Abstract
Developmental exposure to endocrine-disrupting compounds is hypothesized to adversely affect female reproductive physiology by interfering with the organization of the hypothalamic-pituitary-gonadal axis. Here, we compared the effects of neonatal exposure to two environmentally relevant doses of the plastics component bisphenol-A (BPA; 50 μg/kg and 50 mg/kg) with the ESR1 (formerly known as ERalpha)-selective agonist 4,4′,4″-(4-propyl-[1H]pyrazole-1,3,5-triyl)trisphenol (PPT; 1 mg/kg) on the development of the female rat hypothalamus and ovary. An oil vehicle and estradiol benzoate (EB; 25 μg) were used as negative and positive controls. Exposure to EB, PPT, or the low dose of BPA advanced pubertal onset. A total of 67% of females exposed to the high BPA dose were acyclic by 15 wk after vaginal opening compared with 14% of those exposed to the low BPA dose, all of the EB- and PPT-treated females, and none of the control animals. Ovaries from the EB-treated females were undersized and showed no evidence of folliculogenesis, whereas ovaries from the PPT-treated females were characterized by large antral-like follicles, which did not appear to support ovulation. Severity of deficits within the BPA-treated groups increased with dose and included large antral-like follicles and lower numbers of corpora lutea. Sexual receptivity, examined after ovariectomy and hormone replacement, was normal in all groups except those neonatally exposed to EB. FOS induction in hypothalamic gonadotropic (GnRH) neurons after hormone priming was impaired in the EB- and PPT-treated groups but neither of the BPA-treated groups. Our data suggest that BPA disrupts ovarian development but not the ability of GnRH neurons to respond to steroid-positive feedback.
Keywords: AVPV, corpora lutea, development, disruption, endocrine disruptors, ERα, ESR1, estradiol, estradiol receptor, estrogen, estrogen receptor, GnRH, gonad, hypothalamus, lordosis, neuroendocrinology, ovary, PPT, puberty
Neonatal exposure to bisphenol-A induces early puberty, anestrus, and ovarian malformations but does not defeminize the hypothalamus in the rat.
INTRODUCTION
Bisphenol-A (BPA) initially entered commercial development in the 1930s as a synthetic estrogen [1] but is now used primarily in the production of polycarbonate plastic products, epoxy resins, and the linings of soda and soup cans. The U.S. Centers for Disease Control recently estimated that nearly all Americans have detectable levels of BPA in their bodies and that children have higher levels than adults [2, 3]. Infants in neonatal intensive care units may have notably high exposure to BPA, presumably from its use in medical devices [4]. Newborns can also be exposed through lactational transfer [5]. Fetal exposure is also highly likely because relatively high levels in umbilical cord blood and fetal plasma indicate that BPA fails to bind to the estrogen-sequestering protein alpha-fetoprotein and can cross the placenta [6, 7]. In multiple species, exposure to BPA during the prenatal or postnatal period has been shown to have an impact on female reproductive physiology, including the timing of pubertal onset and the induction of an early, persistent estrus [8–10]. Presumably, BPA produces its effects by interfering with one or both of the primary forms of the estrogen receptor (ER; ESR1 or ESR2, formerly known as ERα and ERβ) within the hypothalamic-pituitary-gonadal (HPG) axis, but it is not well understood through which ER BPA primarily acts in vivo. In the present study, we took a comparative approach and examined the effects of neonatal exposure to BPA or an ESR1-selective agonist on the structure and function of the adult hypothalamus and ovary in female rats. We have shown previously that exposure to the ESR1-specific agonist 4,4′,4″-(4-propyl-[1H]-pyrazole-1,3,5-triyl)trisphenol (PPT) but not the ESR2-specific agonist diarylpropionitrile (DPN) during the neonatal period can defeminize the female rat hypothalamus and impair steroid-positive feedback [11]. Here, we sought to determine whether neonatal exposure to BPA could similarly impact hypothalamic organization, a result which would then implicate a mechanistic role for ESR1 in endocrine disruption by BPA in the female hypothalamus.
Within the HPG axis, reproductive maturation and function are coordinated by the release of gonadotropin-releasing hormone (GnRH) [12, 13]. The neural components of the HPG axis that regulate GnRH secretion are sexually differentiated by endogenous gonadal hormones, primarily estradiol, through a series of gestational, prenatal, and perinatal critical periods [14]. The GnRH release is regulated through feedback effects of gonadal steroids. In both males and females, GnRH secretion is suppressed by steroid-negative feedback, the signal for which is thought to arise from the arcuate nucleus of the hypothalamus [15, 16]. In females, however, GnRH release is augmented once per cycle by estrogens. This positive feedback potentiates the surge in GnRH and, subsequently, luteinizing hormone (LH) that precedes ovulation [17]. In rats, this process is now thought to be mediated within the anterior ventral periventricular nucleus (AVPV) of the hypothalamus [15, 16, 18].
In rodents, sexual differentiation of this feedback circuit takes place primarily during the neonatal period and has been shown to be particularly sensitive to disruption by hormones or hormone-like compounds [11, 19, 20]. It is well established that the administration of steroid hormones, including testosterone or estradiol benzoate (EB), during the neonatal critical period can defeminize the female rodent brain, whereas castration can effectively prevent defeminization of the male rodent brain [21–23]. Thus, in males castrated as neonates, the potential for estrogen to evoke a GnRH surge is preserved whereas, conversely, in females neonatally exposed to estrogens, this capacity is diminished or lost. Exposure to sex steroids or endocrine disrupting compounds (EDCs) during the neonatal critical period can also advance puberty and alter ovarian morphology [15, 24–26]. The present experiments targeted this neonatal critical window, which corresponds to approximately the third trimester of gestation in humans [27]. In a prior study, we demonstrated that neonatal administration of the phytoestrogens genistein (GEN) and equol (EQ) can advance puberty and induce an early, persistent estrus [11]. This disruption of female reproductive physiology was accompanied by impaired GnRH activation (as measured by the colocalization of GnRH and FOS immunoreactivity), suggesting that perturbation of the hormone-dependent organization of steroid-positive feedback circuits within the hypothalamus was a potential mechanism for the effects on pubertal timing and ovarian cyclicity. Animals neonatally exposed to the ESR1-specific agonist PPT but not the ESR2-specific agonist DPN also displayed an early, persistent estrus and inhibited FOS induction in GnRH neurons after hormone priming, demonstrating that ESR1 plays a critical role in the defeminization of the hypothalamus by estrogens. By extension, ESR1 might play a mechanistic role in the disruption of hypothalamic organization by EDCs, such as BPA. Reduced colocalization of GnRH and FOS immunoreactivity after neonatal exposure to BPA would potentially indicate that BPA can interact with ESR1 in the hypothalamus during development, a finding that would provide key information about the possible mechanism(s) by which BPA affects the organization of the female reproductive system.
Developmental exposure to estrogenic EDCs can induce additional effects elsewhere in the HPG axis, such as the ovary [10, 28, 29]. Previous studies have shown that perinatal exposure to GEN can lead to altered ovarian differentiation characterized by multioocyte follicles and reduced fertility in mice [25]. In contrast, relatively little is known about how exposure to BPA at doses considered relevant for human risk assessment and over the neonatal critical period alone can affect ovarian development and function. Therefore, the present study had two main goals: 1) to determine whether advanced puberty and impaired estrus function in female rats after neonatal exposure to one of two relatively low doses of BPA were associated with impaired sexual receptivity and FOS induction in hypothalamic GnRH neurons and 2) to characterize ovarian morphology in the adult after neonatal BPA exposure.
