Abstract
Aims
The aim of this study is to investigate whether protection with rubber or plastic gloves during post-mortem explantation of an implantable cardioverter defibrillator (ICD) offers enough protection for the explanting operator during a worst-case scenario (i.e. ICD shock).
Methods and results
We investigated the insulating properties of rubber and plastic gloves (double layer) within the first 60 min exposure (mimicking the maximum time of an explantation procedure) to saline (simulating the effects of body fluids on the gloves). For latex gloves, we measured an increase in voltage up to 68.1 V (P < 0.0001), for neoprene a maximum voltage of 5.3 V (P = 0.245), and for plastic a voltage of 2.3 V within the first hour. If the exposure time to fluid did not exceed 50 min, a double pair of intact gloves made of latex, neoprene, or plastic constituted such a large resistance that the resting voltage over the operating person would not exceed 50 V.
Conclusion
The use of intact medical gloves made of latex, neoprene, or plastic eliminates the potential electrical risk during explantation of an ICD. Two gloves on each hand offer sufficient protection. We will recommend the use of neoprene gloves.
Keywords: ICD, Explantation, Safety, Gloves, Resuscitation
Introduction
Pacemakers (PMs) and implantable cardioverter defibrillators (ICDs) must be removed post-mortem in a number of countries. Both PM and ICD batteries contain lithium which causes an environmental risk. In addition, the lithium battery may explode during temperature rise in crematory ovens, which will have economic consequences and cause a potential risk for the staff working near the oven.
Normal PMs deliver only a small amount of voltage, which is harmless to the explanting person. When an ICD gives a high-voltage therapy (shock), it delivers 30–40 J (∼800 V), which may—at least in theory—be dangerous to the explanting person [e.g. discomfort, difficulty in breathing, atrial fibrillation, burns, breathing arrest, or ventricular fibrillation (VF)].1
Implantable cardioverter defibrillator explantation brings up two problems—the loss of ICD data, which can clarify the cause of death, and the personal safety.2,3 Walley et al.1 described an episode where a pathologist experienced shocks from an ICD after it had been explanted from the deceased person. In addition, there are four case reports about resuscitation, where a rescuer not wearing gloves experienced a shock from the patient's ICD. Therefore, the safety issue is not hypothetical.1,4–7
Most recommendations regarding safety during post-mortem ICD explantation suggest that the PM/ICD is electronically inactivated by transcutaneous programming.1,8,9 This is also the standard recommendation from the ICD manufacturing companies. However, this is often not realistic as a device-specific programmer is not available or the manufacturer of the device is not known, and in these cases, it should be safe using either an ICD-magnet (or a PM/ICD-screwdriver to disconnect the electrode from the device) in combination with gloves, or only gloves. Until now, there are no data to support the latter recommendations.1,10 The mentioned recommendations concern only latex gloves, and the investigation is presented in a not reproducible manner, as the author did not describe the method.10
With the ICD-magnet placed over the ICD all antitachycardia therapies will be disabled and the device memory will not be filled with electrical noise during and after cutting the electrode. Therefore, details about an arrhythmia causing the death of the deceased are not overwritten and can be retrieved from the device. In practice, there is a risk of the ICD delivering a shock, if the magnet is not correctly placed all the time.1 Alternatively, a PM/ICD-screwdriver can also be used—thereby avoiding the need to cut the leads. Most general practitioners do not have an ICD-magnet or a PM/ICD-screwdriver, which might be a hindrance for removing an ICD from the body of a person who dies at home. In addition, the explanting person may not be aware of whether it is a PM or an ICD that is being explanted.
The aim of this study is to investigate whether protection with rubber or plastic gloves during post-mortem explantation of an ICD offers enough protection for the explanting operator during a worst-case scenario, i.e. when exposed to a shock therapy from an ICD during explantation.
Methods
We constructed a laboratory model, which simulated the situation where the explanting person was holding the ICD in one hand and was supposed to cut the still implanted ICD electrode with the other hand. The rubber or plastic gloves were the only protection of the operating person, since there was no ICD-magnet present in the model.
