Abstract
Use of warfarin, clopidogrel, or aspirin associates with mortality among patients with ESRD, but the risk-benefit ratio may depend on underlying comorbidities. Here, we investigated the association between these medications and new stroke, mortality, and hospitalization in a retrospective cohort analysis of 1671 incident hemodialysis patients with preexisting atrial fibrillation. We followed patient outcomes from the time of initiation of dialysis for an average of 1.6 yr. Compared with nonuse, warfarin use associated with a significantly increased risk for new stroke (hazard ratio 1.93; 95% confidence interval 1.29 to 2.90); clopidogrel or aspirin use did not associate with increased risk for new stroke. Analysis using international normalized ratio (INR) suggested a dose-response relationship between the degree of anticoagulation and new stroke in patients on warfarin (P = 0.02 for trend). Warfarin users who received no INR monitoring in the first 90 d of dialysis had the highest risk for stroke compared with nonusers (hazard ratio 2.79; 95% confidence interval 1.65 to 4.70). Warfarin use did not associate with statistically significant increases in all-cause mortality or hospitalization. In conclusion, warfarin use among patients with both ESRD and atrial fibrillation associates with an increased risk for stroke. The risk is greatest in warfarin users who do not receive in-facility INR monitoring.
Atrial fibrillation is a common comorbidity in patients with ESRD, with a prevalence of 9%.1 Even though the drug's efficacy and safety have yet to be shown in ESRD by prospective trials,2 warfarin is often prescribed in such dialysis patients3 as a carryover from recommendations in the general population on the basis of several studies that established its role in stroke prevention.4–11
We previously reported a significant excess mortality associated with anticoagulation and/or antiplatelet use in a large, heterogeneous population of incident hemodialysis (HD) patients.12 In an effort to develop a focused understanding for the indications for warfarin, clopidogrel, and aspirin prescription for patients with ESRD, we performed a follow-up study to determine the potential risk-benefit ratio of these drugs specifically in dialysis patients with coexisting atrial fibrillation.
The population of patients with atrial fibrillation is heterogeneous13–16 in terms of risk for stroke, and the hazards of anticoagulation may outweigh its benefits in certain subpopulations who are at increased risk for hemorrhage.17–23 Factors associated with serious hemorrhagic complications in warfarin users without renal failure include polypharmacy,24 advanced age,25 cerebrovascular disease,26 and heart failure19; such factors are also highly prevalent in the ESRD population.27–33 In addition, dialysis patients have several platelet defects and receive heparin during their dialysis treatment, which contributes to their coagulopathy.34,35
Taken together, warfarin use in dialysis patients may confer additional risk that is not appreciated in patients without renal failure.2,36 Given the paucity of clinical studies of patients with ESRD, it is currently unresolved whether accepted therapeutic interventions for atrial fibrillation4 can also be applied to patients who are on dialysis.2,37 Consequently, we conducted a retrospective cohort study to assess the overall risk-benefit ratio of anticoagulation and antiplatelet therapy in this specific population. We sought to determine the association between warfarin, clopidogrel, and aspirin use and stroke, mortality, and hospitalization in a large population of incident dialysis patients with preexisting atrial fibrillation. Such retrospective studies need to be viewed as hypothesis generating for future prospective clinical trials.
Results
Patient Population
A total of 48,825 incident HD patients were identified between January 1, 2003, and December 31, 2004, 2193 (4.5%) of whom had documented coexisting atrial fibrillation at the time of dialysis initiation. After exclusion of patients with <3 mo of follow-up (256 died, 114 discontinued dialysis treatment, 62 transferred to a non-Fresenius facility, 59 had renal recovery, 28 patients changed modality, one received a transplant, and two are unknown), the final cohort consisted of 1671 patients who were alive at 90 d after the initiation of dialysis. Among these patients with atrial fibrillation, 44.7% were receiving warfarin, 11.4% clopidogrel, and 37.3% aspirin. A total of 14.3% were on warfarin and at least one antiplatelet agent, and 5.8% of patients were on both clopidogrel and aspirin. A total of 28.7% of patients who initiated dialysis with a concurrent diagnosis of atrial fibrillation were on no anticoagulation or antiplatelet therapy. Baseline patient characteristics by drug exposure are shown in Table 1.
Table 1.
Baseline patient characteristics
| Characteristic | Warfarin Only | Clopidogrel Only | Aspirin Only | ≥2 Drugsa | None | p-valueb |
|---|---|---|---|---|---|---|
| No. of patients | 508 | 43 | 304 | 336 | 480 | |
| Age (yr) | 72.6 (0.4) | 74.1 (1.0) | 72.9 (0.6) | 72.3 (0.5) | 71.3 (0.6) | 0.21 |
| Male gender (%) | 57.8 (2) | 46.5 (8) | 51.6 (3) | 65.5 (3) | 54.4 (2) | 0.02 |
| Race (%) | ||||||
| white | 82.2 (2) | 86.0 (5) | 77.0 (2) | 82.4 (2) | 78.5 (2) | 0.35 |
| black | 12.8 (1) | 7.0 (4) | 17.4 (2) | 11.6 (2) | 15.8 (2) | |
| other | 4.9 (1) | 7.0 (4) | 5.6 (1) | 6.0 (1) | 5.6 (1) | |
| Cause of ESRD (%) | ||||||
| diabetes | 40.6 (1) | 53.5(8) | 43.8 (3) | 50.0 (3) | 34.4 (2) | 0.002 |
| hypertension | 32.9 (2) | 27.9 (7) | 32.2 (3) | 30.1 (3) | 35.8 (2) | |
| glomerulonephritis | 7.3 (1) | 9.3 (4) | 4.9 (1) | 2.7 (1) | 7.3 (1) | |
| other | 19.3 (2) | 9.3 (4) | 19.1 (2) | 17.3 (2) | 22.5 (2) | |
| Pre-HD SBP (mmHg) | 134.9 (1) | 147.4 (4) | 139.7 (1) | 136.2 (1) | 139.7 (1) | <0.0001 |
| Pre-HD DBP (mmHg) | 67.6 (0.5) | 70.0 (2) | 68.7 (0.6) | 67.8 (0.6) | 70.0 (0.5) | 0.006 |
| Heparin (1000 IU per session) | 4.2 (0.1) | 4.4 (0.4) | 4.5 (0.2) | 4.4 (0.2) | 4.6 (0.2) | 0.48 |
| Facility SMR | 0.97 (0.02) | 0.96 (0.06) | 0.98 (0.03) | 0.93 (0.02) | 0.99 (0.02) | 0.49 |
| Access (%) | ||||||
| fistula | 16.5 (2) | 9.3 (4) | 18.1 (2) | 21.7 (2) | 14.6 (2) | 0.28 |
| graft | 18.5 (2) | 20.9 (6) | 13.8 (2) | 15.2 (2) | 15.4 (2) | |
| catheter | 59.3 (2) | 62.8 (7) | 62.8 (3) | 58.3 (3) | 65.2 (2) | |
| unknown | 5.7 (1) | 7.0 (4) | 5.3 (1) | 4.8 (1) | 4.8 (1) | |
| CAD (%) | 41.7 (2) | 62.8 (7) | 49.0 (3) | 53.6 (3) | 32.3 (2) | <0.0001 |
| Myocardial infarction (%) | 12.2 (1) | 18.6 (6) | 17.1 (2) | 22.3 (2) | 11.3 (1) | <0.0001 |
| Stroke (%) | 14.4 (2) | 20.9 (6) | 9.9 (2) | 15.5 (2) | 11.9 (1) | 0.09 |
| Hypertension (%) | 79.7 (2) | 88.4 (5) | 78.9 (2) | 78.3 (2) | 79.8 (2) | 0.65 |
| CHF (%) | 58.3 (2) | 55.8 (8) | 55.3 (3) | 50.9 (3) | 52.9 (2) | 0.26 |
| Charlson comorbidity index | 5.46 (0.1) | 5.88 (0.3) | 5.34 (0.1) | 5.68 (0.1) | 5.35 (0.1) | 0.08 |
| CHADS2 index | 2.75 (0.05) | 3.12 (0.10) | 2.59 (0.06) | 2.74 (0.07) | 2.58 (0.06) | 0.01 |
| Digoxin use (%) | 30.5 (2) | 18.6 (6) | 19.4 (2) | 21.1 (2) | 13.5 (2) | <0.0001 |
Results are displayed as mean (standard error).
