Abstract
Background
US black and Hispanic populations are growing at a steady pace. In contrast, the medical profession lacks the same minority growth and representation. Women are also under-represented in many surgical disciplines. The purpose of this study was to assess trends in the proportion of women, blacks and Hispanics admitted to vascular surgery (VS) and related specialties, and to compare them to each other and to a surgical specialty, orthopedic surgery (OS), with a formal diversity initiative.
Methods
Data on the fellowship pool of VS, interventional radiology (IR), and interventional cardiology (IC), as well as the resident pools of general surgery (GS) and orthopedic surgery (OS) were obtained from US graduate medical education reports for 1999 through 2005. Cochrane-Armitage trend tests were used to assess trends in the proportion of females, blacks and Hispanics in relation to the total physician workforce for each subspecialty.
Results
No significant trends in the proportion of females, blacks or Hispanics accepted into VS and IC fellowship programs occurred during the study period. In contrast, IR, GS, and OS programs revealed significant trends for increasing proportions of at least one of the underrepresented study groups. In particular, OS, which has implemented a diversity awareness program, showed a positive trend in female and Hispanic trainees (P < .04 and P <.02, respectively). Blacks showed a significant increasing trend only in IR (P =.05). Conversely, a positive trend toward continued growth in the Hispanic group was seen in GS (P <.001), IR and OS (P =.04 and P =0.02, respectively).
Conclusions
The racial/ethnic and gender composition of the physician trainee pool in vascular specialties, particularly VS, has not matched the increasing growth of underrepresented groups in the US population of patients with vascular disease. Formal programs to recruit qualified women and minorities appear successful in increasing workforce diversity.
Under-represented racial and ethnic groups are growing at a steady pace in the United States. According to the US census, the Hispanic population that now constitutes 15% of the US population increased by 57.9% between 1990 and 2000, compared with an increase of 13.2% of the total U.S. population.1 Similarly, the proportion of African-Americans has increased to 12%, albeit at a slower rate. These numbers are expected to climb dramatically in the next 50 years, with Hispanics representing almost a quarter of the US population.
Health disparities associated with race and ethnicity have been reported for several conditions, including vascular disease. Selvin et al2 in their observational study confirmed earlier findings of a higher prevalence of peripheral arterial disease (PAD) among blacks, up to 3 times as high as in non-Hispanic whites. Moreover, blacks are estimated to have a higher rate of primary amputation and less limb-salvaging procedures, likely related to poor access to health care.3. Similar findings were reported by Morrissey et al4 for Hispanics, who were also found to have higher amputation rates after lower extremity revascularization
The ethnic and racial composition of the physician workforce does not match the diversity of the US population. This may be particularly true for physicians treating vascular disorders. Most vascular patients from minority groups seeking care are, therefore, not able to find assistance from vascular physicians with their same ethnic or racial background. Similarly, women who comprise a little over 50% of the US general population,1 see a wide disparity in the gender distribution of vascular specialists, with men still making up most of the physician pool.
Some surgical subspecialties have made efforts to improve female and minority representation, including targeting medical students and implementing cultural awareness programs.5-8 In 1996-2004, levels of gender and racial diversity in the entire ACGME-resident workforce increased.6 Moreover, the number of underrepresented groupsentering the medical field sharply rose. Changes in work hours and the evolution of endovascular techniques have resulted in a rise in the number of applicants for vascular surgery (VS) fellowships, particularly in the past three years.9 Nevertheless, the VS applicant pool has suffered a small, but steady decline in quality. Thus, strategies implemented by the Society for Vascular Surgery (SVS) have been developed to attract more talented medical school and residency graduates.10 It is unknown, however, to what extent gender and ethnic diversity has changed in VS and other related specialties. The purpose of this study was to assess trends in the proportion of women and minorities in VS training programs and related specialties and to compare them to general surgery (GS) and, particularly, orthopedic surgery (OS), a surgical specialty with a formal diversity initiative.
