Abstract
Background:
Previous uncontrolled studies have suggested that there is late cognitive decline after coronary artery bypass grafting that may be attributable to use of the cardiopulmonary bypass pump.
Methods:
In this prospective, nonrandomized, longitudinal study, we compared cognitive outcomes after on-pump coronary artery bypass surgery (n=152) with: off-pump bypass surgery (n=75); nonsurgical cardiac comparison subjects (n=99); and 69 heart-healthy comparison (HHC) subjects. The primary outcome measure was change from baseline to 72 months in the following cognitive domains: Verbal memory, Visual memory, Visuoconstruction, Language, Motor speed, Psychomotor speed, Attention, Executive function, and a composite Global score.
Results:
There were no consistent differences in 72-month cognitive outcomes among the 3 groups with coronary artery disease (CAD). The CAD groups had lower baseline performance, and a greater degree of decline compared to HHC. The degree of change was small with none of the groups having > 0.5 SD decline. None of the groups were substantially worse at 72 months compared to baseline.
Conclusions:
Compared to subjects with no vascular disease risk factors, the CAD patients had lower baseline cognitive performance and greater degrees of decline over 72 months, suggesting that in these patients, vascular disease may have an impact on cognitive performance. We found no significant differences in the long-term cognitive outcomes among patients with various CAD therapies, indicating that management strategy for CAD is not an important determinant of long-term cognitive outcomes.
Keywords: Neurocognitive deficits, Outcomes, CABG, vascular disease
INTRODUCTION
Coronary artery bypass grafting (CABG) surgery is effective for the treatment of angina, but the prospect of postoperative cognitive decline associated with the use of cardiopulmonary bypass (CPB) has become a significant concern for many patients.
Short-term cognitive changes have been documented in some patients after CABG, but these changes are generally mild and reversible by 3 – 6 months after surgery.1 It has been suggested, however, that these short-term changes set the stage for a “late decline” several years after surgery. One study found that compared with their preoperative baseline performance, 42% of patients had lower cognitive performance 5 years after surgery.2 Although the etiology of these late cognitive changes was unclear in that report since there was no control group, it was hypothesized that it might be related to the use of CPB.
Off-pump surgery (OPCAB) was developed to avoid or reduce the presumptive adverse neurocognitive outcomes associated with the use of CPB. Although some early observational studies reported lower incidence of cognitive decline after OPCAB, more recent randomized controlled trials have not found significant differences between on- and off-pump surgeries in the degree of early or late cognitive outcomes. 3-5 These findings indicate that long-term cognitive changes may not be specific to a CABG population.
The interpretation of most studies of cognitive outcomes after CABG has been difficult because of the lack of comparison groups either with or without coronary artery disease. In the present study, we compared the 72-month longitudinal cognitive test performance of patients undergoing CABG with that of patients having off-pump surgery and two other groups: patients with diagnosed coronary artery disease but no surgery, and a group of “heart-healthy” subjects with no known risk factors for coronary artery or cerebrovascular disease. The principal goal of our study was to determine if CAD patients treated surgically had long-term cognitive decline and if there was evidence of disproportionate decline relative to those treated with nonsurgical medical therapy.
PATIENTS AND METHODS
Study Design
This prospective, nonrandomized study was approved by the Johns Hopkins IRB committee on 7/14/97. We compared 4 groups: conventional on-pump CABG; off-pump CAB; medically treated patients with diagnosed coronary artery disease but no surgery (NSCC); and a heart-healthy comparison (HHC) group. Inclusion criteria required that subjects be able to undergo neuropsychological testing: able to give written informed consent, able to sit upright, were native English speaking, and not mechanically ventilated. Patients were not excluded for medical reasons. All participants had a standardized neuropsychological test battery, assessment of depressive symptoms, and medical history review at baseline (preoperatively for the surgical groups), and at 3, 12, 36, and 72 months. The 72-month data collection was completed in August 2008. The primary outcome measures for this study were within-subject cognitive change over time.
Patients
Coronary Artery Bypass Grafting (CABG) group (n=152)
Patients scheduled to undergo isolated on-pump coronary artery bypass grafting were enrolled from all eight surgeons between September 1997 and March 1999 at our institution. There were minimal differences in the surgical and anesthetic techniques as would be expected within a single institution; these procedures have been described elsewhere. 1
Off-Pump Coronary Artery Bypass (OPCAB) Group (n= 75)
Patients scheduled to undergo off-pump CABG surgery without the use of the cardiopulmonary bypass pump were asked to participate. As a single institution could not provide enough cases to meet our sample size needs, off-pump patients were recruited from five different area hospitals. Off-pump patients were enrolled between March 1998 and October 2003. Separate IRB approval was obtained from all participating institutions. Because multiple sites were involved, anesthetic medications and surgical techniques differed, as described elsewhere.6 This group was used to control for the effects of the cardiopulmonary bypass pump.
Nonsurgical Cardiac Comparison (NSCC) Group (n=99)
Four cardiologists at our institution referred patients who were under medical management for diagnosed stable coronary artery disease (by coronary angiography) for inclusion into the study. Those who had had a cardiac surgical procedure in the past were not eligible. Patients were enrolled from September 1997 through April 2003. This group was used to control for surgical and anesthetic effects.
Heart-Healthy Comparison (HHC) Group (n=69)
Community-dwelling subjects were recruited via IRB-approved newspaper advertisements from November 2001 to September 2003. We enrolled heart-healthy subjects with comparable age, gender, and education profiles to match our other study groups. To exclude subjects with risk factors for heart disease, this group was screened by telephone interview for the following medical history variables: diabetes mellitus, kidney disease, hypertension, coronary artery disease (including myocardial infarction, angina, and high cholesterol), stroke/transient ischemic attack, peripheral vascular disease, and medications used to treat the above conditions. This group was added to control for the effects of vascular disease on the brain.