Because ERs are expressed in all three HPG components, not just the hypothalamus, disruption by BPA could potentially occur anywhere within it, including the pituitary, the ovary, the brain, or any combination of the three. It is not well understood whether ovarian deficits after neonatal exposure to endocrine disruptors result from direct effects in the ovary itself, disrupted organization of the hypothalamus, both of these mechanisms, or some other potential mechanism, perhaps at the level of the pituitary. Although the present experiments were not designed to explore this critical knowledge gap directly, we again compared the effects of PPT and BPA as a first step in the exploration of this key issue. A recent study by Nakamura and colleagues reported that ovaries collected from mice neonatally exposed to PPT, but not the ESR2 agonist DPN, at 13 wk of age lack corpora lutea (CLs), a condition that is accompanied by persistent estrus [30]. This finding suggests that ESR1 may have an important mechanistic role in endocrine disruption of ovarian function. We have also reported persistent estrus in female rats after neonatal exposure to PPT [11] but did not explore ovarian morphology in that prior study. Thus, in the present study, we sought to determine whether neonatal exposure to BPA or PPT induces similar ovarian malformations.
Multiple laboratories have now demonstrated that BPA can impair female reproductive function at doses equivalent to or below those that regulatory bodies have deemed to be “safe” for human exposure, but the question of whether or not there are significant “low-dose effects” of BPA remains controversial. At the time the present studies were undertaken, the lowest observed adverse effect level (LOAEL) for BPA established by the U.S. Environmental Protection Agency (EPA) was 50 mg/kg body weight (bw) per day, and the EPA reference dose (the dose considered “safe” for human exposure) was 50 μg/kg bw per day. For our experiments, we used the EPA LOAEL as our high dose and the EPA reference dose as our low dose. The synthetic estrogen EB, at a dose sufficient to masculinize the hypothalamus, advance pubertal onset, and prevent the onset of regular estrous cycles, was used as a positive control [31–33].
Animals were exposed to either vehicle, EB, PPT, low-dose BPA (50 μg/kg bw), or high-dose BPA (50 mg/kg bw) in the first 4 days of life via subcutaneous injection. Injection has recently been demonstrated to produce equivalent or lower plasma BPA levels in neonatal rodents than oral administration, thus making injection an appropriate route of exposure when considering potential effects in humans [34, 35]. After neonatal exposure, females were then monitored for changes in reproductive physiology, sexual receptivity, GnRH activation, and ovarian morphology. We hypothesized that BPA would adversely affect all endpoints examined in a dose-dependent manner.
MATERIALS AND METHODS
Animals and Neonatal Treatment
Animal care, maintenance, and surgery were conducted in accordance with the applicable portions of the Animal Welfare Act and the U.S. Department of Health and Human Services “Guide for the Care and use of Laboratory Animals” and were approved by the North Carolina State University (NCSU) Institutional Animal Care and Use Committee. Female pups were obtained from cross-fostered litters born to timed pregnant Long Evans rats (n = 10; Charles River Laboratories). Cross-fostering was done to minimize potential litter effects. Each litter contained a mixture of animals (12 maximum), only two of which were genetically related to each other. All dams were individually housed in a humidity- and temperature-controlled room with a 12-h light cycle (lights on from 0700 to 1900 h) at 23°C and 50% average relative humidity at the Biological Resource Facility at NCSU and were maintained on a semipurified, phytoestrogen-free diet ad libitum for the duration of the experiment (AIN-93G; Test Diet, Richmond, IN).
Beginning on the day of birth, the female pups were cross-fostered and subcutaneously (sc) injected with vehicle (0.05 ml), EB (25 μg; Sigma, St. Louis, MO), 50 μg/kg bw BPA (low-dose BPA; Sigma), 50 mg/kg bw bisphenol-A (high-dose BPA), or the ESR1 agonist PPT (1 mg/kg bw; Tocris Biosciences, Ellisville, MS). PPT is a selective agonist for ESR1, with a 400-fold preference for ESR1 and minimal binding to ESR2 [36]. The EB was used as a positive control and administered at a dose previously established to masculinize the hypothalamus and eliminate GnRH activation in response to hormone priming [31–33]. All compounds were dissolved in ethanol and then sesame oil at a ratio of 10% EtOH and 90% oil, as we have done previously [11, 37]. The vehicle was also prepared with this ratio. We have found this vehicle to cause less skin irritation than the alternative vehicle, DMSO. The animals (n = 10–12 per group) received injections daily from the day of birth, defined as Postnatal Day 0 (PND 0), through PND 3 (four injections total).
All pups were weaned into same-sex littermate pairs on PND 22, ear tagged, and maintained on a reverse light schedule (lights off from 1000 to 2200 h) for the remainder of the experiment. Upon weaning, a cohort of animals (n = 8–9 per group) were checked daily for day of vaginal opening (DOV). The primary mechanism for pubertal onset remains unclear [38, 39], but in rats, DOV is a hallmark of puberty and was therefore used as the physiological indicator of puberty. Monitoring of the estrous cycle by vaginal lavage [40] commenced approximately 2 wk after vaginal opening and occurred every 24 h for 4 days (longer if needed) every other week, for 13 wk. We opted to sample every other week to reduce handling stress and minimize the potential for inducing a pseudopregnancy. All animals observed to have stopped cycling (defined by the failure to sequentially progress through proestrus, estrus, and diestrus) were resampled (for 3–5 days) 2 wk later to confirm that the failure to cycle was not due to a pseudopregnancy.
Females were ovariectomized (OVX) under isoflurane anesthesia (completed during 3 wk beginning on Postnatal Day 148) and allowed 2 wk to recover to provide adequate time for endogenous hormone levels to diminish. At the time of OVX, ovaries were removed and fixed in 10% formalin for 24 h at 4°C, then postfixed in 70% ethanol and stored at 4°C until processing.
Testing for Sexual Receptivity
To induce sexual receptivity and test for lordosis behavior, the OVX females were injected sc with 10 μg of EB at 0900 h, followed 48 h later by an sc injection of 500 μg of progesterone (same vehicle as above) and paired with vigorous males as described previously [41–43]. Lordosis quotient (LQ) was calculated by dividing the number of lordosis responses in each trial (10 min) by the number of mount attempts, then multiplying the result by 100. In two pairings, the male made no attempt to mount the female. These trials were not included in the analysis.
Ovarian Histology
Ovaries were coded at collection and were subsequently processed at the National Institute of Environmental Health Sciences (NIEHS). For each animal, both ovaries were paraffin embedded side by side and sliced into 6-μm sections. Sections were slide mounted (Superfrost Plus; Fisher, Pittsburgh, PA), and two slides per animal were deparaffinized, stained with hematoxylin-eosin, coverslipped, and qualitatively examined for histological abnormalities at NIEHS. The slides and the remaining uncut tissue were then returned to NCSU for the quantification of CLs. Corpus luteum counts are a reliable indicator of successful ovulation [24]. Although the morphological appearance of CLs changes across the cycle, the overall number does not [44], eliminating the need to control for cycle stage at OVX. For each animal, CLs were counted on two slides (each containing one section from each ovary) and averaged to yield a final value for statistical analysis.
