Abstract
Background
Multiple factors may contribute to hammer toe deformity at the metatarsophalangeal joint. The purposes of this study were to (1) compare the ratio of toe extensor/flexor muscle strength in toes 2-4 among groups with and without hammer toe deformity, (2) to determine correlations between the ratio of toe extensor/flexor muscle strength in toes 2-4, and metatarsophalangeal joint deformity (3) to determine if other clinical measures differ between groups and if these measures are correlated with metatarsophalangeal joint angle.
Methods
27 feet with visible hammer toe deformity and 31 age matched feet without hammer toe deformity were tested. Toe muscle strength was measured using a dynamometer and the ratio of toe extensor muscle strength to flexor muscle strength was calculated. Metatarsophalangeal joint angle was measured from a computerized tomography image. Ankle and subtalar joint range of motion, and tibial torsion were measured using goniometry.
Findings
Extensor/flexor toe muscle strength ratio was 2.3-3.0 times higher in the hammer toe group compared to the non-hammer toe group, in toes 2-4. The ratios of extensor/flexor toe muscle strength for toes 2-4 and metatarsophalangeal joint angle were highly correlated (r=0.69-0.80). Ankle dorsiflexion and metatarsophalangeal joint angle were negatively correlated for toes 2-4 (r= -0.38- -0.56) as were eversion and metatarsophalangeal joint angle.
Interpretation
These results provide insight into potential risk factors for the development of hammer toe deformity. Additional research is needed to determine the causal relationship between hammer toe deformity and the ratio of toe extensor/flexor muscle strength in toes 2-4.
Introduction
A hammer toe deformity is defined as dorsiflexion at the metatarsophalangeal joint (MTPJ), plantarflexion at the proximal interphalangeal joint and either normal position or dorsiflexion at the distal interphalangeal joint (Tollafild and Merriman, 1995). Hammer toe deformity is a common problem particularly in the second toe and can be a source of discomfort in the forefoot (Dhukaram et al., 2002). The incidence of hammer toe deformity increases with age. Hammer toe deformity may cause pain and callus over the proximal interphalangeal joint due to irritation from shoe wear, and may also cause metatarsalgia and callus formation under the metatarsal head. Hammer toe deformity is common in people with diabetes and peripheral neuropathy and is associated with increased forefoot plantar pressure and increased risk of ulceration (Lavery et al., 1998; Mueller et al., 2003).
Potential risk factors for hammer toe deformity are diverse and include (among others) muscular imbalance, ineffectiveness of the toe flexors (atrophy and weakness of intrinsic muscles of the foot), hallux valgus, trauma, inflammatory arthritis, contracted extensor digitorum longus (EDL), diabetes, foot type and biomechanical factors (Coughlin, 1984; Coughlin et al., 2000; Dhukaram et al., 2002; Parrish, 1973; Hansen 2000). Muscle imbalance between the toe extensors and intrinsic toe flexors has been considered a primary cause for some types of hammer toe deformity (Scheck, 1977; Schnepp, 1937; Hansen 2000). The strong extension forces of the EDL and extensor digitorum brevis (EDB) muscles at the MTPJ are balanced by the flexor digitorum longus, interosseus and lumbrical (intrinsic foot muscles) muscles (Bhatia et al., 1994). When the intrinsic muscles of the foot are weak, the prolonged unopposed action of the extensor muscles is believed to cause hammer toe deformity (Boulton, 1988). However, a recent study in people with diabetes and neuropathy did not confirm this belief (Bus et al., 2009). A prolonged extension position of the toes may cause shortening of the EDL muscle and lengthening of the foot intrinsic muscles. This problem could be compounded in the presence of limited dorsiflexion range of motion (ROM) at the ankle (Hansen 2000) or at the subtalar joint which may lead to increased activity of the EDL in an effort to increase ROM at the ankle.
Although muscle imbalance has been considered as a major etiology of hammer toe deformity, we are aware of no studies that have attempted to quantitatively measure the ratio of toe extensor/flexor muscle strength of individual toe muscles. A few studies have attempted to directly measure toe flexor muscle strength as a whole (Allen and Gross, 2003; Menz et al., 2006; Nihal et al., 2002; Senda et al., 1999). However, we are aware of no studies that have attempted to quantitatively measure individual toe flexor and toe extensor muscle strength in people with and people without hammer toe deformity. The purposes of this study were to (1) compare the ratio of toe extensor/flexor muscle strength in toes 2-4 among groups of subjects with and without hammer toe deformity (HT and NHT) and (2) to determine the correlations between the ratio of toe extensor/flexor muscle strength in toes 2-4, and MTPJ deformity (3) to determine if other clinical measures (ankle ROM, subtalar ROM, tibial torsion) differ between HT and NHT groups and if these measures are correlated with MTPJ angle.
