Abstract
Background
Lipophilic and hydrophilic statins have different effects on adiponectin and insulin resistance in experimental studies and different effects on the rate of onset of new diabetes in large scale clinical studies. Therefore, we hypothesized that simvastatin and pravastatin may have differential metabolic effects in hypercholesterolemic patients.
Methods
This was a randomized, single-blind, placebo-controlled, parallel study. Age, gender, and body mass index were matched. Forty-three patients were given placebo, simvastatin 20 mg, or pravastatin 40 mg, respectively once daily for 2 months.
Results
Simvastatin and pravastatin therapy significantly changed lipoprotein levels and improved flow-mediated dilation after 2 months when compared with baseline (P < 0.001) or placebo treatment (P < 0.001 by ANOVA). Simvastatin therapy significantly increased insulin levels (mean % changes; 127%, P = 0.014) and decreased plasma adiponectin levels (10%, P = 0.012) and insulin sensitivity as assessed by QUICKI (6%, P = 0.007) when compared with baseline. By contrast, pravastatin therapy did not significantly change insulin levels (−3%, P = 0.437) but significantly increased plasma adiponectin levels (9%, P = 0.011) and insulin sensitivity (6%, P = 0.008) when compared with baseline. In addition, these effects of simvastatin were significant when compared with pravastatin (P < 0.001 for insulin levels by ANOVA on Ranks, P < 0.001 for adiponectin and P = 0.001 for QUICKI by ANOVA). When compared with baseline, simvastatin significantly increased plasma leptin levels (35%, P = 0.028), but pravastatin did not (1%, P = 0.822).
Conclusions
Despite causing comparable changes in lipoprotein and endothelium-dependent dilation, simvastatin and pravastatin therapy had differential metabolic effects in hypercholesterolemic patients that may be clinically relevant.
Keywords: Statins, Adipocytokines, Insulin resistance, Endothelial function
1. Introduction
Many patients on statin therapy have initial or recurrent coronary heart disease events despite reductions in low-density lipoprotein (LDL) cholesterol [1]. Coronary heart disease is characterized by endothelial dysfunction and frequently clusters with disorders of metabolic homeostasis including obesity and type 2 diabetes that are characterized by insulin resistance [2–4]. These comorbidities may be explained, in part, by reciprocal relationships between endothelial dysfunction and insulin resistance [2–4].
The effects of statins on insulin sensitivity are controversial. Simvastatin improves insulin sensitivity in some diabetic patients [5]. However, others have reported that simvastatin either did not change or worsened insulin sensitivity in diabetic patients [6,7]. Lipophilic statins may cause unfavorable pleiotropic effects including reduction of insulin secretion and exacerbation of insulin resistance [8–10]. Indeed, recent large scale clinical studies suggest that lipophilic statins increase the rate of onset of new diabetes [11–13]. By contrast, hydrophilic statins may not cause unfavorable pleiotropic effects such as reduction of insulin secretion and exacerbation of insulin resistance [8,10]. Pravastatin improves insulin sensitivity in some patients [14–16]; however, others have reported that pravastatin does not alter insulin sensitivity in healthy nondiabetic patients [17]. A recent large scale clinical study demonstrates that pravastatin reduces the rate of onset of new diabetes by 30% [18]. A nested case-control study demonstrates an adjusted odds ratio for pravastatin use alone and simvastatin use alone compared with non-exposed of 0.7 and 1.0, respectively. This suggests a long-term protective effect with pravastatin on the rate of onset of new diabetes [11]. Further, the long-term follow-up (10 years extended from the original 5 years) of West of Scotland Coronary Prevention Study (WOSCOPS) demonstrates that the risk of death from coronary heart disease, nonfatal myocardial infarction, rate of death from cardiovascular causes is significantly reduced with pravastatin [19].
Adiponectin is an anti-inflammatory adipocytokine secreted specifically by adipose cells [20]. In humans, plasma levels of adiponectin are negatively correlated with adiposity and insulin resistance. Indeed, decreased plasma adiponectin levels are observed in patients with diabetes [21]. We recently reported that fenofibrate, candesartan, or efonidipine increases adiponectin levels and insulin sensitivity in patients without changing body mass index [22–24]. Thus, decreased levels of adiponectin may promote insulin resistance rather than simply serving as a biomarker for insulin sensitivity. We also reported that simvastatin 20 mg tended to reduce plasma levels of adiponectin and insulin sensitivity (although these changes did not achieve statistical significance) [25]. Leptin may play an important role in atherosclerotic lesion formation and progression [26,27]. Leptin may potentiate pressor effects of hyperinsulinemia in insulin resistant states, which may have deleterious cardiovascular effects in obesity [28]. Adiponectin and leptin may represent important links between metabolic signals, inflammation, and atherosclerosis [20,27]. Therefore, we hypothesized that simvastatin and pravastatin may have differential metabolic effects in hypercholesterolemic patients.
2. Methods
2.1. Study population and design
We used a randomized, single-blind, placebo-controlled, parallel study design. Age, gender, and body mass index were matched among all subjects. We recruited the patients from a primary care setting in the Vascular Medicine and Atherosclerosis Unit, Cardiology, Gil Medical Center, Gachon University. Before and during the study period a dietitian educated patients to maintain a low fat diet. Patients with hypercholesterolemia (low-density lipoprotein cholesterol levels ≥ 130 mg/dl) participated in this study. We excluded patients with overt liver disease, chronic renal failure, hypothyroidism, myopathy, uncontrolled diabetes, severe hypertension, stroke, acute coronary events, coronary revascularization within the preceding 3 months, or alcohol abuse. No patient had taken any lipid-lowering agent, hormone replacement therapy, or antioxidant vitamin supplements during the 2 months preceding our study. All the forty-three patients were given placebo, simvastatin 20 mg, and pravastatin 40 mg, respectively once daily during a 2-month treatment period. A research nurse counted pills at the end of treatment to monitor compliance. The patients were seen at least every 14 days during the study. To minimize side effects, we measured serum asparate aminotransferase, alanine aminotransferase, creatine kinase, blood urea nitrogen and creatinine before and after therapy. Each patient on placebo and pravastatin 40 mg withdrew from the study because they moved to other places and they dropped out from the study. Thus, 42 patients on placebo, 43 patients on simvastatin 20 mg, and 42 patients on pravastatin 40 mg, respectively finished the study. None of the patients were diabetic. Six patients taking placebo, 7 patients taking simvastatin, and 7 patients taking pravastatin were smokers. Seven patients taking placebo, 7 patients taking simvastatin, and 8 patients taking pravastatin were also taking beta adrenergic blockers. Six patients taking placebo, 7 patients taking simvastatin, and 8 patients taking pravastatin were also taking calcium channel blockers to control blood pressure. No additional medications including aspirin or nonsteroidal anti-inflammatory drugs were allowed during the study period to avoid confounding effects of other drugs. Calcium channel or beta adrenergic blockers were withheld for ≥48 h before the study.
