Abstract
Background
Self-reported cognitive and memory complaints following coronary artery bypass graft surgery (CABG) are common. Several studies have attempted to quantify the incidence of such complaints and to examine the relationship between subjective and objective cognitive functioning, but the etiology and longitudinal course of these self-reports remain unclear.
Methods
Measures of subjective memory complaints were compared in two groups: 220 CABG patients and 92 nonsurgical cardiac comparisons at 3 months, and 1, 3, and 6 years. At 6 years, additional measures were used to quantify memory self-assessment. The frequency of subjective complaints at each time point was determined and associations with objective cognitive performance as well as depression were examined.
Results
At early (3-month and/or 1-year) follow-up, subjective memory complaints were reported more often by the CABG than the nonsurgical group (45.5% vs. 17.0%, p<0.0001). By 6 years, the frequency of complaints was similar (52%) in both groups. Subjective memory ratings were significantly correlated with performance on several memory tests at 6 years. This relationship was not confounded by depression.
Conclusions
Subjective memory complaints are more frequent early in follow-up in patients undergoing CABG than in controls, but by 6 years they are similar. The increase in subjective complaints over time may be related to progression of underlying cerebrovascular disease. Unlike previous studies, we found that subjective memory assessments were correlated with objective performance on several memory tests. Although subjective memory complaints are more common in patients with depression, they cannot be explained by depression alone.
Keywords: CABG, neurocognitive deficits, outcomes, brain
INTRODUCTION
Complaints of cognitive problems, especially memory, are frequently reported by patients who have had coronary artery bypass surgery (CABG). In part on the basis of the lack of correlation between subjective symptoms and objective neuropsychological test findings, previous studies have suggested that self-reported memory symptoms reflect underlying depression.(1;2) Nonetheless, since most of these studies involved only patients undergoing CABG, the possibility that patients with coronary artery disease who did not have surgery might also develop memory symptoms was not examined. Therefore, in a previous study(3) we compared subjective memory complaints in patients undergoing CABG with those in patients with angiographically proven coronary artery disease but without surgery over a 12-month period. We found that those undergoing CABG were more likely to report memory changes at 3 and 12 months after baseline. Moreover, these differences remained even after adjustment for demographic variables and for depression.
In attempting to define further the time course and mechanism underlying subjective complaints among CABG patients, the present report is an extension of our previous study by continuing to evaluate their memory complaints in greater detail. Among several questions raised by the previous study we considered whether the difference in subjective memory complaints between the CABG and nonsurgical comparison group persisted over time (primary outcome), and if so, were subjective memory complaints a manifestation of depression. We also considered the possible predictive value of early subjective complaints with respect to long term outcome and cognitive decline. Lastly, as we have previously reported no differences in cognitive change at 6 years between the CABG and nonsurgical comparison patients,(4) we wished to determine whether there were correlations between subjective memory reports and level of cognitive performance at 6 years or change in cognitive performance from baseline to 6 years, as measured by objective tests (secondary outcome). Answers to these questions may provide insight into the origin of the memory complaints that are of considerable concern to patients undergoing CABG surgery.
PATIENTS AND METHODS
Patients
Three groups of patients with coronary artery disease were included in this observational, longitudinal study: 152 conventional on-pump coronary artery bypass grafting surgery patients; 68 “off-pump” coronary artery bypass patients; and 92 nonsurgical cardiac comparison (NSCC) patients. The nonsurgical comparison patients, recruited from the cardiology group at our institution all had stable, diagnosed, medically managed coronary disease, but did not have cardiac surgery at the time of enrollment. These populations are described elsewhere in detail.(5) The study was originally approved by the institutional review board on July 14, 1997 (to include baseline, and 3 & 12 month visits) and all patients gave written informed consent. The 3 year follow-up was approved on September 22, 2000 and the 6 year follow-up on July 28, 2003.
Study design and cognitive testing
All patients were seen on the following timeline: baseline, 3 month, and 1, 3, and 6 years. Subjective memory symptoms, our primary outcomes, were assessed in the following 3 ways: yes/no complaint, Likert scale, and Lund questionnaire. At each follow-up time point (3 months, and 1, 3, and 6 years) patients were asked if they felt as though their memory had become worse (yes/no complaint) since their previous visit. This question was asked prior to cognitive testing. In addition at 6 years, a more extensive evaluation of subjective complaints was given. This included a Likert scale, in which patients were asked to rank their memory (as it is today) on a scale of 1 to 10 (10 being the best memory score). This ranking was completed prior to the actual cognitive testing.