A closed circuit was established. The current was generated in the (patient's) ICD and passed through the electrode, via the scissors and a glove into the person's right hand, through the person, and from the person's left hand, via a glove, back to the ICD.
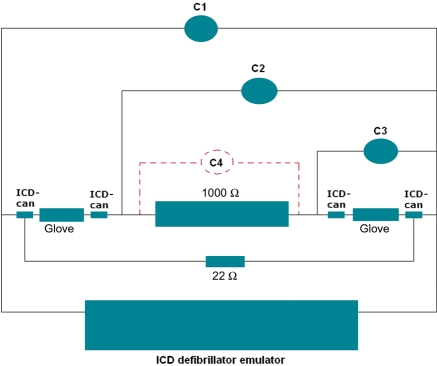
In the setup (Figure 1), we used an ICD defibrillator emulator by means of an implant support device (which correspond to a Medtronic model 5358, Minneapolis, MN, USA), which delivered a shock via two empty ICD-cans (mimicking the low impedance ICD electrodes). The ICD emulator delivers a bipolar pulse of maximal 750 V from a 120 µF capacitor using a fixed tilt of 65% (which correspond to a Medtronic model 7219, Minneapolis, MN, USA). The ICD-cans had only their shelves left, since they were emptied for all electronic parts. The empty ICD-cans were placed in a container (build in plastic glass) filled with saline [isotonic sodium chloride (NaCl, 9 g/L)]. The two gloves were placed in the container (resembling the dead patient's body impedance and allowing the defibrillator to generate realistic shocks)—one glove on each side close to an ICD-can connected to the defibrillator. The gloves were also filled with saline, and in each glove, we placed an empty ICD-can interconnected via a 1000 Ω resistor as substitute of the operators approximate body impedance (‘worst case value’). This means that four empty ICD-cans were used in the circuit.
Figure 1.
The experiment setup. The C's are voltage drop measurements on an oscilloscope used as a voltmeter. C1 was the voltage drop over the two gloves and the 1000 Ω resistance. C2 was the voltage drop over the 1000 Ω resistance and one of the gloves. C3 was the voltage drop over the aforementioned glove. C4 was the voltage drop over the 1000 Ω resistance and was calculated by subtracting C3 from C2. The 1000 Ω resistance represented the operating person. The 22 Ω resistance represented body fluids (e.g. sweat and blood). The shock was generated in the ICD defibrillator emulator.
One major issue in an experimental setup is the triggering of an ICD to deliver a shock. If the impedance is too high or too low, the ICD will not deliver a shock. The ICD can be seen as an ideal voltage source designed for impedances of ∼75 Ω. In our setup, the current could either pass through the gloves and the 1000 Ω resistance or through the saline (22 Ω). By means of the resistance of the saline, we were able to create a normal operating condition for the ICD to deliver a shock. The measurement on the oscilloscope (C1) verified that the ICD delivered a normal pulse of ∼750 V during discharge.
The measuring equipment consisted of an oscilloscope (LeCroy model Wave Surfer 424, New York, USA), which showed the curve for voltage drop over time.
The oscilloscope measured three different voltage drops: (i) the defibrillator voltage (C1 on Figures 1 and 2), (ii) the voltage in the right glove and the 1000 Ω resistance (C2 on Figures 1 and 2), and (iii) the voltage in the right glove (C3 on Figures 1 and 2). Finally, the oscilloscope calculated the voltage drop over the 1000 Ω resistance (operator) by subtracting C3 from C2 (C4 on Figure 1 and C2–C3 on Figure 2). The oscilloscope was set to measure voltage peak values (Figure 2). The oscilloscope used high-voltage probes with an attenuation factor of 0.01. Therefore, the values shown on the oscilloscope had to be multiplied by a factor 100 (Figure 2).
Figure 2.
Oscilloscope voltage curves [voltage (V) vs. time (ms)]. C1 (yellow line) is the voltage drop over the two gloves and the 1000 Ω resistance. C2 (pink line) is the voltage drop over the 1000 Ω resistance and one of the gloves. C3 (green line) is the voltage drop over the aforementioned glove. C2–C3 is the voltage drop over the 1000 Ω resistance and is calculated by subtracting C3 from C2. The voltage drop values on the oscilloscope had to be multiplied by a factor 100 (due to high-voltage probes).
