Abstract
Alzheimer’s disease is the main cause of dementia in elderly people and is becoming an ever greater problem as societies worldwide age. Treatments that stop or at least effectively modify disease course do not yet exist. In Alzheimer’s disease, the conversion of the amyloid-β peptide (Aβ) from a physiological water-soluble monomeric form into neurotoxic oligomeric and fibrillar forms rich in stable β-sheet conformations is an important event. The most toxic forms of Aβ are thought to be oligomers, and dimers might be the smallest neurotoxic species. Numerous immunological approaches that prevent the conversion of the normal precursor protein into pathological forms or that accelerate clearance are in development. More than ten new approaches to active and passive immunotherapy are under investigation in clinical trials with the aim of producing safe methods for immunological therapy and prevention. A delicate balance between immunological clearance of an endogenous protein with acquired toxic properties and the induction of an autoimmune reaction must be found.
Introduction
Alzheimer’s disease is one of several disorders associated with conformational protein aggregations with overlap in pathological mechanism; others include prion, Parkinson’s, and Huntington’s diseases.1 The basic pathological mechanism in these disorders is a conformational change of a normally expressed protein. In the case of Alzheimer’s disease, both water-soluble amyloid-β peptides (Aβ) and tau proteins form β-sheet toxic forms. Deposits of Aβ form neuritic plaques and cerebral amyloid angiopathy, and hyperphosphorylated tau aggregates within neurons as paired helical filaments in neurofibrillary tangles.2
Aggregation and structural conversion occurs without changes to the amino-acid sequence of the proteins and results in a highly complex dynamic equilibrium of fibrillation intermediates in which early oligomeric species can act as seeds for fibrillation. Aβ is a 40–43 residue peptide that is a cleavage product of the amyloid precursor protein.3 Missense mutations in the gene encoding this protein, APP, or in the presenilin genes PRES1 and PRES2 can cause early-onset, familial forms of Alzheimer’s disease; however, the most common form of Alzheimer’s disease is sporadic and late-onset.
Derivatives of amyloid precursor protein, including water-soluble Aβ peptides, are present in most physiological fluids including plasma and CSF.1 In Alzheimer’s disease, aggregation of water-soluble, monomeric Aβ peptides into oligomeric forms is associated with conformational changes and neurotoxicity, including the impairment of long-term potentiation and accelerated formation of neurofibrillary tangles.1,4 Whether Aβ peptide aggregation into oligomers and deposited fibrils are steps in the same pathway or independent pathways is unknown.
Conformational change in soluble Aβ
Several proteins can promote the conformational transformation of disease-specific proteins and stabilise their abnormal structure; in Alzheimer’s disease, these include apolipoprotein E (APOE), especially its ε4 isoform,5 αl-antichymotrypsin,6 and C1q complement factor.7,8 These proteins greatly increase formation of Aβ fibrils from water-soluble Aβ.5,6 These pathological chaperone proteins have been found histologically and biochemically in association with fibrillar Aβ deposits9 but not in preamyloid aggregates, which are not associated with neuronal loss.10 An important event in the pathomechanism of Alzheimer’s disease is thought to be the reaching of a crucial concentration of water-soluble Aβ or chaperone proteins in the brain, at which point conformational change occurs, leading to formation of aggregates, initiating a neurodegenerative cascade. In sporadic Alzheimer’s disease, this crucial concentration might be reached because of any combination of age-associated overproduction of Aβ, impaired clearance from the brain, or influx of circulatory Aβ into the CNS .11
Aβ in familial and sporadic AD
Accumulation of toxic, aggregated forms of Aβ seem crucial in the pathogenesis of familial forms of Alzheimer’s disease.12 Some inherited forms are linked to mutations in APP, PRES1, or PRES2 that affect the processing of amyloid precursor protein, leading to overproduction of soluble Aβ or production of aggregation-prone forms, such as Aβ1–42.13 Down’s syndrome, in which there is an extra copy of APP because of trisomy 21, is associated with Alzheimer’s disease pathology at a very early age.14 In transgenic and other models of coexpressed Aβ and tau, Aβ oligomer formation precedes and accentuates tau-related pathology, which is consistent with the hypothesis that formation of neurofibrillary tangles is downstream of Aβ aggregation.15–17 In transgenic mouse models of mutant APP overexpression without tau pathology, therapeutic prevention or removal of Aβ is associated with cognitive benefits.18–21 Importantly, in transgenic mouse models of mutant APP and tau overexpression, prevention of Aβ pathology leads to amelioration of both cognitive deficits and tau-related pathology.22–24
Evidence linking Aβ to sporadic Alzheimer’s disease is less extensive. Many studies show a weak correlation between Aβ deposits and cognitive status,25 and some show that cognitively healthy elderly people can have substantial amyloid burden.26,27 Specific evidence for a central role of Aβ in sporadic disease includes an association between biochemically extracted Aβ peptides from brains of people with cognitive decline (by contrast with studies of histologically measured amyloid deposits).28 Furthermore, Aβ extracted from the brains of patients with sporadic disease induces amyloid deposits when injected into transgenic mice,29 and directly isolated Aβ dimers impair synaptic structure and function.31 Although the amyloid-cascade hypothesis is the dominant theory, some researchers suggest that Aβ accumulation is a marker for the presence of disease, rather than central to pathogenesis.25,31 The ultimate test of this theory will be when treatments that prevent or remove Aβ aggregates are fully tested in human beings.
