Abstract
AIM: To evaluate the effect of different approaches in the treatment of achalasia in China.
METHODS: We performed a systematic review and meta-analysis of Chinese literature by searching the Chinese Biomedical Database and Chinese scientific Journals database (up to March 2008). All cohort studies (controlled or uncontrolled) in which the patients were observed for more than a year were reviewed in detail. Dichotomous outcomes were reported as relative risks (RR) with 95% confidence interval (CI) for controlled trials. The efficacy in uncontrolled trials was assessed by a pooled estimate of response rate with individual studies weighted in proportion to the sample size.
RESULTS: Seven controlled trials compared the effect of botulinum toxin injection (BoTx) with pneumatic dilation (PD). PD was superior to BoTx [65.2% vs 45.3%; RR 1.47 (95% CI 1.23-1.77), P < 0.0001], and had a lower clinical relapse rate (BoTx 30.2% vs PD 10%, RR 0.32 (0.16-0.65), P = 0.001). Heller myotomy (HM) had superior remission rate compared to PD [HM 94.0% vs PD 64.1%, RR 1.48 (1.15-1.99), P = 0.002]. In uncontrolled trials, the effectiveness of PD was 86.6% (23.9%) vs 94.8% (10.6%) for HM. The main complications of PD were perforation and gastroesophageal reflux disease.
CONCLUSION: HM is the most effective long-term treatment for patients with achalasia in China. In the future, controlled clinical trials on the treatment of achalasia should focus on comparing laparoscopic myotomy with or without antireflux procedure, including different partial and total fundoplication techniques.
Keywords: Meta-analysis, Achalasia, Esophageal, Treatment, Pneumatic dilation, Botulinum toxin injection, Laparoscopic myotomy
INTRODUCTION
Achalasia is an idiopathic primary motility disorder, characterized manometrically by poor relaxation of the lower esophageal sphincter (LES) and complete loss of primary peristalsis, which leads to a compromise in the primary function of the esophagus[1]. The cause of achalasia is not known. Untreated, it leads to an extremely poor quality of life because of progressive dysphagia, esophageal dilation, and stasis[2]. Botulinum toxin (BoTx) injection of the LES, pneumatic dilation (PD) and Heller myotomy (HM) are the most commonly used techniques for the treatment of achalasia[3].
BoTx prompted a great deal of enthusiasm because it is safe, simple to use and can be easily repeated[4]. There are no reports of any serious complications after BoTx injection. However, symptoms often recur after the first injection and serial injections are required, with the efficacy waning over time due to the production of antibodies[5]. Currently, newly diagnosed achalasia patients are offered serial PDs, followed by surgical intervention if the dilatations fail[6]. With the introduction of HM, there has been a change in the initial management approach to the treatment of achalasia. However, there is much controversy as to which treatment provides the best efficacy, sustained symptom relief and low complication rate[7], especially in China[8]. Therefore, the aim of the present study was to evaluate the effects of different treatment modalities by reviewing the published trials in China.
MATERIALS AND METHODS
Study design
All controlled and uncontrolled studies were included in the analysis if the patients underwent clinical, manometric, radiographic and endoscopic evaluation to confirm the diagnosis of primary achalasia. The presence of symptoms and esophageal function were reassessed at 6 mo and 1 year after therapy. Treatment efficacy was determined by the improvement rate (%) in the symptom score, 1 year after therapy. Treatment failure was defined as the lack of any reduction in the symptom grade of > 1, or a recurrence of symptoms 1 year after therapy.
Search strategy and data extraction
Two investigators independently searched the Chinese literature published in the Chinese Biomedical Database and Chinese scientific Journals database (up to March 2008). All controlled or uncontrolled trials involving patients with achalasia who were given any form of treatment were included in the analysis. The search terms used were “esophageal” or “oesophagus”, “achalasia”, and “therapy” or “treatment”. Data was extracted by the same investigators using standardized forms. The date obtained included the number of patients, the exact methods of therapy, the outcome variables listed above, and any reported adverse effects of therapy. The quality of all selected articles was ranked in accordance with the Jadad composite scale. According to this scale, low quality studies had a score of ≤ 2 and high quality studies had a score of ≥ 3.
Statistical analysis
We performed the meta-analysis using the RevMan 4.2.10 software (provided by the Cochrane Collaboration, Oxford, UK) for the controlled studies. The relative risk (RR) was calculated with 95% confidence intervals (CI). We used χ2 to assess statistical heterogeneity and the Higgins I2 statistic to determine the percentage of total variations across studies due to heterogeneity. If the I2 statistic was ≤ 50%, the fixed effect model was used to pool studies, otherwise, the random effects model was used. The efficacy in uncontrolled trials was assessed by a pooled estimate of the response rate with individual studies weighted proportionally to the sample size[9]. In calculating the weighted mean response for each treatment modality (ƥ), the studies were characterized by the number of subjects included (n) and the response rate in those subjects (p). Ellipses represents scant data.
ƥ = (n1p1 + n2p2 + nxpx)/(n1 + n2 + n3)
SE (ƥ) = Sqrt {[p1(1-p1)/n1] + [p2(1-p2)/n2] + [px(1-px)/nx]}
RESULTS
Study characteristics
The search strategy generated 612 studies. From these, we identified 43 studies (12 controlled studies and 31 uncontrolled studies) that met the inclusion criteria. Only studies that included more than 10 patients, and had a follow-up of at least 12 mo were tabulated (Table 1). Sample sizes in the trials ranged from 10 to 125 participants (total 1791); 46.9% of the participants were male. Ten controlled studies were considered to be of low quality, and two controlled trials were graded as high quality (Table 2).