METHODS
The study population consisted of the resident physicians and fellows enrolled in selected specialty and subspecialty programs accredited by the Accreditation Council for Graduate Medical Education (ACGME) and in combined specialty Graduate Medical Education (GME) programs for the years 1999 to 2005. The selected programs included VS, Interventional Radiology (IR), Interventional Cardiology (IC), GS, and OS. The number of on-duty fellows and residents for the above mentioned specialties was obtained from reports on data from the National Graduate Medical Education Census and from a database of training programs accredited by the ACGME, which are sponsored and administered by the American Medical Association and the Association of American Medical Colleges (AAMC).11-17 Each year the database is updated by adding to it the new residents who match into programs through the National Resident Matching Program (NRMP) as well as from information collected through the AAMC's follow-up report of medical schools. Data on gender and race/ethnicity of the residents and fellows are available on the database. Race and ethnicity were defined according with the classification used by the US Census Bureau.1 Ethnic origin was defined as Hispanic or Non-Hispanic. The racial categories included black, American Indian/Alaskan Native, White, Asian, Native Hawaiian/Pacific Islander, and other/unknown. For the purpose of the study, two minority racial/ethnic groups, blacks and Hispanics, were included in the analyses since these are the largest racial/ethnic minority groups in the United States. The proportion of female trainees, as well as the proportion of blacks and Hispanics for each specialty was calculated by dividing the number of trainees in each specific gender or racial/ethnic category by the total number of trainees in the respective specialty each year. Proportions, expressed as percentages, were analyzed over the seven-year period as trends within each specialty training program and compared between the programs. In addition, the proportion of females, blacks and Hispanics in vascular surgery within each study year were compared to the proportions in other vascular subspecialties, including IR and IC. Trends in VS were further compared with those seen in OS.
Table analyses using Chi-square or Fisher's exact tests were conducted as appropriate to assess differences in the proportions of women, blacks, and Hispanics across the specialties. The Cochrane-Armitage trend test was used to assess trends in the proportion of gender and racial/ethnic minorities in relation to the total physician workforce for each subspecialty over time. A P value of less than .05 was considered statistically significant. All analyses were performed with SAS 9.1 (SAS Institute, Cary, NC) and MedCalc 8.1.0.0 for Windows (MedCalc Software, Mariakerke, Belgium).