2.2. Laboratory assays and vascular studies
Blood samples for laboratory assays were obtained at approximately 8:00 a.m. following overnight fasting before and at the end of each 2-month treatment period. These samples were immediately coded so that investigators performing laboratory assays were blinded to subject identity or study sequence. Assays for lipids, glucose, and plasma adiponectin and leptin were performed in duplicate by ELISA (R&D Systems, Inc., Minneapolis, Minnesota), assays for high sensitivity C-reactive protein (CRP) levels by latex agglutination (CRP-Latex(II)®, Denka-Seiken, Tokyo, Japan), and assays for plasma insulin levels by immunoradiometric assay (INSULIN-RIABEAD® II, SRL, Inc., Tokyo, Japan) as previously described [22–25,29,30]. The interassay and intraassay coefficients of variation were <6%. Quantitative Insulin-Sensitivity Check Index (QUICKI), a surrogate index of insulin sensitivity based on fasting glucose and insulin levels, was calculated as follows (insulin is expressed in microU/ml and glucose in mg/dl): QUICKI = 1/[log(insulin) + log(glucose)] [31,32]. Imaging studies of the right brachial artery were performed using an ATL HDI 3000 ultrasound machine (ATL Philips, Bothell, WA, USA) equipped with a 10 MHz linear-array transducer, based on a previously published technique [22–25,29,30].
2.3. Statistical analysis
Data are expressed as mean ± SEM or median (range:25%–75%). After testing data for normality, we used Student’s paired t or Wilcoxon Signed Rank test to compare values between baseline and treatment at 2 months, as reported in Table 1. We used one way analysis of variance (ANOVA) or Kruskal–Wallis ANOVA on Ranks to compare baseline or treatment effects among treatment groups. Post-hoc comparisons between different treatment pairs were made using the Student–Newman–Keuls multiple comparison procedures or Dunn’s method. Pearson or Spearman correlation coefficient analysis was used to assess associations between measured parameters, as reported in Table 2. We calculated that 30 subjects would provide 80% power for detecting an absolute increase of 1.5% or greater in flow-mediated dilation of the brachial artery between baseline and simvastatin 20 mg, with α = 0.05 based on our previous studies [25]. The comparison of endothelium-dependent dilation was prospectively designated as the primary end-point of the study. All other comparisons were considered secondary. A value of P < 0.05 was considered to represent statistical significance.
Table 1.
Effects of placebo, simvastatin 20 mg, and pravastatin 40 mg in hypercholesterolemic patients.
| Variables | Placebo (P) (n = 42) |
Simvastatin (S) (n = 43) |
Pravastatin (M) (n = 42) |
ANOVA | P/S | S/M | P/M | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Treatment | Baseline | Treatment | Baseline | Treatment | |||||
| Age | 59 ± 1 | 58 ± 2 | 56 ± 2 | 0.382 | ||||||
| Sex (M:F) | 16:26 | 17:26 | 15:27 | |||||||
| BMI, kg/m2 | 24.52 ± 0.54 | 24.42 ± 0.54 | 25.25 ± 0.53 | 25.11 ± 0.51 | 25.48 ± 0.48 | 25.41 ± 0.44 | 0.392 | |||
| Lipids (mg/dl) | ||||||||||
| Total cholesterol | 267 ± 5 | 251 ± 6‡ | 260 ± 5 | 187 ± 5‡ | 254 ± 5 | 193 ± 5‡ | <0.001 | <0.05 | NS | <0.05 |
| Triglycerides | 147 ± 12 | 164 ± 15 | 143 ± 13 | 125 ± 12* | 162 ± 9 | 143 ± 10* | 0.012 | <0.05 | NS | <0.05 |
| LDL cholesterol | 177 ± 6 | 163 ± 6‡ | 178 ± 5 | 107 ± 5‡ | 170 ± 5 | 110 ± 5‡ | <0.001 | <0.05 | NS | <0.05 |
| Apo B | 134 ± 3 | 132 ± 4 | 134 ± 3 | 91 ± 3‡ | 125 ± 5 | 92 ± 4‡ | <0.001 | <0.05 | <0.05 | <0.05 |
| HDL cholesterol | 55 ± 2 | 51 ± 2* | 51 ± 2 | 50 ± 2 | 54 ± 2 | 54 ± 2 | 0.199 | |||
| Apo A1 | 163 ± 3 | 160 ± 3 | 160 ± 3 | 163 ± 4 | 153 ± 4 | 162 ± 5* | 0.129 | |||
| LDL/HDL ratio | 3.3 ± 0.1 | 3.3 ± 0.1 | 3.6 ± 0.1 | 2.2 ± 0.1‡ | 3.4 ± 0.2 | 2.2 ± 0.1‡ | <0.001 | <0.05 | NS | <0.05 |
| Vasomotor | ||||||||||
| FMD Dilation (%) | 4.56 ± 0.18 | 4.88 ± 0.14 | 4.98 ± 0.16 | 7.87 ± 0.15‡ | 4.37 ± 0.26 | 6.94 ± 0.30‡ | <0.001 | <0.05 | NS | <0.05 |
| NTG Dilation (%) | 14.51 ± 0.57 | 14.49 ± 0.56 | 14.13 ± 0.45 | 14.75 ± 0.55 | 14.62 ± 0.71 | 14.45 ± 0.72 | 0.496 | |||
| Inflammation | ||||||||||
| CRP (mg/l) | 1.00 (0.70–2.20) | 1.00 (0.40–2.10) | 1.00 (0.40–3.10) | 1.00 (0.50–2.05) | 1.45 (0.60–2.10) | 1.15 (0.40–1.80) | 0.677 | |||
| Insulin resistance | ||||||||||
| ADP (μg/ml) | 6.2 ± 0.7 | 6.0 ± 0.7 | 5.8 ± 0.8 | 5.2 ± 0.8* | 5.6 ± 0.6 | 6.1 ± 0.6* | <0.001 | <0.05 | <0.05 | NS |
| Insulin (μU/ml) | 3.05 ± 0.35 | 3.25 ± 0.25 | 2.81 ± 0.36 | 4.25 ± 0.57* | 3.18 ± 0.29 | 3.01 ± 0.35 | <0.001 | NS | <0.05 | NS |
| Glucose (mg/dl) | 94 ± 3 | 91 ± 2 | 97 ± 2 | 97 ± 2 | 99 ± 3 | 96 ± 3 | 0.478 | |||
| QUICKI | 0.429 ± 0.008 | 0.427 ± 0.011 | 0.460 ± 0.016 | 0.424 ± 0.013+ | 0.417 ± 0.007 | 0.443 ± 0.013+ | 0.001 | NS | <0.05 | <0.05 |
| Leptin (ng/ml) | 9.51 (4.80–13.86) | 10.47 (6.14–12.63) | 6.73 (3.76–14.25) | 9.34 (4.09–16.21)* | 7.43 (4.27–10.97) | 6.54 (3.98–12.31) | 0.056 | |||
Data are expressed as means ± SEM or median (25th percentile–75th percentile).
