Abstract
Individuals with co-occurring substance use and psychiatric disorders have a more severe clinical course and poorer outcomes than do individuals with one disorder. In an attempt to find intervening variables that may contribute to improvement in treatment outcomes among individuals with co-occurring disorders, we investigated the roles of social support and self-efficacy in a sample of 351 clients with co-occurring disorders in residential drug abuse treatment programs (53% male; 35% African American, 13% Hispanic). Given their demographic variability, we also explored how ethnicity and age influence self-efficacy and access to social support, as well as their relationships to the outcomes. Structural equation modeling was used to examine the impact of the demographics and baseline psychological status, substance use, social support, and self-efficacy on mental health and substance use outcomes 6 months after treatment entry. Time in treatment was included as a control. Greater social support at baseline predicted better mental health status and less heroin and cocaine use; greater self-efficacy predicted less alcohol and cocaine use. Older clients reported less social support. African-American ethnicity was associated with more cocaine use at baseline and follow-up; however, African Americans reported more self-efficacy, which moderated their cocaine use. The current study highlights the potential therapeutic importance of clients' personal resources, even among a sample of severely impaired individuals.
Keywords: Co-occurring disorders, Self-efficacy, Social support, Treatment outcomes
1. Introduction
Several studies have demonstrated that individuals with mental disorders are prevalent within substance abuse treatment programs (ranging from about one fifth to one half) (Compton et al., 2000; Havassy et al., 2004; Primm et al., 2000; Watkins et al., 2004). In contrast to the past, when such individuals were routinely excluded from substance abuse treatment, individuals with severe psychiatric disorders are increasingly being treated within substance abuse treatment programs (McGovern et al., 2006). Prior research has shown that individuals with co-occurring substance use and mental health disorders have lower rates of treatment completion, shorter stays in treatment, and higher rates of post-treatment relapse and rehospitalization, compared with individuals with substance use problems only (Compton et al., 2003; Weisner et al., 2003). In response to the growing awareness of the treatment needs of this population, increasing attention has been paid to implementing integrated services, developing standards for “best practices,” and tailoring treatment protocols for individuals with co-occurring disorders (American Association of Community Psychiatrists, 2000; Drake et al., 2001; Mangrum et al., 2006; Minkoff, 2001). Other efforts to improve treatment for this population include matching patients to programs of differing levels of intensity based on their symptom severity (Timko and Sempel, 2004).
These attempts to improve treatment for individuals with co-occurring disorders are further complicated by the heterogeneity of this population, including sub-groups based on demographic characteristics (i.e., gender, ethnicity, age), types of substances used, and types of mental disorders, including various combinations of the above (Quello et al., 2005; Watkins et al., 2001). Moreover, individuals enter treatment with varying levels of functioning, access to social and familial support, and other resources that may influence their short- and long-term treatment outcomes and functioning. Yet few studies have specifically examined differences in treatment outcomes among clients with co-occurring disorders based on either their “fixed” (i.e., demographic) characteristics or other factors that may be amenable to change (e.g., access to resources, social support). In order to better understand how these factors influence treatment outcomes for individuals with co-occurring disorders, the present study tested a model in which immutable demographic predictors influenced more mutable intervening variables of social support and self-efficacy, which in turn predicted dependent variables of substance use and mental health status.
1.1. Social support and self-efficacy
Prior research has shown that both social support and self-efficacy may influence the treatment outcomes for individuals in substance abuse treatment (DiClemente, 1986; Greenfield et al., 2000, McKay et al., 2003). Social support for recovery from drug use is particularly important during the early stages of treatment, which is when an individual is most likely to experience ambivalence about ceasing drug use (Laudet et al., 2004). In one study, abstinence self-efficacy was the best predictor of post-treatment abstinence for both alcohol and drug use (Ilgen et al., 2005). Research suggests that there is a critical period at baseline for individuals with a high self-efficacy to change (Burleson and Kaminer, 2005; Litt et al., 2003). This suggests the importance of cultivating the resources that individuals have when initially entering treatment.
1.2. Ethnicity
Few studies have specifically examined differences among individuals with co-occurring disorders based on ethnicity, particularly concerning possible intervening psychosocial variables that can improve treatment outcomes. One study (Jerrell and Wilson, 1997) found it difficult to place young African-American males into clean and sober housing following their treatment, which the authors speculated was because of a lack of culturally appropriate placements. African-Americans are also more likely to use crack in comparison to Caucasians (Alvidrez and Havassy, 2005; Havassy et al., 1995; McKay et al., 2003). Hence, the specific treatment needs of African-Americans with co-occurring disorders may differ from those of Caucasians with co-occurring disorders.
Overall, ethnic minority clients may suffer from more severe symptomatology (Jerrell and Wilson, 1997). Prior research indicates that African Americans with co-occurring disorders are less likely to receive mental health treatment when compared to Caucasians with co-occurring disorders, and that social relationships seem to protect cocaine-using Caucasians, but not cocaine-using African-Americans (Alvidrez and Havassy, 2005; Havassy et al., 1995). Thus, ethnic minority clients with cooccurring disorders may enter treatment programs with more limited resources and less access to support.
1.3. Age
Since older adults are the fastest growing subgroup within the United States, considerable attention has been paid to projecting their future health-related needs and the anticipated effects for the health services system (Jeste et al., 1999; Knickman and Snell, 2002; Menninger, 2002). Research suggests that by the year 2020, approximately 4.4 million adults aged 50 or older will need treatment for substance abuse problems (Gfroerer et al., 2003). The current mental health and substance abuse treatment systems have been described as both unprepared and ill-equipped to manage and treat the projected population of older adults with co-occurring disorders (Speer et al., 1991).
