Abstract
Background
Suicide represents 1.8% of the global burden of disease, yet the prevalence and correlates of suicidal behavior in low income countries are unclear. This study examines the prevalence, age of onset and sociodemographic correlates of suicide ideation, planning, and attempts among South Africans.
Method
Nationally representative data are from the South Africa Stress and Health Study (SASH), a national household probability sample of 4,351 South African respondents aged 18 years and older conducted between 2002 and 2003, using the World Health Organization version of the composite international diagnostic interview (CIDI). Bivariate and survival analyses were employed to delineate patterns and correlates of nonfatal suicidal behavior. Transitions are estimated using life table analysis. Risk factors are examined using survival analysis.
Results
The risk for attempted suicide is highest in the age group 18–34 and Coloureds had highest lifetime prevalence for attempts. Cumulative probabilities are 43% for the transition from ideation to a plan, 65% from a plan to an attempt, and 12% from ideation to an unplanned attempt. About 7.5% of unplanned and 50% of planned first attempts occur within 1 year of the onset of ideation. South Africans at higher risk for suicide attempts were younger, female, and less educated.
Conclusions
The burden of nonfatal suicidality in South Africa underscores the need for suicide prevention to be a national priority. Suicide prevention efforts should focus on planned attempts due to the rapid onset and unpredictability of unplanned attempts.
Keywords: suicide attempts, self-harming behaviors, South Africa, sociodemographic, ethnicity
Introduction
The World Health Organization estimates that in 2002 alone, approximately 877,000 deaths worldwide were due to suicide [35], making it an important worldwide public health concern for high income as well as low income countries [18]. While there is a wealth of research literature on suicide and nonfatal suicidal behavior in high income countries such as the United States [14, 15], the United Kingdom [23], and Australia [33], information on the prevalence and trends of suicide and nonfatal suicidal behavior in low income countries is often scarce. When data are available, it is believed that they underestimate rates of suicidal behavior in low income countries [34]. Suicide prevention efforts should be based on sound epidemiological research, which can constitute a primary and necessary building block to inform universal, selective, and effective prevention strategies [9, 34]. Therefore, the need to have more reliable and extensive scientific data on nonfatal suicidal behaviors from low income countries is critical, as these are among the strongest predictors of suicide [11]. This report presents for the first time nationally representative data on the prevalence and risk factors of nonfatal suicidal behavior in the South Africa Stress and Health Study [36].
The most current data on suicidal behavior in South Africa is available primarily from the Durban parasuicide study (DPS), a large, multicenter program involved in studying suicidal behavior in South Africa, as well as data from South African national injury mortality surveillance system (NIMSS) [19, 28]. While programs such as the DPS and NIMSS are working to increase accuracy in the reporting of fatal suicidal behavior in South Africa, there is no current systematic national data collection of nonfatal suicide behavior [28]. While completed suicides represent a major public health problem, they represent only a small fraction of suicidal behaviors. It is commonly known in suicide research that the strongest predictor of suicide is a prior experience of nonfatal suicidal behavior [11]. Research in South Africa has estimated that at least twenty nonfatal suicide attempts occur for every death by suicide [25], yet nationally representative research on nonfatal suicidal behavior is lacking. The substantial body of South African research on nonfatal suicidal behavior tends to be based on clinical and community samples and often does not present data from the largest ethnic group, namely those of African descent, that is, Blacks [22]. National estimates of the lifetime prevalence and correlates of suicide ideation, planning, and attempts among South Africans, including specific cultural groups, are reported for the first time using the recently collected South Africa Stress and Health Study (SASH).
Method
The SASH study, collected between January 2002 and June 2004, was a national probability sample of 4,351 adult South Africans living in both households and hostel quarters [37]. Hostel quarters were included to maximize coverage of the nation’s young working age males, many of whom lived in these urban group quarter constructed by mine owner during the Apartheid era to house and control the migrant laborers, South Africa’s primary labor reserves. The sample did not include individuals in institutions or in the military. Individuals of all racial and ethnic backgrounds were included in the study. The sample was selected using a three-stage clustered area probability sample design. The first stage involved the selection of stratified primary sample areas based on the 2001 South African Census enumeration areas (EAs). The second stage involved the sampling of housing units within clusters selected within each EA. Within each of these strata, 600 households were listed from maps, census data, or aerial photographs. Sampled residences were stratified into 10 diverse housing categories: Rural–commercial, agricultural, rural traditional subsistence areas, African townships, informal urban or peri-urban shack areas, Coloured townships, Indian townships, general metropolitan residential areas, general large metropolitan residential areas, and domestic servant accommodation in urban areas. The third stage involved the random selection of one adult respondent in each sampled housing unit.
Since the data collection procedure proceeded province by province, cohorts of 40–60 SASH interviewers in each province were trained in centralized group sessions lasting one week. The interviews were conducted face to face in seven different languages: English, Afrikaans, Zulu, Xhosa, Northern Sotho, Southern Sotho and Tswana. Interviews lasted an average of three and a half hours, with many requiring more than one visit to complete. Field interviewers made up to three attempts to contact each respondent. The overall response rate was 85.5%. All recruitment, consent and field procedures were approved by the Human Subjects Committees of the University of Michigan and the Harvard Medical School, and by a single project assurance of compliance from the Medical University of South Africa (MEDUNSA) that was approved by the National Institute of Mental Health.