Methods
Subjects
Twenty-nine subjects participated in this study (16 females and 13 males). Twenty-seven feet (10 female feet, 17 male feet) with flexible hammer toe deformity and a mean age (SD) of 32 (14) years were designated as the hammer toe group (HT). Thirty-one feet (22 female feet, 9 male feet) without hammer toe deformity and a mean age (SD) of 29 (8) years were designated as the non-hammer toe group (NHT). Subjects with noticeable metatarsal phalangeal joint hyperextension (beyond 30 degrees of extension) that was visible during standing and sitting were classified in the HT. Surprisingly, males were more likely to be in the hammer toe group than females (Table 1). This gender difference likely also contributed to a significant difference in weight, height, and foot length between the HT and the NHT groups (p<0.01), (Table 1). Individuals with a history of foot surgery, peripheral neuropathy, systemic disease, neurological disease, Morton’s neuroma, severe foot deformity, fixed hammer toe deformity, foot ulceration, claustrophobia, cognitive impairment or malignant tumor were excluded from this study. Participants were recruited from among the staff and students at Washington University, and outpatients from the Department of Orthopedic Surgery at Barnes-Jewish Hospital, Washington University Medical Center. All subjects provided informed consent as approved by the Washington University School of Medicine Human Research Protection Office.
Table 1.
Descriptive characteristics of the subjects
| Characteristic mean (SD) | Group |
|
|---|---|---|
| HT | NHT | |
| Age (years) | 32 (14) | 29 (8) |
| Gender | ||
| Female feet (%) | 10 ( 27%) | 22 ( 71% )* |
| Male feet (%) | 17 (63%) | 9 (29% )* |
| Weight (kg) | 78.3 (14.2) | 63.2 (13.4)* |
| Height (cm) | 173.2 (9.1) | 164.4 (9.6)* |
| Foot length(cm) | 258.3 (16.9) | 243.7(23.3)* |
| BMI | 26.4 (3.4) | 23.2 (3.1) |
HT, hammer toe deformity; NHT, non-hammer toe deformity
p<0.01
Muscle Strength Measures
Toe muscle strength was measured using a digital dynamometer (MSC-100, Chatillon) mounted vertically on a stable wooden board (Figure 1). A thin leather cuff (1.5 cm width) was connected to the hook attachment of the dynamometer. Toe flexor muscle strength was measured in a sitting position with the knee at 90 degrees of flexion and the ankle in a neutral position (0 degrees of dorsiflexion and plantarflexion). Multiple authors recommend placing the foot and ankle in a neutral position to test toe muscle strength to minimize the influence of the opposing long extrinsic toe muscles (Kendall et al., 1993; Hislop and Montgomery, 1995). The participant’s foot was stabilized by the examiner to prevent lifting of the heel and to prevent movement of the foot during the muscle strength tests. The height of the platform was controlled according to the participant’s foot height. The leather cuff was placed on the plantar side of the proximal phalanx of the toe to be measured. The participant was asked to push down as hard as possible with his/her toe for 5 seconds without lifting the heel. The participant practiced 3 times before any of the values were recorded. After the participant became familiar with the test, 3 trials were collected and the mean of the 3 trials was used for the ratio of toe extensor/flexor muscle strength. A one minute rest period was given between trials to minimize muscle fatigue.
Figure 1.
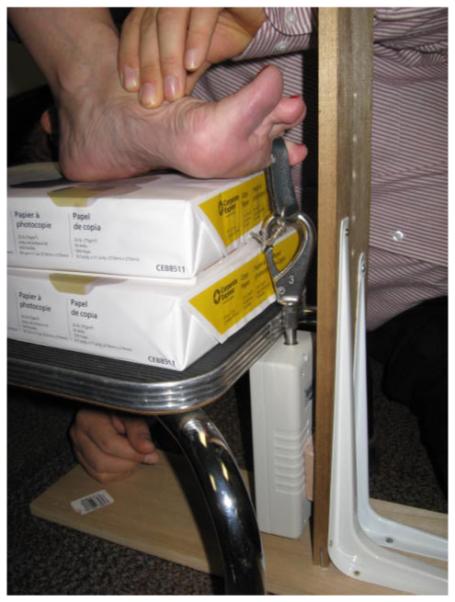
Toe extensor muscle strength testing of the 4th toe. The examiner stabilizes the foot to prevent the heel and the 4th metatarsal head from lifting during the test.