Older adults may enter into treatment with more severe deficits in functioning and attenuated social networks. One study showed that among older adults in substance abuse treatment, more prior treatment episodes were associated with lower self-efficacy, perhaps stemming from multiple prior unsuccessful treatment attempts (Grella et al., 1999). In addition, lower self-efficacy was associated with poorer mental health status. Thus older adults with a history of prior treatment attempts, coupled with the mental and physical health problems that often accompany aging, may pose a particular clinical challenge for providers. In another study of a large sample (over 20,000) of older-age substance abuse inpatients (average of 62 years of age) treated through the Department of Veterans Affairs, individuals who had a co-occurring psychiatric disorder were more likely than others to be readmitted for treatment for up to 4 years following initial treatment (Moos et al., 1994a,b). In light of the anticipated treatment needs of older individuals with cooccurring disorders, research is needed that directly addresses the treatment responses of this population and the mediators that may influence their outcomes.
1.4. Current study
This study examined the roles of social support and abstinence self-efficacy as possible intervening variables in predicting treatment outcomes among clients with co-occurring disorders. In addition, this study specifically examined age and ethnicity as further direct predictors of treatment outcomes. African-American ethnicity was used as a predictor within this multiethnic sample, in part due to their higher rates of cocaine use, which have been shown to be associated with generally poorer outcomes among this population. The goal of the study was to better understand the problems presented by subgroups of individuals with co-occurring disorders and the personal resources and characteristics that may mediate their outcomes.
2. Method
2.1. Procedure
Participants were individuals with co-occurring substance abuse and mental health disorders who were sampled from 11 residential drug abuse treatment programs that provided publicly funded substance abuse treatment to adults within Los Angeles County from August 1999 to April 2002; follow-up assessments were conducted through April 2003. Upon admission, program staff screened potential study participants based on several indicators of mental disorders (i.e., use of medications for a psychiatric problem, referral from a mental health provider, past inpatient treatment). Administrative records obtained from the state Department of Mental Health subsequently verified that 97% of the sample had received treatment within the public mental health system for a serious mental disorder. Eligible clients were referred to research staff who then conducted study intake procedures, including obtaining clients' informed consent for study participation.
Baseline assessments were conducted at least 48 h following treatment admission to allow for initial stabilization. These interviews took approximately 6 h to complete and were usually conducted in multiple sittings. Participants received payment of $40 for the interview in the form of non-cash vouchers that were redeemable at local stores or restaurants. Face-to-face follow-up interviews (lasting an average of 2–3 h) were scheduled with all participants at 6 months following treatment intake; participants were paid $50 in non-cash vouchers for completion of these interviews.
All study procedures were reviewed and approved by the UCLA Institutional Review Board, and a federal Certificate of Confidentiality to protect subject confidentiality was obtained from the National Institute on Drug Abuse.
2.2. Study treatment programs
The treatment programs in the study were recruited from among those that had participated in a countywide initiative to improve service delivery to individuals with co-occurring disorders by designating “partnerships” between addiction and mental health providers in the same geographic areas (Grella and Gilmore, 2002). Static capacity of the programs ranged from 30 to 309 (mean = 119, S.D. = 89) and estimates of the proportion of clients who had cooccurring disorders ranged from 10 to 100% (mean = 0.40, S.D. = 0.34). All programs provided a minimum of 90 days of residential treatment and generally adhered to an eclectic treatment approach that emphasized 12-step recovery principles, along with varying degrees of emphasis on counseling and rehabilitation services. Characteristics of study programs have been described in depth elsewhere (Gil-Rivas and Grella, 2005; Grella and Gilmore, 2002; Grella et al., 2004).
2.3. Participants
Participants were 400 adult men and women recruited from the 11 residential drug treatment programs described above. The average age of participants was 36 years (S.D. = 8.4) and they ranged in age from 18 to 60 years old. There were slightly more males (n = 213, 53%) than females (n = 187, 47%). Of the total, 140 participants (35%) were African American, 176 (44%) were White, 52 (13%) were Hispanic, and 32 (8%) were of other ethnicities. Over half of the sample (n = 211, 53%) had never been married and one third (n = 133, 33%) had less than a high school degree. Over half of the sample (n = 248, 62%) had been homeless within the year prior to entering treatment, and most of the sample (n = 328, 82%) had been homeless at some point in their lifetime. A majority (n = 236, 59%) had been under legal supervision in the past. Most of the sample (97%) reported having prior mental health treatment, with an average of 6 inpatient episodes, and 70% had received prior substance abuse treatment.
Participants were assessed on the Structured Clinical Interview for the DSMIV Axis I Disorders–Patient Edition (SCID-I/P, Version 2.0: First et al., 1997) for mood, psychotic, posttraumatic stress, and substance use disorders. Interviewers were trained to conduct the SCID by diagnosticians from the Diagnosis and Psychopathology Unit of the UCLA Center for Research on Treatment and Rehabilitation of Psychosis. Interviewers were required to achieve a minimum overall kappa of 0.75, a minimum sensitivity kappa of 0.75, and a specificity kappa of 0.75 on symptom agreement, and 90% accuracy of agreement on diagnosis (Ventura et al., 1998). Nearly two thirds of the sample (n = 255, 64%) had a diagnosis of mood disorder (i.e., major depression, dysthymia, bipolar disorder, mood disorder not otherwise specified, NOS) and the remainder (n = 145, 36%) were diagnosed with a psychotic disorder (i.e., schizophrenia, schizoaffective disorder, psychosis NOS). Additionally, over half (n = 208, 52%) were diagnosed with posttraumatic stress disorder.
