato ML, Luo Z, Wilcox CS. Dimethylarginine dimethylaminohydrolase (DDAH): expression, regulation, and function in the cardiovascular and renal systems. Am J Physiol Heart Circ Physiol. 2007;293:H3227–H3245. doi: 10.1152/ajpheart.00998.2007. [DOI] [PubMed] [Google Scholar]
- Stadler K, Bonini MG, Dallas S, Jiang J, Radi R, Mason RP, Kadiiska MB. Involvement of inducible nitric oxide synthase in hydroxyl radical-mediated lipid peroxidation in streptozotocin-induced diabetes. Free Radic Biol Med. 2008;45:866–874. doi: 10.1016/j.freeradbiomed.2008.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erusalimsky JD, Moncada S. Nitric oxide and mitochondrial signaling: from physiology to pathophysiology. Arterioscler Thromb Vasc Biol. 2007;27:2524–2531. doi: 10.1161/ATVBAHA.107.151167. [DOI] [PubMed] [Google Scholar]
- West MB, Rokosh G, Obal D, Velayutham M, Xuan YT, Hill BG, Keith RJ, Schrader J, Guo Y, Conklin DJ, Prabhu SD, Zweier JL, Bolli R, Bhatnagar A. Cardiac myocyte-specific expression of inducible nitric oxide synthase protects against ischemia/reperfusion injury by preventing mitochondrial permeability transition. Circulation. 2008;118:1970–1978. doi: 10.1161/CIRCULATIONAHA.108.791533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraham E, Singer M. Mechanisms of sepsis-induced organ dysfunction. Crit Care Med. 2007;35:2408–2416. doi: 10.1097/01.CCM.0000282072.56245.91. [DOI] [PubMed] [Google Scholar]
- Brealey D, Karyampudi S, Jacques TS, Novelli M, Stidwill R, Taylor V, Smolenski RT, Singer M. Mitochondrial dysfunction in a long-term rodent model of sepsis and organ failure. Am J Physiol Regul Integr Comp Physiol. 2004;286:R491–R497. doi: 10.1152/ajpregu.00432.2003. [DOI] [PubMed] [Google Scholar]
- Brealey D, Brand M, Hargreaves I, Heales S, Land J, Smolenski R, Davies NA, Cooper CE, Singer M. Association between mitochondrial dysfunction and severity and outcome of septic shock. Lancet. 2002;360:219–223. doi: 10.1016/S0140-6736(02)09459-X. [DOI] [PubMed] [Google Scholar]
- Singer M. Mitochondrial function in sepsis: acute phase versus multiple organ failure. Crit Care Med. 2007;35(9 Suppl):S441–S448. doi: 10.1097/01.CCM.0000278049.48333.78. [DOI] [PubMed] [Google Scholar]
- Trzeciak S, Dellinger RP, Parrillo JE, Guglielmi M, Bajaj J, Abate NL, Arnold RC, Colilla S, Zanotti S, Hollenberg SM. Early micro-circulatory perfusion derangements in patients with severe sepsis and septic shock: relationship to hemodynamics, oxygen transport, and survival. Ann Emerg Med. 2007;49:88–98. doi: 10.1016/j.annemergmed.2006.08.021. 98e81–98e82. [DOI] [PubMed] [Google Scholar]
- Assadi A, Desebbe O, Kaminski C, Rimmele T, Benatir F, Goudable J, Chassard D, Allaouchiche B. Effects of sodium nitroprusside on splanchnic microcirculation in a resuscitated porcine model of septic shock. Br J Anaesth. 2008;100:55–65. doi: 10.1093/bja/aem278. [DOI] [PubMed] [Google Scholar]
- Siegemund M, Van Bommel J, Sinaasappel M, Schwarte LA, Studer W, Girard T, Vollebregt K, Ince C. The NO donor SIN-1 improves intestinal-arterial P(CO2) gap in experimental endotoxemia: an animal study. Acta Anaesthesiol Scand. 2007;51:693–700. doi: 10.1111/j.1399-6576.2007.01334.x. [DOI] [PubMed] [Google Scholar]
- De Backer D, Creteur J, Dubois MJ, Sakr Y, Vincent JL. Microvascular alterations in patients with acute severe heart failure and cardiogenic shock. Am Heart J. 2004;147:91–99. doi: 10.1016/j.ahj.2003.07.006. [DOI] [PubMed] [Google Scholar]
- Spronk PE, Ince C, Gardien MJ, Mathura KR, Oudemansvan Straaten HM, Zandstra DF. Nitroglycerin in septic shock after intravascular volume resuscitation. Lancet. 2002;360:1395–1396. doi: 10.1016/S0140-6736(02)11393-6. [DOI] [PubMed] [Google Scholar]
- Nagasaka Y, Fernandez BO, Garcia-Saura MF, Petersen B, Ichinose F, Bloch KD, Feelisch M, Zapol WM. Brief periods of nitric oxide inhalation protect against myocardial ischemia–reperfusion injury. Anesthesiology. 2008;109:675–682. doi: 10.1097/ALN.0b013e318186316e. [DOI] [PMC free article] [PubMed] [Google Scholar]