CAD, coronary artery disease; CHF, congestive heart failure; DBP, diastolic BP; SBP systolic BP; SMR, standardized mortality ratio.
aPatient on any two of warfarin, clopidogrel, or aspirin.
bFive-way ANOVA among warfarin, clopidogrel, aspirin, two or more drugs, and no drug group.
Primary Analysis for Stroke
The 1671 patients were followed-up for a mean of 1.6 yr (maximum 5 yr). During 2740 patient-years of follow-up, 102 patients developed the primary outcome of new stroke (4.8 events per 100 patient-years; 95% confidence interval [CI] 4.0 to 5.7).
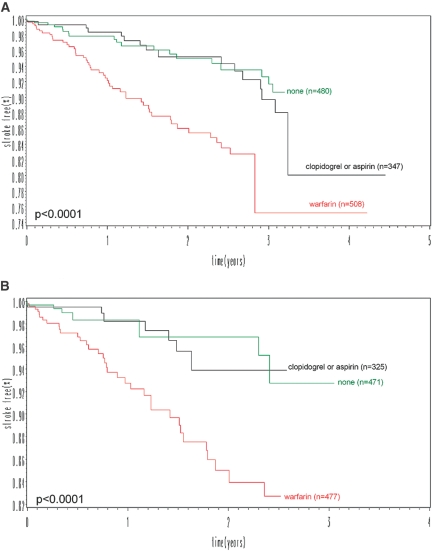
After the initiation of long-term HD, the risk for new stroke significantly differed between exposure groups (log-rank test P < 0.0001; Figure 1A). The new stroke rate was highest in patients who were on warfarin (7.1 per 100 person-years; 95% CI 5.7 to 8.7), followed by patients who were on aspirin (3.5 per 100 person-years; 95% CI 2.5 to 4.7), no drugs (2.9 per 100 person-years; 95% CI 2.0 to 4.4), and clopidogrel (2.7 per 100 person-years; 95% CI 1.5 to 5.2).
Figure 1.
Crude stroke curves by drug exposure. (A) Under an intention-to-treat assumption, increased incidence of new stroke was associated with patients who were on warfarin. (B) Similar results were noted when patients were censored when they changed their warfarin, clopidogrel, or aspirin prescription after study enrollment.
Cox regression analysis indicated warfarin use (versus nonuse) doubled the risk for new stroke (P = 0.001), whereas aspirin use (versus nonuse) or clopidogrel use (versus nonuse) was not statistically significant in influencing the outcome (Table 2). Backward elimination revealed the CHADS2 index as the only covariate to affect significantly the risk for stroke in the Cox model. A one-point increase in CHADS2 score was associated with a 27% increase in the risk for new stroke (P = 0.003), which is similar to its ability to predict stroke in the general population.38 Dosage of heparin used during the dialysis procedure did not increase the risk for new stroke (hazard ratio [HR] 1.01 per 1000 units; P = 0.85). Interaction terms among warfarin, clopidogrel, and aspirin were not found to be significant when included in the Cox model.
Table 2.
HRs for stroke by drug therapy
| Parameter | n | Warfarin (HR [95% CI]) | Clopidogrel (HR [95% CI]) | Aspirin (HR [95% CI]) |
|---|---|---|---|---|
| HR for stroke (intention to treat) | ||||
| unadjusted model | 1671 | 2.00 (1.34 to 2.99) | 0.67 (0.31 to 1.47) | 0.87 (0.57 to 1.33) |
| covariatea adjusted model | 1671 | 1.93 (1.29 to 2.90) | 0.66 (0.30 to 1.46) | 0.86 (0.56 to 1.32) |
| covariatea and propensity score adjusted modelb | 1400 | 1.74 (1.11 to 2.72) | 0.61 (0.25 to 1.50) | 0.98 (0.58 to 1.63) |
| HR for stroke (patients censored on drug status change) | ||||
| unadjusted model | 1671 | 2.94 (1.60 to 5.40) | 0.63 (0.15 to 2.64) | 0.73 (0.37 to 1.41) |
| covariatea adjusted model | 1671 | 2.75 (1.49 to 5.08) | 0.59 (0.14 to 2.49) | 1.20 (0.96 to 1.49) |
| covariatea and propensity score adjusted modelb | 1400 | 1.95 (0.99 to 3.84) | 0.31 (0.04 to 2.45) | 0.70 (0.31 to 1.59) |
aAdjusted for CHADS2 score, gender, race, Charlson comorbidity index, entry date, access, body mass index, facility standardized mortality ratio, cardiovascular drugs, dialysis adequacy, baseline laboratory values (albumin, hemoglobin, creatinine, ferritin, and white blood cell count), heparin dosage (units per treatment), and heparin regimen (bolus versus continuous versus unknown).
bParameters used to calculate the propensity score: CHADS2 score, gender, race, entry date, access, body mass index, facility standardized mortality ratio, cardiovascular drugs, dialysis adequacy, baseline laboratory values (albumin, hemoglobin, creatinine, ferritin, and white blood cell count), heparin dosage (units per treatment), heparin regimen (bolus versus continuous versus unknown), stroke, myocardial infarction, hypertension, peptic ulcer disease, AIDS, peripheral vascular disease, coronary artery disease, dementia, chronic obstructive pulmonary disease, hemiplegia, diabetes, cancer, liver disease, arterial clot, deep vein thrombosis, mechanical heart valve, pulmonary embolism, and hypercoagulable state.
Secondary Stroke Analysis
Implementation of propensity scoring did not significantly alter the findings of the primary analysis. A statistically and clinically significant association between warfarin use (versus nonuse) and increased stroke remained even when the propensity score was added as a covariate to the model (Table 2) or in a propensity-matched subcohort (HR 2.00; 95% CI 1.32 to 3.04 in 746 warfarin users matched to 746 nonusers with a similar propensity score).
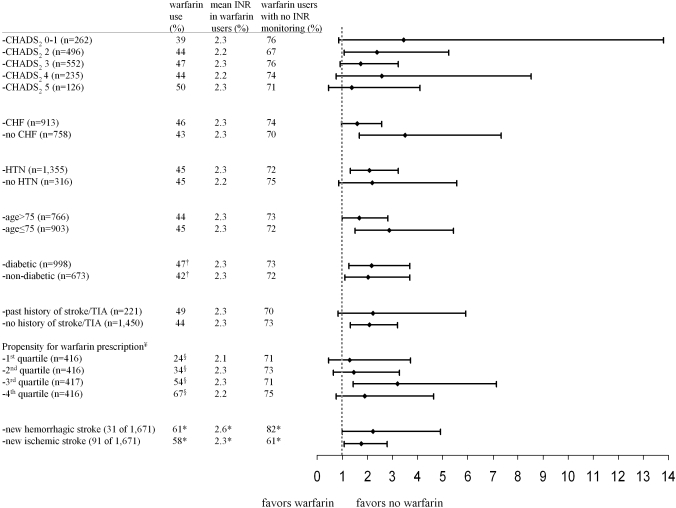
When compared with patients who were not on the drug, warfarin increased the risk for new stroke regardless of whether a patient had congestive heart failure, hypertension, an age >75 yr, previous stroke/transient ischemic attack (TIA), or diabetes. Although warfarin use was also associated with an increased risk for new stroke in all CHADS2 strata, the margin between the risk and benefit decreased with increasing CHADS2 score (Figure 2). Thus, the risk associated with warfarin use was reduced in patients who had atrial fibrillation and were at high risk for future stroke (higher CHADS2 score) relative to those at low risk, which is consistent with treatment guidelines in the general population.39,40 When analyzed separately, the adjusted ischemic stroke HR with warfarin use (versus nonuse) was 1.81 (95% CI 1.12 to 2.92; Figure 2), whereas the risk for hemorrhagic stroke with warfarin use was greater (HR 2.22; 95% CI 1.01 to 4.91; Figure 2); furthermore, 29% of patients who were on warfarin and survived their stroke stopped the drug on discharge from hospital, which suggests a reasonable number of strokes were likely hemorrhagic in nature.