Measures
Suicidal behavior
Suicidality is assessed in its own section of the WHO Composite International Diagnostic Interview Version 3.0 [CIDI 3.010, 16] [WMH-CIDI] by a series of questions about lifetime suicidal behaviors including ideation, planning, and attempts. The CIDI is a fully structured diagnostic interview that is lay administered and can generate diagnoses according to both the ICD-10 [WHO, 38] and DSM [APA, 1] diagnostic systems. Good inter-rater reliability, test–retest reliability, and validity have been found in earlier versions of the CIDI [2], while good validity of CIDI diagnoses compared to diagnoses based on blinded clinical reappraisal interviews have been found in WMH methodological studies [10]. The translation of the English version of the CIDI into the five other languages used in the SASH was carried out according to WHO recommendations of iterative back-translation conducted by panels of bilingual and multilingual experts. Discrepancies found in the back-translation were resolved by consensus of an expert panel.
Respondents were screened in to the suicidality section of the WMH-CIDI if they answered affirmatively to the question “Have you ever seriously thought about committing suicide?” These respondents are said to have engaged in suicidal ideation and will be referred to as ideators in this report, while those answering negatively will be referred to as non-ideators. Only the ideators went on to answer questions to determine if they ever made plans to commit suicide (“Have you ever made a plan for committing suicide?”) and if they ever attempted suicide (“Have you ever attempted suicide?”). Information on the age of first occurrence of the three main outcomes was also obtained. To get a better understanding of the progression from ideation to attempt, we also examined three conditional associations corresponding to different pathways individuals may follow from suicidal ideation to attempted suicide: plan given ideation, attempt given ideation but no plan (unplanned suicide attempt), and finally attempt given ideation and a plan (planned suicide attempt) [15]. Four additional control variables were constructed to assess the age of onset, time since onset of ideation, whether respondents had a plan, and time since onset of plan.
Sociodemographic status
Sociodemographic correlates include age, sex, race (Africans, Coloured, Indian, White), and marital and employment status. The marital and employment status was coded to differentiate whether the suicide-related events occurred prior to the respondents’ first employment or before getting married. Educational status was divided into five groups: no formal education, elementary school education (one to 7 years of education), some high school education (8–11 years), high school education completed, and tertiary education. Cohort was coded to differentiate respondents born in the age groups 18–34, 35–49, 50–64, and 65 and older.
Analysis procedures
All analyses were weighted to be nationally representative of the populations and subgroups of interests and were carried out using the SAS Version 9.1.3 software package [24]. Univariate cross-tabulations were used to calculate the nationally representative prevalences of the suicidal behaviors by sociodemographic characteristics. Life table methods were used to derive the age of onset distributions. Discrete-time survival analysis with time-varying covariates was used to study the risk factors of lifetime suicide ideation, plans, and attempts [7]. Retrospective reports were used in the survival analyses to create the time-varying risk factors (e.g., ages of changes in marital status, [12] and to date the ages of onset of the seven risk pathways to suicide (i.e., ideation, attempt, planning, planning among ideators, attempts among ideators, attempt given ideation but no plan, and finally attempt given ideation and a plan). Graphical and statistical techniques were used to assess each of the risk factors for proportionality of hazards. The ages of onset, as well as a time-varying marital and employment status, and time since onset of ideation or plan risk factors, were determined from the respondents’ retrospective reports.
In order to account for the stratified multistage sample design, the data were weighted to adjust for differential probability of selection within households as a function of household size and clustering of the data, and for differential non-response. A post-stratification weight was also used to make the sample distribution comparable to the population distribution in the 2001 South African Census for age, sex, and province (Table 1). The weighting and geographic clustering of the data were taken into account in data analyses by using the jackknife repeated replications (JRR) simulation method implemented in a SAS macro [17]. The JRR estimates adjust for the clustering and weighting of cases. The survival coefficients were exponentiated and are reported below in the form of odds-ratios. The 95% confidence intervals of these coefficients are also reported and have been adjusted for design effects. Multivariate tests are based on χ2’s computed from coefficient variance-covariance matrices that were adjusted for design effects using JRR. When a result is specified as being “significant” below, it is referring to statistical significance based on two-sided design-based tests evaluated at the 0.05 level.
Table 1.
Sociodemograpic distribution of the South African sample compared to the population
| Unweighed n (%) | Weighed n (%) | 2001 Census (%) | |
|---|---|---|---|
| Sex | |||
| Male | 39.8 | 46.3 | 46.8 |
| Female | 60.2 | 53.7 | 53.2 |
| Age | |||
| 20–34 | 47.1 | 47.2 | 45.5 |
| 35–49 | 31.2 | 30.4 | 30.5 |
| 50–64 | 15.8 | 16.9 | 15.3 |
| 0–65 | 5.9 | 5.5 | 8.7 |
| Race | |||
| African | 76.2 | 76.2 | 79 |
| Coloured | 12.9 | 10.4 | 8.9 |
| Indian or Asian | 3.7 | 3.4 | 2.5 |
| White | 7.2 | 10 | 9.6 |
| Province | |||
| Eastern Cape | 14.2 | 13.1 | 13.3 |
| Free State | 9.7 | 6.2 | 6.2 |
| Guateng | 13.6 | 23 | 22.2 |
| Kwazulu Natal | 17.2 | 19.5 | 20.2 |
| Limpopo | 9.6 | 10.5 | 10.5 |
| Mpumalanga | 9.5 | 6.6 | 6.6 |
| Northern Cape | 5.4 | 1.9 | 1.3 |
| North West | 10.4 | 8.3 | 8.3 |
| Western Cape | 10.3 | 11.1 | 10.8 |
Results
Prevalences
Table 2 presents the estimated lifetime prevalences of suicidal behaviors. The estimated lifetime prevalences (with standard errors in parentheses) of suicide ideation, plans, and attempts among South Africans are 9.1% (0.7), 3.8% (0.4), and 2.9% (0.3), respectively. There were noticeable gender differences, with females reporting twice as many attempts as males, 3.8% (0.5) and 1.8% (0.3), respectively. The reported rate of attempted suicide varies significantly by race, with Coloureds [mixed racial origin) (7.1%; SE: 1.3) reporting levels of attempted suicide that were approximately three times higher than any other are racial groups, including both Whites (2.4%; SE: 0.7) and Africans (2.4%; SE: 0.3).
