Abstract
Background
Minimally invasive video-assisted thyroidectomy (MIVAT) has received increasing attention as a technique applicable for a subset of thyroid nodules.
Methods
We prospectively assessed 51 MIVAT procedures in 40 patients. Demographic and clinical data were collected, relating to indications, outcome, and oncologic completeness.
Results
Twenty-nine (29) benign and 22 malignant lesions up to 5.9 cm were removed (median, 1.7 cm). All surgical margins of resection were negative. Residual thyroid tissue in the operative bed was assessed by radioiodine uptake in 16 patients (median, 1.76%). Eighty percent (41/51) of procedures were performed on an outpatient basis, and 94% (48/51) did not require a suction drain. No bleeding events or permanent injuries to the recurrent laryngeal nerve occurred.
Conclusions
MIVAT is a safe, thorough, and adaptable procedure. An expanded set of indications makes this procedure available to a broader population of patients.
Keywords: thyroidectomy, endoscopic, minimally invasive surgery, endoscopic thyroid surgery, video-assisted thyroid surgery
Indications for thyroidectomy are primarily based on cytopathologic findings from fine-needle aspiration biopsy (FNAB).1 Unfortunately, these results can be indeterminate and may not rule out malignancy.2 Other clinical situations include small nodules (1–2 cm) where highly suspicious, atypical, or clearly malignant cells are identified without clinical or radiographic evidence of central or lateral neck metastasis. In these situations, some authors have recently advocated a minimally invasive approach using endoscopic-assisted visualization during the thyroidectomy procedure.3–6 Current patient selection criteria for minimally invasive video-assisted thyroidectomy (MIVAT) include small thyroid nodules (25–30 mm in diameter), a relatively normal thyroid gland (about 20 cm3), no evidence of thyroiditis, and no previous neck surgery or radiation.7,8 Benefits include a less extensive surgical field, much smaller incision lengths, and decreased postoperative pain. As thyroid disease is more common in young women, a smaller incision has obvious cosmetic appeal. However, concern has been raised over whether this procedure is oncologically safe and adaptable beyond the few medical centers where it has been developed and optimized.
We have adopted a MIVAT approach for selected patients. We performed a prospective, observational study of our cohort to document whether expanded indications are feasible for this technique after a short learning phase (3–5 cases) and collected follow-up data regarding the potential for outpatient surgery without suction drain tubes. We also used the radioiodine scan and central compartment iodine uptake value as a short-term measure of the completeness of thyroid tissue excision by MIVAT. Our goal was to assess the safety, feasibility, and oncological completeness of MIVAT.
PATIENTS AND METHODS
We performed a prospective, nonrandomized analysis of consecutive MIVAT procedures performed at the University of Pittsburgh Medical Center, between May 2006 and August 2007. Patients were assessed under a protocol approved by the Institutional Review Board. Demographic and clinical data were prospectively collected, including age, sex, surgical indications, thyroid lobe size, and dominant nodule size. Surgical data included incision length, operative time, estimated blood loss, pathological findings, and the need to extend the incision. Surgical drain placement and hospital admissions were also noted. In thyroid cancer patients, postoperative data included radioiodine uptake in the diagnostic scan; the dose of radioiodine for ablation; and laboratory measurements of serum calcium, thyroglobulin, and thyroid-stimulating hormone (TSH). Laryngoscopy was performed in the preoperative and postoperative settings to verify vocal fold motion.
RESULTS
Expanded Indications for Minimally Invasive Video-Assisted Thyroidectomy
Our patients ranged from 17 to 77 years of age (median, 49), and there were 15 men and 25 women (Table 1). Of 51 MIVAT procedures, 43 (84.3%) were hemithyroidectomy and 8 (15.7%) were planned total thyroidectomy procedures. Twenty-nine (56.9%) lesions excised were benign and 22 (43.1%) were malignant.
Table 1.
Patient and thyroid disease characteristics.
| Characteristic | No. | % |
|---|---|---|
| Age | ||
| Median | 49 y | |
| Range | 17–77 y | |
| Sex | ||
| Male | 15 | 37.5 |
| Female | 25 | 63.5 |
| MIVAT procedure | ||
| Hemithyroidectomy | 43 | 84.3 |
| Total thyroidectomy | 8 | 15.7 |
| Thyroid pathology | ||
| Benign | 29 | 56.9 |
| Malignant | 22 | 43.1 |
| Surgical margins | ||
| Negative | 22 | 100 |
| Positive | 0 | 0 |
| Radioiodine (131I) uptake postoperative | ||
| Median | 1.76 | |
| Range | 0.21–3.02 | |
| Radioiodine ablation dose | ||
| Range | 101.4–164.7 mCi | |
Abbreviation: MIVAT, minimally invasive video-assisted thyroidectomy.