BMI, body mass index; CRP, high-sensitivity C-reactive protein; ADP, adiponectin; Quantitative Insulin-Sensitivity Check Index (QUICKI) = 1/[log(insulin) + log(glucose)] [31].
P/S, placebo vs simvastatin 20 mg; S/M, simvastatin 20 mg vs pravastatin 40 mg; P/M, placebo vs pravastatin 40 mg; NS, not significant.
There were no significant differences among each baseline values.
P < 0.05.
P < 0.01.
P < 0.001 for comparison with each baseline value.
Table 2.
Correlations before and after placebo, simvastatin 20 mg and pravastatin 40 mg in hypercholesterolemic patients.
| Placebo |
Simvastatin |
Pravastatin |
||||
|---|---|---|---|---|---|---|
| r | p | r | p | r | p | |
| Before treatment | ||||||
| Adiponectin vs BMI | −0.308 | 0.048 | −0.454 | 0.002 | −0.320 | 0.039 |
| Adiponectin vs HDL cholesterol | 0.379 | 0.013 | 0.315 | 0.040 | 0.420 | 0.006 |
| Adiponectin vs CRP | −0.009 | 0.955 | 0.361 | 0.018 | −0.214 | 0.173 |
| Leptin vs BMI | 0.592 | <0.001 | 0.307 | 0.046 | 0.507 | <0.001 |
| Leptin vs insulin | 0.274 | 0.079 | 0.382 | 0.011 | 0.374 | 0.015 |
| Leptin vs QUICKI | −0.346 | 0.025 | −0.346 | 0.023 | −0.378 | 0.014 |
| After treatment | ||||||
| %Adiponectin vs %insulin | −0.574 | <0.001 | −0.465 | 0.002 | −0.325 | 0.036 |
| %Adiponectin vs %QUICKI | 0.657 | <0.001 | 0.440 | 0.003 | 0.330 | 0.033 |
| %Adiponectin vs %Leptin | −0.144 | 0.362 | 0.185 | 0.233 | 0.013 | 0.933 |
| %Adiponectin vs %CRP | −0.191 | 0.225 | −0.031 | 0.843 | 0.063 | 0.689 |
| %QUICKI vs %insulin | −0.878 | <0.001 | −0.677 | <0.001 | −0.486 | 0.001 |
| %QUICKI vs %Leptin | −0.152 | 0.337 | 0.067 | 0.671 | −0.139 | 0.379 |
| %Leptin vs %insulin | 0.204 | 0.194 | 0.183 | 0.241 | 0.416 | 0.006 |
Pearson or Spearman correlation coefficient analysis was used to assess associations between measured parameters. BMI, body mass index; CRP, C-reactive protein; QUICKI, Quantitative Insulin-Sensitivity Check Index.
3. Results
There were no significant differences between groups for any of the baseline measurements (Table 1).
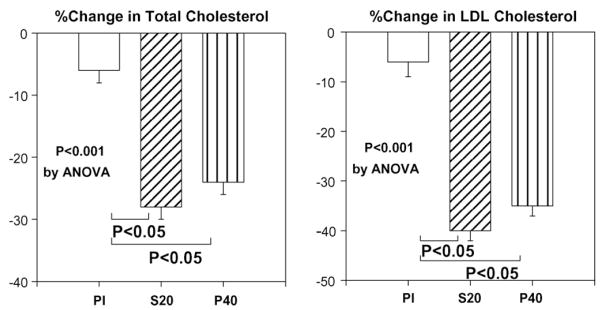
3.1. Effects on lipids
Placebo treatment significantly reduced total, LDL, and high-density lipoprotein (HDL) cholesterol levels from baseline. Simvastatin and pravastatin therapy also significantly reduced total cholesterol, LDL cholesterol, apolipoprotein B levels, and LDL/HDL ratio from baseline (all P < 0.001 by paired t-test) after 2 months administration. Moreover, these effects of simvastatin and pravastatin were also significant when compared with placebo treatment (P < 0.001 by ANOVA; Fig. 1). Simvastatin and pravastatin significantly reduced triglycerides levels from baseline (all P < 0.05 by paired t-test) after 2 months administration. These effects of simvastatin and pravastatin were also significant when compared with placebo treatment (P = 0.012 by ANOVA). Pravastatin significantly increased apolipoprotein AI levels from baseline (P = 0.012 by paired t-test) after 2 months administration.
Fig. 1.
