Abstract
Objective
To evaluate whether a programme of multifactorial home visits reduces falls and impairments in mobility in elderly people living in the community.
Design
Randomised controlled trial with 18 months of follow up.
Setting
Six general practices in Hoensbroek, the Netherlands.
Participants
316 people aged 70 and over living in the community, with moderate impairments in mobility or a history of recent falls.
Intervention
Five home visits by a community nurse over a period of one year. Visits consisted of screening for medical, environmental, and behavioural factors causing falls and impairments in mobility, followed by specific advice, referrals, and other actions aimed at dealing with the observed hazards.
Main outcome measures
Falls and impairments in mobility.
Results
No differences were found in falls and mobility outcomes between the intervention and usual care groups.
Conclusion
Multifactorial home visits had no effects on falls and impairments in mobility in elderly people at risk who were living in the community. Because falls and impairments in mobility remain a serious problem among elderly people, alternative strategies should be developed and evaluated.
Introduction
Falls and impairments in mobility are a common problem among elderly people.1,2 In the past two decades the prevention of falls has received much attention. Gillespie et al systematically reviewed randomised controlled trials studying the effects of programmes on prevention of falls among elderly people.3 They concluded that programmes of multifactorial interventions (such as preventive home visits) seem to be effective when targeted to specific risk factors identified in individuals by screening. Although a recent systematic review showed no clear evidence for the effectiveness of preventive home visits in the general population of elderly people, programmes of home visits that target specific risk factors among particular people at risk seem to be more promising.3–5
Because falls and impairments in mobility are strongly interrelated problems that show many overlapping and interacting causes, we developed a programme of multifactorial home visits targeted at both preventing falls and reducing impairments in mobility in elderly people who are at risk of falls or have moderately impaired mobility.6–9 We aimed to determine if people receiving this programme of home visits had better outcomes than people receiving usual care.
Participants and methods
Design
We carried out a randomised controlled trial (with ethical approval) to assess the effectiveness of a programme of home visits. In calculating the required sample size, we chose as the main outcome measure the proportion of people sustaining any fall in the previous year. We considered our intervention clinically successful if it reduced the number of people having a fall among people aged 70 or over to that of people aged 55 to 70 years (respectively 34% and 18% yearly, among elderly Dutch people10). We calculated that a sample size of 115 per group would provide a power of 0.80 at 5% significance.11 With an expected drop out rate of about 25% during 18 months of follow up, this indicated that we would need to enrol about 150 participants per group.
Selection criteria and randomisation
We recruited participants from six general practices in Hoensbroek, the Netherlands, by means of a screening questionnaire. Participants had to be aged 70 years or over, be living in the community, and have reported two or more falls in the previous six months or have scored three or more on the mobility control scale of the short version of the sickness impact profile.12,13
We excluded people who were bedridden, fully dependent on a wheelchair, terminally ill, on the waiting list for admission to a nursing home, or receiving home care from a community nurse on a regular basis. Eligible patients were randomised to the home visit group or usual care group by computer generated random numbers directly after screening. People sharing a household were always allocated to the same group.
Intervention
Intervention group
Participants in the intervention group received five home visits from a community nurse over a period of one year. During the home visits they were screened for several medical, environmental, and behavioural factors potentially influencing falls and mobility. The screening was followed by advice, referrals, and other actions aimed at dealing with the hazards observed. The nurses followed a structured protocol for the home visits, which focused on falls, fear of falling, mobility, physical health, drugs, activities of daily living, social functioning, cognitive functioning, and psychosocial functioning. The protocol also included a checklist for home safety.14
Usual care
Participants in the usual care group did not receive any special attention or intervention on prevention of falls and impairments in mobility. The doctors and healthcare staff dealing with the participants were not told which patients were allocated to the usual care group.
Outcome measures
Primary outcome measures
The primary outcome measures were falls (the number of individuals sustaining any fall, more than one fall, any injurious fall, and any fall resulting in medical care) and impairments in mobility; as assessed by the mobility control scale and mobility range scale of the short version of the sickness impact profile.12,13
Secondary outcome measures
Secondary outcome measures were number of physical complaints (out of a total of 18), perceived health (first item RAND-36),15,16 perceived gait problems (five point Likert scale), daily activity (13 item Frenchay activities index),17,18 fear of falling (falls efficacy scale),19,20 mental health (mental health, RAND-36),15,16 social functioning (adjusted version of item 4 and 5 of the social activities battery),21 and loneliness (six point Likert scale).
