Abstract
Patients with acute coronary syndromes (ACS) who are accompanied by atypical symptoms are frequently misdiagnosed and under-treated. This study was conducted to examine and compare the factors associated with atypical symptoms other than chest pain in younger (<70 yr) and older (≥70 yr) patients with first-time ACS. Data were obtained from the electronic medical records of the patients (n=931) who were newly diagnosed as ACS and hospitalized from 2005 to 2006. The 7.8% (n=49) of the younger patients and 13.4% (n=41) of the older patients were found to have atypical symptoms. Older patients were more likely to complain of indigestion or abdominal discomfort (P=0.019), nausea and/or vomiting (P=0.040), and dyspnea (P<0.001), and less likely to have chest pain (P=0.007) and pains in the arm and shoulder (P=0.018). A logistic regression analysis showed that after adjustment made for the gender and ACS type, diabetes and hyperlipidemia significantly predicted atypical symptoms in the younger patients. In the older patients, the co-morbid conditions such as stroke or chronic obstructive pulmonary disease were positive predictors. Health care providers need to have an increased awareness of possible presence of ACS in younger persons with diabetes and older persons with chronic concomitant diseases when evaluating patients with no chest pain.
Keywords: Acute coronary syndrome, Symptoms
INTRODUCTION
Patients with acute coronary syndromes (ACS) showing atypical symptoms other than chest pain are frequently misdiagnosed on initial evaluation and highly likely face unfavorable prognoses such as under-treatment and poor clinical outcome (1, 2). The primary complaint of the patients with ACS is characterized predominantly by chest pain. However, a substantial number of patients may have atypical or no symptoms on initial evaluation (1, 2). Atypical symptom indicates that the patient's chief complaint is not chest pain but other gastrointestinal or respiratory symptoms with less intense chest pain. The absence of chest pain at the hospital presentation was the most significant factors predicting lower use of thrombolytic therapy (2, 3), and was associated with the hospital complications and with an increased risk of hospital death compared with a typical presentation (1, 2, 5).
Symptoms, which are a key component in the patients' decision to seek care, are critical to appropriate triage, and influence the decision on whether to pursue further evaluation and initiation of treatment (4). Previous research showed that typical symptoms including chest pain are predictive of ACS in younger patients <70 yr and less predictive in older patients (4). This atypical symptom most likely make it impossible to determine if the patient has a cardiac problem, thereby leading to a delay in decision-making as to seeking medical treatment.
Understanding the factors associated with atypical presentations may help in the earlier detection and more appropriate medical treatments of the patients with ACS within the first 24 hr. While many studies have described the association of aging, gender, and diabetes with atypical symptoms (5, 6, 7, 19), few studies have examined the predictors of atypical symptoms in younger and older patients separately. Age grouping for the comparison in this study was based on a 70 yr of age according to recent clinical studies (1, 4, 12). Therefore, this study proposes to examine and compare the factors associated with atypical symptoms without chest pain in younger (<70 yr) and older (≥70 yr) patients with the first attack of ACS.
MATERIALS AND METHODS
Study design and subjects
A cross-sectional, descriptive design was adopted using the review of electronic medical records (EMR) to examine factors associated with atypical symptoms among younger and older adults with ACS.
Data were obtained, after approval of the institutional review board of the hospital, from the EMR of the patients who had been hospitalized at Chonnam National University Hospital for the period 2005-2006. The patients had undergone treatment with diagnoses of the first attack of ACS, which was determined on the basis of ECG changes, myocardial serum markers, and a history of clinically appropriate symptoms including unstable angina, ST-segment elevation myocardial infarction (STEMI), and Non-ST-segment elevation myocardial infarction (NSTEMI). STEMI is defined by complete obstruction of a coronary artery, and causes damage that involves the full thickness of the heart muscle. In contrast, NSTEMI is defined by partial obstruction of a coronary artery, and causes damage that does not involve the full thickness of the heart wall. In unstable angina, the clot does not completely occlude the artery, and cardiac enzymes are not elevated.