Thyroid lesions ranged from 0 cm to 5.9 cm. Overall median nodule size was 1.7 cm. Benign nodules were 1.0 cm to 5.0 cm (median, 1.9 cm), and malignant lesions were 0.5 cm to 5.9 cm (median, 1.7 cm). The thyroid lobe containing the largest nodule was 6.5 × 4.5 × 4.0 cm. Additionally, 3 patients had microscopic foci of papillary thyroid carcinoma. On gross pathologic analysis, the largest thyroid gland dimension was 8.5 cm (median, 5.0 cm) and the thyroid lobes weighed 3.9 to 62 gm (median, 10.4 gm). All thyroid specimens were removed using initial incisions measuring 2.0 cm. In 3 cases, the incision was extended by 0.5 cm intraoperatively to deliver the thyroid lobe. In all cases, estimated blood loss was minimal and we were able to identify critical structures, including the recurrent laryngeal nerve and parathyroid glands. No conversion to a standard open thyroidectomy was necessary. We observed that the incisions stretched 3 to 5 mm intraoperatively due to manual retraction. Follow-up outpatient measurements demonstrated that these stretched incisions reverted to length of 2.0 to 2.5 cm (Figure 1).
FIGURE 1.

Postoperative incision site following minimally invasive video-assisted thyroidectomy (MIVAT) procedure. The incision has reverted to the 2.0-cm initial length approximately 1 month after MIVAT. [Color figure can be viewed in the online issue, which is available at www.interscience.wiley.com.]
Surgical times ranged from 43 to 131 minutes (median, 91 minutes) for hemithyroidectomy and 103 to 215 minutes (median, 151 minutes) for total thyroidectomy. Several difficult cases required increased operative time. These cases included 2 patients with benign histology: 1 patient with Graves’ disease and another with Hashimoto’s thyroiditis. In another case, the operative time of 215 minutes included not only a total thyroidectomy but also an endoscopic central compartment dissection. These difficult cases increased the operative time but did not obviate application of the MIVAT procedure or increase the length of the initial incision.
Suction drainage tubes were used in 3 (5.9%) patients and were not needed in 48 (94.1%). Oxidized regenerated cellulose (Surgicel Fibrillar; Johnson & Johnson) was placed in the operative bed as a precaution. Initially, a number of patients without a surgical drain were observed overnight as inpatients without incident. Based on this experience and publications by others,9,10 most procedures (41, 80.4%) were performed in the outpatient setting. In 8 cases (15.7%), the patients were kept overnight for postoperative calcium monitoring.
Assessment of Minimally Invasive Video-Assisted Thyroidectomy Oncologic Completeness
In the 16 patients with malignant disease, 4 total thyroidectomies, and 12 completion thyroid lobectomies were performed with additional disease identified in 6 (50%) of the contralateral lobes. The surgical margins were negative in every case. All 16 patients with malignant tumors underwent radioactive iodine uptake scans and subsequent 131I ablation. The range of 131I uptake was 0.21% to 3.02%(median, 1.76%) in the thyroid bed. Radioiodine ablation doses were 101.4 to 164.7 mCi. Postoperative thyroglobulin levels were available for 12 patients and were undetectable in each case. Postablative thyroglobulin levels were undetectable in all 16 patients. In 6 patients, central compartment lymph nodes were incidentally or intentionally excised. Five of those 6 patients (83.3%) demonstrated metastatic disease in the central compartment. A complete central compartment dissection was performed through the MIVAT incision in 1 patient with papillary thyroid carcinoma and a preoperative ultrasound that was suspicious for central compartment disease. In this case, 1 of 7 lymph nodes demonstrated metastatic papillary thyroid carcinoma. The postoperative radioiodine uptake for this patient was 0.21%.
Complications
There were no wound infections, hematomas, or seromas. None of the patients had hypertrophic scars or keloid formation. One patient had a temporary recurrent laryngeal nerve (RLN) palsy with spontaneous recovery approximately 3 months postoperatively. No cases of severe hypoparathyroidism occurred, although 2 patients required temporary oral calcium supplementation (2/20; 10%). One of those patients has continued her oral calcium supplementation as she had done preoperatively.