Regarding lifetime substance use, 278 participants (70%) had a diagnosis of alcohol dependence, 260 (65%) cocaine dependence, 176 (44%) cannabis dependence, 168 (42%) amphetamine dependence, 115 (29%) opioid dependence, and 99 (25%) sedative dependence. Background characteristics of the study sample have been described in-depth previously (Grella, 2003).
Out of the total sample, 90% (n = 361) were located for follow-up; 88% (n = 351) completed the follow-up interview; 2% did not complete the follow-up because they refused (n = 5), were deceased (n = 3), or could not be scheduled (n = 2); the remainder (n = 39, 10%) were not able to be located for follow-up. Comparisons between those who did and did not complete the 6-month follow-up interview revealed no significant differences in background characteristics or in follow-up rates by program where they were treated.
2.4. Measures
2.4.1. Baseline patient-level measures
Background patient characteristics included in the analyses consist of ethnicity (African American: 1 = yes, 0 = no), age, one measure of psychological functioning, and substance use frequency (alcohol, heroin, cocaine). Other demographic characteristics, including Hispanic or White ethnicity, gender, marital status, and education, were examined as possible predictors, but were not significantly associated with the outcome measures and thus were dropped from the analyses.
The measure of psychological distress used was a latent variable indicated by three composite parcels formed from the means of 9 items from the RAND Health Survey SF-36 (Ware and Sherbourne, 1992) that constitute the Mental Health subscale entitled “Energy and Emotions.” To keep the number of indicators to a reasonable level based on the sample size, the 9 items were combined randomly to form 3 separate indicators. This parceling process was acceptable because of the high coefficient alphas among the items at baseline (0.83) and follow-up (0.94; Yuan et al., 1997). The items assessed depressed mood in the previous 4 weeks. Scores range from 1 (all of the time) to 6 (none of the time) and were reverse-scored where appropriate so that higher scores indicate more distress. Sample items include: “The past 4 weeks I was full of pep,” “I was downhearted or blue,” “I was tired.”
Social support was assessed at baseline with 6 items (Coefficient alpha = 0.99). Scores ranged from 1 (never or rarely) to 3 (almost always). A typical question was “How often can you talk about your deepest problems with at least some of your family?” To avoid too many variables in the model, the items were combined into three indicators.
Abstinence self-efficacy was assessed with a 20-item scale that was based on the Situational Confidence Questionnaire (Annis and Graham, 1988). Twenty items regarding likelihood that one could resist drug use in different situations were rated on a 3-point scale, with 1 (not at all confident or sure) to 3 (very confident or sure; Coefficient alpha = 0.94). The 20 items were combined at random into four parcels.
Three items assessed substance use frequency of three substances in the 30 days prior to treatment admission. Heroin, cocaine/crack (mean of use of cocaine and crack), and heavy alcohol use (alcohol use to intoxication) were included. Each variable was assessed on a 8-point scale, with: 0 = no use; (1) 1–3 times per month; (2) 1–2 times per week; (3) 3–4 times per week; (4) 5–6 times/week; (5) daily/almost every day; (6) 2–3 times/day; (7) 4 times/day.
2.4.2. Follow-up measures
Time in drug treatment (measured in days) was included as a control variable in the path model predicting the outcomes, since time in treatment alone could have impacted the observed outcomes rather than individual characteristics of social support and self-efficacy. Ninety-five percent of the sample was in treatment for less than 6 months; the mean number of days of treatment was about 94 days.
Psychological distress and substance use were assessed in the same fashion at the 6-month follow-up as they were at baseline (Rand SF-36 Mental Health subscale, and frequencies of substance use).
2.5. Analytic method
The EQS structural equations program was used to perform the latent variable analyses (Bentler, 2005). Goodness-of-fit of the models was assessed with the maximum-likelihood χ2 statistic (ML χ2), the Comparative Fit Index (CFI), the Satorra–Bentler χ2 (S–B χ2), the Robust Comparative Fit Index (RCFI), and the root mean squared error of approximation (RMSEA) (Bentler, 2005; Hu and Bentler, 1999). The S–B χ2 was used in addition to the maximum likelihood χ2 because it is more appropriate and robust when the data depart from multivariate normality. The CFI and RCFI range from 0 to 1 and reflect the improvement in fit of a hypothesized model over a model of complete independence among the measured variables. The RCFI adjusts for sample size; values at 0.95 or greater are desirable, indicating that the hypothesized model reproduces 95% or more of the covariation in the data (Hu and Bentler, 1999). The RMSEA is a measure of fit per degrees of freedom, controlling for sample size, and values less than 0.06 indicate a relatively good fit between the hypothesized model and the observed data (Hu and Bentler, 1999).
An initial confirmatory factor analysis (CFA) assessed the adequacy of the measurement model and the associations among the latent variables. Suggestions from the LaGrange Multiplier test, which reports modifications to the original model that will improve the fit, were evaluated (LM test; Chou and Bentler, 1990). Modifications were only allowed that made sense theoretically and logically.
We then tested a predictive path model that positioned the baseline patient characteristics as predictors of the mediators of social support and self-efficacy as well as the outcome variables reflecting psychological distress and substance use. Time in drug treatment was also added as a direct predictor of the outcomes to avoid a possibly spurious relationship between patient characteristics and improvement in the outcome variables due to a longer drug treatment history, which may also have been related to the possible mediators. Relationships that were significant among the predictive background variables were also included in this model as covariates. Nonsignificant paths and correlations in this model were trimmed gradually following the recommended model-evaluation procedure of MacCallum (1986).