The cases that had confirmed by ACS when they discharged were only collected for this study. Patients' data were documented and coded from EMR into a dataset in terms of demographic and clinical characteristics, symptom presentations, and other significant laboratory data. The dominant symptoms that had been recorded at emergency department (ED) presentations and other accompanying symptoms were documented as well. A typical presentation was defined in case the reported symptoms included chest pain. An atypical presentation was regarded as a presentation not accompanied by chest pain. The patients presented with a cardiac arrest were not included in this analysis because their early symptoms could not be assessed. Standardized definitions of all patient-related variables and clinical diagnoses were used for data analyses. A total of 931 data including 626 younger (67.2%) and 305 older patients (32.8%) were finally used for analysis.
Statistical analysis
Data were analyzed using SPSS version 12.0. Differences in demographic and clinical variables between younger and older patients and between patients showing typical and atypical symptoms were assessed using the chi-square test or t-tests. Multiple logistic regression analyses were conducted to find independent factors on atypical symptoms in younger and older patients' data.
RESULTS
Baseline clinical characteristics
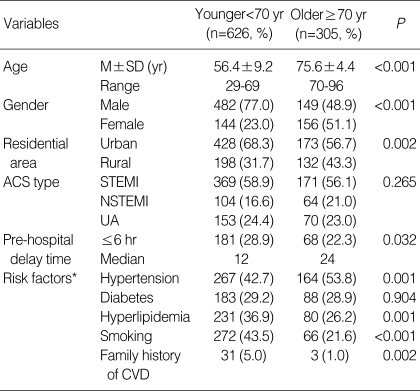
The 67.2% (n=626) of the patients sampled was 70 yr of age or lower and 32.8% (n=305) was over 70 yr of age. The 58% (n=540), 18% (n=168), and 24% (n=223) of those sampled were STEMI, NSTEMI, and unstable angina, respectively. About 68% of the sample was male (n=631) and 32% female (n=300). Younger patients were more likely to reach the hospital within 6 hr or less, compared with older patients (28.9% vs. 22.3%). For risk factors, bivariate analyses showed that older patients were more likely to have hypertension and less likely to have multiple risk factors for cardiovascular diseases, compared with those of younger patients (P<0.001). However, younger patients were more likely to be accompanied by hyperlipidemia (total cholesterol ≥220 mg/dL), current smoking, and family history of cardiovascular diseases, compared with older patients. General characteristics of the group sampled are shown in Table 1.
Table 1.
Baseline characteristics of the younger and older patients with ACS
*The number of risk factors was duplicated.
ACS, Acute coronary syndrome; STEMI, ST-elevation myocardial infarction; NSTEMI, Non-ST-elevation myocardial infarction; UA, Unstable Angina; CVD, Cerebro-cardiovascular disease.
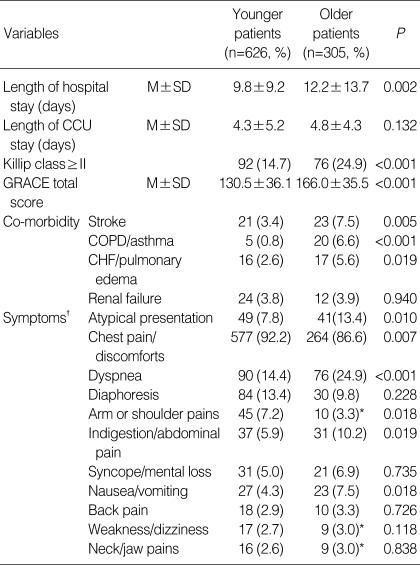
Older patients had hospital stays (12.2±13.7 days) significantly longer than younger patients (9.8±9.2 days). However, the duration of stay at the coronary care unit did not significantly differ between the two groups. The 9.7% (n=90) had atypical symptoms without chest pain, when they presented themselves at the hospital, including 7.8% of younger patients and 13.4% of older patients. Older patients were more likely to complain of indigestion or abdominal discomfort (P=0.019), nausea or vomiting (P=0.040), and dyspnea (P<0.001). However, they were less likely to have chest pain (P=0.007) and arm or shoulder pain (P=0.018), compared with younger patients. There were no significant differences in the symptoms of dizziness and diaphoresis between the two groups (Table 2).
Table 2.