Following the cognitive test battery, patients completed a 7-item memory questionnaire, (from the Lund questionnaire)(6). Patients were asked if each of the following memory items had become better (score of +1), worse (score of -1), or remained the same (score of 0) when comparing their memory today to 6 years ago, before the study started. The seven memory items were: remembering appointments; remembering whether you’ve taken your medication; remembering names of persons and places; remembering items on a grocery list; remembering telephone numbers; walking into a room and forgetting what you wanted to do there; Is it easier to remember things today than before the start of our study (6 years ago)? The scores to these 7 items were summed for a total memory score and were therefore focused on change in memory from baseline to 6 year follow-up. Thus, a negative score indicated that overall the patient’s memory was worse over time.
Patients completed a cognitive test battery (16 tests/subtests as shown in Table 4), that measured 8 cognitive areas: verbal memory, visual memory, visuoconstruction, language, motor speed, psychomotor speed, attention, and executive function(7). Additional questionnaires that were completed at all study time points include: The Center for Epidemiological Study of Depression (CES-D)(8), a measure of depression; the Mini-Mental Status Exam(9), a global measure of cognitive function; and the Beth Israel Functional Status questionnaire(10), which measured physical functioning. At the 6-year time point, we included the Letter-Number sequencing test, which is a measure of working memory.(11)
Table 4.
Data Analysis of Subjective Memory Complaints and Objective Neuropsychological Testing using Pearson*
| Cross-sectional Dataa | Change Datab | ||
|---|---|---|---|
| Cognitive Domains and Neuropsychological Test Components | Correlation between Likert score and 6 year cognitive score (95%CI) | Sample Partial Correlation between Likert score and 6 year score given CESD (95%CI) | Correlation between Lund score and change in actual cognitive scores from baseline to 6 years (95% CI) |
| Verbal Memory | |||
| RAVLT - total score | .24 (.09, .38) | .28 (.14, .41) | .18 (.04, .33) |
| RAVLT – delayed recall | .17 (.02, .31) | .20 (.05, .34) | |
| RAVLT – retention | .16 (.01, .30) | ||
| RAVLT – recognition | |||
| Visual Memory | |||
| RCF – retention | .18 (.03, .32) | ||
| RCF – delayed recall | .17 (.02, .32) | ||
| Visuoconstruction | |||
| RCF – copy | .16 (.01, .30) | ||
| Block design | |||
| Language | |||
| Boston Naming | .17 (.02, .31) | .26 (.11, .39) | |
| Motor Speed | |||
| Pegboard – dominant | .23 (.09, .37) | ||
| Pegboard – non-dom | |||
| Psychomotor Speed | |||
| Trail Making – Part A | .20 (.05, .34) | ||
| Written Alphabet | .18 (.03, .32) | ||
| Attention | |||
| RAVLT – Trial 1 | .15 (.00, .29) | .17 (.02, .31) | |
| Mini-mental – attention | |||
| Executive Function | |||
| Trail Making – Part B | |||
| Working Memory | |||
| Letter-Number | .18 (.03, .32) | n/a | |
| sequencing task | |||
Cognitive test scores adjusted for age, gender, education;
for this cross-sectional analysis, we asked: Are there correlations between the Likert memory scale score, which asks patients to rank their memory at their 6 year visit, and their 6 year cognitive test scores? For the Likert memory scale score – subjects were asked to rank their memory on a scale of 1-10 (with 10 being the best memory score) at their 6 year visit.
For this change analysis, we asked: Are there correlations between the Lund memory questionnaire score, which asks patients to compare their memory at 6 years to before the study started and the change in their cognitive test scores from baseline to 6 years? Lund memory score is a composite of 7-items (from the Lund questionnaire)(6). Patients were asked if each of the memory items had become better (score of +1), worse (score of -1), or remained the same (score of 0) when comparing their memory today to 6 years ago, before the study started. CES-D is the depression index score (8).
Statistical analysis
For our initial analysis, we compared the demographic and medical characteristics of the CABG group and the nonsurgical comparison group using T-test and Chi-square test of the null hypothesis that the means or proportions were the same in the two groups respectively.
For our primary outcome, we estimated the frequency of subjective memory complaints at each follow-up time point for the two groups with 95% confidence intervals and the odds ratio at each time with its confidence interval using logistic regression and generalized estimating equations (GEE)(12) to account for the correlation among repeated measures on a person. In this analysis we controlled for age, gender, education level, and baseline depression score. This is an analysis of variance model with treatment group, time, and the time by treatment interaction, controlling for potential confounders because this is an observational rather than randomized study.
