Abstract
Various treatment methods have been adopted in the management of warts; however, there is still no consensus on first-line treatment. This study was designed to evaluate the efficacy of long-pulsed Nd:YAG laser in the treatment of warts. Over the course of 1 yr, 369 patients with recalcitrant or untreated warts were exposed to a long-pulsed Nd:YAG laser. The following parameters were used: spot size, 5 mm; pulse duration, 20 msec; and fluence, 200 J/cm2. No concomitant topical treatment was used. In all, 21 patients were lost during follow up; hence, the data for 348 patients were evaluated. The clearance rate was 96% (336 of the 348 treated warts were eradicated). The clearance rate of verruca vulgaris after the first treatment was very high (72.6%), whereas the clearance rate of deep palmopantar warts after the first treatment was low (44.1%). During a median follow-up period of 2.24 months (range, 2-10 months), 11 relapses were seen (recurrence rate, 3.27%). In conclusion, long-pulsed Nd:YAG laser is safe and effective for the removal or reduction of warts and is less dependent on patient compliance than are other treatment options.
Keywords: Lasers, Warts
INTRODUCTION
Warts are benign epithelial neoplasms of the skin and mucosa resulting from human papillomavirus (HPV) infection. They are a common dermatologic complaint, with an estimated incidence of 10% in children and young adults (1). Even if disease progression is naturally self-limited, the course of the disease is unpredictable, and treatment may be necessary. Several treatment methods are available for treatment of warts; however, most methods have specific disadvantages and side effects. Invasive methods have the drawbacks of pain and long recovery periods. Topical management requires the application of drugs for long durations and treatment success is, therefore, highly dependent on patient compliance (2).
Laser treatment is based on the principle of photodermal or photomechanical destruction of the target tissue. Target structures absorb monochromatic coherent light of specific wavelength and fluence. Light energy gets converted to thermal energy, thus destroying the target structure. Depending on the pulse duration and energy density, this may result in the coagulation (photodermal effect) or blasting (photomechanical effect) of these structures (2). A wart is a lesion characterized by proliferation and dilation of vessels. Many studies have used 585-nm pulsed dye lasers for the treatment of warts, with the wart blood vessels as the target tissue (1-4). This is because hemoglobin in blood has strong absorption peaks at wavelengths ranging from 585 to 595 nm (5). Moreover, hemoglobin has a significant, albeit more modest, absorption peak between 800 and 1,100 nm. Therefore, it has been postulated that 1,064-nm Nd:YAG lasers could be used in the treatment of telangiectases (5). In addition, since there is decreased light absorption by melanin at this wavelength, there is reduced risk of pigmentary side effects (4). Previous studies have shown that 1,064-nm Nd:YAG lasers used at longer widths can be used to treat telangiectasias of the lower extremities (5), face (6), and venous lake (7). We used a long-pulsed Nd:YAG laser in the treatment of warts, with the wart blood vessels as the target, and evaluated clinical outcomes.
MATERIALS AND METHODS
Patients
Over the course of 1 yr, 369 patients (mean age, 21 yr; range, 3-67 yr) (Table 1) with recalcitrant or untreated warts were treated with a long-pulsed Nd:YAG laser. Informed written consent was obtained from all participants before inclusion in the study. In all, 21 patients were lost during follow up, and therefore, the data of 348 patients were evaluated. Warts were classified into three types-verruca vulgaris (212 patients), deep palmoplantar warts (68 patients), and periungual warts (68 patients). Prior to the study, photographs of all the lesions were taken and the size of each lesion was recorded.
Table 1.
Characteristics of the subjects enrolled in this study
Treatment
The study employed a 1,064-nm long-pulsed Nd:YAG laser (Cutera, Inc., Brisbane, CA, U.S.A.). The following parameters were used: spot size, 5 mm; pulse duration, 20 msec; and fluence, 200 J/cm2. Prior to laser treatment, warts were treated with EMLA® cream or a local lidocaine injection and were peeled with a razor blade. One or two courses of slightly overlapping laser pulses were applied to each wart, covering the wart itself and a 1-mm margin on the surrounding skin. Around the third treatment date, crusts were found to be formed on the treated parts. At 1 to 2 weeks after treatment, the crusts were removed, and the warts were cleared, leaving only a small scar (Figs. 5-7). The treatment interval was 4 weeks, with up to four treatment sessions. Clearance was defined as the complete absence of a clinically apparent wart, and treatment failure was defined as a persistent lesion after four treatments.
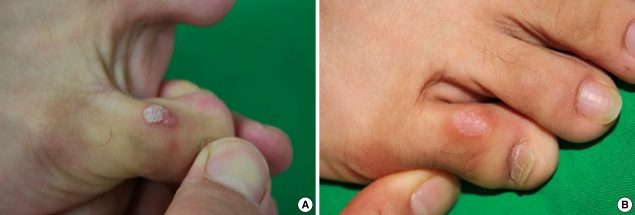
Fig. 5.