Neuropsychological and mood assessment
All participants were administered a battery of standardized neuropsychological tests on the following longitudinal schedule: baseline (preoperatively for surgical patients), 3, 12, 36, and 72 months. The scores from these 16 tests and subtests were combined as an unweighted average into the following eight cognitive domain scores: Verbal memory; Visual memory; Visuoconstruction; Language; Motor speed; Psychomotor speed; Attention; Executive function. In addition, all the neuropsychological measures were combined into a composite Global measure of cognition. The Mini-Mental State Exam (MMSE),7 The Center for Epidemiological Studies Depression scale (CESD),8 and Beth Israel Functional Status Questionnaire (FSQ) 9 were also administered at each time point.
All subjects were tested by the same team of study investigators, irrespective of the site where they were enrolled and interviewed. Over the entire course of the study, six cognitive testers were involved in this study, all of whom were trained in a standardized manner. These testers then traveled to all the sites to examine patients as needed. The same tester attempted to see the same subjects for follow-up. Previous test results were not reviewed before subsequent testing.
Statistical methods
The primary data analysis examined the degree of improvement or decline in cognitive domain scores at 72 months relative to an individual's baseline or 12-month performance (late decline). We analyzed z-scores adjusting for age (with 2 degrees of freedom), gender and education (with 2 degrees of freedom), and standardized with respect to the heart-healthy control group's mean and standard deviation. For timed tests the original scores were inverted so that improved performance resulted in a higher score, as was the case for non-timed scores.
To examine how the changes in neuropsychological test z-scores over time might be related to subject-specific covariates, we used a linear mixed effects model for the z-scores from each test estimating a separate learning effect and time trend for each group. To calculate the change scores in the eight domains, we pooled the estimates from the separate tests in each domain and used bootstrapping to quantify the statistical uncertainty of these pooled values. This methodology has been reported elsewhere. 10,11
Power was based on the standard errors of the group differences in average change from baseline (Table 4). This study has a greater than 95%, 95% and 98% power to detect a difference between each of the CABG, off-pump, and non-surgical controls in the Global composite score as compared to the HHC group of 0.3 population standard deviation true differences. A 0.3 standard deviation difference between the groups over 6 years is equivalent to a difference in the trend in cognitive decline between the two groups of 0.5 standard deviation per year post intervention.
Table 4.
Difference in average adjusted change scores from baseline to 72 months comparing each coronary artery disease group to the heart healthy controls
| CABG compared to HHC a |
OPCAB compared to HHC a |
NSCC compared to HHC a |
||||
|---|---|---|---|---|---|---|
| Cognitive Domain | Difference | Difference | Difference | |||
| (95% CI) | p-value | (95% CI) | p-value | (95% CI) | p-value | |
| Verbal memory | −0.24 (−0.48, 0.01) |
0.06 | −0.04 (−0.30, 0.23) |
0.78 | −0.24 (−0.54, 0.06) |
0.12 |
| Visual memory |
−0.34 (−0.59, −0.09) |
0.01 | −0.03 (−0.31, 0.26) |
0.86 |
−0.38 (−0.75, −0.02) |
0.04 |
| Visuoconstruction |
−0.30 (−0.50, −0.10) |
< 0.01 | 0.00 (−0.21, 0.21) |
1.00 |
−0.29 (−0.50, −0.08) |
0.01 |
| Language | −0.27 (−0.55, 0.01) |
0.06 | −0.30 (−0.61, 0.01) |
0.06 | −0.20 (−0.46, 0.05) |
0.12 |
| Motor Speed | −0.19 (−0.47, 0.08) |
0.17 | 0.00 (−0.29, 0.28) |
0.98 |
−0.40 (−0.69, −0.12) |
0.01 |
| Psychomotor Speed |
−0.19 (−0.41, 0.02) |
0.07 | −0.15 (−0.38, 0.08) |
0.21 | −0.11 (−0.35, 0.13) |
0.37 |
| Attention | −0.20 (−0.52, 0.12) |
0.23 |
−0.34 (−0.65, −0.03) |
0.03 | −0.12 (−0.51, 0.26) |
0.54 |
| Executive Function |
−0.39 (−0.65, −0.12) |
< 0.01 | −0.22 (−0.52, 0.09) |
0.17 | −0.30 (−0.61, 0.02) |
0.07 |
| Global |
−0.25 (−0.41, −0.09) |
< 0.01 | −0.11 (−0.26, 0.05) |
0.18 |
−0.25 (−0.45, −0.06) |
0.01 |
CABG = coronary artery bypass grafting; HHC = heart healthy control; NSCC = non-surgical cardiac comparison; OPCAB = off-pump coronary artery bypass;
negative number indicates that group declined more than the HHC group; statistically significant differences are shown in bold
RESULTS
Demographics and baseline medical characteristics
Baseline demographic and medical characteristics of the study groups are summarized in Table 1. The 4 groups were well-balanced in terms of age, education, and gender. The surgical groups had similar prevalence of risk factors for coronary artery disease. The number of patients with triple vessel coronary artery disease was significantly higher in the CABG group (79%) than in the off-pump (59%) and NSCC groups (26%). The follow-up time was about 30% longer for the CABG as compared with the HHC group. This difference was controlled for in the regression models used for the estimates of the group differences at 6-year follow-up.
Table 1.
