Abstract
Aims
Prior studies find that stress contributes to problem drinking while social support can buffer its effects. However, these studies are largely confined to middle class and general populations. We extend what is known by examining how the unique stressors and forms of social support experienced by women in poverty impact alcohol problems over a 4-year time period.
Design and Participants
This prospective study used GEE transition modeling and 4 annual waves of survey data from 392 American mothers receiving Temporary Assistance for Needy Families (TANF) in a large Northern California county.
Measurements
We examined the effects of neighborhood disorder, stressful life events and economic hardship on psychological distress and problem drinking over time, and whether social support moderated these relationships for women in poverty.
Findings
Neighborhood disorder and stressful life events significantly increased the risk for problem drinking, largely through their effect on psychological distress. We found little evidence, however, that social support buffers poor women from the effects of these stressors.
Conclusions
Women in poverty are exposed to severe, chronic stressors within their communities and immediate social networks which increase vulnerability to psychological distress and problem drinking. The finding that social support does not buffer stress among these women may reflect their high level of exposure to stressors, as well as the hardships and scarce resources within their networks. If the “private safety net” of the social network fails to provide a strong buffer, more effective environmental interventions that reduce exposure to stressors may be needed to prevent alcohol problems in poor women’s lives.
Keywords: Poverty, women, alcohol problems, stress, social support
There is a long tradition of research addressing the role of stress in alcohol problems. On the whole, researchers report significant associations between stress and alcohol use and problems, and that this relationship is partly influenced by social resources for managing stress [1–4]. While some studies find that moderate drinking is associated with reduced stress [5–7], excessive drinking and alcohol problems have been linked to elevated stress—especially chronic stress—and to psychological distress [1, 8–10]. Social support, a resource widely studied in relation to stress and health, has been shown to play a role in problem drinking through its direct associations with anxiety, depression and distress [11, 12]. It has also been found to promote positive coping responses to stress [13], and to improve treatment retention and recovery from alcohol problems [14–16]. Still other studies document a stress-buffering role for social support [17] —that the impact of stressors on alcohol consumption can be reduced in the presence of high levels of support [2, 4]—although this finding is not uniformly born out in the literature (see: [9, 18]).
Most research on stress and alcohol is conducted in middle class and general population samples. Findings from the literature may not, therefore, generalize to populations in poverty where the patterning of alcohol problems, stressors and social support differs from the population at large [19–21]. Those studies that do examine poor populations find little evidence that social support reduces substance abuse, and do not address the potential stress-buffering role of social support [22–24]. In this study, we propose and empirically test a model of stress, social support and problem drinking that reflects the distinctive lives of women in poverty. This work is motivated by the growing burden of alcohol problems in economically disadvantaged groups [25, 26], growing public policy concerns about addiction in welfare populations [27, 28], and recent developments in social epidemiology that focus attention on neighborhood-level and social network conditions influencing risk and health [29, 30].
Towards a Model of Stress and Alcohol Problems for Women in Poverty
The tendency towards middle-class cultural bias in standard models of stress and alcohol problems raises questions about their applicability to populations of low-income women. Life in poverty brings with it several unique sources of stress, most obviously, the chronic burdens associated with economic deprivation [31, 32]. Other stressors originate in the conditions of daily life in impoverished, high-crime areas, which take a well-documented toll on mental and physical health [33–35]. As shown in observational studies, the lives of poor women tend to be punctuated by severe disruptions and personal crises, such as threats from bill collectors, loss of housing, family fragmentation, incarceration and violent victimization [36, 37]. A plausible model of stress and alcohol problems in poor women’s lives should therefore incorporate measures of severe financial hardship, the kinds of stressful events that arise during everyday life in poverty, and the stressful conditions that typify disadvantaged neighborhoods.
Social resources for managing stress may also differ for women in poverty compared to the population at large. Poverty researchers have long noted the unique strength and interdependencies in the social networks of low-income women. Carol Stack’s All Our Kin [38], first illustrated how resource sharing within kinship networks proved essential for the daily survival of low-income, African-American families. More recently, Edin and Lein [31] demonstrated that most welfare mothers are able to make ends meet only by falling back on the “private safety net” of family members and friends. Recent inquiries have, however, questioned the extent to which social support networks actually mitigate stress for poor women. Ecological studies document a gradual weakening of neighborly ties in poor neighborhoods, as residents withdraw from a community life increasingly strained by concentrated poverty, crime, and drug addiction [39, 40]. Moreover, recent ethnographic studies tend to “de-romanticize” the ideal of the family as a social safety net. Rather, they suggest that the resource-deprived networks of poor women might actually serve as “conduits of stress” [41] by placing additional demands on these women’s already-meager resources [42]. What may be most relevant here is the balance of reciprocity within low-income women’s exchange relationships. Imbalanced exchanges characterized by excessive network demands can potentially increase stress, whereas a more favorable balance may have the opposite effect [43].
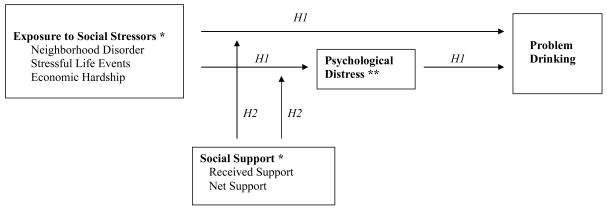
In this study, we propose a “stress process model” [44] in which psychological distress and problem drinking are specified as a function of exposure to severe economic hardship, stressful life events and disadvantaged, unsafe neighborhoods (see Figure 1). A stress process model underscores the need to measure both the presence of stressors, as well as the stress that results. In the past, researchers have only often assessed the direct effects of stressors upon alcohol use, tacitly assuming that stressors are a viable proxy for the actual experience of stress—an unsafe assumption according to some [45, 46]. Here we model both the direct effects of stressors on problem drinking, and the intervening role of psychological distress in this relationship. The proposed model also investigates the potential stress-buffering role of social support. In keeping with recent arguments concerning reciprocity in poor women’s social networks, we examine not only the social support received from others but also net support, that is, the level of support received net of the support given to others. The following hypotheses guide our study of women in poverty: (1) Greater exposure to poverty-related social stressors will increase the likelihood of problem drinking due, in part, to increased psychological distress; and (2) Higher levels of social support will buffer the effects of social stressors on psychological distress and problem drinking.