DISCUSSION
The use of MIVAT has received considerable attention and some controversy in recent years.4,11 Whether this procedure is appropriate or applicable to a sufficient population of patients to merit its adoption at additional medical centers has been questioned. With the existing indications, 1 group performed MIVAT procedures in approximately 30% of their patients.8 During our study period, we performed MIVAT in approximately 40% of our thyroid patients. Current indications for MIVAT include indeterminate nodules (<3.5 cm), no previous neck surgery, no palpable metastasis, and small, low-risk papillary thyroid carcinomas.11 As our experience with MIVAT increased, we were able to remove larger thyroid nodules. In the case of indeterminate solitary or multinodular thyroid disease, we removed a 5.9-cm nodule that was diagnosed as papillary thyroid carcinoma. The surgical resection margins were negative and the patient had 2.00% radioiodine uptake in the thyroid bed following completion thyroidectomy. Additionally, we removed a papillary thyroid carcinoma that was 3.8 cm in diameter. These are slightly larger than the sizes described in the current literature but suggest that indications may be expanded as surgeons gain expertise and comfort with MIVAT. The expansion of the indications (Table 2) did not affect patient safety or increase complication rates. However, additional study and follow-up is clearly necessary to validate this observation. Although traditional contraindications for MIVAT include thyroiditis and previous neck surgery, we have also been able to perform the MIVAT procedure on patients with thyroiditis (n = 4) and prior neck surgery (n = 3), without any complications. Our incorporation of this approach for an expanded set of indications has been successful and well received by our patients and the multi-disciplinary thyroid team, consisting of surgeons, endocrinologists, and nuclear medicine radiologists. We caution that careful patient selection and the experience of the surgeon remain critical in ensuring optimal patient outcomes with MIVAT.
Table 2.
Indications for minimally invasive video-assisted thyroidectomy.
| Gland size <9 cm |
| Solitary indeterminate lesions (<3.5 cm) |
| Solitary well-differentiated malignant lesions (<3 cm) |
| No significant substernal extension |
| No evidence of significant metastasis |
Patient satisfaction has been very high with MIVAT. We employed a small incision (2 cm or less) and avoided partial closure or a second incision site as significantly fewer suction drains were placed (48/51; 94.1%). Our patients frequently commented on their pleasure from the cosmetic result, especially once any oncologic issues were resolved. In our experience, there was no additional risk related to voice outcomes or hypoparathyroidism. As other surgeons have noted, the magnification provided through the 5-mm 30° endoscope provided excellent visualization of not only the RLN and parathyroid glands, but also the superior laryngeal nerve (SLN) during isolation and ligation of the superior thyroid vessels (Figure 2). There is additional cost incurred due to the use of the Harmonic Scalpel (Ethicon Endo-Surgery, LLC.; $376/ACE handpiece) Also, 2 video towers are necessary to allow the entire surgical team to view the endoscopic images. However, most otolaryngology surgical suites already have these video towers available for sinus and laryngology procedures. However, others and we have found that extended recovery room observation in low-risk patients is a safe and feasible approach to provide convenience and decrease cost to the healthcare system.8–10 In our series, most of the procedures were performed on an outpatient basis (41/51; 80.4%). A precise cost-benefit analysis of MIVAT as compared with conventional thyroidectomy is warranted and is currently in progress. This approach is only appropriate for a highly selected population, and whether it is an appropriate approach to use in a specific clinical circumstance remains a decision to be made between the surgeon and patient. Overall, our experience demonstrates that this procedure can be easily and safely transferred to experienced thyroid surgeons after a short learning period.
FIGURE 2.
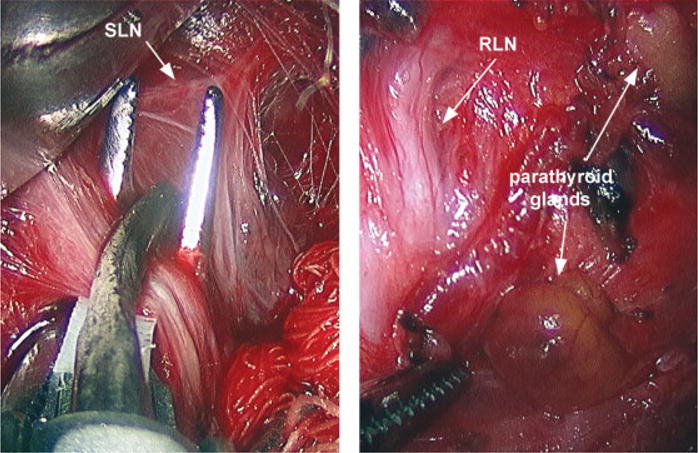
Improved visualization of critical anatomic structures. Minimally invasive video-assisted thyroidectomy (MIVAT) permits excellent intraoperative visualization of the superior laryngeal nerve (SLN; left panel) as well as the recurrent laryngeal nerve (RLN) and parathyroid glands (right panel). [Color figure can be viewed in the online issue, which is available at www.interscience.wiley.com.]