We measured the strength of linear association between subjective complaints, as measured by the Likert scale at 6 years and each objective cognitive test at 6 years, by estimating the Pearson correlation coefficient between these two continuous measures. As we have previously determined that there are no differences in objective cognitive test performance between the CABG and nonsurgical comparison patients at 6 years,(4) we then combined these groups and correlations were calculated for both the Likert score and the change in z-score from baseline to 6 years on each cognitive test (secondary outcome). To assure that the correlation was not affected by depression, we also calculated the Pearson correlation after both measures were linearly adjusted for the CES-D score at the 6-year time point.
RESULTS
Comparison of “on-pump” and “off-pump” patients
The frequencies of subjective complaints were essentially the same in the two surgical groups at all time points, as follows: 3 months: on-pump 27.0%(33/122), off-pump 26.4%(14/53); 1 year; on-pump 37.8%(48/127), off-pump 31.4%(16/51); 3 years: on-pump 47.4%(36/76), off-pump 41.4%(12/29); 6 years: on-pump 51.5%(50/97), off-pump 56.1%(23/41). As none of these differences were statistically significant, these two surgical groups were combined for all the further analyses shown below and from this point forward will be referred to as the CABG group.
Demographic comparison and frequency of subjective complaints by study group
There were some differences in medical history variables between the CABG and nonsurgical comparison group at baseline as shown in Table 1. At each follow-up time point, the frequency of memory complaints is shown on the following schedule (3 months 1, 3, and 6 years): for CABG – 26.9%, 36.0%, 45.7%, 52.9%; and for the nonsurgical comparison group – 6.0%, 15.3%, 29.0%, 51.6%. These differences between the groups are statistically significant (see Table 2), except at 6 years. When examining the early complaints together (at either 3 month and/or 1 year), the CABG patients have more subjective complaints (45% vs. 17%; p<0.0001). The number of complaints increased for both groups over time. The probabilities of subjective complaints at each follow-up point are shown by group in Figure 1. In addition, at 6 years, the mean scores for the Likert scale memory ranking and Lund questionnaire were not significantly different between the groups. Therefore, these data show that while the CABG group has more complaints in the early (3-month and 1-year) time periods, the frequency of memory complaints in both groups equalizes over time.
Table 1.
Comparison of patient characteristics between study groups
|
Variables Baseline (preoperative) Data |
NSCC Group (n = 92) |
CABG Group (n = 220) |
p-value* |
|---|---|---|---|
| Gender | |||
| Male | 77.2% | 73.6% | |
| Female | 22.8% | 26.4% | |
| Non-white race | 6.5% | 9.1% | |
| Less than high school education | 16.3% | 20.9% | |
| On antidepressant | 13.0% | 11.0% | |
| History of past stroke or TIA | 5.4% | 9.5% | |
| History of hypertension | 50.0% | 65.5% | 0.008 |
| History of diabetes mellitus | 22.8% | 31.4% | |
| History of peripheral vascular disease | 6.6% | 20.0% | 0.002 |
| History of myocardial infarction | 48.9% | 49.1% | |
| History of angina | 60.9% | 79.1% | 0.001 |
| History of atrial fibrillation | 14.6% | 13.2% | |
| Family history of Alzheimer’s disease | 9.8% | 12.8% | |
| History of smoking | 55.4% | 70.0% | 0.01 |
| History of PTCA | 53.3% | 21.8% | 0.0001 |
| Apo-e4 present | 32.2% | 25.9% | |
| Mean age (years) | 65.9 (±9.2) | 64.6 (±9.8) | |
| Mean education (years) | 14.4 (±3.4) | 13.9 (±3.8) | |
| Mean # of disease coronary arteries | 1.95 (±0.8) | 2.66 (±0.6) | 0.0001 |