Comparison of all study groups at baseline entry into the study (N=395)
| Variable | CABG (n=152) |
OPCAB (N=75) |
NSCC (N=99) |
HHC (N=69) |
|---|---|---|---|---|
| Demographics | ||||
| Mean age (years) | 63.6 (9.4) | 66.0 (10.5) | 65.7 (9.2) | 62.5 (10.9) |
| Age ≥ 75 (years) | 13% | 20% | 16% | 16% |
| Male gender | 76% | 72% | 75% | 71% |
| Mean education (years) c | 14.1 (4.0) | 13.4 (3.3) | 14.4 (3.4) | 16.0 (2.6) |
| College education (>bachelors) | 26% | 17% | 32% | 36% |
| Caucasian | 90% | 93% | 93% | 96% |
| Retired c | 46% | 60% | 59% | 36% |
| Medical History | ||||
| Past stroke | 5% | 3% | 4% | 0 a |
| Carotid bruit | 17% | 12% | 8% | X |
| Hypertension | 64% | 68% | 52% | 0 a |
| Diabetes mellitus | 30% | 37% | 22% | 0 a |
| High risk for stroke b | 9% | 15% | 8% | 0 a |
| Peripheral vascular disease d | 16% | 25% | 6% | 0 a |
| Transient ischemic attack | 5% | 4% | 2% | 0 a |
| Myocardial infarction | 47% | 56% | 49% | 0 a |
| Myocardial infarction past month d | 18% | 15% | 2% | 0 a |
| History of chest pain/angina d | 79% | 78% | 62% | 0 a |
| History of atrial fibrillation | 10% | 17% | 15% | 0 a |
| Three vessel coronary disease d | 78% | 59% | 26% | 0 a |
| Mean # diseased coronaries d | 2.73 (0.5) | 2.49 (0.7) | 1.95 (0.7) | 0 a |
| PCI d | 21% | 27% | 52% | 0 a |
| Past cardiac surgery | 9% | 6% | 0 a | 0 a |
| Taking a beta-blocker | 66% | 59% | 62% | 1% a |
| Taking a statin | 60% | 59% | 61% | 0 a |
| Taking an antidepressant | 10% | 12% | 14% | 7% |
| General anesthesia in past 5 years | 24% | 32% | 25% | 35% |
| Chronic obstructive pulmonary dis. | 9% | 7% | 5% | 1% |
| Family history Alzheimer's disease | 13% | 12% | 9% | 23% |
| Smoking history | 70% | 71% | 57% | 55% |
| Currently smoking c | 11% | 16% | 4% | 3% a |
| Elective surgical case | 61% | 63% | - | - |
| Physiologic Data | ||||
| Mean serum BUN (mg/L) d | 17.5 (6.5) | 21.7 (13.5) | 16.8 (5.7) | X |
| Mean serum creatinine (mg/L) | 1.05 (.44) | 1.18 (.57) | 1.04 (.27) | X |
| Any APO-e4 genotype | 25% | 29% | 30% | 25% |
| Mean systolic BP (mmHg) c/ d | 131 (22) | 132 (20) | 141 (27) | 127 (17) |
| Mean diastolic BP (mmHg) c/ d | 73 (11) | 72 (11) | 79 (13) | 77 (11) |
| Mean MAP (mmHg) c/ d | 92 (13) | 92 (12) | 100 (16) | 94 (12) |
| Mean heart rate (BPM) | 66 (14) | 71 (17) | 66 (11) | 69 (11) |
| Mean pulse pressure c | 58.0 (19) | 60.5 (17) | 62.0 (21) | 49.6 (12) |
| Pulse pressure >65 c | 29.5% | 34.7% | 34.0% | 11.8% |
| Test Data | ||||
| Mean MMSE score c | 27.6 (2.4) | 27.7 (2.0) | 27.9 (2.0) | 28.5 (1.9) |
| MMSE score <24 | 4.6% | 4.2% | 6.1% | 1.4% |
| Mean CES-D score c/ d | 13.2 (9.6) | 12.6 (10.4) | 9.3 (8.3) | 6.2 (7.2) |
| CES-D score >15 c | 33% | 30% | 17% | 10% |
| Mean FSQ score c/ d | 30.6 (5.1) | 29.9 (5.6) | 32.9 (3.9) | 34.6 (2.6) |
| Mean cognitive testing times (mins) | 56 (11) | 57 (11) | 56 (9) | 52 (8) |
APO = apolipoprotein e-4 allele present; BP = blood pressure in mmHg = millimeters of mercury; BPM = beats per minute; BUN = blood urea nitrogen; mg/L = milligrams per liter; CABG = coronary artery bypass grafting; CES-D = Center for Epidemiological Study-Depression, score >15 indicative of depressive symptoms 8; FSQ = Beth Israel Functional Status Questionnaire, physical functioning score (best functional score = 36)9; HHC = healthy heart control; MAP = mean arterial pressure; MMSE = Mini-Mental Status Exam (best score = 30) 7; means shown with standard deviations in brackets; NSCC = non-surgical cardiac comparison; OPCAB = off-pump coronary artery bypass; PCI = Percutaneous coronary intervention, either angioplasty and/or stent placement; Pulse pressure = systolic minus diastolic blood pressure; X = data not collected for this group.
subjects screened for this/these variables prior to enrollment
McKhann et al. Arch Neurol 200223
indicates significant difference (p<0.01) between the 4 study groups
indicates significant difference (p<0.01) between the 3 coronary artery disease groups.
Completeness of follow-up and mortality
The patterns of follow-up and mortality are shown in Table 2. The 72-month mortality did not differ among the 3 groups with coronary artery disease. Of the surviving patients, the percentage of patients completing the follow-up testing at 72 months was >75% in all groups. The numbers of patients who were lost to follow-up or who refused follow-up testing were comparable among the groups with coronary artery disease, but there were fewer in the heart-healthy group.
Table 2.