Table.
Proportions of Women, Black, and Hispanic Residents/Fellows in the Accreditation Council on Graduate Medical Education-Res by Specialty, 1999-2005
| SPECIALITY | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Vascular surgery | ||||||||||||||||
| Total | 145 | 138 | 139 | 128 | 166 | 178 | 173 | 1067 | ||||||||
| Women | 20 | 13.8 | 18 | 13.0 | 14 | 10.1 | 19 | 14.8 | 17 | 10.2 | 30 | 16.9 | 29 | 16.8 | 147 | 13.8 |
| Blacks | 5 | 3.4 | 8 | 5.8 | 4 | 2.9 | 7 | 5.5 | 5 | 3.0 | 9 | 5.1 | 8 | 4.6 | 46 | 4.3 |
| Hispanics | 6 | 4.1 | 7 | 5.1 | 7 | 5.0 | 9 | 7.0 | 10 | 6.0 | 6 | 3.4 | 10 | 5.8 | 55 | 5.2 |
| General surgery | ||||||||||||||||
| Total | 7748 | 7548 | 7484 | 7412 | 7623 | 7689 | 7628 | 53132 | ||||||||
| Women | 1640 | 21.2 | 1706 | 22.6 | 1777 | 23.7 | 1853 | 25.0 | 1939 | 25.4 | 2053 | 26.7 | 2130 | 27.9 | 13098 | 24.7 |
| Blacks | 429 | 5.5 | 484 | 6.4 | 494 | 6.6 | 460 | 6.2 | 435 | 5.7 | 449 | 5.8 | 409 | 5.4 | 3160 | 5.9 |
| Hispanics | 360 | 4.6 | 413 | 5.5 | 470 | 6.3 | 486 | 6.6 | 528 | 6.9 | 492 | 6.4 | 467 | 6.1 | 3216 | 6.1 |
| Interventional Radiology | ||||||||||||||||
| Total | 185 | 134 | 129 | 128 | 118 | 109 | 108 | 911 | ||||||||
| Women | 12 | 6.5 | 9 | 6.7 | 13 | 10.1 | 15 | 11.7 | 6 | 5.1 | 6 | 5.5 | 11 | 10.2 | 72 | 7.9 |
| Blacks | 5 | 2.7 | 2 | 1.5 | 4 | 3.1 | 4 | 3.1 | 8 | 6.8 | 6 | 5.5 | 5 | 4.6 | 34 | 3.7 |
| Hispanics | 5 | 2.7 | 2 | 1.5 | 14 | 10.9 | 13 | 10.2 | 9 | 7.6 | 6 | 5.5 | 8 | 7.4 | 57 | 6.3 |
| Interventional Cardiology | ||||||||||||||||
| Total | 68 | 77 | 114 | 121 | 166 | 206 | 203 | 955 | ||||||||
| Women | 3 | 4.4 | 3 | 3.9 | 6 | 5.3 | 8 | 6.6 | 8 | 4.8 | 18 | 8.7 | 17 | 8.4 | 63 | 6.6 |
| Blacks | 1 | 1.5 | 3 | 3.9 | 2 | 1.8 | 3 | 2.5 | 4 | 2.4 | 5 | 2.4 | 2 | 1.0 | 20 | 2.1 |
| Hispanics | 4 | 5.9 | 7 | 9.1 | 6 | 5.3 | 5 | 4.1 | 10 | 6.0 | 11 | 5.3 | 14 | 6.9 | 57 | 6.0 |
| Orthopedic surgery | ||||||||||||||||
| Total | 2744 | 2915 | 2955 | 3002 | 3024 | 3085 | 3151 | 20876 | ||||||||
| Women | 401 | 14.6 | 235 | 8.1 | 265 | 9.0 | 271 | 9.0 | 285 | 9.4 | 303 | 9.8 | 346 | 11.0 | 2106 | 10.1 |
| Blacks | 101 | 3.7 | 139 | 4.8 | 132 | 4.5 | 118 | 3.9 | 120 | 4.0 | 116 | 3.8 | 119 | 3.8 | 845 | 4.0 |
| Hispanics | 66 | 2.4 | 84 | 2.9 | 107 | 3.6 | 109 | 3.6 | 116 | 3.8 | 111 | 3.6 | 103 | 3.3 | 696 | 3.3 |
RESULTS