3. Results
3.1. Confirmatory factor analysis
The initial CFA had an excellent fit: S–B χ2 = 172.90, 131 d.f.; RCFI = 0.97; RMSEA = 0.032. The maximum-likelihood solution also was very good (ML χ2 = 181.32, 131 d.f.; CFI = 0.98, RMSEA = 0.035). All hypothesized factor loadings were significant (p ≤ 0.001). Table 1 presents the factor loadings, means, and standard deviations of the measured variables. Table 2 reports the correlations among all of the latent variables and the demographic and single-item variables in the CFA. Two correlated error residuals were added for further fit improvement, even though the initial model was quite good. There were supplemental relationships between (1) two of the self-efficacy indicators, and (2) the same two measures from the RAND SF-36 taken at baseline and at follow-up (an autocorrelation). These two additions improved the fit considerably. The final fit of the CFA was: S–B χ2 = 140.41, 129 d.f.; RCFI = 0.99; RMSEA = 0.017. The maximum-likelihood solution was also improved (ML χ2 = 146.46, 129 d.f.; CFI = 0.99, RMSEA = 0.021).
Table 1.
Summary statistics and factor loadings of variables used in analyses
| Variables |
|||
|---|---|---|---|
| Mean | S.D. | Factor loading* | |
| Demographics | |||
| Age (years) | 36.75 | 9.75 | – |
| African American | 0.34 | 0.48 | – |
| Baseline | |||
| RAND SF-36 (1–6) | |||
| Composite 1 | 3.83 | 1.00 | 0.86 |
| Composite 2 | 3.81 | 1.07 | 0.77 |
| Composite 3 | 3.73 | 1.14 | 0.76 |
| Alcohol (0–7) | 4.59 | 8.76 | – |
| Heroin (0–7) | 1.25 | 5.22 | – |
| Cocaine/Crack (0–7) | 2.33 | 4.93 | – |
| Social support | |||
| Composite 1 | 2.13 | 0.82 | 0.84 |
| Composite 2 | 1.86 | 0.84 | 0.84 |
| Composite 3 | 2.16 | 0.89 | 0.84 |
| Self-efficacy (1–3) | |||
| Composite 1 | 2.31 | 0.53 | 0.84 |
| Composite 2 | 2.40 | 0.50 | 0.84 |
| Composite 3 | 2.05 | 0.63 | 0.92 |
| Composite 4 | 2.12 | 0.60 | 0.89 |
| 6-Month follow-up | |||
| RAND SF-36 (1–6) | |||
| Composite 1 | 3.59 | 1.02 | 0.83 |
| Composite 2 | 3.44 | 1.08 | 0.79 |
| Composite 3 | 3.13 | 1.14 | 0.71 |
| Alcohol (0–7) | 0.78 | 1.93 | – |
| Heroin (0–7) | 0.08 | 0.65 | – |
| Cocaine/Crack (0–7) | 0.26 | 0.84 | – |
| Time in treatment (days) | 93.8 | 4.9 | – |
All factor loadings significant, p≤0.001.
Table 2.
Correlations among variables in confirmatory factor model
| Variables |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
| Baseline | |||||||||||
| 1. RAND SF-36 | – | ||||||||||
| 2. Alcohol | 0.06 | – | |||||||||
| 3. Heroin | 0.16** | 0.17** | – | ||||||||
| 4. Cocaine | 0.03 | 0.41*** | 0.22*** | – | |||||||
| 5. Social support | −0.08 | −0.06 | −0.04 | −0.01 | – | ||||||
| 6. Self-efficacy | −0.25*** | −0.13* | −0.13* | −0.05 | 0.06 | – | |||||
| Six-month follow-up | |||||||||||
| 7. RAND SF-36 | 0.50*** | 0.05 | 0.15** | −0.05 | −0.18** | −0.17** | – | ||||
| 8. Alcohol | 0.02 | 0.22*** | −0.04 | −0.01 | 0.03 | −0.13* | 0.29*** | – | |||
| 9. Heroin | −0.06 | −0.07 | 0.09 | −0.04 | −0.10* | 0.09 | 0.05 | −0.02 | – | ||
| 10. Cocaine | −0.01 | −0.03 | −0.01 | 0.08 | −0.21*** | −0.08* | 0.25*** | 0.30*** | 0.23*** | – | |
| Demographics | |||||||||||
| 11. Age | 0.06 | 0.07 | 0.07 | 0.07 | −0.13* | 0.05 | 0.17** | −0.09 | 0.01 | 0.03 | – |
| 12. African American | −0.08 | 0.03 | −0.10* | 0.23*** | −0.10 | 0.15** | 0.04 | −0.04 | −0.09* | 0.16** | 0.12* |
p≤0.05.
p≤0.01.
p≤0.001.
As expected, there were highly significant associations among some of the latent and measured variables in the model. Among the most notable associations were a negative relationship between the baseline RAND SF-36 and self-efficacy (−0.25, p ≤ 0.001), positive relationships between use of cocaine and alcohol at baseline (0.41, p ≤ 0.001) and use of cocaine and heroin at baseline (0.22, p ≤ 0.001), a negative relationship between social support at baseline and cocaine at follow-up (−0.21, p ≤ 0.001), and positive relationships between the RAND SF-36 follow-up and alcohol at follow-up (0.29, p ≤ 0.001), the RAND SF-36 follow-up and cocaine at follow-up (0.25, p ≤ 0.001), cocaine and alcohol at follow-up (0.30, p ≤ 0.001), and cocaine and heroin at follow-up (0.23, p ≤ 0.001). Greater age was significantly associated with less social support and more emotional distress at follow-up. African-American ethnicity was significantly associated with cocaine use at both time periods, greater self-efficacy, less heroin use at both time periods, and greater age.