| Three vessel coronary disease | 26.8% | 72.0% | 0.0001 |
| Mean systolic blood pressure (mmHg) | 141 (±26) | 131 (±21) | 0.001 |
| Mean diastolic blood pressure(mmHg) | 79 (±13) | 72 (±11) | 0.0001 |
| Ave. mean arterial pressure (mmHg) | 100 (±16) | 92 (±13) | 0.0001 |
| Interim Follow-up Time Point Datac | |||
| 3 month | |||
| Died | 1/92 (1%) | 3/220 (1%) | |
| Refused/No contact | 7 (8%) | 47 (22%) | |
| Interviewed/tested | 84 (92%) | 170 (78%) | |
| Chest pain | 16 (19%) | 27 (16%) | |
| Myocardial infarction | 1 (1%) | 3 (2%) | |
| Redo cardiac angiogram | 2 (2%) | 6 (3%) | |
| PTCA | 1 (1%) | 2 (1%) | |
| 1 year | |||
| Died | 3/92 (3%) | 8/220 (4%) | |
| Refused/No contact | 5 (6%) | 32 (18%) | |
| Interviewed/tested | 84 (94%) | 174 (82%) | |
| Chest pain | 24 (29%) | 36 (21%) | |
| Myocardial infarction | 0 | 0 | |
| Redo cardiac angiogram | 4 (5%) | 8 (5%) | |
| PTCA | 1 (1%) | 3 (2%) | |
| 3 Year | |||
| Died | 6/92 (6%) | 20/220 (9%) | |
| Refused/No contact | 26 (30%) | 98 (49%) | |
| Interviewed/tested | 60 (70%) | 102 (51%) | |
| Chest pain | 22 (37%) | 24 (23%) | |
| Myocardial infarction | 1 (2%) | 2 (2%) | |
| Redo cardiac angiogram | 11 (18%) | 17 (17%) | |
| PTCA | 7 (12%) | 5 (5%) | |
| Had CABG surgery since last visit | 3 (5%) | 0 | |
| 6 Year | |||
| Died | 19/92 (21%) | 42/220 (19%) | |
| Refused/No contact | 12 (16%) | 42 (24%) | |
| Interviewed/tested | 61 (84%) | 136 (76%) | |
| Chest pain | 21 (34%) | 40 (29%) | |
| Myocardial infarction | 1 (2%) | 4 (3%) | |
| Redo cardiac angiogram | 13 (21%) | 24 (18%) | |
| PTCA | 5 (8%) | 10 (7%) | |
| Had CABG surgery since last visit | 7 (11%) | 0 |
only significant values shown;
not all patients were seen at each interim follow-up;
CABG – includes both on- and off-pump coronary artery bypass patients; NSCC – nonsurgical cardiac comparison; PTCA – percutaneous transluminal coronary angioplasty; TIA – transient ischemic attack
Table 2.
Test/Questionnaire scores at each study time point
| Test | Group | Baseline | 3 Month | 1 Year | 3 Year | 6 Year |
|---|---|---|---|---|---|---|
| NSCC | N = 92 | n = 84 | n = 84 | n = 60 | n = 61 | |
| CABG | N = 220 | n = 170 | n = 174 | n = 102 | n = 136 | |
| Mean Mini-Mental Status Exam score a | NSCC | 28.0 (±2.0) | 28.4 (±1.8) | 28.5 (±1.5) | 28.3 (±1.7) | 28.0 (±2.4) |
| CABG | 27.6 (±2.3) | 28.1 (±2.1) | 28.0 (±2.2) | 28.5 (±1.5) | 27.7 (±2.4) | |
| Mini-Mental Status Exam score <24 | NSCC | 6.5% | 3.6% | 2.4% | 1.7% | 8.2% |
| CABG | 4.6% | 3.0% | 2.9% | 1.0% | 5.9% | |
| Mean Functional Status Score b | NSCC | 33.0 (±3.9) | 32.6 (±4.1) | 32.2 (±4.6) | 31.4 (±5.2) | 32.1 (±5.5) |
| CABG | 30.3 (±5.3) * | 32.1 (±4.5) | 32.2 (±4.7) | 31.5 (±5.1) | 30.4 (±6.0) | |
| Mean CES-D score c | NSCC | 8.8 (±7.6) | 8.1 (±7.0) | 7.7 (±7.5) | 6.9 (±6.4) | 9.0 (±8.9) |
| CABG | 13.2 (±9.8) * | 10.2 (±9.9) | 9.1 (±9.8) | 8.9 (±9.5) | 10.1 (±9.4) | |
| Depressed (CES-D >15) | NSCC | 15.2% | 10.7% | 16.7% | 11.9% | 14.8% |
| CABG | 32.4% * | 24.1% * | 17.3% | 11.8% | 16.8% | |
| (Yes/No) Subjective memory complaint | NSCC | - | 6.0% | 15.3% | 29.0% | 51.6% |
| CABG | 26.9% * | 36.0% * | 45.7% | 52.9% | ||
| Mean Lund questionnaire score d | NSCC | - | - | - | - | -2.84 (±2.4) |
| CABG | -2.47 (±2.2) | |||||
| Mean Likert scale score e | NSCC | - | - | - | - | 7.08 (±1.7) |
| CABG | 6.87 (±1.7) |
indicates statistically significant differences (p<0.01);
Mini-Mental Status Exam score maximum = 30 (9);
Higher scores equated with better physical functioning (maximum score = 36) (10);
Higher CES-D scores (Center for Epidemiological Studies of Depression) (8) equated with depressive symptoms;
Lund questionnaire – memory items (6);
on the likert scale we asked patients to rank their memory (as it is today), on a scale from 1-10, with 10 being the best.