The trial was conducted from September 1997 to June 1999. Participants were assessed by means of self administered questionnaires before the start of the intervention programme and after 12 and 18 months of follow up. During follow up participants recorded falls in a weekly diary.
Statistical analysis
We analysed data according to a preplanned protocol by using an intention to treat approach. Differences in baseline characteristics between the home visit and usual care groups were tested with the independent samples t test, Mann Whitney U test, or χ2 test. We analysed differences in outcomes after 12 and 18 months of follow up with logistic and multiple linear regression (hierarchical backward elimination method), adjusting for possible differences in baseline scores and background characteristics (sex, age, educational level, income, composition of household, and course of gait problems experienced).
Results
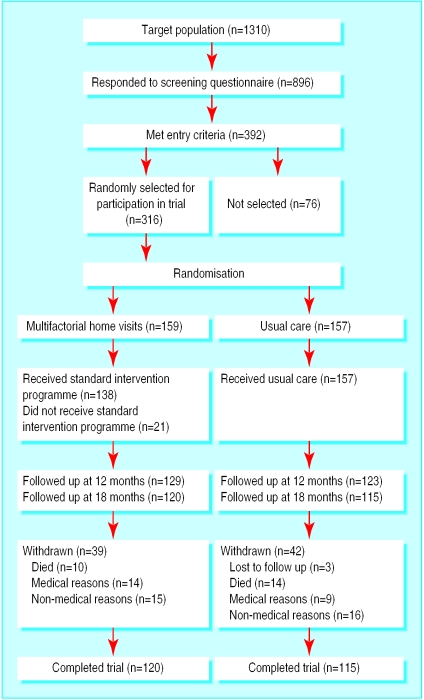
The figure shows the progress of the participants through the trial. Overall, 316 people met the inclusion criteria and were randomly allocated to either the home visit group (159 people) or usual care group (157). Twenty four people died during the 18 months of follow up, three were lost to follow up, and 23 withdrew from the study because of illness or admission to institutional care. Non-medical reasons for withdrawal were lack of motivation,18 illness or death of spouse,6 and moving to another area or long holiday.7 The reasons for drop-out were comparable in both groups.
The home visits were implemented according to plan, and no adjustments were made to the protocol. On average the home visits lasted 51 minutes. Overall, 138 (87%) of the 159 people in the intervention group received the complete intervention; owing to drop out in the first 12 months of the study, 12 people did not receive any home visits and nine received only part of the visits. The participants complied with 46% of the specific advice given by the nurses regarding referrals, home adjustments, drugs, exercise, and other preventive measures.
Outcomes
Table 1 shows the distribution of baseline characteristics of the two study groups. No significant differences were observed between the groups.
Table 1.
Baseline characteristics of patients receiving multifactorial home visits and usual care
| Home visits (n=159) | Usual care (n=157) | P value | |
|---|---|---|---|
| Background characteristics | |||
| Mean (SD) age | 77.2 (5.1) | 77.2 (5.0) | 0.926 |
| No (%) female | 104 (65) | 105 (67) | 0.782 |
| No (%) of elementary school education or less | 73 (46) | 88 (56) | 0.071 |
| No (%) below average income | 99 (62) | 104 (66) | 0.461 |
| No (%) living alone | 79 (50) | 79 (50) | 0.910 |
| No (%) with deteriorated course of gait disorders | 95 (60) | 93 (59) | 0.926 |
| Falls | |||
| No (%) with at least one fall | 60 (38) | 57 (36) | 0.792 |
| No (%) with more than one fall | 36 (23) | 25 (16) | 0.130 |
| Mobility impairment | |||
| Mean (SD) mobility control (0 (favourable) to 12) | 5.4 (2.5) | 5.7 (2.4) | 0.282 |
| Mean (SD) mobility range (0 (favourable) to 10) | 2.0 (2.4) | 2.4 (2.9) | 0.149* |
| Secondary outcomes | |||
| Mean (SD) physical complaints (0 (favourable) to 18) | 6.8 (3.3) | 7.0 (3.5) | 0.677 |
| Mean (SD) daily activity (13 to 52 (favourable)) | 33.0 (7.5) | 31.8 (7.6) | 0.159 |
| Mean (SD) fear of falling (10 (favourable) to 40) | 18.5 (7.7) | 17.5 (7.0) | 0.244 |
| Mean (SD) mental health (5 to 30 (favourable)) | 22.4 (5.1) | 21.5 (5.5) | 0.137 |
| Mean (SD) social functioning (2 (favourable) to 12) | 6.5 (1.9) | 6.4 (1.9) | 0.550 |
| Median perceived health (1 to 5 (favourable)) | 2 | 2 | 0.142 |
| Median perceived gait problems (1 (favourable) to 5) | 3 | 4 | 0.732 |
| Median loneliness (1 (favourable) to 6) | 2 | 2 | 0.403 |
This had moderate negative skewness, so independent samples t test was performed with transformed versions of this measure (square root).