Table 1.
Demographic data of studies included in systematic review
| No. of patients | Age (yr) (median) (range) | Sex (M/F) | Remission rate (%) (mo) | Relapse rate (%) (mo) | Follow up time (mo) | Complications (n/N, type) | |
| Cai et al 2003[10] | 62 BoTx | 38.7 ± 32.8 | 72/46 | 67.35 (12) | 25.8 (12) | 24 | |
| 56 PD | 92 | 5.40 | 1/56 EF | ||||
| Liu et al 2003[11] | 16 BoTx | 36.2 ± 13.4 | 7/9 | 18.75 (12) | NA | 12 | 0/16 |
| 16 PD | 35.2 ± 10.2 | 6/10 | 37.50 | ||||
| 16 BoTx + PD | 38.1 ± 12.6 | 8/8 | 87.50 | ||||
| Gui et al 2006[12] | 16 BoTx | 32.3 ± 10.2 | 5/11 | 87.5 (12 ) | 37.5 (12) | 12 | 0/16 |
| 16 PD | 7/9 | 93.80 | 18.80 | ||||
| Yang et al 2002[13] | 24 BoTx | 42.2 ± 13.1 | 10/14 | 16.67 (12) | NA | 12 | 0/24 |
| 24 PD | 12/12 | 33.33 | |||||
| Jin et al 2004[14] | 14 BoTx | 35.3 ± 15.3 | 6/8 | 21.4 (12) | NA | 24 | |
| 16 PD | 7/9 | 62.50 | NA | 1/16 PF | |||
| Qian et al 2006[15] | 20 BoTx | 53.4 ± 10.4 | 12/8 | 50 (12) | NA | 24 | 0/20 |
| 20 PD | 10/10 | 85 | 2/20 | ||||
| Yin et al 2003[16] | 18 BoTx | 36.8 ± 12.1 | 10/8 | 50 (12) | 38.9 (12) | ||
| 13 PD | 7/6 | 76.90 | 23.10 | ||||
| Yang et al 2006[17] | 25 PD | 37.1 ± 13.6 | 13/12 | 28 (12) | 36 (12) | 24 | 13 MH |
| 18 BoTx + PD | 8/10 | 61 | 16.70 | 3 MH | |||
| Jia et al 2001[18] | 20 PD | 43.4 ± 15.1 | 12/8 | 52.63 (12) | 47.06 (12) | unclear | |
| 19 HM | 41.8 ± 13.9 | 10/9 | 94.4 (12) | 0 | 8 GER | ||
| Ge et al 1997[19] | 20 PD | 39.5 ± 11.2 | 16/24 | 75 (12) | NA | 24 | 1 GER |
| 20 HM | 93 (12) | 168 | 3 GER | ||||
| Jiang et al 2007[20] | 27 TM | 43.4 ± 15.1 | 12/15 | 85.2 (24) | 11 (12) | 24 | 3 PF |
| 8 LM + Dor | 50.3 ± 13.5 | 3/5 | 87.50 | 12.50 | 1 PF | ||
| Guo et al 2005[21] | 29 LM | 38.2 ± 10.6 | 15/14 | 100 (24) | 0 | 2-60 | |
| 54 TM | 39.1 ± 12.1 | 21/33 | 98.1 (24) | 1.9 (12) | 1-80 | 1 PA | |
| Li et al 1994[22] | 15 HM | 38.6 ± 15.6 | 28/44 | 86.4 (12) | NA | 36 | 3/15 GER |
| 52 HM + Dor | 96 | 5/52 GER | |||||
| Jiang et al 2002[23] | 30 PD | 36 ± 10.6 | 19/21 | 87 (12) | 13 (12) | ||
| 10 HM | 100 | 0 (120) | 3/10 GER | ||||
| Jiang et al 2007[24] | 30 TM | 45.2 ± 13.1 | 12/18 | 90 (48) | 3.3 (2y) | 96 | 3 PF |
| Gu et al 2007[25] | 125 PD | 48.3 ± 19.3 | 57/68 | 92.14 (12) | 7.86 (60) | 60 | 1 PF; 1 GER |
| Zhang et al 2005[26] | 90 Open - TM | 37.1 ± 20.1 | 40/50 | 100 (12) | 0 (12) | 3 | 1 PF |
| Xu et al 2007[27] | 29 BoTx - PD | 40.6 ± 13.3 | 12/17 | 93.1 (12) | 6.9 (12) | 12 | NA |
| Xu et al 2003[28] | 28 PD | 32.6 ± 14.2 | 4/24 | 85.7 (12) | 14.3 (12) | 24 | None |
| Li et al 2004[29] | 75 PD | 37 ± 11.1 | 39/36 | 91 (12) | 10.7 (12) | 12 | 2 PF |
| Jia et al 2003[30] | 38 PD | 31.3 ± 12.0 | 12/26 | 89.5 (12) | 10.5 (12) | 36 | 1 MH |
| Chen et al 2005[31] | 32 PD | 40.2 ± 10.6 | 8/24 | 81.25 (24) | 18.6 (24) | 24 | 3 MH |
| Zhu et al 2005[32] | 23 PD | 33.4 ± 12.3 | 9/14 | 75 (24) | 25 (24) | 24 | 17 MH |
| Ma et al 2002[33] | 26 PD | 34.2 ± 11.3 | 14/12 | 92.3 (24) | 3.8 (24) | 4-36 | 7 CP |
| Wu et al 2007[34] | 29 PD | 38.2 ± 14.1 | 21/8 | 82.7 (12) | 10.3 (12) | 12-102 | 3 GER |
| Lin et al 2004[35] | 37 PD | 33.1 ± 12.3 | 21/16 | 91.9 (24) | 8 (12) | 12 | 8 CP |
| Jia et al 2003[36] | 19 PD | 26.2 ± 8.90 | 8/11 | 82 (24) | 18.8 (24) | 24 | 8 GER |
| Wei et al 2005[37] | 18 HM | 32.1 ± 10.1 | 12/6 | 94.4 (12) | 5.6 (12) | 24 | 2 GER |
| Zhong et al 2003[38] | 58 PD | 42.5 ± 2.5 | 28/27 | 93.1 (12) | 6.9 (12) | 16-24 | 4 GER |