Brain Collection and Immunohistochemistry
Nineteen days after the behavioral tests were completed, all animals were again sequentially administered EB and progesterone and were killed by transcardial perfusion with 4% paraformaldehyde 6–8 h after the progesterone injection, as we have done in past experiments [11]. It is well established that this is the point at which GnRH activity, after sequential steroid hormone administration, is maximal [45, 46]. Brains were removed, postfixed, cryoprotected, and stored at −80°C (14), then sliced into 35-μm coronal sections and divided into four series of free-floating alternating sections, one of which was used for the present study. For each animal, one set of coronal sections comprising the organum vasculosum of the lamina terminalis (OVLT) through the caudal border of the AVPV were immunolabeled for GnRH and FOS using immunohistochemistry methods described in detail elsewhere [11, 47]. The GnRH and FOS were detected using a cocktail of primary antibodies directed against GnRH (raised in rabbit; 1:20 000; generously gifted by Dr. Robert Benoit, McGill University Health Center, Montreal, QC, Canada) and FOS (raised in goat; 1:250; SC-52–6; Santa Cruz Biotechnology), followed by the secondary antibodies Alexa-Fluor donkey anti-rabbit 488 and Alexa-Fluor donkey anti-goat 568, each at 1:200. After secondary antibody incubation, sections were rinsed, mounted onto slides (Superfrost Plus; Fisher, Pittsburgh, PA), and coverslipped using a glycerol-based mountant (50% glycerol in 4 M sodium bicarbonate).
Quantification of GnRH and FOS Immunoreactivity
The GnRH/FOS double-immunofluorescent label was visualized and quantified as described in our prior publications [11, 48]. Briefly, GnRH and FOS immunostaining was observed to be consistent and distributed both laterally and dorsally to the third ventricle throughout the OVLT, as has been described previously [49, 50]. Thus, two to three midlevel sections per animal were selected for analysis. Only those sections showing consistent GnRH and FOS immunostaining were used. They were photographed with a Retiga 1800 monochrome camera attached to a Leica 5000DM microscope fitted with 20× and 40× objective lenses and filter cubes for Cy3 and fluorescein isothiocyanate. Anatomical identification was made using a brain atlas [51]. The images of each label (GnRH and FOS) were then merged using the MCID Elite Image Analysis (Interfocus Imaging Ltd., Cambridge, England) software package. Cells immunostained for GnRH only and cells immunolabeled for both GnRH and FOS were then hand counted by an individual blind to the treatment groups and were verified by a second independent observer.
Statistical Analysis
The DOV, LQ, CL number, and percentage of GnRH and FOS colabeled cells were compared across treatment groups by one-way ANOVA with treatment as a factor and were followed up with Fisher least significant difference posthoc tests for individual comparisons (SYSTAT; Systat Software Inc., Chicago, IL). As anticipated [49, 50], the number of GnRH neurons counted did not significantly differ between groups (data not shown). In all cases, comparisons were two tailed, and the significance level was set at P ≤ 0.05.
RESULTS
Age at Vaginal Opening
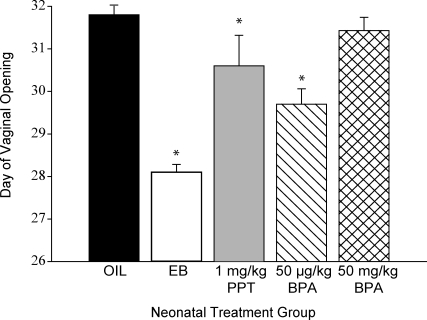
There was a significant effect of treatment on DOV (F[5,50] = 18.34; P ≤ 0.001). Compared with the oil-treated controls (n = 9), DOV was significantly advanced by neonatal exposure to EB (n = 11; P ≤ 0.001), PPT (n = 8; P ≤ 0.04), and the low dose of BPA (50 μg/kg bw; n = 8; P ≤ 0.01; Fig. 1). The high dose of BPA (50 mg/kg bw; n = 14), however, had no significant effect on DOV.
FIG. 1.
The DOV was significantly advanced by neonatal (PND 0 to PND 3) administration of EB and the low (50 μg/kg bw) dose of BPA but not the high (50 mg/kg bw) dose of BPA or the ESR1-selective agonist PPT compared with the control animals (means ± SEM; *P ≤ 0.04).
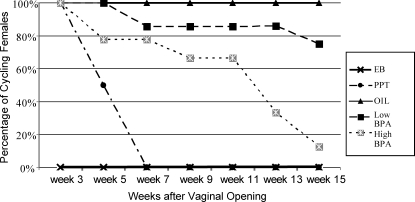
Estrous Cycle Data
Beginning approximately 2 wk after DOV, regularity of the estrous cycle was assessed every 24 h for 4 days (longer if needed) every other week, for 13 wk by vaginal lavage in a cohort of animals. Regular 4-day estrous cycles commenced in all treatment groups except the group neonatally exposed to EB (Fig. 2). As expected [31–33], all of the EB-treated females (n = 8) displayed persistent estrus or diestrus and failed to enter a normal estrous cycle. By 7 wk after DOV, all (n = 8) neonatally treated PPT females had entered a state of persistent estrus or diestrus. By 15 wk after DOV, only 33% of the females exposed to the high dose of BPA (n = 9) were still cycling, compared with 86% of the females exposed to the low dose of BPA (n = 8).
FIG. 2.
Regular estrous cycles commenced in all groups except the group neonatally exposed to EB. The percentage of females within each treatment group displaying a regular estrous cycle diminished over time in all groups except for the control group. By 15 wk after vaginal opening, only 33% of animals exposed to the low (50 μg/kg bw) dose of BPA neonatally still displayed a regular estrous cycle compared with 86% of the animals exposed to the high (50 mg/kg bw) dose of BPA.
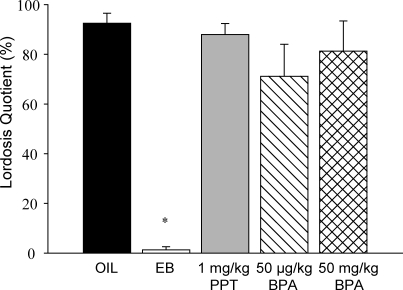
Sexual Behavior
Sexual receptivity was assessed after ovariectomy and hormone replacement. There was a significant main effect of treatment on LQ (F[4,35] = 17.046; P ≤ 0.001; Fig. 3); however, this effect was exclusively due to the abolition of sexual behavior in the group neonatally treated with EB (n = 9; P ≤ 0.001). There was a trend for suppressed LQ in the group neonatally exposed to low-dose BPA, but this effect did not reach statistical significance (n = 7; P = 0.157). Both the PPT and high-dose BPA exposures had no appreciable effect on LQ. These observations are consistent with what we have observed in past studies [43].
FIG. 3.
Female sexual receptivity after hormone priming was not significantly affected by neonatal exposure to any of the compounds except for EB (means ± SEM; *P ≤ 0.001).