To measure toe extensor muscle strength, the digital dynamometer was inverted and remounted on the board. The leather cuff was placed on the dorsal side of the proximal phalanx of the toe to be measured. The participant was asked to pull up with his/her toe as hard as possible for 5 seconds without lifting the metatarsal head. The examiner stabilized the foot to prevent lifting of the forefoot and lifting of the metatarsal head (Figure 1). The participant was given 3 practice trials and then 3 trials were collected with a one minute rest between trials to prevent fatigue. The average of the 3 trials was used for the ratio of toe extensor/flexor muscle strength. In our study, intra-tester reliability for these measures on two separate occasions (2-5 days apart) on a subset of 32 feet was high (ICC values 0.88-0.96).
CT Measures
The MTPJ angle of toes 2-4 were measured from CT data using previously established methods (Commean et al., 2002). CT scanning was performed with the subject in a long sitting position with the ankle positioned in 30 degrees of plantarflexion with an ankle board to ensure the same testing position between subjects. MTPJ angle is affected by the passive tension of the toe extrinsic muscles which cross the ankle joint. If the ankle is in a dorsiflexed postion, the passive tension of the flexor digitorum longus will contribute to a decrease in the MTPJ angle. In a plantarflexed position of the ankle, the increased passive tension of the EDL muscle will increase the MTPJ angle. To minimize the effect of the passive tension of toe extrinsic muscles on MTPJ angle during the test, we chose to position the ankle in 30 degrees of plantarflexion, which is the approximate mid positon of physiological ankle range of motion from 10 degree dorsiflexion to 50 degrees plantarflexion. Although this ankle joint position is different than the position used to measure muscle strength, we thought each position was optimal to capture the respective strength or ROM measure. The participant’s hip was positioned in neutral (no internal or external rotation) and adhesive tape was used to stabilize the leg. Each subject was scanned from the knees to the toes. All images were reformed and analyzed using Analyze 7.0 software (Biomedical Imaging Resource, Mayo Clinic, Rochester MN). The MTPJ angle was measured from the maximum intensity projection of the lateral view image of each tested toe (Commean et al., 2002) (Figure.2). Intra-tester reliability for these measures on two separate occasions was high (ICC=0.98) (Commean et al., 2002).
Figure 2.
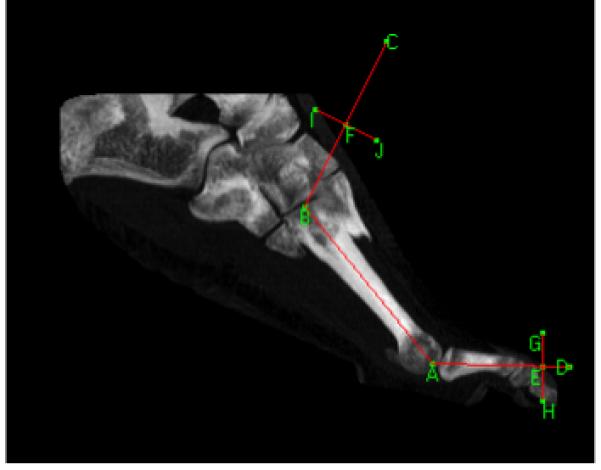
Lateral view maximum intensity projection through the third metatarsal. Angle BAD is measured to determine hammer toe deformity angle.
Goniometry Measures
Ankle dorsiflexion and plantarflexion ROM, calcaneal inversion and eversion ROM, and tibial torsion were measured using a plastic goniometer with a 2 degree interval scale. For measures of ankle dorsiflexion, ankle plantarflexion, calcaneal inversion, and calcaneal eversion, the participant was positioned in prone with the knee extended and the foot and ankle positioned off the end of the plinth. When measuring ankle dorsiflexion and plantarflexion ROM, the stationary arm was placed at the midline of the lateral side of the fibula and the axis was placed at the intersection of the lines through the lateral midline of the fibula and the lateral midline of the 5th metatarsal. The foot was moved passively by the examiner and the ROM was recorded. To measure inversion and eversion ROM of the calcaneous, the stationary arm was placed on the posterior midline of the leg and the axis was placed over the calcaneal tendon in line with the malleoli. The moving arm was placed at the posterior midline of the calcaneus. The examiner moved the calcaneus to create a starting position of 0 degrees of inversion and eversion and then the calcaneus was moved passively medially and laterally for inversion and eversion respectively and the ROM values were recorded. Intra-tester reliability for these measures on two separate occasions was high (ICC value 0.89-0.96) (Diamond et al., 1989).