The oncologic efficacy of MIVAT procedures has continued to be debated. We assessed residual thyroid tissue in the central compartment by 131I uptake and the ablative doses of radioiodine required postoperatively. In all of our cases, the malignant thyroid lesions were excised with negative margins. Radioiodine uptake in the thyroid bed (median, 1.76%) was comparable to open thyroidectomy procedures and consistent with a previous report.12 The dose of radioiodine delivered was similar to patients treated by open thyroidectomy approaches at our institution and reported elsewhere (data not shown).12 Additionally, thyroglobulin levels were undetectable in the patients with malignant disease following MIVAT and radioiodine ablation. Lymph nodes adjacent to the thyroid lobe could be intentionally or incidentally removed and histopathologically examined for metastatic disease. Given the potential for central compartment lymph node excision through the MIVAT incision, we elected to perform a central compartment dissection in 1 patient. The procedure was safely completed with clear identification of the RLN and parathyroid glands. Although the biological and clinical significance of metastatic disease is unclear in the current TNM staging of individuals under 45 years of age, the successful removal of lymph nodes from the central compartment demonstrates that MIVAT can provide a comparable degree of histopathologic information as conventional open thyroidectomy procedures. Cumulatively, these findings indicate that MIVAT procedures are safe and oncologically complete for selected low-risk or intermediate-risk thyroid cancer patients. Longer-term follow-up is obviously necessary to document similar outcomes as open thyroidectomy approaches. However, the indolent nature of thyroid malignancy prevents any informative follow-up data from being available until these patients have been clinically followed for at least 5 to 10 years.
References
- 1.Wein RO, Weber RS. Contemporary management of differentiated thyroid carcinoma. Otolaryngol Clin North Am. 2005;38:161–178. doi: 10.1016/j.otc.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 2.Tee YY, Lowe AJ, Brand CA, Judson RT. Fine-needle aspiration may miss a third of all malignancy in palpable thyroid nodules: a comprehensive literature review. Ann Surg. 2007;246:714–720. doi: 10.1097/SLA.0b013e3180f61adc. [DOI] [PubMed] [Google Scholar]
- 3.Miccoli P, Berti P, Conte M, Bendinelli C, Marcocci C. Minimally invasive surgery for thyroid small nodules: preliminary report. J Endocrinol Invest. 1999;22:849–851. doi: 10.1007/BF03343657. [DOI] [PubMed] [Google Scholar]
- 4.Miccoli P, Berti P, Raffaelli M, Materazzi G, Baldacci S, Rossi G. Comparison between minimally invasive video-assisted thyroidectomy and conventional thyroidectomy: a prospective randomized study. Surgery. 2001;130:1039–1043. doi: 10.1067/msy.2001.118264. [DOI] [PubMed] [Google Scholar]
- 5.Ikeda Y, Takami H, Sasaki Y, Kan S, Niimi M. Endoscopic resection of thyroid tumors by the axillary approach. J Cardiovasc Surg (Torino) 2000;41:791–792. [PubMed] [Google Scholar]
- 6.Palazzo FF, Sebag F, Henry JF. Endocrine surgical technique: endoscopic thyroidectomy via the lateral approach. Surg Endosc. 2006;20:339–342. doi: 10.1007/s00464-005-0385-1. [DOI] [PubMed] [Google Scholar]
- 7.Miccoli P. Minimally invasive surgery for thyroid and parathyroid diseases. Surg Endosc. 2002;16:3–6. doi: 10.1007/s00464-001-8140-8. [DOI] [PubMed] [Google Scholar]
- 8.Terris DJ, Chin E. Clinical implementation of endoscopic thyroidectomy in selected patients. Laryngoscope. 2006;116:1745–1748. doi: 10.1097/01.mlg.0000233243.28872.26. [DOI] [PubMed] [Google Scholar]
- 9.Miccoli P, Bellantone R, Mourad M, Walz M, Raffaelli M, Berti P. Minimally invasive video-assisted thyroidectomy: multiinstitutional experience. World J Surg. 2002;26:972–975. doi: 10.1007/s00268-002-6627-7. [DOI] [PubMed] [Google Scholar]
- 10.Terris DJ, Moister B, Seybt MW, Gourin CG, Chin E. Outpatient thyroid surgery is safe and desirable. Otolaryngol Head Neck Surg. 2007;136:556–559. doi: 10.1016/j.otohns.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 11.Terris DJ, Gourin CG, Chin E. Minimally invasive thyroidectomy: basic and advanced techniques. Laryngoscope. 2006;116:350–356. doi: 10.1097/01.mlg.0000191462.58630.e4. [DOI] [PubMed] [Google Scholar]
- 12.Miccoli P, Elisei R, Materazzi G, et al. Minimally invasive video-assisted thyroidectomy for papillary carcinoma: a prospective study of its completeness. Surgery. 2002;132:1070–1073. doi: 10.1067/msy.2002.128694. Discussion 1073–1074. [DOI] [PubMed] [Google Scholar]


