Abstract
Background
We conducted a clinical trial to test whether prophylactic cranial irradiation could be omitted in all children with newly diagnosed acute lymphoblastic leukemia.
Methods
A total of 498 evaluable patients were enrolled. Treatment intensity was based on presenting features and the level of minimal residual disease after remission induction treatment. Continuous complete remission was compared between the 71 patients who previously would have received prophylactic cranial irradiation and the 56 historical controls who received it.
Results
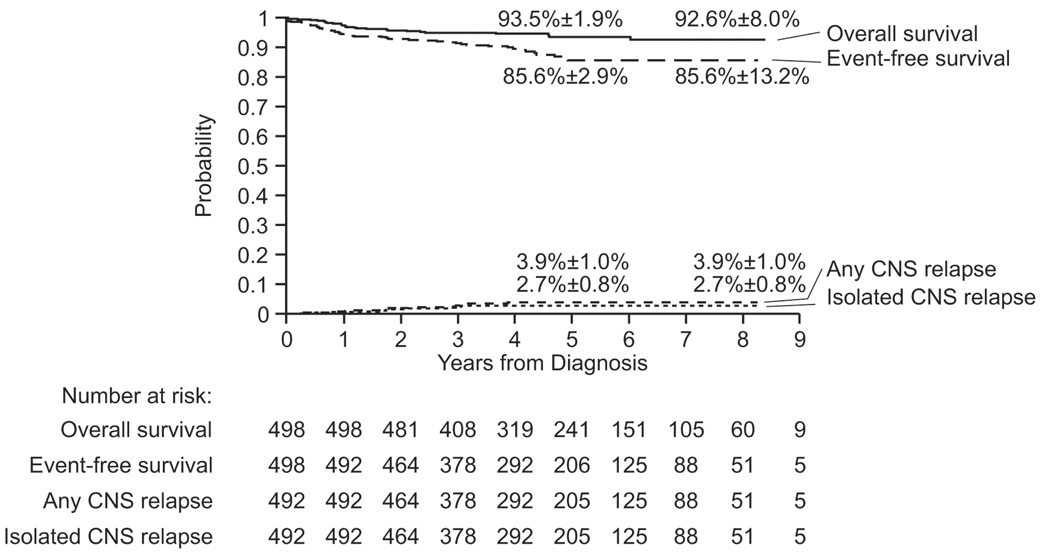
The 5-year event-free and overall survival probabilities (95% confidence interval) for all 498 patients were 85.6% (79.9% to 91.3%) and 93.5% (89.8% to 97.2%), respectively. The 5-year cumulative risk of isolated central-nervous-system (CNS) relapse was 2.7% (1.1% to 4.2%), and that of any CNS relapse (isolated plus combined) was 3.9% (1.9% to 5.9%). The 71 patients had significantly better continuous complete remission than the 56 historical controls (P=0.04). All 11 patients with isolated CNS relapse remain in second remission for 0.4 to 5.5 years. CNS leukemia (CNS-3 status) or a traumatic lumbar puncture with blasts at diagnosis and a high level of minimal residual disease (≥ 1%) after 6 weeks of remission induction were significantly associated with poorer event-free survival. Risk factors for CNS relapse included the presence of the t(1;19)[TCF3-PBX1], any CNS involvement at diagnosis, and T-cell immunophenotype. Common adverse effects included allergic reactions to L-asparaginase, osteonecrosis, thrombosis, and disseminated fungal infection.
Conclusions
With effective risk-adjusted chemotherapy, prophylactic cranial irradiation can be safely omitted in the treatment of childhood acute lymphoblastic leukemia.
Contemporary clinical trials have yielded 5-year event-free survival rates of 79% to 82% for children with acute lymphoblastic leukemia (ALL).1–3 A major challenge is to reduce treatment-related late effects that may occur in more than two-thirds of long-term survivors.4 For a growing proportion of patients, prophylactic cranial irradiation, once a standard treatment, is being replaced by intrathecal and systemic chemotherapy to reduce radiation-associated late complications, such as second cancers, neurocognitive deficits, and endocrinopathy.4–8
Two pediatric clinical trials tested whether prophylactic cranial irradiation could be completely omitted.9,10 Although the cumulative risks of isolated central-nervous-system (CNS) relapse in these trials were relatively low (4% and 3%), event-free survival rates were only 68.4% and 60.7%, respectively. In another study, prophylactic cranial irradiation appeared to improve outcome of children with T-cell ALL.11 Thus, there is a persistent concern that residual leukemic cells remaining after inadequate CNS treatment could not only cause CNS relapse but also reseed bone marrow, leading to hematologic relapse. Thus, virtually all study groups continue to use prophylactic cranial irradiation for up to 20% of patients.12
In our Total XIIIA study, 22% of the patients received prophylactic cranial irradiation, overall 5-year event-free survival rate was 77.6%, and cumulative risk of isolated CNS relapse was 1.2%.13 We substituted prednisone with dexamethasone in post-remission therapy and limited prophylactic cranial irradiation to 12% of the patients in the subsequent Total XIIIB study, resulting in a 5-year event-free survival of 80.8% and a cumulative risk of an isolated CNS relapse of 1.7%.3 In the Total XV study reported here, we tested whether intensification of systemic drugs that affect CNS control, together with optimal intrathecal treatment, would allow the complete omission of prophylactic cranial irradiation without compromising overall survival. These modifications were made in the context of risk assignment based on sequential measurements of minimal residual disease (MRD), and adjustment of chemotherapy dosages based on pharmacogenetics and pharmacokinetics.
METHODS
PATIENTS
From June 2000 to October 2007, 501 consecutive patients (1 to 18 years old) with newly diagnosed ALL were enrolled in Total XV Study at St. Jude Children’s Research Hospital (n=411) or at Cook Children’s Medical Center (n=90). Three patients were subsequently excluded because of a revised diagnosis of myeloid leukemia. The protocol was approved by the institutional review boards and registered at ClinicalTrials.gov, number NCT00137111. Signed informed consent was obtained from the parents or guardians, with assent from the patients, as appropriate.
The diagnostic criteria of ALL was described previously.14 CNS status was defined as CNS-1, CNS-2, CNS-3, or traumatic lumbar puncture with blasts.12 MRD was determined by flow cytometry and/or polymerase-chain-reaction.15,16
STUDY AIMS AND MONITORING
Our major therapeutic aims were (i) to determine whether prophylactic cranial irradiation can be safely omitted in all patients, especially those who would have received this treatment at approximately 1 year of continuous complete remission based on previous criteria (presenting leukocyte count ≥ 100 × 109/L, Philadelphia chromosome, CNS-3 status, or T-cell ALL with leukocyte count ≥ 50 × 109/L),3,13 and (ii) to estimate the overall event-free survival. The study was monitored by an independent Data Safety Monitoring Board. Group-sequential designs were used to provide guidelines for stopping decisions based on safety and efficacy (See Supplementary Appendix for details).
RISK CLASSIFICATION
Risk classification was based on presenting features and treatment response. B-cell precursor cases with age between 1 and 10 years and leukocyte count <50 × 109/L, DNA index ≥ 1.16, or t(12;21)[ETV6-RUNX1] were provisionally classified as low-risk ALL. Cases with t(9;22)[BCR-ABL1] were considered to have high-risk ALL, while the remaining cases were provisionally classified as standard (intermediate)-risk ALL. The final risk status was determined by MRD levels. Any patient with ≥ 1% bone marrow MRD on day 19 of remission induction, or 0.1% to 0.99% MRD after completion of 6-week induction therapy was considered to have standard-risk ALL. MRD ≥ 1% after completion of induction therapy denoted high-risk ALL.
