Abstract
Previous studies have established the therapeutic efficacy of humanized E16 (hE16) monoclonal antibody against West Nile virus (WNV) in animals. Here, we assess the potential for WNV strains encoding mutations in the hE16 epitope to resist passive immunotherapy and for the selection of neutralization escape variants during hE16 treatment. Resistance to hE16 in vivo was less common than expected, as several mutations that affected neutralization in vitro did not significantly affect protection in mice. Moreover, emergence of resistant variants after infection with fully sensitive virus occurred but was relatively rare, even in highly immunocompromised B and T cell-deficient RAG mice.
Keywords: West Nile virus, Flavivirus, passive immunotherapy, neutralization escape, monoclonal antibody
West Nile virus (WNV) is a mosquito-borne flavivirus that has emerged as the primary cause of epidemic encephalitis in the United States. Although case numbers have declined somewhat since the peak activity of 2002 and 2003, virus transmission continues throughout the continental United States and thousands of cases of neurological disease have been reported each year since 2004. At present there is no WNV vaccine or antiviral therapy approved for use in humans, although promising treatment results were observed in case reports using purified immunoglobulin derived from Israeli donors [1, 2].
The potential of passive immunotherapy for treatment of WNV infection has led to the development and evaluation of potently neutralizing human or humanized mouse monoclonal antibodies (mAbs) [3, 4]. One therapeutic candidate, hE16, binds to a highly conserved epitope on the upper lateral ridge of WNV envelope (E) protein domain III (E-DIII) and neutralizes WNV at low stoichiometric occupancy apparently by inhibiting conformational changes in E that are required for fusion of the virus with host cell membranes [3, 5, 6]. However, mapping studies by several groups have identified mutations in the hE16 epitope that significantly reduce or abolish binding of this and other neutralizing WNV mAbs [3, 7–9]. A few of these mutations are found in WNV strains isolated in the field [8] suggesting that the efficacy of hE16 could be limited. Furthermore, flaviviruses have an error-prone genome replication, which results in significant genetic diversity within any individual isolate. Indeed, this property has been used as the basis for in vitro selection of variants resistant to a particular selective pressure, such as that imposed by antiviral inhibitors or neutralizing mAbs. The potential for in vivo selection of mAb-resistant variants of flaviviruses has not yet been examined in detail.
In this study, we assessed (1) the potential for WNV strains encoding engineered mutations in the hE16 binding site to resist passive immunotherapy with hE16 in two mouse models of WNV neuroinvasive disease, and (2) the potential for neutralization resistant variants to be selected in vivo during hE16 treatment.
Methods
All WNV strains and infectious clone-derived variants used in this study (Table 1 and Results) were grown and plaque titrated on Vero cells. Neutralization assays were performed on Vero or BHK-21 cells, as previously described [3]. RNA extractions, RT-PCR and nucleotide sequencing of the pre-membrane (prM) and E coding regions of WNV genomes were performed using protocols and primers as previously described [7].
Table 1.
Outcomes of infections with West Nile virus strains/variants following pre- or post-exposure treatment with neutralizing mAb hE16.