Clinical characteristics of the younger and older patients with ACS
*Where the number of subjects in a cell was less than 5, Fisher's exact test was used; †The number of symptoms was duplicated.
ACS, Acute coronary syndrome; CCU, coronary care unit; COPD, chronic obstructive pulmonary disease; CHF, congestive heart failure; GRACE, Global Registry of Acute Coronary Events.
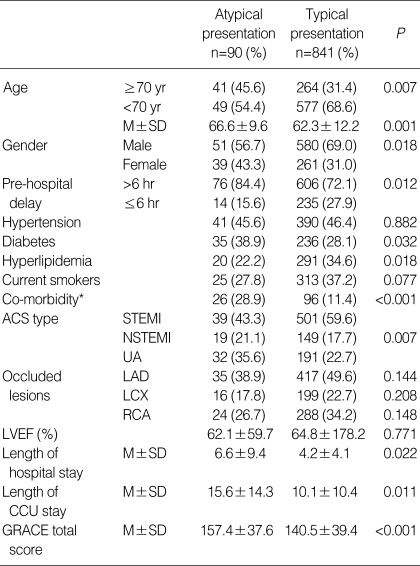
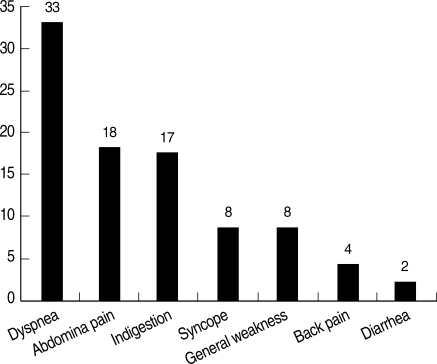
The characteristics of patients with atypical and typical symptoms are compared in Table 3. Patients with atypical presentation were significantly older and more female gender than patients with typical presentation (P<0.05). The patients with atypical symptoms took significantly longer >6 hr to present to the hospital than did those with typical symptoms (P=0.012). In terms of the risk factors that patients had, the patients presenting with atypical symptoms were more likely to have a history of diabetes and greater prevalence of co-morbid conditions but they were less likely to have hyperlipidemia compared to the patients with typical symptoms (P<0.001). The patients with atypical symptoms had significant longer hospital stays including a stay at a coronary care unit and the score predicting hospital mortality, Global Registry of Acute Coronary Events (GRACE) score, was also significantly higher than the patients with typical symptoms (P<0.05) (Table 3). The types and frequencies of chief atypical symptoms are shown in Fig.1.
Table 3.
Characteristics of the patients presenting with atypical and typical symptoms (n=931)
*Co-morbidity represents the number of patients who had more than one incidence of stroke, chronic obstructive pulmonary disease, asthma, chronic heart failure or renal failure.
ACS, Acute coronary syndrome; STEMI, ST-elevation myocardial infarction; NSTEMI, Non-ST-elevation myocardial infarction; LAD, Left anterior descending artery; LCX, Left circumflex artery; RCA, Right coronary artery; LVEF, left ventricular ejection fraction; GRACE, Global Registry of Acute Coronary Events.
Fig. 1.
Type and frequency of chief atypical symptoms in patients with atypical presentation.
Factors associated with atypical symptoms among younger and older patients
First, logistic multiple regression analysis was conducted to determine the factors for the atypical presentation in whole patient group and found that aging (included as a continuous variable; Adjusted odds ratio (OR) 1.023, 95% confidence interval (CI) 1.001-1.046, P=0.042) and the presence of comorbidities (Adjusted OR 2.634, 95% CI 1.542-4.498, P<0.001) were independent predicting factors, but female gender (P=0.432) and a history of diabetes (P=0.131) were not associated with atypical presentation.