| Du et al 2003[39] | 48 HM | 35.0 ± 11.2 | 22/26 | 100 (24) | 0 (24) | 75 | 3 GER |
| Li et al 2005[40] | 19 HM | 32.8 ± 11.6 | 20/12 | 94.4 (12) | 5.3 (12) | 12-120 | 4 GER |
| 13 HM + Dor | 100 (12) | 0 | 1 GER | ||||
| Song et al 2001[41] | 21 HM | 34.5 ± 9.30 | 12/9 | 90.5 (12) | 0 | 12-144 | 2 GER |
| Li et al 2005[42] | 15 HM | 29 ± 7.80 | 5/10 | 100 (12) | 0 | 36-156 | 0 |
| Xiao et al 2004[43] | 27 LM | 48.1 ± 12.6 | 15/12 | 96.3 (24) | 3.7 (24) | 14 | 0 |
| Sun et al 2003[44] | 39 HM | 31.3 ± 7.60 | 15/24 | 83.8 (24) | 1.7 (24) | 12-120 | 9 LM |
| Wang et al 2005[45] | 21 HM+Dor | 45.5 ± 13.5 | 6/15 | 100 (24) | 0 | 24-60 | 0 |
| Lu et al 2002[46] | 56 HM | 37 ± 11.2 | 24/32 | 96.4 (36) | 3.6 (36) | 3-178 | 16 GER |
| Zhu et al 2007[47] | 56 PD | 37.5 ± 10.7 | 17/39 | 84.4 (12) | 15 (12) | 1-48 | 0 |
| Chen et al 2003[48] | 32 PD | 35 ± 13.2 | 14/18 | 81.3 (12) | 3.8 (12) | 1-6 | 6 CP |
| Wang et al 2007[49] | 25 PD | 35.8 ± 9.30 | 10/15 | 89 (12) | 8 (12) | 12-36 | 5 GER |
| Han et al 2004[50] | 34 PD | 32.3 ± 11.8 | 20/14 | 92 (24) | 5.9 (12) | 24-35 | 1 PF |
| Yang et al 2007[51] | 16 TM | 42.5 ± 10.2 | 6/10 | 93.3 (12) | 6.7 (12) | 14 | 1 ML |
| Huang et al 2005[52] | 18 TM | 39 ± 8.90 | 7/11 | 94 (12) | 6 (12) | 1-80 | 1 PA; 3 ML |
BoTx: Botulinum toxin; PD: Pneumatic dilation; BoTx-PD: Botulinum toxin plus Pneumatic dilation; HM: Heller myotomy; HM + Dor: Heller myotomy and Dor fundoplication; EF: Esophageal fistula; PF: Perforation; MH: Mucosae hemorrhage; PA: Pulmonary atelectasis; CP: Chest pain; MIS: Metal internal stent; ML: Mucosae laceration; CP: Chest pain; PA: Pulmonary atelectasis.
Table 2.
Methodological quality of randomized controlled trials included in systematic review
| Yr | Randomisation method | Blind | Explanation for withdrawals | Allocation concealment | Jadad score | |
| Cai et al[10] | 2003 | Random | Unclear | Yes | Unclear | 3 |
| Liu et al[11] | 2003 | Random | Unclear | Yes | Unclear | 3 |
| Gui et al[12] | 2006 | Unclear | Unclear | Yes | Unclear | 2 |
| Yang et al[13] | 2002 | Unclear | Unclear | Yes | Unclear | 2 |
| Jin et al[14] | 2004 | Unclear | Unclear | Yes | Unclear | 2 |
| Qian et al[15] | 2006 | Unclear | Unclear | Yes | Unclear | 2 |
| Yin et al[16] | 2003 | Unclear | Unclear | Yes | Unclear | 2 |
| Yang et al[17] | 2006 | Unclear | Unclear | Yes | Unclear | 2 |
| Jia et al[18] | 2001 | Random | Unclear | Yes | Unclear | 3 |
| Ge et al[19] | 1997 | Unclear | Unclear | Yes | Unclear | 2 |
| Jiang et al[20] | 2007 | Unclear | Unclear | Yes | Unclear | 2 |
| Guo et al[21] | 2005 | Unclear | Unclear | Yes | Unclear | 2 |
Effects of the treatment of achalasia
Control studies: There were five controlled studies[10-14], while two studies[15,16] compared the clinical effect of BoTx with that of PD. Our meta-analysis showed that BoTx was significantly more effective than PD in the incidence of symptom remission [PD 65.2% vs BoTx 45.3%, RR 1.47 (95% CI 1.23-1.77), P < 0.0001, Figure 1A], whereas PD had a lower relapse rate than BoTx [PD 10% vs BoTx 30.2%, RR 0.32 (0.16-0.65), P = 0.001, Figure 1B]. The main adverse effect of BoTx injection was chest pain which was controlled by medical therapy. Complications with PD consisted of perforation and gastroesophageal reflux disease (GERD). Some patients were referred for Heller myotomy. We believe that PD is the preferred medical treatment for achalasia, if performed by a skillful expert.