Table 2.
Life time prevalence of suicide-related outcomes: South Africa
| Total sample (n = 4315) | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ideation | Plan | Attempt | Plan among ideators (n = 394) |
Attempt among ideators (n = 394) |
Attempt among ideators w/o a lifetime plan (n = 223) |
Attempt among ideators w/a a lifetime plan (n = 171) |
||||||||||||||||
| % | SE | n | % | SE | n | % | SE | n | % | SE | n | % | SE | n | % | SE | n | % | SE | n | ||
| Male | 8.0 | 1.0 | 132 | 3.3 | 0.5 | 58 | 1.8 | 0.4 | 36 | 41.6 | 3.8 | 58 | 22.7 | 4.3 | 36 | 7.1 | 3.3 | 9 | 44.6 | 7.9 | 27 | |
| Female | 10.1 | 0.7 | 262 | 4.2 | 0.4 | 113 | 3.8 | 0.5 | 104 | 41.7 | 3.2 | 113 | 37.9 | 3.3 | 104 | 14.0 | 2.7 | 24 | 71.3 | 5.0 | 80 | |
| African | 8.2 | 0.8 | 277 | 3.9 | 0.4 | 127 | 2.4 | 0.3 | 85 | 47.1 | 3.2 | 127 | 28.8 | 2.9 | 85 | 5.6 | 1.5 | 12 | 55.0 | 4.7 | 73 | |
| Coloured | 13.2 | 1.4 | 73 | 5.7 | 1.1 | 32 | 7.1 | 1.3 | 39 | 43.5 | 5.6 | 32 | 54.1 | 6.6 | 39 | 33.4 | 9.6 | 15 | 81.0 | 7.9 | 24 | |
| White | 12.4 | 3.2 | 32 | 1.7 | 0.7 | 8 | 2.4 | 0.7 | 11 | 14.0 | 3.8 | 8 | 19.6 | 4.6 | 11 | 10.0 | 3.8 | 4 | 78.0 | 18.5 | 7 | |
| Indian | 5.8 | 1.2 | 12 | 1.6 | 0.9 | 4 | 2.5 | 1.6 | 5 | 27.4 | 17.6 | 4 | 43.1 | 28.6 | 5 | 27.0 | 29.0 | 2 | 85.7 | 15.0 | 3 | |
| Total sample | 9.1 | 0.7 | 394 | 3.8 | 0.4 | 171 | 2.9 | 0.3 | 140 | 41.7 | 2.3 | 171 | 31.7 | 2.6 | 140 | 11.2 | 2.3 | 33 | 60.5 | 4.5 | 107 | |
The conditional probability of ever making a plan among lifetime ideators is 41.7% (2.3), while the conditional probabilities of making an attempt among ideators are 31.7% (2.6) with a plan and 11.2% (2.3) without a plan; 60.5% (4.5) of attempters reporting that they had a plan prior to making their first attempt. An ethnicity analysis reveals important differences in the conditional probability of making an attempt among ideators without a plan. Africans (5.6, SE: 1.5) are less likely to engage in unplanned suicide attempts, while Coloureds (33.4, SE: 9.6) reporting the highest level of unplanned suicide attempts.
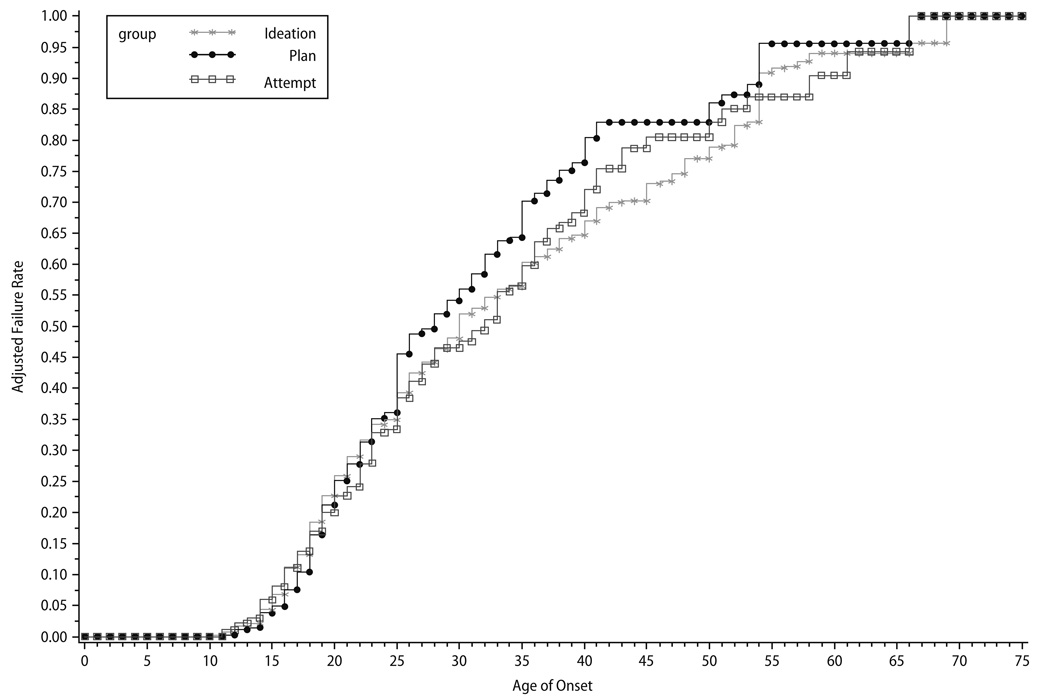
Age of onset distributions
Figure 1 show the median ages of onset for initial suicide ideation, plans, and attempts. These curves shows that the median ages of onset for ideation and planning are in the late twenties, but for attempts the median age of onset is the early thirties. A comparison of the curves for suicide planning and attempts reveal that the onset of suicide planning lags behind attempts for the ages 10–20 years, suggesting that unplanned suicide attempts are more common than planned attempts for those younger age groups.