After 12 and 18 months of follow up, data on 252 (80%) and 235 people (74%) were available for analysis respectively. Table 2 presents the fall outcomes according to group. The observed differences in fall outcomes between the home visit group and usual care group were not statistically significant. In addition no significant differences between the groups were found on mobility control, mobility range, physical complaints, mental health, and social functioning (table 3). After 12 months of follow up, people in the home visit group showed significantly less decline in daily activity than those in the usual care group. After 18 months this effect was no longer significant. In addition, significant effects of the intervention were observed on fear of falling after 12 and 18 months of follow up; people in the home visit group were less afraid of falling than those receiving usual care. No significant effects were detected on perceived health, perceived gait problems, and loneliness (table 4).
Table 2.
Effects on falls after 12 and 18 months of follow up according to treatment. Values are numbers (percentages) of patients unless stated otherwise
| Outcome measures | 12 month follow up
|
18 month follow up
|
|||||
|---|---|---|---|---|---|---|---|
| Home visits (n=129) | Usual care (n=123) | Odds ratio* (95% CI) | Home visits (n=120) | Usual care (n=115) | Odds ratio* (95% CI) | ||
| At least one fall† | 63 (50) | 53 (44) | 1.2 (0.7 to 2.0) | 68 (57) | 58 (52) | 1.3 (0.7 to 2.1) | |
| More than one fall† | 34 (27) | 29 (24) | 1.0 (0.5 to 1.8) | 43 (36) | 35 (31) | 1.0 (0.6 to 1.9) | |
| Injurious fall‡ | 26 (20) | 21 (17) | 1.2 (0.6 to 2.3) | 33 (28) | 25 (22) | 1.4 (0.8 to 2.6) | |
| Fall resulting in medical care‡ | 15 (12) | 11 (9) | 1.3 (0.6 to 3.1) | 21 (18) | 14 (12) | 1.6 (0.7 to 3.2) | |
As assessed by logistic regression analysis.
Patients who completed at least 75% of their diaries were included in analyses. Missing diaries were replaced by individual mean of valid diaries. Numbers of patients included at 12 months of follow up were 127 for home visits and 120 for usual care and at 18 months of follow up were 119 for home visits and 112 for usual care.
No baseline measurement available.
Table 3.