TREATMENT
Remission induction/Consolidation
Patients who consented to the optional therapeutic window were randomized to receive upfront methotrexate over 4 or 24 hours. Four days after methotrexate treatment, remission induction therapy began with prednisone, vincristine, daunorubicin, and asparaginase (Table 1). Patients with ≥ 1% MRD on day 19 received three additional doses of asparaginase. Subsequent induction therapy consisted of cyclophosphamide, mercaptopurine and cytarabine. Upon hematopoietic recovery (between days 43 and 46), MRD was assessed, and consolidation therapy began (Table 1).
TABLE 1.
Remission Induction, Consolidation, and Early Continuation/Reinduction Therapy
| A Remission induction | ||
|---|---|---|
| Agent | Dosage | Schedule |
| Methotrexate | 1 g/m2 IV over 4 or 24 hours | Day 1 |
| Prednisone | 40 mg/m2/day | Days 5–32 |
| Vincristine | 1.5 mg/m2 per week | Days 5, 12, 19, 26 |
| Daunorubicin | 25 mg/m2 per week | Days 5, 12 |
| L-asparaginase (Elspar) | 10,000 U/m2 per dose IM (thrice weekly) | Days 6, 8, 10, 12, 14, 16, (19, 21, 23)* |
| Cyclophosphamide | 1000 mg/m2 IV | Day 26 |
| Cytarabine | 75 mg/m2 per day IV | Days 27–30, 34–37 |
| Mercaptopurine | 60 mg/m2 per night | Days 26–39 |
| Intrathecal cytarabine | Age-dependent | Day 1 |
| Triple intrathecal | Age-dependent | Day 19 (8, 26)** |
| B Consolidation therapy | ||
|---|---|---|
| Agent | Dosage | Schedule |
| High-dose methotrexate* | Targeted to 33µM (low-risk) or 65µM (standard-/or high-risk) | Days 1, 15, 29 and 43 |
| Mercaptopurine | 50 mg/m2 per night | Days 1 to 56 |
| Triple intrathecal | Age-dependent | Day 1, 15, 29 and 43 |
| C Early continuation/reinduction therapy | ||
|---|---|---|
| Week | Low-risk Patients | Standard- or high-risk Patients |
| 1 | Mercaptopurine + dexamethasone + vincristine | Asparaginase + mercaptopurine + dexamethasone + vincristine + doxorubicin |
| 2 | Mercaptopurine + methotrexate | Asparaginase + mercaptopurine |
| 3 | Mercaptopurine + methotrexate | Asparaginase + mercaptopurine |
| 4 | Mercaptopurine + dexamethasone + vincristine | Asparaginase + mercaptopurine + dexamethasone + vincristine + doxorubicin |
| 5 | Mercaptopurine + methotrexate | Asparaginase + mercaptopurine |
| 6 | Mercaptopurine + methotrexate | Asparaginase + mercaptopurine |
| 7 | Dexamethasone + vincristine + asparaginase + doxorubicin | Asparaginase + dexamethasone + vincristine + doxorubicin |
| 8 | Vincristine + asparaginase | Asparaginase + vincristine + doxorubicin |
| 9 | Dexamethasone + vincristine + asparaginase | Asparaginase + dexamethasone + vincristine |
| 10 | Mercaptopurine + methotrexate | Asparaginase + mercaptopurine |
| 11 | Mercaptopurine + methotrexate | Asparaginase + mercaptopurine + vincristine + doxorubicin |
| 12 | Mercaptopurine + methotrexate | Asparaginase + mercaptopurine |
| 13 | Mercaptopurine + methotrexate | Asparaginase + mercaptopurine |
| 14 | Mercaptopurine + dexamethasone + vincristine | Asparaginase + mercaptopurine + dexamethasone + vincristine + doxorubicin |
| 15 | Mercaptopurine + methotrexate | Asparaginase + mercaptopurine |
| 16 | Mercaptopurine + methotrexate | Asparaginase + mercaptopurine |
| 17 | Dexamethasone + vincristine + asparaginase + doxorubicin | Asparaginase + dexamethasone + vincristine |
| 18 | Vincristine + asparaginase | Asparaginase + vincristine |
| 19 | Dexamethasone + vincristine + asparaginase | Asparaginase + vincristine + dexamethasone + high-dose cytarabine |
| 20 | Mercaptopurine + methotrexate | ----------------------------------- |
| 21 | Mercaptopurine + methotrexate | Mercaptopurine + methotrexate |
| 22 | Mercaptopurine + methotrexate | Mercaptopurine + methotrexate |
| 23 | Mercaptopurine + methotrexate | Cyclophosphamide + cytarabine |
| 24 | Mercaptopurine + dexamethasone + vincristine | dexamethasone + vincristine |
Intrathecal cytarabine (40, 50 or 60 mg for ages 1 to 1.99, 2 to 2.99 and ≥ 3 years, respectively). Triple intrathecal treatments (methotrexate 8, 10 or 12 mg; hydrocortisone 16, 20 or 24 mg; and cytarabine 24, 30 or 36 mg for ages 1 to 1.99, 2 to 2.99 and ≥ 3 years, respectively)
Extra triple intrathecal treatment on days 8 and 26 for patients with high-risk features of CNS relapse (CNS-2, CNS-3, traumatic lumbar puncture with blasts, T-cell ALL with leukocyte count > 50×109/L, B-cell precursor ALL with leukocyte count > 100 × 109/L, or the presence of t(9;22)[BCR-ABL1], MLL rearrangement, or hypodiploidy < 45 chromosomes).
Extra asparaginase on days 19, 21, and 23 for patients with ≥ 1% residual leukemia cells in the bone marrow on day 19.
Methotrexate dosage was adjusted according to prior patient-specific pharmacokinetic data to achieve a steady-state concentration of 65 µM (corresponding to an average dose of approximately 5 g/m2) in standard-risk cases, and 33 µM (average 2.5 g/m2) in low-risk cases.
Mercaptopurine – 75 mg/m2 PO every evening for 7 days for low-risk group; 50 mg/m2 in the first 16 weeks and 75 mg/m2 thereafter for the standard- and high-risk groups. The starting dose for patients with heterozygous deficiency of thiopurine methyltransferase was 60 mg/m2 instead of 75 mg/m2.
Dexamethasone – 8 mg/m2 PO per day in 3 divided doses for 5 days for low-risk group and 12 mg/m2 for standard-risk group; 8 mg/m2 on days 1 to 8 and 15 to 21 during reinduction I (weeks 7 to 9) and reinduction II (weeks 17 to 19) for both groups.
Asparaginase – 10,000 U/m2 IM thrice weekly for 9 doses during each reinduction for low-risk group; and 25,000 units /m2 IM weekly for 19 doses for the standard- and high-risk groups; in patients with allergic reactions to E coli asparaginase, Erwinia asparaginase 20,000 units /m2 thrice weekly during reinduction treatment for the low-risk group, and 25,000 units /m2 twice weekly in standard-risk group; in patients with allergic reactions to both E coli and Erwinia asparaginase, or in those for whom Erwinia asparaginase was not available, polyethylene glycol-asparaginase (Oncospar) 2500 units /m2 per week.
Vincristine – 2 mg/m2 IV, except for weeks 7–9 and 17–19 when given at 1.5 mg/m2; Methotrexate - 40 mg/m2 IV or IM; Doxorubicin 30 mg/m2 IV; High-dose cytarabine - 2 g/m2 IV every 12 hours for 4 doses; Cyclophosphamide - 300 mg/m2 IV; Cytarabine - 300 mg/m2 IV.