Figure 1. Conceptual Model of Stress, Social Support and Problem Drinking among Women in Poverty.
*Time-varying predictors of psychological distress and problem drinking. ** Time-varying predictor of problem drinking.
Control variables include race/ethnicity, education, marital status, number of children, weekly drug use, outcomes at the prior time point and wave of interview.
METHODS
Study Sample
The current study utilizes data from the Welfare Client Longitudinal Study (WCLS), which followed over 4 years a representative sample of poor women with children receiving Temporary Aid to Needy Families (TANF), the predominant form of welfare in America. While the WCLS is representative of only a segment of poor women, namely those with children receiving government aid, it may provide better sample coverage of poor households than general population surveys which often under-represent the poor and people with substance abuse problems [47, 48]. The study was conducted in a metropolitan county in Northern California selected for its demographic and geographic heterogeneity. The sample bears a close resemblance to the U.S. TANF caseload (see: [49]). It is ethnically diverse (31% white, 39% African American, 17% Latina, and 13% multi-ethnic or other), has a mean age of 29 years, and limited education (28% do not have a high school diploma). More than two-thirds of the women are in single-parent families (75%) and the majority (68%) tend one or two children in the home.
Recruitment and Data Collection Procedures
TANF applicants were recruited in 2001 from the rosters of all welfare offices in the study site. Systematic sampling was used in which every “nth” welfare applicant was selected for participation. Informed consent was obtained and persons assured that study participation was independent of receiving public assistance, and that all data were protected by a federal Certificate of Confidentiality from the US government. Interviews were conducted in English or Spanish using a standardized questionnaire, and lasted one hour. Approximately 85% of all eligible welfare applicants were interviewed, with non-response mainly due to the inability to locate an individual after the initial welfare screening process.
Due to the expense of following low-income populations, we over-sampled TANF recipients who reported either problem drinking or weekly drug use (167 persons, or 24% of TANF recipients, all of whom were selected for follow-up). Among the remaining TANF recipients, a random sample was drawn to yield a total of 455 study participants, among whom 419 were female. Women abstaining from alcohol throughout the entire study period were excluded from this analysis (27 participants, leaving 392 cases for analysis).
An intensive, community-based tracking approach was used to maintain contact with this sample. To minimize fieldwork time and costs, and inconvenience to study participants, follow-up interviews were conducted by telephone whenever possible (an estimated 80% of the sample). Those without phones or who could not otherwise be reached were interviewed in-person in their homes, jails, prisons, treatment facilities, homeless shelters, and parks. At the 4th year of follow-up, 81% of the sample was located and re-interviewed, and over 90% had completed at least one post-baseline interview. The overall refusal rate was below 2% and the mortality rate was 2%. A published non-response simulation study demonstrated that the intensive tracking efforts taken with the hard-to-reach, who tended to be poorer and substance dependent, contributed nearly 20 percent to the annual response rate and that published results would have been biased in the absence of this intensive tracking effort [50].
Key Measures
The primary dependent variable in this analysis was problem drinking, a measure that has been widely used in epidemiologic research [51, 52]. Problem drinking was defined as a drinking pattern during the past year that meets at least two of the following three conditions: 1) consumption of five or more drinks in a sitting at least once a month, 2) one or more alcohol dependence symptoms, and 3) one or more tangible consequences of drinking, such as problems with police, at work, or with family members. This multidimensional measure correlates well with clinical measures of substance abuse, and is consistent with many previous studies of alcohol problems among women and welfare populations [53–57]. Psychological distress was incorporated as a more proximal dependent measure of distress. Here, we used the mean score on the Global Severity Index (GSI) derived from the 53-item Brief Symptom Inventory, which has well-established validity and reliability in clinical and general populations [58, 59] (alpha=0.96).
Three different types of social stressors served as key independent variables. Economic hardship was measured in terms of the average income per family member for each year of the study. This was computed by dividing the respondent’s household income by the number of immediate family members in the household. A log transformation reduced skewness.
Neighborhood disorder was measured by averaging across eight items on the perceived frequency of the following neighborhood occurrences: (1) drug arrests or busts, (2) people getting mugged, (3) people selling drugs, (4) drive-by shootings, (5) people sleeping in public places at night, (6) homes getting robbed, (7) arrests for public drunkenness, and (8) teenagers loitering during school hours. Response categories included “never” (0), “sometimes” (1), and “frequently” (2) (alpha=0.87). This measure was developed specifically for this project with careful pre-testing, and was informed by the poverty literature which supports the validity of self-report measures of neighborhood disorder [60, 61].
To assess stressful life events, we used a seven-item index of stressful events adapted from the University of Michigan’s Women’s Employment Study [62] for use in studies of women in poverty. Respondents were asked whether any of the following events had occurred to them in the past 12 months: (1) a relative or close friend was in jail, (2) people living with them who they wish weren’t there, (3) someone close to them died or was killed, (4) hassles by bill collectors, (5) a life threatening accident, (6) a fire, flood, or natural disaster, and (7) a family member was seriously ill or injured. For each item, no was coded as “0” and yes as “1” to give a score ranging from 0 to 7.
Given the lack of measures capturing the reciprocity in poor women’s exchange relationships, we developed measures of social support based upon the literature and our own prior qualitative studies of poor women [37, 63]. Respondents were asked a parallel series of eight questions on the frequency of receiving and giving support to family, friends, and neighbors, including: emotional support (help when upset, depressed or needed to talk), practical support (care when sick, help with food or clothing, help with leads for job seeking, running errands, watching children, and providing transportation), and financial support (help with money or a loan to get by). Responses ranged from never (0) to frequently (2) (alphas = 0.81 and 0.77 for receiving and giving help, respectively). Social support received was the summed score, where emotional, practical and financial help were weighted equally to account for the uneven number of items for each type of support (range=0 to 6). Net social support was derived by first subtracting support given from support received on an item-by-item basis, then computing a total, weighted, net score (range= −6 to +6). A negative value on the net support measure indicates that a respondent perceived that she was more frequently giving, than receiving, support.
Weekly drug use was based upon the self-reported use of illicit drugs or nonprescribed use of prescription drugs within the past 12 months. This measure was used as an oversample selection criterion and as a control variable in all models.