Mechanisms of Aβ-directed immunomodulation
Vaccination was the first treatment approach to have genuine effect on the Alzheimer’s disease process, at least in animal models. Vaccination of transgenic mice with Aβ1–42 or an Aβ homologue and Freund’s adjuvant prevented Aβ deposition and, as a consequence, prevented behavioural impairments related to Aβ deposition.18–21,32,33 Peripheral injections of monoclonal antibodies against Aβ have similar effects on Aβ load and behaviour, indicating that the therapeutic effect of the vaccine is based primarily on the eliciting of a humoral response.34,35
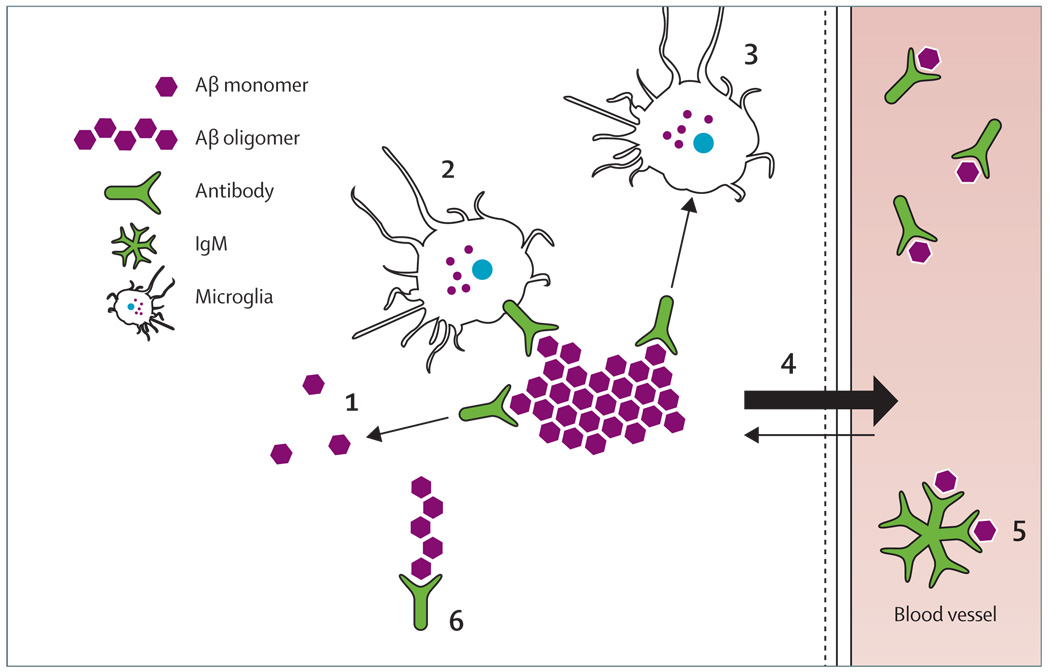
Aβ vaccination could elicit a humoral response by at least six possible mechanisms that are not mutually exclusive (figure).36–38 Aβ antibodies that are selective for specific conformations might target Aβ deposits in the brain leading to direct disassembly.39 Some antibodies are able to dissolve Aβ fibrils in vitro, preventing reassembly and inhibiting toxicity;40–42 in the brain, these antibodies might also activate microglia to clear plaques by eliciting Fc-mediated phagocytosis.34 The Fc portion of Aβ antibodies is not necessary for Aβ clearance, and APP transgenic mice crossed with FcRγ-chain knockout mice, which have complete impairment of phagocytosis of Aβ immune complexes via FcR, respond to vaccination in much the same way as FcR-sufficient mice.43 Furthermore, direct application of F(ab´)2 fragments of Aβ antibodies can clear amyloid deposits in vivo.44 These findings, along with observations of microglial activation after passive immunisation,45 suggest an Fc-independent mechanism of phagocytosis and degradation.38 The fourth mechanism by which antibodies could prevent Aβ deposition is the creation of a peripheral-sink effect, in which the removal of excess circulatory soluble Aβ draws soluble Aβ from the brain.19,32,35,46 The potential importance of this mechanism is illustrated by active immunisation experiments in which a non-toxic, non-fibrillogenic modified Aβ peptide was used with alum as an adjuvant that primarily stimulates a humoral immune response.32 This active immunisation protocol only elicited an IgM immune response to Aβ. Because of its larger size, IgM crosses the blood–brain barrier much less than does IgG, but vaccinated mice had both reduction of amyloid burden and cognitive improvement. These effects were presumably mediated mainly via a peripheral-sink mechanism. IgM might also function by hydrolysing Aβ. Antibodies might also neutralise neurotoxic oligomers.47
Figure 1. Potential mechanisms of immunomodulation for amyloid-β related pathology.
Direct disassembly of plaques by conformation-selective antibodies (1); antibody mediated activation of microglial cells (2); non-Fc mediated activation of microglia (3); creation of periferal sink by clearance of circulating amyloid β (4); IgM-mediated hydrolysis (5); neutralisation of oligomer toxicity (6). These mechanisms are not mutually exclusive. More than one mechanism could play a part at any give time, with different mechanisms potentially having a role at different stages of disease.
Aβ vaccination in human beings
Active immunisation
The striking biological effect of vaccination in preclinical testing and the apparent lack of side-effects in transgenic mice encouraged the launch of clinical trials with AN 1792, a vaccine that contained preaggregated Aβ1–42 and QS21. Because QS21 strongly induces Th1 lymphocytes, this vaccine design aimed to induce a strong cell-mediated immune response.48
The initial UK trial in 80 patients with mild to moderate Alzheimer’s disease49 was designed to assess the antigenicity and toxicity of multiple-dose immunisation. 53% of patients developed an anti-Aβ humoral response. During the later stages of the phase I trial, the emulsifier polysorbate 80 was added causing a shift from a predominantly Th2 response to a proinflammatory Thl response.50 In the subsequent phase II trial, 372 patients were enrolled, with 300 receiving the aggregated Aβ1–42 (AN1792) with QS21 in the polysorbate 80 formulation. This trial was stopped early when 18 (6%) of 298 of vaccinated patients had symptoms of acute meningoence phalitis.48,51,52
Autopsy investigations of a few participants showed clearance of parenchymal plaques, similar to that in the animal studies, confirming the validity of this approach for amyloid clearance in human beings.52–57 Extensive areas of cerebral cortex were devoid of plaques, with residual plaques having a “moth-eaten” appearance or lasting as “naked” dense cores. Amyloid clearance in most cases was associated with microglia that showed Aβ immunoreactivity, suggesting phagocytosis. Additional notable features were the persistence of amyloid in cerebral vessels and unaltered tau-immunoreactive neurofibrillary tangles and neuropil threads in regions of cerebral cortex where plaque clearance had apparently occurred.55–57 Some patients also had a deleterious T-cell reaction surrounding some cerebral vessels, suggestive of an excessive Th1 immune response.