Figure 2.
Stratified analysis. Patients at higher risk for future stroke (higher CHADS2 score) had better risk-benefit profiles (warfarin*CHADS2 = 0.84; P = 0.31 for interaction) with warfarin use when compared with nonusers. With the exception of diabetes, there were no statistical differences in the prevalence of warfarin use, INR level, or INR monitoring with increasing risk for stroke (CHADS2 score) and by five well-established risk factors for future stroke in atrial fibrillation.38 The crude ischemic stroke rate in warfarin users was 5.8 strokes per 100 patient-years (95% CI 4.6 to 7.4) versus 2.3 strokes per 100 patient-years in nonusers (95% CI 1.5 to 3.6). The crude hemorrhagic stroke rate in warfarin users was 1.2 strokes per 100 patient-years (95% CI 0.7 to 2.1) versus 0.5 strokes per 100 patient-years in nonusers (95% CI 0.2 to 1.4).
†Statistically significant difference (P = 0.03) in prevalence of warfarin use in diabetic versus nondiabetic incident dialysis patients with atrial fibrillation.
§As expected, patients with a higher propensity for warfarin prescription had a higher prevalence of warfarin use.
¥After matching, the caliper width of the propensity score between the two groups was found to be ±0.6 SD.
*Values reported only for patients who had a stroke outcome.
CHF, congestive heart failure; HTN, hypertension.
After matching for facility and then adjustment for the CHADS2 and propensity score (c-statistic = 0.73) warfarin prescription trended toward an increased risk for new stroke (HR 1.43; 95% CI 0.75 to 2.71; n = 646). Matching for physician produced similar findings (HR 1.25; 95% CI 0.59 to 2.67; n = 554). These results remained consistent with the primary analysis (n = 1671) but with wider CIs, consistent with a two-thirds reduction in the number of patients used in the 1:1 matched analysis.
Because some patients changed their warfarin, clopidogrel, or aspirin prescription after group assignment, we repeated the primary analysis whereby patients were censored when their prescription status changed. Again, the risk for stroke did not change after censoring (stroke HR for warfarin 2.75; 95% CI 1.49 to 5.08; Figure 1B, Table 2). Alternatively, a time-varying analysis accounted for month-to-month changes in drug prescription during the entire study enrollment period and demonstrated an association between warfarin and new stroke (HR 1.84; 95% CI 1.23 to 2.75). These results did not differ appreciably from the findings in the primary intention-to-treat analysis, in which exposure status was determined in the first 90 d of dialysis.
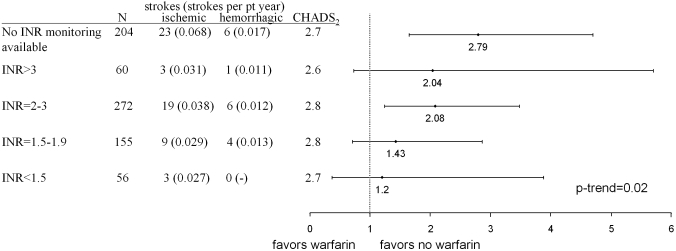
Analysis using the international normalized ratio (INR) suggested a dose-response relationship among the dosage of warfarin, degree of anticoagulation, and risk for new stroke. Increasing baseline INR level in warfarin users (versus nonusers) was positively associated with new stroke (HR 1.35 per unit of INR; 95% CI 0.91 to 2.00; P = 0.02 for trend; Figure 3). The highest risk for stroke was seen in warfarin users who survived beyond 90 d and did not receive INR monitoring in the first 90 d of dialysis (HR 2.79; 95% CI 1.65 to 4.70; reference group was nonusers). The positive relationship between INR and stroke was also preserved longitudinally over time when the INR level was modeled (monthly changing) as a time-dependent running mean of INR (HR 1.78 per unit of INR; P = 0.02) or a time-dependent variable (HR 1.15 per unit of INR; P = 0.39). Increasing warfarin dosage was also temporally and significantly associated with an increase in INR value (R2 = 0.42; P < 0.0001; n = 382). On average, an absolute increase of 0.41 in INR was seen per 1-mg increase in daily warfarin dosage.
Figure 3.
HRs for stroke with warfarin use (versus nonuse) by strata of INR level. The graph demonstrates a dose-response relationship between warfarin and new stroke. Patients with higher levels of anticoagulation, as quantified by the INR level, have an increased risk for new stroke (P = 0.04 for trend) with warfarin use (versus nonuse). Patients who were on warfarin and had no INR monitoring had the highest risk for new stroke. The stroke risk, as quantified by the CHADS2 score, among the five categories of INR were statistically (P = 0.11) and clinically no different.
Survival and Hospitalization Analysis Associated with Stroke
Warfarin use (compared with nonuse) was associated with a significant four-fold increase in death risk from stroke (P = 0.009; Table 3) and an 89% increase in hospitalization for stroke (P = 0.01; Table 4); however, these findings did not translate into statistically significant increases in all-cause mortality and hospitalization with warfarin use (versus nonuse) given that the incidence of stroke was relatively small.
Table 3.
HRs for mortality by warfarin therapy
| Parameter | Warfarin Users(n = 746) |
Warfarin Nonusers(n = 925) |
Warfarin Use (versus Nonuse) | |
|---|---|---|---|---|
| Total Deaths (Deaths per 100 Patient-Years) | n | HR (95% CI) | ||
| HR for mortality | ||||
| unadjusted model | 333 (27.4) | 425 (25.7) | 1671 | 1.03 (0.89 to 1.19) |
| covariate adjusted model | 1671 | 1.10 (0.94 to 1.30) | ||
| covariate and propensity score adjusted model | 1400 | 1.10 (0.93 to 1.30) | ||
| death from stroke | 16 (1.3) | 6 (0.4) | 1400 | 4.31 (1.44 to 12.9) |
| death from cardiovascular disease | 205 (16.9) | 265 (16.5) | 1400 | 1.04 (0.85 to 1.28) |
| death from bleeding | 5 (0.41) | 6 (0.37) | 1400 | 1.24 (0.26 to 5.87) |
| death from infection | 24 (2.0) | 41 (2.6) | 1400 | 0.87 (0.48 to 1.55) |
| other causes of death | 83 (6.8) | 107 (5.8) | 1400 | 1.22 (0.89 to 1.69) |
Table 4.