Fig. 1.
Failure rate of first suicide ideation, plan, and attempt for South Africa
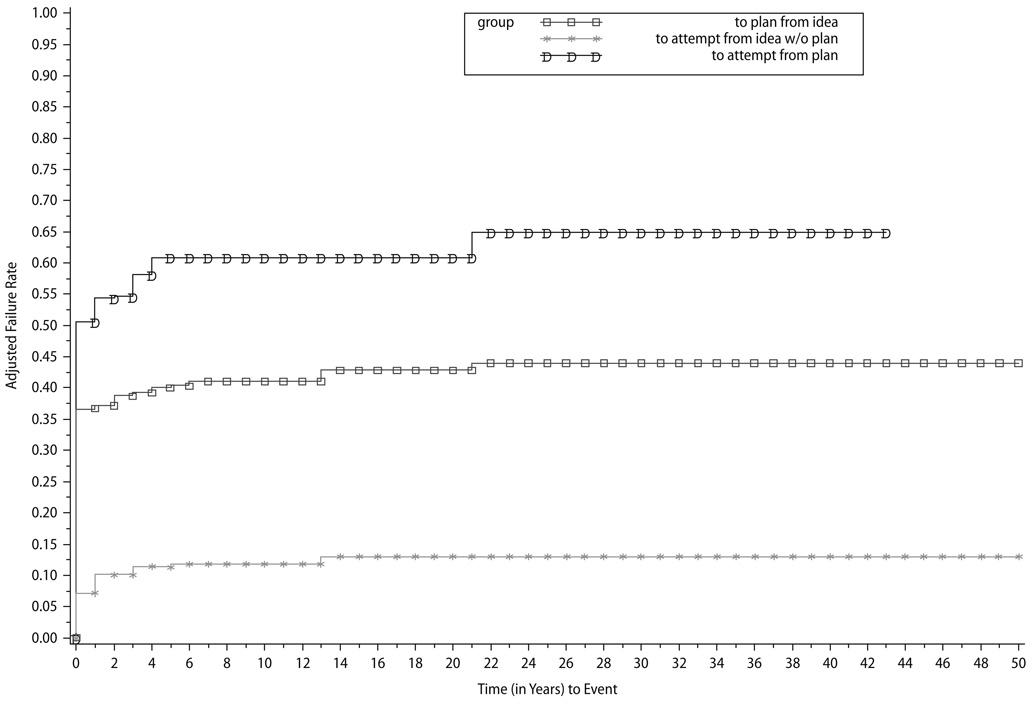
Figure 2 displays curves representing how soon after initial ideation onset respondents progressed to more serious suicidal behaviors. The curves show that progression from ideation to first onset of a plan, from a plan to first attempt (planned attempt), and from ideation to first attempt in the absence of a plan (unplanned attempt) are all highest in the first year after onset of the earlier stage. The risk of an attempt is substantially greater in the presence of a plan. While attempts are almost exclusively confined to the first year after ideation onset in the absence of a plan, the risk of an attempt among ideators with a plan continues for many years after their first onset of ideation, approximately 8 years longer than those making unplanned attempts. In all, roughly 7.5% of unplanned attempts and 50% of planned attempts occur within one year of the onset of ideation.
Fig. 2.
Failure rate for transitions for South Africa
Socioeconomic risk factors
Risk of a suicide attempt is significantly associated with being female, being in the age group 18–34, and having low/medium education levels (Table 3). In addition, attempted suicides are less likely to occur prior to starting formal employment (OR = 0.5, 95% CI 0.3–0.8). The higher odds of an attempt among women compared with men reflect both a higher conditional odds of an attempt among ideators and higher conditional odds of an attempt among ideators with a plan. There is no significant gender difference in the odds of making a plan among ideators.
Table 3.