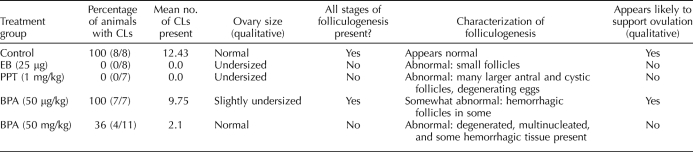
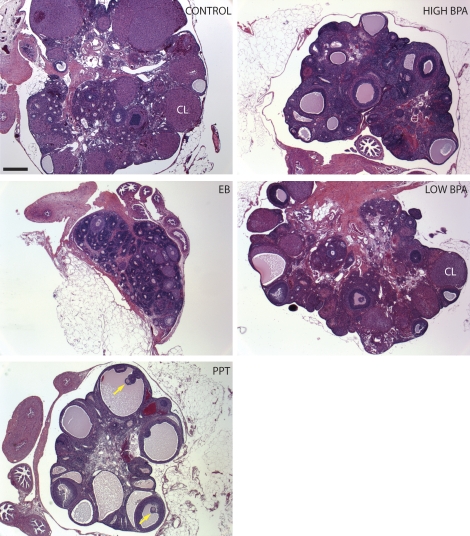
Ovarian Morphology
Both a qualitative and quantitative analysis of ovarian morphology was conducted (Table 1). Qualitative histological comparison between groups revealed that only the negative control group showed consistently healthy ovaries characterized by all stages of follicular development and the presence of numerous healthy CLs (Fig. 4). All other groups displayed some degree of abnormalities, including hemorrhagic follicles, large antral-like follicles that did not seem to support ovulation, multioocyte follicles, and ovarian cysts. The type and severity of abnormalities present differed between treatment groups (Table 1). Females neonatally exposed to EB as our positive control group (Fig. 4) displayed the most severe effects, qualitatively characterized by undersized ovaries, no CLs, and no signs of folliculogenesis. Females neonatally exposed to the ESR1-selective agonist PPT also displayed abnormal ovarian development, but not in the same way that the EB females did. Ovaries from PPT-treated females (Fig. 4) were also undersized and lacked CLs but were characterized by numerous large antral-like follicles that did not appear to support ovulation. Some contained oocytes (Fig. 4, yellow arrows), but most did not. Females neonatally exposed to the high dose of BPA (50 mg/kg) displayed abnormal folliculogenesis and follicle degeneration, with a few follicles containing multinucleated cells. Ovaries from females exposed to the low dose of BPA (50 μg/kg) displayed all stages of follicular development; however, a few animals had hemorrhagic follicles. Ovaries from both BPA-treated groups also contained a number of large antral-like follicles that were similar in appearance to those seen in the PPT-treated animals and were structurally consistent with ovarian cysts. All of the PPT-treated animals and most of the high-dose BPA-treated animals were acyclic at the time of ovariectomy, and CLs were not typically observed in these animals. Thus, it is unlikely that these follicles progressed to ovulation. Because the number of antral follicles changes across the estrus cycle and we did not stage our animals at OVX, we did not compare the mean number of antral-like follicles across treatment groups.
TABLE 1.
Summary of ovarian morphology.
FIG. 4.
Ovarian morphology was distinctly different across treatment groups. Females neonatally exposed to EB had very small ovaries with no clear signs of active oogenesis or ovulation. Ovaries from females neonatally exposed to PPT were characterized by numerous large antral-like follicles, only some of which contained oocytes (yellow arrows). Similar structures were observed in both of the BPA-treated groups but not to the degree seen in females neonatally exposed to PPT. Generally, ovaries from the high-dose (50 mg/kg bw) BPA treatment group more closely resembled those from the PPT treatment group than the EB treatment group. Bar = 500 μm.
Quantitative analysis of ovulatory capacity was made by counting CLs (Table 1). Corpora lutea appear after the release of an egg from the ovary and are a reliable and quantitative indicator of successful ovulation, regardless of cycle stage [24, 43, 52]. There was a significant treatment effect on the number of CLs present (F[4,35] = 22.484; P ≤ 0.001). Compared with the control females, a significant decrease in CL number was observed in the females neonatally exposed to EB (n = 8; P < 0.001) or PPT (n = 7; P < 0.001), neither of which displayed any CLs. The number of CLs was also significantly lower in the high-dose BPA-treated females (n = 10; P < 0.001), with only 3 of 10 containing any CLs. The mean number of CLs also trended lower in the low-dose-treated BPA females compared with the control group, but this effect did not reach statistical significance (n = 8; P < 0.36). This was largely because whereas most animals in the low-dose BPA group had fewer CLs than the vehicle-treated control animals, two animals had nearly twice as many. Both of these animals were still cyclic, but not staged, at the time of ovariectomy.
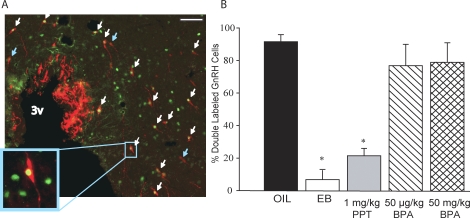
Colocalization of GnRH and FOS in the OVLT
Hormone treatment was repeated approximately 2 wk after sexual testing was completed, and animals were killed 6 h after the progesterone injection. This is the point at which FOS expression in GnRH neurons (an indicator of GnRH activation) is known to be maximal [45, 46]. The GnRH activation was assessed by quantifying the percentage of GnRH and FOS colabeled OVLT neurons. There was a significant effect of treatment (F[4,29] = 17.331; P ≤ 0.001). Hormone administration successfully induced FOS immunoreactivity (-ir) in 93% of GnRH neurons of the oil-treated control females (n = 7; Fig. 5). In contrast, 6% of GnRH neurons in EB-treated females (n = 5; P < 0.001), and only 22% in PPT-treated females (n = 7; P < 0.001), were immunoreactive for FOS. This PPT effect is consistent with what we have reported in past studies [11]. FOS labeling within GnRH neurons was not significantly reduced in either of the BPA groups compared with the controls, suggesting that the sex-specific organization of the hypothalamus may not have been disrupted by neonatal BPA exposure at the doses used.
FIG. 5.
A) Immunolabeling of GnRH (red) and FOS (green) in the OVLT. Double-labeled cells are indicated by the white arrows, and single-labeled GnRH neurons are indicated by the blue arrows. The number of GnRH-immunopositive cells did not significantly differ among groups. Original magnification ×20 (A) and ×63 (inset); bar = 40 μm. B) The percentage of GnRH cells that were colabeled with FOS was significantly lower in animals neonatally exposed to PPT or EB but not significantly affected by neonatal exposure to either the low (50 μg/kg bw) or high (50 mg/kg bw) doses of BPA (means ± SEM; P ≤ 0.001; *P ≤ 0.001). 3v, third ventricle.
DISCUSSION
The accelerated pubertal timing, premature anestrus, and ovarian malformations induced by neonatal exposure to BPA could result from disrupted organization anywhere within the HPG axis, including the hypothalamus, ovary, and/or pituitary gland. The exposure was specifically timed to target the hypothalamus. Our results do not support the hypothesis that BPA can defeminize the hypothalamus, a process in which, as we have shown previously [11], ESR1 appears to play a significant mechanistic role. Instead, GnRH neurons seem to retain the capacity to respond (by producing FOS) to hormone priming by estrogen and progesterone. These results suggest that steroid-positive feedback was not defeminized by BPA but do not rule out the possibility, however, that other signaling mechanisms on GnRH neurons could have been altered.
Effects through ESR1 (by PPT or other endocrine disruptors) on GnRH are most likely indirect, because ESR1 is not known to be present in GnRH neurons. Instead, disruption likely occurs within ESR1-containing neurons in the AVPV, the arcuate nucleus (ARC), or elsewhere, which send projections to GnRH neurons [23]. This may include the recently discovered population of neurons in the AVPV that express the peptide kisspeptin and send afferents to GnRH neurons [15, 16]. The vast majority of kisspeptin neurons in this region coexpress ESR1, and the administration of kisspeptin can induce early puberty in adolescent animals and generate a GnRH surge in ovariectomized animals [53, 54]. A recent study by Navarro et al. [55] found reductions in hypothalamic Kiss1 mRNA levels after neonatal BPA exposure at doses higher than those used here. We subsequently determined that the density of hypothalamic kisspeptin-immunoreactive fibers is reduced by the high, but not the low, dose of BPA used in the present study, and that the effect was more pronounced in the ARC than the AVPV [43]. Collectively, these observations support the hypothesis that signaling pathways on GnRH neurons may be altered by developmental exposure to BPA and that steroid-negative (rather than positive) feedback may be impaired.