| hE16 treated | PBS only | ||||||
|---|---|---|---|---|---|---|---|
| Mouse strain | hE16 Treatment* | Virus | % survivors | AST±sd† | % survivors | AST±sd | Survival P value‡ |
| Swiss Webster | 100µg day −1 | NY99 wt | 100 | n/a | 20 | 8.4±1.2 | 0.0003 |
| NY99ic T332A | 100 | n/a | 10 | 8.1±0.3 | <0.0001 | ||
| NY99ic T332M | 90 | 8.0±0.0 | 0 | 8.4±0.8 | <0.0001 | ||
| NY99ic T332K | 30 | 7.4±0.8 | 10 | 8.8±1.5 | 0.8984 | ||
| NY99ic T330I | 90 | 8.0±0.0 | 0 | 7.8±0.4 | 0.0008 | ||
| SA58 | 0 | 7.2±0.4 | 0 | 7.5±0.5 | 0.1704 | ||
| SA58 K332T | 100 | n/a | 0 | 7.5±0.7 | <0.0001 | ||
| C57BL/6 | 100µg day +2 | NY99ic wt | 100 | n/a | 30 | 11.0±1.7 | <0.0001 |
| NY99ic T332A | 100 | n/a | 20 | 9.3±1.9 | 0.0003 | ||
| NY99ic T332M | 100 | n/a | 30 | 10.7±1.6 | <0.0001 | ||
| NY99ic T330I | 100 | n/a | 10 | 9.4±1.8 | <0.0001 | ||
| SA58 | 10 | 10.8±1.6 | 0 | 9.3±1.1 | 0.0207 | ||
| SA58 K332T | 100 | n/a | 10 | 10.2±1.4 | <0.0001 | ||
| Swiss Webster | 100µg day −1 | NY99 K307E | 10 | 8.8±1.3 | 0 | 7.8±0.4 | 0.0773 |
| NY99 T332M | 70 | 13.3±3.8 | 0 | 8.0±0.7 | 0.0001 | ||
Swiss Webster mice were treated with 100µg hE16 or PBS only, then challenged 1 day later with 100 PFU of indicated WNV strains (1000 pfu for NY99ic T332K). C57BL/6 mice were inoculated with 100 PFU of indicated WNV strains, then treated 2 days later with 100 µg hE16 or with PBS only. n=10 for each virus/treatment group, except for NY99 K307E/T332M “PBS only” groups, where n=5.
AST – average survival time; sd – standard deviation; n/a – not applicable
Significant differences in survival curves for hE16 treated vs. PBS only groups determined by log rank test using the Prism application (Graphpad Software).
Swiss Webster mice (female, 3–4 weeks of age) were obtained from Harlan Laboratories; C57BL/6 wild type and congenic RAG mice (female, 5 weeks of age) were obtained from The Jackson Laboratory. All mice were housed in AAALAC accredited animal biosafety level 3 (ABSL3) facilities and experiments were conducted under protocols approved by the Animal Care and Use Committee of the University of Texas Medical Branch or Washington University School of Medicine. Details of individual passive protection experiments are described below.
Results
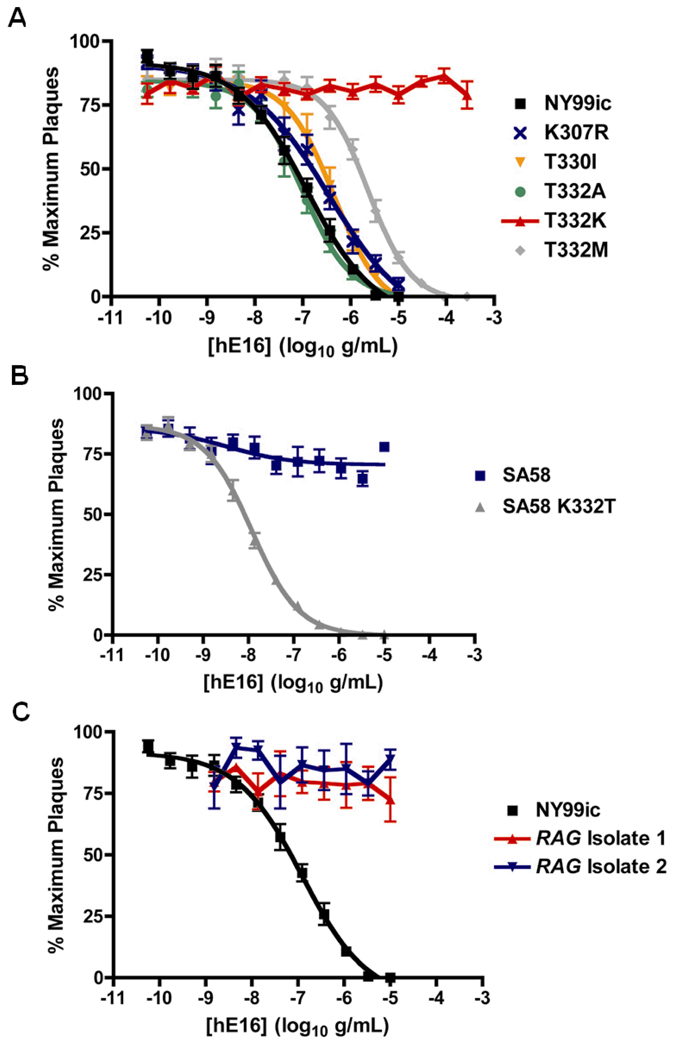
Previous crystallographic and epitope mapping studies suggested that hE16 had key contacts at residues 307, 330, and 332 of the WNV E protein [3, 5]. The ability of hE16 to neutralize selected WNV strains and NY99 infectious clone-derived variants encoding single amino acid changes at these residues was initially assessed by a plaque reduction neutralization assay on Vero cells. These viruses were shown previously to variably escape neutralization by other anti-WNV E-DIII specific neutralizing mAbs [7, 8]. Notably, only a mutation T332K resulted in substantial loss of hE16 neutralizing activity, whereas other mutations (K307R, T330I, T332A/M) showed only modest changes in neutralization compared to the wild-type lineage 1 NY99 virus (Figure 1a). Lineage 2 South African strain H442 (SA58), isolated in 1958 from a human patient, normally encodes a lysine at residue 332 and was previously reported to be resistant to neutralization by several E-DIII-reactive antibodies raised against NY99 [7]; this virus was also resistant to neutralization by hE16, whereas an SA58 variant encoding threonine at 332 [7] was efficiently neutralized (Figure 1b).