The annual numbers and percentages of female, black, and Hispanic residents and fellows for VS, GS, IR, IC, and OS for the years 1999 to 2005 are detailed in the Table. The proportion of female trainees was significantly lower than the proportion of male trainees in all the specialties across the study period (P<.001). On average, the specialty with the higher proportion of women was GS (24.7%), followed by VS (13.8%), and OS (10.1%).Hispanic and black trainees represented, on average, 3.3% - 6.3% and 1% - 5.9%, respectively, of the resident/fellow workforce in each vascular and surgery specialty.
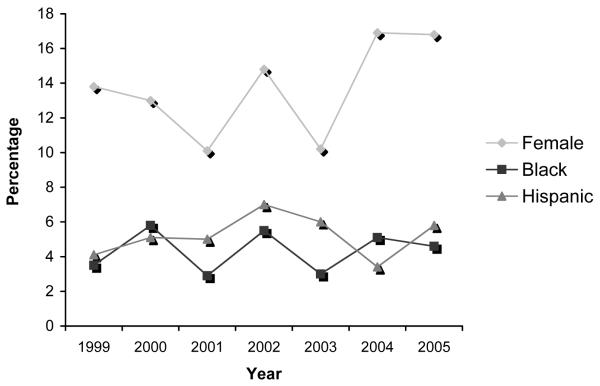
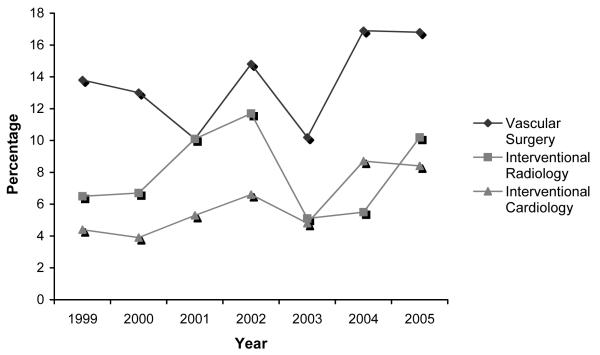
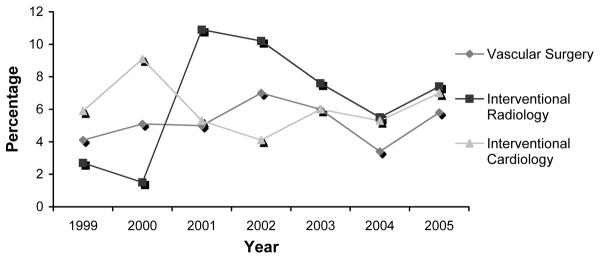
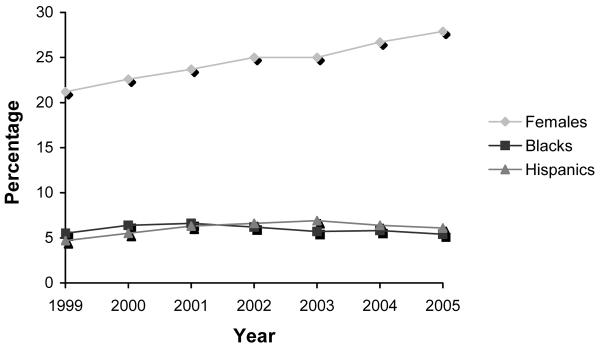
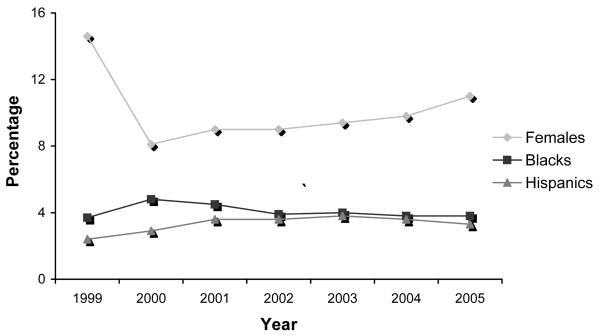
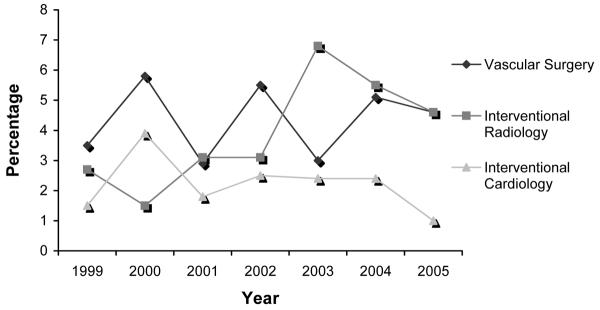
No significant trends in the proportion of women, blacks, or Hispanics enrolled in VS fellowship programs occurred over the seven-year period (P for trend, 0.2, 0.7, and 0.8, respectively) (Fig 1). Similarly, non-significant trends were observed for IC (P for trend, 0.06, 0.46, and 0.9, for women, blacks, and Hispanics, respectively) (Figs. 3-5). Conversely, the proportion of women enrolled in GS increased significantly over the seven-year study period (P for trend, <.001), and although the number of women enrolled in OS programs decreased from 1999 to 2000, their proportion increased significantly between 2000 and 2005 (P=0.02) (Figs. 2 and 6). Likewise, GS, IR and OS demonstrated a significant increase in the proportion of Hispanic trainees over the study period (P for trend <.001, .04 and .02, respectively). Black trainees showed a significant increasing trend only in IR (P =.05) (Fig. 4).
Figure 1.
Trends in vascular surgery trainees, 1999-2005. No significant changes seen in the three study groups, females, blacks, and Hispanics. (P=0.2, P=0.8, and P=0.8, respectively).
Figure 3.
Trends in female trainees among the three vascular specialties, 1999-2005. No significant trends seen in VS, IR, or IC. (P=0.2, P=0.66, P=0.06)
Figure 5.
Trends in Hispanic trainees among the three vascular specialties, 1999-2005. Again, IR showed an increase in the number of Hispanic trainees. (P=0.04).
Figure 2.
Trends in general surgery trainees, 1999-2005. Both female and Hispanic trainee participation increased in the seven year study period. (P<0.0001 and P<0.0001, respectively).
Figure 6.
Trends among female, black, and Hispanic trainees in orthopedic surgery, 1999-2005. Small, but significant increase seen among female and Hispanic trainees (P=0.04 and P=0.02).
Figure 4.