Interim data and cumulative medical history reporting at 72 months
| Variables | CABG (n=152) |
OPCAB (n=75) |
NSCC (n=99) |
HHC (n=69) |
|---|---|---|---|---|
| Testing Status at 72 months | ||||
| Deceased | 26/152 (17%) | 18/75 (24%) | 19/99 (19%) | 3/69 (4%) |
| Completed cognitive testing | 96/126 (76%) | 43/57 (75%) | 67/80 (84%) | 60/66 (91%) |
| Refused cognitive testing | 23/126 (18%) | 9/57 (16%) | 9/80 (11%) | 3/66 (4.5%) |
| No contact/lost to follow-up | 7/126 (6%) | 5/57 (9%) | 4/80 (5%) | 3/66 (4.5%) |
| Patients in nursing home | 2 | 3 | 0 | 0 |
| Mean days since enrollment a/ b | 2525 (436) | 2108 (321) | 2272 (381) | 1858 (45) |
| Tested in clinic location a/ b | 51% | 39% | 69% | 83% |
| Mean testing time (min) a | 62 (14) | 60 (12) | 61 (13) | 56 (11) |
| Mean age at 72 months (yrs) | 71.2 (9.7) | 70.4 (9.9) | 71.9 (9.6) | 67.6 (10.7) |
|
Test Data and Subjective Reporting at 72 months |
(n = 96) | (n=43) | (n=67) | (n=60) |
| Mean MMSE score a | 27.4 (2.5) | 28.5 (1.8) | 28.0 (2.3) | 28.6 (1.7) |
| MMSE score <24 | 7% | 2% | 7% | 2% |
| MMSE change from baseline | −0.22 (2.0) | −0.40 (1.6) | −0.12 (2.5) | 0.02 (1.5) |
| Mean CES-D score a | 9.5 (9.2) | 11.3 (9.7) | 9.0 (9.4) | 6.0 (6.2) |
| CES-D score >15 | 15% | 21% | 15% | 10% |
| Mean FSQ score a | 29.9 (6) | 31.7 (5) | 31.9 (5) | 34.1 (4) |
| Vision complaints | 57% | 48% | 54% | 62% |
| Memory change for the worse a | 51% | 52% | 50% | 30% |
| Personality change for the worse | 21% | 29% | 18% | 12% |
| Working for wages a | 40% | 25% | 28% | 53% |
| Physiologic Data at 72 months | ||||
| Mean systolic BP (mmHg) | 132 (20) | 134 (20) | 135 (19) | 129 (16) |
| Mean diastolic BP (mmHg) a | 71 (10) | 69 (12) | 73 (10) | 76 (10) |
| Mean MAP (mmHg) | 91 (11) | 91 (12) | 94 (11) | 94 (11) |
| Mean heart rate (BPM) a | 65 (10) | 66 (10) | 64 (9) | 69 (11) |
| Mean pulse pressure (mmHg) a | 62 (19) | 65 (19) | 63 (18) | 52 (12) |
| Pulse pressure >65 mmHg a | 45% | 44% | 40% | 12% |
|
Cumulative Medical Data Reporting Since Baseline c |
(n=136) | (n=68) | (n=96) | (n=68) |
| Hospitalized a | 58% | 47% | 59% | 33% |
| Surgical procedure w/GA | 42% | 39% | 32% | 34% |
| Chest pain reported a/d | 22% | 21% | 28% | 2% |
| Visit to cardiologist/internist a | 99% | 100% | 100% | 90% |
| ECG done a | 94% | 96% | 99% | 80% |
| Stress testing done a | 81% | 76% | 83% | 31% |
| Myocardial infarction | 6% | 4% | 4% | 0 |
| Coronary angiogram a | 24% | 27% | 28% | 4% |
| PCI | 10% | 10% | 13% | 3% |
| Had a new CABG | 0 | 0 | 19% | 0 |
| Atrial fibrillation | 28% | 21% | 15% | 6% |
| New diagnosis of hypertension | 13% | 7% | 12% | 15% |
| New diagnosis of diabetes | 9% | 6% | 12% | 4% |
| New diagnosis of thyroid disease | 9% | 9% | 12% | 2% |
| Stroke | 6% | 4% | 3% | 0 |
| TIA | 7% | 3% | 4% | 1% |
| Current smoking | 5% | 15% | 10% | 4% |
| Cancer/cancer therapy | 18% | 24% | 19% | 21% |
| Takes medications as ordered | 93% | 91% | 98% | 94% |
| Taking a beta-blocker a | 72% | 73% | 69% | 3% |
| Taking antidepressants a | 7% | 20% | 18% | 7% |
| Taking a benzodiazepine a | 5% | 11% | 10% | 0 |
| Taking a statin a | 85% | 77% | 75% | 12% |
| Taking cognitive enhancing drug | 4% | 4% | 6% | 0 |
BP = blood pressure in mmHg = millimeters of mercury; BPM = beats per minute; CABG = coronary artery bypass grafting; CES-D = Center for Epidemiological Study-Depression score >15 indicative of depressive symptoms 8; ECG = electrocardiogram; FSQ = Beth Israel Functional Status Questionnaire9, physical functioning score (best functional score = 36); GA = general anesthesia; HHC = healthy heart control; MAP = mean arterial pressure; MMSE = Mini-Mental Status Exam7 score (best score = 30); Means are shown with standard deviations in brackets; NSCC = non-surgical cardiac comparison; NTG = sublingual nitroglycerine; OPCAB = off-pump coronary artery bypass; PCI = percutaneous coronary intervention, either angioplasty and/or stent placement; Pulse pressure = systolic minus diastolic blood pressure; TIA = transient ischemic attack.