Data Analysis
Statistical weights were developed to adjust for design differences, including the intentional oversampling of substance abusers and non-response. Univariate and bivariate analyses were conducted using SPSS 12.0 (SPSS Inc. Chicago, IL) and multivariate models were run using generalized estimating equations (GEE) implemented in STATA 9 [64].
To assess longitudinal relationships, we employed transition models [65] which predict changes from one year to the next in problem drinking and psychological distress. Transition modeling is an ideal approach for our purposes because it recognizes that problem drinking at time t may be highly related to problem drinking at time t-1, and treats the latter as an additional explanatory variable. Transition models allow us to quantify, for instance, the increased risk of problem drinking per one-unit increase in a given independent variable (e.g., stressful life events), among women who were not problem drinkers during the prior year (see: [65, p.130]. The models also adjust for the correlation of errors in prediction across time.
To test the first hypothesis pertaining to the effects of stressors, we specified transition models where problem drinking and psychological distress were modeled as conditional upon social stressors, control variables (race/ethnicity, education, marital status, number of children living at home, wave of interview and weekly drug use), and the outcome variables at the prior time point. To test the second hypothesis regarding the stress-buffering effects of social support, we specified a series of interaction models to assess whether social support moderates the relationships between social stressors and psychological distress and problem drinking over time. Throughout all analyses, social stressors, psychological distress, and problem drinking were allowed to vary over time, along with covariates such as number of children in the home and weekly drug use. Other demographic covariates were measured at baseline and modeled as time-invariant.
RESULTS
Social Stressors and Problem Drinking among Poor Women
Preliminary analysis of the baseline data underscored the ubiquity of social stressors in poor women’s lives (data not shown). Approximately three-fourths (74%) of the women lived in neighborhoods characterized by disorder, most commonly evidenced by teenage loitering during school hours, drug-related arrests, or people selling drugs. Many (69%) reported at least two stressful life events in the past year alone, including the incarceration of a relative or friend, and the death or killing of someone close to them (reported by 53% and 38%, respectively). Half of the women had household incomes below $15,000, which is less than one-fifth of the county’s median household income [66]. Nearly one-third (30%) reported clinically significant levels of psychological distress, and 7% were classified as problem drinkers. In this sample of very poor women, we found no racial/ethnic differences in exposure to social stressors, or in rates of distress and problem drinking. While both neighborhood disorder and stressful events were positively correlated with psychological distress and problem drinking (see Table 1), economic hardship was not, possibly reflecting the constrained income distribution in this sample of very poor women.
Table 1.
Intercorrelations and Descriptive Statistics for Key Variables at Baseline (N=392)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | M | SD |
|---|---|---|---|---|---|---|---|---|---|
| 1. Problem drinking | 1.0 | 0.07 | .26 | ||||||
| 2. Psychological distress | .10* | 1.0 | 0.63 | .56 | |||||
| 3. Neighborhood disorder | .11* | .20*** | 1.0 | 0.49 | .50 | ||||
| 4. Stressful life events | .11* | .35*** | .28*** | 1.0 | 2.15 | 1.36 | |||
| 5. Income (logged) | −.04 | .04 | −.11* | .02 | 1.0 | 8.44 | 1.20 | ||
| 6. Received Support | −.03 | −.11* | −.13* | −.05 | .07 | 1.0 | 3.44 | 1.52 | |
| 7. Net Support | −.04 | −.12* | −.16** | −.15** | .03 | .68*** | 1.0 | 0.03 | 1.78 |
p<.05,
p<.01,
p<.001
Unweighted N, results are weighted.
Table 2 maps year-to-year changes in the women’s exposure to stressors, psychological distress, and problem drinking. From one time point to the next, on average 32% were exposed to greater neighborhood disorder, 15% reported more stressful life events, 43% experienced more economic hardship, and 19% reported greater distress. On average, 5 to 6% of non-problem drinkers became problem drinkers in the following year.
Table 2.
Transitions in Exposure to Stressors, Psychological Distress and Problem Drinking across Time
| Time 1 |
Time 2 % High |
Time 2 |
Time 3 % High |
Time 3 |
Time 4 % High |
Time 4 |
|
|---|---|---|---|---|---|---|---|
| Neighborhood disorder | High (n=212) | 70.8 | High (n=195) | 73.0 | High (n=197) | 75.7 | High (n=180) |
| Low (n=180) | 37.8 | Low (n=149) | 34.5 | Low (n=140) | 23.7 | Low (n=142) | |
| Stressful life events | High (n=179) | 40.8 | High (n= 103) | 49.4 | High (n=87) | 47.4 | High (n=88) |
| Low (n= 212) | 14.6 | Low (n= 241) | 14.2 | Low (n= 250) | 15.2 | Low (n= 234) | |
| Economic hardship | High (n=204) | 84.6 | High (n=235) | 73.6 | High (n=224) | 78.9 | High (n=209) |
| Low (n=184) | 51.8 | Low (n=104) | 46.1 | Low (n=112) | 31.7 | Low (n=109) | |
| Psychological distress | High (n=212) | 55.3 | High (n=141) | 63.9 | High (n=135) | 67.0 | High (n=127) |
| Low (n=180) | 19.5 | Low (n=203) | 20.8 | Low (n=202) | 16.8 | Low (n=194) | |
| % Case | % Case | % Case | |||||
| Problem drinker | Case (n=69) | 47.8 | Case (n=44) | 42.3 | Case (n=36) | 36.0 | Case (n=39) |
| Not case(n=323) | 5.3 | Not case (n=300) | 5.4 | Not case (n=301) | 6.3 | Not case (n=283) | |
Unweighted n’s, results are weighted. “High” exposure to neighborhood disorder, stressful life events, and psychological distress is defined as a score greater than the baseline median for that variable. Severe or “high” economic hardship is defined as an income below the baseline median income per family member.
Table 3 presents the results of transition models that predict year-to-year changes in problem drinking and levels of psychological distress. On the whole, the results substantially support the hypothesis that social stressors increase the risk of problem drinking among women in poverty (Model 1). Even after adjusting for weekly drug use and other covariates, each additional stressful life event corresponded to a 27% increase in the odds of becoming a problem drinker from one year to the next. Moreover, a one-unit increase in the neighborhood disorder score – for example, from never observing any indicators of neighborhood disorder, to observing all indicators “sometimes” – increased the odds of a transition to problem drinking by 94%. This effectively doubles the odds that a low-income woman becomes a problem drinker.