Sociodemograpic risk factors for 1st onset of suicide-related outcomes: South Africa
| Total sample (n = 4274) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ideation | Plan | Attempt | Plan among ideators (n = 353) |
Attempt among ideators (n = 353) |
Plan among ideators without a lifetime plan (n = 199) |
Attempt among ideators with a lifetime plan (n = 154) |
||||||||
| OR | (95%Cl) | OR | (95%Cl) | OR | (95%Cl) | OR | (95%Cl) | OR | (95%Cl) | OR | (95%Cl) | OR | (95%Cl) | |
| Sex | ||||||||||||||
| Female | 1.3 | 0.9 –1.8 | 1.4 | 0.9–2.1 | 2.7* | 1.6–4.4 | 1.1 | 0.7–1.8 | 2.9* | 1.4 –6.0 | 3.0 | 0.8–11.1 | 3.3* | 1.4–7.8) |
| Male | 1.0 | – | 1.0 | – | 1.0 | – | 1.00 | – | 1.0 | – | 1.0 | – | 1.0 | – |
| 2.2 | 0.136 | 1.9 | 0.169 | 15.8** | 0.000 | 0.3 | 0.606 | 8.8** | 0.003 | 2.9 | 0.088 | 8.2** | 0.004 | |
| Cohort | ||||||||||||||
| 18–34 | 9.6* | 2.9–32.1 | 19.0* | 2.3–159.7 | 11.6* | 2.1–65.9 | 5.5 | 0.7–41.1 | 0.8 | 0. 2–3.0 | 0.9 | 0.1–16.3 | 0.0* | 0.0–0.0 |
| 35–49 | 2.5 | 0.7–8.1 | 3.9 | 0.5–31.4 | 2.2 | 0.4–12.7 | 2.8 | 0.4–18.0 | 0.5 | 0.1–1.9 | 1.1 | 0.1–17.4 | 0.0* | 0.0–0.0 |
| 50–64 | 1.4 | 0.5–4.1 | 2.0 | 0.3–14.4 | 1.3 | 0.2–6.9 | 2.5 | 0.4–15.2 | 0.5 | 0.1–2.6 | 1.7 | 0.1–34.5 | 0.0* | 0.0–0.0 |
| 65+ | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – |
| 135.77** | 0.000 | 73.4** | 0.000 | 85.2** | 0.000 | 4.6 | 0.204 | 1.8 | 0.617 | 0.9 | 0.820 | 87.0.1** | 0.000 | |
| Education | ||||||||||||||
| Student | 1.3 | 0.6–2.7 | 1.6 | 0.3–7.7 | 3.4 | 1.0–12.2 | 1.2 | 0.2–7.0 | 3.2 | 0.8–12.2 | 1.5 | 0.4–5.8 | 4.6 | 0.8–26.4 |
| Low | 1.5 | 0.7–3.5 | 2.3 | 0.6–9.5 | 3.8 | 0.9–17.2 | 2.2 | 0.3–14.6 | 2.1 | 0.4–12.0 | 0.7 | 0.1–3.1 | 2.5 | 0.2–26.6 |
| Low/medium | 1.6 | 0.9–2.9 | 3.0 | 0.8–10.4 | 5.7* | 1.9–17.0 | 3.0 | 0.6–14.8 | 3.8 | 1.1–13.0 | 1.1 | 0.3–4.7 | 4.8* | 1.4–16.8 |
| Medium | 1.6 | 0.9–2.7 | 2.7 | 0.8–8.9 | 4.0* | 1.4–11.3 | 2.5 | 0.6–11.3 | 1.8 | 0.7–4.6 | 1.0 | – | 1.8 | 0.5–6.6 |
| High | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – |
| 4.0 | 0.404 | 7.8 | 0.099 | 13.2** | 0.010 | 11.0** | 0.026 | 6 | 0.200 | 0.6 | 0.900 | 9.4 | 0.052 | |
| Employment | ||||||||||||||
| Before first employment |
0.8 | 0.6–1.1 | 0.7 | 0.4–1.1 | 0.5* | 0.3–0.8 | 0.6 | 0.3–1.2 | 0.7 | 0.4–1.2 | 0.6 | 0.2–1.7 | 0.8 | 0.4–1.9 |
| After first employment |
1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – |
| 1.9 | 0.170 | 2.9 | 0.091 | 8.0* | 0.005 | 2.1 | 0.143 | 1.9 | 0.164 | 0.8 | 0.357 | 0.2 | 0.643 | |
| Marriage | ||||||||||||||
| Before ever married |
0.8 | 0.6–1.2 | 0.8 | 0.5–1.4 | 0.9 | 0.5–1.5 | 1.0 | 0.5–1.9 | 1.2 | 0.7–2.3 | 1.7 | 0.4–6.3 | 1.2 | 0.5–2.7 |
| After ever married |
1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – |
| 1.3 | 0.260 | 0.8 | 0.384 | 0.3 | 0.568 | 0.00 | 0.997 | 0.4 | 0.505 | 0.60 | 0.454 | 0.1 | 0.713 | |
| Age of onset of ideation | ||||||||||||||
| Early | – | – | – | – | – | – | 1.4 | 0.5–4.0 | 0.6 | 0.2–2.0 | 0.8 | 0.1–5.7 | 0.4 | 0.1–1.7 |
| Middle | – | – | – | – | – | – | 1.3 | 0.5–3.3 | 0.7 | 0.3–1.7 | 0.2* | 0.0–0.8 | 0.9 | 0.3–2.5 |
| Late | – | – | – | – | – | – | 1.00 | – | 1.0 | – | 1.0 | – | 1.0 | – |
| – | – | – | – | – | – | 0.6 | 0.746 | 0.8 | 0.676 | 6.0** | 0.049 | 2.1 | 0.356 | |
| Time since onset of ideation± | ||||||||||||||
| 0 | – | – | – | – | – | – | 108.4* | 36.2–324.1 | 194.4* | 41.0–921.7 | 70.0* | 7.2–680.0 | – | – |
| 1–5 | – | – | – | – | – | – | 2.3 | 0.7–7.5 | 15.4* | 3.3–73.0 | 8.8 | 0.9–81.1 | – | – |
| 6–10 | – | – | – | – | – | – | 1.4 | 0.3–6.6 | 1.1 | 0.1–13.8 | 0.0* | 0.0–0.0 | – | – |
| 11+ | – | – | – | – | – | – | 1.00 | – | 1.0 | – | 1.0 | – | – | – |
| – | – | – | – | – | – | 149.00* | 0.000 | 98.3** | 0.000 | 1,150.3** | 0.000 | – | – | |
| Having plan | ||||||||||||||
| Yes | – | – | – | – | – | – | – | – | 10.8 | 6.5–17.8 | – | – | – | – |
| No | – | – | – | – | – | – | – | – | 1.0 | – | – | – | – | – |
| – | – | – | – | – | – | – | – | 90.3** | 0.000 | – | – | – | – | |
| Times since onset of plan± | ||||||||||||||
| 0 | – | – | – | – | – | – | – | – | – | – | – | – | 189.6* | 23.0–1,563.5 |
| 1–5 | – | – | – | – | – | – | – | – | – | – | – | – | 11.1* | 1.4–90.2 |
| 6–10 | – | – | – | – | – | – | – | – | – | – | – | – | 0.0* | 0.0–0.0 |
| 11+ | – | – | – | – | – | – | – | – | – | – | – | – | 1.00 | – |
| – | – | – | – | – | – | – | – | – | – | – | – | 1575.9** | 0.000 | |
– indicates that it is not used as a predicator in the model. Results are based on multivariate discrete-time survival model with person-year as the unit of analysis.