Immune reaction triggered by AN1792 seemed to be a double-edge sword: the benefits of humoral response against Aβ were overshadowed in some individuals by a detrimental T-cell-mediated inflammatory response.52,58 Not all patients who received AN1792 responded with antibody production. Most had a humoral response, modest but statistically significant improvement on some cognitive testing scales compared with baseline, and a slowed rate of disease progression compared with patients who did not form antibodies.49,59 Follow-up data from the Zurich cohort, a subset of the AN1792 trial,59,60 indicate that the vaccination approach might be beneficial for patients with Alzheimer’s disease. And immune responders with high antibody titres in the multicentre cohort scored significantly better in composite scores of memory functions than did non-responders or patients who received placebo.50
Despite the apparent success in amyloid clearance indicated by autopsy data, clinical cognitive benefits in the active vaccination group compared with placebo were very modest.61 This finding could be related to the small decline in cognitive function in the placebo group,61,62 although a similar result in a vaccination study in dogs might suggest otherwise.63 Elderly dogs are a natural model of Aβ amyloidosis, because the canine APP protein sequence is about 98% similar to human APP. In a 2-year study, cortical Aβ immunoreactivity decreased by about 80% in most areas; however, this decline was not associated with any improvements in complex learning, spatial memory, or attention.63 As in the human data, maintenance of executive function was recorded in the dogs. These data suggest that active vaccination needs to start before the development of clinically significant Alzheimer’s disease-related pathology.
Persistence of tau-related pathology in cortical areas cleared of amyloid indicates that intervention might have been too late. This idea is supported by recent data from the follow-up of the 80 patients in the phase I AN1792 trial, eight of whom had an autopsy.62 Despite evidence of very significant amyloid plaque removal (which was related to antibody titre) in six patients, in the overall group there was no evidence of improved survival or lengthening of time to severe dementia.62 If immunisation begins early, Aβ-lowering might prevent formation of neurofibrillary tangles, which seems to be a result of AP-related toxicity,15,27 and thus vaccination could provide better cognitive benefits than it has in trials to date.
In transgenic mice, antibodies cleared both Aβ and early, but not late, forms of hyperphosphorylated tau aggregations.64 Therefore, Aβ immunotherapy could prevent formation of new tangles without affecting numbers or morphology of those already formed. Several trials of active human immunisation are underway (table).49,50,61,65
Table 1.
Current randomised, double-blind, parallel-assignment studies of immunotherapy in Alzheimer’s disease
| Phase | Intervention | Primaryoutcomes | Size | Duration | |
|---|---|---|---|---|---|
| Active immunisation | |||||
| NCT00498602 | Phase II | ACC-001+QS21 vs ACC-001 vs placebo | Safety, tolerability | 228 | Nov, 2007, to March, 2012 |
| NCT00411580 | Phase I | CAD106 | Safety, tolerability | 60 | June, 2005, to April, 2008 |
| NCT00464334 | Phase I | V950 | Safety | 70 | April, 2007, to Sept, 2011 |
| Passive immunisation | |||||
| NCT00575055 | Phase III | Bapineuzumab | Cognitive, functional | 800 | Dec, 2007, to Dec, 2010 |
| NCT00329082 | Phase II | LY2062430 | Safety, tolerability | 25 | May, 2006, to May, 2008 |
| NCT00299988 | Phase II | Intravenous immunoglobulin | ADAS-cog,ADAS-CGIC | 24 | Start Feb, 2006; ongoing but recruitment complete |
| NCT00455000 | Phase I | PF-04360365 | Safety, tolerability, pharmacokinetics | 36 | March, 2007, to June, 2008 |
| NCT00531804 | Phase I | R1450 | Adverse events, laboratory measures, vital signs | 80 | Dec, 2006, to Jan, 2009 |
ADAS-cog/CGIC=Alzheimer’s disease assessment score cognitive scale/clinician’s global impression of change.
The cause of toxicity in 6% of patients in the AN 1792 trial is unknown; however, cytotoxic T-cell reactions surrounding some cerebral vessels as seen at autopsy suggest an excessive Thl-mediated response.66 The likely involvement of excess cell-mediated response in toxicity was supported by analysis of participants’ peripheral-blood mononuclear cells. When stimulated in vitro with Aβ, cells from most participants who showed a response produced interleukin 2 and interferon γ indicative of a class II (CD4+) Th1-type response.50 Hence, a redesigned vaccine will need to avoid this cell-mediated response by avoiding stimulation of Th1 lymphocytes so that the vaccine could potentially elicit a purely humoral response; by using non-toxic and non-fibrillogenic Aβ homologous peptides, so that the immunogen does not produce direct toxicity; and by enhancing the peripheral-sink effect rather than central action.
Passive immunisation
Passive transfer of exogenous monoclonal Aβ antibodies seems the easiest way to provide antibodies without eliciting Th1-mediated autoimmunity. Transgenic mice treated this way had significant decreases in Aβ concentration and cognitive benefit.34,35 Major challenges of this approach are high costs, blood-brain barrier penetration, microhaemorrhage, off-target cross-reactivity, and loss of the antibody to a peripheral sink. Nevertheless, at least four clinical trials for passive immunisation with various approaches are underway (table).