HRs for hospitalization by warfarin therapy
| Parameter | Warfarin Users(n = 746) |
Warfarin Nonusers(n = 925) |
Warfarin Use (versus Nonuse) | |
|---|---|---|---|---|
| Total Hospitalizations (Hospitalizations per 100 Patient-Years) | n | HR (95% CI) | ||
| HR for hospitalization | ||||
| unadjusted model | 3360 (2.6) | 2818 (2.3) | 1671 | 1.03 (0.92 to 1.14) |
| covariate adjusted model | 1671 | 1.04 (0.92 to 1.16) | ||
| covariate and propensity score adjusted model | 1400 | 1.02 (0.90 to 1.15) | ||
| hospitalization from stroke | 65 (0.06) | 40 (0.03) | 1400 | 1.89 (1.16 to 3.09) |
| hospitalization from cardiovascular disease | 345 (0.32) | 396 (0.27) | 1400 | 1.14 (0.93 to 1.40) |
| hospitalization from bleeding | 97 (0.09) | 107 (0.07) | 1400 | 1.04 (0.73 to 1.46) |
| hospitalization from infection | 468 (0.43) | 577 (0.40) | 1400 | 0.96 (0.80 to 1.16) |
| other causes of hospitalization | 2385 (1.7) | 1698 (1.5) | 1400 | 1.03 (0.91 to 1.17) |
Incidence densities (hospitalizations per 100 patient years) were calculated using all hospitalization visits that occurred during the study enrollment period. HRs were calculated as the time to first hospitalization.
Discussion
In this retrospective cohort study of incident patients with ESRD and coexisting atrial fibrillation, warfarin use was associated with a statistically increased incidence of stroke. The association persisted after controlling for potential confounders, time-dependent changes, and confounding by indication, as well as with matched, stratified, and validation analyses. The finding could have clinical implications because warfarin is used primarily to prevent future stroke in patients with atrial fibrillation, and its use in the ESRD population may instead be associated with increased risk for cerebrovascular accidents.
To date, only three retrospective studies have examined warfarin use for atrial fibrillation in the ESRD population. Stroke rates in warfarin users were statistically no different from rates in nonwarfarin users in a study of patients who had atrial fibrillation and were on dialysis36 (n = 61). Another study found no difference (P = 0.4) in the incidence of stroke when comparing an “undertreated” population (24% prevalence of warfarin use in patients with atrial fibrillation; n = 127) with patients without atrial fibrillation (n = 349) in the same cohort.41 Abbott et al.42 reported a survival advantage in 123 hospitalized dialysis patients who had atrial fibrillation and were on warfarin; however, the results apply to a specific subpopulation of patients who survived hospitalization for atrial fibrillation and were presumed to be on warfarin before admission to hospital.42 Overall, limited hypotheses can be generated from these studies because of methodologic limitations and small sample sizes.
Although the association between stroke and warfarin use that was found in this study may seem to challenge general recommendations for stroke prevention, several clinical studies indirectly support this reassessment of the relative risk-benefit ratio for anticoagulation use in dialysis patients.2 the US Renal Data System reported a 10-fold increase in subdural hemorrhages in dialysis patients (although their medication was not specified) when compared with nondialysis patients,43 whereas a review of 28 studies of warfarin use in dialysis patients suggested its use doubled the risk for major bleeding.44 Treated hypertension,18–20,45,46 cerebrovascular disease,23 ischemic stroke,21,47 serious heart disease,23 renal insufficiency,23,48–50 and advanced age25,49,51–53 have been reported to potentiate bleeding during warfarin therapy and are highly prevalent in the dialysis population. Our study also suggests that warfarin users with no in-facility INR monitoring had the greatest risk for stroke, and hemorrhagic complications may be minimized with frequent monitoring and tight management of a patient's anticoagulation status.
An important factor that may play a role in this risk-benefit profile is that the intrinsic platelet dysfunction of ESRD may reduce the risk for stroke in dialysis patients with atrial fibrillation, which could also explain why the untreated stroke rate in the study population (2.9 events per 100 patient-years) is lower than a similar untreated cohort of patients without kidney disease (4.4 events per 100 patient-years).38 In addition to a hemorrhagic mechanism for stroke, warfarin may potentiate vascular calcification to increase the risk for ischemic stroke,54 which was also reported in warfarin users in our study cohort.
This study cohort was derived from all patients receiving chronic renal replacement therapy with a large, national dialysis provider. Inclusion of patients from a large number of clinics likely minimized bias.55 Despite this, we acknowledge several limitations of this study, which include the following:
Misclassification bias: The diagnosis of stroke and atrial fibrillation abstracted from medical records may not have been accurate, because confirmatory tests such as neuroimaging and electrocardiograms were not consistently documented in the medical records abstracted for the definitive confirmation of these conditions.
Confounding by indication: The increase in strokes among warfarin users may have been because patients who were anticoagulated and had higher INR levels may have had an inherently higher baseline stroke risk that was not fully adjusted for by covariates such as the CHADS2 score.
Survivorship bias: Patients who had pre-ESRD and were at increased risk for mortality were less likely prescribed warfarin and preferentially left censored before the initiation of dialysis (i.e., early death in nonusers prevented the patient's enrollment in the analysis).
Ascertainment bias: The outcome of stroke was not adjudicated under a research protocol, such that the charting of “stroke” may have been preferentially favored in high-risk patients who were more likely to be on warfarin.
Selection bias from missing data: Patients with atrial fibrillation and concurrent anticoagulation or antiplatelet therapy may have been on warfarin for a separate indication (i.e., the medical records did not chart whether warfarin was specifically given for secondary stroke prevention). Some patients on warfarin may have had their INR monitoring in “anticoagulation clinics” external to the dialysis facility and the data not inputted into our database. Furthermore, INR was rarely drawn on the day of the stroke; therefore, we could not measure a patient's coagulation status at the time of the event. Time-varying Cox regression models used the most recent INR level, which could be different at the time of the event (INR was drawn on average 44 d before the admission for stroke).
In summary, this large retrospective study found a significant association between warfarin use and the incidence of stroke in patients with ESRD and coexisting atrial fibrillation. This finding, in addition to the results of the previous study that also found an increased risk for mortality with anticoagulation use in patients with ESRD in general,12 raises concerns about the use of these drugs in dialysis patients; however, before definitive conclusions can be drawn, large, prospective, randomized, controlled trials are required. Until then, physicians should be cognizant of the possible risks associated with warfarin use for atrial fibrillation in patients with ESRD, with careful evaluation of the risks and benefits of intervention at the individual patient level. Close monitoring of the degree of anticoagulation (INR) in patients who are on warfarin would also be a reasonable recommendation to minimize the risk for hemorrhagic complications.
Concise Methods
Population
All incident long-term HD patients who had preexisting atrial fibrillation documented in the electronic medical record were identified from >1300 Fresenius Medical Care North America dialysis clinics for the analysis. Incident patients were those who were admitted to an outpatient clinic from January 1, 2003, through December 31, 2004, and started long-term HD for the first time within the preceding 30 d. We excluded patients with <90 d of study enrollment. Patient outcomes were followed from the date of dialysis initiation up to December 31, 2007.
Data Collection
Computerized medical records are a reliable source of clinical data that have been validated against electrocardiograms to accurately identify patients with atrial fibrillation.56–60 The diagnostic accuracy of atrial fibrillation documented in the Fresenius electronic medical record was recently found to be 75% when compared against electrocardiograms obtained for the same patients; furthermore, the reasonable charting of atrial fibrillation can be implied from statistically significant higher levels (P < 0.0001 for each variable) of age, Charlson scores, coronary artery disease, myocardial infarctions, previous stroke, hypertension, warfarin use, digoxin use, β blocker use, amiodarone use, and INR level in the study cohort when compared with incident patients without coexisting atrial fibrillation. The documentation of atrial fibrillation was also examined in a cohort of 22,010 incident dialysis patients drawn from the same 1300 Fresenius clinics where this study was conducted; however, the time frame was from 2005 to 2008, when nurses began documenting heart rhythms of patients in the electronic medical record. A significantly higher prevalence of irregular heart rhythms were found in patients with atrial fibrillation when compared with patients who did not have atrial fibrillation (odds ratio 3.25; P < 0.0001; sensitivity 8%; specificity 97%).