Trends in black trainees among the three vascular specialties, 1999-2005. IR was the only specialty to show an increase in the number of black participants in training programs. (P=0.04)
Overall, VS had a statistically significant higher proportion of female trainees than IC (P<.001), IR (P<.001), and OS (P=.001) (Figs. 1, 3-5). However, the proportion of women was significantly higher in GS compared with VS (P<.001). The proportion of blacks in VS was significantly higher compared with IC (P=.005), but lower compared with GS (P<.025), IR (P=.51) and OS (P=.51). The proportion of Hispanic trainees was significantly lower in VS than in OS (P=.001). No significant differences were observed however, in the proportion of Hispanics enrolled in VS programs compared with IC, IR, or GS (P= .42, .29, and .22, respectively). No other significant trends over time were noted in the proportion of racial/ethnic minorities within the specialties.
DISCUSSION
This study demonstrates that the gender and racial/ethnic composition of the physician workforce in vascular specialties has not matched the increasing proportion of underrepresented groups in the US population, including patients with vascular disease. Compared to other surgical and interventional specialties, VS has particularly revealed no significant changes in the gender or racial make-up of its fellowship positions. A recent report from the Association of American Medical Colleges based on the American Medical Association (AMA) Physician Masterfile revealed that in 2006 in the United States there were 2,452 active physicians in vascular surgery.18 Also shown in the report, VS is one the specialties with the lowest proportion of active physicians per 100,000 people in the general population of the United States.19 In other words, there is one active physician in VS per 121,600 people. This high rate of population per vascular surgeon amplifies the disproportion between the workforce of VS and the composition of the US general population.
VS remains a predominantly white, male surgical specialty.9 One explanation may be that women are not attracted to a subspecialty with longer work hours and more rigorous training. After completing five years of intense general surgical training, women may look to more time-friendly specialties, allowing them to start families. Childbearing during training remains difficult for the trainee, and the fear of little support by programs may affect the female trainees choice to enter specialties like VS.20 Another possible reason may be the minimal effort made by VS programs to welcome more females in the applicant pool.20 Most vascular programs, as shown in our study, still contain primarily male trainees.
Despite these findings, it is notable that of the training programs studied, only GS had a higher proportion of women than VS. In fact, VS had significantly more women trainees than other vascular disciplines. These data suggest that VS programs have been attracting competitive female candidates. However, the proportion of VS women trainees has remained flat over the study period with no significant increase. Further recruitment efforts aimed at women could improve the VS workforce to reflect the increase in women graduates from medical schools and GS training programs.
Similar to the gender disparities seen in VS, a small number of underrepresented racial and ethnic groups, particularly blacks and Hispanics, are enrolled in VS training programs. Conversely, other specialties, like OS, IR and GS have shown increasing proportions of underrepresented groups. In particular, OS had positive trends in females and Hispanics. This finding may be a direct result of a recruiting initiative aimed at improving diversity within OS.7 The American Academy of Orthopedic Surgeons (AAOS) developed a program five years ago based on “culturally competent care”.8 A web-based learning center was created, which includes a quiz testing the physician's cultural awareness and ways to enrich one's cultural knowledge base. In addition, a mandate related to this effort was set forth encouraging residency programs to target qualified minorities and females in the applicant process. Recruiters identified talented students in minority medical organizations. Such efforts have led to a steady increase in numbers of minorities and females in the orthopedic applicant pool.
A basic premise of this and related studies is that a physician workforce that reflects proportionally the racial, ethnic and gender make-up of the population that it serves will improve healthcare. Multiple studies have documented disproportionally poor outcomes in Hispanic and black populations for common vascular conditions such as abdominal aortic aneurysm, carotid disease and lower extremity revascularization procedures. Huber et al21, for instance, examined the impact of race on PAD and found higher amputation and lower revascularization rates among blacks with lower extremity vascular disease. Other observational studies have also revealed that blacks are significantly less likely to undergo cerebral arteriography and carotid endarterectomy than whites.22,23 Hispanic patients with vascular disease also have lower rates of lower extremity and carotid artery revascularizations and abdominal aortic aneurysm (AAA) repairs.4 In fact, Hispanics, when compared to non-Hispanic whites, were more likely to present with limb-threatening ischemia, symptomatic carotid artery disease and ruptured AAAs. Although the precise causes of comparatively poor outcomes in minority populations remain unclear and are probably multifactorial, limited access to vascular care and late presentation in the disease course are documented factors.4,21
Socioeconomic differences, including a higher uninsured rate, contribute to delays in presentation, poor access to care, poor access to quality care and poor compliance among minority groups. The opportunity to seek care from physicians who share common cultural backgrounds may be important and necessary to improve communication and allow treatment at an earlier stage of disease course, thereby improving treatment response. In addition, compliance, quality of life, and satisfaction with more effective physician communication may also improve. Studies from the late 1990s showed that communities with high proportions of black and Hispanic residents were four times as likely as others to have a shortage of physicians.24 Moreover, the physicians who did practice in underserved areas with predominantly minority populations were black or Hispanics. There is, therefore, a need to increase the proportion of minorities in the pool of qualified individuals in vascular training programs.