Even if GnRH release following estrogen administration is normal, the subsequent release of LH from the anterior pituitary may not be. A new study by Fernandez and colleagues [56] targeted the critical period for pituitary differentiation (PND 13) in female rats. Levels of GnRH-induced LH released from pituitary cells in vivo and in vitro were lower than controls in BPA-treated animals. Additionally, BPA-treated animals showed increased GnRH pulse frequency, hypothesized to cause desensitization of the pituitary, thus leading to blunted LH secretion [56, 57]. Prepubertal exposure to BPA has also been shown to decrease LH pulse frequency and amplitude in gonadally intact ewes [58, 59]. Similarly, perinatal but not adult exposure to 1.2 mg/kg bw BPA decreased plasma LH levels in adult OVX mice, an observation that also indicates possible interference with hypothalamic organization and emphasizes that exposure sensitivity is heightened during critical developmental periods. Bisphenol-A has also been shown to reduce ERK activation, which may in turn affect GnRH receptor expression [60]. Reduced GnRH receptor expression in the pituitary could be a mechanism by which LH release is reduced while steroid-induced GnRH activation remains intact. Collectively, these prior results combined with the abnormalities seen in the present study could also be indicative of disrupted steroid-negative feedback.
Although it is still unclear by what mechanism it might occur, our results clearly demonstrate that ovarian cyclicity is compromised by a very brief, neonatal BPA exposure at doses at and above the current EPA reference dose for human exposure. Prior studies examining whether BPA can affect ovarian function have used equivalent or higher doses than those used here, and they have shown that the window of vulnerability may extend beyond the neonatal period [56, 61, 62]. For example, exposures to 10 mg/kg BPA on PNDs 15–18, 100 μg/kg BPA across PNDs 1–5, or 50 mg/kg BPA on Gestational Days 6–21 have all been shown to result in ovarian and vaginal malformations in mice [63–65], including the absence of CLs, cystic ovaries, endometrial hyperplasia, and lack of ESR1 expression in the vagina. Higher doses of BPA (1 or 4 mg per pup) have also been reported to decrease ovarian area occupied by CLs and multiple cystic follicles in rats [66]. Within that study, however, a dose of 250 μg per pup was not found to alter ovarian morphology, a finding which is inconsistent with our own, but the ovaries were collected approximately 6 wk after vaginal opening (earlier than was done in the present study), so it is possible that abnormalities following low-dose exposure could have manifested later. Although the low dose of BPA accelerated pubertal onset in the present study, most of these animals maintained a regular estrous cycle for 15 wk after DOV, whereas animals exposed to the high dose did not. Our results indicate that lower doses of neonatal BPA exposure may result in reduced ovulatory capacity, although the onset of irregular cycles may take somewhat longer to manifest. This type of effect has also been observed after neonatal low-dose exposure to the phytoestrogen GEN [24]. Therefore, it is important to observe animals for several weeks beyond pubertal onset when seeking to determine whether an EDC can affect ovarian function. The effect of low-dose BPA on ovarian cyclicity may be more robust if exposure comprises both the gestational and neonatal periods, a condition that is more consistent with human exposure, which is low and lifelong [6].
It has been hypothesized that neonatal exposure to EDCs enhances ovulation rate when animals are young, which then results in compromised fertility later in life and induces a premature reproductive senescence [24]. The intriguing observation that two females exposed to the low (50 μg/kg bw) dose of BPA in the present study had nearly twice as many CLs as control females whereas the rest had fewer is consistent with this hypothesis and requires further investigation. It is possible that among these animals, CL counts were different simply because they were at different points in their estrous cycle when the ovaries were collected. A recent study, however, found that although the morphologic features of CLs change across the cycle, the number of CLs does not [44].
Our results also indicate that lower rather than higher doses of BPA have the greatest potential to accelerate pubertal onset, a finding that is counterintuitive but consistent with what has been seen in other studies. An even lower dose (20 μg/kg) administered over Gestational Days 11–17 has also been shown to advance vaginal opening [67], demonstrating that perturbations of the hormonal milieu in other critical developmental windows besides the neonatal period have the potential to advance puberty. Conversely, higher doses of BPA typically fail to affect pubertal timing, or they delay rather than advance it [64]. The mechanism by which lower, but not higher, doses of BPA can advance puberty remains poorly understood. It has been hypothesized previously that BPA, like hormones, has a U-shaped or “nonmonotonic” dose-response curve [8, 68–70]. Our results are consistent with that hypothesis. The mechanism(s) by which this might occur have not been satisfactorily elucidated but could include stimulation of hormone receptors at low doses but downregulation of hormone receptors at higher doses. (For a critical discussion of nonmonotonic dose curves, see Vandenberg et al. [71].) It is important to note that although the effect of neonatal exposure to the low dose of BPA on DOV was significant, it was not as robust as neonatal exposure to EB. Neonatal exposure to the ESR1 agonist PPT was also not sufficient to advance pubertal onset to the same degree as EB. This could suggest that strong agonism of both ESR1 and ESR2 is necessary to evoke a maximal response.
It is also possible that BPA alters pubertal timing by an ER-independent mechanism. For example, bw at the time of vaginal opening may influence this endpoint, and could therefore be a confounding factor. Delayed pubertal onset after exposure to 500 mg/kg BPA via maternal dietary exposure during gestation and nursing was most pronounced in the lightest animals [72]. Other studies in rats and sheep have also found an effect of BPA on body weight at pubertal onset [59, 61]. Therefore, it could be that vaginal opening in our high-dose (50 mg/kg) animals was later than in our low-dose (50 μg/kg) animals because of a difference in bw. Unfortunately, this possibility was not taken into account; however, we did not note any obvious differences in bw at the time of vaginal opening. Regardless, our data suggest that exposure to BPA during a developmental window that corresponds to late gestation in humans, at levels relevant to human exposure, has the potential to accelerate pubertal onset. The specific mechanisms by which this occurs remain to be determined.
Malformations in the ovary after exposure to EDCs, including BPA, during development have been reported previously, but the mechanism(s) by which they might occur has not been well established [9]. For this aspect of the present study, the ESR1-selective agonist PPT was employed for comparative purposes. All groups except the control group showed some degree of abnormalities, the characteristics of which were distinctly different between groups. Malformations within the BPA females were dose dependent, with ovaries from the high-dose group showing the most significant adverse effects. Generally, the BPA ovaries more closely resembled those from the PPT than the EB group which, as expected from prior reports [73], were notably undersized (a qualitative assessment) and showed no sign of folliculogenesis. Unlike the EB group, ovaries from animals in the PPT and high-dose BPA groups were characterized by numerous antral-like cavities, most of which contained either a degenerating or no oocyte. In many cases, these cavities resembled cystic follicles, but some appeared to be large atretic follicles, particularly in the PPT animals (Fig. 4). This observation is consistent with a previous study that also described the presence of large, antral-like cavities in the ovaries of mice exposed to 250 μg/kg bw BPA in utero [74], and to a more recent study [75] that observed similar structures in cultured follicles directly exposed to BPA. It should be noted, however, that a different mechanism of action is likely involved in the cell culture study, because the ovarian malformations arose from acute rather than developmental exposure. Finally, none of the PPT females had CLs, an observation that is consistent with what has been reported previously in mice [30] and suggests that the PPT animals are anovulatory and fail to progress beyond the follicular phase. It appears that agonism of ESR1 during the rodent neonatal period can curtail the capacity of oogenesis to progress into the luteal phase.