3.2. Path analysis
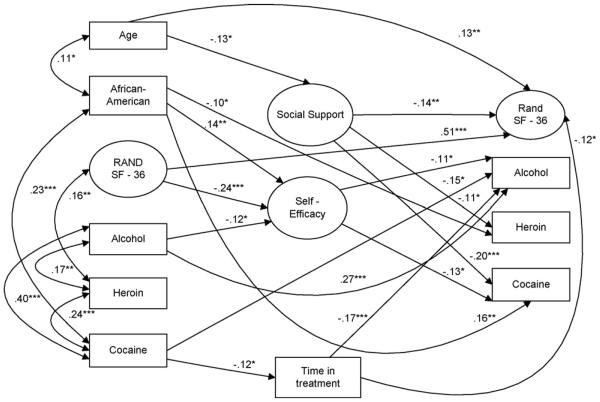
Fig. 1 presents the final trimmed path model in which time in treatment was added as a control in the model. This model has excellent fit statistics (S–B χ2 = 224.20, 190 d.f.; RCFI = 0.98, RMSEA = 0.024) as did the ML solution (ML χ2 = 226.42, 190 d.f., CFI = 0.99, RMSEA = 0.025). A greater time in treatment predicted less alcohol use and lower RAND SF-36 scores, indicating that time in treatment exerted a positive influence on both substance use and mental illness. Greater use of cocaine at baseline predicted a shorter time in treatment. Baseline use of alcohol and lower RAND SF-36 scores at baseline significantly predicted less self-efficacy; greater age predicted less social support. Social support at baseline predicted less heroin use, cocaine use, and lower RAND SF-36 scores at follow-up. More self-efficacy at baseline predicted less alcohol use and less cocaine use at follow-up. African-American ethnicity predicted greater self-efficacy but also more cocaine use.
Fig. 1.
Longitudinal path model testing influence of social support and self-efficacy on improvement in substance use and mental health status among clients with co-occurring disorders in residential treatment (N = 351). Latent constructs are in circles, single items are in rectangles; one-headed arrows depict standardized regression paths and two-headed arrows represent correlations (standardized covariances). (*p≤0.05, **p≤0.01, ***p≤0.001).
There were some interesting indirect effects between the predictors and outcomes mediated through the intervening variables of social support and self-efficacy. Baseline RAND SF-36 score had a positive indirect effect on cocaine use at follow-up based on its significant negative effect on self-efficacy. In addition, although African-American ethnicity was positively associated with more cocaine use directly, the effect through self-efficacy was significantly negative (one-tailed test only, however). Thus, greater self-efficacy among African-Americans tended to moderate their use of cocaine. Further study is warranted regarding this relationship to see if it is more robust in other situations or can be exploited to improve outcomes for this subgroup. In addition, there was a significant indirect effect of cocaine use at baseline on more alcohol use due to less time in treatment.
4. Discussion
This study examined the intervening and direct effects of social support and abstinence self-efficacy at baseline on the six-month outcomes among a diverse sample of clients with co-occurring disorders in residential substance abuse treatment. Study findings demonstrated that these personal resources, which clients brought with them when they entered treatment, were predictive of more improvement in both their substance use and mental health status. The results draw attention to several important areas for clinicians to target within the context of efforts to improve treatment for this population: (1) the importance of social support, particularly among older clients; (2) the positive benefits of abstinence self-efficacy, especially among African-American clients; (3) the greater difficulty of treating polydrug users who have co-occurring disorders. In addition, we found several relationships with time in treatment that varied by type of substance use.
4.1. Social support
Among this population, which is characterized by low levels of psychosocial functioning, those individuals who could draw on greater support from others and who felt more strongly that they could abstain from substance use following treatment had the most positive outcomes. Higher social support was predictive of better psychological status, less heroin use, and less cocaine use at follow-up. This was an especially compelling result given that social support was not significantly correlated, and indeed was only minimally correlated, with these same variables at baseline.
The sample included enough variability across age to determine that age has both a direct and indirect relationship with outcomes. Older age predicted less social support at treatment admission as well as poorer mental health status at follow-up. Other studies have shown that older adults have reported that good social resources are important to having a good quality of life, and more specifically, to feeling that others care for them when they encounter problems (Gabriel and Bowling, 2004). The unmet needs of older adults, including social needs, are associated with an increased risk of behavior problems, anxiety, and depression (Hancock et al., 2006). Since age is a fixed trait, and thus immutable, these results suggest that clinicians should explore an older adult's access to social networks and resources, and if needed, link clients with resources targeted specifically for older adults. Overall, assessing this subgroup's social resources at baseline and helping to provide greater support networks when they are needed can help improve their post-treatment functioning.
4.2. Self-efficacy
Abstinence self-efficacy was predictive of less use of alcohol and less use of cocaine at follow-up for the whole sample and was associated with a greater sense of well-being and less alcohol use at baseline. African-Americans reported more abstinence self-efficacy, and this relationship helped moderate the high association of cocaine use with African-American ethnicity. This finding is noteworthy because previous studies of individuals with co-occurring disorders have shown that African Americans have higher rates of cocaine use compared with Whites (Alvidrez and Havassy, 2005; Havassy et al., 1995; McKay et al., 2003; Mueser et al., 2001). Furthermore, since ethnicity is a fixed trait, these results point towards an avenue that clinicians can explore in order to improve outcomes among this particular subgroup. Previous research with this study sample showed that African Americans were less likely to be treated in programs that provided on-site mental health services (Grella and Stein, 2006), yet greater access to treatment resources may potentially enhance the effects of self-efficacy for this population.