CABG – includes both on- and off-pump coronary artery bypass patients; NSCC – nonsurgical cardiac comparison group
Figure 1.
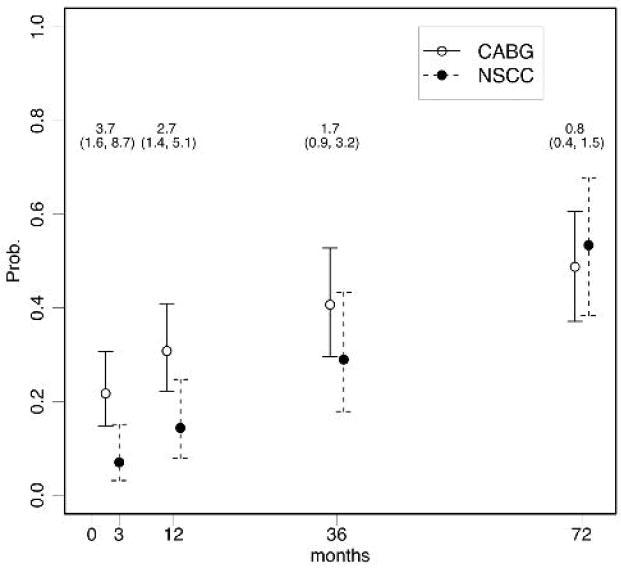
Risk-adjusted probability of having a (yes/no) memory complaint at each study follow-up time point. The CABG group is a combination of conventional and off-pump surgical patients. NSCC is the nonsurgical comparison group. Odds ratios are shown above the bars and 95% confidence intervals are shown in parentheses. In all situations, except at 72 months (6 years), the CABG group has greater odds of a memory complaint than the nonsurgical comparison group. Data are adjusted for age, gender, education and CES-D score at baseline.
Depression status and differences in subjective complaints between study groups
As shown in Table 2, at both baseline and 3-month follow-up, the CABG group had significantly more depressive symptoms than did the nonsurgical comparison group. This difference was not found at later follow-up times, however, and the frequency of depressive symptoms decreased over time. Next, we sought to determine if depression played a role in the difference in subjective complaints between the CABG and nonsurgical groups at each time point. This comparison is shown in Table 3. Although we found that depressed patients tended to have more memory complaints, depression does not account for the differences between the CABG and nonsurgical groups. At 3 months, even after adjusting for baseline CES-D score, the odds of a CABG patient having a subjective complaint is 3.7 times higher than that of a nonsurgical comparison patient (95%CI 1.6, 8.7), see Figure 1. When we adjusted for CES-D score at each corresponding follow-up time point, the odds of having a subjective complaint were essentially unchanged (data not shown). Thus, depression does not explain the differences in subjective complaints between the two groups.
Table 3.
Comparison of surgical and nonsurgical groups and the relationship of subjective complaints to depression status* at each study follow-up time
| Patients with depressive symptoms | NSCC | CABG | p-value | NSCC | CABG | p-value |
|---|---|---|---|---|---|---|
| No memory complaint at 3 month | Memory complaint at 3 month | |||||
| At 3 months | (7/79) | (21/125) | (2/5) | 20/45 | ||
| 8.9% | 16.8% | 0.079 | 40.0% | 44.4% | 0.616 | |
| No memory complaint at 1 year | Memory complaint at 1 year | |||||
| At 1 year | (7/71) | (10/111) | (7/13) | (20/62) | ||
| 9.9% | 9.0% | 0.521 | 53.8% | 32.3% | 0.125 | |
| No memory complaint at 3 year | Memory complaint at 3 year | |||||
| At 3 years | (3/42) | (4/54) | (4/17) | (8/48) | ||
| 7.1% | 7.4% | 0.639 | 23.5% | 16.7% | 0.383 | |
| No memory complaint at 6 year | Memory complaint at 6 year | |||||
| At 6 years | (3/30) | (7/64) | (6/31) | (16/73) | ||
| 10.0% | 10.9% | 0.600 | 19.4% | 21.9% | 0.496 | |
depression status determined by using the CES-D (8) score in which a cut-off >15 is indicative of depressive symptoms.
CABG – includes both on- and off-pump coronary artery bypass patients; NSCC – nonsurgical cardiac comparison group
Early subjective memory complaints and long-term subjective (6-year) follow-up
Since we determined that there were no differences in subjective complaints between the CABG and nonsurgical groups at 6 years, we combined the groups and examined the patients based on their memory complaint status. Patients who had early memory complaints (at 3 months and/or 1 year) were significantly more likely to have memory complaints at 6 years compared to those who did not have an early complaint (51.5% vs. 22.2%, p<0.0001). Those with early complaints were also more likely to have lower functional status scores at 6 years (29.5 vs. 32.0, p<0.01). In addition, early complaints predicted worse Likert scale ranking (6.3 vs. 7.2, p<0.001), and worse memory scores on the Lund questionnaire (-3.6 vs. -2.0, p<0.0001). These data show that there are consistent associations between patient perception about their memory at early follow-up, and how they rate themselves at long-term follow-up.