Figure 1.
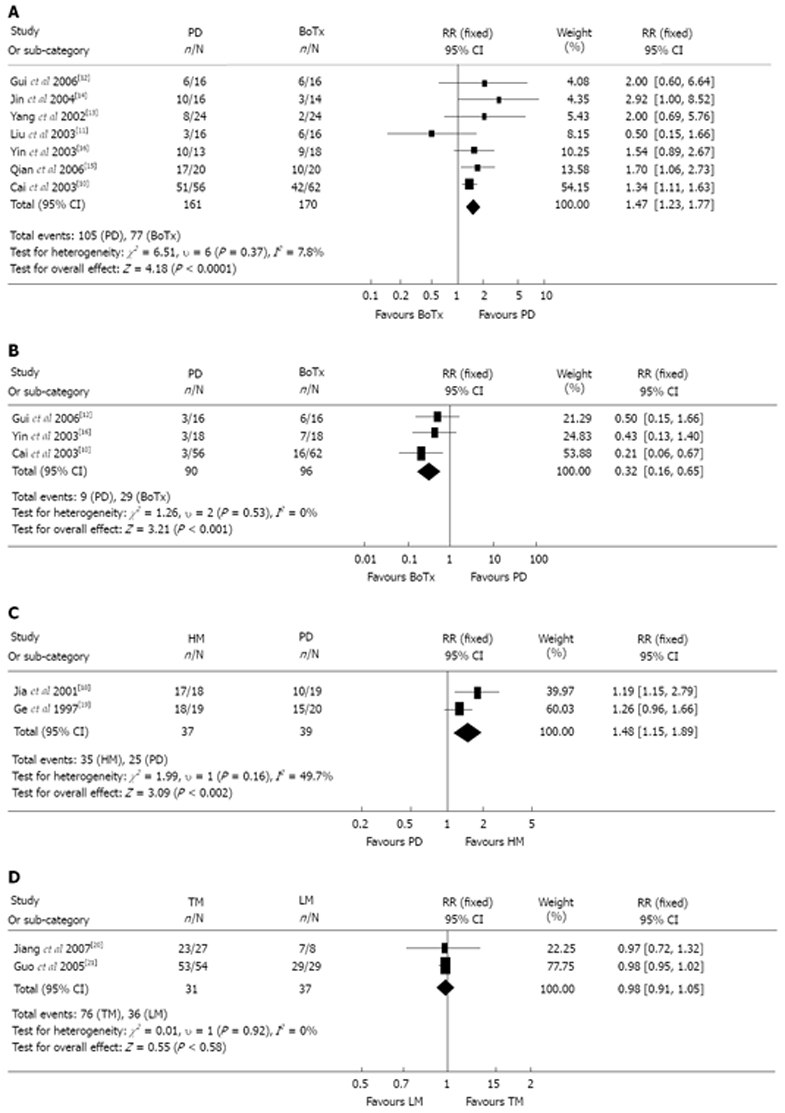
Meta-analysis. A: Treatment effect of pneumatic dilation vs botulinum toxin injection; B: Relapse rate of pneumatic dilation vs botulinum toxin injection; C: Treatment effect of pneumatic dilation vs Heller myotomy; D: Treatment effect of laparoscopic myotomy vs thoracoscopic myotomy.
One trial[17] compared PD with BoTX-PD. The one year remission rate in the BoTX-PD group was 61% compared with 28% in the PD group (P < 0.05). It was suggested that BoTx injection before PD improved the efficacy of PD. However, some studies have shown that primary BoTx treatment increased the risk for PD[53]. Therefore, more randomized controlled studies are required to evaluate whether combined therapy is superior to single treatment in achalasia.
Two controlled studies[18,19] compared the effect of PD with HM. Our meta-analysis showed that HM had superior remission rate compared to PD [HM 94.0% vs PD 64.1%, RR 1.48 (1.15-1.99), P = 0.002), (Figure 1C]. There was no difference in the complication rate between HM and PD. These findings suggest that HM offers better long-term clinical results than PD. Two trials[20,21] assessed the efficacy of laparoscopic myotomy (LM) with thoracoscopic myotomy (TM). The results showed that good or excellent relief of symptoms was obtained in 93.8% after TM and 98% after LM, with no difference in the remission rate [RR 1.48 (0.91-1.05, P = 0.58), Figure 1D]. These findings need further confirmation and validation.