Time intervals (INT) are used as a control, but in different form for the 1st 3 columns and the last 4 columns. Cases with any missing values (including 998 and 999) on the suicidality AOO variables are deleted
OR significant at the 0.05 level, two-sided test
Significant at the 0.05 level, two-sided test
Time is measure in years
The higher odds of an attempt in the younger than in the older cohort is also due to two significant pathways: a higher unconditional odds of initial ideation (OR = 9.6) and planning (OR = 19.0). The results for cohorts also suggest the presence of a linear trend for the three outcomes (i.e., ideation, plan, attempts). In particular, those born in recent cohorts are significantly more likely to develop a suicide plan and to attempt suicide There is a significant difference across age of ideation onset in the risk for an unplanned attempt with younger rather than older South Africans being more likely to engage in such behavior. Having a plan is associated with higher (OR = 10.8) conditional odds of attempts among ideators, although the risk is highest only within the first 5 years after onset of plan.
Discussion
Reported for the first time are important ethnic differences among South Africans in the lifetime prevalence of suicide ideation, planning, and attempts. The 2.9% lifetime prevalence estimate of attempted suicide among South Africans is within the range of the 4.1–4.6% reported for American samples [13, 14]. Coloured South Africans reported a 7.1% prevalence rate of attempted suicide, which was the highest, reported in this general population survey. Coloureds’ patterns of suicidal behavior might represent their levels of stressful adjustment to South Africa’s rapid political and socio-economic transitions [5], wherein they are not experiencing growths in employment and other social opportunities they once held over Africans under apartheid. A lack of an external source of blame for hardships, combined with expectations of a high quality of life in post-apartheid era, has also been proposed to explain racial differences in suicide risk in South Africa [4]. Reasons for the substantially higher risk for attempted suicide among Coloureds and planned attempts must be examined in future research that attends to these hypotheses, including examining the role substance abuse among Coloureds, as well as other unique stressors for this population in a post-apartheid society.
Similar to the results for the United States based on the National Comorbidity Survey and National Survey of American Life, SASH data indicate that the greatest risk of progressing to suicide planning and to attempts among ideators occurs within the first year after ideation onset. The SASH finding of rapid transition from first onset of suicide ideation and plans to attempts cannot be compared with previous research on South Africa as no other population surveys examine this issue. Notably, ideators with a plan continued to make initial suicide attempts up to 21 years after the first onset of ideation. The higher prevalence of attempted suicide among females is consistent with previous studies of South African suicidal behaviors [27]. In addition, the 9.1% estimated prevalence of suicide ideation is comparable to previous estimates from studies using clinical samples [6, 27].
The SASH provides the first nationally representative general population data on the estimated age of onset distributions, the intercohort differences, and correlates of lifetime suicide attempts for South Africans. The finding that the risk for attempted suicide is highest in the age group 18–34 is consistent with independent evidence that younger South Africans are at significantly higher risk of nonfatal suicidal behavior [8, 19, 29]. Research on the reasons for the higher suicide risk among younger South African are unclear [28], yet tenable hypotheses are abundant, including younger Africans having to face higher levels of stress [32] stemming from experiences of human rights violations (even though one would think these are more common in older Africans who lived through apartheid and social role transformations) [26, 30, 31], and the onset of diseases such as HIV/AIDS [21] in this age group.
The relationship between the risk for suicide attempts and other sociodemographic correlates is consistent with previous results based on cross-sectional surveys and clinical or community samples. For instance, previous research has established that there is an inverse relationship between education and attempted suicide [15]. According to our analyses, South Africans with low to medium levels of education (high school education) were more likely to have attempted suicide than those with higher levels of education. The higher risk for the onset of attempted suicide after first employment might be due to unique stressors associated with employment in South Africa, particularly for Coloured and Africans, who are more likely to be employed in low class jobs. The risk of suicide is greater for workers in occupations of lower prestige, class, and salary [3]. Analyses showed that marital status, though often found to be an important correlate [20], was not a significant predictor of suicide planning or attempts.