Outcome, exposure, and baseline covariate measurements used for the study were prospectively entered by clinical staff into the Fresenius clinical data system, which is an electronic health record that integrates physician orders, charting, and results from all clinics with ancillary, billing, and clinical support services. The system actively tracks patient events and comorbidity, which is obtained from hospital discharge summaries or physician notes to prevent inaccurate diagnoses. The diagnostic accuracy of TIAs, stroke, and subtypes of stroke (ischemic versus hemorrhagic) obtained through clinical notes, discharge summaries, and mortality reports has been supported by multiple publications that have cross-validated these diagnoses with medical records, laboratory testing, and radiologic imaging.59,61–63 Further details about the clinical data system with respect to the validation of data quality, the extraction of oral medication information, and its ability to facilitate the anonymous analysis of health care information are outlined in our previous publication.12
Outcomes, Exposures, and Baseline Covariates
The primary outcome for the study was death or hospitalization from new stroke. Patients who were hospitalized for stroke were identified from the diagnoses obtained from hospital discharge summaries, whereas cause of death was determined by the patient's primary nephrologist and noted in the medical records. TIAs were also considered part of the primary outcome given the management of stroke prevention is the same regardless of the diagnosis. Study patients who achieved the primary outcome of stroke were older (P = 0.008) with higher CHADS2 scores (P = 0.01), frequency of INR monitoring (P < 0.0001), systolic BP (P = 0.04), warfarin use (P = 0.0007), and prevalence of congestive heart failure (P = 0.02) than patients who were censored, supporting the valid classification of patients with stroke in the clinical data system; furthermore, previous studies validate the diagnostic accuracy of stroke abstracted from medical records.59,61–63
Drug exposure status was determined by any use of warfarin (versus nonuse), clopidogrel (versus nonuse), or aspirin (versus nonuse) in the first 90 d of dialysis. Subsequent analysis confirms the accurate classification of warfarin prescription in the electronic medical records and patient compliance to the drug. Patients receiving warfarin had higher INR levels (2.3 versus 1.9; P = 0.0003) and more INR lab draws (1.9 per 90 d versus 0.2 per 90 d; P < 0.0001), and a higher proportions of patients received INR monitoring (72.7 versus only 11.6% in nonusers; P < 0.0001). A total of 68.3% of warfarin users (versus 7.8% in nonusers; P < 0.0001) had at least one elevated INR reading of ≥1.5 in the first 90 d of dialysis.
Baseline patient characteristics were measured during the first 90 d of study enrollment. Measured covariates included race (white, black, or other), active dialysis access used on the 90th day after the start of HD (graft, fistula, catheter, or unknown), gender, Charlson comorbidity index, CHADS2 index (baseline stroke risk that incorporates congestive heart failure, hypertension, age, diabetes, and history of stroke or TIA), dialysis adequacy (Kt/V, which included residual renal function), cardiovascular drug use, body mass index, baseline laboratory values (hemoglobin, albumin, creatinine, white blood cell count, and ferritin), propensity score, heparin dosage (units of heparin administered per dialysis session and did not include units used for catheter locking), heparin regimen used on the 90th day after the start of HD (bolus, continuous, or unknown), study entry date (days after January 1, 2003), and standardized mortality ratio (facility-specific standardized mortality ratio on January 1, 2003). Many of the covariates were chosen because of their reported association with stroke in the general64 and ESRD65 populations. The INR assay used by our central laboratory (Spectra Laboratory, Rockleigh, NJ) incorporated heparin adsorbent to remove heparin from the plasma of blood samples before INR testing (Inotech Biosystems International, Rockville, MD).
To adjust for differences in baseline ischemic stroke risk in patients, we used the CHADS2 scheme, a prognostic scoring algorithm developed from the amalgamation of several randomized trials of atrial fibrillation and stroke in the general population.38,66 CHADS2 is an acronym for the stroke risk factors and their scoring: 1 point for each of congestive heart failure, hypertension (as charted in the comorbidity list or those with an average systolic BP >160 mmHg in the first 90 d of dialysis), age ≥75 yr, or diabetes and 2 points for a history of previous stroke or TIA. Nondialysis patients with a cumulative score of >2 are at high enough risk for future stroke to justify the risks of warfarin prescription.67 We generated individual patient CHADS2 scores from comorbidity lists in the electronic medical records. The CHADS2 index was also validated in our study population to demonstrate that it can also be applied in our dialysis population to predict accurately future stroke when patients are on no anticoagulation or antiplatelet therapy68 (c-statistic 0.71; 95% CI 0.61 to 0.81).
Baseline comorbidities were also used to determine the Charlson score for each patient. The index scores comorbidity through the presence or absence of 19 possible chronic conditions in an individual patient recorded in the first 90 d of dialysis. The index has been validated as a predictor of mortality in the dialysis population69–71 and can be accurately derived with patient information abstracted from medical records or International Classification of Diseases, Ninth Revision coding72–77
Primary Statistical Analysis for Stroke
The primary analysis estimated the risk for new stroke (>90 d after the start of dialysis) associated with the baseline use of warfarin, clopidogrel, and/or aspirin. The new stroke rate for the study cohort and by exposure group (none, warfarin only, aspirin or clopidogrel, two or more drugs) was calculated using Poisson regression. Crude stroke survival by exposure group was determined using Kaplan-Meier analysis with a log-rank test. Cox regression analysis using backward variable selection with variable exit criteria set at P < 0.10 was used to adjust progressively for baseline covariates (Table 2). Drug exposure was modeled as three distinct categorical variables (warfarin use, clopidogrel use, and aspirin use) in the Cox model. Interaction effects were tested in separate models through the inclusion of cross-product terms between warfarin, clopidogrel, and aspirin.
Secondary Analysis for stroke
To validate the findings of our primary analysis, we performed the following five sensitivity analyses. We incorporated a propensity score as a covariate into the Cox regression model to balance selection and residual confounding effects between our exposure groups. To do this, we used multinomial logistic regression78,79 to model the probability of six different outcomes that represented all combinations of warfarin, clopidogrel, and/or aspirin that a patient could receive (none as the reference group, clopidogrel only, aspirin only, warfarin only or in combination with clopidogrel and aspirin, and warfarin with clopidogrel and/or aspirin) as a function of the laboratory and demographic variables used in the primary analysis and 19 comorbid diagnoses (stroke, myocardial infarction, hypertension, peptic ulcer disease, AIDS, peripheral vascular disease, coronary artery disease, dementia, chronic obstructive pulmonary disease, hemiplegia, diabetes, cancer, liver disease, arterial clot, deep vein thrombosis, mechanical heart valve, pulmonary embolism, and hypercoagulable state). We also determined the stroke HR stratified by quartiles of propensity score and in a subcohort of patients in which each warfarin user was matched to a nonuser by propensity for warfarin prescription (see Appendix 1 for patient characteristics of warfarin users versus nonusers after matching on propensity score).
We determined whether the effectiveness of warfarin for new stroke prevention improved in higher risk patients as seen in the general population. To do this, we performed a Cox regression analysis stratified by CHADS2 score to determine the relative benefit of warfarin in preventing stroke as a function of increasing strata of stroke risk (CHADS2 score) and by the individual components of the score itself (congestive heart failure, hypertension, age >75 yr, diabetes, and history of stroke or TIA). Risk by subtype of stroke (hemorrhagic and ischemic) was also evaluated separately using covariate adjusted Cox survival models.
To account for the possibility of residual and nonlinear confounding from the treating facility and physician that was not fully accounted for with standardized mortality ratios, we performed a series of 1:1 matched analysis using a “greedy nearest available” matching algorithm.80,81 For example, we performed a sensitivity analysis to determine the risk for new stroke associated with warfarin use versus nonuse using Cox regression, after matching to ensure patients in the two groups were from the same facility or attending physician, with adjustment for CHADS2 and propensity score.