Uncontrolled trials: There were 31 uncontrolled trials on different treatment methods for achalasia. Table 3 summarizes the results obtained with endoscopic and surgical treatment. Some studies were conducted prospectively[22-26], while others[27-31] were retrospective reviews. These studies evaluated the clinical effect of PD[32-36] and the long term efficacy of HM by the abdominal approach[37,39-42]. One study[43] assessed the efficacy of LM. Some studies[44-46] evaluated the remission rate of HM with fundoplication, while others[38,47-50] reported the efficacy of large diameter balloon dilation. Three trials[24,51-52] evaluated the efficacy of TM. The results were combined (shown in Table 3) because the findings were identical. In calculating the response rate of each study, we extracted the number of individuals with a good-to-excellent response that was sustained until the end of the observation period, without further therapy. Thus, if a patient required a second dilation or a second injection, or if a laparoscopic operation was converted to an open procedure, these were considered as failures of initial treatment. The results show that PD and HM are the most popular treatment methods for achalasia in China; the effectiveness of PD [weighted mean (SD)] was 86.6% (23.9%) vs 94.8% (10.6%) for HM. Only 3 of the 31 uncontrolled trials evaluated the clinical effect of TM [weighted mean (SD)] [92.0% (10.0%)], while one study evaluated the effect of LM (96.3%). However, in most western countries, the majority of patients undergo LM, with excellent results[54]. Some workers regard LM as the gold standard treatment for achalasia[55]. More randomized controlled trials should be carried out in China to evaluate the effect of LM. There was a significant difference in the effect of PD between controlled trials and uncontrolled trials (controlled 65.2% vs uncontrolled 86.6%). Therefore, a uniform standard for evaluating the effect of achalasia treatment should be developed.
Table 3.
Pooled estimate of response rate of non-controlled trials for achalasia treatments across referenced trials
| Therapy and references | Total No. of patients |
Weighted response of treatment methods for achalasia (1 yr after treatment) |
||
| Remission rate (ƥ) mean ± SE, % | Relapse rate (ƥ) mean ± SE, % | Weighted follow-up mean (range), mo | ||
| PD | 667 | 86.6 ± 23.9 | 10.7 ± 21.0 | 26 (4-102) |
| HM | 354 | 94.8 ± 10.6 | 1.5 ± 6.3 | 46 (1-178) |
| TM | 64 | 92.0 ± 10.0 | 4.91 ± 9.0 | 30 (1-80) |
PD: Pneumatic dilation; BoTx-PD: Botulinum toxin plus Pneumatic dilation; HM: Heller myotomy. In calculating the weighted mean response for each treatment modality (ƥ), included studies were characterized by the number of subjects included (n) and the response rate for those subjects (p). Ellipses represent scant data.
DISCUSSION
The present review indicates that HM is the best choice for the treatment of achalasia in China. HM has gained widespread popularity for its excellent results and the advantage of a 1-shot therapy. There was no significant difference in the complication rate between LM and PD. PD was also a popular therapy in Chinese patients. Although side effects, such as perforation and bleeding occur with PD, the remission rate was higher with PD compared to BoTx. Moreover, the recurrence rate was higher with BoTx compared to PD.
However, Bassotti et al[56] using a different BoTx regimen, consisting of two injections within a 4-wk period, reported a success rate 80% at 12 mo. These findings may encourage new interest in this therapy. Moreover, BoTx treatment is less expensive, is virtually risk-free, is easy to administer by any endoscopist, and the results are reproducible. Therefore, there is an urgent need for high quality studies to evaluate the efficacy of repeated injections of BoTx, and BoTx combined with other treatment methods.
HM is an invasive and risky treatment modality for achalasia, and requires surgical skills that are not always available (the results obtained with HM depend largely on the surgeon’s expertise). To reduce the complications and risks of HM, several modifications have been developed[57], including HM with partial fundoplication, and minimally invasive myotomy, using different endoscopic techniques. In the past, both laparoscopy and thoracoscopy were used to perform HM. However, it soon became clear that laparoscopy offers several inherent advantages, including superior visualization of the gastroesophageal junction, a single lumen endotracheal intubation, the ability to add an anti-reflux procedure, and a shorter hospital stay. In addition, laparoscopy provided better symptomatic outcome and lower incidence of postoperative gastroesophageal reflux (GER)[58]. Our meta-analysis showed that there was no significant difference in the remission rate between LM and TM within 12 mo of the initial intervention. However, LM has a relatively higher response rate in uncontrolled studies (LM 96.3% vs TM 91.95%). Patients experienced greater relief of dysphagia after LM compared to TM. Moreover, GER is the most common complication after HM, and fundoplication cannot be performed at the same time with TM. Therefore, more studies are required to determine whether LM is superior to TM in the treatment of achalasia.
The number of trials included in the present meta-analysis, and the number of patients randomized to receive the different treatment modalities was relatively small. This was compounded by stratification of the subjects into smaller subgroups. Moreover, poor randomization techniques and inadequate follow-up further limited the interpretation of the findings. Few studies provided proper definitions of the postoperative events. Future trials should include standard measures to allow objective and comparable assessment of the outcomes. Standardization was lacking in the reporting of treatment outcomes, length of trial, and the proportion of recruited sample that was kept under follow-up. Several trials failed to accurately present such information. Disease recurrence may also be underestimated, since some studies used telephone contact or questionnaire-based follow-up. Therefore it is possible that a small number of patients with macroscopic but asymptomatic recurrence may not be detected using such assessment techniques.
Our results indicate that in China, HM is the most effective treatment for achalasia and can safely and durably relieve the symptoms of dysphagia. BoTx injection is recommended if multiple injections are given or is combined with other treatment modalities. PD provides better dysphagia control, but is associated with the risk of perforation. It is important that more randomized controlled clinical trials are carried out in China to compare LM, with and without an antireflux procedure, and with partial or total fundoplication.
COMMENTS
Background
Botulinum toxin injection (BoTx), pneumatic dilatation and Heller myotomy (HM) are the most commonly used techniques for the treatment of achalasia in China. However, it unclear as to which is the best treatment modality for achalasia.
Research frontiers
The aim of the present study was to evaluate the outcome of different approaches for the treatment of achalasia in Chinese patients.