Table 3.
Effects of Social Stressors on Changes in Psychological Distress and Problem Drinking among Women in Poverty (N=392)
| Predictors | Problem Drinking Model 1 | Psychological Distress Model 2 | Problem Drinking Model 3 | |||
|---|---|---|---|---|---|---|
| AOR | 95% CI | Coeff. | SE | AOR | 95% CI | |
| At time, T-1 | ||||||
| Psychological distress | -- | -- | 0.632*** | (0.033) | -- | -- |
| Problem drinking | 4.68*** | (2.09, 10.5) | -- | -- | 6.28*** | (3.04,13.0) |
| At time, T | ||||||
| Neighborhood disorder | 1.94** | (1.24, 3.03) | 0.130*** | (0.030) | 1.55 | (0.98, 2.45) |
| Stressful life events | 1.27** | (1.08, 1.50) | 0.065*** | (0.013) | 1.13 | (0.95,1.35) |
| Income, logged | 0.99 | (0.76, 1.29) | −0.028* | (0.014) | 1.04 | (0.81,1.33) |
| Psychological distress | -- | -- | -- | -- | 2.69*** | (1.77,4.08) |
p< .05,
p < .001
Unweighted N, results are weighted. Adjusted odds ratios with 95% confidence intervals are shown for dichotomized outcomes, unstandardized coefficients with standard errors are shown for a continuous outcome. Control variables not shown above include fixed covariates (race/ethnicity, education, marital status) and time-varying covariates (number of children at home, weekly drug use, wave of interview). The percent reduction in the AOR may be computed by (AOR model 1 – AOR model 3)/(AOR model 1 – 1) [71].
The results further show that neighborhood disorder and stressful events are strongly predictive of increases in psychological distress (Model 2), and suggest that distress plays an important role in their relationship to problem drinking. This is seen in Model 3, where the addition of distress reduced the odds ratios for neighborhood disorder and stressful life events by 42% and 52% respectively, to nonsignificance (p=.049 and p=.053, respectively, using Sobel’s one-sided test of mediation). Economic hardship was also predictive of increases in psychological distress, which, in turn, nearly triples the risk of becoming a problem drinker. None of the demographic covariates (race/ethnicity, education, marital status, and number of children) predicted changes in either problem drinking or levels of distress.
The Stress-Buffering Role of Social Support among Low-Income Women
In keeping with the poverty literature, many women in the study were deeply engaged in resource exchanges with family, friends and neighbors. Virtually all reported receiving (99%) and giving (98%) help at least occasionally (data not shown). Emotional support and help when sick were the two kinds of aid exchanged the most, with roughly half reporting that they frequently gave, and received, such help. Practical support, such as the sharing of food and clothing, child care, job advice, help with errands, and transportation, was less commonly exchanged. Roughly one-fourth to one-third of the women reported frequently receiving and providing such help. Financial support was the most rarely mentioned, with 25% frequently receiving such help and 16% frequently giving it. With regard to reciprocity, most women were in relatively balanced exchange relationships (36%) or received more help than they provided to others (33%). However, roughly one-third (31%) netted out negatively, that is, they received less support than they gave.
Social support was inversely associated with exposure to social stressors, in some instances, and with psychological distress (Table 1). Living in a more disadvantaged neighborhood was associated with receiving less support (F=8.59, p<.01), and experiencing more stressful life events was associated with giving more support to others (F=3.9, p<.05) (data not shown). This is consistent with the idea that poor women’s social networks can, in and of themselves, be a source of stress; for example, when impoverished family members and friends require help with housing, illness or injury.
In Table 4 we present the results of transition analyses which replicate the models in Table 3, but with the addition of interaction terms that assess the stress-buffering hypothesis. If the social support networks of women in poverty can buffer the harmful effects of neighborhood, eventful, and economic stressors, then we would expect the impact of stressors on psychological distress and problem drinking to be weaker at higher levels of social support. As seen in the table, none of the interaction terms were significant. Levels of received support did not appear to alter the relationship between stressors and psychological distress (shown in the upper half of the table), nor the relationship between stressors and problem drinking (shown in the lower half of table). In addition, although our earlier, correlational analyses suggested a protective, main effect for received support on psychological distress, this effect was no longer apparent in the multivariate model that controlled for other factors (see Model 1). Examination of the buffering and main effects of net social support yielded similarly null findings (see right hand side of table).
Table 4.
Effects of Perceived Social Support on Changes in Psychological Distress and Problem Drinking among Women in Poverty (N=392)
| Effect of Received Support on Distress unstandardized coeff. (SE) | Effect of Net Support on Distress unstandardized coeff. (SE) | |||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 | |
| Main Effects | ||||||||
| Received Support | −.016 (.010) | −.015 (.010) | −.017 (.011) | −.016 (.010) | ||||
| Net Support | −.010 (.009) | −.010 (.009) | −.010 (.009) | −.011 (.009) | ||||
| Interaction Effects | ||||||||
| Neighborhood disorder by social support | −.013 (.019) | −.021 (.018) | ||||||
| Stressful life events by social support | −.005 (.009) | .000 (.007) | ||||||
| Income by social support | .014 (.012) | .020 (.012) | ||||||
| Effect of Received Support on Problem Drinking AOR (95% CI) | Effect of Net Support on Problem Drinking AOR (95% CI) | |||||||
| Main Effects | ||||||||
| Received Support | 0.96 (0.79,1.16) | 0.92 (0.74,1.13) | 0.97 (0.80,1.17) | 0.95 (0.78,1.16) | ||||
| Net Support | 0.96 (0.82,1.12) | 0.95 (0.80,1.11) | 0.98 (0.83,1.16) | 0.96 (0.82,1.11) | ||||
| Moderating Effects | ||||||||
| Neighborhood disorder by social support | 1.17 (0.85,1.60) | 1.10 (0.82,1.46) | ||||||
| Stressful life events by social support | 0.97 (0.85,1.10) | 0.96 (0.89,1.05) | ||||||
| Income by Social support | 0.94 (0.80,1.09) | 0.94 (0.81,1.08) | ||||||
Unweighted N, results are weighted. All models adjust for outcomes at the prior time point, neighborhood disorder, stressful life events, income, race/ethnicity, education, marital status, number of children at home, weekly drug use and wave of interview. Models predicting problem drinking also adjust for psychological distress.