indicates significant (p<0.01) difference between the 4 study groups
indicates significant (p<0.01) difference between the 3 coronary artery disease groups
cumulative data -reported at any study follow-up time point (3, 12, 36, or 72 months)
patient self-report of chest pain/angina following structured questioning by interviewers
Baseline cognitive performance
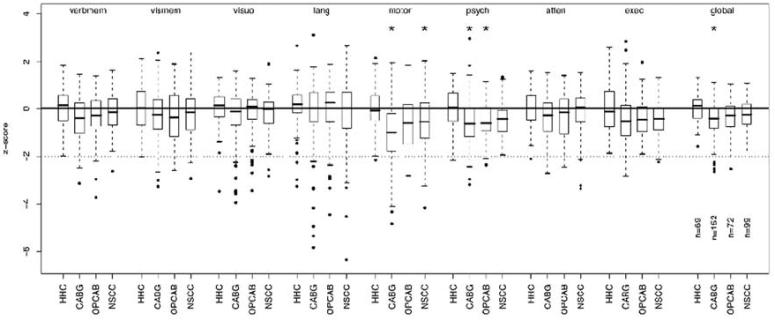
Figure 1 compares the baseline cognitive test performance of the HHC group with that of the 3 groups with coronary artery disease. The unadjusted mean scores for individual neuropsychological measures for all groups at baseline, 12, and 72 months are shown in Appendix 1* in the supplemental materials. Overall, the adjusted median baseline test scores were higher in the HHC group than in the CAD groups for all cognitive domains, with statistically significant differences for the domains of motor speed, psychomotor speed, and the global cognitive domain score. In addition, there were a number of participants in the CAD groups who had baseline scores more than 2 standard deviations below the median of the HHC group. The number of study participants with below normal (< 24) baseline MMSE scores was low, ranging from only 1.4% in the HHC group to 6% in the NSCC group.
Figure 1. Boxplots showing the median distribution of baseline z-scores for each cognitive domain by study group.
Verbmem = verbal memory; vismem = visual memory; visuo = visuoconstruction; lang = language; motor = motor speed; psych = psychomotor speed; atten = attention; exec = executive function; global = global composite scores * These coronary artery disease groups have a difference in their baseline means compared to HHC that are statistically significant at alpha=.05. HHC = heart healthy controls; CABG = coronary artery bypass grafting; OPCAB = off-pump coronary artery bypass (3 patients did not complete baseline testing); NSCC = nonsurgical cardiac comparison group.
Performance of the HHC group
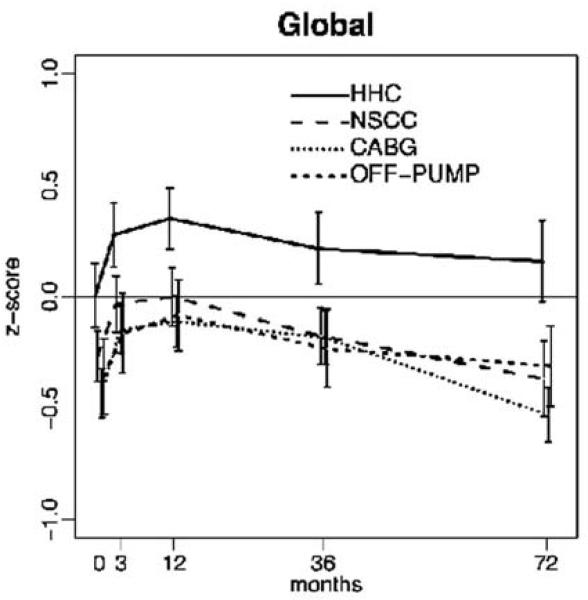
From baseline to 72 months, the heart-healthy comparison group had mild improvements in all cognitive domains, with statistically significant improvement in visual memory (p= 0.03), attention (p< 0.01), and the global score (p=0.01). From 12 months to 72 months, the HHC group had mild decline in all but one domain, with statistically significant decline in verbal memory (p=0.01), visual memory (p<0.01), motor speed (p=0.02)), attention, (p=0.02), and the composite global score (p<0.01). (Within-group changes for all study groups are shown in Supplemental Appendices 2* and 3*) The longitudinal changes in the composite global score are illustrated in Figure 2.
Figure 2. Distribution of longitudinal composite global score pattern for each study group.
HHC = heart healthy controls; NSCC = nonsurgical cardiac comparisons; CABG = coronary artery bypass grafting; OPCAB = off-pump coronary artery bypass group.
Change from baseline to 72 months for coronary artery groups
To evaluate the overall magnitude of change from baseline to the 72-month follow-up, we compared the baseline adjusted z-scores with the 72-month scores for each of the coronary artery groups. We found no consistent differences in the degree of cognitive change over time among these 3 groups with coronary artery disease. The off-pump group showed less change over time for two cognitive domains (visual memory and visuoconstruction), but there were no significant differences in the degree of change for the other 6 cognitive domains and composite global score (see Table 3).
Table 3.
Average change scores from baseline to 72 months for the 3 coronary artery disease groups
| CABG | OPCAB | NSCC | ||
|---|---|---|---|---|
| Cognitive Domain | Change Score (95% CI) |
Change Score (95% CI) |
Change Score (95% CI) |
p-value a |
| Verbal memory | −0.05 (−0.20, 0.10) |
0.15 (−0.01, 0.30) |
−0.06 (−0.28, 0.17) |
0.15 |
| Visual memory | −0.11 (−0.28, 0.06) |
0.20 (−0.02, 0.41) |
−0.16 (−0.43, 0.11) |
0.03 |
| Visuoconstruction | −0.29 (−0.43, −0.15) |
0.01 (−0.15, 0.16) |
−0.29 (−0.46, −0.12) |
0.02 |
| Language | −0.18 (−0.38, 0.02) |
−0.20 (−0.45, 0.04) |
−0.11 (−0.29, 0.07) |
0.72 |
| Motor Speed | −0.16 (−0.32, 0.01) |
0.04 (−0.18, 0.25) |
−0.37 (−0.59, −0.14) |
0.08 |
| Psychomotor speed | −0.09 (−0.22, 0.04) |
−0.04 (−0.21, 0.12) |
−0.01 (−0.17, 0.16) |
0.63 |
| Attention | 0.14 (−0.08, 0.37) |
0.01 (−0.21, 0.21) |
0.22 (−0.06, 0.50) |
0.35 |
| Executive function | −0.19 (−0.34, −0.03) |
−0.01 (−0.18, 0.16) |
−0.10 (−0.29, 0.09) |
0.38 |
| Global | −0.10 (−0.19, −0.01) |
0.05 (−0.05, 0.15) |
−0.10 (−0.25, 0.05) |
0.10 |
CABG = coronary artery bypass grafting; NSCC = non-surgical cardiac comparison; OPCAB = off-pump coronary artery bypass;
p-values for null hypothesis that the average adjusted changes are the same in the 3 groups are calculated from a Wald test of the relevant coefficients from the linear mixed model for the z-scores adjusted for age, gender and education; statistically significant comparisons are shown in bold.