(A) Periungual wart. (B) Crusts were formed three days after treatment.
Fig. 7.
(A) Verruca vulgaris on the toe. (B) Complete clearance after only one treatment session.
RESULTS
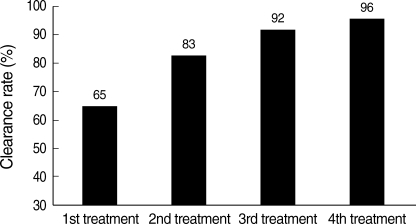
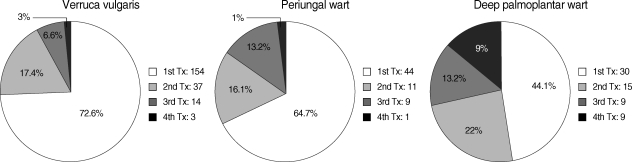
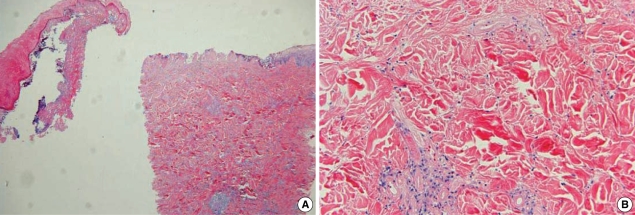
The average number of treatment sessions required for clearance was 1.49 (range, 1-4 sessions) (Fig. 1). At the end of the first treatment, 64% of warts were cleared, while 96% (336/348) of warts were cleared after the fourth treatment (Fig. 2). Verruca vulgaris responded better than the other types of warts and required fewer treatments for clearance (mean, 1.35 sessions). Deep palmoplantar warts required a mean of 1.95 sessions for clearance (Fig. 1). The clearance rate after the first treatment was also higher in the verruca vulgaris group (72.6%) than 64.7% in the periungual warts group and 44.1% in the deep palmoplantar warts group (Fig. 3). The size of the warts was reduced by an average of 10% based on the diameter. This was observed in 69.1% of the verruca vulgaris warts, 52.5% of the periungual warts, and 27.4% of the deep palmoplantar warts. Histopathologic examination after treatment showed separation of the dermoepidermal junction, epidermal necrosis, and red blood cell (RBC) extravasation. Destroyed blood vessels surrounded by a dense inflammatory infiltrate were also shown in the dermis (Fig. 4). Since most (82%) patients who were anesthetized with EMLA® cream complained of serious pain during treatment, local lidocaine injections were administered during the second treatment. Other side effects included transient numbness (15%), hemorrhagic bullae (7%), hyperpigmentation (5%), and hypopigmentation (4%). In addition, 2% of patients with periungual warts experienced nail dystrophy. During a median follow-up period of 2.24 months (range, 2-10 months), 11 relapses were seen (recurrence rate, 3.3%).
Fig. 1.
Average number of treatments according to subtypes of warts.
Fig. 2.
Cumulative clearance by successive treatments.
Fig. 3.
Clearance rates according to number of laser sessions per subtype.
Tx, treatment.
Fig. 4.
Histopathological findings by H&E staining. (A) Separation of dermo-epidermal junction (×40). (B) Destroyed blood vessels in the dermis surrounded by a dense inflammatory infiltrate (×200).
DISCUSSION
Warts are very common, with an incidence of approximately 10% in children and young adults. An estimated 4-million-patient visits were recorded in 1982 for nonvenereal warts. Approximately 70% of these patients were between 10 and 39 yr of age, and 50% presented to a dermatologist. Peak incidence occurs between the ages of 12 and 16 yr (8). Warts often cause pain and may interfere with function. These complications, along with cosmetic embarrassment and risk of translocation to other areas of the skin, are indications for treatment, which can be challenging. Effective therapy must provide reduction in pain and improvement in quality of life. Many different types of therapy have been used in the treatment of warts (9-13). Commonly used methods of physical destruction include surgical excision, electrodesiccation, cryosurgery, and pulsed dye or carbon dioxide laser therapy. Chemical destruction can be induced with salicylic acid, cantharidin, formaldehyde, or glutaraldehyde, among other agents. Chemotherapeutic agents include podophyllin, podophyllotoxin, 5-fluorouracil, and bleomycin. Allergic contact agents used against warts include dinitrochlorobenzene and squaric acid dibutyl ester. More recently, immunomodulators such as interferon, systemic retinoids, cimetidine, and topical imiquimod have been used (14-16).