DISCUSSION
This study has sought to better understand how social stressors linked to the conditions of poverty contribute to alcohol problems in low-income women, and whether the stress-buffering role of social support pertains to this population. From the standpoint of public policy, these are timely issues given the growing international awareness that economic disparities give rise to disparities in health, as well as growing challenges to welfare entitlement programs in some developed countries [67, 68]. From the standpoint of theory, these are also important concerns. Our findings on stress buffering add fodder to current debates about the potential for social support to have both beneficial and detrimental effects on economic mobility and individual well-being among the poor [41, 42]. As noted at the outset, general population research has documented a positive association between exposure to stressors and alcohol problems, and has provided some evidence that social support helps to buffer the effects of stressors on alcohol problems. By contrast, the very limited research conducted in low-income populations suggests that social support may provide little protective effect against substance abuse. In fact, some researchers argue that the social networks of poor women can themselves be “conduits of stress” rather than resources for buffering stress.
For those concerned about the problems of stress, poverty and alcohol-related health disparities, our results speak to the value of utilizing measures that capture the particular sources of stress that arise from the conditions of poverty. Our approach emphasized neighborhood, eventful and economic stressors often faced by low-income women and those close to them. Our empirical analyses demonstrate not only the ubiquity of these stressors in welfare mothers’ lives, but also their important role in the risk of developing a drinking problem. All three social stressors—economic deprivation, stressful life events and especially neighborhood disorder—significantly contributed to psychological distress over time, which, in turn, strongly influenced the likelihood of developing alcohol problems. Let us emphasize that these effects were observed using a conservative statistical approach that took into account an individual’s prior level, or history, of problem drinking, which is by far the strongest predictor of later problem drinking. Additionally, the models controlled for heavy drug use and other predictors of alcohol problems. This conservative analytic approach lends credence to our finding that social stressors linked to poverty play a significant role in the development of problem drinking in low-income women, and extends prior research documenting the adverse effects of such stressors on alcohol and drug use [69,70].
In light of the strong interconnection between stressful living conditions and problem drinking, it becomes all the more important to consider factors that might mitigate stress, such as social support. Poverty researchers, particularly ethnographers studying the lives of poor women up-close, have frequently commented on the strength of social ties and reciprocity in their social networks. Following this, we hypothesized that social support would buffer poor women from the stresses of poverty, thereby reducing the likelihood of developing a drinking problem. Our longitudinal analyses, however, failed to find evidence of stress buffering. Our extra efforts to correctly measure social network support, and in multiple ways, supports the negation of the stress-buffering hypothesis in this population. These findings thus add a cautionary note to portrayals of the poor that romanticize the strength of their social networks.
STUDY LIMITATIONS
Although these data are particularly well-suited to the aims and hypotheses of this study, several important limitations should be noted. First, this study is restricted to women who received federal cash-aid in a single county, which limits the generalizability of results. Although the sample is demographically similar to other TANF populations [71], by virtue of this, it is necessarily confined to poor women with children, the majority of whom are single parents. While single-parent families predominate among American families in poverty [72], other analyses, including our own, have shown that poor women without children are significantly more likely to suffer exposure to social stressors and alcohol problems [57, 73, 74].
Other limitations stem from our reliance on self-report measures, particularly of neighborhood disorder. Debate remains as to whether respondent or researcher assessments are best for reducing reporting error [75], although at least one study has found that resident and researcher assessments perform comparably [61]. In the absence of standardized measures of social support and reciprocity developed for this population, we developed our own. Although we performed careful pre-testing and analysis of scale properties, our measures of social support have not been tested elsewhere.
Finally, this study does not explore the possibility of reciprocal effects. It is plausible that problem drinking could result in greater exposure to social stressors and distress and less social support, which, in turn, could reinforce or exacerbate problem drinking. Our conceptual framework thus presents a simplification of potential longitudinal effects. Future studies should consider these additional pathways.
IMPLICATIONS
Our findings have implications for both research and public policy. With respects to future research, our largely null findings regarding the stress-buffering hypothesis raise more questions than they can answer. In particular, they force us to ask why the social networks of women in poverty fail to buffer stress when they appear to do so in the general population. On the one hand, we can speculate that the stressors to which these women are exposed are more severe and chronic than those experienced in the larger population. The chronicity and intensity of the stressors arising from poverty might simply dwarf any mitigating effects that social support can provide (for a similar argument, see: [23]). Notably, the wider literature suggests a link between exposure to chronic stressors and lower levels of social support. Thus Lepore [76] found that while social support buffered the effects of a relatively short-term stressor, prolonged exposure to the same stressor was accompanied by an attenuation of this protective effect.
On the other hand, these findings may reflect differences in the social networks of low-income women. As noted, the social networks of poor women may themselves be a source of stress, and thus might actually increase, rather than mitigate, stress and problem drinking among poor women. It may also be the case that impoverished social networks simply have very little support available to adequately buffer stress [2, 77]. Thus, researchers have argued that a poor woman’s chances to better her situation by finding a well-paying job and safer neighborhood may depend upon the socioeconomic heterogeneity within her network, particularly her ties to people with far greater resources and access to opportunities [42, 78].
From the perspective of social policy, our findings suggest that the natural flow of resources and support within poor women’s social networks—the so-called “private safety net” – cannot be counted upon to buffer poor women from the effects of poverty-related stressors. These limitations in the private safety net suggest the need for a stronger public safety net, namely, government programs designed to mitigate the stresses of poverty and to address socioeconomic disparities in alcohol-related problems. Alegría and colleagues [79] note that income support programs that target high-poverty communities with tax credits, incremental increases in the minimum wage, and housing assistance are not necessarily designed to improve health. Even so, these economic policies have profound spillover effects that reduce the burden of health problems and mental illness at the population level. A similar case can be made for community mobilization efforts to reduce crime and violence at the neighborhood level, which tend to have spillover effects on “drug saturation” in low-income communities [80]. Individual-level interventions that help poor women to develop coping strategies, and that directly prevent and treat alcohol problems may be needed as well. However, given the ubiquity of stressors and the lack of effective support resources observed in this study, one may question their long-term effectiveness if the underlying sources of poverty-related stress remain unchecked.