To take into account systematic factors like practice effects and differences in age, gender, education, and to account for random variability associated with repeated administration of the same tests over time, we contrasted the average change observed in each of the CAD groups from that seen in the HHC participants (Table 4) using the linear mixed effect model described above. Relative to the changes observed in the HHC group, the CABG group had mild decline in all cognitive domains, with statistically significant decline in visual memory, visuoconstruction, executive function, and the global score (all p-values <0.01), while the OPCAB group had statistically significant greater decline for the domain of attention (p=0.03). The NSCC group had statistically significant decline in visual memory (p= 0.04), visuoconstruction, motor speed, and the global domains (all p-values <0.01). Overall, the magnitude of changes from baseline to 72 months was small, with none of the groups declining in performance more than one-half standard deviation.
Change from 12 months to 72 months (late decline)
To evaluate the degree of late cognitive decline, we compared the adjusted 12-month z-scores with the scores at 72 months for each group. Relative to the changes observed in the HHC group, the CABG had a greater degree of late decline in several cognitive domains, with statistically significant greater decline for the domains of verbal memory, (p= 0.04) visuoconstruction, (p< 0.01) language (p= 0.03), executive function (p<0.01) and the global composite domain (p<0.01). The pattern of late decline was similar in the nonsurgical group, who showed significantly greater decline than did the HHC group for the cognitive domains of visuoconstruction, (p < 0.01) motor speed, (p < 0.01) executive function (p= 0.03) and the composite global domain (p= 0.04). The off-pump group did not differ from the HHC group in the degree of late decline for any of the cognitive domains. Overall, the degree of change from 12 to 72 months was greater than that from baseline to 72 months. (data not shown)
Changes in Mini-Mental State Exam scores
We also examined changes in scores on the Mini-Mental State exam from baseline to follow-up points for all study groups. From baseline to 72 months, the average within-patient change on the MMSE ranged from a decline of 0.4 point for the OPCAB group to an improvement of 0.02 point for the HHC group. The number of patients with an MMSE score in the clinically impaired range (< 24) at 72 months was similar for the CABG and NSCC groups (7%) and somewhat lower (2%) for the OPCAB and HHC groups (Table 2).
COMMENT
The principal finding of this study was that although there is mild cognitive decline over time in all groups with CAD, we found no evidence of disproportionate long-term decline in patients who had conventional on-pump surgery when compared with patients with off-pump surgery or nonsurgical medical management. Comparison of changes in cognitive performance in these groups from baseline to 72 months or from 12 to 72 months showed greater decline in the groups with coronary artery disease than in the HHC comparison group, but no statistically significant differences in the degree of decline among the 3 groups with coronary artery disease. The lack of evidence for a clinically meaningful difference among CABG, off-pump, and nonsurgically treated patients suggests that choice of management strategies for coronary artery disease does not influence the long-term cognitive performance of these patients.
Compared with the HHC group, the 3 groups with coronary artery disease had lower performance even at baseline. This finding is consistent with results from several other studies that have reported lower than expected cognitive performance among candidates for CABG before surgery. 12,13 Jensen and colleagues found that 20% of their CABG candidates had a Mini-Mental State score in the impaired range (< 24) before surgery,3 and another recent study reported that 45% of their patients met operational criteria for cognitive impairment before surgery. 14 Studies that have examined the nature of the preoperative cognitive impairment have reported that the cognitive domains most commonly impaired include executive functioning, memory, and speed of processing.15 These are also the cognitive domains that have been found to be impaired in patients with subcortical small vessel disease,16 suggesting that patients with coronary artery disease may also have cerebrovascular disease.
Subjects in all 4 groups improved from baseline to 3 months, as well as from 3 to12 months. Other studies have also shown this trend.1,2 We attribute this improvement to a combination of postoperative recovery and practice effects associated with greater familiarity with the neuropsychological tests. Changes in cognitive performance from 3, 6, or 12 months to 5 years has been considered as “late” decline in previous studies.2,4,17 In our study, we observed decline in performance from 12 to 72 months for all groups, including the HHC group for some cognitive domains. Compared with the HHC group there were also statistically greater, but nonetheless modest, late changes in the CABG and NSCC groups. This suggests to us that there is mild late decline after CABG, but because a similar degree of decline was found in the NSCC group, they are not specific to CABG patients. Previous longitudinal studies of community-dwelling individuals have also reported decline in performance on some cognitive tests with longer follow-up periods 18 and attributed this decline to a combination of reduced practice effects and age-related changes in performance. Thus, although there has been considerable interest in the phenomenon of “late” cognitive decline after medical interventions, we believe that comparison with the actual baseline performance provides a clinically more useful measure of long-term cognitive changes.