This prospective study evaluated the efficacy of long-pulsed Nd:YAG lasers in the treatment of warts. The results show that long-pulsed Nd:YAG lasers are a safe and effective approach to wart treatment, with clearance rates higher than those achieved with other common therapies. Previous studies of cryotherapy in the treatment of warts report clearance rates ranging from 63% to 69% (10, 17, 18). In a study using imiquimod, 56% of the patients reported total clearance (19). Efficacy studies of cantharidin show success rates of approximately 80% (20). The pooled data from six randomized controlled studies demonstrated a cure rate of 75% in those treated with salicylic acid compared with 48% in the control group (21). One study performed using bleomycin prick method demonstrated complete resolution of warts in 92% of participants (22).
Long-pulsed Nd:YAG lasers emit a visible light spectrum at 1,064 nm. When a 1,064-nm long-pulsed Nd:YAG laser is used on the skin, a short, strong laser pulse is absorbed by red structures such as cutaneous blood vessels. As a result, blood vessels heat up rapidly and burst. Upon blood vessel rupture, purpura appear, which subside 5 to 7 days later. Vascular lesions become pale with repeat treatment.
The mechanism of action of a long-pulsed Nd:YAG laser in the treatment of warts is not fully understood. Dilated vessels in the papillary dermis are a characteristic feature of warts (23). Light microscopic evaluation of treated areas at 7 days after treatment in this study showed separation of the dermoepidermal junction, epidermal necrosis, and RBC extravasation. In addition to these findings, destroyed blood vessels in the dermis were found to be surrounded by a dense inflammatory infiltrate. This destruction may obliterate the nutrient supply to the wart or destroy the rapidly dividing epidermal cells that contain HPV. Minimal destruction of the surrounding tissue is anticipated with long-pulsed Nd:YAG lasers.
In our study, the overall clearance rate was 96% (336 of the 348 treated warts were eradicated). The clearance rate of verruca vulgaris after the first treatment was very high (72.6%), whereas the clearance rate of deep palmopantar warts after the first treatment was low (44.1%). Most patients required repeated treatments. The average number of treatments required for clearance was 1.49. During a median follow-up period of 2.24 months (range, 2-10 months), 11 relapses were seen (recurrence rate 3.3%). This low recurrence rate seems to be due to the short follow-up period in this study; therefore, a study with a longer follow-up period and examination of recurrence is needed. The clearance rate after pulsed dye laser treatment, which employs the same mechanism of action as the Nd:YAG laser, has been reported to be 48% to 92% (1-4), while the laser used in the current study showed a higher clearance rate (96%). Therefore, a comparative study between these two types of lasers is required.
Side effects noted in our study included transient pain during treatment (82%), posttreatment numbness (15%), hemorrhagic bullae (7%), hyperpigmentation (5%), and hypopigmentation (4%). A crust formed in most patients and was removed within 1 to 2 weeks. Side effects were generally mild and did not prevent normal activity.
In conclusion, long-pulsed Nd:YAG lasers are a safe and effective treatment for warts, with response rates higher than those obtained with conventional therapies. No single optimal treatment has been inclicated for warts; therefore, long-pulsed Nd:YAG lasers should be considered a reasonable addition to the therapeutic options available. Future studies examining optimal laser parameters and treatment intervals would expand our knowledge on how best to use long-pulsed Nd:YAG laser therapy in managing warts.
Fig. 6.
(A) Deep palmoplantar wart three days after treatment. (B) After one week. (C) After two weeks.
References
- 1.Robson KJ, Cunningham NM, Kruzan KL, Petal DS, Kreiter CD, O'Donnell MJ, Arpey CJ. Pulsed-dye laser versus conventional therapy in the treatment of warts: a prospective randomized trial. J Am Acad Dermatol. 2000;43:275–280. doi: 10.1067/mjd.2000.106365. [DOI] [PubMed] [Google Scholar]