Limitations
The SASH findings must be considered in the context of several important limitations. First, the results reported here are limited by the fact that we do not know the extent to which cultural factors affected the willingness of our respondents to either admit or recall suicidal behavior over their lifetime and does this bias vary by ethnicity. The study results may also be affected by recall bias associated with the respondents’ age and mental health status. Second, the SASH is retrospective and cross-sectional; thus the prevalence estimates are likely to be lower-bound estimates [15]. Third, the validity of the CIDI in the different ethnic groups studied in this survey might bias our results, particularly on the measures of ideation, plans, and attempts. Despite these constraints and the possibility that they may well have different effects in the different ethnic groups, the effect of most of the limitations noted above is to make our estimates of non-fatal suicidal behavior more conservative than might otherwise be the case.
In conclusion, the SASH provides the first nationally representative general population data on lifetime estimates of suicide ideation, planning, and attempts among South Africans. The study results provide evidence that South Africans engage in suicidal thought and behaviors at levels nearly comparable to other nations. Prior to this study, relatively little was known about the ethnic differences in the national prevalence of nonfatal suicidal behavior among South Africans. The results of the study should impact physicians and mental health professionals who screen for risk for suicide. For instance, the higher reported rates of attempted suicide, notably among Coloured South Africans, and the role of ethnicity should be addressed in future research and considered by clinicians when screening and treating South Africans who might be suicidal. Clinicians should also consider the higher risk for unplanned attempts in young South Africans adults versus a greater likelihood of planned suicide attempts in older adults.
Contributor Information
Sean Joe, School of Social Work, University of Michigan, 1080 South University Ave, Room 2780, Ann Arbor (MI) 48109, USA, Tel.: +1-734/763-6288, Fax: +1-734/763-3372, E-Mail: sjoe@ssw.umich.edu.
Dan J. Stein, Dept. of Psychiatry and Mental Health, University of Cape Town Cape Town, South Africa
Soraya Seedat, Dept. of Psychiatry, University of Stellenbosch, Cape Town, South Africa
Allen Herman, National School of Public Health, South Africa.
David R. Williams, School of Public Health, Harvard University, Boston (MA), USA
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders; American Psychiatric Association; Washington. 1994. [Google Scholar]
- 2.Andrews G, Peters L. The psychometric properties of the composite international diagnostic interview. Soc Psychiatry Psychiatr Epidemiol. 1998;33:80–88. doi: 10.1007/s001270050026. [DOI] [PubMed] [Google Scholar]
- 3.Boxer PA, Burnett C, Swanson N. Suicide and occupation: a review of the literature. J Occup Environ Med. 1995;37:442–452. doi: 10.1097/00043764-199504000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Burrows S, Laflamme L. Suicide mortality in South Africa: a city-level comparison across socio-demographic groups. Soc Psychiatry Psychiatr Epidemiol. 2006;41:108–114. doi: 10.1007/s00127-005-0004-4. [DOI] [PubMed] [Google Scholar]
- 5.Burrows S, Vaez M, Butchart A, Laflamme L. The share of suicide in injury deaths in the South African context: sociodemographic distribution. Public Health. 2003;117:3–10. doi: 10.1016/s0033-3506(02)00019-7. [DOI] [PubMed] [Google Scholar]
- 6.Deonarain M, Pillay BJ. A study of parasuicide behaviour at the Chris Hani Baragwanath Hospital. In: Schlebusch L, Bosch BA, editors. Suicidal Behaviour 4: proceedings of the fourth Southern African conference on suicidology; Department of Medically Applied Psychology, Faculty of Medicine, University of Natal; Durban. 2000. pp. 112–127. [Google Scholar]
- 7.Efron B. Logistic regression, survival analysis, and the Kaplan–Meier curve. J Am Sociol Assoc. 1988;83:414–425. [Google Scholar]
- 8.Flisher A, Liang H, Laubscher R, Lombard CF. Suicide trends in South Africa, 1968-90. Scand J Public Health. 2004;32:411–418. doi: 10.1080/14034940410029469. [DOI] [PubMed] [Google Scholar]
- 9.Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE. Reducing suicide: a national imperative. Washington: Institute of Medicine, National Academies Press; 2002. [PubMed] [Google Scholar]
- 10.Haro JM, Arbabzadeh-Bouchez SBTS, Girolamo GD, Guyer M, Jin R, et al. Concordance of the composite international diagnostic interview version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO world mental health surveys. Int J Methods Psychiatr Res. 2008 doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harris EC, Barraclough B. Suicide as an outcome for mental disorders: a meta-analysis. Br J Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- 12.Hosmer DW, Lemeshow S. Applied survival analysis: regression modeling of time to event data. New York: Wiley; 2000. [Google Scholar]
- 13.Joe S, Baser R, Breeden G, Neighbors HW, Jackson J. Prevalence of and risk factors of lifetime suicide attempts among blacks in the United States. J Am Med Assoc. 2006;296:2112–2123. doi: 10.1001/jama.296.17.2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. J Am Med Assoc. 2005;293:2487–2495. doi: 10.1001/jama.293.20.2487. [DOI] [PubMed] [Google Scholar]