Early subjective memory complaints and long-term cognitive outcomes
Using Pearson correlation coefficients, we asked whether or not early subjective memory complaints predict late cognitive decline at 6 years. For each cognitive test, the z-score changes from 1- to 6-year follow-up were compared between those with and without early complaints. There were no statistically significant correlations. Therefore, despite some nonsignificant trends, we were not able to demonstrate that early memory complaints predicted late cognitive decline.
Correlation of subjective memory ratings and objective cognitive tests at 6 years
We sought to determine if there were correlations between subjective memory scores and specific cognitive tests. The cognitive test scores were adjusted for baseline age, gender, and education level. First, when examining the correlations between the Likert scale score and cross-sectional cognitive test scores at 6 years (Table 4), there were statistically significant positive correlations with 5 memory tests (Total Rey Auditory Verbal Learning Test [RAVLT] score, delayed recall on the RAVLT, Rey Complex Figure-retention, Rey Complex Figure-delayed recall, and Letter-Number Sequencing)(13) (Table 3). In addition, there were also correlations with tests of language (Boston Naming Test) and attention (RAVLT-Trial 1). After adjusting for depression, 2 of the 5 memory tests remained statistically significant (Total RAVLT and RAVLT Trial 1) as well as the Boston Naming Test. Second, we compared the Likert scale score to the cognitive test z-scores examining cognitive change from baseline to 6 years. There were statistically significant positive correlations between the Likert scale scores and change on multiple cognitive tests, not only memory tests (data not shown). Therefore, patients rating themselves lower on the Likert scale tended to have a negative change in z-score indicating cognitive decline, while those rating themselves higher on the Likert scale tended to have a positive change in z-score indicating improvement in cognitive scores. These relationships remained statistically significant even after adjusting for depression scores (CES-D) at 6 years.
In addition, we tested the associations between the Lund memory questionnaire score and change (from baseline to 6 years) in cognitive tests (see Table 4). As the Lund questions are designed to measure change, we found significant correlations between the Lund memory scores and change in cognitive test scores for 3 of the 6 memory tests in our cognitive battery (RAVLT total, RAVLT delayed recall and RAVLT retention).
COMMENT
In a previous study, we compared self-reported subjective memory problems at 3 months and 1 year in patients who had undergone on-pump CABG with those in patients with stable coronary artery disease but without surgery. We reported that the frequency of memory problems was significantly higher in the CABG patients than in the nonsurgical group.(3) The reasons for this were not entirely clear, but may have included effects of general anesthesia, postoperative pain and narcotic use, and interactions with depression. In part due to increased media attention to postoperative cognitive complications, these symptoms are of considerable concern to patients. In the present study, we evaluated a larger group of surgical patients including those with both on- and off-pump treatment as well as a nonsurgical group at 3 and 6 years later. We found that there were no differences between the on- and off-pump patients, which suggest that subjective memory symptoms are not specific to the use of cardiopulmonary bypass. Unlike the differences in the frequency of memory complaints that existed between the surgical and nonsurgical groups at the early time points, by 6 years, the groups were similar although with greatly increased frequency of complaints. The question remains, however, as to the reasons for these increases in subjective complaints.
There are several plausible explanations for the increase in memory complaints over a 6-year time period, including aging, progression of cerebrovascular disease, and depression. It is possible that the gradual increase in memory complaints over time may be related to aging during the 6 years of the study. Nonetheless, aging and vascular disease changes in this cohort of patients with diagnosed coronary disease may be interrelated, and therefore may not represent “normal” aging. Additionally, the increase in complaints may be related to the progression of underlying cerebrovascular disease. We have shown that at baseline the surgery groups have more hypertension, diabetes, previous strokes, peripheral vascular disease, and triple vessel disease, all risk factors or characteristics of significant vascular disease.(5) Thus, we postulate that the CABG patients may have begun the study having already reached their vascular disease threshold with associated lower cognitive function, but over time the nonsurgical patients reach a similar threshold, although it may have developed on a slightly different time course.