Figure 1.
Neutralization by mAb hE16 of: (a) lineage 1 WNV strain NY99ic and K307R, T330I and T332A/K/M variants; (b) lineage 2 WNV strain SA58 and K332T variant; and (c) K307E escape variants selected in vivo from hE16-treated RAG mice. The data are an average of two to four independent experiments performed in triplicate on (a, b) Vero or (c) BHK21–15 cells.
Two independent mouse challenge models were employed to assess the protection provided by hE16 against the neutralization sensitive and resistant WNV strains and variants. Groups of outbred Swiss Webster mice, which are highly susceptible to peripheral challenge with neuroinvasive WNV strains, were pre-treated with 100 µg doses of hE16 or PBS only and challenged 24 hours later with 102 plaque forming units (PFU) of each WNV strain/variant (equivalent to approximately 100 LD50s in each case). Alternatively, groups of inbred C57BL/6 mice, which are more resistant to WNV NY99 and have been used in previous evaluations of hE16 [3, 10] were challenged with 102 PFU of each virus and treated at two days post-infection with 100 µg hE16 or PBS only. The hE16 mAb afforded significant protection (90–100% survival) for mice in either the pre- or post-exposure model against NY99 and variants that were efficiently neutralized in vitro by hE16 (T330I, T332A/M). However, little or no protection was observed after challenge with the NY99ic T332K mutant or SA58 (Table 1).
Although mutagenesis of an infectious clone or in vitro selection can readily generate resistant viruses against hE16 and other mAbs, we questioned whether this occurred commonly under selective pressure during the course of treatment. To assess the potential for selection of resistant variants in vivo during mAb treatment, Swiss Webster mice pre-treated with 100 µg hE16 were exposed to a high dose (104 PFU) of NY99 virus. This challenge dose was chosen based on the known frequency of mAb escape variants selected from this virus population during earlier studies [7] and because this represents a virus dose reliably introduced during feeding by Culex spp. mosquitoes [11]. All untreated control animals succumbed by day 9 post-infection (average survival time 7.4±1.0 days). Two of ten treated mice showed signs of neuroinvasive disease and were euthanized on days 8 and 9. Virus was isolated from the brain of each mouse and these encoded single nucleotide changes in E coding for mutations K307E and T332M, respectively. Both retained the highly neuroinvasive phenotype of the parental NY99 virus (data not shown).