Although the ovaries from the animals neonatally treated with PPT and the high dose of BPA share some similar characteristics, they do not necessarily indicate a mechanistic role for ESR1 in the emergence of the BPA-induced effects. Moreover, a mechanistic role for ESR2 in the disruption of ovarian function by BPA cannot be ruled out. Recent studies have reported that ESR2-deficient mice exposed gestationally to 400 ng/day BPA do not display the same abnormalities as BPA-exposed wild-type controls [76], leading the authors to conclude that BPA exerts its effects in the ovary via ESR2 [76, 77]. It is important to be mindful, however, that effects resulting from the elimination of ESR2 function across the lifespan may differ from those observed after selectively agonizing or silencing ESR2 during discrete time periods. We and others have shown that postnatal exposure to ESR2-specific agonists can also result in the premature loss of a regular estrous cycle, although not necessarily at the same rate as animals exposed to ESR1-specific agonists [11, 78]. Therefore, the loss of ovarian cyclicity appears to be possible after postnatal agonism of either of the two major ER subtypes. ESR1 is primarily expressed in the interstitial and thecal cells as early as PND 1, whereas ESR2, expressed in the granulosa cells, is not detectable on PND 1 but is present by PND 5 [79]. Thus, the BPA exposure in our study was sufficiently long enough for either ER subtype to play a mechanistic role. It is also possible that BPA is acting as an ESR 1 or ESR2 antagonist. Selective antagonists for ESR1 and ESR2 are only now becoming available, so it may soon be possible to directly test how ER-specific antagonism affects ovarian structure and function as part of future studies. These and other types of experiments are needed delineate the relative roles each ER subtype play in the organization and function of the HPG axis, including the ovary.
It is also possible that BPA action on ovarian development and HPG organization may not be limited to ERs. Bisphenol-A is thought to bind to the thyroid hormone receptor, androgen receptor, estrogen-related receptor, and the aryl hydrocarbon receptor [71, 80–82], and it may have direct or indirect actions on the ovary through these alternate pathways. For example, estrogen-related receptor gamma (ESRRG) and estrogen-related receptor alpha (ESRRA) expression have been found in human ovarian cells, with increased expression in ovarian cancer cells [83, 84]. Bisphenol-A can also bind to a membrane-bound form of the ER and a transmembrane ER called G protein-coupled receptor 30 (GPER, formerly called GPR30) [85–87]. Emerging evidence now indicates that epigenetic modifications, such as DNA methylation of transposable elements and cis-acting, imprinting regulatory elements, may also be a potential mechanism by which BPA and other endocrine disruptors affect reproductive function [88, 89]. The potential for BPA and other endocrine disruptors to modify the epigenome and the health consequences of those disruptions remain largely unexplored.
Interestingly, when hormone primed after ovariectomy, all of the animals except those treated with EB displayed normal sexual receptivity, regardless of whether or not they had lost their estrous cycle, demonstrating that the capacity to display sexual behavior may persist despite impaired reproductive physiology. This observation is consistent with what we have seen before following neonatal exposure to GEN, EQ, PPT, or DPN [11, 43]. Enhanced lordosis has been reported previously after gestational exposure to 40 μg/kg per day BPA [90] or a low (5 mg/kg) dose of the chlorinated pesticide chlordecone, a compound which is also classified as an estrogenic EDC [91]. Our observations are also consistent with a body of literature produced by Gorski [92], Dohler [93], and Yanase and Gorski [94] showing that lordosis behavior can persist after postnatal hormone manipulation, depending on dose and timing of administration. We have yet to determine whether or not these females would display normal sexual behavior if tested with ovaries in place and without hormone priming.
Here, we have shown that neonatal exposure to BPA at or below the LOAEL set by the EPA adversely affects pubertal timing and ovarian function. Our results are consistent with the conclusions of the National Toxicology Program [35], which stated that there is “some concern for adverse effects of developmental toxicity for fetuses, infants and children.” The National Toxicology Program also concluded that there is “minimal” concern for effects on puberty in females, largely because the mouse literature on this effect is inconsistent, and not enough information has been obtained from rat studies. Therefore, our study adds to the literature demonstrating an effect on sexual maturation in females. Bisphenol-A is known to cross the placenta and pass to infants by lactational transfer [5, 95, 96]. Blood and amniotic fluid samples obtained from pregnant women reveal that amniotic levels of BPA (8.3–8.7 ng/ml) can be even higher than fetal serum levels (1–2 ng/ml) [97–99]. Whether or not the levels of BPA obtained through maternal exposure in humans are sufficient to elicit reproductive deficits remains to be determined. However, as contamination levels and routes of exposure to both naturally occurring and synthetic EDCs differ across populations, determining exactly how they interfere with normal reproductive development warrants further exploration. Our finding that the capacity for GnRH neurons to produce FOS in response to hormone priming is apparently intact in female rats neonatally exposed to BPA suggests that defeminization of the hypothalamus may not be a mechanism by which developmental exposure to BPA can affect DOV, estrous cyclicity, and ovarian morphology. Further studies are needed to better characterize the specific mechanisms through which BPA and similar EDCs disrupt the organization of the HPG axis and impair female reproduction.
Acknowledgments
The authors thank Barbara (BJ) Welker and Linda Hester for their assistance with animal husbandry, as well as Jillian Mickens and Karina Todd for their help with the tissue slicing and labeling. We are also grateful to the pathologists at National Institute of Environmental Health Services for helping us with ovarian histology, and Dr. Robert Benoit (McGill University Health Center, Montreal, QC, Canada) for supplying us with the GnRH antibody. We appreciate John Vandenbergh for his constructive comments on the experimental design and Charles Patisaul for his critical reading of this manuscript.
Footnotes
1Supported by National Institute of Environmental Health Sciences grant R01 ES016001 to H.B.P.
REFERENCES
- Dodds EC, Lawson W.Synthetic estrogen agents without the phenanthrene nucleus. Nature 1936; 137: 996 [Google Scholar]
- Calafat AM, Kuklenyik Z, Reidy JA, Caudill SP, Ekong J, Needham LL.Urinary concentrations of bisphenol A and 4-nonylphenol in a human reference population. Environ Health Perspect 2005; 113: 391–395.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calafat AM, Ye X, Wong LY, Reidy JA, Needham LL.Exposure of the U.S. population to bisphenol A and 4-tertiary-octylphenol: 2003–2004. Environ Health Perspect 2008; 116: 39–44.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calafat AM, Weuve J, Ye X, Jia LT, Hu H, Ringer S, Huttner K, Hauser R.Exposure to Bisphenol A and other phenols in neonatal intensive care unit premature infants. Environ Health Perspect 2009; 117: 639–644.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsutsumi O.Assessment of human contamination of estrogenic endocrine-disrupting chemicals and their risk for human reproduction. J Steroid Biochem Mol Biol 2005; 93: 325–330.. [DOI] [PubMed] [Google Scholar]