Triple intrathecal therapy – low-risk cases with CNS-1 status: weeks 7, 12, 17, 24, 32, 40, and 48; low-risk cases with CNS-2, traumatic lumbar punctures with blasts or leukocyte count ≥ 100 × 109/L: weeks 7, 12, 17, 24, 28, 32, 36, 40, 44, and 48; standard-risk cases: weeks 7, 12, 17, 24, 28, 32, 36, 40, 44 and 48; other standard-risk cases with leukocyte count ≥ 100 × 109/L, T-cell ALL with WBC ≥ 50 × 109/L, presence of Philadelphia chromosome, MLL rearrangement, hypodiploidy <45, or CNS-3 status: weeks 3, 7, 12, 17, 24, 28, 32, 36, 40, 44, 48, 56, 64, 72, 80, 88 and 96.
Continuation therapy
During initial continuation therapy (Table 1), low-risk cases received daily mercaptopurine and weekly methotrexate with pulses of mercaptopurine, dexamethasone and vincristine. Two reinduction treatments were given between weeks 7–9 and weeks 17–19. Standard-risk cases received weekly asparaginase and daily mercaptopurine with pulses of doxorubicin plus vincristine plus dexamethasone. They also received two reinduction treatments between weeks 7–9 and weeks 17–20.
For the remaining continuation therapy (Supplementary Table 1), low-risk patients received mercaptopurine and methotrexate, with pulses of dexamethasone, vincristine and mercaptopurine, and standard-risk patients received three rotating drug pairs (mercaptopurine plus methotrexate, cyclophosphamide plus cytarabine, and dexamethasone plus vincristine). Dosages of mercaptopurine and methotrexate were adjusted according to the tolerance, and thiopurine methyltransferase phenotype and genotypes.17 Total scheduled dosages of anthracyclines and cyclophosphamide were limited to 110 mg/m2 and 230 mg/m2, and 1 g/m2 and 4.6 g/m2, for low-risk and standard-risk patients, respectively. Continuation treatment lasted 120 weeks in girls and 146 weeks in boys.
CNS-directed therapy
Intrathecal cytarabine was instilled following diagnostic lumbar puncture and triple intrathecal chemotherapy was given for all subsequent treatments (Table 1). Depending on the presenting features and the CNS status, low-risk patients received 13 to 18, and standard-risk patients 16 to 25, intrathecal treatments.
Allogeneic hematopoietic stem-cell transplantation
This procedure was an option for patients with high-risk leukemia (whose early treatment was identical to that for standard-risk patients). Reintensification therapy (Supplementary Table 2) was given to maximize MRD reduction before transplantation. The median time to transplantation after remission induction was 4.1 months (range, 2 to 12 months).
STATISTICAL ANALYSIS
All analyses were pre-specified in the protocol. To assess the effect of omitting prophylactic cranial irradiation, we compared the continuous complete remission rate after 1 year of continuation therapy of the subset of patients who met our previous criteria for prophylactic cranial irradiation at 1 year to that of historical controls who received irradiation,3,13 using an unstratified Mantel-Haenszel test.
Event-free survival and overall survival distributions were compared with the Mantel-Haenszel test. The Cox proportional hazards model was used to identify independent prognostic factors without using any variable selection methods. The cumulative incidence of isolated CNS or any CNS relapse (isolated plus combined), as well as other adverse events, were constructed by the method of Kalbfleisch and Prentice, and compared using Gray’s test. Fine and Gray’s model and the weighted logistic regression model18 were used to identify independent factors for prognosis and toxicities, respectively.
The database on January 5, 2009 was used for analysis; 97% of the survivors had been seen within 1 year. The median follow-up time was 4.0 years (range, 1.2 to 8.4 years). All reported P-values are 2-sided and not adjusted for multiple tests.
RESULTS
Presenting characteristics of the 498 evaluable patients are summarized in Table 2. Median age at diagnosis was 5.3 years (range, 1.0 to 18.9 years) and median leukocyte count was 11.7 × 109/L (range, 0.4 to 1014 × 109/L). We had increased proportions of T-cell ALL (15.3%) or t(1;19)[TCF3-PBX1] (5.8%) cases, owing to the overrepresentation of African-American patients relative to other series.19 Based on MRD measurements successfully done on all patients, we reclassified the risk status of 58 patients: 30 from low to standard, 6 from low to high, and 22 from standard to high.
TABLE 2.
Treatment outcome according to selected clinical and biologic features
| % 5-year event-free survival (SE) | % 5-year overall survival (SE) | |||||
|---|---|---|---|---|---|---|
| Features | No. of patients | P-value | P-value | |||
| Randomization arms | ||||||
| 4 - hour group | 177 | 88.2 (4.2) | 0.22 | 95.0 (2.7) | 0.20 | |
| 24 - hour group | 180 | 85.6 (4.6) | 94.0 (2.9) | |||
| Not randomized* | 141 | 82.4 (6.8) | 91.2 (4.9) | |||
| Risk Group | ||||||
| Low | 239 | 95.4 (2.6) | <0.001 | 98.7 (1.3) | <0.001 | |
| Standard | 217 | 82.4 (4.5) | 92.5 (3.0) | |||
| High | 42 | 47.2 (15.3) | 67.9 (12.8) | |||
| NCI risk group (B-cell precursor ALL) | ||||||
| Standard | 258 | 89.7 (3.7) | 0.01 | 97.7 (1.7) | 0.002 | |
| High | 164 | 82.4 (5.2) | 89.7 (4.0) | |||
| NCI risk group (T-cell ALL) | ||||||
| NCI Standard | 16 | 73.9 (15.4) | 0.71 | 93.8 (8.9) | 0.44 | |
| NCI High | 60 | 79.6 (8.7) | 86.0 (7.6) | |||
| Sex | ||||||
| Male | 279 | 83.5 (4.1) | 0.16 | 93.6 (2.4) | 0.64 | |
| Female | 219 | 88.8 (4.3) | 93.3 (3.1) | |||
| Age | ||||||
| 1 to 10 years | 372 | 87.8 (3.1) | 0.005 | 96.7 (1.6) | <0.001 | |
| >10 years | 126 | 79.1 (6.4) | 83.8 (5.5) | |||
| Leukocyte count | ||||||
| <10 × 109/L | 227 | 86.8 (4.1) | 0.1 | 93.7 (2.8) | 0.33 | |
| 10 to 49 × 109/L | 144 | 85.9 (5.4) | 95.9 (3.0) | |||
| 50 to 99 × 109/L | 64 | 83.9 (7.9) | 91.0 (6.0) | |||
| 100 to 300 × 109/L | 44 | 86.1 (8.9) | 90.4 (7.5) | |||
| ≥300 × 109/L | 19 | 73.3 (18.9) | 89.2 (12.0) | |||
| Race | ||||||
| White | 340 | 87.8 (3.2) | 0.02 | 94.8 (2.0) | 0.23 | |