With respect to the role of depression, previous cross-sectional studies that comprised only CABG patients(14) suggested that subjective memory complaints are all related to or explained by underlying depression.(15) The results from our longitudinal study indicate that depression alone cannot explain the subjective symptoms. First, our results show that the percentage of patients reporting memory complaints is increasing, while the percentage of those with depression is decreasing over time. Second, when we adjust for depression levels, the probability of reporting a subjective complaint persists. Thus, consistent with findings from a recent study which highlights the very complex relationship of depression with other disease processes,(16) our work shows that depression alone does not account for the increased frequency of complaints, but other interactions may be present.
In assessing the possible predictive value of whether early subjective memory complaints predict long term memory complaints, and whether such complaints predict late cognitive change, we found that patients with memory complaints at early time points were more likely to rank their memory lower at 6 years on both the Likert scale and to report changes over time on the Lund questionnaire. This suggests that subjective memory complaints may reflect a progressive underlying pathology, as would be expected with cerebrovascular disease. Some studies in the general population have reported associations with early cognitive complaints and future cognitive disease diagnoses.(17;18) Although in our study, early complaints predicted (late) 6-year memory complaints, they did not predict actual late cognitive decline from 1 to 6 years. This finding may highlight the multiple reasons for memory complaints; that is, the interactions of a patient’s perception, depression, and poor physical well-being, at the four times that we have measured them in this study. Early complaints may be more closely related to a person’s perception of worse physical functioning and depression status, which are both at their peak in the early time points, while later complaints may more accurately reflect actual cognitive functioning at the time. Indeed, we found a correlation with subjective symptoms at 6 years and actual cognitive and memory performance at 6 years (cross-sectional comparison). Performance on other measures of cognition frequently associated with subcortical disease, such as executive function and psychomotor speed, do not appear to be correlated with memory self-reports at 6 years.
We believe that our study has significant strengths: it is a prospective longitudinal evaluation comparing CABG to nonsurgical patients with known coronary artery and presumed cerebrovascular disease. In addition, we have used multiple subjective and objective measures to evaluate patients. Among the limitations are that we did not obtain data on memory complaints at baseline. Therefore, we do not know whether there were subjective differences between the groups at the start of the study. Moreover, we did not have imaging studies to assess the degree of underlying cerebrovascular disease. Other studies, however, have reported an association of self-reported cognitive complaints with white matter lesions,(19;20) as well as severity of lesions.(21) These studies suggest that self-reported cognitive symptoms may reflect the severity of underlying cerebrovascular disease.
The mechanism underlying the progression of memory complaints among patients with cardiovascular disease remains elusive. Based on these findings, we conclude that subjective complaints reflect, at least in part, changes in underlying cognitive performance, are not solely a manifestation of depression, nor do they appear to be related to treatment group. We speculate that the longitudinal increase in subjective complaints may be a manifestation of increasing cerebrovascular disease. It may also be important for future candidates for cardiac surgery to know that they are no more likely than nonsurgical patients to have changes in memory over time.
Acknowledgments
This study was supported by grant 35610 from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, Bethesda, MD; by the Dana Foundation, New York, N.Y., and the Johns Hopkins Medical Institution GCRC grant RR 00052.
We thank Pamela Talalay, Ph.D., Rebecca Gottesman, M.D., and Charles Hogue, M.D. for their help during the preparation of this manuscript. Louis M. Borowicz Jr. helped with the data acquisition. We also thank the cardiologists, cardiac surgeons, and anesthesiologists at our institution as well as Johns Hopkins Bayview Medical Center, who helped with this study. Special thanks are extended to our study participants who volunteered their time and energy to make this study possible.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Vingerhoets G, De Soete G, Jannes C. Subjective complaints versus neuropsychological test performance after cardiopulmonary bypass. J Psychosom Res. 1995;39:843–53. doi: 10.1016/0022-3999(95)00021-3. [DOI] [PubMed] [Google Scholar]