4.3. Polydrug use
In addition to our major findings about social support and abstinence self-efficacy, our analysis also had implications for those clients who abuse multiple drugs. Alcohol, cocaine, and heroin use were all highly correlated at baseline and use of all substances was reduced at follow-up. Although this finding is not surprising, the correlations among these substances at follow-up were substantially higher than the corresponding associations at baseline. This heightened relationship suggests that the subset of clients in this sample who were polydrug users, in comparison to those who were non-polydrug users, had the most intractable substance abuse problems. If they were not abstinent at follow-up, they were even more likely to be using multiple substances, compared to their baseline levels of use. This may be due in particular to high rates of cocaine use among this sample. In a study conducted with clients in a hospital setting, more than half of the clients with co-occurring disorders were polydrug users, and of those, approximately 45% were cocaine users (Havassy and Arns, 1998). Furthermore, some researchers have speculated that cocaine users rely on other drugs to assuage the acute negative effects of cocaine (e.g., Carroll and Rounsaville, 1992). This finding suggests that treatment for individuals with co-occurring disorders, who are polydrug users, requires longer and more intensive treatment to achieve abstinence.
4.4. Time in treatment
Longer time in treatment was associated with less alcohol use and better mental health status at follow-up. Other relationships with time in treatment were negligible and time in treatment was only entered into the model as a control variable. However, we noted that there was also a significant relationship between use of cocaine at baseline and shorter time in treatment. This finding provides additional evidence regarding the need for more intensive interventions in order to engage those with severe drug use disorders and problems in psychosocial functioning, since they are least likely to respond to treatment and are more likely to relapse following treatment (Simpson et al., 2002).
4.5. Study limitations
There are some potential limitations in the current study. The study was conducted with clients sampled from programs within a large urban county. Although efforts were made to sample from diverse programs in order to capture a range of clients, the study findings may not generalize beyond the specific sample selected from these programs. Further, since the clients were sampled from residential treatment programs, they were generally at a high level of severity of substance use disorders and low levels of psychosocial functioning. This is evident in their relatively high rates of prior history of homelessness and of past substance abuse and mental health treatment utilization. Yet these characteristics are typical of clients treated in residential drug treatment programs, as clients in these programs have more severe clinical profiles compared with those in outpatient programs (Drug and Alcohol Services Information System, 2006).
In addition, post-treatment outcomes were only examined at 6 months; the stability of the effects of the predictors and of improvement in substance abuse over a longer follow-up period needs to be examined, especially in this type of population. Furthermore, we relied upon self-report measures of psychological distress and substance use, both of which are subject to reporting bias. Lastly, our ability to draw causal inferences from the study findings is limited by the observational nature of the study.
4.6. Conclusion
Overall, because individuals who have co-occurring disorders often present to treatment with complex service needs, it is important to assess not only their treatment needs, but also their available resources and resiliency at the time they enter into treatment. Past studies suggest that there are many potential combinations of co-occurring disorders among clients in substance abuse treatment, making it imperative to evaluate “packages” of the best services that can be applied to specific sub-types of these combinations (Watkins et al., 2005). The current findings add to this suggestion by highlighting the potential therapeutic importance of social support and abstinence self-efficacy, particularly for various sub-groups among the broader population of clients with co-occurring disorders.
Footnotes
Support for this research was provided by grants RO1-DA11966 (Grella) and PO1-DA01070-33 (Warren, Stein) from the National Institute on Drug Abuse.
References
- Alvidrez J, Havassy BE. Racial distribution of dual-diagnosis clients in public sector mental health and drug treatment setting. J. Health Care Poor Underserved. 2005;16:53–62. doi: 10.1353/hpu.2005.0002. [DOI] [PubMed] [Google Scholar]
- American Association of Community Psychiatrists Principles for the care and treatment of persons with co-occurring psychiatric and substance disorders. 2000 http://www.comm.psych.pitt.edu/finds/dualdx.html (accessed April 7, 2006)
- Annis HM, Graham JM. Situational Confidence Questionnaire. Addiction Research Foundation; Toronto, Canada: 1988. [Google Scholar]
- Bentler PM. EQS 6 Structural Equations Program Manual. Multivariate Software, Inc.; Encino, CA: 2005. [Google Scholar]
- Burleson JA, Kaminer Y. Self-efficacy as a predictor of treatment outcome in adolescent substance use disorders. Addict. Behav. 2005;30:1751–1764. doi: 10.1016/j.addbeh.2005.07.006. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ. Contrast of treatment-seeking and untreated cocaine abusers. Arch. Gen. Psychiatry. 1992;49:464–471. doi: 10.1001/archpsyc.1992.01820060044007. [DOI] [PubMed] [Google Scholar]