The primary analysis was intention-to-treat whereby patients who started on any of these drugs after the first 90 d of dialysis were not reclassified. To account for the possibility of longitudinal changes in drug prescription over time, we performed two additional validation analyses: (1) A repeat of the primary Cox model whereby patients were censored when their warfarin, clopidogrel, or aspirin exposure changed and (2) a time-varying Cox model whereby warfarin, clopidogrel, and aspirin exposure variables were updated every month in the model.
Last, we examined whether a dose-response relationship existed between new stoke and warfarin. Patients were grouped into one of six categories: Nonwarfarin users were the reference category, whereas patients who were on warfarin had their reported INR categorized as <1.5, 1.5 to 1.9, 2.0 to 3.0, >3.0, or no monitoring on the basis of their average INR level during the first 90 d of dialysis. Cox models with adjustment for the CHADS2 index were used to examine the relative change in HR for new stroke in warfarin users (versus nonusers) by increasing ordinals of INR. P value for INR trend was calculated using the median value for each INR ordinal. Because baseline INR values do not account for longitudinal fluctuations in INR for the duration of the study, we also modeled INR as a time-varying variable during successive 1-mo intervals and as a running mean during previous time intervals in our Cox model.
Analysis for Mortality and Hospitalization
We used unadjusted and adjusted Cox models to determine the association of warfarin use (versus nonuse) with survival and hospitalization. Covariates entered into the models included age, race, gender, Charlson comorbidity index, CHADS2 index, entry date, dialysis access, dialysis adequacy, cardiovascular drug use, body mass index, baseline laboratory values (hemoglobin, albumin, creatinine, bicarbonate, white blood cell count, ferritin, parathyroid hormone, calcium, and phosphorus), dialysate calcium, propensity score, heparin dosage, heparin regimen, and the facility standardized mortality ratio. All statistical analysis was done using SAS 9.1 (SAS Institute, Cary, NC).
Disclosures
None.
Acknowledgments
We thank Dr. Norma Ofsthun and Dr. Eduardo Lacson for help in the data analysis and manuscript preparation. We also express appreciation to the staff in more than 1300 Fresenius dialysis clinics, who continually make great efforts to ensure the accurate charting of clinical data in the computer system.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Warfarin and Stroke Outcomes in Hemodialysis Patients with Atrial Fibrillation,” on pages 2090–2092.
REFERENCES
- 1.US Renal Data System: Cardiovascular Special Studies, Bethesda, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2005 [Google Scholar]
- 2.Reinecke H, Brand E, Mesters R, Schabitz WR, Fisher M, Pavenstadt H, Breithardt G: Dilemmas in the management of atrial fibrillation in chronic kidney disease. J Am Soc Nephrol 20: 705–711, 2009 [DOI] [PubMed] [Google Scholar]
- 3.Miller LM, Hopman WM, Garland JS, Yeates KE, Pilkey RM: Cardioprotective medication use in hemodialysis patients. Can J Cardiol 22: 755–760, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fuster V, Ryden LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Le Heuzey JY, Kay GN, Lowe JE, Olsson SB, Prystowsky EN, Tamargo JL, Wann S, Smith SC, Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Halperin JL, Hunt SA, Nishimura R, Ornato JP, Page RL, Riegel B, Priori SG, Blanc JJ, Budaj A, Camm AJ, Dean V, Deckers JW, Despres C, Dickstein K, Lekakis J, McGregor K, Metra M, Morais J, Osterspey A, Tamargo JL, Zamorano JL: ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation). Developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation 114: e257–e354, 2006 [DOI] [PubMed] [Google Scholar]
- 5.Singer DE, Albers GW, Dalen JE, Go AS, Halperin JL, Manning WJ: Antithrombotic therapy in atrial fibrillation: The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 126: 429S–456S, 2004 [DOI] [PubMed] [Google Scholar]
- 6.Connolly SJ, Laupacis A, Gent M, Roberts RS, Cairns JA, Joyner C: Canadian Atrial Fibrillation Anticoagulation (CAFA) Study. J Am Coll Cardiol 18: 349–355, 1991 [DOI] [PubMed] [Google Scholar]
- 7.Stroke Prevention in Atrial Fibrillation Study: Final results. Circulation 84: 527–539, 1991 [DOI] [PubMed] [Google Scholar]
- 8.Petersen P, Boysen G, Godtfredsen J, Andersen ED, Andersen B: Placebo-controlled, randomised trial of warfarin and aspirin for prevention of thromboembolic complications in chronic atrial fibrillation. The Copenhagen AFASAK study. Lancet 1: 175–179, 1989 [DOI] [PubMed] [Google Scholar]
- 9.The effect of low-dose warfarin on the risk of stroke in patients with nonrheumatic atrial fibrillation. The Boston Area Anticoagulation Trial for Atrial Fibrillation Investigators. N Engl J Med 323: 1505–1511, 1990 [DOI] [PubMed] [Google Scholar]
- 10.Ezekowitz MD, Bridgers SL, James KE, Carliner NH, Colling CL, Gornick CC, Krause-Steinrauf H, Kurtzke JF, Nazarian SM, Radford MJ: Warfarin in the prevention of stroke associated with nonrheumatic atrial fibrillation. Veterans Affairs Stroke Prevention in Nonrheumatic Atrial Fibrillation Investigators. N Engl J Med 327: 1406–1412, 1992 [DOI] [PubMed] [Google Scholar]
- 11.Connolly S, Pogue J, Hart R, Pfeffer M, Hohnloser S, Chrolavicius S, Pfeffer M, Hohnloser S, Yusuf S: Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): A randomised controlled trial. Lancet 367: 1903–1912, 2006 [DOI] [PubMed] [Google Scholar]
- 12.Chan KE, Lazarus JM, Thadhani R, Hakim RM: Anticoagulant and antiplatelet usage associates with mortality among hemodialysis patients. J Am Soc Nephrol 20: 872–881, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kopecky SL, Gersh BJ, McGoon MD, Chu CP, Ilstrup DM, Chesebro JH, Whisnant JP: Lone atrial fibrillation in elderly persons: A marker for cardiovascular risk. Arch Intern Med 159: 1118–1122, 1999 [DOI] [PubMed] [Google Scholar]
- 14.Patients with nonvalvular atrial fibrillation at low risk of stroke during treatment with aspirin: Stroke Prevention in Atrial Fibrillation III Study. The SPAF III: Writing Committee for the Stroke Prevention in Atrial Fibrillation Investigators. JAMA 279: 1273–1277, 1998 [PubMed] [Google Scholar]
- 15.Predictors of thromboembolism in atrial fibrillation: I. Clinical features of patients at risk. The Stroke Prevention in Atrial Fibrillation Investigators. Ann Intern Med 116: 1–5, 1992 [DOI] [PubMed] [Google Scholar]
- 16.van Latum JC, Koudstaal PJ, Venables GS, van Gijn J, Kappelle LJ, Algra A: Predictors of major vascular events in patients with a transient ischemic attack or minor ischemic stroke and with nonrheumatic atrial fibrillation. European Atrial Fibrillation Trial (EAFT) Study Group. Stroke 26: 801–806, 1995 [DOI] [PubMed] [Google Scholar]