- Vandenberg LN, Hauser R, Marcus M, Olea N, Welshons WV.Human exposure to bisphenol A (BPA). Reprod Toxicol 2007; 24: 139–177.. [DOI] [PubMed] [Google Scholar]
- Ikezuki Y, Tsutsumi O, Takai Y, Kamei Y, Taketani Y.Determination of bisphenol A concentrations in human biological fluids reveals significant early prenatal exposure. Hum Reprod 2002; 17: 2839–2841.. [DOI] [PubMed] [Google Scholar]
- vom Saal FS, Akingbemi BT, Belcher SM, Birnbaum LS, Crain DA, Eriksen M, Farabollini F, Guillette LJ, Hauser R, Heindel JJ, Ho SM, Hunt PA, et al. Chapel Hill bisphenol A expert panel consensus statement: integration of mechanisms, effects in animals and potential to impact human health at current levels of exposure. Reprod Toxicol 2007; 24: 131–138.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crain DA, Janssen SJ, Edwards TM, Heindel J, Ho SM, Hunt P, Iguchi T, Juul A, McLachlan JA, Schwartz J, Skakkebaek N, Soto AM, et al. Female reproductive disorders: the roles of endocrine-disrupting compounds and developmental timing. Fertil Steril 2008; 90: 911–940.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maffini MV, Rubin BS, Sonnenschein C, Soto AM.Endocrine disruptors and reproductive health: the case of bisphenol-A. Mol Cell Endocrinol 2006; 254–255: 179–186.. [DOI] [PubMed] [Google Scholar]
- Bateman HL, Patisaul HB.Disrupted female reproductive physiology following neonatal exposure to phytoestrogens or estrogen specific ligands is associated with decreased GnRH activation and kisspeptin fiber density in the hypothalamus. Neurotoxicology 2008; 29: 988–997.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkind-Hirsch K, King JC, Gerall AA, Arimura AA.The luteinizing hormone-releasing hormone (LHRH) system in normal and estrogenized neonatal rats. Brain Res Bull 1981; 7: 645–654.. [DOI] [PubMed] [Google Scholar]
- Gorski RA, Mennin SP, Kubo K.The neural and hormonal bases of the reproductive cycle of the rat. Adv Exp Med Biol 1975; 54: 115–153.. [DOI] [PubMed] [Google Scholar]
- Cooke B, Hegstrom CD, Villeneuve LS, Breedlove SM.Sexual differentiation of the vertebrate brain: principles and mechanisms. Front Neuroendocrinol 1998; 19: 323–362.. [DOI] [PubMed] [Google Scholar]
- Kauffman AS, Park JH, McPhie-Lalmansingh AA, Gottsch ML, Bodo C, Hohmann JG, Pavlova MN, Rohde AD, Clifton DK, Steiner RA, Rissman EF.The kisspeptin receptor GPR54 is required for sexual differentiation of the brain and behavior. J Neurosci 2007; 27: 8826–8835.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tena-Sempere MM.KiSS-1 and reproduction: focus on its role in the metabolic regulation of fertility. Neuroendocrinology 2006; 83: 275–281.. [DOI] [PubMed] [Google Scholar]
- Clarke IJ, Pompolo S.Synthesis and secretion of GnRH. Anim Reprod Sci 2005; 88: 29–55.. [DOI] [PubMed] [Google Scholar]
- Adachi S, Yamada S, Takatsu Y, Matsui H, Kinoshita M, Takase K, Sugiura H, Ohtaki T, Matsumoto H, Uenoyama Y, Tsukamura H, Inoue K, et al. Involvement of anteroventral periventricular metastin/kisspeptin neurons in estrogen positive feedback action on luteinizing hormone release in female rats. J Reprod Dev 2007; 53: 367–378.. [DOI] [PubMed] [Google Scholar]
- Bern H.The fragile fetus. Colborn T, Clement C.Chemically-Induced Alterations in Sexual and Functional Development: The Wildlife/Human Connection Princeton:Princeton Scientific;1992: 9–15.. [Google Scholar]
- Kauffman AS, Gottsch ML, Roa J, Byquist AC, Crown A, Clifton DK, Hoffman GE, Steiner RA, Tena-Sempere M.Sexual differentiation of Kiss1 gene expression in the brain of the rat. Endocrinology 2007; 148: 1774–1783.. [DOI] [PubMed] [Google Scholar]
- Bakker J, Baum MJ.Role for estradiol in female-typical brain and behavioral sexual differentiation. Front Neuroendocrinol 2008; 29: 1–16.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baum MJ.Differentiation of coital behavior in mammals: a comparative analysis. Neurosci Biobehav Rev 1979; 3: 265–284.. [DOI] [PubMed] [Google Scholar]
- Simerly RB.Wired for reproduction: organization and development of sexually dimorphic circuits in the mammalian forebrain. Annu Rev Neurosci 2002; 25: 507–536.. [DOI] [PubMed] [Google Scholar]
- Jefferson WN, Padilla-Banks E, Newbold RR.Adverse effects on female development and reproduction in CD-1 mice following neonatal exposure to the phytoestrogen genistein at environmentally relevant doses. Biol Reprod 2005; 73: 798–806.. [DOI] [PubMed] [Google Scholar]
- Jefferson WN, Padilla-Banks E, Newbold RR.Disruption of the developing female reproductive system by phytoestrogens: genistein as an example. Mol Nutr Food Res 2007; 51: 832–844.. [DOI] [PubMed] [Google Scholar]
- Arai Y.Critical exposure time for androgenization of developing hypothalamus in female rat. Endocrinology 1968; 82: 1010 [DOI] [PubMed] [Google Scholar]
- Grumbach MM.The neuroendocrinology of human puberty revisited. Horm Res 2002; 57(suppl 2):2–14.. [DOI] [PubMed] [Google Scholar]
- Crain DA, Eriksen M, Iguchi T, Jobling S, Laufer H, LeBlanc GA, Guillette LJ.An ecological assessment of bisphenol-A: evidence from comparative biology. Reprod Toxicol 2007; 24: 225–239.. [DOI] [PubMed] [Google Scholar]
- Mlynarcikova A, Nagyova E, Fickova M, Scsukova S.Effects of selected endocrine disruptors on meiotic maturation, cumulus expansion, synthesis of hyaluronan and progesterone by porcine oocyte-cumulus complexes. Toxicol In Vitro 2009; 23: 371–377.. [DOI] [PubMed] [Google Scholar]
- Nakamura T, Katsu Y, Watanabe H, Iguchi T.Estrogen receptor subtypes selectively mediate female mouse reproductive abnormalities induced by neonatal exposure to estrogenic chemicals. Toxicology 2008; 253: 117–124.. [DOI] [PubMed] [Google Scholar]
- Aihara M, Hayashi S.Induction of persistent diestrus followed by persistent estrus is indicative of delayed maturation of tonic gonadotropin-releasing systems in rats. Biol Reprod 1989; 40: 96–101.. [DOI] [PubMed] [Google Scholar]
- Nagao T, Saito Y, Usumi K, Kuwagata M, Imai K.Reproductive function in rats exposed neonatally to bisphenol A and estradiol benzoate. Reprod Toxicol 1999; 13: 303–311.. [DOI] [PubMed] [Google Scholar]
- Pinilla L, Barreiro ML, Gonzalez LC, Tena-Sempere M, Aguilar E.Comparative effects of testosterone propionate, oestradiol benzoate, ICI 182,780, tamoxifen and raloxifene on hypothalamic differentiation in the female rat. J Endocrinol 2002; 172: 441–448.. [DOI] [PubMed] [Google Scholar]
- Taylor JA, Welshons WV, Vom Saal FS.No effect of route of exposure (oral; subcutaneous injection) on plasma bisphenol A throughout 24h after administration in neonatal female mice. Reprod Toxicol 2008; 25: 169–176.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Toxicology Program. vol. 08-5994. National Institutes of Health,; Bethesda, MD.: NTP-CERHR monograph on the potential human reproductive and developmental effects of bisphenol A. [Internet]. March 2009. Available from http://cerhr.niehs.nih.gov/chemicals/bisphenol/BPADraftBriefVF_04_14_08.pdf. [Google Scholar]