- Chou CP, Bentler PM. Model modification in covariance structure modeling: a comparison among likelihood ratio, Lagrange multiplier, and Wald tests. Multivariate Behav. Res. 1990;25:115–136. doi: 10.1207/s15327906mbr2501_13. [DOI] [PubMed] [Google Scholar]
- Compton WM, Cottler LB, Ben Abdallah A, Phelps DL, Spitznagel EL, Horton JC. Substance dependence and other psychiatric disorders among drug dependent subjects: race and gender correlates. Am. J. Addict. 2000;9:113–125. doi: 10.1080/10550490050173181. [DOI] [PubMed] [Google Scholar]
- Compton WM, Cottler LB, Jacobs JL, Ben-Abdallah A, Spitznagel EL. The role of psychiatric disorders in predicting drug dependence treatment outcomes. Am. J. Psychiatry. 2003;160:890–895. doi: 10.1176/appi.ajp.160.5.890. [DOI] [PubMed] [Google Scholar]
- DiClemente CC. Self-efficacy and the addictive behaviors. J. Soc. Clin. Psychol. 1986;4:302–315. [Google Scholar]
- Drake RE, Essock SM, Shaner A, Carey KB, Minkoff K, Kola L, Lynde D, Osher FC, Clark RE, Rickards L. Implementing dual diagnosis services for clients with severe mental illness. Psychiatr. Serv. 2001;52:469–476. doi: 10.1176/appi.ps.52.4.469. [DOI] [PubMed] [Google Scholar]
- Drug and Alcohol Services Information System (DASIS) Homeless Admissions to Substance Abuse Treatment: 2004. Office of Applied Studies, SAMHSA; 2006. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders: Patient Edition (SCID-I/P, Version 2.0, 4/97 rev.) Biometrics Research, New York State Psychiatric Institute; New York: 1997. [Google Scholar]
- Gabriel Z, Bowling A. Quality of life from the perspectives of older people. Ageing Soc. 2004;24:675–691. [Google Scholar]
- Gfroerer J, Penne M, Pemberton M, Folsom R. Substance abuse treatment need among older adults in 2020: the impact of the aging baby-boom cohort. Drug Alcohol Depend. 2003;69:127–135. doi: 10.1016/s0376-8716(02)00307-1. [DOI] [PubMed] [Google Scholar]
- Gil-Rivas V, Grella CE. Treatment services and service delivery models for dually diagnosed clients: variations across mental health and substance abuse providers. Community Ment. Health J. 2005;41:251–266. doi: 10.1007/s10597-005-5000-3. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Hufford MR, Vagge LM, Muenz LR, Costello ME, Weiss RD. The relationship of self-efficacy expectations to relapse among alcohol dependent men and women: a prospective study. J. Stud. Alcohol. 2000;61:345–351. doi: 10.15288/jsa.2000.61.345. [DOI] [PubMed] [Google Scholar]
- Grella CE. Effects of gender and diagnosis on addiction history, treatment utilization, and psychosocial functioning among a dually diagnosed sample in drug treatment. J. Psychoactive Drugs. 2003;35:169–179. doi: 10.1080/02791072.2003.10400512. [DOI] [PubMed] [Google Scholar]
- Grella CE, Gilmore J. Improving service delivery to the dually diagnosed in Los Angeles County. J. Subst. Abuse Treat. 2002;23:115–122. doi: 10.1016/s0740-5472(02)00254-4. [DOI] [PubMed] [Google Scholar]
- Grella CE, Gil-Rivas V, Cooper L. Perceptions of mental health and substance abuse program administrators and staff on service delivery to persons with co-occurring substance abuse and mental disorders. J. Behav. Health. Serv. Res. 2004;31:38–49. doi: 10.1007/BF02287337. [DOI] [PubMed] [Google Scholar]
- Grella CE, Hser YI, Joshi V, Anglin MD. Patient histories, retention and outcome models for younger and older adults in DATOS. Drug Alcohol Depend. 1999;57(2):151–166. doi: 10.1016/s0376-8716(99)00082-4. [DOI] [PubMed] [Google Scholar]
- Grella CE, Stein JA. Impact of program services on treatment outcomes of patients with comorbid mental and substance use disorders. Psychiatr. Serv. 2006;57(7):1007–1015. doi: 10.1176/appi.ps.57.7.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hancock GA, Woods B, Challis D, Orrell M. The needs of older people with dementia in residential care. Int. J. Geriatr. Psychiatry. 2006;21:43–49. doi: 10.1002/gps.1421. [DOI] [PubMed] [Google Scholar]
- Havassy BE, Alvidrez J, Owen KK. Comparisons of patients with comorbid psychiatric and substance use disorders: implications for treatment and service delivery. Am. J. Psychiatry. 2004;161:139–145. doi: 10.1176/appi.ajp.161.1.139. [DOI] [PubMed] [Google Scholar]
- Havassy BE, Arns PG. Relationship of cocaine and other substance dependence to well-being of high-risk psychiatric patients. Psychiatr. Serv. 1998;49:935–940. doi: 10.1176/ps.49.7.935. [DOI] [PubMed] [Google Scholar]
- Havassy BE, Wasserman DA, Hall SM. Social relationships and abstinence from cocaine in an American treatment sample. Addiction. 1995;90:699–710. doi: 10.1046/j.1360-0443.1995.90569911.x. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equations Model. 1999;6:1–55. [Google Scholar]
- Ilgen M, McKeller J, Tiet Q. Abstinence self-efficacy and abstinence 1 year after substance use disorder treatment. J. Consult. Clin. Psychol. 2005;73:1175–2110. doi: 10.1037/0022-006X.73.6.1175. [DOI] [PubMed] [Google Scholar]
- Jerrell JM, Wilson JL. Ethnic differences in the treatment of dual mental and substance disorders. J. Subst. Abuse Treat. 1997;14:133–140. doi: 10.1016/s0740-5472(96)00125-0. [DOI] [PubMed] [Google Scholar]
- Jeste DV, Alexopoulos GS, Bartels SJ, Cummings JL, Gallo JJ, Gottlieb GL, Halpain MC, Palmer BW, Patterson TL, Reynolds CF, Lebowitz BD. Consensus statement on the upcoming crisis in geriatric mental health. Arch. Gen. Psychiatry. 1999;56:848–853. doi: 10.1001/archpsyc.56.9.848. [DOI] [PubMed] [Google Scholar]