Effects on mobility and secondary outcome measures at 12 and 18 months of follow up according to treatment. Values are mean (SD) unless stated otherwise
| Outcome measures | 12 month follow up
|
18 month follow up
|
|||||
|---|---|---|---|---|---|---|---|
| Home visits (n=129) | Usual care (n=123) | Adjusted difference* (95% CI) | Home visits (n=120) | Usual care (n=115) | Adjusted difference* (95% CI) | ||
| Mobility impairments | |||||||
| Mobility control (0 (favourable) to 12) | 5.1 (2.8) | 5.3 (2.7) | −0.0 (−0.6 to 0.5) | 5.5 (2.8) | 5.5 (2.7) | 0.0 (−0.6 to 0.6) | |
| Mobility range† (0 (favourable) to 10) | 2.0 (2.5) | 2.6 (3.0) | −0.1 (−0.3 to 0.1) | 2.2 (2.4) | 2.3 (2.7) | 0.0 (−0.2 to 0.2) | |
| Secondary outcomes | |||||||
| Physical complaints (0 (favourable) to 18) | 6.1 (3.2) | 6.2 (3.6) | 0.2 (−0.4 to 0.8) | 6.2 (3.2) | 6.4 (3.4) | −0.2 (−0.9 to 0.4) | |
| Daily activity (13 to 52 (favourable)) | 33.5 (6.9) | 30.9 (8.0) | 1.6 (0.6 to 2.7) | 33.1 (7.3) | 31.5 (7.7) | 1.0 (−0.2 to 2.2) | |
| Fear of falling (10 (favourable) to 40) | 16.5 (6.1) | 17.9 (7.9) | −2.5 (−4.0 to −1.0) | 16.1 (5.7) | 17.6 (7.3) | −1.9 (−3.3 to −0.5) | |
| Mental health (5 to 30 (favourable)) | 22.0 (5.3) | 22.2 (5.3) | −0.7 (−1.7 to 0.3) | 22.0 (4.8) | 21.9 (5.4) | −0.1 (−1.0 to 0.8) | |
| Social functioning (2 (favourable) to 12) | 6.4 (2.0) | 6.5 (1.9) | −0.3 (−0.7 to 0.1) | 6.4 (1.9) | 6.3 (2.0) | 0.0 (−0.4 to 0.4) | |
As assessed by multiple linear regression analyses.
This had moderate negative skewness, so multiple regression analyses were performed on transformed versions of this measure (square root).
Table 4.
Effects on perceived health, perceived gait problems, and loneliness at 12 and 18 months of follow up according to treatment. Values are medians unless stated otherwise
| Outcome measures | 12 month follow up
|
18 month follow up
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Home visits (n=129) | Usual care (n=123) | P value* | Odds ratio† (95% CI) | Home visits (n=120) | Usual care (n=115) | P value* | Odds ratio† (95% CI) | ||
| Perceived health | 3 | 2 | 0.167 | 1.2 (0.6 to 2.2) | 2 | 2 | 0.315 | 1.3 (0.7 to 2.3) | |
| Perceived gait problems | 3 | 3 | 0.734 | 1.0 (0.5 to 1.8) | 4 | 4 | 0.579 | 0.8 (0.4 to 1.5) | |
| Loneliness | 1 | 2 | 0.139 | 0.9 (0.4 to 2.0) | 2 | 2 | 0.689 | 0.9 (0.4 to 2.1) | |
Mann-Whitney U test.
As assessed by logistic regression analyses on dichotomised versions of ordinal outcome measures—perceived health: 0=bad to moderate, and 1=good or better; perceived gait problems, 0=no to few problems, and 1=considerable problems or greater; loneliness, 0=never to sometimes, and 1=often or more.
Owing to the large number of secondary outcome measures, there is a considerable risk of type I error. When using Bonferroni correction (α=0.05/8=>α=0.006), the favourable effects for daily activity and fear of falling are still significant after 12 months of follow up, but the effect on fear of falling after 18 months no longer reaches significance.
Drop outs
The 81 people who dropped out of the study during the 18 months of follow up were on average older than those who completed the study (78.6 versus 76.7, P=0.011) and had a lower educational level (elementary school education or less: 49 (61%) versus 112 (48%), P=0.046). Also, the number of people having any fall or more than one fall was higher among those who dropped out (at least one fall: 39 (48%) versus 78 (33%), P=0.016); more than one fall: 25 (31%) versus 36 (15%), P=0.002), and they also had more impairments in range of mobility at baseline (3.5 versus 1.8, P=0.000). After both 12 and 18 months of follow up, however, those participants remaining in the home visit and usual care groups did not differ significantly for background characteristics and fall and mobility outcomes measured at baseline.
Discussion
Multifactorial home visits by community nurses did not reduce falls and impairments in mobility among a group of elderly people at risk. Furthermore, the home visits had no effects on physical complaints, perceived health, perceived gait problems, mental health, social functioning, and loneliness. The home visits did have favourable effects on fear of falling and daily activity after 12 months of follow up, but these effects diminished after 18 months of follow up.