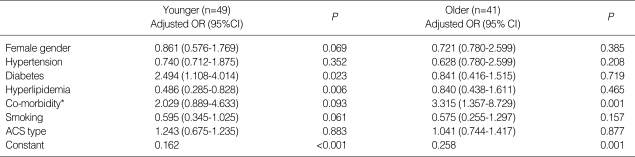
Logistic regression analyses were then conducted to determine which variables predicted atypical symptoms in younger and older groups. All significant variables confirmed by bivariate analyses were entered in the analysis. The logistic regressions model testing the prediction of atypical symptoms in both groups (coded as 0=typical symptom, 1=atypical symptom) were significant (χ2=29.50, df=8, P<0.001; χ2=23.61, df=8, P<0.05). The models explained 46.0% to 109.0% of variances for the younger group and 44% to 80% for the older one in the atypical symptom category (Cox & Snell R2=0.046, Nagelkerke R2=0.109; Cox & Snell R2=0.044, Nagelkerke R2=0.080). After an adjustment was made for gender and ACS type, diabetes and hyperlipidemia significantly predicted atypical symptoms in younger patients (Table 4). This result indicates that younger adults with diabetes have 2.5 times more chances of experiencing atypical symptoms compared with the younger adults without diabetes. On the contrary, hyperlipidemic younger adults have 50% less chances of having atypical symptoms. In the older group, the result shows that the older adults with co-morbid chronic diseases such as stroke, chronic obstructive pulmonary disease (COPD), asthma, congestive heart failure or renal failure likely have 3.3 times more chances of having atypical symptoms compared with healthy older adults.
Table 4.
Predicting factors on the atypical symptoms in younger (n=626) and older (n=305) patients with ACS
Odds ratios (OR) were calculated using a binary logistic regression analysis and all variables entered on step 1 in younger and older patients; *Co-morbidity includes incidences of stroke, chronic obstructive pulmonary disease, asthma, chronic heart failure or renal failure.
ACS, Acute coronary syndrome; CI, confidence interval.
DISCUSSION
Accurate recognition of ACS on initial presentation is a key for healthcare providers inside and outside of the hospital setting to the minimization of morbidity and mortality. In this study, older patients (13.4%) visited the hospital significantly more frequently for other symptoms without chest pain, compared with younger patients (7.8%). This is comparable with previous observational studies in which as much as 16.6% of acute myocardial infarction (AMI) patients (8) and 8.4% of the AMI patients enrolled in the GRACE study experienced no chest symptoms (1). This finding is in support of the facts that an old age is a factor affecting atypical presentation (2, 12) and typical symptoms are positive predictors of ACS in younger patients (4, 5).
Identifying the symptoms of ACS is important for successful management and especially useful as a guide to their timely treatment of those with atypical symptom presentations. We found that the patients with atypical presentations had a considerable delay in seeking care and had a worse clinical outcome such as longer hospital stay. The dominant presenting symptoms in patients with atypical presentations in this study were abdominal pain/discomforts (38.8%) and dyspnea (36.6%). The GRACE study involving 95 hospitals in 14 countries (1999-2002) reported that 23.8% of the patients presented to the hospital without chest pain were not initially recognized as having an ACS and dominant symptoms were dyspnea (49.3%) and diaphoresis (26.2%) (1). They were less likely to receive effective cardiac medications, and experienced greater hospital morbidity and mortality than did patients with typical symptoms. After adjustments for confounding variables, an increase in hospital mortality rates was noted in patients with dominant symptoms of syncope, nausea and vomiting, and dyspnea (1).
This study for the whole patient group demonstrated that female gender and the histories of diabetes and hypertension were associated with atypical presentation in bivariate analyses, but were not supported as predicting factors by multivariate analysis. This finding is not consistent with previous studies demonstrated that patients with atypical symptoms were more likely to be older, female, hypertensive, diabetic, and to have a history of congestive heart failure (1, 9, 10). This controversy can be explained by the bivariate analyses of this study that diabetic younger patients were more likely to have atypical presentation compared to non-diabetic younger patients (12.6% vs. 5.9%, P=0.005), but no association was found in older patients (13.6% vs. 13.4%, P=0.950). Therefore, diabetes should be carefully interpreted in view of confounding variables such as age distribution or clinical characteristics and the adjustment for them using a multivariate analysis may be required for whole patient group in future study.