| African American | 79 | 77.8 (8.2) | 88.3 (6.2) | |||
| Hispanic | 60 | 74.2 (13.3) | 89.1 (8.9) | |||
| Asian or Others | 19 | 100 (0.0) | 100 (0.0) | |||
| Immunophenotype | ||||||
| B-cell precursor | 422 | 86.9 (3.1) | <0.001 | 94.6 (1.9) | 0.013 | |
| T-cell | 76 | 78.4 (7.8) | 87.6 (6.3) | |||
| CNS status† | ||||||
| CNS-1 | 359 | 87.5 (3.1) | <0.001 | 94.6 (2.0) | 0.02 | |
| CNS-2 | 102 | 86.2 (7.5) | 95.1 (4.3) | |||
| Traumatic with blasts | 28 | 81.4 (14.3) | 81.9 (13.2) | |||
| CNS-3 | 9 | 43.2 (23.0) | 71.1 (22.1) | |||
| DNA Index†† | ||||||
| ≥ 1.16 | 121 | 91.2 (4.6) | 0.02 | 96.2 (3.0) | 0.09 | |
| <1.16 | 377 | 83.8 (3.5) | 92.8 (2.5) | |||
| t(9;22)[ BCR-ABL1] | ||||||
| Present | 10 | 40.0 (21.9) | <0.001 | 48.0 (20.0) | <0.001 | |
| Absent | 488 | 86.7 (2.8) | 94.5 (1.8) | |||
| t(1;19)[TCF3-PBX1] | ||||||
| Present | 28 | 85.9 (11.4) | 0.99 | 100 (0.0) | 0.18 | |
| Absent | 470 | 85.6 (3.0) | 93.1 (2.0) | |||
| t(12;21)[ETV6-RUNX1] | ||||||
| Present | 96 | 97.6 (3.2) | 0.004 | 98.9 (2.0) | 0.03 | |
| Absent | 402 | 83.0 (3.3) | 92.2 (2.3) | |||
| t(4;11)[MLL-AF4] | ||||||
| Present | 3 | 100 (0.0) | 0.59 | 100 (0.0) | 0.70 | |
| Absent | 495 | 85.6 (2.9) | 93.5 (1.9) | |||
| Minimal residual diseases on day 19 induction | ||||||
| < 0.01% | 198 | 92.6 (3.2) | <0.001 | 97.5 (1.9) | <0.001 | |
| 0.01% to 0.99% | 192 | 87.8 (5.1) | 93.8 (3.2) | |||
| 1% to 4.99% | 43 | 77.4 (10.6) | 96.8 (4.5) | |||
| ≥ 5% | 55 | 56.8 (14.1) | 78.1(10.6) | |||
| Minimal residual disease on remission date‡ | ||||||
| < 0.01% | 392 | 89.6 (2.9) | <0.001 | 94.5 (1.9) | <0.001 | |
| 0.01% to 0.99% | 77 | 79.5 (8.0) | 90.9 (5.4) | |||
| 1% to 4.99% | 14 | 38.1 (21.2) | 71.4 (27.0) | |||
| ≥ 5% | 9 | 55.6 (26.2) | 87.5 (13.8) | |||
The reasons for not being randomized included parental refusal (n=62), completion of accrual for the pharmacologic study aims (n=21), the presence of mediastinal mass or respiratory distress (n=17), physician decision (n=17), Down syndrome (n=12), organ dysfunction or infection (n=11), and unknown reason (n=1).
CNS-1: no detectable blast cells in cerebrospinal fluid sample; CNS-2: <5 leukocytes/µL with blast cells in an atraumatic sample; CNS-3: ≥ 5 leukocytes/µL with blast cells in an atraumatic sample or the presence of a cranial nerve palsy; and traumatic lumbar puncture with blasts (≥ 10 erythrocytes/µL with blasts.11
Ratio of DNA content as measured by flow cytometry in leukemic cells versus normal diploid G0/G1 cells.
Flow cytometry, clone-specific PCR or both were used to study minimal residual disease (PCR studies were done only in patients with B-lineage ALL). 482 of 492 patients (98%) were studied by flow cytometry and 403 of 492 (82%) by PCR. Both studies yielded virtually identical results. In the few cases with discrepant results, we used the highest MRD value. The two methods could be applied to study 491 of 492 patients (99.8%) of the patients. The single patient with no available immunophenotypic or gene-rearrangement marker had a MLL-AF9 fusion transcript and was monitored by RT-PCR.
TREATMENT OUTCOME
Outcomes were similar for patients treated in the two centers. Of the 498 patients, 492 (98.8%) entered complete remission (low-risk, 99.6%; standard-risk, 99.5%, and high-risk, 90.4%). Induction failures were due to 2 fatal infections and 4 refractory leukemias. Three of the latter four patients remain in remission for 4.6, 4.6 and 6.1 years after allogeneic transplantation.
Thirty-three patients underwent allogeneic transplantation (9 from matched-sibling, 17 matched-unrelated and 7 haploidentical donors) 2 to 12 months after remission induction (median, 4.1 months). Transplantation was performed in 6 patients for t(9;22)[BCR-ABL1] ALL, 21 for MRD ≥ 1% at the end of induction, 5 for persistent MRD on week 16 post-remission and 1 for near-haploidy. Twenty-four patients remain alive in remission, 7 died of complications, and 2 relapsed.
There were 17 hematologic, 11 isolated CNS, 4 combined CNS and hematologic, and 1 testicular relapses, 1 secondary myelodysplastic syndrome, and 12 deaths in remission (including those after transplantation). The 5-year cumulative risk (95% confidence interval) of isolated CNS relapse was 2.7% (1.1% to 4.3%), any CNS relapse was 3.9% (1.9% to 5.9%) (Fig.1), and any relapse was 9.3% (6.0% to 12.6%). Pertinent features of the 11 patients with isolated CNS relapse are summarized in Supplementary Table 3. Notably, all 11 patients remain alive in second remission for 0.4 to 5.5 years (median, 2.5 years); 10 have been off therapy (3 after transplantation) for 1 month to 4.1 years (median, 2.0 years). The 5-year event-free survival and overall survival estimates were 85.6% (79.9% to 91.3%) and 93.5% (89.8% to 97.2%) for all 498 patients (Fig. 1). All 30 low-risk patients reclassified into the standard-risk group remain free of relapse.
Figure 1.
Overall survival, event-free survival, cumulative risk of any CNS relapse (combined plus isolated), and cumulative risk of isolated CNS relapse for all patients. The 5-year and 8-year rates are means ± standard error.
Among the 71 patients who met our previous criteria for receiving prophylactic CNS irradiation, two had bone marrow relapse, one CNS relapse, and one remission death. Their continuous complete remission after 1 year of continuation therapy was significantly better than that of the 56 historical controls (P=0.04):3,13 the 5-year rate was 90.8% (76% to 100%) versus 73.0% (61.2% to 84.8%) (Supplementary Fig. 1); the relative risk was 0.34 (0.11 to 1.02).
PROGNOSTIC FACTORS
Table 2 shows treatment outcome by selected features. Only CNS-3 status or traumatic lumbar puncture with blasts and MRD ≥ 1% at the end of induction were independently associated with poorer event-free survival (Table 3). Features independently associated with isolated CNS relapse included T-cell ALL, African-American race, the t(1;19)[TCF3-PBX1] and any CNS involvement (Table 3).
TABLE 3.