To measure tibial torsion, the participant was positioned in prone with the knee flexed to 90 degrees and the ankle positioned in neutral. The examiner first found the middle of the medial malleolus in the anterior-posterior direction at the level of the ankle joint and marked a dot at the midpoint using a pen. Next, the most prominent aspect of the lateral malleolus was marked with a dot using a pen. The examiner then drew a line on the plantar surface of the heel that connected the dots on the medial and lateral malleoli to mark the transmalleolar axis (Milner and Soames, 1998; Staheli et al., 1985; Valmassy and Stanton, 1989). One arm of the goniometer was then aligned with the transmalleolar axis that had been drawn on the plantar surface of the heel and the other arm was aligned perpendicular to the long axis of the thigh and the angle between these two lines was recorded as the angle of tibial torsion (Stuberg et al., 1991). The participant was asked to stay relaxed to minimize lower leg rotation during the measurements. In our study, intra-tester reliability for these measures on two separate occasions (2-5 days apart) on a subset of 32 feet was acceptable (ICC=0.75). Piva et al(2006) reported that reliability of goniometeric measurement for tibial torsion with the subject in a prone position was moderate (ICC=0.70).
Statistical Analysis
Independent t-tests were used to determine any significant differences between HT and NHT groups. The correlation between the ratio of toe extensor/flexor muscle strength and MTPJ angle was tested using Pearson correlations. Multiple regression analysis was performed to determine the individual contributions to MTPJ angle from the ratio of toe extensor/flexor muscle strength, ankle dorsiflexion ROM, and subtalar joint eversion ROM. The significance level for all analyses was set at p=0.05.
Results
The extensor/flexor toe muscle strength ratio was 2.3-3.0 times higher in the HT group compared to the NHT group, in toes 2-4 (mean (SD): 2.4 (1.6) vs. 0.8 (0.2); 1.9 (0.7) vs. 0.8 (0.20); 1.6 (0.8) vs. 0.7 (0.2), all p<0.001). The HT group had less ankle dorsiflexion ROM (mean (SD): 4.7(5.4) vs. 10.3 (2.6) degrees, p<0.01) and less calcaneal eversion ROM (mean (SD): 7.1 (3.3) vs. 9.9 (2.7) degrees, p<0.01) compared to the NHT group. The ratio of extensor/flexor toe muscle strength for toes 2-4 and MTPJ angle were highly correlated (r=0.69, r=0.80, r=0.77, Table 3). Ankle dorsiflexion and MTPJ angle were negatively correlated for toes 2-4 (r= -0.46, -0.56, -0.38) as were calcaneal eversion and MTPJ angle (r=-0.60, r=-0.59, r=-0.45). See Table 2 for a description of the magnitude of each variable compared between groups and Table 3 for the correlations between the variables for each toe. The ratio of toe extensor/flexor muscle strength accounted for 48-64% of the variance in MTPJ angle in toes 2-4 (p<0.001). Eversion ROM added a unique additional 6-11% of the variance in MTPJ angle in toes 2-4 to explain a total of 59-73% of the total variance in MTPJ angle in toes 2-4 (p<0.001). Ankle dorsiflexion ROM did not account for a unique amount of the variance in MTPJ angle once ratio of extensor/flexor muscle strength had been added. See Table 4 for the complete results of the multiple regression analysis.
Table 3.
Correlation Matrix of key variables for toes 2-4
| Second Toe | MTPJ Angle | Extensor/Flexor Muscle Strength | Ankle Dorsiflexion ROM | Subtalar Eversion ROM |
|---|---|---|---|---|
| MTPJ Angle | 1.00 | |||
| Extensor/Flexor Muscle Strength | 0.69-0.80 | 1.00 | ||
| Ankle Dorsiflexion ROM | -0.38 - - 0.56 | -0.42 - -0.61 | 1.00 | |
| Subtalar Eversion ROM | -0.45 - -0.60 | -0.29 - -0.45 | 0.51 | 1.00 |
All correlation values significant, p<0.05
Table 2.