The most advanced trial is of bapineuzumab: Elan/ Wyeth recently initiated a phase III trial and released preliminary analysis of the phase II results.67 The phase II trial was a randomised, double-blind, placebo-controlled trial testing three doses of a humanised Aβ antibody in 240 participants. In each of the escalating doses of the antibody, about 32 patients received active agent and 28 received placebo. Although the study did not attain statistical significance on the primary efficacy endpoints in the whole study population over the 18-month trial period, in the subgroup of participants who did not have the APOE ε4 allele clinically significant benefits were recorded on several scales, including the mini-mental state examination and the Alzheimer’s disease assessment scale battery. Furthermore, in the same subgroup, MRI showed less loss of brain volume in treated patients than in control patients. These findings suggest that this form of therapy might be effective. However, some patients in the treatment group, but not in the control group, had vasogenic oedema, a serious adverse event. In another study, intravenous immunoglobulin containing antibodies against Aβ affected Aβ plasma concentrations in patients,65 and this approach is undergoing further studies. Alternative approaches for passive immunisation less likely to be associated with toxicity include the use of Fv fragments or mimetics of the active antibody-binding site.68
Microhaemorrhage is a particular concern in studies of passive immunisation. The mechanism of microhaemorrhage is probably related to vascular amyloid deposits (congophilic amyloid angiopathy), which cause degeneration of smooth muscle cells and weakening of the blood-vessel wall. Congophilic amyloid angiopathy is present in nearly all patients with Alzheimer’s disease and is severe in about 20%.69 Furthermore, amyloid angiopathy is present in about 33% of cognitively healthy elderly control populations.70 Several reports have shown an increase in microhaemorrhages in mouse models of Alzheimer’s disease after passive intraperitoneal immunisation with different monoclonal antibodies with high affinity for Aβ plaques and congophilic amyloid angiopathy.71–73 Microhaemorrhages after active immunisation in a transgenic mouse model were noted in one study.74 In such models, Aβ antibodies both prevent the deposition of vascular amyloid and remove aggregates, thus contributing to vascular repair. However, early autopsies from the AN1792 trial indicated no clearance of vascular amyloid; one patient had numerous cortical bleeds, which are typically rare in patients with Alzheimer’s disease and might, therefore, have been related to immunisation.54 The need for vascular repair and regeneration during Aβ immunotherapy is another argument for early treatment and subtle clearance over a long time period.
Alternative strategies for vaccination
Understanding the antigenic profile of Aβ peptide allows engineering of modifications that favour a humoral response and reduce the potential for a Thl-mediated response. This approach has been termed altered peptide ligands. Computer models have predicted that Aβ1–42 has one major antibody-binding site located on its N-terminus and two major T-cell epitopes located at the central and C-terminal hydrophobic regions encompassing residues 17–21 and 29–42, respectively.75,76 Therefore, elimination or modification of these sites provides a double gain by eliminating toxicity and the potential for T-cell stimulation. Sigurdsson and colleagues32 immunised transgenic mice with K6Aβ1–30[E18E19], a non-toxic AP-homologous peptide in which the first T-cell epitope was modified and the second removed. Polyamino-acid chains coupled to its N-terminus were designed to increase the immunogenicity and solubility of the peptide. The mice produced mainly IgM class antibodies; IgG was absent or present at low titres and showed behavioural improvement and a partial clearance of Aβ deposits.32,33 One of the advantages of this design is that IgM, with a molecular weight of 900 kDa, penetrates the blood–brain barrier to a lesser degree than IgG and is therefore less likely to be associated with immune reaction in the brain. As with passive immunisation, this type of vaccine focuses its mechanism of action on the peripheral sink. Furthermore, the IgM response is reversible because it is T-cell independent; hence, memory T cells that could maintain the immune response are not generated. Therefore, this vaccination method might be safer than typical active immunisation.
Mucosal vaccination is an alternative way to achieve a primarily humoral response. This mechanism is based on the presence of lymphocytes in the mucosa of the nasal cavity and gastrointestinal tract. This type of response produces primarily secretory IgA antibodies, but when the antigen is coadministrated with adjuvants such as cholera toxin subunit B or heat-labile Escherichia coli enterotoxin, substantial serum IgG titres can be achieved.77,78 Immunisation of transgenic mice with Aβ as an antigen reduces amyloid burden.78,75 Mucosal immunisation is highly effective for prion infection.80 The great potential advantage of mucosal immunisation is a more limited humoral immune response with little or no cell-mediated immunity.
Another potentially attractive means to produce a robust humoral response that is mainly Th2 is with the use of DNA epitope vaccines.81 One such prototype vaccine that consisted of three copies of the B-cell epitope (Aβ1–11), a non-self Th-cell epitope (PADRE), and a macrophage-derived chemokine (MDC/CCL22) as an adjuvant to drive a Th2 response, is highly effective in a mouse model of Alzheimer’s disease.81 This type of technology has received substantial interest because of the ease of selectively designing these vaccines to elicit specific immune responses.
Stimulation of innate immunity rather than adaptive immune responses of T cells and B cells can produce an immune response to a self protein. Such stimulation can be achieved by direct activation of microglia via Toll-like receptors and might help avoid toxicity. Toll-like receptors are a family of innate immune mediators expressed by various immune and non-immune cells.82 Results of studies in prion diseases suggest that stimulation of Toll-like receptor 9 with CpG oligodeoxynucleotides is an attractive candidate for Alzheimer’s disease prevention and treatment.83,84 The potential therapeutic importance of the innate immune system to Aβ pathology is illustrated by reductions in the amyloid burden of up to 90% in transgenic mice in which the TGF-β-Smad2/3 signalling pathway was blocked in innate immune cells.85
Future directions
Numerous studies in animal models of Alzheimer’s disease suggest that vaccination can prevent the devastating effects of this prevalent disorder. However, a balance must be achieved between effective prevention and clearance of amyloid deposits and the induction of autoimmunity. Initial human trials of active vaccination did not achieve this balance, and a minority of patients developed encephalitis because of excessive Thl-cell responses. New active vaccines are being engineered to drive Th2 orTh3 responses or stimulate innate immunity. Apart from overcoming toxicity, effective vaccines need to provide greater benefit for cognition than those tested so far. This benefit is likely to rely on identification of preclinical amyloidosis with imaging techniques and other interventions, such as cognitive rehabilitation, that might restore neuronal health after removal of toxicity. With the multiple approaches to amyloid prevention in development, we believe that the near future will produce a final answer on whether the amyloid-cascade hypothesis is correct.
Search strategy and selection criteria.
References for this review were identified by searches of Pubmed from January 1972 to July 2008 with the terms “vaccine”, “vaccination”, “Alzheimer’s disease”, “immunomodulation”, “immunotherapy”, “clinical trials”, “amyloid”, and “amyloid β”. Only papers published in English were reviewed.
Acknowledgments
TW is supported by National Institutes of Health grants AG15408, AG20245, and AG008051, and the Alzheimer’s Disease Association. UK is supported by Swiss National Science Foundation grants 112616 and 51NF40-1U381. We thank Roger M Nitsch (University of Zurich, Switzerland, and director of Neurimmune Therapeutics AG) for his helpful review of this paper.
Footnotes
Both authors contributed to the data search and writing of the Review. TW wrote a draft and UK provided revisions.