Simvastatin and pravastatin significantly reduced total cholesterol (mean % changes; 28 and 24%) and LDL cholesterol (40 and 35%) from baseline (both P < 0.001 by paired t-test) after 2 months administration. And these effects of simvastatin and pravastatin were also significant when compared with placebo (P < 0.001 by ANOVA). Pl, placebo; S20, simvastatin 20 mg; P40, pravastatin 40 mg. Standard error of the mean is identified by the bars.
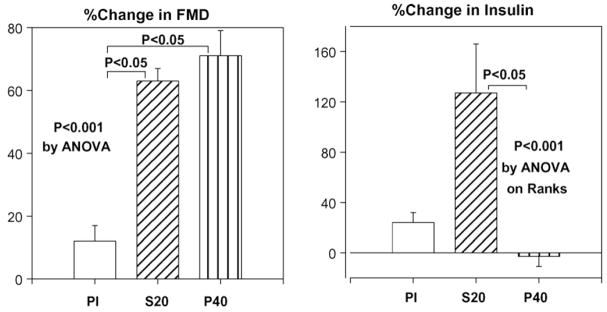
3.2. Effects on vasomotor function and high sensitivity c-reactive protein
Placebo treatment did not significantly improve flow-mediated dilator response to hyperemia (FMD) relative to baseline measurements. By contrast, both simvastatin and pravastatin significantly improved FMD after 2 months therapy when compared with baseline (P < 0.001 by paired t-test) or when compared with placebo treatment (P < 0.001 by ANOVA; Fig. 2). Brachial artery dilator responses to nitroglycerin were not significantly different between any of the therapies. Placebo treatment did not significantly change high sensitivity CRP levels relative to baseline measurements. Simvastatin and pravastatin tended to reduce high sensitivity CRP levels relative to baseline measurements.
Fig. 2.
Simvastatin and pravastatin significantly improved flow-mediated dilator response to hyperemia (FMD) (mean % changes; 63 and 71%) after 2 months therapy when compared with baseline (both P < 0.001 by paired t-test). All of these effects were also significant when compared with placebo (P < 0.001 by ANOVA). Simvastatin significantly increased insulin levels (mean % changes; 127%) after 2 months therapy when compared with baseline (P = 0.014 by paired t-test). Pravastatin did not significantly change insulin levels (mean % changes; −3%) after 2 months therapy when compared with baseline (P = 0.437 by paired t-test). The effects of simvastatin to raise fasting insulin levels were significant when compared with pravastatin (P < 0.001 by ANOVA on Ranks). Pl, placebo; S20, simvastatin 20 mg; P40, pravastatin 40 mg. Standard error of the mean is identified by the bars.
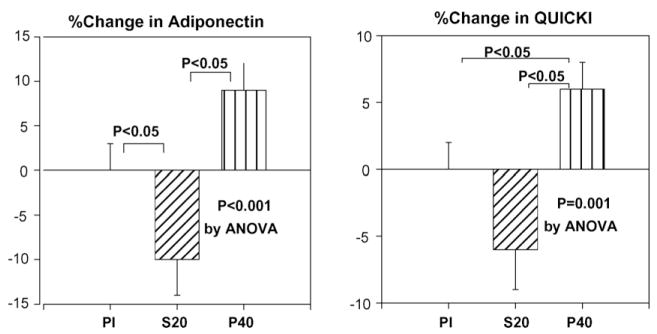
3.3. Effects on adipocytokines and insulin resistance
Placebo did not significantly change insulin or glucose levels from baseline. Simvastatin and pravastatin did not significantly change glucose levels after 2 months administration when compared with baseline. However, simvastatin significantly increased insulin levels after 2 months therapy when compared with baseline (P = 0.014 by paired t-test). Importantly, pravastatin did not significantly change insulin levels after 2 months therapy when compared with baseline (P = 0.437 by paired t-test). The effects of simvastatin treatment to raise fasting insulin levels were significant when compared with pravastatin treatment (P < 0.001 by ANOVA on Ranks; Fig. 2).
We observed significant inverse correlations between baseline body mass index and baseline adiponectin levels and significant correlations between baseline high density lipoprotein cholesterol levels and baseline adiponectin levels (Table 2). Placebo did not significantly change plasma adiponectin levels and insulin sensitivity (determined by QUICKI) relative to baseline measurements. Simvastatin significantly decreased plasma adiponectin levels (P = 0.012 by paired t-test) and insulin sensitivity (P = 0.007 by paired t-test) when compared with baseline. Pravastatin significantly increased plasma adiponectin levels (P = 0.011 by paired t-test) and insulin sensitivity (P = 0.008 by paired t-test) when compared with baseline. Moreover, these effects of pravastatin were significant when compared with either placebo or simvastatin (P < 0.001 for adiponectin and P = 0.001 for QUICKI by ANOVA; Fig. 3). The magnitude of change in insulin, adiponectin, and QUICKI were significantly different between simvastatin and pravastatin despite similar extent of changes in lipoprotein levels with both therapies.
Fig. 3.
Simvastatin significantly decreased plasma adiponectin levels (mean % changes; 10%, P = 0.012 by paired t-test) and insulin sensitivity (mean % changes; 6%, P = 0.007 by paired t-test) when compared with baseline. Pravastatin significantly increased plasma adiponectin levels (mean % changes; 9%, P = 0.011 by paired t-test) and insulin sensitivity (mean % changes; 6%, P = 0.008 by paired t-test) when compared with baseline. Moreover, these effects of pravastatin were significant when compared with placebo and simvastatin (P < 0.001 for adiponectin and P = 0.001 for QUICKI by ANOVA). Pl, placebo; S20, simvastatin 20 mg; P40, pravastatin 40 mg. Standard error of the mean is identified by the bars.
We observed significant correlations between baseline body mass index and baseline leptin levels and between baseline insulin levels and baseline leptin levels and significant inverse correlations between baseline QUICKI and baseline leptin levels (Table 2). Placebo did not significantly change plasma leptin levels relative to baseline measurements. Simvastatin significantly increased plasma leptin levels (P = 0.028 by Wilcoxon Signed Rank test) when compared with baseline. Pravastatin did not significantly change plasma leptin levels (P = 0.822 by Wilcoxon Signed Rank test) when compared with baseline. These effects of simvastatin were not significant when compared with placebo and pravastatin (P = 0.056 by ANOVA).