Immune dysfunction is a significant risk factor for development of severe WNV disease [reviewed in 12], suggesting that therapeutic antibodies and other treatments may be especially important for immunodeficient patients. To assess the potential for emergence of resistant variants during treatment of an immunocompromised host, a group of 30 B and T cell-deficient RAG mice was exposed to a low dose (102 PFU) of strain WNV-NY2000 (3000-0259), which has an E gene sequence identical to that of NY99 [13], and then treated with 500 µg doses of hE16 administered one day post-infection and at 14 day intervals thereafter. Whereas 24 mice remained healthy over a period of several months, six mice became ill and were found dead or were euthanized on days 18 (2 mice), 20 (2 mice), 32 and 34. Brains recovered from the latter two animals each yielded WNV encoding a K307E E protein mutation.
Consistent with previous studies [3], the recovered K307E variants were resistant to in vitro neutralization (Figure 1c) or in vivo protection (Table 1) by hE16, whereas the recovered T332M variant was only modestly resistant to E16 neutralization in vitro (not shown) or in vivo (Table 1), similar to the NY99ic T332M variant.
Discussion
The use of polyclonal or monoclonal immunotherapy is currently being explored for treatment of infections caused by many families of viruses and clearly offers a promising approach for post-exposure treatment of flavivirus infections. In the case of hE16 for treatment of WNV infections, the presence of naturally occurring mutations in some WNV strains at the mAb binding site suggests that treatment coverage will not be universal, as evidenced by resistance of lineage 2 strain SA58 in vitro and in vivo. Nonetheless, hE16 still afforded strong protection against variants encoding other mutations that increased resistance to neutralization but did not abolish binding. Analysis of more than 650 derived amino acid sequences in the NCBI Protein database representing human, avian, equine or mosquito North American WNV isolates during 1999–2005 identified none with amino acid variation at positions 307, 330, or 332, which could impair hE16 recognition and neutralization.
These studies have also demonstrated the potential for in vivo selection of mAb escape variants. Although surprisingly infrequent, in vivo resistance may occur via selection of a pre-existing mutant subpopulation following exposure to higher doses of virus, a phenomenon which has also recently been reported in passively immunized monkeys exposed to 106 PFU doses of dengue virus type 2 [14]. Alternatively, resistance can develop through the emergence of variant viruses during prolonged treatment.
The length of time required for the emergence of the resistant K307E variants following 102 PFU challenge in RAG mice (up to 34 days) compared with the rapid selection of variants from the 104 PFU challenge in Swiss Webster mice (8–9 days), was somewhat surprising. Based on the inherent error rate of the flavivirus RNA polymerase (approximately one mutation per genome replication), the occurrence of resistant mutations at the genetic level should be expected to occur rapidly. The delay in emergence of resistance in RAG mice could be explained by packaging of early variant genomes in virions that also contain sufficient levels of wild-type E protein that allow neutralization by hE16. This is possible because flavivirus RNA can be encapsidated by structural proteins in trans [15] and complete neutralization (>99%) of WNV virions by hE16 requires occupancy of less than 50% of the available epitopes [6]. Although further studies are necessary, high levels of circulating hE16 with a long half-life may adequately neutralize virions comprised of wild type and resistant E protein variants to prevent rapid or eventual emergence of pathogenic escape variants, even in a highly immunocompromised subject.
Overall, these findings suggest that resistance to neutralizing anti-WNV antibody therapy can occur in vivo, although at frequencies that are perhaps lower than anticipated based on analogous studies on resistance to antiviral drugs that target virus replication. However, our data suggest that clinical evaluation of hE16 and other mAb therapeutics for flavivirus infections should monitor for selection or emergence of resistant variants, especially in immunocompromised patients who are a likely target population for treatment of severe WNV infections. Such studies should include characterization of viral populations for detection of resistance and possibly, in some patients, the use of combinations of neutralizing antibodies that recognize distinct epitopes.
Acknowledgments
The authors thank S. Johnson and J. Nordstrom (MacroGenics, Inc) for preparation of the purified hE16 antibody.
This study was supported in part by the NIAID (R21 AI063468 to DWCB; U01-AI061373 and Contract No. HHSN266200600013C to MSD), and the Institute for Human Infections and Immunity at UTMB (to DWCB).
Footnotes
Potential conflicts of interest: M.S.D is a consultant for MacroGenics, Inc., which has licensed the E16 antibody from Washington University for potential clinical use. All other authors have no conflicts of interest.