Independent prognostic factors for event-free survival, overall survival, and isolated CNS relapse
| All Patients | B-cell precursor ALL | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Hazard ratio | 95% CI | P-value | Hazard ratio | 95% CI | P-value | |||||
| Total | Adverse Events | Total | Adverse Events | |||||||
| Event-free survival | ||||||||||
| Minimal residual disease ≥ 1% on remission date | 23 | 11 | 5.3 | 2.5 to 11.3 | <0.001 | 15 | 8 | 8.7 | 3.5 to 21.7 | <0.001 |
| Others | 469 | 39 | 1.0 | ----- | ----- | 403 | 27 | 1.0 | ----- | ----- |
| CNS-3 or traumatic with blasts | 37 | 9 | 2.5 | 1.2 to 5.2 | 0.02 | 26 | 4 | 1.8 | 0.6 to 5.4 | 0.29 |
| Others | 461 | 43 | 1.0 | ----- | ----- | 396 | 32 | 1.0 | ----- | ----- |
| Age > 10 years | 126 | 21 | 1.5 | 0.8 to 2.8 | 0.16 | 98 | 17 | 2.1 | 1.1 to 4.3 | 0.04 |
| Others | 372 | 31 | 1.0 | ----- | ----- | 324 | 19 | 1.0 | ----- | ----- |
| Overall survival | ||||||||||
| Age >10 years | 126 | 17 | 3.8 | 1.7 to 8.3 | 0.001 | 98 | 14 | 8.6 | 3.0 to 24.2 | <0.001 |
| Others | 372 | 11 | 1.0 | ----- | ----- | 324 | 5 | 1.0 | ----- | ----- |
| t(9;22)[ BCR-ABL1] | 10 | 3 | 4.7 | 1.3 to 16.7 | 0.02 | 10 | 3 | 4.0 | 1.1 to 14.2 | 0.04 |
| Others | 488 | 25 | 1.0 | ----- | ----- | 412 | 16 | 1.0 | ----- | ----- |
| CNS-3 or traumatic with blasts | 37 | 6 | 2.6 | 1.0 to 6.5 | 0.05 | 26 | 3 | 2.3 | 0.6 to 8.1 | 0.20 |
| Others | 461 | 22 | 1.0 | ----- | ----- | 396 | 16 | 1.0 | ----- | ----- |
| T-cell | 76 | 9 | 2.1 | 0.9 to 5.0 | 0.07 | ----- | ----- | ----- | ----- | ----- |
| B-cell precursor | 422 | 19 | 1.0 | ----- | ----- | ----- | ----- | ----- | ----- | ----- |
| Isolated CNS relapse | ||||||||||
| T-cell | 74 | 6 | 7.7 | 1.4 to 43 | 0.02 | ----- | ----- | ----- | ----- | ----- |
| B-cell precursor | 418 | 5 | 1.0 | ----- | ----- | ----- | ----- | ----- | ----- | ----- |
| African American | 79 | 5 | 3.9 | 1.6 to 14 | 0.04 | 63 | 4 | 9.5 | 1.2 to 75 | 0.03 |
| Others | 413 | 6 | 1.0 | ----- | ----- | 355 | 1 | 1.0 | ||
| t(1;19)[TCF3-PBX1] | 28 | 3 | 15 | 3.1 to 73 | 0.001 | 28 | 3 | 11.7 | 2.3 to 59 | 0.003 |
| Others | 464 | 8 | 1.0 | ----- | ----- | 390 | 2 | |||
| CNS-1 | 358 | 3 | 1.0 | ----- | 0.005 | 317 | 2 | 1.0 | 0.8 to 20 | 0.1 |
| Others CNS status* | 134 | 8 | 6.4 | 1.7 to 23 | ----- | 101 | 3 | 4.0 | ||
any CNS involvement (CNS-2, CNS-3 or traumatic lumbar puncture with blasts)
In B-cell precursor ALL, the 5-year cumulative risk of isolated CNS relapse was 14.1% [8.0%] among cases with the t(1;19)[TCF3-PBX1] versus 0.8% [0.6%] among all other patients; and was 8.6% [4.2%] among African-American versus 0.4% [0.4%] among other patients.
TOXICITY
Table 4 summarizes the most relevant toxicities. The cumulative risk of toxic death during chemotherapy was 1.4% (0.4% to 2.4%). T-cell cases had a higher risk of seizures than B-cell precursor cases. Osteonecrosis, thrombosis and hyperglycemia occurred more often in the standard- and high-risk arms, which featured higher doses of dexamethasone and asparaginase, than in the low-risk arm. Age >10 years was independently associated with an increased risk of severe infections, osteonecrosis, hyperglycemia, and thrombosis.
TABLE 4.
Summary of selected toxicities
| Toxicity | No. of Patients | % 3-year cumulative risk (SE) | P-value | |
|---|---|---|---|---|
| Seizures (grade 2, 3 or 4)* | ||||
| All patients | 22 | 4.7 (1.0) | ||
| standard - or high-risk group | 14 | 5.8 (1.5) | } | 0.19 |
| low-risk group | 8 | 3.6 (1.3) | ||
| Severe infection (grade 4 or 5)† | ||||
| All patients | 23 | 4.8 (1.0) | ||
| standard - or high-risk group | 8 | 3.4 (1.2) | } | 0.18 |
| low-risk group | 13 | 6.4 (1.7) | ||
| Disseminated fungal infection | ||||
| All patients | 25 | 5.5 (1.1) | ||
| standard - or high-risk group | 13 | 5.8 (1.6) | } | 0.84 |
| low-risk group | 12 | 5.3 (1.5) | ||
| Allergic reactions to L-asparaginase (grade 2, 3 or 4) | ||||
| All patients | 198 | 41.2 (2.3) | ||
| standard - or high-risk group | 85 | 34.3 (3.1) | } | 0.10 |
| low-risk group | 113 | 47.6 (3.3) | ||
| Osteonecrosis (grade 3 or 4)‡ | ||||
| All patients | 32 | 8.8 (1.6) | ||
| standard - or high-risk group | 28 | 15.5 (2.8) | } | <0.001 |
| low-risk group | 4 | 2.4 (1.3) | ||
| Thrombosis (grade 2, 3 or 4)§ | ||||
| All patients | 36 | 7.5 (1.2) | ||
| standard - or high-risk group | 31 | 12.9 (2.2) | } | <0.001 |
| low-risk group | 5 | 2.1 (0.9) | ||
| Hyperglycemia (grade 3 or 4) ¥ | ||||
| All patients | 41 | 8.5 (1.3) | ||
| standard - or high-risk group | 32 | 13.2 (2.2) | } | <0.001 |
| low-risk group | 9 | 3.8 (1.2) | ||
Seizures occurred during remission induction in 6 patients, consolidation therapy in 5, reinduction treatment in 1, and continuation therapy in 9, and after transplantation in 1. T-cell cases had a higher cumulative risk of seizures than B-cell precursor cases (P=0.02; 9.6% [2.7% to 16.5%] versus 3.8% [1.8% to 5.8%] at 3 years]. A grade 3 leukoencephalopathy developed in a child after therapeutic cranial irradiation for CNS relapse.
Two patients died of Bacillus cereus sepsis during remission induction, one of typhlitis during consolidation treatment, two of bacterial sepsis and one of hepatic failure during reinduction, and one of bacterial sepsis during continuation therapy. Age >10 years was independently associated with an increased cumulative risk of severe infections (P=0.005, 7.5% [2.8% to 12.2%] versus 3.8% [1.6% to 6.0%] at 3 years),
Age >10 years was independently associated with an increased cumulative risk of osteonecrosis (P<0.0001; 30.1% [18.9% to 41.3%] versus 2.6% [0.6% to 4.6%]), Of the 32 cases with grade 3 or 4 osteonecrosis, 14 underwent core decompression, with subsequent arthroplasty in six and joint resurfacing procedures in two.
Age >10 years was independently associated with an increased cumulative risk of thrombosis (P=0.03; 16.3% [9.4% to 23.2%] versus 4.7% [2.5% to 6.9%]).