The experiment had three variables. The first variable was the material, of which latex (Ansell, Conform+®, powder free, size M, Richmond, VIC, Australia), neoprene (GLECOglove, powder free, size L, Richmond, VIC, Australia), and plastic [Ansell, Ethiparat™, ethylene-vinyl-acetate (EVA), powder free, size M, Richmond, VIC, Australia] were used. The second variable was the number of layers of material. Only double layer (i.e. two pairs) was used. The third variable was the time in which the gloves had been exposed to saline, i.e. simulating the time of the procedure in which the operator is exposed to fluids (the operator sweat and the deceased's body fluids).
The current was generated by forcing the ICD defibrillator emulator to deliver a shock. Every 5 min, six measurements were performed (and a mean value was calculated). After 40 min, measurements were made every 10 min up to 1 h (mimicking the maximum time of an explantation procedure).
Finally, the isolating properties of a polyethylene house holding bag (used for freezing purposes) were investigated.
Statistical analysis
Due to the size of data and the nature of the results, a Gaussian distribution could not be expected. Voltage drop per time was compared using the Kruskal–Wallis non-parametrical comparison of mean rank. A P-value of <0.05 was considered to be statistically significant. All analyses were performed using the Statistical Package for Social Sciences (SPSS®) 15.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
The mean values of voltage drop over time during the experiment are shown in Table 1.
Table 1.
Voltage drop (V) values vs. time (min) in different material of gloves (double layers)
| Time (min) | Ethylene-Vinyl-Acetate gloves, mean (SD) | Neoprene gloves, mean (SD) | Latex gloves, mean (SD) | Polyethylene house-hold bag, mean (SD) |
|---|---|---|---|---|
| 0 | 2.27 V (1.87 V) | 1.90 V (2.06 V) | 3.70 V (2.92 V) | 0.00 V (0.00 V) |
| 5 | 4.98 V (3.12 V) | 3.25 V (2.74 V) | ||
| 10 | 2.83 V (2.21 V) | 4.02 V (3.33 V) | ||
| 15 | 2.05 V (2.30 V) | 2.32 V (3.03 V) | ||
| 20 | 4.98 V (1.89 V) | 5.15 V (1.60 V) | ||
| 25 | 5.27 V (2.91 V) | 5.47 V (4.37 V) | ||
| 30 | 2.72 V (2.24 V) | 9.55 V (3.35 V) | ||
| 35 | 3.85 V (2.53 V) | 10.28 V (4.66 V) | ||
| 40 | 2.28 V (2.67 V) | 15.50 V (4.44 V) | ||
| 50 | 4.02 V (3.48 V) | 31.73 V (2.47 V) | ||
| 60 | 4.72 V (4.64 V) | 68.08 V (4.70 V) |
The insulating properties of latex gloves are time-dependent with an exponential falling resistance over time. This time dependency is statistical significant with P < 0.0001. The insulating properties of neoprene gloves are not time-dependent within the first 60 min exposure to saline. For neoprene, there is no statistical significant difference between voltage drop values per time unit (P = 0.294).
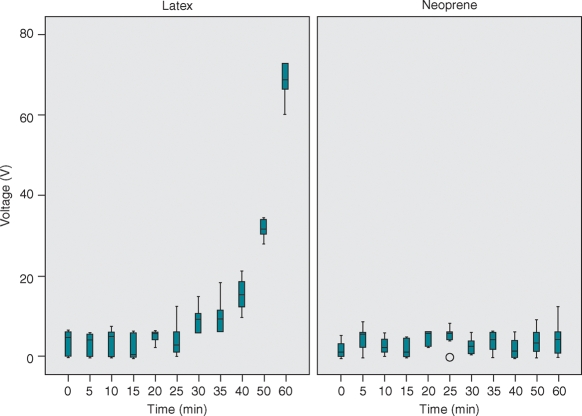
The main results of this study were the significant differences in the insulating properties of the gloves with respect to the time during which the gloves were exposed to saline. The insulating properties of latex gloves were time-dependent with an exponentially falling resistance over time (Figure 3). This time dependency was statistically significant (P < 0.0001). Within the first 50 min, <50 V (50 mA) passed through the latex gloves. The insulating properties of the neoprene gloves were not altered during the first 60 min exposure to saline (Figure 3), which was not statistically significant (P = 0.245). Within the first hour, <6 V (6 mA) passed through the neoprene gloves and <3 V (3 mA) passed through the ethylene gloves.