Acknowledgments
This study was supported by grants from the US National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism P50 AA05595, R01 AA13136, R01 AA0149918 and R21AA015397. We thank the study participants and welfare agencies that have so graciously given of their time to make this research possible, the fieldwork team at the Center for Applied Local Research in Richmond, CA, Kenny Garron, and members of the Welfare Client Longitudinal Study Team. We also thank the anonymous reviewers for their thoughtful comments.
References
- 1.Moos RH, Fenn CB, Billings AG, Moos BS. Assessing life stressors and social resources: applications to alcoholic patients . J Subst Abuse. 1989;1:135–52. doi: 10.1016/s0899-3289(88)80017-8. [DOI] [PubMed] [Google Scholar]
- 2.Johnson KA, Jennison KM. Stressful loss and the buffering effect of social support on drinking behavior among African-Americans: results of a national survey. J Alcohol Drug Educ. 1994;39:1–24. [Google Scholar]
- 3.McCreary DR, Sadava SW. Stress, alcohol use and alcohol-related problems: the influence of negative and positive affect in two cohorts of young adults . J Stud Alcohol. 2000;61:466–74. doi: 10.15288/jsa.2000.61.466. [DOI] [PubMed] [Google Scholar]
- 4.Peirce RS, Frone MR, Russell M, Cooper ML. Financial stress, social support, and alcohol involvement: a longitudinal test of the buffering hypothesis in a general population survey. Health Psychol. 1996;15:38–47. doi: 10.1037//0278-6133.15.1.38. [DOI] [PubMed] [Google Scholar]
- 5.Baum-Baicker C. Psychological benefits of moderate alcohol consumption: a review of the literature. Drug Alcohol Depend. 1985;15:305–22. doi: 10.1016/0376-8716(85)90008-0. [DOI] [PubMed] [Google Scholar]
- 6.Brennan PL, Schutte KK, Moos RH. Reciprocal relations between stressors and drinking behavior: a three-wave panel study of late middle-aged and older women and men. Addiction. 1999;94:737–49. doi: 10.1046/j.1360-0443.1999.94573712.x. [DOI] [PubMed] [Google Scholar]
- 7.Peele S, Brodsky A. Exploring psychological benefits associated with moderate alcohol use: A necessary corrective to assessments of drinking outcomes? Drug Alcohol Depend. 2000;60:221–47. doi: 10.1016/s0376-8716(00)00112-5. [DOI] [PubMed] [Google Scholar]
- 8.Boyd MR, Bland A, Herman J, Mestler L, Murr L, Potts L. Stress and coping in rural women with alcohol and other drug disorders. Arch Psychiat Nurs. 2002;16:254–62. doi: 10.1053/apnu.2002.37280. [DOI] [PubMed] [Google Scholar]
- 9.Windle M. A longitudinal study of stress buffering for adolescent problem behaviors. Develop Psychol. 1992;28:522–30. [Google Scholar]
- 10.Welte JW, Mirand AL. Drinking, problem drinking and life stressors in the elderly general population. J Stud Alcohol. 1995;56:67–73. doi: 10.15288/jsa.1995.56.67. [DOI] [PubMed] [Google Scholar]
- 11.Peirce RS, Frone MR, Russell M, Cooper ML. Relationship of financial strain and psychosocial resources to alcohol use and abuse: the mediating role of negative affect and drinking motives. J Health Soc Behav. 1994;35:291–308. [PubMed] [Google Scholar]
- 12.Peirce RS, Frone MR, Russell M, Cooper ML. A longitudinal model of social contact, social support, depression, and alcohol use. Health Psychol. 2000;19:28–38. doi: 10.1037//0278-6133.19.1.28. [DOI] [PubMed] [Google Scholar]
- 13.Humphreys K, Mankowski ES, Moos RH, Finney JW. Do enhanced friendship networks and active coping mediate the effect of self-help groups on substance abuse? Ann Behav Med. 1999;21:54–60. doi: 10.1007/BF02895034. [DOI] [PubMed] [Google Scholar]
- 14.Broome KM, Simpson DD, Joe GW. The role of social support following short-term inpatient treatment . Am J Addict. 2002;11:57–65. doi: 10.1080/10550490252801648. [DOI] [PubMed] [Google Scholar]
- 15.Bond J, Kaskutas LA, Weisner C. The persistent influence of social networks and Alcoholics Anonymous on abstinence. J Stud Alcohol. 2003;64:579–88. doi: 10.15288/jsa.2003.64.579. [DOI] [PubMed] [Google Scholar]
- 16.Kaskutas LA, Bond J, Humphreys K. Social networks as mediators of the effect of Alcoholics Anonymous. Addiction. 2002;97:891–900. doi: 10.1046/j.1360-0443.2002.00118.x. [DOI] [PubMed] [Google Scholar]
- 17.Cohen S, Syme SL, editors. Social Support and Health. New York: Academic Press; 1985. [Google Scholar]
- 18.Cooper ML, Russell M, Skinner JB, Frone MR, Mudar P. Stress and alcohol use: Moderating effects of gender, coping, and alcohol expectancies. J Abnorm Psych. 1992;101:139–52. doi: 10.1037//0021-843x.101.1.139. [DOI] [PubMed] [Google Scholar]
- 19.Park P. Social-class factors in alcoholism. In: Kissin B, Begleiter H, editors. The Pathogenesis of Alcoholism: Psychosocial Factors. New York: Plenum; 1983. pp. 365–404. [Google Scholar]
- 20.Romelsjo A, Lundberg M. The changes in the social class distribution of moderate and high alcohol consumption and of alcohol-related disabilities over time in Stockholm County and in Sweden. Addiction. 1996;91:1307–23. doi: 10.1046/j.1360-0443.1996.91913076.x. [DOI] [PubMed] [Google Scholar]
- 21.Thoits PA. Stress, coping, and social support processes: where are we? what next? J Health Soc Behav. 1995;35 (Extra Issue):53–79. [PubMed] [Google Scholar]