- 17.Warfarin versus aspirin for prevention of thromboembolism in atrial fibrillation: Stroke Prevention in Atrial Fibrillation II Study. Lancet 343: 687–691, 1994 [PubMed] [Google Scholar]
- 18.Launbjerg J, Egeblad H, Heaf J, Nielsen NH, Fugleholm AM, Ladefoged K: Bleeding complications to oral anticoagulant therapy: Multivariate analysis of 1010 treatment years in 551 outpatients. J Intern Med 229: 351–355, 1991 [DOI] [PubMed] [Google Scholar]
- 19.Petitti DB, Strom BL, Melmon KL: Duration of warfarin anticoagulant therapy and the probabilities of recurrent thromboembolism and hemorrhage. Am J Med 81: 255–259, 1986 [DOI] [PubMed] [Google Scholar]
- 20.Landefeld CS, Goldman L: Major bleeding in outpatients treated with warfarin: Incidence and prediction by factors known at the start of outpatient therapy. Am J Med 87: 144–152, 1989 [DOI] [PubMed] [Google Scholar]
- 21.Optimal oral anticoagulant therapy in patients with nonrheumatic atrial fibrillation and recent cerebral ischemia. The European Atrial Fibrillation Trial Study Group. N Engl J Med 333: 5–10, 1995 [DOI] [PubMed] [Google Scholar]
- 22.Cannegieter SC, Rosendaal FR, Wintzen AR, van der Meer FJ, Vandenbroucke JP, Briet E: Optimal oral anticoagulant therapy in patients with mechanical heart valves. N Engl J Med 333: 11–17, 1995 [DOI] [PubMed] [Google Scholar]
- 23.Bleeding during antithrombotic therapy in patients with atrial fibrillation. The Stroke Prevention in Atrial Fibrillation Investigators. Arch Intern Med 156: 409–416, 1996 [PubMed] [Google Scholar]
- 24.Beyth RJ, Landefeld CS: Anticoagulants in older patients: A safety perspective. Drugs Aging 6: 45–54, 1995 [DOI] [PubMed] [Google Scholar]
- 25.Rosand J, Eckman MH, Knudsen KA, Singer DE, Greenberg SM: The effect of warfarin and intensity of anticoagulation on outcome of intracerebral hemorrhage. Arch Intern Med 164: 880–884, 2004 [DOI] [PubMed] [Google Scholar]
- 26.Hylek EM, Singer DE: Risk factors for intracranial hemorrhage in outpatients taking warfarin. Ann Intern Med 120: 897–902, 1994 [DOI] [PubMed] [Google Scholar]
- 27.Miskulin DC, Athienites NV, Yan G, Martin AA, Ornt DB, Kusek JW, Meyer KB, Levey AS: Comorbidity assessment using the Index of Coexistent Diseases in a multicenter clinical trial. Kidney Int 60: 1498–1510, 2001 [DOI] [PubMed] [Google Scholar]
- 28.Patient characteristics at the start of ESRD: Data from the HCFA medical evidence form. Am J Kidney Dis 34: S63–S73, 1999 [DOI] [PubMed] [Google Scholar]
- 29.Mailloux LU, Napolitano B, Bellucci AG, Mossey RT, Vernace MA, Wilkes BM: The impact of co-morbid risk factors at the start of dialysis upon the survival of ESRD patients. ASAIO J 42: 164–169, 1996 [PubMed] [Google Scholar]
- 30.Keane WF, Collins AJ: Influence of co-morbidity on mortality and morbidity in patients treated with hemodialysis. Am J Kidney Dis 24: 1010–1018, 1994 [DOI] [PubMed] [Google Scholar]
- 31.Comorbid conditions and correlations with mortality risk among 3,399 incident hemodialysis patients. Am J Kidney Dis 20: 32–38, 1992 [PubMed] [Google Scholar]
- 32.McClellan W, Soucie JM: Facility mortality rates for new end-stage renal disease patients: Implications for quality improvement. Am J Kidney Dis 24: 280–289, 1994 [DOI] [PubMed] [Google Scholar]
- 33.Manley HJ, Garvin CG, Drayer DK, Reid GM, Bender WL, Neufeld TK, Hebbar S, Muther RS: Medication prescribing patterns in ambulatory haemodialysis patients: Comparisons of USRDS to a large not-for-profit dialysis provider. Nephrol Dial Transplant 19: 1842–1848, 2004 [DOI] [PubMed] [Google Scholar]
- 34.Sreedhara R, Itagaki I, Lynn B, Hakim RM: Defective platelet aggregation in uremia is transiently worsened by hemodialysis. Am J Kidney Dis 25: 555–563, 1995 [DOI] [PubMed] [Google Scholar]
- 35.Janssen MJ, van der Meulen J: The bleeding risk in chronic haemodialysis: Preventive strategies in high-risk patients. Neth J Med 48: 198–207, 1996 [DOI] [PubMed] [Google Scholar]
- 36.Wiesholzer M, Harm F, Tomasec G, Barbieri G, Putz D, Balcke P: Incidence of stroke among chronic hemodialysis patients with nonrheumatic atrial fibrillation. Am J Nephrol 21: 35–39, 2001 [DOI] [PubMed] [Google Scholar]
- 37.Lo DS, Rabbat CG, Clase CM: Thromboembolism and anticoagulant management in hemodialysis patients: A practical guide to clinical management. Thromb Res 118: 385–395, 2006 [DOI] [PubMed] [Google Scholar]
- 38.Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ: Validation of clinical classification schemes for predicting stroke: Results from the National Registry of Atrial Fibrillation. JAMA 285: 2864–2870, 2001 [DOI] [PubMed] [Google Scholar]
- 39.Laupacis A, Albers G, Dalen J, Dunn MI, Jacobson AK, Singer DE: Antithrombotic therapy in atrial fibrillation. Chest 114: 579S–589S, 1998 [DOI] [PubMed] [Google Scholar]
- 40.Gage BF, Cardinalli AB, Albers GW, Owens DK: Cost-effectiveness of warfarin and aspirin for prophylaxis of stroke in patients with nonvalvular atrial fibrillation. JAMA 274: 1839–1845, 1995 [PubMed] [Google Scholar]
- 41.Genovesi S, Vincenti A, Rossi E, Pogliani D, Acquistapace I, Stella A, Valsecchi MG: Atrial fibrillation and morbidity and mortality in a cohort of long-term hemodialysis patients. Am J Kidney Dis 51: 255–262, 2008 [DOI] [PubMed] [Google Scholar]
- 42.Abbott KC, Trespalacios FC, Taylor AJ, Agodoa LY: Atrial fibrillation in chronic dialysis patients in the United States: Risk factors for hospitalization and mortality. BMC Nephrol 4: 1, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sood P, Sinson GP, Cohen EP: Subdural hematomas in chronic dialysis patients: Significant and increasing. Clin J Am Soc Nephrol 2: 956–959, 2007 [DOI] [PubMed] [Google Scholar]
- 44.Elliott MJ, Zimmerman D, Holden RM: Warfarin anticoagulation in hemodialysis patients: A systematic review of bleeding rates. Am J Kidney Dis 50:433–440, 2007 [DOI] [PubMed] [Google Scholar]
- 45.Pollard JW, Hamilton MJ, Christensen NA, Achor RW: Problems associated with long-term anticoagulant therapy: Observations in 139 cases. Circulation 25: 311–317, 1962 [DOI] [PubMed] [Google Scholar]
- 46.Lundstrom T, Ryden L: Haemorrhagic and thromboembolic complications in patients with atrial fibrillation on anticoagulant prophylaxis. J Intern Med 225: 137–142, 1989 [DOI] [PubMed] [Google Scholar]
- 47.Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. EAFT (European Atrial Fibrillation Trial) Study Group. Lancet 342: 1255–1262, 1993 [PubMed] [Google Scholar]
- 48.Fihn SD, McDonell M, Martin D, Henikoff J, Vermes D, Kent D, White RH: Risk factors for complications of chronic anticoagulation: A multicenter study. Warfarin Optimized Outpatient Follow-up Study Group. Ann Intern Med 118: 511–520, 1993 [DOI] [PubMed] [Google Scholar]
- 49.Beyth RJ, Quinn LM, Landefeld CS: Prospective evaluation of an index for predicting the risk of major bleeding in outpatients treated with warfarin. Am J Med 105: 91–99, 1998 [DOI] [PubMed] [Google Scholar]