We did not find evidence of clinically relevant changes over 72 months in a commonly used screening measure of cognitive performance (the Mini-Mental State Exam), and there were no significant differences among the coronary artery disease groups in the degree of change in MMSE over time. The changes observed in the MMSE scores in our study are comparable to those that have been reported for community-dwelling older persons.19 Some previous studies have suggested that CABG may be associated with greater risk of developing Alzheimer's disease.20 However, we found no difference between the CABG and NSCC in the frequency of patients with an MMSE score in the clinically impaired range at 72 months.
Our findings are consistent with those of previous studies that have compared cognitive outcomes after on- versus off-pump surgery. One large randomized controlled trial reported that both on- and off-pump patients had comparable incidence of decline at 5 years in the two groups. They concluded that factors other than the use of cardiopulmonary bypass were responsible for the long-term cognitive decline.4 They hypothesized that use of general anesthesia and the systemic inflammatory response associated with major surgery could account for the late decline, but could not rule out other factors such as, for example, normal aging. We observed a similar degree of long-term cognitive change in both the nonsurgical and CABG patients, suggesting that these changes may not be attributable to anesthesia or major surgery. Rather, the changes in these two groups may be related to a combination of increasing age and cerebrovascular disease. In previous studies, one of the most consistent predictor's of late cognitive decline has been older age. 2,4 Patients with coronary artery disease have been found to have a high prevalence of cerebrovascular disease, even before surgery. 21,22 The lower cognitive performance observed at baseline in all groups with coronary artery disease would be consistent with possible manifestations of cerebrovascular disease.
This study has limitations: it was not randomized as it was not possible at the time of inception of our study to design or implement such a study. Further, it was not ethically appropriate to randomize patients with triple vessel coronary artery disease to surgical or nonsurgical treatment. The changes from baseline to 72 months observed in the composite global score in our CAD groups are of similar magnitude (ranging from −0.10 to 0.05 standard deviation units) to that observed in previous randomized comparisons of on- and off-pump patients (ranging from −0.06 to −0.09 standard deviations units), 4 suggesting that our findings are similar to those from the only prospective randomized study of these two populations. The majority of patients, with the exception of the off-pump group, were from a single institution. Although it is possible that these findings would not apply to a larger population, the patient demographics for this study are similar to those in many studies of CABG populations in academic medical centers in the United States. It is also possible that selective drop-out of poorly performing subjects would bias the findings from this study. Our statistical methods adjusted for differential drop-out rates that are predictable from observed variables, but not for those that cannot be observed.
The strengths of this study are in its design, with appropriate comparison groups, length of follow-up, and testing by the same closely knit, experienced team. The overall loss to follow-up in this study is similar to what has been reported in previous long-term studies of cognition after CABG. The mortality and follow-up rates were similar in the 3 coronary artery groups. Hence, comparisons of change in cognitive performance among the groups with CAD are not biased by differential mortality. There was, however, higher mortality among the CAD groups than in the HHC group, and we therefore cannot rule out some bias in these comparisons.
In contrast with many previously published studies of long-term cognitive change, we included all eligible subjects in each group with no exclusions for medical reasons. Previous studies of late cognitive decline after CABG have generally focused on the incidence of late decline. 2,4,17 In the absence of appropriate comparison groups, however, the choice of a criterion for what constitutes actual decline is largely arbitrary. Thus, previously reported incidences of decline have limited clinical applicability. We chose to analyze within-patient changes in performance over time using comparison patients with and without coronary artery disease, which allowed us to take into account factors associated with repeated cognitive testing such as practice effects, random variability, and regression to the mean.
In summary, this study indicates that there is mild decline in cognitive performance over the 72-month follow-up period for all 3 groups with coronary artery disease. The lack of significant differences in the late cognitive outcomes between the groups with coronary artery disease groups rules out any selective effects attributable to the surgery, anesthesia, or the use of cardiopulmonary bypass. Thus, we conclude that long-term cognitive performance should not be a factor in choice of therapy for coronary artery disease.
Supplementary Material
Acknowledgements
This study was supported by grant 35610 from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, Bethesda, MD; by the Dana Foundation, New York, N.Y., and the Johns Hopkins Medical Institution GCRC grant RR 00052. The authors thank the participating physicians and surgeons who contributed to patient recruitment from our institution, as well as referring off-pump surgical sites. We acknowledge the efforts of Louis M. Borowicz, Jr. who assisted in the coordination of the study and neuropsychological testing, and thank Pamela Talalay, PhD, Rebecca Gottesman, MD, and Marilyn Albert, PhD, for their assistance in manuscript preparation. Special thanks are extended to our study participants who volunteered their time and energy to make this study possible.