Comparison of variables between HT and NHT groups
| Variable | Group |
|
|---|---|---|
| HT Mean(SD) |
NHT Mean(SD) |
|
| Ratio of toe strength(extensor/flexor) | ||
| 2nd toe ** | 2.4 (1.6) | 0.8 (0.2) |
| 3rd toe ** | 1.9 (0.7) | 0.8 (0.2) |
| 4th toe ** | 1.6 (0.8) | 0.7 (0.2) |
| MTPJ angle (°)-CT data | ||
| 2nd toe * | 58.6 (11.9) | 40.2 (10.0) |
| 3rd toe * | 59.0 (13.2) | 39.4 (8.8) |
| 4th toe * | 48.3 (12.6) | 30.1 (9.3) |
| Ankle ROM (°) | ||
| Dorsiflexion * | 4.7 (5.4) | 10.3 (2.6) |
| Plantarflexion | 55.0 (8.4) | 57.4 (5.6) |
| Tibial torsion (°) | 33.4 (5.0) | 33.2 (3.8) |
| Subtalar joint motion (°) | ||
| Calcaneal inversion | 40.6 (6.5) | 38.7 (4.0) |
| Calcaneal eversion * | 7.1 (3.3) | 9.9 (2.7) |
HT=hammer toe; NHT=non hammer toe; ROM=range of motion; MTPJ=metatarsophalangeal joint
p<0.01
p<0.001
Table 4.
Multiple Regression Analysis
| Unique Contribution | Overall Model | |||||
|---|---|---|---|---|---|---|
| MTPJ Angle Location | Independent Variablesa | rb | sr2c | p | R2 | p |
| 2nd toe | Extensor/Flexor (2) | 0.69 | 0.48 | <0.001 | 0.48 | <0.001 |
| DF ROM | -0.46 | 0.00 | NS | 0.48 | NS | |
| EV ROM | -0.60 | 0.11 | <0.001 | 0.59 | <0.001 | |
| 3rd toe | Extensor/Flexor (3) | 0.80 | 0.64 | <0.001 | 0.64 | <0.001 |
| DF ROM | -0.56 | 0.01 | NS | 0.65 | NS | |
| EV ROM | -0.59 | 0.08 | <0.001 | 0.73 | <0.001 | |
| 4th toe | Extensor/Flexor (4) | 0.77 | 0.60 | <0.001 | 0.60 | <0.001 |
| DF ROM | -0.38 | 0.00 | NS | 0.60 | NS | |
| EV ROM | -0.45 | 0.06 | 0.004 | 0.66 | <0.001 | |
Independent variables listed in order of entry to multiple regression analysis.
simple correlation
sr2=square of the simpartial correlation indicating the unique variance accounted for by the individual independent variable
MTPJ angle=metatarsophalangeal joint angle
extensor/flexor=ratio of toe extensor/flexor muscle strength
DF ROM=ankle dorsiflexion range of motion
EV ROM=subtalar joint eversion range of motion
NS=not significant
Discussion
Although muscle imbalance between the extensors and flexors of the toes has been described as a risk factor for developing hammer toe deformity, this study is the first to quantify this difference and to find a relationship between the ratio of toe extensor/flexor muscle strength and MTPJ angle. In this study, the ratio of toe extensor/flexor muscle strength was 2.3-3 times higher in the HT group compared to the NHT group. In addition, the ratio of toe extensor/flexor muscle strength and MTPJ angle in toes 2-4 was highly correlated (r=0.69, r=0.80, r=.75 respectively, Figure 2). The EDL muscle dorsiflexes the ankle and extends the toes, while the EDB muscle extends the toes only. In the HT group, the toe extensor muscles were stronger than the toe flexor muscles, while in the NHT group the toe extensor muscles were weaker than the toe flexor muscles.
Other studies have attempted to measure toe flexor muscle strength using dynamometers (Senda et al., 1999), pressure sensors (Menz et al., 2006; Nihal et al., 2002), and force platforms (Endo et al., 2002). However, our study is the first to quantitatively measure toe flexor and toe extensor muscle strength and is the first to measure both toe flexor and toe extensor muscle strength of individual toes. In the present study, toe muscle strength was measured using a digital dynamometer with high reliability. It is possible that this device could be used clinically to measure toe muscle strength. Each extensor and flexor tendon of toes 2-4 originates from the common tendon of the EDL and flexor digitorum longus muscles. Since the tendons share a common tendon, one might argue that there is no need to measure each toe separately. However, we found differences between force productions at toes 2-4. In this study, mean values of each toe extensor muscle strength were 5.99 kg for the 2nd toe, 5.04 kg for the 3rd toe, and 4.46 kg for the 4th toe. Mean values of toe flexor muscle strength were 4.69 kg for the 2nd toe, 4.43 kg for the 3rd toe, and 4.37 kg for the 4th toe. For flexor and extensor muscle strength, the 4th toe was weaker than the 3rd and 2nd toes. The tendon of 4th toe runs more oblique from the common tendon compared to the tendon of the 2nd and 3rd toe and this orientation of tendon could be a possible reason why the 4th toe muscle strength was weaker than that of 2nd and 3rd toes.