- 15.Kessler RC, Borges G, Walters EE. Prevalence of risk factors for lifetime suicide attempts in the national comorbidity survey. Arch Gen Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- 16.Kessler RC, Ustun TB. The world mental health (WMH) survey initiative version of the world health organization (WHO) composite international diagnostic interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kish L, Frankel MR. Balanced repeated replications for standard errors. J Am Stat Assoc. 1970;65:1071–1094. [Google Scholar]
- 18.Mann JJ, Apter A, Bertolote J, Beautruis A, Currier D, Haas A, Hegerl U, Lonnqvist J, Malone K, Marusic A, Mehlum L, Patton G, Phillips M, Rutz W, Rihmer Z, Schmidtke A, Shaffer D, Silverman M, Takahashi Y, Varnik A, Wasserman D, Yip P, Hendin H. Suicide prevention strategies. JAMA. 2005;294:2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 19.Matzopoulos R, Cassim M, Seedat M. A profile of fatal injuries in South Africa: fourth annual report of the national injury mortality surveillance system. Tygerberg: Medical research Council-UNISA Crime, Violence and Injury Lead Programme; 2003. [Google Scholar]
- 20.Nisbet PA. Protective factors for suicidal black females. Suicide Life Threat Behav. 1996;26:325–341. [PubMed] [Google Scholar]
- 21.Noor Mahomed SB, Karim E. Suicidal ideation and suicide attempts in patients with HIV presenting at a general hospital. In: Schlebusch L, Bosch BA, editors. Suicidal behaviour 4: proceedings of the fourth Southern African conference on suicidology; Department of Medically Applied Psychology, Faculty of Medicine, University of Natal; Durban. 2000. pp. 38–48. [Google Scholar]
- 22.Pillay A, Wassenaar D, Kramers A. Non-fatal suicidal behaviour in South Africa: a study of patients of African descent. J Psychol Afr. 2001;11:73–87. [Google Scholar]
- 23.Pritchard C, Hansen L. Child, adolescent and youth suicide and undetermined deaths in England and Wales compared with Australia, Canada, France, Germany, Italy, Japan and the USA for the 1974–1999 period. Int J Adolesc Med Health. 2005;17:239–253. doi: 10.1515/ijamh.2005.17.3.239. [DOI] [PubMed] [Google Scholar]
- 24.SAS Institute. SAS/STAT user’s guide, version 9.1. Cary: SAS Institute, Inc.; 2005. [Google Scholar]
- 25.Schlebusch L. An overview of suicidal behavior in South Africa at the dawn of the new millenium. In: Schlebusch L, Bosch BA, editors. Suicidal behavior 4: proceedings of the fourth Southern African conference on suicidology; Department of Medically Applied Psychology, Faculty of Medicine, University of Natal; Durban. 2000. pp. 3–11. [Google Scholar]
- 26.Schlebusch L. Current perspectives on suicidal behavior in South Africa. In: Suffla S, Niekerk Av, Duncan D, editors. Crime, violence and injury prevention in South Africa: developments and challenges. Tygerberg: Medical Research Council-UNISA Crime, Violence and Injury Lead Programme; 2004. pp. 9–21. [Google Scholar]
- 27.Schlebusch L. Current perspectives on suicidal behaviour in South Africa. In: Suffla S, van Niekerk A, Duncan D, editors. Crime, violence and injury prevention in South Africa: developments and challenges. Tygerberg: Medical Research Council-UNISA Crime, Violence and Injury Lead Programme; 2004. pp. 9–21. [Google Scholar]
- 28.Schlebusch L. Suicidal behaviour in South Africa. Scottsville: University of KwaZulu-Natal Press; 2005. [Google Scholar]
- 29.Schlebusch L, Bosch BA. Suicidal behaviour 4: proceedings of the fourth Southern African conference on suicidology; Department of Medically Applied Psychology, Faculty of Medicine, University of Natal; Durban. 2000. [Google Scholar]
- 30.Schlebusch L, Bosch BA. The emotional injuries of indirect trauma. In: Scout CE, editor. The psychology of terrorism: clinical aspects and responses. Westport: Preager; 2002. pp. 133–141. [Google Scholar]
- 31.Schlebusch L, Noor Mahomed SB. Sucidal behaviour in cancer and HIV/AIDS patients in South Africa; Tenth European symposium on suicide and suicidal Behaviour. Books of Abstracts, 84; Copenhagen. [Google Scholar]
- 32.Schlebusch L, Vawda N, Bosch BA. A brief review of research on suicidal behaviour in black South Africans. Crisis. 2003;24:24–28. doi: 10.1027//0227-5910.24.1.24. [DOI] [PubMed] [Google Scholar]
- 33.Sonowdon J, Hunt GE. Age, period and cohort effects on suicide rates in Australia, 1919–1999. Acta Psychiatr Scand. 2002;105:265–270. doi: 10.1034/j.1600-0447.2002.1193.x. [DOI] [PubMed] [Google Scholar]
- 34.Vijayakumar L, John S, Pirkis J, Whiteford H. Suicide in devloping countries (1) frequency, distribution, and association with socioeconomic indicators. Crisis. 2005;26:104–111. doi: 10.1027/0227-5910.26.3.104. [DOI] [PubMed] [Google Scholar]
- 35.WHO. Geneva: World Health Organization; World health report 2003: shaping the future. 2003
- 36.WHO World Mental Health Survey Consortium. Prevalence, severity, and unmet need for treatment of mental disorders in the world health organization world mental health surveys. JAMA. 2004;291:2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 37.Williams DR, Herman A, Kessler RC, Sonnega J, Seedat S, Stein DJ, Moomal H, Wilson CM. The South Africa stress and health study: rationale and design. Metab Brain Dis. 2004;19:135–147. doi: 10.1023/b:mebr.0000027424.86587.74. [DOI] [PubMed] [Google Scholar]
- 38.World Health Organization. Geneva: injuries and causes of death; Manual of the international statistical classification of diseases. (Ninth Revision edn) 1992