The results of this study have not been reported at any scientific meeting.
REFERENCES
- 1.Shimoni Z, Niven MJ, Pitlick S, Bulvik S. Treatment of West Nile virus encephalitis with intravenous immunoglobulin. Emerg Infect Dis. 2001;7:759. doi: 10.3201/eid0704.010432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hamdan A, Green P, Mendelson E, Kramer MR, Pitlik S, Weinberger M. Possible benefit of intravenous immunoglobulin therapy in a lung transplant recipient with West Nile virus encephalitis. Transpl Infect Dis. 2002;4:160–162. doi: 10.1034/j.1399-3062.2002.01014.x. [DOI] [PubMed] [Google Scholar]
- 3.Oliphant T, Engle M, Nybakken GE, et al. Development of a humanized monoclonal antibody with therapeutic potential against West Nile virus. Nat Med. 2005;11:522–530. doi: 10.1038/nm1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Throsby M, Geuijen C, Goudsmit J, et al. Isolation and characterization of human monoclonal antibodies from individuals infected with West Nile Virus. J Virol. 2006;80:6982–6992. doi: 10.1128/JVI.00551-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nybakken GE, Oliphant T, Johnson S, Burke S, Diamond MS, Fremont DH. Structural basis of West Nile virus neutralization by a therapeutic antibody. Nature. 2005;437:764–769. doi: 10.1038/nature03956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pierson TC, Xu Q, Nelson S, et al. The stoichiometry of antibody-mediated neutralization and enhancement of West Nile virus infection. Cell Host Microbe. 2007;1:135–145. doi: 10.1016/j.chom.2007.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beasley DW, Barrett AD. Identification of neutralizing epitopes within structural domain III of the West Nile virus envelope protein. J Virol. 2002;76:13097–13100. doi: 10.1128/JVI.76.24.13097-13100.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li L, Barrett AD, Beasley DW. Differential expression of domain III neutralizing epitopes on the envelope proteins of West Nile virus strains. Virology. 2005;335:99–105. doi: 10.1016/j.virol.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 9.Sanchez MD, Pierson TC, McAllister D, et al. Characterization of neutralizing antibodies to West Nile virus. Virology. 2005;336:70–82. doi: 10.1016/j.virol.2005.02.020. [DOI] [PubMed] [Google Scholar]
- 10.Morrey JD, Siddharthan V, Olsen AL, et al. Humanized monoclonal antibody against West Nile virus envelope protein administered after neuronal infection protects against lethal encephalitis in hamsters. J Infect Dis. 2006;194:1300–1308. doi: 10.1086/508293. [DOI] [PubMed] [Google Scholar]
- 11.Styer LM, Kent KA, Albright RG, Bennett CJ, Kramer LD, Bernard KA. Mosquitoes inoculate high doses of West Nile virus as they probe and feed on live hosts. PLoS Pathog. 2007;3:1262–1270. doi: 10.1371/journal.ppat.0030132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Samuel MA, Diamond MS. Pathogenesis of West Nile Virus infection: a balance between virulence, innate and adaptive immunity, and viral evasion. J Virol. 2006;80:9349–9360. doi: 10.1128/JVI.01122-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ebel GD, Dupuis AP, 2nd, Ngo K, et al. Partial genetic characterization of West Nile virus strains, New York State, 2000. Emerg Infect Dis. 2001;7:650–653. doi: 10.3201/eid0704.010408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lai CJ, Goncalvez AP, Men R, et al. Epitope determinants of a chimpanzee dengue virus type 4 (DENV-4)-neutralizing antibody and protection against DENV-4 challenge in mice and rhesus monkeys by passively transferred humanized antibody. J Virol. 2007;81:12766–12774. doi: 10.1128/JVI.01420-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khromykh AA, Varnavski AN, Westaway EG. Encapsidation of the flavivirus kunjin replicon RNA by using a complementation system providing Kunjin virus structural proteins in trans. J Virol. 1998;72:5967–5977. doi: 10.1128/jvi.72.7.5967-5977.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]