We investigated whether changes in percent flow-mediated dilator response to hyperemia, plasma levels of adiponectin, insulin, insulin resistance, or leptin were related to changes in lipoprotein levels. There were no significant correlations between changes in these parameters and changes in lipoprotein levels following any of therapies. There were inverse correlations between percent changes in adiponectin levels and percent changes in insulin and correlations between percent changes in adiponectin levels and percent changes in QUICKI and inverse correlations between percent changes in QUICKI and percent changes in insulin following therapies (Table 2).
Because CRP inhibits adiponectin gene expression and production [33] and insulin stimulates leptin secretion [34] by adipocytes, we investigated these correlations. There were no significant correlations between adiponectin and CRP levels before or following therapies. There were correlations between leptin and insulin levels before therapies. However, there were no significant correlations between percent changes in leptin and percent changes in insulin levels following therapies (Table 2).
We compared study outcomes between men and women. We did not find any significant differences among men and women with respect to any of the study outcomes (data not shown).
4. Discussion
We observed that simvastatin and pravastatin both significantly reduced total cholesterol, LDL cholesterol, apolipoprotein B, LDL/HDL ratio, and triglycerides levels with comparable reduction after 2 months administration, when compared with placebo. Simvastatin and pravastatin also both significantly improved endothelium-dependent dilation to a comparable extent after 2 months therapy when compared with placebo. However, simvastatin significantly increased insulin and leptin levels and decreased adiponectin levels and insulin sensitivity. By contrast, pravastatin significantly increased adiponectin levels and insulin sensitivity and did not change insulin and leptin levels. Thus, despite comparable changes in lipoprotein and endothelium-dependent dilation, simvastatin and pravastatin had differential metabolic effects in hypercholesterolemic patients.
Due to reciprocal relationships between endothelial dysfunction and insulin resistance [2–4], we hypothesized that improvements in endothelial dysfunction may be accompanied by simultaneous improvement in metabolic parameters. However, simvastatin significantly reduced adiponectin levels and insulin sensitivity and increased insulin and leptin levels despite of improvement of endothelium-dependent dilation in hypercholesterolemic patients. Further, there were no significant correlations between endothelial dysfunction and metabolic parameters. By contrast, pravastatin significantly increased adiponectin levels and insulin sensitivity with improvement of endothelium-dependent dilation in hypercholesterolemic patients. In previous studies with fenofibrate, ramipril, angiotensin II receptor blockers, or efonidipine, improvement in endothelial dysfunction was accompanied by simultaneous improvement in insulin sensitivity and increased adiponectin levels [22–25,29]. Taken together, this suggests that not all mechanisms for improving endothelial dysfunction are tightly coupled to metabolic homeostasis. Alternatively, potential improvements in insulin sensitivity and adiponectin levels caused by improvement in endothelial function after simvastatin therapy may be masked by other endothelial-independent effects of simvastatin that worsen insulin resistance and lower adiponectin and increase leptin levels. The fact that some statins improve insulin sensitivity while others do not is consistent with this interpretation.
Adiponectin is an adipose-derived factor that augments and mimics metabolic and vascular actions of insulin [20]. In our study, simvastatin and pravastatin therapies significantly changed adiponectin levels. Plasma adiponectin and leptin levels are highly related to body fat content. In the current study, there were significant correlations between adiponectin or leptin levels and body mass index before therapies. Because we did not measure fat mass change by fat CT scan, it might be possible that fat mass change is different in the two groups. However, when we look at the different effects of simvastatin and pravastatin without a corresponding change in body mass index, both drugs may be directly altering adiponectin levels independent of adiposity. Indeed, pravastatin enhances adiponectin secretion from 3T3-L1 adipocytes. Moreover, pravastatin treatment causes an increase in adiponectin mRNA levels and increases plasma levels of adiponectin in C57BL/6J mice (without body weight changes) that is associated with enhanced insulin sensitivity [35]. By contrast, simvastatin does not increase production of adiponectin in 3T3L1 adipoctytes [35]. In humans, pravastatin therapy significantly increases plasma adiponectin levels and insulin sensitivity without a corresponding change in body mass index in patients with impaired glucose tolerance and coronary artery disease [16]. Pravastatin therapy does not affect adiponectin and insulin sensitivity in healthy nondiabetic patients [17]. However, it significantly increases plasma adiponectin levels in samples from the WOSCOPS biobank [35] and significantly increases insulin sensitivity [15]. Decreasing adiponectin levels is predicted to worsen insulin sensitivity by multiple mechanisms [20,36]. In the current study, there were correlations between percent changes in adiponectin levels and percent changes in insulin or QUICKI following therapies.
There may be additional mechanisms to reduce insulin sensitivity and adiponectin levels following simvastatin therapies. Lipophilic statins, particularly at high doses, may cause unfavorable pleiotropic effects such as reduction of insulin secretion and exacerbation of insulin resistance [8–10]. Lipophilic statins inhibit the synthesis of isoprenoid and suppress ubiquinone (CoQ10) biosynthesis. Lipophilic statins can thus delay formation of ATP by pancreatic β cells, leading to disturbed secretion of insulin [37]. Simvastatin suppresses glucose-induced elevation of intra-cellular Ca2+ level in a dose-dependent manner when assessed using the patch clamp method. When the influence of statins on glucose-stimulated insulin secretion was evaluated by direct measurement, simvastatin exerted significant suppression. The less lipophilic inhibitor, simvastatin-acid, inhibited the first phase cytosolic Ca2+ increase but was two orders of magnitude less potent. The hydrophilic inhibitor, pravastatin was without effect on cytosolic Ca2+. Simvastatin inhibited glucose-induced insulin secretion from islets, whereas pravastatin had no effect. Inhibitory potencies of statins parallel their lipophilicities [8]. The possibility of lipophilic statins reducing sensitivity to insulin was suggested by an experiment using rats with streptozotocin-induced diabetes mellitus. The blood glucose level, as determined by oral glucose tolerance test after 6 weeks of treatment, was higher in the atorvastatin treatment group than in the control group. By contrast, pravastatin does not influence glucose tolerance [10]. It is possible that lipophilic statins are taken up by the pancreas, fat tissue, and muscle where they may cause unfavorable pleiotropic effects such as reduction of insulin secretion and exacerbation of insulin resistance.