Innovations and breakthroughs
Previous studies in China suggest that pneumatic dilatation is as effective as HM. It remains unclear whether pneumatic dilatation can achieve sustained symptom remission. In the present study, HM was found to provide better results compared with other treatment modalities in China.
Applications
Our results helped to identify the best treatment method for Chinese patients. They also offer directions for randomized controlled trials in the future.
Terminology
Achalasia is a primary motor disorder, characterized by incomplete relaxation of the lower esophageal sphincter and aperistalsis of the esophageal body, secondary to the loss of the inhibitory ganglion cells in the myenteric plexus. The etiology of achalasia is unknown; genetic, autoimmune, infectious, and environmental factors have been implicated.
Peer review
This is a systematic review and meta-analysis of the current treatments options for achalasia, namely BoTx, pneumatic dilation, and Heller myotomy. The authors concluded that Heller myotomy is superior to endoscopic approaches. This is a very interesting study.
Acknowledgments
We are grateful to Dr. Yinglong Tao for his excellent assistance in the statistical analysis.
Footnotes
Peer reviewer: Luigi Bonavina, Professor, Department of Surgery, Policlinico San Donato, University of Milano, via Morandi 30, Milano 20097, Italy
S- Editor Li DL L- Editor Anand BS E- Editor Yin DH
References
- 1.Massey BT. Management of idiopathic achalasia: short-term and long-term outcomes. Curr Gastroenterol Rep. 2000;2:196–200. doi: 10.1007/s11894-000-0061-5. [DOI] [PubMed] [Google Scholar]
- 2.Pohl D, Tutuian R. Achalasia: an overview of diagnosis and treatment. J Gastrointestin Liver Dis. 2007;16:297–303. [PubMed] [Google Scholar]
- 3.Da Silveira EB, Rogers AI. Achalasia: a review of therapeutic options and outcomes. Compr Ther. 2002;28:15–22. doi: 10.1007/s12019-002-0038-4. [DOI] [PubMed] [Google Scholar]
- 4.Zaninotto G, Vergadoro V, Annese V, Costantini M, Costantino M, Molena D, Rizzetto C, Epifani M, Ruol A, Nicoletti L, et al. Botulinum toxin injection versus laparoscopic myotomy for the treatment of esophageal achalasia: economic analysis of a randomized trial. Surg Endosc. 2004;18:691–695. doi: 10.1007/s00464-003-8910-6. [DOI] [PubMed] [Google Scholar]
- 5.Vaezi MF, Richter JE, Wilcox CM, Schroeder PL, Birgisson S, Slaughter RL, Koehler RE, Baker ME. Botulinum toxin versus pneumatic dilatation in the treatment of achalasia: a randomised trial. Gut. 1999;44:231–239. doi: 10.1136/gut.44.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kostic S, Kjellin A, Ruth M, Lonroth H, Johnsson E, Andersson M, Lundell L. Pneumatic dilatation or laparoscopic cardiomyotomy in the management of newly diagnosed idiopathic achalasia. Results of a randomized controlled trial. World J Surg. 2007;31:470–478. doi: 10.1007/s00268-006-0600-9. [DOI] [PubMed] [Google Scholar]
- 7.Lake JM, Wong RK. Review article: the management of achalasia - a comparison of different treatment modalities. Aliment Pharmacol Ther. 2006;24:909–918. doi: 10.1111/j.1365-2036.2006.03079.x. [DOI] [PubMed] [Google Scholar]
- 8.Zhang L, Wang MW, Wu BY. Botulinum toxin versus pneumatic dilatation in the treatment of achalasia and a review analysis. Zhongguo Shiyong NeikKe Zazhi. 2005;25:938–939. [Google Scholar]
- 9.Spiess AE, Kahrilas PJ. Treating achalasia: from whalebone to laparoscope. JAMA. 1998;280:638–642. doi: 10.1001/jama.280.7.638. [DOI] [PubMed] [Google Scholar]
- 10.Cai FC, Liu QS, Guo RB, Men JY, Cheng LF. The kinetic changes in esophageal achalasia treated by pneumatic dilation or intrasphincteric injection of botulinum toxin. Shiyong Yixue Zazhi. 2003;19:341–343. [Google Scholar]
- 11.Liu JY, Yang CM, Zhang AZ, Cui Y, Wang HB. Clinical study on intrasphincteric injection of botulinum toxin and/or small balloon dilation in patients with esophageal achalasia. Zhonghua Xiaohua Neijing Zazhi. 2003;20:158–160. [Google Scholar]
- 12.Gui RH, Zheng XP, Leng JH, Wang XP, Duan XM. Clinical study on intrasphinctive injection of botul inum toxin or small balloon dilation in patients with esophageal achalasia. Zhongguo Xiandai Yu Linchuang. 2006;3:31–32. [Google Scholar]