Acronyms and Abbreviations
- CABG
Coronary Artery Bypass Grafting
- CAD
Coronary Artery Disease
- CPB
Cardiopulmonary Bypass
- CES-D
Center for Epidemiological Studies – Depression scale
- FSQ
Functional Status Questionnaire
- HHC
Heart-Healthy Comparison group
- MMSE
Mini-Mental Status Examination
- NSCC
Nonsurgical Comparison group
- OPCAB
Off-pump Coronary Artery Grafting
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Selnes OA, Grega MA, Borowicz LM, Jr., Royall RM, McKhann GM, Baumgartner WA. Cognitive changes with coronary artery disease: a prospective study of coronary artery bypass graft patients and nonsurgical controls. Ann Thorac Surg. 2003;75:1377–1384. doi: 10.1016/s0003-4975(03)00021-3. [DOI] [PubMed] [Google Scholar]
- 2.Newman MF, Kirchner JL, Phillips-Bute B, et al. Longitudinal assessment of neurocognitive function after coronary- artery bypass surgery. N Engl J Med. 2001;344:395–402. doi: 10.1056/NEJM200102083440601. [DOI] [PubMed] [Google Scholar]
- 3.Jensen BO, Hughes P, Rasmussen LS, Pedersen PU, Steinbruchel DA. Cognitive outcomes in elderly high-risk patients after off-pump versus conventional coronary artery bypass grafting: a randomized trial. Circulation. 2006;113:2790–2795. doi: 10.1161/CIRCULATIONAHA.105.587931. [DOI] [PubMed] [Google Scholar]
- 4.van Dijk D, Spoor M, Hijman R, et al. Cognitive and cardiac outcomes 5 years after off-pump vs on-pump coronary artery bypass graft surgery. JAMA. 2007;297:701–708. doi: 10.1001/jama.297.7.701. [DOI] [PubMed] [Google Scholar]
- 5.Takagi H, Tanabashi T, Kawai N, Umemoto T. Cognitive decline after off-pump versus on-pump coronary artery bypass graft surgery: meta-analysis of randomized controlled trials. J Thorac Cardiovasc Surg. 2007;134:512–513. doi: 10.1016/j.jtcvs.2007.04.035. [DOI] [PubMed] [Google Scholar]
- 6.McKhann GM, Grega MA, Borowicz LM, Jr., et al. Is there cognitive decline 1 year after CABG? Comparison with surgical and nonsurgical controls. Neurology. 2005;65:991–999. doi: 10.1212/01.wnl.0000175220.78475.99. [DOI] [PubMed] [Google Scholar]
- 7.Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 8.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Measurement. 1977;1:385–401. [Google Scholar]
- 9.Jette AM, Davies AR, Cleary PD, et al. The Functional Status Questionnaire: reliability and validity when used in primary care. J Gen Intern Med. 1986;1:143–149. doi: 10.1007/BF02602324. [DOI] [PubMed] [Google Scholar]
- 10.Barry SJ, Zeger SL, Selnes OA, Grega MA, Borowicz LM, Jr., McKhann GM. Quantitative methods for tracking cognitive change 3 years after coronary artery bypass surgery. Ann Thorac Surg. 2005;79:1104–1109. doi: 10.1016/j.athoracsur.2004.10.016. [DOI] [PubMed] [Google Scholar]
- 11.Selnes OA, Grega MA, Bailey MM, et al. Neurocognitive outcomes 3 years after coronary artery bypass graft surgery: a controlled study. Ann Thorac Surg. 2007;84:1885–1896. doi: 10.1016/j.athoracsur.2007.06.054. [DOI] [PubMed] [Google Scholar]
- 12.Vingerhoets G, Van Nooten G, Jannes C. Neuropsychological impairment in candidates for cardiac surgery. J Int Neuropsychol Soc. 1997;3:480–484. [PubMed] [Google Scholar]
- 13.Millar K, Asbury AJ, Murray GD. Pre-existing cognitive impairment as a factor influencing outcome after cardiac surgery. Br J Anaesth. 2001;86:63–67. doi: 10.1093/bja/86.1.63. [DOI] [PubMed] [Google Scholar]
- 14.Hogue CW, Fucetola R, Hershey T, et al. Risk factors for neurocognitive dysfunction after cardiac surgery in postmenopausal women. Ann Thorac Surg. 2008;86:511–516. doi: 10.1016/j.athoracsur.2008.04.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ernest CS, Murphy BM, Worcester MU, et al. Cognitive function in candidates for coronary artery bypass graft surgery. Ann Thorac Surg. 2006;82:812–818. doi: 10.1016/j.athoracsur.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 16.Prins ND, van Dijk EJ, den HT, et al. Cerebral small-vessel disease and decline in information processing speed, executive function and memory. Brain. 2005;128:2034–2041. doi: 10.1093/brain/awh553. [DOI] [PubMed] [Google Scholar]
- 17.Nathan HJ, Wells GA, Munson JL, Wozny D. Neuroprotective effect of mild hypothermia in patients undergoing coronary artery surgery with cardiopulmonary bypass: a randomized trial. Circulation. 2001;104:I85–I91. doi: 10.1161/hc37t1.094710. [DOI] [PubMed] [Google Scholar]
- 18.Ratcliff G, Dodge H, Birzescu M, Ganguli M. Tracking cognitive functioning over time: Ten-year longitudinal data from a community-based study. Applied Neuropsychology. 2003;10:76–88. doi: 10.1207/S15324826AN1002_03. [DOI] [PubMed] [Google Scholar]
- 19.Eslinger PJ, Swan GE, Carmelli D. Changes in Mini-Mental State Exam in community-dwelling older persons over 6 years: relationship to health and neuropsychological measures. Neuroepidemiology. 2003;22:23–30. doi: 10.1159/000067113. [DOI] [PubMed] [Google Scholar]
- 20.Lee TA, Wolozin B, Weiss KB, Bednar MM. Assessment of the emergence of Alzheimer's disease following coronary artery bypass graft surgery or percutaneous transluminal coronary angioplasty. J Alzheimer's Dis. 2005;7:319–324. doi: 10.3233/jad-2005-7408. [DOI] [PubMed] [Google Scholar]
- 21.Goto T, Baba T, Honma K, et al. Magnetic resonance imaging findings and postoperative neurologic dysfunction in elderly patients undergoing coronary artery bypass grafting. Ann Thorac Surg. 2001;72:137–142. doi: 10.1016/s0003-4975(01)02676-5. [DOI] [PubMed] [Google Scholar]
- 22.Vermeer SE, Longstreth WT, Jr., Koudstaal PJ. Silent brain infarcts: a systematic review. Lancet Neurol. 2007;6:611–619. doi: 10.1016/S1474-4422(07)70170-9. [DOI] [PubMed] [Google Scholar]
- 23.McKhann GM, Goldsborough MA, Borowicz LM, Jr., et al. Predictors of stroke risk in coronary artery bypass patients. Ann Thorac Surg. 1997;63:516–521. doi: 10.1016/s0003-4975(97)83384-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.