Figure 3.
Box-plot with voltage drop (V) vs. time (min) for latex gloves and for neoprene gloves. The horizontal bar represents the median, the box represents the inter-quartile range, and the whiskers the range. Outliers are shown with a circle. The insulating properties of latex gloves are time-dependent with an exponential falling resistance—increasing voltage—over time (P < 0.0001). The insulating properties of neoprene gloves were not time-dependent within the first 60 min exposure to saline (P = 0.245).
When we investigated a polyethylene house-holding bag with the properties 20 cm × 13.5 cm and 0.2 mm thick (folded), only one of six measurements was above zero (and showed 0.2 V).
The result from a typical experiment demonstrating the oscilloscope measurements is shown in Figure 2.
Discussion
The main results of this study were the significant differences in the insulating properties of the gloves with respect to the time in which the gloves were exposed to saline. Plastic and neoprene gloves had superior insulating properties when compared with latex gloves. However, within the first 25 min, the insulating properties were the same. Moreover, most explantations of ICDs would be expected to be performed within 15 min of total procedure time.
This experiment was built on a worst-case scenario: the delivery of a shock discharge during explant of the ICD directly in the hands of the operator. In real life, several unfavourable conditions should be present before an ICD is able to deliver a shock. First, the operator has to hold the ICD with one hand and the non-isolated part of the ICD electrode with the other hand. Secondly, the ICD has to interpret the ‘noise’—which emerges when the electrode is cut—as ventricular tachycardia (VT) or VF. When VT or VF is detected, the ICD starts charging its capacitor and is thereafter ready to deliver a shock. Thirdly, VT or VF has to be reconfirmed before the shock finally is delivered. This means that one has to create a closed circuit with the ICD and its electrode, trigger the ICD, and sustain the ‘noise’ until the shock is delivered. So, working with two hands may create a current path via the operator's body.
Another important issue is the resistance of the connections. In our setup, we used an empty ICD-can to defibrillate instead of an endocardial defibrillation lead. This will result in lower defibrillation impedance and, therefore, a shorter duration of the shock. However, the peak pulse voltage is not affected.
The contact side between the gloves and the scissors is a second issue regarding the resistance of the connections. There may be a high pressure between the gloves and the scissors at the side where the fingers grab the metal. This local contact is difficult to simulate because of large differences in pressure. However, the contact surface area will be small. Moreover, the resistance is a function of the surface area. Therefore, in our experimental setup, we used a significantly larger contact surface on both hands—in order to mimic a worst case.
In this experiment, we used a resistance of 1000 Ω, which corresponds to the resistance of an adult person. In our experiment, we measured a resistance of ∼1000 Ω from hand-to-hand in an adult person. The literature has reported similar values.11,12
In an unpublished pilot study, we tested one layer of latex, neoprene, and EVA gloves. From the pilot study, we could conclude that latex had the least isolating properties which changed very quickly over time when kept in saline for 24 h. Neoprene had better isolating properties, which also changed over time, when kept in saline for 24 h—however, the changes happened very slowly. Ethylene-vinyl-acetate did not change its isolating properties, when kept in saline for 24 h. For all the materials, there was a voltage drop >50 V when only one layer was used. Therefore, we only investigated double-layer gloves in this study.
Only one of six measurements showed a voltage value above zero when we investigated the polyethylene house-holding bag. This was probably due to a minimal capacitive coupling.