- 13.Yang CM, Liu JY, Liu QY, Zhang AZ, Xiu HW, Wang HB. Clinical study on intrasphincteric injection of botulinum toxin in the treatment of achalasia. Shandong Yixue Zazhi. 2002;42:1–2. [Google Scholar]
- 14.Jin Y. The efficacy of patients with achalasia by intrasphincteric injection of botul inum toxin versus balloon dilation. Xiandai Yiyao Weisheng. 2004;20:1728–1729. [Google Scholar]
- 15.Qian F. Clinical study on intrasphincteric injection of botulinum toxin versus balloon dilation in the treatment of achalasia. Shiyong Zhenduan Yu Zhiliao. 2006;20:908–909. [Google Scholar]
- 16.Yin YM, Lin L, Shi RH, Zhao ZQ. A comparative study on treating achalasia by balloon dilatation and botulinum toxin lical injection. Nanjing Yike Daxue Xuebao. 2003;23:51–53. [Google Scholar]
- 17.Yang ZW, Shao XY, Bu LX, Ma LX, Zhang LP. Clinical study on intrasphinctive injection of botulinum toxin A and balloon dilation in patients with esophageal achalasia. Zhonghua Neijing Zazhi. 2006;12:706–709. [Google Scholar]
- 18.Jia DQ, Ouyang Q, Wang ZQ, Luo CF. The value of pneumatic dilation in treament of esophageal achalasia. Zhonghua Xiaohua Neijing Zazhi. 2001;18:358–359. [Google Scholar]
- 19.Ge F, Zhang LJ, Li ZJ, Ke MY, Wang ZF. To assess the effect of pneumatic dilation and surgery treament of esophageal achalasia. Zhonghua Xiongxin Xueguan Waike Zazhi. 2001;18:301–302. [Google Scholar]
- 20.Jiang W, Tan LJ, Wang Q, Xu ZL, Zheng RH, Zhang Y. Comparison of thoracoscopic and laparoscopic Heller myotomy for achalasia. Zhongguo Linchuang Yixue. 2007;14:55–57. [Google Scholar]
- 21.Guo L, Gu JW, Zhu JY, Wang CS, Tao WD, Gu ML, Huang YG. Laparoscopic management of esophageal achalasia. Fuqiangjing Waike Zazhi. 2005;10:326–327. [Google Scholar]
- 22.Li ZM, Dong WH, Jiang XM. The surgery treatment for achalasia. Zhongguo Xinxueguan Waike Linchuang Zazhi. 1994;1:97–98. [Google Scholar]
- 23.Jiang M, Zhang L, Chu YL, Bai XP, Zhu JX. A comparative study on treating achalasia by Pharmacological therapy, balloon dilatation and botulinum toxin lical injection. Xiandai Xiaohua Ji Jieru Zhenliao. 2002;7:47–49. [Google Scholar]
- 24.Jiang W, Wang Q, Tan LJ, Xu ZL, Zheng RH. The clinical experience of thoracoscopic Heller myotomy for achalasia. Fudan Xuebao (Yixue Ban) 2007;34:296–299. [Google Scholar]
- 25.Gu XH, Zhang ZB, Wang B, Sheng JW. Evaluation of Pneumatic dilation for treatment of primary achalasia under gastroendoscopy. Linchuang Xiaohuabing Zazhi. 2007;19:233–235. [Google Scholar]
- 26.Zhang WX, Wang BX, Chen SX, Luo WJ, Jiang HH, Long L, Zhang CF. Treatment of achalasia of cardia by transthoracic Heller myotomy with tricavity biocapsule tube. Zhongguo Xiandai Yixue Zazhi. 2005;15:2517–2518. [Google Scholar]
- 27.Xu EB, Bai HX, Cai YG, Huang ZW, Xiong YH, Zhang ZB. Study on Intrasphincteric Injection of Botulinum Toxin Combined with Small Balloon Dilation. Shiyong Linchuang Yixue. 2007;8:14–16. [Google Scholar]
- 28.Xu MF, Yu WH, Liu ZW. Evaluation of Pneumtic dilation for treatment of achalasia with 28 patients. Yixue Lilun Yu Shijian. 2003;16:1042–1043. [Google Scholar]
- 29.Li YF, Cui Y, Li CJ, Nie XY. The effect of Pneumtic dilation for treatment of achalasia in the long term. Xin Yixue. 2004;35:677–679. [Google Scholar]
- 30.Jia JZ, Ma YP, Geng JM, Kou HW. Endoscopic direct optional balloon dilatation Therapy for achalasia. Zhongguo Neijing Zazhi. 2003;9:17–19. [Google Scholar]
- 31.Chen Z, Zou YB. Endoscopic Balloon Dilatation for Achalasia. Keji Tongbao. 2005;21:577–579. [Google Scholar]
- 32.Zhu X, Chi BR, Meng XW, Chen LG. The evaluation of endoscopic direct balloon dilation therapy for achalasia. Jiling Yixue. 2005;26:169–170. [Google Scholar]
- 33.Ma YC, Xiong YZ, Zhou CP, Du J, Yang YG. Endoscopic pneumatic dilation for Achalasia. Zhonghua Xiaohua Neijing Zazhi. 2002;19:174–175. [Google Scholar]
- 34.Wu J, Jia YG, Li HY, Chen S, Gan HY. Inside endoscopy next air sac expansion treatment achalasia long-term curative effect in observe. Zhongguo Neijing Zazhi. 2007;13:117–119. [Google Scholar]
- 35.Lin ZG, Liang YG, Huang LZ, Huang Y. Pneumatic dilation treatment for Achalasia with 37 patients. Xiandai Xiaohua Ji Jieru Zhenliao. 2004;9:101. [Google Scholar]
- 36.Jia JZ, Ma YP, Geng JM, Kou HW, Lei XH. Endoscopic direct optical balloon dilatation therapy for achalasia. Ningxia Yixue Zazhi. 2003;25:264–265. [Google Scholar]