Our findings show that dyspnea, indigestion, and nausea/vomiting were more likely to be accompanied by older patients, which is similar to the previous study results (8). In contrast, older adults with AMI are less likely to complain of chest pain and arm or shoulder pains, which was also consistent with previous studies (8, 11). This finding supported a previous study that typical chest pain was significantly associated with ACS in younger patients (12). The dyspnea was represented as a major component of dominant complaints in AMI patients without chest pain (1). The AMI patients without chest pain were more likely to complain of pulmonary edema (Killip class II and III), require drug treatment for heart failure, and have a prior history of congestive heart failure than patients with chest pain (2).
This study found diabetes, which was not a predictor in the whole patient group, to be an independent predicting factor in younger patients presented to the hospital with atypical symptoms when gender and ACS type were controlled for. This finding, which was consistent with previous studies that patients with atypical symptoms were more likely to have diabetes compared with patients having typical symptoms (1, 9, 10), and identified diabetes as an independent predictor of atypical presentation in women with AMI (13). About 29% of those sampled for this study had suffered from diabetes, and this was slightly higher than the 25% of the AMI patients with a history of diabetes in the GRACE study (14). Previous studies reported the impacts of diabetes on the prognosis after ACS such as poor clinical outcomes including heart and renal failure, cardiogenic shock, and death (14-21). It is proposed that physicians and primary health care nurses should educate on the management of diabetes and their possible signs and symptoms of ACS for middle-aged diabetic persons at risk for cardiovascular diseases.
However, younger patients with hypercholesterolemia had 50% less chances of having atypical symptoms compared with those with normal serum cholesterol levels. This finding is associated with the fact that the 74% (n=231) of the patients with hyperlipidemia were younger than 70 yr of age in this study. The finding that hyperlipidemic persons were less likely to have atypical symptoms was consistent with the result of GRACE study (1).
This study showed that female gender and smoking had slight meaningful negative relationships, which had 14% and 40% respectively less chances of having atypical symptoms in a younger group. Many previous studies supported that women were more likely to have atypical symptoms but those studies were conducted for all age group (1, 2, 6, 7). Women, in this study, were distributed more than double in older group ≥70 yr compared to younger group (23.0% vs. 51.1%). This supports aging is a more powerful factor on the atypical presentations and female gender should be interpreted with caution for their age distribution.
A significant predicting factor that helps in identifying atypical symptoms in older patients was co-morbidities that they had. This finding was consistent with a previous observational study that the presentation of an atypical symptom was significantly related with a prior history of heart failure or stroke (2). A qualitative study also supported that women with a concomitant illness thought their symptoms were normal considering their current state of health at the time of their cardiac event (22). This suggests that the recognition of symptoms on the part of older adults could be masked by concurrent illnesses and that health professionals need to be more alert on the possibility of cardiac related symptoms. This study found about 20% of the older patients sampled had comorbid diseases such as stroke, COPD/asthma, or congestive heart failure. The presence of chronic and persistent diseases was significantly higher in older patients compared with younger patients, who were not affected by atypical symptoms. This greater prevalence of co-morbid chronic diseases might be associated with the fact that having diabetes was not associated with the atypical symptoms among older patients. The 64% of the older patients had hypertension or diabetes (or both), and these risk factors were adjusted for the analysis.
Health care providers should have more concern about diabetic younger adults, and about older adults with chronic concomitant diseases such as stroke and COPD when evaluating patients with no chest pains. Nurse researchers recommended the education targeting individuals at the risk of ACS as well as their families is more efficient method than mass public education campaigns to reduce pre-hospital delays (23-25). Therefore, such educational efforts should focus on enhancing awareness of any ACS signs and symptoms in this highrisk group. In addition, it is to be emphasized that the management of social, cognitive, and behavioral manifestations that accompany these symptoms and contribute to the delay.
Further research needs to be undertaken qualitatively for ACS patients with atypical symptoms who delayed presentation to the hospital to have a better understanding the pattern of symptoms and their cognitive responses to their symptoms. In Korea, diabetes and hyperlipidemia significantly predict atypical symptoms in the younger patients with acute coronary syndrome. In the older patients, the co-morbid conditions such as stroke or chronic obstructive pulmonary disease are positive predictors of atypical symptoms. Health care providers need to have an increased awareness of possible presence of ACS in younger persons with diabetes and older persons with chronic concomitant diseases when evaluating patients with no chest pain.