This study identified that muscle imbalances and reduced ankle joint ROM were associated with hammer toe deformity. The mechanism of developing a muscle imbalance that might contribute to hammer toe deformity is unknown. Hansen (2000) and Sahrmann (2002) postulated that some people with hammer toe deformity dorsiflex the foot by contracting the EDL muscle more dominantly than the tibialis anterior muscle during functional activities. It is possible that this use of a primary toe extensor to control ankle movement may lead to increased use of the EDL which could then lead to a muscle imbalance and potentially a hammer toe deformity.
In addition, Hansen (2002, p 224) speculated that decreased dorsiflexion ROM due to a tight plantar flexor muscles could contribute to hammer toe deformity. In support of this speculation, we found that dorsiflexion ROM at the ankle joint was significantly less in the HT group compared to the NHT group (4.7 (5.4) vs. 10.3(2.6) degrees, p<0.01) and that dorsiflexion ROM was negatively correlated with MTPJ angle in toes 2-4 (r= -0.46, -0.56, -0.38). Hansen (2000) argues that tight plantar flexor muscles can contribute to over utilization of the EDL and suggests treatment with lengthening of the gastrocnemius muscle.
In our study, subtalar joint calcaneal eversion ROM was significantly lower in the HT group compared to the NHT group (7.1±3.3 vs. 9.9±2.7 degrees, p<0.01) and calcaneal eversion ROM was negatively correlated with MTPJ angle for toes 2-4 (r=-0.60, r=-0.59, r=-0.45). We did not expect to see this relationship and can only speculate at its cause. The EDL muscle is a strong pronator at the subtalar joint. When there is limited subtalar joint pronation (eversion), perhaps the EDL muscle has to work harder than if the subtalar joint has full range of motion and the EDL becomes shortened contributing to the hammer toe deformity.
We also measured ankle plantarflexion ROM, calcaneal inversion ROM, and tibial torsion in this study and we found no significant difference in these measures between the HT group and the NHT group.
We used the ratio of toe extensor/flexor muscle strength, ankle dorsiflexion ROM, and subtalar eversion ROM as factors in our multiple regression analysis based on their correlations with MTPJ angle. We found that the ratio of toe extensor/flexor muscle strength explained 48-64% of the MTPJ angle variance of toes 2-4 and that eversion ROM explained an additional 6-11% of the variance. Dorsiflexion ROM did not explain any unique variance once toe extensor/flexor muscle strength was included. Dorsiflexion ROM was highly correlated with the ratio of toe extensor/flexor muscle strength, so it is likely that dorsiflexion ROM did not uniquely contribute to the variance in MTPJ angle because of this correlation.
These results suggest that 1) muscle strength imbalance between flexors and extensors of toes 2-4, 2) decreased ankle dorsiflexion range of motion, and 3) decreased subtalar joint eversion range of motion may contribute to hammer toe deformity. Further study is needed to determine whether strengthening toe flexors and increasing ankle dorsiflexion and eversion range of motion could decrease or prevent hammer toe deformity angle in subjects with early hammer toe deformity.