- 50.McMahan DA, Smith DM, Carey MA, Zhou XH: Risk of major hemorrhage for outpatients treated with warfarin. J Gen Intern Med 13: 311–316, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Torn M, Bollen WL, van der Meer FJ, van der Wall EE, Rosendaal FR: Risks of oral anticoagulant therapy with increasing age. Arch Intern Med 165: 1527–1532, 2005 [DOI] [PubMed] [Google Scholar]
- 52.Copland M, Walker ID, Tait RC: Oral anticoagulation and hemorrhagic complications in an elderly population with atrial fibrillation. Arch Intern Med 161: 2125–2128, 2001 [DOI] [PubMed] [Google Scholar]
- 53.Kuijer PM, Hutten BA, Prins MH, Buller HR: Prediction of the risk of bleeding during anticoagulant treatment for venous thromboembolism. Arch Intern Med 159: 457–460, 1999 [DOI] [PubMed] [Google Scholar]
- 54.Wang Y, Zhang W, Zhang Y, Yang Y, Sun L, Hu S, Chen J, Zhang C, Zheng Y, Zhen Y, Sun K, Fu C, Yang T, Wang J, Sun J, Wu H, Glasgow WC, Hui R: VKORC1 haplotypes are associated with arterial vascular diseases (stroke, coronary heart disease, and aortic dissection). Circulation 113: 1615–1621, 2006 [DOI] [PubMed] [Google Scholar]
- 55.Concato J, Shah N, Horwitz RI: Randomized, controlled trials, observational studies, and the hierarchy of research designs. N Engl J Med 342: 1887–1892, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Brophy MT, Snyder KE, Gaehde S, Ives C, Gagnon D, Fiore LD: Anticoagulant use for atrial fibrillation in the elderly. J Am Geriatr Soc 52: 1151–1156, 2004 [DOI] [PubMed] [Google Scholar]
- 57.Frost L, Andersen LV, Vestergaard P, Husted S, Mortensen LS: Trend in mortality after stroke with atrial fibrillation. Am J Med 120: 47–53, 2007 [DOI] [PubMed] [Google Scholar]
- 58.Frost L, Vukelic AL, Vestergaard P, Husted S, Mortensen LS: Trends in risk of stroke in patients with a hospital diagnosis of nonvalvular atrial fibrillation: National Cohort Study in Denmark, 1980–2002. Neuroepidemiology 26: 212–219, 2006 [DOI] [PubMed] [Google Scholar]
- 59.Kokotailo RA, Hill MD: Coding of stroke and stroke risk factors using International Classification of Diseases, Revisions 9 and 10. Stroke 36: 1776–1781, 2005 [DOI] [PubMed] [Google Scholar]
- 60.Ruigomez A, Johansson S, Wallander MA, Rodriguez LA: Incidence of chronic atrial fibrillation in general practice and its treatment pattern. J Clin Epidemiol 55: 358–363, 2002 [DOI] [PubMed] [Google Scholar]
- 61.Spolaore P, Brocco S, Fedeli U, Visentin C, Schievano E, Avossa F, Milan G, Toso V, Vanuzzo D, Pilotto L, Pessina AC, Bonita R: Measuring accuracy of discharge diagnoses for a region-wide surveillance of hospitalized strokes. Stroke 36: 1031–1034, 2005 [DOI] [PubMed] [Google Scholar]
- 62.Rosamond WD, Folsom AR, Chambless LE, Wang CH, McGovern PG, Howard G, Copper LS, Shahar E: Stroke incidence and survival among middle-aged adults: 9-Year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke 30: 736–743, 1999 [DOI] [PubMed] [Google Scholar]
- 63.Jick H, Jick SS, Derby LE: Validation of information recorded on general practitioner based computerised data resource in the United Kingdom. BMJ 302: 766–768, 1991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Goldstein LB, Adams R, Alberts MJ, Appel LJ, Brass LM, Bushnell CD, Culebras A, DeGraba TJ, Gorelick PB, Guyton JR, Hart RG, Howard G, Kelly-Hayes M, Nixon JV, Sacco RL: Primary prevention of ischemic stroke: A guideline from the American Heart Association/American Stroke Association Stroke Council. Cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation 113: e873–e923, 2006 [DOI] [PubMed] [Google Scholar]
- 65.Seliger SL, Gillen DL, Tirschwell D, Wasse H, Kestenbaum BR, Stehman-Breen CO: Risk factors for incident stroke among patients with end-stage renal disease. J Am Soc Nephrol 14: 2623–2631, 2003 [DOI] [PubMed] [Google Scholar]
- 66.Gage BF, van WC, Pearce L, Hart RG, Koudstaal PJ, Boode BS, Petersen P: Selecting patients with atrial fibrillation for anticoagulation: Stroke risk stratification in patients taking aspirin. Circulation 110: 2287–2292, 2004 [DOI] [PubMed] [Google Scholar]
- 67.Lip GY, Boos CJ: Antithrombotic treatment in atrial fibrillation. Postgrad Med J 84: 252–258, 2008 [DOI] [PubMed] [Google Scholar]
- 68.Chambless LE: Estimation of time-dependent area under the ROC curve for long-term risk prediction. Stat Med 25: 3474–3486, 2006 [DOI] [PubMed] [Google Scholar]
- 69.Miskulin DC, Martin AA, Brown R, Fink NE, Coresh J, Powe NR, Zager PG, Meyer KB, Levey AS: Predicting 1 year mortality in an outpatient haemodialysis population: A comparison of comorbidity instruments. Nephrol Dial Transplant 19: 413–420, 2004 [DOI] [PubMed] [Google Scholar]
- 70.van Manen JG, Korevaar JC, Dekker FW, Boeschoten EW, Bossuyt PM, Krediet RT: How to adjust for comorbidity in survival studies inESRD patients: A comparison of different indices. Am J Kidney Dis 40: 82–89, 2002 [DOI] [PubMed] [Google Scholar]
- 71.Charlson ME, Pompei P, Ales KL, MacKenzie CR: A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 40: 373–383, 1987 [DOI] [PubMed] [Google Scholar]
- 72.Robinson JR, Young TK, Roos LL, Gelskey DE: Estimating the burden of disease: Comparing administrative data and self-reports. Med Care 35: 932–947, 1997 [DOI] [PubMed] [Google Scholar]
- 73.Luthi JC, Troillet N, Eisenring MC, Sax H, Burnand B, Quan H, Ghali W: Administrative data outperformed single-day chart review for comorbidity measure. Int J Qual Health Care 19: 225–231, 2007 [DOI] [PubMed] [Google Scholar]
- 74.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA: Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43: 1130–1139, 2005 [DOI] [PubMed] [Google Scholar]
- 75.Quan H, Parsons GA, Ghali WA: Validity of information on comorbidity derived rom ICD-9-CCM administrative data. Med Care 40: 675–685, 2002 [DOI] [PubMed] [Google Scholar]
- 76.Chaudhry S, Jin L, Meltzer D: Use of a self-report-generated Charlson Comorbidity Index for predicting mortality. Med Care 43: 607–615, 2005 [DOI] [PubMed] [Google Scholar]
- 77.Department of Health and Human Services: The International Classification of Diseases, 9th Rev., Clinical Modification: ICD-9-CM, Washington, DC, Government Printing Office, 1980. DHHS Publication No. (PHS) 80-1260 [Google Scholar]
- 78.Rosenbaum P, Rubin D: The central role of the propensity score in observational studies for causal effect. Biometrika 70: 41–55, 1983 [Google Scholar]
- 79.Imbens G: The role of propensity score in estimating dose-response in observational studies for causal effect. Biometrika 3: 706–710, 2000 [Google Scholar]
- 80.Kosanke J BE: Gmatch: SAS macro. Available at: http://mayoresearch.mayo.edu/biostat/upload/gmatch.sas Accessed December 12, 2008
- 81.Rubin D: Matching to remove bias in observational studies. Biometrics 29: 159–183, 1973 [Google Scholar]