Age >10 years was independently associated with an increased cumulative risk of hyperglycemia (P<0.0001; 21.7% [14.3% to 29.2%] versus 4.2% [2.0% to 6.4%]).
DISCUSSION
Total XV study achieved a 5-year survival rate of 93.5%, which is superior to results of all major studies reported to date.1–3,13,20–27 This outcome also compares favorably with the recent result (87.5%) reported by the Surveillance, End Results, and Epidemiology Program for patients less than 15 years old treated between 2000 and 2004.28 The 5-year survival rates of 97.7% for low-risk and 89.7% for standard-risk B-cell precursor ALL were especially gratifying. Importantly, our study demonstrated that with intensification of systemic and intrathecal chemotherapy, prophylactic cranial irradiation can be totally omitted without compromising overall survival. Indeed, the 71 patients who met previous criteria to receive prophylactic cranial irradiation fared significantly better than the 56 historical controls.3,13 Because etoposide and irradiation were given only to the small subgroup of patients who underwent transplantation, we expect a very low rate of therapy-induced cancers. Extrapolating from the long-term results of reported studies,1–3,20–26 we predict that no more than 4% of patients might develop major adverse events 5 to 10 years after diagnosis, and this treatment protocol should yield a 10-year survival rate, and perhaps a cure rate, of 90%.5
We attribute this improved outcome to the incorporation of effective treatment components from earlier clinical trials1–3,13,20–26 coupled with a stringent risk classification based on MRD and dose adjustments based on the pharmacogenetic and pharmacodynamic characteristics. We used increased dosage of methotrexate in T-cell or t(1;19)[TCF3-PBX1] ALL because these blasts accumulate methotrexate polyglutamates less avidly than blasts of other subtypes.29 Indeed, high-dose methotrexate has improved outcome in T-cell ALL,30 whereas relatively lower doses appear adequate for low-risk B-cell precursor ALL.31 We targeted methotrexate dose individually, a strategy that improved outcome in our previous trial,31 and used two courses of reinduction treatment which have been shown to benefit patients with intermediate-risk ALL.32
Intensified asparaginase treatment was used because this approach has improved outcome in previous trials.2,33 For patients with hypersensitivity reactions to native E coli asparaginase, Erwinia asparaginase was substituted at high and frequent doses because an inadequate dose of this drug led to inferior outcome.34 Because we used a relatively high dose of mercaptopurine, we prospectively identified patients with inherited deficiency of thiopurine-S-methyltransferase and lowered mercaptopurine dosage accordingly to avoid toxicities.17 We regularly monitored levels of thioguanine nucleotides to assess mercaptopurine treatment and administered methotrexate intravenously to ensure compliance. Dosages of mercaptopurine and methotrexate were adjusted to the limits of tolerance but not overzealously to avoid undue interruptions of therapy.27,35 Dexamethasone was used post-remission because it has yielded better outcome than prednisone or prednisolone.36,37
We relied on high-dose methotrexate, intensive asparaginase, dexamethasone, and optimal intrathecal therapy to control CNS leukemia. Intrathecal therapy was intensified in patients with blasts in the CSF, even from traumatic lumbar puncture, which has been associated with poor outcome, 38–41 Special precautions12 were taken to decrease the rate of traumatic lumbar punctures from 24% in previous studies42 to 8% in this study. We gave intrathecal therapy in a large volume (8 mL or more, depending on age), and kept patients in the prone position for at least 60 minutes after intrathecal therapy,12 which improves intraventricular distribution.43,44 Finally, we used triple intrathecal therapy, which proved more effective than intrathecal methotrexate for CNS control.45 With these measures, the isolated CNS relapse rate was 2.7%, well within the 1.5% to 4.5% range in clinical trials that used prophylactic cranial irradiation.1–3,13,20–26,37 Only 1 of our 9 patients with CNS-3 status developed CNS relapse. Although a remarkably low rate (0.6%) of isolated CNS relapse was achieved in one study, approximately two-thirds of those patients received cranial irradiation.2
Our improved therapy has abolished most historically important prognostic factors, including leukocyte count. Even though high levels of MRD (i.e., ≥ 1%) at the end of induction were still associated with a poor outcome, use of this measure for risk-directed therapy has undoubtedly contributed to the improved results in this study. Indeed, while patients with MRD levels between 0.01% and 0.99% had a cumulative risk of relapse of 43% in our previous trials,15 those with the same levels had a 5-year event-free survival rate of 79.5% in this study. Despite intensive treatment, vigilant supportive care resulted in a toxic death rate of only 1.4%. Rates of disseminated fungal infection and thrombosis were relatively high but no patient died of these complications. Children over 10 years of age were more likely than younger patients to develop severe infection, osteonecrosis, thrombosis, and hyperglycemia, a finding that may be explained by slower clearance of dexamethasone in older patients.46
The complete omission of prophylactic cranial irradiation allowed us to clearly identify risk factors for CNS relapse: any CNS involvement, the t(1;19)[TCF3-PBX1] and T-cell ALL. We would argue against using prophylactic cranial irradiation even in patients with these features because approximately 90% would have received unnecessary irradiation. Further, since CNS and hematologic relapses are competing events, eradication of occult CNS leukemia by cranial irradiation alone may allow overt systemic relapse from residual leukemia in the bone marrow or other sites, which is more difficult to salvage. Indeed, in one study, triple intrathecal treatment reduced the frequency of CNS relapse compared with intrathecal methotrexate, but was associated with increased bone marrow and testicular relapse rates, leading to a poor overall survival.45 Moreover, patients with isolated CNS relapse who have not received prophylactic irradiation are highly curable, especially if their bone marrow is not involved, as assessed by MRD determination.47,48 In this regard, all of our 11 patients with an isolated CNS relapse remain in second remission, and most are likely cured after one course of therapeutic irradiation. For patients at high risk of CNS relapse, we have further intensified early intrathecal treatments in our ongoing clinical trial.
Supplementary Material
Acknowledgments
This work was supported by grants (CA21765, CA51001, CA60419, CA78224, CA36401, and GM61393) from the National Institutes of Health, by American Cancer Society F.M. Kirby Clinical Research Professorship, and by the American Lebanese Syrian Associated Charities (ALSAC).
We are indebted to Julie Groff for assistance with the figure, Jeana Cromer, Emily Baum and Linda Holloway for data management, Dr. Sheila Shurtleff for molecular analysis, our clinical and laboratory colleagues, and many patients and parents who participated in the research program.