The concern is whether a single impulse of maximum 50 ms duration with a voltage drop of <50 V (50 mA) is dangerous? According to Lloyd et al.,13 there are no directly comparable safety standards. However, according to Parise,14 voltage drops <50 V in <5 s would be expected to be safe. In the study by Lloyd et al., the authors investigated rescuer–patient contact during external defibrillation with one layer of polyethylene gloves as the only protection against shock loads up to 360 J (biphasic). Without going into any discussion about the experimental setup, the authors found a voltage drop of a maximum of 14.1 V and a current of maximum 0.9 mA across the rescuer. None of the rescuers was able to sense the shock of maximum 360 J (biphasic).
Based on our results, we make the following recommendations. Ideally, the ICD should be interrogated and turned off by means of an ICD-programmer. If this is not possible, an ICD-magnet can be used in order to inactivate antitachycardia therapies. Alternatively, a PM/ICD-screwdriver can also be used—thereby avoiding the need to cut the leads. In case, the operator does not have an ICD-magnet or a PM/ICD-screwdriver, he or she can remove the ICD by wearing two pairs of intact neoprene gloves on each hand, and be protected from the exposure of potentially dangerous current in the case of a shock from the ICD. The ICD is dissected free and placed outside the dead body, where it is packed into two pairs of neoprene gloves. Now the ICD may detect high shock impedance and disable the shock. Finally, the cutting of the electrode is done as close to the ICD as possible starting with the pace-sense electrode. A quick cut should be made with a sharp pair of scissors (or wire-cutters) and—if possible—avoiding to contact the ICD system with two hands at the same time.
With the results of this study, we have gained new knowledge about the insulating properties from gloves against shock from an ICD. Until now, single layers of gloves most likely will be the routine during ICD explantation post-mortem. However, our study might change practice. The use of two layers of gloves eliminates the potential electrical risk regardless of the material of the gloves, even if the procedure time is prolonged substantial. Moreover, the use of two layers of gloves on each hand regarding operations on high-risk patients is well known from other medical fields (e.g. surgical procedures on HIV patients). Also, recently, Stockwell et al.7 described a case report about a rescuer who received a shock from a patient's ICD. The rescuer was wearing latex-free nitrile gloves as he was performing chest compressions during a cardiac arrest, and still he received a shock. The shock caused a nerve injury that lasted for more than half a year. Seen in the light of the increasing number of ICD implants, the case from Stockwell et al. will—unfortunately—not be the last reported unless resuscitation guidelines take our findings into consideration.
Conclusion
A guideline for safe ICD explantation post-mortem should deal with securing stored data, safety aspects of the explantation, and safe transport of the device to the read out institution. Data can be secured by using an ICD-programmer, an ICD-magnet, or a PM/ICD-screwdriver which is only possible in a hospital—unless the general practitioner has an ICD-magnet or PM/ICD-screwdriver as a part of his or her normal equipment.
A practical guideline shall be built on the use of simple equipment, because general practitioners must be able to perform an ICD explantation in a deceased person, who has died out of hospital.
Under the assumption that certified insulation gloves are not available, explantation of an ICD can be performed safely by using two pairs of intact rubber or plastic gloves and the transport can also be done safely by packing the ICD in a double rubber or plastic glove (or plastic house holding bag).15
Funding
This study was supported by Medtronic, Denmark, and Medtronic, Bakken Research Center, The Netherlands. J.H.S. receives research grants from the Danish National Research Foundation Centre for Cardiac Arrhythmia and the John and Birthe Meyer Foundation. Funding to pay the Open Access publication charges for this article was provided by Medtronic, Denmark.
Acknowledgements
We gratefully acknowledge helpful support by Per Christiansen (Medtronic, Denmark) and the assistance during testing from John Feron (Medtronic, Bakken Research Center, The Netherlands). We would also like to gratefully acknowledge the help from Arne Sørensen and Ole Knudsen (Department of Biomedical Engineering, Rigshospitalet, Denmark).
Conflict of interest: V.Z. works for Medtronic, Bakken Research Center, Maastricht, The Netherlands. S.P. and J.H.S. have received research grants from Medtronic Corporation. The first author reports no conflicts.