- 37.Wei K. Heller myotomy for the treatment of achalasia with 18 patients. Youjiang Mingzu Yixueyuan Xuebao. 2005;27:836. [Google Scholar]
- 38.Zhong M. Pneumatic dilation for the treatment of achalsia by the Endoscopic direct. Zhongguo Neijing Zazhi. 2003;9:41–42. [Google Scholar]
- 39.Du C, Wang RW, Jiang YG, Zhao YP, Tian QY. Treatment of achalasia of cardia by transabdominal cardiomyotomy plus posteroesophageal partial gastric fundoplication. Disan Junyi Daxue Xuebao. 2003;25:528–530. [Google Scholar]
- 40.Li JY, Jiang J, Wei B, Yu T. Long-term results of modified Heller myotomy for achalasia by abdominal approach. Zhonghua Xiongxin Xueguan Waike Zazhi. 2005;21:149–121. [Google Scholar]
- 41.Song QQ, Zhang YR, Zhou Z, Wang YJ, Wei DQ. Modified Heller myotomy for the treatment of achalasia. Zhongguo Putong Waike Zazhi. 2002;11:187–188. [Google Scholar]
- 42.Li B, Zhu LY, Dong ZY, Wang WZ. Heller myotomy for the treatment of achalasia with 15 patients and review. Zhongguo Yiyao Daobao. 2007;4:118–119. [Google Scholar]
- 43.Xiao HB, Melvin WS. Robot-assisted laparoscopic Heller cardiomyotomy. Zhonghua Weichang Waike Zazhi. 2004;7:33–34. [Google Scholar]
- 44.Sun JT, Dai WC, Du MX. Heller and fundoplication for achalasia with 39 patients. Heilongjiang Yixue. 2003;27:823. [Google Scholar]
- 45.Wang XZ, Gao WJ, Fu JS, Wang CJ, Hou XS, Meng QY. Heller and fundoplication for the treatment of achalasia. Zhongguo Xiongxin Xueguan Waike Zazhi. 2005;12:295–296. [Google Scholar]
- 46.Lu SR. The treatment of achalasia with 56 patients. Jiangsu Daxue Xuebao (Yi Xue Ban) 2002;12:172. [Google Scholar]
- 47.Zhu X, Zhong MR, Li BM, Liu ZJ, Xu P, Yu GH. The clinical research of endoscopic balloon dilation for achalasia. Zhongguo Neijing Zazhi. 2007;13:193–196. [Google Scholar]
- 48.Chen X, Qiao XL. The evaluation of endoscopic balloon dilation for achalasia. Shanxi Yiyao Zazhi. 2003;32:46–48. [Google Scholar]
- 49.Wang QZ, Yan SJ, Wang JC, Li DP, Wang QW. The treatment of endoscopic balloon dilation for achalasia. Shiyong Quanke Yixue. 2007;15:668–669. [Google Scholar]
- 50.Han XW, Wu G, Xing GS, Ma B, Li TX, Liu BS, Shi J. The big balloon dilatation for the treatment of cardiac achalasia. Yixue Yingxiangxue Zazhi. 2004;14:226–228. [Google Scholar]
- 51.Yang HD, Song SM, Song XY. TV-assisted thoracoscopy Heller myotomy for the treatment of achalasia. Zhongguo Weichuang Waike Zazhi. 2007;7:543–544. [Google Scholar]
- 52.Huang YQ, Li XG, Liu J, Zhao H, Li Y, Wang J. TV-assisted thoracoscopy myotomy for the treatment of achalasia with 18 patients. Zhonghua Waike Zazhi. 2005;43:636–637. [Google Scholar]
- 53.Mikaeli J, Bishehsari F, Montazeri G, Mahdavinia M, Yaghoobi M, Darvish-Moghadam S, Farrokhi F, Shirani S, Estakhri A, Malekzadeh R. Injection of botulinum toxin before pneumatic dilatation in achalasia treatment: a randomized-controlled trial. Aliment Pharmacol Ther. 2006;24:983–989. doi: 10.1111/j.1365-2036.2006.03083.x. [DOI] [PubMed] [Google Scholar]
- 54.Omura N, Kashiwagi H, Ishibashi Y, Yano F, Tsuboi K, Kawasaki N, Suzuki Y, Yanaga K. Laparoscopic Heller myotomy and Dor fundoplication for the treatment of achalasia. Assessment in relation to morphologic type. Surg Endosc. 2006;20:210–213. doi: 10.1007/s00464-005-0365-5. [DOI] [PubMed] [Google Scholar]
- 55.Sharp KW, Khaitan L, Scholz S, Holzman MD, Richards WO. 100 consecutive minimally invasive Heller myotomies: lessons learned. Ann Surg. 2002;235:631–638; discussion 638-639. doi: 10.1097/00000658-200205000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bassotti G, D'Onofrio V, Battaglia E, Fiorella S, Dughera L, Iaquinto G, Mazzocchi A, Morelli A, Annese V. Treatment with botulinum toxin of octo-nonagerians with oesophageal achalasia: a two-year follow-up study. Aliment Pharmacol Ther. 2006;23:1615–1619. doi: 10.1111/j.1365-2036.2006.02907.x. [DOI] [PubMed] [Google Scholar]
- 57.Bonavina L. Minimally invasive surgery for esophageal achalasia. World J Gastroenterol. 2006;12:5921–5925. doi: 10.3748/wjg.v12.i37.5921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hunter JG, Trus TL, Branum GD, Waring JP. Laparoscopic Heller myotomy and fundoplication for achalasia. Ann Surg. 1997;225:655–664; discussion 664-665. doi: 10.1097/00000658-199706000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]