Disclosure
Dr. Pui reports receiving lecture fees from Enzon Pharmaceuticals; Dr. Cheng, receiving consulting fees and grant support from Enzon Pharmaceuticals, Dr. Jeha, receiving research support from Genzyme, Sanofi-Aventis, and EUSA Pharma; Dr. Downing, relationship with the American Society for Investigative Pathology as a Council Member; and Dr. Relling, research support from Enzon Pharmaceutical and consulting fees from Genome Explorations. No other potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Möricke A, Reiter A, Zimmermann M, et al. Risk-adjusted therapy of acute lymphoblastic leukemia can decrease treatment burden and improve survival: treatment results of 2169 unselected pediatric and adolescent patients enrolled in the trial ALL-BFM 96. Blood. 2008;111:4477–4489. doi: 10.1182/blood-2007-09-112920. [DOI] [PubMed] [Google Scholar]
- 2.Moghrabi A, Levy DE, Asselin B, et al. Results of the Dana-Farber Cancer Institute ALL Consortium Protocol 95–01 for children with acute lymphoblastic leukemia. Blood. 2007;109:896–904. doi: 10.1182/blood-2006-06-027714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pui CH, Sandlund JT, Pei D, et al. Improved outcome for children with acute lymphoblastic leukemia: results of Total Therapy Study XIIIB at St. Jude Children’s Research Hospital. Blood. 2004;104:2690–2696. doi: 10.1182/blood-2004-04-1616. [DOI] [PubMed] [Google Scholar]
- 4.Oeffinger KC, Mertesn AC, Sklar CA, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006;355:1572–1582. doi: 10.1056/NEJMsa060185. [DOI] [PubMed] [Google Scholar]
- 5.Pui CH, Cheng C, Leung W, et al. Extended follow-up of long-term survivors of childhood acute lymphoblastic leukemia. N Engl J Med. 2003;349:640–649. doi: 10.1056/NEJMoa035091. [DOI] [PubMed] [Google Scholar]
- 6.Hijiya N, Hudson MM, Lensing S, et al. Cumulative incidence of secondary neoplasms as a first event after childhood acute lymphoblastic leukemia. JAMA. 2007;297:1207–1215. doi: 10.1001/jama.297.11.1207. [DOI] [PubMed] [Google Scholar]
- 7.Geenen MM, Cardous-Ubbink MC, Kremer LCM, et al. Medical assessment of adverse health outcomes in long-term survivors of childhood cancer. JAMA. 2007;297:2705–2715. doi: 10.1001/jama.297.24.2705. [DOI] [PubMed] [Google Scholar]
- 8.Waber DP, Turek J, Catania L, et al. Neuropsychological outcomes from a randomized trial of triple intrathecal chemotherapy compared with 18 Gy cranial radiation as CNS treatment in acute lymphoblastic leukemia: findings from Dana-Farber Cancer Institute ALL Consortium Protocol 95–01. J Clin Oncol. 2007;25:4914–4921. doi: 10.1200/JCO.2007.10.8464. [DOI] [PubMed] [Google Scholar]
- 9.Vilmer E, Suciu S, Ferster A, et al. Long-term results of three randomized trials (58831, 58832, 58881) in childhood acute lymphoblastic leukemia: a CLCG-EORTC report. Leukemia. 2000;14:2257–2266. doi: 10.1038/sj.leu.2401960. [DOI] [PubMed] [Google Scholar]
- 10.Manera R, Ramirez I, Mullins J, Pinkel D. Pilot studies of species-specific chemotherapy of childhood acute lymphoblastic leukemia using genotype and immunophenotype. Leukemia. 2000;14:1354–1361. doi: 10.1038/sj.leu.2401835. [DOI] [PubMed] [Google Scholar]
- 11.Conter V, Schrappe M, Aricó M, et al. Role of cranial radiotherapy for childhood T-cell acute lymphoblastic leukemia with high WBC count and good response to prednisone. J Clin Oncol. 1997;15:2786–2791. doi: 10.1200/JCO.1997.15.8.2786. [DOI] [PubMed] [Google Scholar]
- 12.Pui CH, Howard SC. Current management and challenges of malignant disease in the CNS in paediatric leukaemia. Lancet Oncol. 2008;9:257–268. doi: 10.1016/S1470-2045(08)70070-6. [DOI] [PubMed] [Google Scholar]
- 13.Pui CH, Mahmoud HH, Rivera GK, et al. Early intensification chemotherapy virtually eliminates central nervous system relapse in children with acute lymphoblastic leukemia. Blood. 1998;92:411–415. [PubMed] [Google Scholar]
- 14.Pui CH, Evans WE. Acute lymphoblastic leukemia. N Engl J Med. 1998;339:605–615. doi: 10.1056/NEJM199808273390907. [DOI] [PubMed] [Google Scholar]
- 15.Coustan-Smith E, Sancho J, Hancock ML, et al. Clinical importance of minimal residual disease in childhood acute lymphoblastic leukemia. Blood. 2000;96:2691–2696. [PubMed] [Google Scholar]
- 16.Neale GAM, Coutsan-Smith E, Stow P, et al. Comparative analysis of polymerase chain reaction and flow cytometry for the detection of minimal residual disease in childhood acute lymphoblastic leukemia. Leukemia. 2004;18:934–938. doi: 10.1038/sj.leu.2403348. [DOI] [PubMed] [Google Scholar]
- 17.Evans WE, Relling MV. Moving towards individualized medicine with pharmacogenomics. Nature. 2004;429:464–468. doi: 10.1038/nature02626. [DOI] [PubMed] [Google Scholar]
- 18.Kishi S, Cheng C, French D, et al. Ancestry and pharmacogenetics of antileukemic drug toxicity. Blood. 2007;109:4151–4157. doi: 10.1182/blood-2006-10-054528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pui CH, Sandlund JT, Pei D, et al. Results of therapy for acute lymphoblastic leukemia in black and white children. JAMA. 2003;290:2001–2007. doi: 10.1001/jama.290.15.2001. [DOI] [PubMed] [Google Scholar]
- 20.Conter V, Arico M, Valsecchi MG, et al. Long-term results of the Italian Association of Pediatric Hematology and Oncology (AIEOP) acute lymphoblastic leukemia studies, 1982–1995. Leukemia. 2000;14:2196–2204. doi: 10.1038/sj.leu.2401963. [DOI] [PubMed] [Google Scholar]
- 21.Gaynon PS, Trigg ME, Heerema NA, et al. Children’s Cancer Group trials in childhood acute lymphoblastic leukemia: 1983–1995. Leukemia. 2000;14:2223–2233. doi: 10.1038/sj.leu.2401939. [DOI] [PubMed] [Google Scholar]
- 22.Harms DO, Göbel U, Spaar HJ, et al. Thioguanine offers no advantage over mercaptopurine in maintenance treatment of childhood ALL: results of the randomized trial COALL-92. Blood. 2003;102:2736–2740. doi: 10.1182/blood-2002-08-2372. [DOI] [PubMed] [Google Scholar]
- 23.Kamps WA, Bokkerink JP, Hakvoort-Cammel FG, et al. BFM-oriented treatment for children with acute lymphoblastic leukemia without cranial irradiation and treatment reduction for standard risk patients: results of DCLSG protocol ALL-8 (1991–1996) Leukemia. 2002;16:1099–1111. doi: 10.1038/sj.leu.2402489. [DOI] [PubMed] [Google Scholar]
- 24.Gustafsson G, Schmiegelow K, Forestier E, et al. Improving outcome through two decades in childhood ALL in the Nordic countries: the impact of high-dose methotrexate in the reduction of central nervous system irradiation. Nordic Society of Pediatric Haematology and Oncology (NOPHO) Leukemia. 2000;14:2267–2275. doi: 10.1038/sj.leu.2401961. [DOI] [PubMed] [Google Scholar]
- 25.Hill FGH, Richards S, Gibson B, et al. Successful treatment without cranial radiotherapy of children receiving intensified chemotherapy for acute lymphoblastic leukaemia: results of the risk-stratified randomized central nervous system treatment trial MRC UKALL XI (ISRC TN 16757172) Br J Haematol. 2004;124:33–46. doi: 10.1046/j.1365-2141.2003.04738.x. [DOI] [PubMed] [Google Scholar]