The effects of statins on adiponectin and insulin sensitivity are controversial in humans. Simvastatin and atorvastatin improve insulin sensitivity in some diabetic patients [5]. However, others have reported that simvastatin either does not change or worsen insulin sensitivity in diabetic patients [6,7]. Rosuvastatin, intermediate between hydrophilic and lipophilic statins does not change plasma levels of adiponectin and insulin sensitivity in patients with familial combined hyperlipidaemia [38]. We reported that simvastatin 20 mg tended to reduce plasma levels of adiponectin and insulin sensitivity in hypercholesterolemic, hypertensive patients [25] and in patients with type 2 diabetes [29]. Recently, we performed another study investigating the effects of simvastatin 10, 20, 40, and 80 mg, respectively. We observed that simvastatin significantly improved endothelium-dependent dilation, but reduced adiponectin levels and insulin sensitivity in hypercholesterolemic patients independent of dosage and the extent of apolipoprotein B reduction [39]. In the current study, we observed similar results. By contrast, pravastatin therapy significantly increased plasma adiponectin levels and insulin sensitivity. The effects of simvastatins on insulin were significant when compared with placebo and pravastatin. Post-hoc comparison demonstrated ignificant differences between simvastatin and pravastatin. Simvastatin significantly increases serum insulin levels whereas a modified Mediterranean-type diet counteracts this effect of simvastatin [40]. Pravastatin tended to lower fasting glucose and insulin levels and significantly increased insulin sensitivity index without changing body weight in patients [16]. Weight loss, diet control, physical exercise, and smoking affect adiponectin levels [20]. However, our study is a 2-month study and patients did not change their life style much during these 2 months except for a low fat diet. Therefore, the effects of lifestyle-related factors may be minimal in our study.
Recent large scale clinical studies have demonstrated that lipophilic statins may increase, rather than decrease the rate of onset of new diabetes [11–13]. In the sub-group analysis of diabetic patients in the Anglo-Scandinavian Cardiac Outcomes Trial–Lipid Lowering Arm (ASCOT–LLA) study, atorvastatin 10 mg treatment group reduced the cumulative incidence of non-fatal myocardial infarction and fatal coronary heart disease. However, onset of diabetes mellitus was seen more frequently in the atorvastatin treatment group than in the placebo group [13]. The onset of diabetes mellitus was seen more frequently in the simvastatin 40 mg treatment group than in the placebo group [12]. A nested case-control study reported that an adjusted odds ratio for simvastatin use alone compared with non-exposed of 1.0 and for pravastatin use alone compared with non-exposed of 0.7 [11]. Indeed, pravastatin reduces the rate of onset of new diabetes by 30% in large scale clinical studies [18]. Thus, different statins have differential effects on the rate of new onset diabetes that may be clinically relevant.
Increasing leptin levels may cause insulin resistance by several mechanisms [27]. Leptin negatively regulates insulin signaling and glucose uptake by increasing serine phosphorylation of insulin receptor substrate 1 [41,42]. Insulin stimulates leptin secretion by adipocytes [34]. In the current study, there were significant correlations between leptin and body mass index, insulin levels, or QUICKI before therapies. Simvastatin increased insulin levels and leptin levels without a corresponding change in body mass index. By contrast, pravastatin did not change both insulin and leptin levels. However, there were no significant correlations between percent changes in leptin and percent changes in insulin levels or QUICKI following therapies. Others reported that pravastatin does not change leptin levels [17]. Simvastatin may be directly altering leptin levels independent of adiposity.
Statins decrease interleukin-induced plasma CRP levels independent of cholesterol lowering effects [43,44]. Statins decrease interleukin-1beta-induced plasma CRP levels. These direct anti-inflammatory effects in vivo occur at the transcriptional level by up-regulating IκB protein expression and reducing nuclear translocation of p50-NF-κB and have been confirmed in cultured human liver slices and in human hepatoma cells [43]. Statins also decrease interleukin-6-induced CRP production directly in human hepatocytes via inhibition of protein geranylgeranylation. These effects are reversed by mevalonate [44]. Thus, there is a direct suppressive effect of statins on CRP expression independent of cholesterol lowering and atherogenesis. We report simvastatin lowers CRP in hyperlipidemic coronary patients [45]. In the current study, we observed that simvastatin and pravastatin did not significantly lower CRP in hyperlipidemic patients. This may be due, in part, to very low baseline CRP levels.
In summary, simvastatin significantly increased insulin and leptin levels and decreased adiponectin levels and insulin sensitivity. By contrast, pravastatin significantly increased adiponectin levels and insulin sensitivity and did not change insulin and leptin levels. Despite comparable changes in lipoprotein and endothelium-dependent dilation, simvastatin and pravastatin have differential metabolic effects in hypercholesterolemic patients that may have therapeutic implications for insulin resistant patients.
Acknowledgments
This study was partly supported by grants from established investigator award (2006-1, 2007-1), Gachon University Gil Medical Center.
Footnotes
Conflict of interest
All authors declare no conflict of interest.