Conflicts of interest
TW has no conflicts of interest. UK is co-author on a patent for the tissue amyloid plaque immunoreactivity (TAPIR) assay, held by the University of Zurich.
Contributor Information
Thomas Wisniewski, Department of Neurology, Department of Pathology, Department of Psychiatry, New York University School of Medicine, New York, NY, USA.
Uwe Konietzko, Division of Psychiatry Research, University of Zurich, Zurich, Switzerland.
References
- 1.Winklhofer KF, Tatzelt J, Haass C. The two faces of protein misfolding: gain-and loss-of-function in neurodegenerative diseases. EMBO J. 2008;27:336–349. doi: 10.1038/sj.emboj.7601930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blennow K, De Leon MJ, Zetterberg H. Alzheimer’s disease. Lancet. 2006;368:387–403. doi: 10.1016/S0140-6736(06)69113-7. [DOI] [PubMed] [Google Scholar]
- 3.Zheng H, Koo EH. The amyloid precursor protein: beyond amyloid. Mol Neurodegener. 2006;1:5. doi: 10.1186/1750-1326-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knobloch M, Farinelli M, Konietzko U, Nitsch RM, Mansuy IM. Abeta oligomer-mediated long-term potentiation impairment involves protein phosphatase 1-dependent mechanisms. J Neurosci. 2007;27:7648–7653. doi: 10.1523/JNEUROSCI.0395-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wisniewski T, Castaño EM, Golabek AA, Vogel T, Frangione B. Acceleration of Alzheimer’s fibril formation by apolipoprotein E in vitro. Am J Pathol. 1994;145:1030–1035. [PMC free article] [PubMed] [Google Scholar]
- 6.Ma J, Yee A, Brewer HB, Jr, Das S, Potter H. Amyloid-associated proteins alpha 1-antichymotrypsin and apolipoprotein E promote assembly of Alzheimer beta-protein into filaments. Nature. 1994;372:92–94. doi: 10.1038/372092a0. [DOI] [PubMed] [Google Scholar]
- 7.Johnson LV, Leitner WP, Rivest AJ, Staples MK, Radeke MJ, Anderson DH. The Alzheimer’s A beta-peptide is deposited at sites of complement activation in pathologic deposits associated with aging and age-related macular degeneration. Proc Natl Acad Sci USA. 2002;99:11830–11835. doi: 10.1073/pnas.192203399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boyett KW, DiCarlo G, Jantzen PT, et al. Increased fibrillar beta-amyloid in response to human Clq injections into hippocampus and cortex of APP+PS1 transgenic mice. Neurochem Pes. 2003;28:83–93. doi: 10.1023/a:1021600212829. [DOI] [PubMed] [Google Scholar]
- 9.Wisniewski T, Lalowski M, Golabek AA, Vogel T, Frangione B. Is Alzheimer’s disease an apolipoprotein E amyloidosis? Lancet. 1995;345:956–958. doi: 10.1016/s0140-6736(95)90701-7. [DOI] [PubMed] [Google Scholar]
- 10.Wisniewski HM, Sadowski M, Jakubowska-Sadowska K, Tamawski M, Wegiel J. Diffuse, lake-like amyloid-beta deposits in the parvopyramidal layer of the presubiculum in Alzheimer disease. j Neuropathol Exp Neurol. 1998;57:674–683. doi: 10.1097/00005072-199807000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Shibata M, Yamada S, Kumar S, et al. Clearance of Alzheimer’s amyloid-β 1–40 peptide from brain by LDL receptor-related protein-1 at the blood-brain barrier. J Clin Invest. 2000;106:1489–1499. doi: 10.1172/JCI10498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hardy J, Selkoe DJ. The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science. 2002;297:353–356. doi: 10.1126/science.1072994. [DOI] [PubMed] [Google Scholar]
- 13.Hardy J. A hundred years of Alzheimer’s disease research. Neuron. 2006;52:3–13. doi: 10.1016/j.neuron.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 14.Lemere CA, Blusztajn JK, Yamaguchi H, Wisniewski T, Saido TC, Selkoe DJ. Sequence of deposition of heterogeneous amyloid β-peptides and APO E in Down syndrome: implications for initial events in amyloid plaque formation. Neurobiol Dis. 1996;3:16–32. doi: 10.1006/nbdi.1996.0003. [DOI] [PubMed] [Google Scholar]
- 15.Gotz J, Chen F, van DJ, Nitsch RM. Formation of neurofibrillary tangles in P301l tau transgenic mice induced by Abeta 42 fibrils. Science. 2001;293:1491–1495. doi: 10.1126/science.1062097. [DOI] [PubMed] [Google Scholar]
- 16.Oddo S, Caccamo A, Shepherd JD, et al. Triple-transgenic model of Alzheimer’s disease with plaques and tangles: intracellular Abeta and synaptic dysfunction. Neuron. 2003;39:409–421. doi: 10.1016/s0896-6273(03)00434-3. [DOI] [PubMed] [Google Scholar]
- 17.King ME, Kan HM, Baas PW, Erisir A, Glabe CG, Bloom GS. Tau-dependent microtubule disassembly initiated by prefibrillar beta-amyloid. J Cell Biol. 2006;175:541–546. doi: 10.1083/jcb.200605187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schenk D, Barbour R, Dunn W, et al. Immunization with amyloid-β attenuates Alzheimer disease-like pathology in the PDAPP mice. Nature. 1999;400:173–177. doi: 10.1038/22124. [DOI] [PubMed] [Google Scholar]
- 19.Sigurdsson EM, Scholtzova H, Mehta P, Frangione B, Wisniewski T. Immunization with a non-toxic/non-fibrillar amyloid-β homologous peptide reduces Alzheimer’s disease associated pathology in transgenic mice. Am J Pathol. 2001;159:439–447. doi: 10.1016/s0002-9440(10)61715-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morgan D, Diamond DM, Gottschall PE, et al. Aβ peptide vaccination prevents memory loss in an animal model of Alzheimer’s disease. Nature. 2001;408:982–985. doi: 10.1038/35050116. [DOI] [PubMed] [Google Scholar]
- 21.Janus C, Pearson J, McLaurin J, et al. Aβ peptide immunization reduces behavioural impairment and plaques in a model of Alzheimer’s disease. Nature. 2000;408:979–982. doi: 10.1038/35050110. [DOI] [PubMed] [Google Scholar]