Footnotes
This study was sponsored by research funds from Chosun University, 2007.
References
- 1.Brieger D, Eagle KA, Goodman SG, Steg PG, Budaj A, White K, Montalescot G GRACE Investigators. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the Global Registry of Acute Coronary Events. Chest. 2004;126:461–469. doi: 10.1378/chest.126.2.461. [DOI] [PubMed] [Google Scholar]
- 2.Canto JG, Shlipak MG, Rogers WJ, Malmgren JA, Frederick PD, Lambrew CT, Ornato JP, Barron HV, Kiefe CI. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. 2000;283:3223–3229. doi: 10.1001/jama.283.24.3223. [DOI] [PubMed] [Google Scholar]
- 3.Barron HV, Bowlby LJ, Breen T, Rogers WJ, Canto JG, Zhang Y, Tiefenbrunn AJ, Weaver WD. Use of reperfusion therapy for acute myocardial infarction in the United States. Circulation. 1998;97:1150–1156. doi: 10.1161/01.cir.97.12.1150. [DOI] [PubMed] [Google Scholar]
- 4.Milner KA, Funk M, Richards S, Vaccarino V, Krumholz HM. Symptom predictors of acute coronary syndromes in younger and older patients. Nurs Res. 2001;50:233–241. doi: 10.1097/00006199-200107000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Gregoratos G. Clinical manifestations of acute myocardial infarction in older patients. Am J Geriatr Cardiol. 2001;10:345–347. doi: 10.1111/j.1076-7460.2001.00641.x. [DOI] [PubMed] [Google Scholar]
- 6.Patel H, Rosengren A, Ekman I. Symptoms in acute coronary syndromes: Does sex make a difference? Am Heart J. 2004;148:27–33. doi: 10.1016/j.ahj.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Arslanian-Engoren C, Patel A, Fang J, Armstrong D, Kline-Rogers E, Duvernoy CS, Eagle KA. Symptoms of men and women presenting with acute coronary syndromes. Am J Cardiol. 2006;98:1177–1181. doi: 10.1016/j.amjcard.2006.05.049. [DOI] [PubMed] [Google Scholar]
- 8.Ryan CJ, DeVon HA, Horne R, King KB, Milner K, Moser DK, Quinn JR, Rosenfeld A, Hwang SY, Zerwic JJ. Symptom clusters in acute myocardial infarction: a secondary data analysis. Nurs Res. 2007;56:72–81. doi: 10.1097/01.NNR.0000263968.01254.d6. [DOI] [PubMed] [Google Scholar]
- 9.Milner KA, Funk M, Arnold A, Vaccarino V. Typical symptoms are predictive of acute coronary syndromes in women. Am Heart J. 2002;143:283–288. doi: 10.1067/mhj.2002.119759. [DOI] [PubMed] [Google Scholar]
- 10.Then KL, Rankin JA, Fofonoff DA. Atypical presentation of acute myocardial infarction in 3 age groups. Heart Lung. 2001;30:285–293. doi: 10.1067/mhl.2001.116010. [DOI] [PubMed] [Google Scholar]
- 11.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. Decade-long trends and factors associated with time to hospital presentation in patients with acute myocardial infarction: The Worcester Heart Attack Study. Arch Intern Med. 2000;160:3217–3223. doi: 10.1001/archinte.160.21.3217. [DOI] [PubMed] [Google Scholar]
- 12.Han JH, Lindsell CJ, Hornung RW, Lewis T, Storrow AB, Hoekstra JW, Hollander JE, Miller CD, Peacock WF, Pollack CV, Gibler WB Emergency medicine cardiac research and education group internet tracking registry for acute coronary syndromes investigators. The elder patient with suspected acute coronary syndromes in the emergency department. Acad Emerg Med. 2007;14:732–739. doi: 10.1197/j.aem.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 13.Stephen SA, Darney BG, Rosenfeld AG. Symptoms of acute coronary syndrome in women with diabetes: an integrative review of the literature. Heart Lung. 2008;37:179–189. doi: 10.1016/j.hrtlng.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 14.Franklin K, Goldberg RJ, Spencer F, Klein W, Budaj A, Brieger D, Marre M, Steg PG, Gowda N, Gore JM GRACE investigators. Implications of diabetes in patients with acute coronary syndromes. Arch Intern Med. 2004;164:1457–1463. doi: 10.1001/archinte.164.13.1457. [DOI] [PubMed] [Google Scholar]