- 26.Pui CH, Boyett JM, Rivera GK, et al. Long-term results of Total Therapy studies of 11, 12 and 13A for childhood acute lymphoblastic leukemia at St. Jude Children’s Research Hospital. Leukemia. 2000;14:2286–2294. doi: 10.1038/sj.leu.2401938. [DOI] [PubMed] [Google Scholar]
- 27.Pui CH, Evans WE. Treatment of acute lymphoblastic leukemia. N Engl J Med. 2006;354:166–178. doi: 10.1056/NEJMra052603. [DOI] [PubMed] [Google Scholar]
- 28.Pulte D, Gondos A, Brenner H. Trends in 5- and 10-year survival after diagnosis with childhood hematologic malignancies in the United States, 1999–2004. J Natl Cancer Inst. 2008;100:1301–1309. doi: 10.1093/jnci/djn276. [DOI] [PubMed] [Google Scholar]
- 29.Kager L, Cheok M, Yang W, et al. Folate pathway gene expression differs in subtypes of acute lymphoblastic leukemia and influences methotrexate pharmacodynamics. J Clin Invest. 2005;115:110–117. doi: 10.1172/JCI22477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schrappe M, Reiter A, Ludwig W-D, et al. Improved outcome in childhood acute lymphoblastic leukemia despite reduced use of anthracyclines and cranial radiotherapy: results of trial ALL-BFM 90. Blood. 2000;95:3310–3322. [PubMed] [Google Scholar]
- 31.Evans WE, Relling MV, Rodman JH, Crom WR, Boyett JM, Pui CH. Conventional compared with individualized chemotherapy for childhood acute lymphoblastic leukemia. N Engl J Med. 1998;338:499–505. doi: 10.1056/NEJM199802193380803. [DOI] [PubMed] [Google Scholar]
- 32.Lange BJ, Bostrom BC, Cherlow JM, et al. Double-delayed intensification improves event-free survival for children with intermediate-risk acute lymphoblastic leukemia: a report from the Children’s Cancer Group. Blood. 2002;99:825–833. doi: 10.1182/blood.v99.3.825. [DOI] [PubMed] [Google Scholar]
- 33.Pession A, Valsecchi MG, Masera G, et al. Long-term results of a randomized trial on extended use of high dose of L-asparaginase for standard risk childhood acute lymphoblastic leukemia. J Clin Oncol. 2005;23:7161–7167. doi: 10.1200/JCO.2005.11.411. [DOI] [PubMed] [Google Scholar]
- 34.Duval M, Suciu S, Ferster A, et al. Comparison of Escherichia coli-asparaginase with Erwinia-asparaginase in the treatment of childhood lymphoid malignancies: results of a randomized European Organization for Research and Treatment of Cancer—Children’s Leukemia Group phase 3 trial. Blood. 2002;99:2734–2739. doi: 10.1182/blood.v99.8.2734. [DOI] [PubMed] [Google Scholar]
- 35.Relling MV, Hancock ML, Boyett JM, et al. Prognostic importance of 6-mercaptopurine dose intensity in acute lymphoblastic leukemia. Blood. 1999;93:2817–2823. [PubMed] [Google Scholar]
- 36.Bostrom BC, Sensel MR, Sather HN, et al. Dexamethasone versus prednisone and daily oral versus weekly intravenous mercaptopurine for patients with standard-risk acute lymphoblastic leukemia: a report from the Children’s Cancer Group. Blood. 2003;101:3809–3817. doi: 10.1182/blood-2002-08-2454. [DOI] [PubMed] [Google Scholar]
- 37.Mitchell CD, Richards SM, Kinsey SE, et al. Benefit of dexamethasone compared with prednisolone for childhood acute lymphoblastic leukaemia: results of the UK Medical Research Council ALL 97 randomized trial. Br J Haematol. 2005;129:734–745. doi: 10.1111/j.1365-2141.2005.05509.x. [DOI] [PubMed] [Google Scholar]
- 38.Mahmoud HH, Rivera GK, Hancock ML, et al. Low leukocyte counts with blast cells in cerebrospinal fluid of children with newly diagnosed acute lymphoblastic leukemia. N Engl J Med. 1993;329:314–319. doi: 10.1056/NEJM199307293290504. [DOI] [PubMed] [Google Scholar]
- 39.Gajjar A, Harrison PL, Sandlund JT, et al. Traumatic lumbar puncture at diagnosis adversely affects outcome in childhood acute lymphoblastic leukemia. Blood. 2000;96:3381–3384. [PubMed] [Google Scholar]
- 40.te Loo DM, Kamps WA, Does-van den Berg AV, van Wering ER, de Graaf SSN. Prognostic significance of blasts in the cerebrospinal fluid without pleiocytosis or a traumatic lumbar puncture in children with acute lymphoblastic leukemia: the experience of the Dutch Childhood Oncology Group. J Clin Oncol. 2006;24:2332–2336. doi: 10.1200/JCO.2005.03.9727. [DOI] [PubMed] [Google Scholar]
- 41.Bürger B, Zimmermann M, Mann G, et al. Diagnostic cerebrospinal fluid examination in children with acute lymphoblastic leukemia: significance of low leukocyte counts with blasts or traumatic lumbar puncture. J Clin Oncol. 2003;21:184–188. doi: 10.1200/JCO.2003.04.096. [DOI] [PubMed] [Google Scholar]
- 42.Howard SC, Gajjar AJ, Cheng C, et al. Risk factors for traumatic lumbar puncture in children with acute lymphoblastic leukemia. JAMA. 2002;288:2001–2007. doi: 10.1001/jama.288.16.2001. [DOI] [PubMed] [Google Scholar]
- 43.Blaney SM, Poplack DG, Godwin K, McCully CL, Murphy R, Balis FM. Effect of body position on ventricular CSF methotrexate concentration following intralumbar administration. J Clin Oncol. 1995;13:177–179. doi: 10.1200/JCO.1995.13.1.177. [DOI] [PubMed] [Google Scholar]
- 44.Salzer W, Widemann B, McCully C, Adamson PC, Balis FM. Effect of probenecid on ventricular cerebrospinal fluid methotrexate pharmacokinetics after intralumbar administration in nonhuman primates. Cancer Chemother Pharmacol. 2001;48:235–240. doi: 10.1007/s002800100328. [DOI] [PubMed] [Google Scholar]
- 45.Matloub Y, Lindemulder S, Gaynon PS, et al. Intrathecal triple therapy decreases central nervous system relapse but fails to improve event-free survival when compared to intrathecal methotrexate: results of the Children’s Cancer Group (CCG) 1952 study for standard-risk acute lymphoblastic leukemia. A report from the Children’s Oncology Group. Blood. 2006;108:1165–1173. doi: 10.1182/blood-2005-12-011809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang L, Panetta JC, Vai X, et al. Asparaginase may influence dexamethasone pharmacokinetics in acute lymphoblastic leukemia. J Clin Oncol. 2008;26:1932–1939. doi: 10.1200/JCO.2007.13.8404. [DOI] [PubMed] [Google Scholar]
- 47.Barredo JC, Devidas M, Lauer SJ, et al. Isolated CNS relapse of acute lymphoblastic leukemia treated with intensive systemic chemotherapy and delayed CNS radiation: a Pediatric Oncology Group Study. J Clin Oncol. 2006;24:3142–3149. doi: 10.1200/JCO.2005.03.3373. [DOI] [PubMed] [Google Scholar]
- 48.Hagedorn N, Acquaviva C, Fronkova E, et al. Submicroscopic bone marrow involvement in isolated extramedullary relapses in childhood acute lymphoblastic leukemia: a more precise definition of “isolated” and its possible clinical implications, a collaborative study of the Resistant Disease Committee of the International BFM study group. Blood. 2007;110:4022–4029. doi: 10.1182/blood-2007-04-082040. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.