While our study demonstrates correlations between muscle imbalances, joint limitations, and hammer toe deformity, there are limitations to consider. First, gender, weight, height, and foot length were not matched between the HT and NHT groups. Surprisingly, males were more likely to be in the hammer toe group than females. This gender difference likely also contributed to a significant difference in weight, height, and foot length between the HT and the NHT groups. However, there was no significant difference in the ratio of toe extensor/flexor muscle strength between the two genders, so differences in this variable between groups is not likely to be due to an unequal gender distribution between the groups. Second, when measuring the toe muscle strength, the leather cuff was placed over the proximal phalanx in an attempt to measure primarily foot intrinsic flexor muscle strength, but it is impossible to exclude the contributions of the long toe flexor muscles in our measure of toe flexor muscle strength. Additional research is needed to understand the specific roles that the intrinsic muscles play in development of HT deformity. Third, we are unable to determine the mechanism for the development of hammer toe deformity from the results of this study. It is unclear whether the muscle imbalance between the toe extensor and flexor muscles precedes hammer toe deformity or is a consequence of the deformity. Further study is needed to determine the causal relationship between hammer toe deformity and the ratio of toe extensor/flexor muscle strength in toes 2-4. Fourth, the participants in this study did not have neuromotor or metabolic disease (such as diabetes and peripheral neuropathy) that could have contributed to the development of hammer toe deformity. Future research should include people with diabetes and peripheral neuropathy and other neuromotor diseases to determine if these results are generalizable to these populations.
Conclusion
The ratio of extensor/flexor toe muscle strength in toes 2-4 was on average 2.5 times higher in the HT group compared to the NHT group. The ratio of extensor/flexor toe muscle strength was positively correlated with MTPJ angle while ankle dorsiflexion ROM and eversion ROM were negatively correlated with MTPJ angle. These results provide insight into potential risk factors (muscle imbalance between toe extensor muscles and toe flexor muscles, limited ankle dorsiflexion ROM and limited eversion ROM) for the development of hammer toe deformity. Additional research is needed to determine if strengthening toe flexor muscles and increasing ankle dorsiflexion or calcaneal eversion ROM could potentially reverse or prevent hammer toe deformity.
Acknowledgements
The authors acknowledge the funding from the following sources that helped support this work: PODS I Award from the Foundation for Physical Therapy (Tuttle), RO1HD36895 (Mueller) and T32 HD007434-14 (Mueller, Tuttle). Sabbatical funding from Yonsei University.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- Allen RH, Gross MT. Toe flexors strength and passive extension range of motion of the first metatarsophalangeal joint in individuals with plantar fasciitis. J. Orthop.Sports Phys. Ther. 2003;33:468–478. doi: 10.2519/jospt.2003.33.8.468. [DOI] [PubMed] [Google Scholar]
- Bhatia D, Myerson MS, Curtis MJ, Cunningham BW, Jinnah RH. Anatomical restraints to dislocation of the second metatarsophalangeal joint and assessment of a repair technique. J. Bone Joint Surg. Am. 1994;76:1371–1375. doi: 10.2106/00004623-199409000-00012. [DOI] [PubMed] [Google Scholar]
- Bus SA, Maas M, Michels RP, Levi M. The role of muscle atrophy in the etiology of claw toe deformity in diabetes may not be as straightforward as widely believed. Diabetes Care. 2009 doi: 10.2337/dc08-2174. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulton AJ. The diabetic foot. Med. Clin. North Am. 1988;72:1513–1530. doi: 10.1016/s0025-7125(16)30719-2. [DOI] [PubMed] [Google Scholar]
- Commean PK, Mueller MJ, Smith KE, Hastings M, Klaesner J, Pilgram T, Robertson DD. Reliability and validity of combined imaging and pressures assessment methods for diabetic feet. Arch. Phys. Med. Rehabil. 2002;83:497–505. doi: 10.1053/apmr.2002.30923. [DOI] [PubMed] [Google Scholar]
- Coughlin MJ. Mallet toes, hammer toes, claw toes, and corns. Causes and treatment of lesser-toe deformities. Postgrad. Med. 1984;75:191–198. doi: 10.1080/00325481.1984.11698001. [DOI] [PubMed] [Google Scholar]