- 2.Kopera D. Verrucae vulgares: flashlamp-pumped pulsed dye laser treatment in 134 patients. Int J Dermatol. 2003;42:905–908. doi: 10.1046/j.1365-4362.2003.01994.x. [DOI] [PubMed] [Google Scholar]
- 3.Kenton-Smith J, Tan ST. Pulsed dye laser therapy for viral warts. Br J Plast Surg. 1999;52:554–558. doi: 10.1054/bjps.1999.3121. [DOI] [PubMed] [Google Scholar]
- 4.Ross BS, Levine VJ, Nehal K, Tse Y, Ashinoff R. Pulsed dye laser treatment of warts: an update. Dermatol Surg. 1999;25:377–380. doi: 10.1046/j.1524-4725.1999.07165.x. [DOI] [PubMed] [Google Scholar]
- 5.Wiess RA, Wiess MA. Early clinical results with a multiple synchronized pulse 1064 NM laser for leg telangiectasias and reticular veins. Dermatol Surg. 1999;25:399–402. doi: 10.1046/j.1524-4725.1999.08268.x. [DOI] [PubMed] [Google Scholar]
- 6.Sarradet DM, Hussain M, Goldberg DJ. Millisecond 1064-nm neodymium: YAG laser treatment of facial telangiectases. Dermatol Surg. 2003;29:56–58. doi: 10.1046/j.1524-4725.2003.29008.x. [DOI] [PubMed] [Google Scholar]
- 7.Bekhor PS. Long-pulsed Nd:YAG laser treatment of venous lakes: report of a series of 34 cases. Dermatol Surg. 2006;32:1151–1154. doi: 10.1111/j.1524-4725.2006.32253.x. [DOI] [PubMed] [Google Scholar]
- 8.Cobb MW. Human papillomavirus infection. J Am Acad Dermatol. 1990;22:547–566. doi: 10.1016/0190-9622(90)70073-q. [DOI] [PubMed] [Google Scholar]
- 9.Bunney MH, Nolan MW, Williams DA. An assessment of methods of treating viral warts by comparative treatment trials based on a standard design. Br J Dermatol. 1976;94:667–679. doi: 10.1111/j.1365-2133.1976.tb05167.x. [DOI] [PubMed] [Google Scholar]
- 10.Gibbs RC, Scheiner AM. Long-term follow-up evaluation of patients with electrosurgically treated warts. Cutis. 1978;21:383–384. [PubMed] [Google Scholar]
- 11.Shumer SM, O'Keefe EJ. Bleomycin in the treatment of recalcitrant warts. J Am Acad Dermatol. 1983;9:91–96. doi: 10.1016/s0190-9622(83)70112-x. [DOI] [PubMed] [Google Scholar]
- 12.Street ML, Roenigk RK. Recalcitrant periungual verrucae: the role of carbon dioxide laser vaporization. J Am Acad Dermatol. 1990;23:115–120. doi: 10.1016/0190-9622(90)70195-n. [DOI] [PubMed] [Google Scholar]
- 13.Tan OT, Hurwitz RM, Stafford TJ. Pulsed dye laser treatment of recalcitrant verrucae: a preliminary report. Laser Surg Med. 1993;13:127–137. doi: 10.1002/lsm.1900130120. [DOI] [PubMed] [Google Scholar]
- 14.Brodell RT, Bredle DL. The treatment of palmar and plantar warts using natural alpha interferon and a needleless injector. Dermatol Surg. 1995;21:213–218. doi: 10.1111/j.1524-4725.1995.tb00155.x. [DOI] [PubMed] [Google Scholar]
- 15.Yilmaz E, Alpsoy E, Basaran E. Cimetidine therapy for warts: a placebo-controlled, double blind study. J Am Acad Dermatol. 1996;34:1005–1007. doi: 10.1016/s0190-9622(96)90279-0. [DOI] [PubMed] [Google Scholar]
- 16.Edwards L. Imiquimod in clinical practice. Australas J Dermatol. 1998;39(Suppl 1):S14–S16. [PubMed] [Google Scholar]
- 17.Allington HV. Liquid nitrogen in the treatment of skin diseases. Calif Med. 1950;72:153–155. [PMC free article] [PubMed] [Google Scholar]
- 18.Zacarian SA. Liquid nitrogen in dermatology. Cutis. 1965;1:237–242. [Google Scholar]
- 19.Hengge UR, Esser S, Schultewolter T, Behrendt C, Meyer T, Stockfleth E, Goos M. Self-administered topical 5% imiquimod for the treatment of common warts and molluscum contagiosum. Br J Dermatol. 2000;143:1026–1031. doi: 10.1046/j.1365-2133.2000.03777.x. [DOI] [PubMed] [Google Scholar]
- 20.Coskey RJ. Treatment of plantar warts in children with a salicylic acid-podophyllin-cantharidin product. Pediatr Dermatol. 1984;2:71–73. doi: 10.1111/j.1525-1470.1984.tb00446.x. [DOI] [PubMed] [Google Scholar]
- 21.Gibbs S, Harvey I, Sterling JC, Stark R. Local treatments for cutaneous warts. Cochrane Database Syst Rev. 2003;3:CD001781. doi: 10.1002/14651858.CD001781. [DOI] [PubMed] [Google Scholar]
- 22.Munn SE, Higgins E, Marshall M, Clement M. A new method of intralesional bleomycin therapy in the treatment of recalcitrant warts. Br J Dermatol. 1996;135:969–971. doi: 10.1046/j.1365-2133.1996.d01-1104.x. [DOI] [PubMed] [Google Scholar]
- 23.Xiaowei X, Erickson LA, Elder DE. Disaese caused by viruses. In: Elder D, Elenitsas R, Johnson B Jr, Murohy GF, editors. Lever's histopathology of the skin. Philadelphia: JB Lippincott; 1997. pp. 651–679. [Google Scholar]