- 22.Oddo S, Caccamo A, Tran L, et al. Temporal profile of amyloid-beta (Abeta) oligomerization in an in vivo model of Alzheimer disease: a link between Abeta and tau pathology. J Biol Chem. 2006;281:1599–1604. doi: 10.1074/jbc.M507892200. [DOI] [PubMed] [Google Scholar]
- 23.Blurton-Jones M, LaFerla FM. Pathways by which Abeta facilitates tau pathology. Curr Alzheimer Res. 2006;3:437–448. doi: 10.2174/156720506779025242. [DOI] [PubMed] [Google Scholar]
- 24.McKee AC, Carreras I, Hossain L, et al. Ibuprofen reduces Abeta, hyperphosphorylated tau and memory deficits in Alzheimer mice. Brain Res. 2008;1207:225–236. doi: 10.1016/j.brainres.2008.01.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Castellani RJ, Lee HG, Zhu X, Perry G, Smith MA. Alzheimer disease pathology as a host response. J Neuropathol Exp Neurol. 2008;67:523–531. doi: 10.1097/NEN.0b013e318177eaf4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Crystal HA, Dickson DW, Sliwinski MJ, et al. Pathological markers associated with normal aging and dementia in the elderly. Ann Neurol. 1993;34:566–573. doi: 10.1002/ana.410340410. [DOI] [PubMed] [Google Scholar]
- 27.Knopman DS, Parisi JE, Salviati A, et al. Neuropathology of cognitively normal elderly. J Neuropathol Exp Neurol. 2003;62:1087–1095. doi: 10.1093/jnen/62.11.1087. [DOI] [PubMed] [Google Scholar]
- 28.Naslund J, Haroutunian V, Mohs R, et al. Correlation between elevated levels of amyloid beta-peptide in the brain and cognitive decline. JAMA. 2000;283:1571–1577. doi: 10.1001/jama.283.12.1571. [DOI] [PubMed] [Google Scholar]
- 29.Meyer-Luehmann M, Coomaraswamy J, Bolmont T, et al. Exogenous induction of cerebral beta-amyloidogenesis is governed by agent and host. Science. 2006;313:1781–1784. doi: 10.1126/science.1131864. [DOI] [PubMed] [Google Scholar]
- 30.Shankar GM, Li S, Mehta TH, et al. Amyloid-beta protein dimers isolated directly from Alzheimer’s brains impair synaptic plasticity and memory. Nat Med. 2008 doi: 10.1038/nm1782. published online June 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shioi J, Georgakopoulos A, Mehta P, et al. FAD mutants unable to increase neurotoxic Abeta 42 suggest that mutation effects on neurodegeneration may be independent of effects on Abeta. j Neurochem. 2007;101:674–681. doi: 10.1111/j.1471-4159.2006.04391.x. [DOI] [PubMed] [Google Scholar]
- 32.Sigurdsson EM, Knudsen EL, Asuni A, et al. An attenuated immune response is sufficient to enhance cognition in an Alzheimer’s disease mouse model immunized with amyloid-β derivatives. J Neurosci. 2004;24:6277–6282. doi: 10.1523/JNEUROSCI.1344-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Asuni A, Boutajangout A, Scholtzova H, et al. Aβ derivative vaccination in alum adjuvant prevents amyloid deposition and does not cause brain microhemorrhages in Alzheimer’s model mice. Eur J Neurosci. 2006;24:2530–2542. doi: 10.1111/j.1460-9568.2006.05149.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bard F, Cannon C, Barbour R, et al. Peripherally administered antibodies against amyloid beta-peptide enter the central nervous system and reduce pathology in a mouse model of alzheimer disease. Nat Med. 2000;6:916–919. doi: 10.1038/78682. [DOI] [PubMed] [Google Scholar]
- 35.DeMattos RB, Bales KR, Cummins DJ, Dodart JC, Paul SM, Holtzman DM. Peripheral anti-A beta antibody alters CNS and plasma A beta clearance and decreases brain A beta burden in a mouse model of Alzheimer’s disease. Proc Natl Acad Sci USA. 2001;98:8850–8855. doi: 10.1073/pnas.151261398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Golde TE. Disease modifying therapy for AD? J Neurochem. 2006;99:689–707. doi: 10.1111/j.1471-4159.2006.04211.x. [DOI] [PubMed] [Google Scholar]
- 37.Kennedy GJ, Golde TE, Tariot PN, Cummings JL. Amyloid-Based interventions in Alzheimer’s disease. CNS Spectr. 2007;12 12 suppl 1:1–14. [Google Scholar]
- 38.Bolmont T, Clavaguera F, Meyer-Luehmann M, et al. Induction of tau pathology by intracerebral infusion of amyloid-beta-containing brain extract and by amyloid-beta deposition in APP x Tau transgenic mice. Am J Pathol. 2007;171:2012–2020. doi: 10.2353/ajpath.2007.070403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bacskai BJ, Kajdasz ST, Christie RH, et al. Imaging of amyloid-β deposits in brains of living mice permits direct observation of clearance of plaques with immunotherapy. Nat Med. 2001;7:369–372. doi: 10.1038/85525. [DOI] [PubMed] [Google Scholar]
- 40.Solomon B, Koppel R, Hanan E, Katzav T. Monoclonal antibodies inhibit in vitro fibrillar aggregation of the Alzheimer β-amyloid peptide. Proc Natl Acad Sci USA. 1996;93:452–455. doi: 10.1073/pnas.93.1.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Solomon B, Koppel R, Frankel D, Hanan-Aharon E. Disaggregation of Alzheimer beta-amyloid by site-directed mAb. Proc Natl Acad Sci USA. 1997;94:4109–4112. doi: 10.1073/pnas.94.8.4109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Frenkel D, Solomon B, Benhar I. Modulation of Alzheimer’s beta-amyloid neurotoxicity by site-directed single-chain antibody. J Neuroimmunol. 2000;106:23–31. doi: 10.1016/s0165-5728(99)00232-5. [DOI] [PubMed] [Google Scholar]