- Coughlin MJ, Dorris J, Polk E. Operative repair of the fixed hammertoe deformity. Foot Ankle Int. 2000;21:94–104. doi: 10.1177/107110070002100202. [DOI] [PubMed] [Google Scholar]
- Dhukaram V, Hossain S, Sampath J, Barrie JL. Correction of hammer toe with an extended release of the metatarsophalangeal joint. J. Bone Joint Surg. Br. 2002;84:986–990. doi: 10.1302/0301-620x.84b7.12811. [DOI] [PubMed] [Google Scholar]
- Diamond JE, Mueller MJ, Delitto A, Sinacore DR. Reliability of a diabetic foot evaluation. Phys. Ther. 1989;69:797–802. doi: 10.1093/ptj/69.10.797. published erratum appears in Phys Ther 1989 Nov;69(11):994. [DOI] [PubMed] [Google Scholar]
- Endo M, shton-Miller JA, Alexander NB. Effects of age and gender on toe flexor muscle strength. J. Gerontol. A Biol. Sci. Med. Sci. 2002;57:M392–M397. doi: 10.1093/gerona/57.6.m392. [DOI] [PubMed] [Google Scholar]
- Hansen ST., Jr . Functional Reconstruction of the Foot and Ankle. Lippincott Williams & Wilkins; Philadephia, PA: 2000. [Google Scholar]
- Hislop HJ, Montgomery J. Daniels and Worthingham’s Muslce Testing: Techniques of Manual Examination. sixth ed. W.B. Saunders Company; Philadelphia, PA: 1995. [Google Scholar]
- Kendall FP, McCreary EK, Provance PG. Muscles: Testing and Function. fourth ed. Lippincott Williams & Wilkins; Philadelphia, PA: 1993. [Google Scholar]
- Lavery LA, Armstrong DG, Vela SA, Quebedeaux TL, Fleischli JG. Practical criteria for screening patients at high risk for diabetic foot ulceration. Arch. Intern. Med. 1998;158:157–162. doi: 10.1001/archinte.158.2.157. [DOI] [PubMed] [Google Scholar]
- Menz HB, Zammit GV, Munteanu SE, Scott G. Plantarflexion strength of the toes: age and gender differences and evaluation of a clinical screening test. Foot Ankle Int. 2006;27:1103–1108. doi: 10.1177/107110070602701217. [DOI] [PubMed] [Google Scholar]
- Milner CE, Soames RW. A comparison of four in vivo methods of measuring tibial torsion. J. Anat. 1998;193:139–144. doi: 10.1046/j.1469-7580.1998.19310139.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller MJ, Hastings MK, Commean PK, Smith KE, Pilgram T, Robertson DD, Johnson JE. Forefoot structural predictors of plantar pressures during walking in people with diabetes and peripheral neuropathy. J. Biomech. 2003;36:1009–1017. doi: 10.1016/s0021-9290(03)00078-2. [DOI] [PubMed] [Google Scholar]
- Nihal A, Goldstein J, Haas J, Hiebert R, Kummer FJ, Liederbach M, Trepman E. Toe flexor forces in dancers and non-dancers. Foot Ankle Int. 2002;23:1119–1123. doi: 10.1177/107110070202301207. [DOI] [PubMed] [Google Scholar]
- Parrish TF. Dynamic correction of clawtoes. Orthop. Clin. North Am. 1973;4:97–102. [PubMed] [Google Scholar]
- Piva SR, Fitzgerald K, Irrgang JJ, Jones S, Hando BR, Browder DA, Childs JD. Reliability of measures of impairments associated with patellofemoral pain syndrome. BMC. Musculoskelet. 2006;7:33. doi: 10.1186/1471-2474-7-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahrmann SA. Diagnosis and movement of movement impairment syndrome. Mosby; St. Louis: 2002. [Google Scholar]
- Scheck M. Etiology of acquired hammertoe deformity. Clin. Orthop. 1977;123:63–69. [PubMed] [Google Scholar]
- Senda M, Takahara Y, Yagata Y, Yamamoto K, Nagashima H, Tukiyama H, Inoue H. Measurement of the muscle power of the toes in female marathon runners using a toe dynamometer. Acta Med. Okayama. 1999;53:189–191. doi: 10.18926/AMO/31617. [DOI] [PubMed] [Google Scholar]
- Schnepp KH. Hammertoe and claw foot. Am. J. Surg. 1937;36:351–359. [Google Scholar]
- Staheli LT, Corbett M, Wyss C, King H. Lower-extremity rotational problems in children. Normal values to guide management. J. Bone Joint Surg. Am. 1985;67:39–47. [PubMed] [Google Scholar]
- Stuberg W, Temme J, Kaplan P, Clarke A, Fuchs R. Measurement of tibial torsion and thigh-foot angle using goniometry and computed tomography. Clin. Orthop. Relat. Res. 1991:208–212. [PubMed] [Google Scholar]
- Tollafild DR, Merriman LM. assessment of the lower limb. In: Merriman LM, Tollafild DR, editors. Assessment of the locomotor system. Churchill Livingstone; 1995. pp. 139–191. [Google Scholar]
- Valmassy R, Stanton B. Tibial torsion. Normal values in children. J Am. Podiatr. Med. Assoc. 1989;79:432–435. doi: 10.7547/87507315-79-9-432. [DOI] [PubMed] [Google Scholar]