Increasing the number of minority and women vascular surgeons to more closely reflect the proportions of women and minorities with vascular disease in the general population might improve vascular care in underserved and underrepresented populations. Strategies aimed to improve diversity in VS programs could include: 1. targeting minority medical students early in their careers and providing mentors that encourage the students to consider VS as a strong option when choosing a specialty; 2. increasing the influence of the VS community in student minority medical organizations; 3. maintaining scholarship programs for students/residents to attend regional/national meetings; 4.increasing diversity in the VS societies such as the Society for Vascular Surgery and 5. developing formal diversity programs in national and regional vascular surgical societies.
Although the present study is recent and based on the entire data available about the physician workforce in training in the selected specialties in the United States, two important limitations should be acknowledged. First, the analyses were performed over a relatively short study period. A longer period of time (i.e. 20-30 years) would be preferable to assess changes made in the application process and recruiting that could have influenced diversity in the physician workforce over time. Moreover, the trends seen over longer periods of time may more effectively reflect societal shifts. However, the data for past years is not readily available and, unfortunately, do not contain all the ethnic/racial data required for our analyses. The data analyzed from 1999-2005 do, however, give an optimal estimate of even minor changes made in the application process, which will show either a positive or negative effect on the absolute numbers in each program. Second, the raw data separating men and women by ethnic group was not available, which prevented multivariate analysis of trends in proportions of enrollment of ethnic minorities in the different specialty programs adjusting for gender. Nevertheless, even if significant gender differences between the ethnic groups exist, the observed trends by ethnic group across the specialties would have not changed. In summary, this report demonstrates that during the seven-year study period, the composition of the physician workforce and pool of trainees in VS and related subspecialties does not mirror the racial/ethnic and gender distribution of the US population. Strategies to increase the recruitment of talented women and minorities in VS programs should be undertaken.
Acknowledgments
This is study was in part supported by CTSA NIH Grant UL1-RR024982.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.US Census Bureau http://www.census.gov. Accessed October 1, 2008.
- 2.Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation. 2004;110:738–43. doi: 10.1161/01.CIR.0000137913.26087.F0. [DOI] [PubMed] [Google Scholar]
- 3.Feinglass J, Rucker-Whitaker C, Lindquist L, McCarthy WJ, Pearce WH. Racial differences in primary and repeat lower extremity amputation: results from a multihospital study. J Vasc Surg. 2005;41:823–9. doi: 10.1016/j.jvs.2005.01.040. [DOI] [PubMed] [Google Scholar]
- 4.Morrissey NJ, Giacovelli J, Egorova N, Gelijns A, Moskowitz A, McKinsey J, et al. Disparities in the treatment and outcomes of vascular disease in Hispanic patients. J Vasc Surg. 2007;46:971–8. doi: 10.1016/j.jvs.2007.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andriole DA, Klingensmith ME, Schechtman KB. Diversity in General Surgery: A Period of Progress. Current Surgery. 2005;62:423–8. doi: 10.1016/j.cursur.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 6.Andriole DA, Jeffe DB, Schechtman KB. Is Surgical Workforce Diversity Increasing? Journal of the American College of Surgeons. 2007;204:469–77. doi: 10.1016/j.jamcollsurg.2006.12.035. [DOI] [PubMed] [Google Scholar]
- 7.Diversity in Orthopaedics. http://www3.aaos.org/About/diversity/index.cfm. Accessed October 9, 2008.