- 22.Lindenberg GS, Strickland O, Solorzano R, Galvis C, Dreher M, Darrow VC. Correlates of alcohol and drug use among low-income Hispanic immigrant childbearing women living in the U.S.A. Int J Nurs Studies. 1999;36:3–11. doi: 10.1016/s0020-7489(98)00046-7. [DOI] [PubMed] [Google Scholar]
- 23.Nyamathi AM. Relationship of resources to emotional distress, somatic complaints, and high-risk behaviors in drug recovery and homeless minority women. Res Nurs Health. 1991;14:269–77. doi: 10.1002/nur.4770140405. [DOI] [PubMed] [Google Scholar]
- 24.Unger JB, Kipke MD, Simon TR, Johnson CJ, Montgomery SB, Iverson E. Stress, coping, and social support among homeless youth. J Adolescent Res. 1998;13:134–57. [Google Scholar]
- 25.Midanik LT, Clark WB. Demographic distribution of US drinking patterns in 1990: Description and trends from 1984. Am J Public Health. 1994;84:1218–22. doi: 10.2105/ajph.84.8.1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harrison L, Gardiner E. Do the rich really die young? Alcohol-related mortality and social class in Great Britain, 1988–94. Addiction. 1999;94:1871–80. doi: 10.1046/j.1360-0443.1999.9412187112.x. [DOI] [PubMed] [Google Scholar]
- 27.Schmidt LA, Wiley JA, Dohan D, Zabkiewicz D, Jacobs L, Henderson S, et al. Changing patterns of addiction and public aid receipt: tracking the unintended consequences of welfare reform policy. J Health Polit Policy Law. 2006;31:945–80. doi: 10.1215/03616878-2006-013. [DOI] [PubMed] [Google Scholar]
- 28.Pollack HA, Danziger S, Seefeldt KS, Jayakody R. Substance use among welfare recipients: trends and policy responses. Soc Serv Rev. 2002;76:256–74. [Google Scholar]
- 29.Berkman LF, Glass TA. Social integration, social networks, social support, and health. In: Berkman LF, Kawachi I, editors. Social Epidemiology. New York: Oxford University Press; 2000. pp. 137–73. [Google Scholar]
- 30.Macintyre S, Ellaway A. Neighborhoods and health: an overview. In: Kawachi I, Berkman LF, editors. Neighborhoods and Health. New York: Oxford University Press; 2003. pp. 20–42. [Google Scholar]
- 31.Edin K, Lein L. Making Ends Meet: How Single Mothers Survive Welfare and Low-Wage Work. New York: Russell Sage Foundation; 1997. [Google Scholar]
- 32.Seccombe K. “So You Think I Drive a Cadillac?”: Welfare Recipients’ Perspectives on the System and Its Reform. Needham Heights, MA: Allyn and Bacon; 1999. [Google Scholar]
- 33.Waitzman NJ, Smith KR. Phantom of the area: poverty-area residence and mortality in the United States . Am J Public Health. 1998;88:973–76. doi: 10.2105/ajph.88.6.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health . J Health Soc Behav. 2001;42:258–76. [PubMed] [Google Scholar]
- 35.Wandersman A, Nation M. Urban neighborhoods and mental health: psychological contributions to understanding toxicity, resilience, and interventions. Am Psychol. 1998;53:647–56. [PubMed] [Google Scholar]
- 36.Leblanc AN. Random Family: Love, Drugs, Trouble, and Coming of Age in the Bronx. New York: Scribner; 2003. [Google Scholar]
- 37.Mulia N, Schmidt LA. Conflicts and trade-offs due to alcohol and drugs: clients’ accounts of leaving welfare. Soc Serv Rev. 2003;77:499–522. [Google Scholar]
- 38.Stack CB. All Our Kin: Strategies for Survival in a Black Community. New York: Harper and Row; 1974. [Google Scholar]
- 39.Skogan WG. Disorder and Decline: Crime and the Spiral of Decay in American Neighborhoods. New York: Free Press; 1990. [Google Scholar]
- 40.Saegert S, Winkel G. Crime, social capital, and community participation. Am J Commun Psychol. 2004;34:219–33. doi: 10.1007/s10464-004-7416-2. [DOI] [PubMed] [Google Scholar]
- 41.Belle D. Poverty and women’s mental health. Am Psychol. 1990;45:385–89. [Google Scholar]
- 42.Domínguez S, Watkins C. Creating networks for survival and mobility: social capital among African-American and Latin-American low-income mothers. Social Probl. 2003;50:111–35. [Google Scholar]
- 43.Brodsky AE. Making it: the components and process of resilience among urban, African-American, single mothers. Am J Orthopsychiatry. 1999;69:148–160. doi: 10.1037/h0080417. [DOI] [PubMed] [Google Scholar]
- 44.Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. J Health Soc Behav. 1981;22:337–56. [PubMed] [Google Scholar]
- 45.Lazarus RS, Folkman S. Stress, appraisal and coping. New York: Springer; 1984. [Google Scholar]
- 46.Carney MA, Armeli S, Tennen H, Affleck G, O’neil TP. Positive and negative daily events, perceived stress and aclohol use: a diary study. J Consult Clin Psychol. 2000;68:788–98. [PubMed] [Google Scholar]
- 47.Weisner C, Schmidt L, Tam TW. Assessing bias in community-based prevalence estimates: towards an unduplicated count of problem drinkers and drug users. Addiction. 1995;90:391–406. doi: 10.1046/j.1360-0443.1995.9033918.x. [DOI] [PubMed] [Google Scholar]
- 48.United States General Accounting Office. Drug Use Measurement: Strengths, Limitations, and Recommendations for Improvement. Washington DC: United States General Accounting Office; 1993. [Google Scholar]
- 49.U.S. Department of Heath and Human Services Administration for Children and Families. [(accessed January 31, 2008)];Fiscal Year 2001 Characteristics and Financial Circumstances of TANF Recipients. 2005 Available at: http://www.acf.hhs.gov//programs/ofa/character/FY2001/characteristics.htm.