- 2.Khatri P, Babyak M, Clancy C, Davis R, Croughwell N, Newman M, et al. Perception of cognitive function in older adults following coronary artery bypass surgery. Health Psychol. 1999;18:301–6. doi: 10.1037//0278-6133.18.3.301. [DOI] [PubMed] [Google Scholar]
- 3.Selnes OA, Grega MA, Borowicz LM, Jr, Barry S, Zeger S, McKhann GM. Self-reported memory symptoms with coronary artery disease: a prospective study of CABG patients and nonsurgical controls. Cogn Behav Neurol. 2004;17:148–56. [PubMed] [Google Scholar]
- 4.Selnes OA, Grega MA, Bailey MM, Pham L, Zeger S, Baumgartner WA, et al. Cognition 6 years after surgical or medical therapy for coronary artery disease. Ann Neurol. 2008;63:581–90. doi: 10.1002/ana.21382. [DOI] [PubMed] [Google Scholar]
- 5.McKhann GM, Grega MA, Borowicz LM, Jr, Bailey MM, Barry SJ, Zeger SL. Is there cognitive decline 1 year after CABG? Comparison with surgical and nonsurgical controls. Neurology. 2005;65:991–99. doi: 10.1212/01.wnl.0000175220.78475.99. [DOI] [PubMed] [Google Scholar]
- 6.Bergh C, Backstrom M, Jonsson H, Havinder L, Johnsson P. In the eye of both patient and spouse: memory is poor 1 to 2 years after coronary bypass and angioplasty. Ann Thorac Surg. 2002;74:689–93. doi: 10.1016/s0003-4975(02)03723-2. [DOI] [PubMed] [Google Scholar]
- 7.Selnes OA, Grega MA, Borowicz LM, Jr, Royall RM, McKhann GM, Baumgartner WA. Cognitive changes with coronary artery disease: a prospective study of coronary artery bypass graft patients and nonsurgical controls. Ann Thorac Surg. 2003;75:1377–84. doi: 10.1016/s0003-4975(03)00021-3. [DOI] [PubMed] [Google Scholar]
- 8.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Measurement. 1977;1:385–401. [Google Scholar]
- 9.Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 10.Jette AM, Davies AR, Cleary PD, Calkins DR, Rubenstein LV, Fink A, et al. The Functional Status Questionnaire: reliability and validity when used in primary care. J Gen Intern Med. 1986;1:143–49. doi: 10.1007/BF02602324. [DOI] [PubMed] [Google Scholar]
- 11.Wechsler D. WAIS-III administration and scoring manual. San Antonio: The Psychological Corporation; 1997. [Google Scholar]
- 12.Diggle PJ, Heagerty P, Liang KY, Zeger SL. The analysis of longitudinal data. 2. Oxford, England: Oxford University Press; 2002. [Google Scholar]
- 13.Lezak M. Neuropsychological Assessment. 3. Oxford University Press; New York: 1995. [Google Scholar]
- 14.Gallo LC, Malek MJ, Gilbertson AD, Moore JL. Perceived cognitive function and emotional distress following coronary artery bypass surgery. J Behav Med. 2005;28:433–42. doi: 10.1007/s10865-005-9010-y. [DOI] [PubMed] [Google Scholar]
- 15.Newman S, Klinger L, Venn G, Smith P, Harrison M, Treasure T. Subjective reports of cognition in relation to assessed cognitive performance following coronary artery bypass surgery. Journal of Psychosomatic Research. 1989;33:227–33. doi: 10.1016/0022-3999(89)90050-0. [DOI] [PubMed] [Google Scholar]
- 16.Golden SH, Lazo M, Carnethon M, Bertoni AG, Schreiner PJ, Diez Roux AV, et al. Examining a bidirectional association between depressive symptoms and diabetes. JAMA. 2008;299:2751–59. doi: 10.1001/jama.299.23.2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.St. John P, Montgomery P. Are cognitively intact seniors with subjective memory loss more likely to develop dementia? Int J Geriatric Psychiatry. 2002;17:814–20. doi: 10.1002/gps.559. [DOI] [PubMed] [Google Scholar]
- 18.Jorm AF, Butterworth P, Anstey KJ, Christensen H, Easteal S, Maller J, et al. Memory complaints in a community sample aged 60-64 years: Associations with cognitive functioning, psychiatric symptoms, medical conditions, APOE genotype, hippocampus and amygdala volumes, and white-matter hyperintensities. Psychol Med. 2004;34:1495–506. doi: 10.1017/s0033291704003162. [DOI] [PubMed] [Google Scholar]
- 19.Stewart R, Dufouil C, Godin O, Ritchie K, Maillard P, Delcroix N, et al. Neuroimaging correlates of subjective memory deficits in a community population. Neurology. 2008;70:1601–7. doi: 10.1212/01.wnl.0000310982.99438.54. [DOI] [PubMed] [Google Scholar]
- 20.Minett TS, Dean JL, Firbank M, English P, O’Brien JT. Subjective memory complaints, white-matter lesions, depressive symptoms, and cognition in elderly patients. Am J Geriatr Psychiatry. 2005;13:665–71. doi: 10.1176/appi.ajgp.13.8.665. [DOI] [PubMed] [Google Scholar]
- 21.de Groot JC, de Leeuw FE, Oudkerk M, Hofman A, Jolles J, Breteler MM. Cerebral white matter lesions and subjective cognitive dysfunction: the Rotterdam Scan Study. Neurology. 2001;56:1539–45. doi: 10.1212/wnl.56.11.1539. [DOI] [PubMed] [Google Scholar]