References
- 1.Sacks FM, Tonkin AM, Shepherd J, et al. Effect of pravastatin on coronary disease events in subgroups defined by coronary risk factors: the Prospective Pravastatin Pooling Project. Circulation. 2000;102:1893–900. doi: 10.1161/01.cir.102.16.1893. [DOI] [PubMed] [Google Scholar]
- 2.Kim J, Montagnani M, Koh KK, Quon MJ. Reciprocal relationships between insulin resistance and endothelial dysfunction: molecular and pathophysiological mechanisms. Circulation. 2006;113:1888–904. doi: 10.1161/CIRCULATIONAHA.105.563213. [DOI] [PubMed] [Google Scholar]
- 3.Han SH, Quon MJ, Koh KK. Reciprocal relationships between abnormal metabolic parameters and endothelial dysfunction. Curr Opin Lipidol. 2007;18:58–65. doi: 10.1097/MOL.0b013e328012b627. [DOI] [PubMed] [Google Scholar]
- 4.Muniyappa R, Montagnani M, Koh KK, Quon MJ. Cardiovascular actions of insulin. Endocr Rev. 2007;28:463–91. doi: 10.1210/er.2007-0006. [DOI] [PubMed] [Google Scholar]
- 5.Paolisso G, Barbagallo M, Petrella G, et al. Effects of simvastatin and atorvastatin administration on insulin resistance and respiratory quotient in aged dyslipidemic non-insulin dependent diabetic patients. Atherosclerosis. 2000;150:121–7. doi: 10.1016/s0021-9150(99)00352-4. [DOI] [PubMed] [Google Scholar]
- 6.Farrer M, Winocour PH, Evans K, et al. Simvastatin in non-insulin-dependent diabetes mellitus: effect on serum lipids, lipoproteins and haemostatic measures. Diabetes Res Clin Pract. 1994;23:111–9. doi: 10.1016/0168-8227(94)90018-3. [DOI] [PubMed] [Google Scholar]
- 7.Ohrvall M, Lithell H, Johansson J, Vessby B. A comparison between the effects of gemfibrozil and simvastatin on insulin sensitivity in patients with non-insulin-dependent diabetes mellitus and hyperlipoproteinemia. Metabolism. 1995;44:212–7. doi: 10.1016/0026-0495(95)90267-8. [DOI] [PubMed] [Google Scholar]
- 8.Yada T, Nakata M, Shiraishi T, Kakei M. Inhibition by simvastatin, but not pravastatin, of glucose-induced cytosolic Ca2+ signalling and insulin secretion due to blockade of L-type Ca2+ channels in rat islet beta-cells. Br J Pharmacol. 1999;126:1205–13. doi: 10.1038/sj.bjp.0702397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chamberlain LH. Inhibition of isoprenoid biosynthesis causes insulin resistance in 3T3-L1 adipocytes. FEBS Lett. 2001;507:357–61. doi: 10.1016/s0014-5793(01)03007-1. [DOI] [PubMed] [Google Scholar]
- 10.Kanda M, Satoh K, Ichihara K. Effects of atorvastatin and pravastatin on glucose tolerance in diabetic rats mildly induced by streptozotocin. Biol Pharm Bull. 2003;26:1681–4. doi: 10.1248/bpb.26.1681. [DOI] [PubMed] [Google Scholar]
- 11.Jick SS, Bradbury BD. Statins and newly diagnosed diabetes. Br J Clin Pharmacol. 2004;58:303–9. doi: 10.1111/j.1365-2125.2004.02142.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7–22. [Google Scholar]
- 13.Sever PS, et al. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial–Lipid Lowering Arm (ASCOT–LLA): a multicentre randomised controlled trial. Lancet. 2003;361:1149–58. doi: 10.1016/S0140-6736(03)12948-0. [DOI] [PubMed] [Google Scholar]
- 14.Chan P, Tomlinson B, Lee CB, et al. Beneficial effects of pravastatin on fasting hyperinsulinemia in elderly hypertensive hypercholesterolemic subjects. Hypertension. 1996;28:647–51. doi: 10.1161/01.hyp.28.4.647. [DOI] [PubMed] [Google Scholar]
- 15.Guclu F, Ozmen B, Hekimsoy Z, Kirmaz C. Effects of a statin group drug, pravastatin, on the insulin resistance in patients with metabolic syndrome. Biomed Pharmacother. 2004;58:614–8. doi: 10.1016/j.biopha.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 16.Sugiyama S, Fukushima H, Kugiyama K, et al. Pravastatin improved glucose metabolism associated with increasing plasma adiponectin in patients with impaired glucose tolerance and coronary artery disease. Atherosclerosis. 2007;194:e43–51. doi: 10.1016/j.atherosclerosis.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 17.Gannage-Yared MH, Azar RR, Amm-Azar M, et al. Pravastatin does not affect insulin sensitivity and adipocytokines levels in healthy nondiabetic patients. Metabolism. 2005;54:947–51. doi: 10.1016/j.metabol.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 18.Freeman DJ, Norrie J, Sattar N, et al. Pravastatin and the development of diabetes mellitus: evidence for a protective treatment effect in the West of Scotland Coronary Prevention Study. Circulation. 2001;103:357–62. doi: 10.1161/01.cir.103.3.357. [DOI] [PubMed] [Google Scholar]
- 19.Ford I, et al. Long-term follow-up of the West of Scotland Coronary Prevention Study. N Engl J Med. 2007;357:1477–86. doi: 10.1056/NEJMoa065994. [DOI] [PubMed] [Google Scholar]
- 20.Han SH, Quon MJ, Kim JA, Koh KK. Adiponectin and cardiovascular disease: response to therapeutic interventions. J Am Coll Cardiol. 2007;49:531–8. doi: 10.1016/j.jacc.2006.08.061. [DOI] [PubMed] [Google Scholar]
- 21.Yu JG, Javorschi S, Hevener AL, et al. The effect of thiazolidinediones on plasma adiponectin levels in normal, obese, and type 2 diabetic subjects. Diabetes. 2002;51:2968–74. doi: 10.2337/diabetes.51.10.2968. [DOI] [PubMed] [Google Scholar]
- 22.Koh KK, Han SH, Quon MJ, et al. Beneficial effects of fenofibrate to improve endothelial dysfunction and raise adiponectin levels in patients with primary hypertriglyceridemia. Diabetes Care. 2005;28:1419–24. doi: 10.2337/diacare.28.6.1419. [DOI] [PubMed] [Google Scholar]