- 15.Chun BY, Dobson AJ, Heller RF. The impact of diabetes on survival among patients with first myocardial infarction. Diabetes Care. 1997;20:704–708. doi: 10.2337/diacare.20.5.704. [DOI] [PubMed] [Google Scholar]
- 16.Lowel H, Koenig W, Engel S, Horman A, Keil U. The impact of diabetes mellitus on survival after myocardial infarction: can it be modified by drug treatment? Results of a population-based myocardial infarction register follow-up study. Diabetologica. 2000;43:218–226. doi: 10.1007/s001250050032. [DOI] [PubMed] [Google Scholar]
- 17.Bakhai A, Collinson J, Flather MD, de Arenaza DP, Shibata MC, Wang D, Adgey JA KAA Fox for the PRAIS-UK Investigators. Diabetic patients with acute coronary syndromes in the UK: high risk and under treated. Results from the prospective registry of acute ischaemic syndromes in the UK (PRAIS-UK) Int J Cardiol. 2005;100:79–84. doi: 10.1016/j.ijcard.2004.08.035. [DOI] [PubMed] [Google Scholar]
- 18.Herlitz J, Karlson BW, Lindqvist J, Sjölin M. Important factors for the 10-year mortality rate in patients with acute chest pain or other symptoms consistent with acute myocardial infarction with particular emphasis on the influence of age. Am Heart J. 2001;142:624–632. doi: 10.1067/mhj.2001.117965. [DOI] [PubMed] [Google Scholar]
- 19.DeVon HA, Ryan CJ. Symptoms across the continuum of acute coronary syndromes: differences between women and men. Am J Crit Care. 2008;17:14–25. [PMC free article] [PubMed] [Google Scholar]
- 20.Lingman M, Herlitz J, Bergfeldt L, Karlsson T, Caidahl K, Hartford M. Acute coronary syndromes-the prognostic impact of hypertension, diabetes and its combination on long-term outcome. Int J Cardiol. 2009;137:29–36. doi: 10.1016/j.ijcard.2008.05.055. [DOI] [PubMed] [Google Scholar]
- 21.Mak KH, Moliterno DJ, Granger CB, Miller DP, White HD, Wilcox RG, Califf RM, Topol EJ. For the global utilization of streptokinase and tissue plasminogen activator for occluded coronary arteries (GUSTO)-1 investigators. Influence of diabetes mellitus on clinical outcome in the thrombolytic era of acute myocardial infarction. J Am Coll Cardiol. 1997;30:171–179. doi: 10.1016/s0735-1097(97)00118-6. [DOI] [PubMed] [Google Scholar]
- 22.Ruston A, Clayton J. Women's interpretation of cardiac symptoms at the time of their cardiac event: The effect of co-occurring illness. Eur J Cardio Nurs. 2007;6:321–328. doi: 10.1016/j.ejcnurse.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 23.Dracup K, McKinley S, Riegel B, Mieschke H, Doering LV, Moser DK. A nursing intervention to reduce prehospital delay in acute coronary syndrome: a randomized clinical trial. J Cardiovasc Nurs. 2006;21:186–193. doi: 10.1097/00005082-200605000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Tullmann DF, Haugh KH, Dracup KA, Bourguignon C. A randomized controlled trial to reduce delay in older adults seeking help for symptoms of acute myocardial infarction. Res Nurs Health. 2007;30:485–497. doi: 10.1002/nur.20245. [DOI] [PubMed] [Google Scholar]
- 25.Buckley T, McKinley S, Gallagher R, Dracup K, Moser DK, Aitken LM. The effect of education and counseling on knowledge, attitudes and beliefs about responses to acute myocardial infarction symptoms. Eur J Cardiovasc Nurs. 2007;6:105–111. doi: 10.1016/j.ejcnurse.2006.05.005. [DOI] [PubMed] [Google Scholar]