- 50.Odierna DH, Schmidt LA. Lost and found: on the effects of failure to include hard-to-reach respondents in public health research. Am J Public Health. doi: 10.2105/AJPH.2007.111138. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Clark W, Hilton M, editors. Alcohol in America: Drinking Practices and Problems in a National Survey. New York, NY: State University of New York Press; 1991. [Google Scholar]
- 52.Wilsnack SC, Klassen AD, Schur BE, Wilsnack RW. Predicting onset and chronicity of women’s problem drinking: a five-year longitudinal analysis. Am J Public Health. 1991;81:305–18. doi: 10.2105/ajph.81.3.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Weisner CM, Schmidt LA. Alcohol and drug problems among diverse health and social service populations. Am J Public Health. 1993;83:824–29. doi: 10.2105/ajph.83.6.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Weisner CM, Schmidt LA. Gender disparities in treatment for alcohol problems . JAMA. 1992;268:1872–76. [PubMed] [Google Scholar]
- 55.Schmidt LA, Weisner CM, Wiley JA. Substance abuse and the course of welfare dependency . Am J Public Health. 1998;88:1616–22. doi: 10.2105/ajph.88.11.1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schmidt LA, Dohan D, Wiley J, Zabkiewicz D. Addiction and welfare dependency: interpreting the connection. Social Probl. 2002;49:221–41. [Google Scholar]
- 57.Lown EA, Schmidt LA, Wiley JA. Interpersonal violence among women seeking welfare: unraveling lives. Am J Public Health. 2006;96:1409–15. doi: 10.2105/AJPH.2004.057786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Boulet J, Boss M. Reliability and validity of the Brief Symptom Inventory . J Consult and Clinl Psych. 1991;3:433–37. [Google Scholar]
- 59.Derogatis LR, Spencer PM. Administration and Procedures: BSI manual -- I. Baltimore, MD: Clinical Psychometric Research, Division of Medicine Psychiatry, John Hopkins University, School of Medicine; 1982. [Google Scholar]
- 60.Ewart CK, Suchday S. Discovering how urban poverty and violence affect health: development and validation of a neighborhood stress index. Health Psych. 2002;21:254–62. doi: 10.1037//0278-6133.21.3.254. [DOI] [PubMed] [Google Scholar]
- 61.Perkins DD, Taylor RB. Ecological assessments of community disorder: their relaitonship to fear of crime and theoretical implications. Am J Commun Psychol. 1996;24:63–107. doi: 10.1007/BF02511883. [DOI] [PubMed] [Google Scholar]
- 62.University of Michigan Ford School of Public Policy. [(accessed January 31, 2008)];The Women’s Health Study: Wave 1 Survey Instrument. 1997 Available at: http://www.fordschool.umich.edu/research/poverty/wes/instrument/wave_1.php.
- 63.Mulia N. Questioning sex: drug-using women and heterosexual relations. J Drug Issues. 2000;30:741–66. [Google Scholar]
- 64.Stata Corp. Stata Statistical Software: Release 9.0. College Station, TX: Stata Corporation; 2005. [Google Scholar]
- 65.Diggle PJ, Heagerty P, Liang K-Y, Zeger SL. Analysis of Longitudinal Data. 2. Oxford, United Kingdom: Oxford University Press; 2002. [Google Scholar]
- 66.Zivot M, Jacobs L. Technical Report 8: Welfare Client Longitudinal Study -Demographic Changes in Our Study County, 1989–2001. Berkeley, CA: Alcohol Research Group; 2004. [Google Scholar]
- 67.National Institute on Alcohol Abuse and Alcoholism. Forecast for the Future: Strategic Plan to Address Health Disparities. Bethesda, MD: National Institute of Health; 2004. [Google Scholar]
- 68.Schmidt L, Greenfield TK, Mulia N. Unequal treatment: racial and ethnic disparities in alcoholism treatment services. Alcohol Res Health. 2006;29:49–54. [PMC free article] [PubMed] [Google Scholar]
- 69.Boardman JD, Finch BK, Ellison CG, Williams DR, Jackson JS. Neighborhood disadvantage, stress, and drug use among adults . J Health Soc Behav. 2001;42:151–65. [PubMed] [Google Scholar]
- 70.Droomers M, Schrijvers CTM, Stronks K, Van De Mheen D, Mackenbach JP. Educational differences in excessive alcohol consumption: the role of psychosocial and material stressors. Prev Med. 1999;29:1–10. doi: 10.1006/pmed.1999.0496. [DOI] [PubMed] [Google Scholar]
- 71.Schmidt L, McCarty D. Welfare reform and the changing landscape of substance abuse services for low-income women. Alcohol Clin Exp Res. 2000;24:1298–311. [PubMed] [Google Scholar]
- 72.Wilson WJ. The Truly Disadvantaged: The Inner City, the Underclass, and Public Policy. Chicago, IL: University of Chicago Press; 1987. [Google Scholar]
- 73.Neve RJM, Lemmens PH, Drop MJ. Changes in alcohol use and drinking problems in relation to role transitions in different stages of the life course. Subst Abus. 2000;21:163–78. doi: 10.1080/08897070009511430. [DOI] [PubMed] [Google Scholar]
- 74.Hajema KJ, Knibbe RA. Changes in social roles as predictors of changes in drinking behaviour. Addiction. 1998;93:1717–27. doi: 10.1046/j.1360-0443.1998.931117179.x. [DOI] [PubMed] [Google Scholar]
- 75.Ross CE, Mirowsky J. Disorder and decay: The concept and measurement of perceived neighborhood disorder. Urban Aff Rev. 1999;34:412–32. [Google Scholar]
- 76.Lepore SJ, Evans GW, Schneider ML. Dynamic role of social support in the link between chronic stress and psychological distress. J Pers Soc Psychol. 1991;61:899–909. doi: 10.1037//0022-3514.61.6.899. [DOI] [PubMed] [Google Scholar]
- 77.Ceballo R, Mcloyd VC. Social support and parenting in poor, dangerous neighborhoods. Child Dev. 2002;73:1310–21. doi: 10.1111/1467-8624.00473. [DOI] [PubMed] [Google Scholar]
- 78.Fernández-Kelly MP. Social and cultural capital in the urban ghetto: Implications for the economic sociology of immigration. In: Portes A, editor. The Economic Sociology of Immigration. New York: Russell Sage Foundation; 1995. pp. 213–47. [Google Scholar]
- 79.Alegría M, Pérez DJ, Williams S. The role of public policies in reducing mental health status disparities for people of color. Health Aff. 2003;22:51–64. doi: 10.1377/hlthaff.22.5.51. [DOI] [PubMed] [Google Scholar]
- 80.Currie E. Reckoning: Drugs, the Cities, and the American Future. New York, NY: Hill and Wang; 1993. [Google Scholar]