References
- 1.Walley VM, Bourke ME, Green M, Stinson WA, Veinot JP. Implantable cardioverter-defibrillators and the pathologist: comment and cautionary notes. J Forensic Sci. 1998;43:969–73. [PubMed] [Google Scholar]
- 2.Bernhardt JH. The establishment of frequency dependent limits for electric and magnetic fields and evaluation of indirect effects. Radiat Environ Biophys. 1988;27:1–27. doi: 10.1007/BF01211106. [DOI] [PubMed] [Google Scholar]
- 3.Kirkpatrick JN, Ghani SN, Burke MC, Knight BP. Postmortem interrogation and retrieval of implantable pacemakers and defibrillators: a survey of morticians and patients. J Cardiovasc Electrophysiol. 2007;18:478–82. doi: 10.1111/j.1540-8167.2007.00773.x. [DOI] [PubMed] [Google Scholar]
- 4.Clements PA. Hazards of performing chest compressions in collapsed patients with internal cardioverter defibrillators. Emerg Med J. 2003;20:379–80. doi: 10.1136/emj.20.4.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lechleuthner A. Electric shock to paramedic during cardiopulmonary resuscitation of patient with implanted cardiodefibrillator. Lancet. 1995;345:253. doi: 10.1016/s0140-6736(95)90247-3. [DOI] [PubMed] [Google Scholar]
- 6.Siniorakis E, Hardavella G, Arvanitakis S, Roulia G, Voutas P, Karidis C. Accidental shock to rescuer from an implantable cardioverter defibrillator. Resuscitation. 2009;80:293–4. doi: 10.1016/j.resuscitation.2008.10.032. [DOI] [PubMed] [Google Scholar]
- 7.Stockwell B, Bellis G, Morton G, Chung K, Merton WL, Andrews N, et al. Electrical injury during ‘hands on’ defibrillation—a potential risk of internal cardioverter defibrillators? Resuscitation. 2009;80:832–4. doi: 10.1016/j.resuscitation.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 8.Cardiac Society of Australia & New Zealand, the Australian Funeral Directors' Associaion and the manufactors (or their agents) of implantable cardioverter defibrillators, PCI (JR Management Pty Ltd), Medtronics, Intermedics (Sulzer), Teletronocs Pacing Systems. Guidelines for the prevention of accidental exposure to high voltage electric shocks during the preparation for burial of deceased persons with implantable cardioverter defibrillators (ICDS) 1999 [Google Scholar]
- 9.Medical Devices Agency UKSnS23. Safety notice SN 2002(35)—removal of implantable cardioverter defibrillators (ICDs) 2002 [Google Scholar]
- 10.Prahlow JA, Guileyardo JM, Barnard JJ. The implantable cardioverter-defibrillator. A potential hazard for autopsy pathologists. Arch Pathol Lab Med. 1997;121:1076–80. [PubMed] [Google Scholar]
- 11.Fish R. Electric shock, Part I: Physics and pathophysiology. J Emerg Med. 1993;11:309–12. doi: 10.1016/0736-4679(93)90051-8. [DOI] [PubMed] [Google Scholar]
- 12.Peters W, Kowallik P, Reisberg M, Meesmann M. Body surface potentials during discharge of the implantable cardioverter defibrillator. J Cardiovasc Electrophysiol. 1998;9:491–7. doi: 10.1111/j.1540-8167.1998.tb01841.x. [DOI] [PubMed] [Google Scholar]
- 13.Lloyd MS, Heeke B, Walter PF, Langberg JJ. Hands-on defibrillation: an analysis of electrical current flow through rescuers in direct contact with patients during biphasic external defibrillation. Circulation. 2008;117:2510–4. doi: 10.1161/CIRCULATIONAHA.107.763011. [DOI] [PubMed] [Google Scholar]
- 14.Parise G. A summary on the IEC protection against electric shock. IEEE Trans Ind Appl. 1998;34:911–22. [Google Scholar]
- 15.American Society for Testing and Materials. Standard Specification for Rubber Insulating Gloves. 2008. Publication D120-79a. [Google Scholar]