- 8.Jimenez RL. Current Activities in Orthopaedic Culturally Competent Care Education. J Am Acad Orthop Surg. 2007;15:S76–S79. doi: 10.5435/00124635-200700001-00017. [DOI] [PubMed] [Google Scholar]
- 9.Eidt JF, Chaikof E, Sidawy AN. Characteristics of the applicant pool to vascular surgery residency programs. Journal of Vascular Surgery. 2005;42:519–23. doi: 10.1016/j.jvs.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 10.VascularWeb Residents and Medical Students Webpage. http://www.vascularweb.org//Residents_and_Students/index.html. Accessed October 8, 2008.
- 11.Brotherton SE, Simon FA, Tomany SC. Appendix II. US graduate medical education, 1999-2000. JAMA. 2000;284:1159–72. doi: 10.1001/jama.284.9.1121. [DOI] [PubMed] [Google Scholar]
- 12.Brotherton SE, Simon FA, Etzel SI. Appendix II. US graduate medical education, 2000-2001. JAMA. 2001;286:1095–107. doi: 10.1001/jama.286.9.1056. [DOI] [PubMed] [Google Scholar]
- 13.Brotherton SE, Simon FA, Etzel SI. Appendix II. US graduate medical education, 2001-2002. Jama-Journal of the American Medical Association. 2002;288:1151–64. [Google Scholar]
- 14.Brotherton SE, Rockey PH, Etzel SI. Appendix II. US graduate medical education, 2002-2003. JAMA. 2003;290:1234–48. doi: 10.1001/jama.290.9.1197. [DOI] [PubMed] [Google Scholar]
- 15.Brotherton SE, Rockey PH, Etzel SI. Appendix II. US graduate medical education, 2003-2004. JAMA. 2004;292:1099–113. doi: 10.1001/jama.292.9.1032. [DOI] [PubMed] [Google Scholar]
- 16.Brotherton SE, Rockey PH, Etzel SI. Appendix II. US graduate medical education, 2004-2005. JAMA. 2005;294:1129–40. doi: 10.1001/jama.294.9.1075. [DOI] [PubMed] [Google Scholar]
- 17.Brotherton SE, Etzel SI. Appendix II. Graduate medical education, 2005-2006. JAMA. 2006;296:1154–69. doi: 10.1001/jama.296.9.1154. [DOI] [PubMed] [Google Scholar]
- 18.Physician Specialty Data: A Chart Book. http://www.aamc.org/workforce/dataandpub.htm. Accessed August 7, 2008.
- 19.Diversity in the Physician Workforce: Facts & Figures 2006. http://www.aamc.org/workforce/dataandpub.htm. Accessed August 7, 2008.
- 20.Harris LM, Chaikof EL, Eidt JF. Altering the career choice: can we attract more women to vascular surgery? J Vasc Surg. 2007;45:846–8. doi: 10.1016/j.jvs.2006.12.072. [DOI] [PubMed] [Google Scholar]
- 21.Huber TS, Wang JG, Wheeler KG, Cuddeback JK, Dame DA, Ozaki CK, et al. Impact of race on the treatment for peripheral arterial occlusive disease. J Vasc Surg. 1999;30:417–25. doi: 10.1016/s0741-5214(99)70068-6. [DOI] [PubMed] [Google Scholar]
- 22.Oddone EZ, Horner RD, Monger ME, Matchar DB. Racial variations in the rates of carotid angiography and endarterectomy in patients with stroke and transient ischemic attack. Arch Intern Med. 1993;153:2781–6. [PubMed] [Google Scholar]
- 23.Huber TS, Wheeler KG, Cuddeback JK, Dame DA, Flynn TC, Seeger JM. Effect of the Asymptomatic Carotid Atherosclerosis Study on carotid endarterectomy in Florida. Stroke. 1998;29:1099–105. doi: 10.1161/01.str.29.6.1099. [DOI] [PubMed] [Google Scholar]
- 24.Komaromy M, Grumbach K, Drake M, Vranizan K, Lurie N, Keane D, et al. The role of black and Hispanic physicians in providing health care for underserved populations. N Engl J Med. 1996;334:1305–10. doi: 10.1056/NEJM199605163342006. [DOI] [PubMed] [Google Scholar]