- 43.Das P, Howard V, Loosbrock N, Dickson D, Murphy MP, Golde TE. Amyloid-beta immunization effectively reduces amyloid deposition in FcRgamma-J-knock-out mice. J Neurosci. 2003;23:8532–8538. doi: 10.1523/JNEUROSCI.23-24-08532.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bacskai BJ, Kajdasz ST, McLellan ME, et al. Non-Fc-mediated mechanisms are involved in clearance of amyloid-beta in vivo by immunotherapy. J Neurosci. 2002;22:7873–7878. doi: 10.1523/JNEUROSCI.22-18-07873.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wilcock DM, Rojiani A, Rosenthal A, et al. Passive amyloid immunotherapy clears amyloid and transiently activates microglia in a transgenic mouse model of amyloid deposition. J Neurosci. 2004;24:6144–6151. doi: 10.1523/JNEUROSCI.1090-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sigurdsson EM, Wisniewski T, Frangione B. A safer vaccine for Alzheimer’s disease? Neurobiol Aging. 2002;23:1001–1008. doi: 10.1016/s0197-4580(02)00124-0. [DOI] [PubMed] [Google Scholar]
- 47.Brody DL, Holtzman DM. Active and passive immunotherapy for neurodegenerative diseass. Annu Rev Neurosci. 2008;31:175–193. doi: 10.1146/annurev.neuro.31.060407.125529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wisniewski T, Frangione B. Immunological and anti-chaperone therapeutic approaches for Alzheimer’s disease. Brain Pathol. 2005;15:72–77. doi: 10.1111/j.1750-3639.2005.tb00102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bayer AJ, Bullock R, Jones RW, et al. Evaluation of the safety and immunogenicity of synthetic Aβ42 (AN 1792) in patients with AD. Neurology. 2005;64:94–101. doi: 10.1212/01.WNL.0000148604.77591.67. [DOI] [PubMed] [Google Scholar]
- 50.Pride M, Seubert P, Grundman M, Hagen M, Eldridge J, Black RS. Progress in the active immunofherapeutic approach to Alzheimer’s disease: clinical investigations into AN1792-associated meningoencephalitis. Neurodegener Dis. 2008;5:194–196. doi: 10.1159/000113700. [DOI] [PubMed] [Google Scholar]
- 51.Wisniewski T. Practice point commentary on “Clinical effects of Aβ immunization (AN 1792) in patients with AD in an interupted trial“. Nat Clin Proc Neurol. 2005;1:84–85. [Google Scholar]
- 52.Boche D, Nicoll JA. The role of the immune system in clearance of Abeta from the brain. Brain Pathol. 2008;18:267–278. doi: 10.1111/j.1750-3639.2008.00134.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bombois S, Maurage CA, Compel M, et al. Absence of beta-amyloid deposits after immunization in Alzheimer disease with Lewy body dementia. Arch Neurol. 2007;64:583–587. doi: 10.1001/archneur.64.4.583. [DOI] [PubMed] [Google Scholar]
- 54.Ferrer I, Boada RM, Sanchez Guerra ML, Rey MJ, Costa-Jussa F. Neuropathology and pathogenesis of encephalitis following amyloid-beta immunization in Alzheimer’s disease. Brain Pathol. 2004;14:11–20. doi: 10.1111/j.1750-3639.2004.tb00493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Masliah E, Hansen L, Adame A, et al. Aβ vaccination effects on plaque pathology in the absence of encephalitis in Alzheimer disease. Neurology. 2005;64:129–131. doi: 10.1212/01.WNL.0000148590.39911.DF. [DOI] [PubMed] [Google Scholar]
- 56.Nicoll JA, Wilkinson D, Holmes C, Steart P, Markham H, Weller RO. Neuropathology of human Alzheimer disease after immunization with amyloid-beta peptide: a case report. Nat Med. 2005;9:448–452. doi: 10.1038/nm840. [DOI] [PubMed] [Google Scholar]
- 57.Nicoll JA, Barton E, Boche D, et al. Abeta species removal after abeta42 immunization. J Neuropathol Exp Neurol. 2006;65:1040–1048. doi: 10.1097/01.jnen.0000240466.10758.ce. [DOI] [PubMed] [Google Scholar]
- 58.Sadowski M, Wisniewski T. Disease modifying approaches for Alzheimer’s pathology. Current Pharmaceutic Design. 2007;13:1943–1954. doi: 10.2174/138161207781039788. [DOI] [PubMed] [Google Scholar]
- 59.Hock C, Konietzko U, Straffer JR, et al. Antibodies against β-amyloid slow cognitive decline in Alzheimer’s disease. Neuron. 2003;38:547–554. doi: 10.1016/s0896-6273(03)00294-0. [DOI] [PubMed] [Google Scholar]
- 60.Hock C, Konietzko U, Paspassotiropoulos A, et al. Generation of antibodies specific for β-amyloid by vaccination of patients with Alzheimer disease. Nat Med. 2002;8:1270–1276. doi: 10.1038/nm783. [DOI] [PubMed] [Google Scholar]
- 61.Gilman S, Roller M, Black RS, et al. Clinical effects of Aβ immunization (AN1792) in patients with AD in an interupted trial. Neurology. 2005;64:1553–1562. doi: 10.1212/01.WNL.0000159740.16984.3C. [DOI] [PubMed] [Google Scholar]
- 62.Holmes C, Boche D, Wilkinson D, et al. Long-term effects of Aβ42 immunisation in Alzheimer’s disease: follow-up of a randomised, placebo-controlled phase I trial. Lancet. 2008;372:216–223. doi: 10.1016/S0140-6736(08)61075-2. [DOI] [PubMed] [Google Scholar]
- 63.Head E, Pop V, Vasilevko V, et al. A two-year study with fibrillar beta-amyloid (Abeta) immunization in aged canines: effects on cognitive function and brain Abeta. J Neurosci. 2008;28:3555–3566. doi: 10.1523/JNEUROSCI.0208-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Oddo S, Billings L, Kesslak JP, Cribbs DH, LaFerla FM. Abeta immunotherapy leads to clearance of early but not late, hyperphosphorylated tau aggregates via the proteasome. Neuron. 2004;43:321–332. doi: 10.1016/j.neuron.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 65.Relkin NR, Szabo P, Adamiak B, et al. 18-Month study of intravenous immunoglobulin for treatment of mild Alzheimer disease. Neurobiol Aging. 2008 doi: 10.1016/j.neurobiolaging.2007.12.021. published online Feb 20. [DOI] [PubMed] [Google Scholar]
- 66.Robinson SR, Bishop GM, Lee HG, Munch G. Lessons from the AN 1792 Alzheimer vaccine: lest we forget. Neurobiol Aging. 2004;25:609–615. doi: 10.1016/j.neurobiolaging.2003.12.020. [DOI] [PubMed] [Google Scholar]
- 67.Wyeth. [accessed July 23, 2008];Elan and Wyeth announce encouraging top-line results from phase 2 clinical trial of bapineuzumab for Alzheimer’s disease. http://wyeth.com/news?nav=display&navTo=/wyeth_html/home/news/pressreleases/2008/1213683456273.html.