There may be several explanations for the fact that we observed no effects of our intervention on falls and impairments of mobility. Firstly, because people in the home visit group showed less fear of falling and higher levels of daily activity than those in the usual care group at follow up, it is possible that the risk abatement was partly counterbalanced by an increase in risk behaviour in the home visit group, leading to a slightly increased number of people falling. Secondly, our intervention programme may not have added enough extra elements to the range of care and services already available for elderly people in the Netherlands.
Thirdly, a lack of adherence by the participants with the intervention programme might have influenced the outcomes of our study. The fact that 138 people completed the whole programme and a further nine completed part of the programme, however, does not indicate that lack of adherence was a large problem. Compliance with the advice given by the nurses also seemed reasonable.
What is already known on this topic
Programmes of multifactorial interventions targeted to the risk profile of the individual showed favourable effects on falls among elderly people living in the community in settings in the United States
Little evidence is yet available about the effects of this kind of intervention on falls and impairments in mobility among elderly people in European settings
What this study adds
A programme of multifactorial home visits aimed at reducing falls and impairments in mobility in elderly people at risk living in the community is not effective in the Dutch healthcare setting
This may also apply to comparable healthcare settings in other European countries
Fourthly, the drop out rate during follow up could have influenced the outcomes of our trial. It turned out that those people who were expected to benefit most from the intervention (people at higher risk for falls and with more impairments to mobility) dropped out of the study. We therefore performed subgroup analyses among a selection of people with the highest baseline scores for falls and range of mobility. The results were comparable to those of our main analyses, which makes it highly unlikely that selective drop out negatively influenced the internal validity of our trial.
The results of our study contrast with those of Gillespie et al's meta-analysis in which they concluded that multifactorial interventions for screening followed by targeted interventions resulted in a notable reduction in falls in elderly people.3 This conclusion was, however, primarily based on the results of four trials performed in the United States.5,22–24 It is likely that the observed differences in effectiveness between our intervention and those undertaken in the United States are related to differences in healthcare settings. Other explanations may be differences between components of the programmes. Owing to the multifactorial character and diversity of the interventions, however, it was not possible to isolate the effective components of the interventions undertaken in the United States.3
We conclude that a programme of multifactorial home visits aimed at reducing falls and impairments in mobility in elderly people at risk who live in the community is not effective in the Dutch healthcare setting. This may also apply to comparable healthcare settings in other European countries. Because falls and impairments in mobility remain a serious problem among elderly people, alternative strategies to prevent falls and reduce impairments in mobility need to be developed and tested in different healthcare settings.
Figure.
Progress of participants through trial
Education and debate p 1007
Footnotes
Funding: This study was supported by grants from Zorg Onderzoek Nederland and Stichting Onderzoek en Ontwikkeling Maatschappelijke Gezondheidszorg.
Competing interests: None declared.
References
- 1.Sattin RW. Falls among older persons: a public health perspective. Ann Rev Public Health. 1992;13:489–508. doi: 10.1146/annurev.pu.13.050192.002421. [DOI] [PubMed] [Google Scholar]
- 2.Lundgren-Lindquist B, Jette AM. Mobility disability among elderly men and women in Sweden. Int Disabil Stud. 1990;12:1–5. doi: 10.3109/03790799009166593. [DOI] [PubMed] [Google Scholar]