- 23.Koh KK, Quon MJ, Han SH, et al. Anti-inflammatory and metabolic effects of candesartan in hypertensive patients. Int J Cardiol. 2006;108:96–100. doi: 10.1016/j.ijcard.2005.07.040. [DOI] [PubMed] [Google Scholar]
- 24.Koh KK, Quon MJ, Lee SJ, et al. Efonidipine simultaneously improves blood pressure, endothelial function, and metabolic parameters in non-diabetic patients with hypertension. Diabetes Care. 2007;30:1605–7. doi: 10.2337/dc06-2267. [DOI] [PubMed] [Google Scholar]
- 25.Koh KK, Quon MJ, Han SH, et al. Additive beneficial effects of losartan combined with simvastatin in the treatment of hypercholesterolemic, hypertensive patients. Circulation. 2004;110:3687–92. doi: 10.1161/01.CIR.0000143085.86697.13. [DOI] [PubMed] [Google Scholar]
- 26.Correia ML, Haynes WG. Leptin, obesity and cardiovascular disease. Curr Opin Nephrol Hypertens. 2004;13:215–23. doi: 10.1097/00041552-200403000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Koh KK, Park SM, Quon MJ. Leptin and cardiovascular disease: response to therapeutic interventions. Circulation. 2008;117:3238–49. doi: 10.1161/CIRCULATIONAHA.107.741645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Skurk T, van Harmelen V, Blum WF, Hauner H. Angiotensin II promotes leptin production in cultured human fat cells by an ERK1/2-dependent pathway. Obes Res. 2005;13:969–73. doi: 10.1038/oby.2005.113. [DOI] [PubMed] [Google Scholar]
- 29.Koh KK, Quon MJ, Han SH, et al. Vascular and metabolic effects of combined therapy with ramipril and simvastatin in patients with type 2 diabetes. Hypertension. 2005;45:1088–93. doi: 10.1161/01.HYP.0000166722.91714.ba. [DOI] [PubMed] [Google Scholar]
- 30.Koh KK, Ahn JY, Han SH, et al. Pleiotropic effects of angiotensin II receptor blocker in hypertensive patients. J Am Coll Cardiol. 2003;42:905–10. doi: 10.1016/s0735-1097(03)00846-5. [DOI] [PubMed] [Google Scholar]
- 31.Katz A, Nambi SS, Mather K, et al. Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab. 2000;85:2402–10. doi: 10.1210/jcem.85.7.6661. [DOI] [PubMed] [Google Scholar]
- 32.Muniyappa R, Lee S, Chen H, Quon MJ. Current approaches for assessing insulin sensitivity and resistance in vivo: advantages, limitations, and appropriate usage. Am J Physiol Endocrinol Metab. 2008;294:e15–26. doi: 10.1152/ajpendo.00645.2007. [DOI] [PubMed] [Google Scholar]
- 33.Ouchi N, Kihara S, Funahashi T, et al. Reciprocal association of C-reactive protein with adiponectin in blood stream and adipose tissue. Circulation. 2003;107:671–4. doi: 10.1161/01.cir.0000055188.83694.b3. [DOI] [PubMed] [Google Scholar]
- 34.de Courten M, Zimmet P, Hodge A, et al. Hyperleptinaemia: the missing link in the metabolic syndrome? Diabet Med. 1997;14:200–8. doi: 10.1002/(SICI)1096-9136(199703)14:3<200::AID-DIA336>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 35.Takagi T, Matsuda M, Abe M, et al. Effect of pravastatin on the development of diabetes and adiponectin production. Atherosclerosis. 2007;196:114–21. doi: 10.1016/j.atherosclerosis.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 36.Koh KK, Han SH, Quon MJ. Inflammatory markers and the metabolic syndrome: insights from therapeutic interventions. J Am Coll Cardiol. 2005;46:1978–85. doi: 10.1016/j.jacc.2005.06.082. [DOI] [PubMed] [Google Scholar]
- 37.Mita T, Watada H, Kawamori R. Recently revealed pleiotropic effects of statins. Endocrinol Diabetol. 2004;18:527–33. [Google Scholar]
- 38.ter Avest E, Abbink EJ, de Graaf J, et al. Effect of rosuvastatin on insulin sensitivity in patients with familial combined hyperlipidaemia. Eur J Clin Invest. 2005;35:558–64. doi: 10.1111/j.1365-2362.2005.01549.x. [DOI] [PubMed] [Google Scholar]
- 39.Koh KK, Quon MJ, Han SH, et al. Simvastatin improves flow-mediated dilation, but reduces adiponectin levels and insulin sensitivity in hypercholesterolemic patients. Diabetes Care. 2008;31:776–82. doi: 10.2337/dc07-2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jula A, Marniemi J, Huupponen R, et al. Effects of diet and simvastatin on serum lipids, insulin, and antioxidants in hypercholesterolemic men: a randomized controlled trial. JAMA. 2002;287:598–605. doi: 10.1001/jama.287.5.598. [DOI] [PubMed] [Google Scholar]
- 41.Cohen B, Novick D, Rubinstein M. Modulation of insulin activities by leptin. Science. 1996;274:1185–8. doi: 10.1126/science.274.5290.1185. [DOI] [PubMed] [Google Scholar]
- 42.Hennige AM, Stefan N, Kapp K, et al. Leptin down-regulates insulin action through phosphorylation of serine-318 in insulin receptor substrate 1. FASEB J. 2006;20:1206–8. doi: 10.1096/fj.05-4635fje. [DOI] [PubMed] [Google Scholar]
- 43.Kleemann R, Verschuren L, de Rooij BJ, et al. Evidence for anti-inflammatory activity of statins and PPARalpha activators in human C-reactive protein transgenic mice in vivo and in cultured human hepatocytes in vitro. Blood. 2004;103:4188–94. doi: 10.1182/blood-2003-11-3791. [DOI] [PubMed] [Google Scholar]
- 44.Arnaud C, Burger F, Steffens S, et al. Statins reduce interleukin-6-induced C-reactive protein in human hepatocytes: new evidence for direct antiinflammatory effects of statins. Arterioscler Thromb Vasc Biol. 2005;25:1231–6. doi: 10.1161/01.ATV.0000163840.63685.0c. [DOI] [PubMed] [Google Scholar]
- 45.Koh KK, Son JW, Ahn JY, et al. Comparative effects of diet and statin on NO bioactivity and matrix metalloproteinases in hypercholesterolemic patients with coronary artery disease. Arterioscler Thromb Vasc Biol. 2002;22:e19–23. doi: 10.1161/01.atv.0000030997.02059.bb. [DOI] [PubMed] [Google Scholar]