- 68.Solomon B. Antibody-mediated immunotherapy for Alzheimer’s disease. Curr Opin Inveslig Drugs. 2007;8:519–524. [PubMed] [Google Scholar]
- 69.Jellinger KA. Alzheimer disease and cerebrovascular pathology: an update. J Neural Transm. 2002;109:813–836. doi: 10.1007/s007020200068. [DOI] [PubMed] [Google Scholar]
- 70.Zhang-Nunes SX, Maat-Schieman ML, Van Duinen SG, Roos RA, Frosch MP, Greenberg SM. The cerebral beta-amyloid angiopathies: hereditary and sporadic. Brain Pathol. 2006;16:30–39. doi: 10.1111/j.1750-3639.2006.tb00559.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pfeifer M, Boncristiano S, Bondolfi L, et al. Cerebral hemorrhage after passive anti-Aβ immunotherapy. Science. 2002;298:1379. doi: 10.1126/science.1078259. [DOI] [PubMed] [Google Scholar]
- 72.Wilcock DM, Rojiani A, Rosenthal A, et al. Passive immunization against Abeta in aged APP-transgenic mice reverses cognitive deficits and depletes parenchymal amyloid deposits in spite of increased vascular amyloid and microhemorrhage. JNeuroinfiammation. 2004;1:24. doi: 10.1186/1742-2094-1-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Racke MM, Boone LI, Hepburn DL, et al. Exacerbation of cerebral amyloid angiopathy-associated microhemorrhages in amyloid precursor protein transgenic mice by immunotherapy is dependent on antibody recognition of deposited forms of amyoid beta. J Neurosci. 2005;25:629–636. doi: 10.1523/JNEUROSCI.4337-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wilcock DM, Jantzen PT, Li Q, Morgan D, Gordon MN. Amyloid-beta vaccination, but not nitro-nonsteroidal anti-inflammatory drug treatment, increases vascular amyloid and microhemorrhage while both reduce parenchymal amyloid. Neuroscience. 2007;144:950–960. doi: 10.1016/j.neuroscience.2006.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Singh H, Raghava GP. ProPred: prediction of HLA-DR binding sites. Bioinformatics. 2001;17:1236–1237. doi: 10.1093/bioinformatics/17.12.1236. [DOI] [PubMed] [Google Scholar]
- 76.Singh H, Raghava GP. ProPredl: prediction of promiscuous MHC class-I binding sites. Bioinformatics. 2003;19:1009–1014. doi: 10.1093/bioinformatics/btg108. [DOI] [PubMed] [Google Scholar]
- 77.Lemere CA, Maron R, Selkoe DJ, Weiner HL. Nasal vaccination with beta-amyloid peptide for the treatment of Alzheimer’s disease. DNA Cell Biol. 2001;20:705–711. doi: 10.1089/10445490152717569. [DOI] [PubMed] [Google Scholar]
- 78.Zhang J, Wu X, Qin C, et al. A novel recombinant adeno-associated virus vaccine reduces behavioral impairment and beta-amyloid plaques in a mouse model of Alzheimer’s disease. Neurobiol Dis. 2003;14:365–379. doi: 10.1016/j.nbd.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 79.Weiner HL, Lemere CA, Maron R, et al. Nasal administration of amyloid-β peptide decreases cerebral amyloid burden in a mouse model of Alzheimer’s disease. Ann Neurol. 2000;48:567–579. [PubMed] [Google Scholar]
- 80.Goni F, Chabalgoity JA, Prelli F, et al. High titers of mucosal and systemic anti-PrP antibodies abrogates oral prion infection in mucosal vaccinated mice. Neuroscience. 2008;153:679–686. doi: 10.1016/j.neuroscience.2008.02.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Movsesyan N, Ghochikyan A, Mkrtichyan M, et al. Reducing AD-like pathology in 3xTg-AD mouse model by DNA epitope vaccine - a novel immunothapeutic strategy. PLoS ONE. 2008;3:e2124. doi: 10.1371/journal.pone.0002124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Crack PJ, Bray PJ. Toll-like receptors in the brain and their potential roles in neuropathology. Immunol Cell Biol. 2007;85:476–480. doi: 10.1038/sj.icb.7100103. [DOI] [PubMed] [Google Scholar]
- 83.Spinner DS, Kascsak RB, LaFauci G, et al. CpG oligodeoxynucleotide-enhanced humoral immune response and production of antibodies to prion protein PrPSc in mice immunized with 139A scrapie-associated fibrils. J Leukoc Biol. 2007;14:36–43. doi: 10.1189/jlb.1106665. [DOI] [PubMed] [Google Scholar]
- 84.Rosset MB, Ballerini C, Gregoire S, Metharom P, Carnaud C, Aucouturier P. Breaking immune tolerance to the prion protein using prion protein peptides plus oligodeoxynucleotide-CpG in mice. J Immunol. 2004;172:5168–5174. doi: 10.4049/jimmunol.172.9.5168. [DOI] [PubMed] [Google Scholar]
- 85.Town T, Laouar Y, Pittenger C, et al. Blocking TGF-beta-Smad2/3 innate immune signaling mitigates Alzheimer-like pathology. Nat Med. 2008;14:681–687. doi: 10.1038/nm1781. [DOI] [PMC free article] [PubMed] [Google Scholar]