- Knickman JR, Snell EK. The 2030 problem: caring for aging baby boomers. Health Serv. Res. 2002;37:849–884. doi: 10.1034/j.1600-0560.2002.56.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB, Cleland CM, Magura S, Vogel HS, Knight EL. Social support mediates the effects of dual-focus mutual aid groups on abstinence from substance use. Am. J. Community Psychol. 2004;34:175–185. doi: 10.1007/s10464-004-7413-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litt MB, Kadden RM, Cooney NL, Kabela E. Coping skills and treatment outcomes in cognitive-behavioral and interactional group therapy for alcoholism. J. Consult. Clin. Psychol. 2003;71:118–128. doi: 10.1037//0022-006x.71.1.118. [DOI] [PubMed] [Google Scholar]
- MacCallum R. Specification searches in covariance structure modeling. Psychol. Bull. 1986;100:107–120. [Google Scholar]
- Mangrum LF, Spence RT, Lopez M. Integrated versus parallel treatment of co-occurring psychiatric and substance us disorders. J. Subst. Abuse. Treat. 2006;30:79–84. doi: 10.1016/j.jsat.2005.10.004. [DOI] [PubMed] [Google Scholar]
- McGovern MP, Xie H, Segal SR, Siembab L, Drake RE. Addiciton treatment services and co-occurring disorders: prevalence estimates, treatment practices, and barriers. J. Subst. Abuse Treat. 2006;31:267–275. doi: 10.1016/j.jsat.2006.05.003. [DOI] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Pettinati HM, Shepard DS. An examination of potential sex and race effects in a study of continuing care for alcohol- and cocaine- dependent patients. Alcohol. Clin. Exp. Res. 2003;27:1321–1323. doi: 10.1097/01.ALC.0000080347.11949.B7. [DOI] [PubMed] [Google Scholar]
- Menninger JA. Assessment and treatment of alcoholism and substance-related disorders in the elderly. B. Menninger Clin. 2002;66:166–183. doi: 10.1521/bumc.66.2.166.23364. [DOI] [PubMed] [Google Scholar]
- Minkoff K. Best practices: developing standards of care for individuals with co- occurring psychiatric and substance use disorders. Psychiatr. Serv. 2001;52:597–599. doi: 10.1176/appi.ps.52.5.597. [DOI] [PubMed] [Google Scholar]
- Moos RH, Brennan PL, Mertens JR. Diagnostic subgroups and predictors of one-year re-admission among late-middle-aged and older substance abuse patients. J. Stud. Alcohol. 1994a;55:173–183. doi: 10.15288/jsa.1994.55.173. [DOI] [PubMed] [Google Scholar]
- Moos RH, Mertens JR, Brennan PL. Rates and predictors of four-year readmission among late-middle-aged and older substance abuse patients. J. Stud. Alcohol. 1994b;55:561–570. doi: 10.15288/jsa.1994.55.561. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Essock SM, Drake RE, Wolfe RS, Frisman L. Rural and urban differences in patients with a dual diagnosis. Schizophr. Res. 2001;48:93–107. doi: 10.1016/s0920-9964(00)00065-7. [DOI] [PubMed] [Google Scholar]
- Quello SB, Brady KT, Sonne SC. Mood disorders and substance use disorder: a complex comorbidity. Sci. Pract. Perspect. 2005;3(1):13–24. doi: 10.1151/spp053113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primm AB, Gomez MB, Tzolova-Iontchev I, Perry W, Vu HT, Crum RM. Mental health versus substance abuse treatment programs for dually diagnosed patients. J. Subst. Abuse Treat. 2000;19(3):285–290. doi: 10.1016/s0740-5472(00)00112-4. [DOI] [PubMed] [Google Scholar]
- Simpson DD, Joe GW, Broome KM. A national 5-year follow-up of treatment outcomes for cocaine dependence. Arch. Gen. Psychiatry. 2002;59:538–544. doi: 10.1001/archpsyc.59.6.538. [DOI] [PubMed] [Google Scholar]
- Speer DC, O'Sullivan M, Schonfeld L. Dual diagnosis among older adults: a new array of policy and planning problems. J. Ment. Health Admin. 1991;18:43–50. doi: 10.1007/BF02521133. [DOI] [PubMed] [Google Scholar]
- Timko C, Sempel JM. Short-term outcomes of matching dual diagnosis patients' symptom severity to treatment intensity. J. Subst. Abuse Treat. 2004;26:209–218. doi: 10.1016/S0740-5472(04)00002-9. [DOI] [PubMed] [Google Scholar]
- Ventura J, Liberman RP, Green MF, Shaner A, Mintz J. Training and quality assurance with the structured clinical interview for DSM-IV (SCID-I/P) Psychiatry Res. 1998;79:163–173. doi: 10.1016/s0165-1781(98)00038-9. [DOI] [PubMed] [Google Scholar]
- Ware J, Sherbourne C. The MOS 36-item Short-Form Health Survey (SF-36) Med. Care. 1992;30:473–483. [PubMed] [Google Scholar]
- Watkins KE, Burnam A, Kung F, Paddock S. A national survey of care for persons with co-occurring mental and substance use disorders. Psychiatr. Serv. 2001;52:1062–1068. doi: 10.1176/appi.ps.52.8.1062. [DOI] [PubMed] [Google Scholar]
- Watkins KE, Hunter SB, Burnam MA, Pincus HA, Nicholson G. Review of treatment recommendations for persons with a co-occurring affective or anxiety and substance use disorder. Psychiatr. Serv. 2005;56:913–926. doi: 10.1176/appi.ps.56.8.913. [DOI] [PubMed] [Google Scholar]
- Watkins KE, Hunter SB, Wenzel SL, Tu W, Paddock SM, Griffin A, Ebener P. Prevalence and characteristics of clients with co-occurring disorders in outpatient substance abuse treatment. Am. J. Drug Alcohol Abuse. 2004;30:749–764. doi: 10.1081/ada-200037538. [DOI] [PubMed] [Google Scholar]
- Weisner C, Matzger H, Kaskutas LA. How important is treatment? one-year outcomes of treated and untreated alcohol-dependent individuals. Addiction. 2003;98:901–911. doi: 10.1046/j.1360-0443.2003.00438.x. [DOI] [PubMed] [Google Scholar]
- Yuan KH, Bentler PM, Kano Y. On averaging variables in a confirmatory factor analysis model. Behaviormetrika. 1997;24:71–83. [Google Scholar]