- 3.Gillespie LD, Gillespie WJ, Cumming R, Lamb SE, Rowe BH. Interventions to reduce the incidence of falling in the elderly. Cochrane Library. 1997;4:1–29. [Google Scholar]
- 4.Van Haastregt JCM, Diederiks JPM, van Rossum E, de Witte LP, Crebolder HFJM. Effects of preventive home visits to elderly people living in the community: systematic review. BMJ. 2000;320:754–758. doi: 10.1136/bmj.320.7237.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, Gottschalk M, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med. 1994;331:821–827. doi: 10.1056/NEJM199409293311301. [DOI] [PubMed] [Google Scholar]
- 6.O'Loughlin JL, Robitaille Y, Boivin J, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137:342–354. doi: 10.1093/oxfordjournals.aje.a116681. [DOI] [PubMed] [Google Scholar]
- 7.Stalenhoef PA, Crebolder HFJM, Knottnerus JA, van der Horst FGEM. Incidence, risk factors and consequences of falls among elderly subjects living in the community. Eur J Public Health. 1997;7:328–334. [Google Scholar]
- 8.Cunha UV. Differential diagnosis of gait disorders in the elderly. Geriatrics. 1988;43:33–42. [PubMed] [Google Scholar]
- 9.Wickham C, Cooper C, Margetts BM, Barker DJP. Muscle strength, activity, housing and the risk of falls in elderly people. Age Ageing. 1989;18:47–51. doi: 10.1093/ageing/18.1.47. [DOI] [PubMed] [Google Scholar]
- 10.Schiricke K, Vloet M. Mobiliteit bij ouderen. Thesis. Hoensbroek, Netherlands: Institute for Rehabilitation Research; 1993. [Google Scholar]
- 11.Pocock SJ. Clinical trials: a practical approach. Chichester: John Wiley; 1983. The size of a clinical trial; pp. 123–141. [Google Scholar]
- 12.De Bruin AF, Diederiks JPM, de Witte LP, Stevens JA, Philipsen H. The development of a short generic version of the sickness impact profile. J Clin Epidemiol. 1994;47:407–418. doi: 10.1016/0895-4356(94)90162-7. [DOI] [PubMed] [Google Scholar]
- 13.De Bruin AF, Buys M, de Witte LP, Diederiks JPM. The sickness impact profile: SIP68, a short generic version; first evaluation of the reliability and reproducibility. J Clin Epidemiol. 1994;47:863–871. doi: 10.1016/0895-4356(94)90189-9. [DOI] [PubMed] [Google Scholar]
- 14.Stalenhoef P, Diederiks J, Knottnerus A, de Witte L, Crebolder H. How predictive is a home-safety checklist of indoor fall risk for the elderly living in the community? Eur J Gen Pract. 1998;4:114–120. [Google Scholar]
- 15.Rand health science program. Santa Monica, CA: Rand; 1992. Rand 36-item health survey. [Google Scholar]
- 16.Van der Zee I, Sanderman R. Het meten van de algemene gezondheidstoestand met de RAND-36: een handleiding. Groningen: Noordelijk Centrum voor Gezondheidsvraagstukken; 1993. [Google Scholar]
- 17.Holbrook M, Skilbeck CE. An activities index for use with stroke patients. Age Ageing. 1983;12:166–170. doi: 10.1093/ageing/12.2.166. [DOI] [PubMed] [Google Scholar]
- 18.Schuling J, de Haan R, Limburg M, Groenier KH. The Frenchay activities index: assessment of functional status in stroke patients. Stroke. 1993;24:1173–1177. doi: 10.1161/01.str.24.8.1173. [DOI] [PubMed] [Google Scholar]
- 19.Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990;45:239–243. doi: 10.1093/geronj/45.6.p239. P. [DOI] [PubMed] [Google Scholar]
- 20.Buchner DM, Hornbrook MC, Kutner NG, Tinetti ME, Ory MG, Mulrow CD, et al. Development of the common data base for the FICSIT trials. J Am Geriatr Soc. 1993;41:297–308. doi: 10.1111/j.1532-5415.1993.tb06708.x. [DOI] [PubMed] [Google Scholar]
- 21.Donald CA, Ware JE, Brook RH, Davies-Avery A. Conceptualization and measurement of health for adults in the health insurance study. Santa Monica, CA: Rand; 1978. [Google Scholar]
- 22.Fabacher D, Josephson K, Pietruszka F, Linderborn K, Morley JE, Rubenstein LZ. An in-home preventive assessment programme for independent older adults. J Am Geriatr Soc. 1994;42:630–638. doi: 10.1111/j.1532-5415.1994.tb06862.x. [DOI] [PubMed] [Google Scholar]
- 23.Rubenstein LZ, Robbins AS, Josephson KR, Schulman BL, Osterweil D. The value of assessing falls in an elderly population. A randomized clinical trial. Ann Intern Med. 1990;113:308–316. doi: 10.7326/0003-4819-113-4-308. [DOI] [PubMed] [Google Scholar]
- 24.Wagner EH, LaCroix AZ, Grothaus L, Leveille SG, Hecht JA, Artz K, et al. Preventing disability and falls in older adults: a population-based randomized trial. Am J Public Health. 1994;84:1800–1806. doi: 10.2105/ajph.84.11.1800. [DOI] [PMC free article] [PubMed] [Google Scholar]