- Stauffer SR, Coletta CJ, Tedesco R, Nishiguchi G, Carlson K, Sun J, Katzenellenbogen BS, Katzenellenbogen JA.Pyrazole ligands: structure-affinity/activity relationships and estrogen receptor-alpha-selective agonists. J Med Chem 2000; 43: 4934–4947.. [DOI] [PubMed] [Google Scholar]
- Patisaul HB, Fortino AE, Polston EK.Neonatal genistein or bisphenol-A exposure alters sexual differentiation of the AVPV. Neurotoxicol Teratol 2006; 28: 111–118.. [DOI] [PubMed] [Google Scholar]
- Sisk C.The neural basis of puberty and adolescence. Nat Neurosci 2004; 7: 1040–1047.. [DOI] [PubMed] [Google Scholar]
- Terasawa E, Fernandez DL.Neurobiological mechanisms of the onset of puberty in primates. Endocr Rev 2001; 22: 111–151.. [DOI] [PubMed] [Google Scholar]
- Becker JB, Arnold AP, Berkley KJ, Blaustein JD, Eckel LA, Hampson E, Herman JP, Marts S, Sadee W, Steiner M, Taylor J, Young E.Strategies and methods for research on sex differences in brain and behavior. Endocrinology 2005; 146: 1650–1673.. [DOI] [PubMed] [Google Scholar]
- Patisaul HB, Dindo M, Whitten PL, Young LJ.Soy isoflavone supplements antagonize reproductive behavior and ERα- and ERβ- dependent gene expression in the brain. Endocrinology 2001; 142: 2946–2952.. [DOI] [PubMed] [Google Scholar]
- Patisaul HB, Luskin JR, Wilson ME.A soy supplement and tamoxifen inhibit sexual behavior in female rats. Horm Behav 2004; 45: 270–277.. [DOI] [PubMed] [Google Scholar]
- Patisaul HB, Todd KL, Mickens JA, Adewale HB.Impact of neonatal exposure to the ERα agonist PPT, bisphenol-a or phytoestrogens on hypothalamic kisspeptin fiber density in male and female rats. Neurotoxicology 2009; 30: 350–357.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshida M, Sanbuissyo A, Hisada S, Takahashi M, Ohno Y, Nishikawa A.Morphological characterization of the ovary under normal cycling in rats and its viewpoints of ovarian toxicity detection. J Toxicol Sci 2009; 34: SP189–SP197.. [DOI] [PubMed] [Google Scholar]
- Finn PD, Steiner RA, Clifton DK.Temporal patterns of gonadotropin-releasing hormone (GnRH), c-fos, and galanin gene expression in GnRH neurons relative to the luteinizing hormone surge in the rat. J Neurosci 1998; 18: 713–719.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu TJ, Segal AZ, Miller GM, Gibson MJ, Silverman AJ.FOS expression in gonadotropin-releasing hormone neurons: enhancement by steroid treatment and mating. Endocrinology 1992; 131: 2045–2050.. [DOI] [PubMed] [Google Scholar]
- Patisaul HB, Fortino AE, Polston EK.Sex differences in serotonergic but not γ-aminobutyric acidergic (GABA) projections to the rat ventromedial nucleus of the hypothalamus. Endocrinology 2008; 149: 397–408.. [DOI] [PubMed] [Google Scholar]
- Patisaul HB, Fortino AE, Polston EK.Differential disruption of nuclear volume and neuronal phenotype in the preoptic area by neonatal exposure to genistein and bisphenol-A. Neurotoxicology 2007; 28: 1–12.. [DOI] [PubMed] [Google Scholar]
- Wray S, Gainer H.Effect of neonatal gonadectomy on the postnatal development of LHRH cell subtypes in male and female rats. Neuroendocrinology 1987; 45: 413–419.. [DOI] [PubMed] [Google Scholar]
- Wray S, Hoffman G.A developmental study of the quantitative distribution of LHRH neurons within the central nervous system of postnatal male and female rats. J Comp Neurol 1986; 252: 522–531.. [DOI] [PubMed] [Google Scholar]
- Paxinos G, Watson C. London:: Elsevier Academic;; 2004. The Rat Brain in Stereotaxic Coordinates : [the new coronal set]. [Google Scholar]
- Lubahn DB, Moyer JS, Golding TS, Couse JF, Korach KS, Smithies O.Alteration of reproductive function but not prenatal sexual development after insertional disruption of the mouse estrogen receptor gene. Proc Natl Acad Sci U S A 1993; 90: 11162–11166.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JT, Clifton DK, Steiner RA.Regulation of the neuroendocrine reproductive axis by kisspeptin-GPR54 signaling. Reproduction 2006; 131: 623–630.. [DOI] [PubMed] [Google Scholar]
- Messager S, Chatzidaki EE, Ma D, Hendrick AG, Zahn D, Dixon J, Thresher RR, Malinge I, Lomet D, Carlton MB, Colledge WH, Caraty A, et al. Kisspeptin directly stimulates gonadotropin-releasing hormone release via G protein-coupled receptor 54. Proc Natl Acad Sci U S A 2005; 102: 1761–1766.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navarro VM, Sánchez-Garrido MA, Castellano JM, Roa J, García-Galiano D, Pineda R, Aguilar E, Pinilla L, Tena-Sempere M.Persistent impairment of hypothalamic KiSS-1 system after exposures to estrogenic compounds at critical periods of brain sex differentiation. Endocrinology 2009; 150: 2359–2367.. [DOI] [PubMed] [Google Scholar]
- Fernandez M, Bianchi M, Lux-Lantos V, Libertun C.Neonatal exposure to bisphenol A alters reproductive parameters and gonadotropin releasing hormone signaling in female rats. Environ Health Perspect 2009; 117: 757–762.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knobil E, Neill JD. New York:: Raven Press;; 1994. The Physiology of Reproduction. [Google Scholar]
- Evans NP, North T, Dye S, Sweeney T.Differential effects of the endocrine-disrupting compounds bisphenol-A and octylphenol on gonadotropin secretion, in prepubertal ewe lambs. Domest Anim Endocrinol 2004; 26: 61–73.. [DOI] [PubMed] [Google Scholar]
- Savabieasfahani M, Kannan K, Astapova O, Evans NP, Padmanabhan V.Developmental programming: differential effects of prenatal exposure to bisphenol-A or methoxychlor on reproductive function. Endocrinology 2006; 147: 5956–5966.. [DOI] [PubMed] [Google Scholar]
- Lin X, Conn PM.Transcriptional activation of gonadotropin-releasing hormone (GnRH) receptor gene by GnRH: involvement of multiple signal transduction pathways. Endocrinology 1999; 140: 358–364.. [DOI] [PubMed] [Google Scholar]
- Rubin BS, Murray MK, Damassa DA, King JC, Soto AM.Perinatal exposure to low doses of bisphenol A affects body weight, patterns of estrous cyclicity, and plasma LH levels. Environ Health Perspect 2001; 109: 675–680.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikaido Y, Yoshizawa K, Danbara N, Tsujita-Kyutoku M, Yuri T, Uehara N, Tsubura A.Effects of maternal xenoestrogen exposure on development of the reproductive tract and mammary gland in female CD-1 mouse offspring. Reprod Toxicol 2004; 18: 803–811.. [DOI] [PubMed] [Google Scholar]
- Newbold RR, Jefferson WN, Padilla-Banks E.Long-term adverse effects of neonatal exposure to bisphenol A on the murine female reproductive tract. Reprod Toxicol 2007; 24: 253–258.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikaido Y, Danbara N, Tsujita-Kyutoku M, Yuri T, Uehara N, Tsubura A.Effects of prepubertal exposure to xenoestrogen on development of estrogen target organs in female CD-1 mice. In Vivo 2005; 19: 487–494.. [PubMed] [Google Scholar]
- Schönfelder GG, Flick BB, Mayr EE, Talsness CC, Paul MM, Chahoud II.In utero exposure to low doses of bisphenol A lead to long-term deleterious effects in the vagina. Neoplasia 2002; 4: 98–102.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kato H, Ota T, Furuhashi T, Ohta Y, Iguchi T.Changes in reproductive organs of female rats treated with bisphenol A during the neonatal period. Reprod Toxicol 2003; 17: 283–288.. [DOI] [PubMed] [Google Scholar]
- Honma SS, Suzuki AA, Buchanan DLDL, Katsu YY, Watanabe HH, Iguchi TT.Low dose effect of in utero exposure to bisphenol A and diethylstilbestrol on female mouse reproduction. Reprod Toxicol 2002; 16: 117–122.. [DOI] [PubMed] [Google Scholar]
- Welshons WV, Nagel SC, vom Saal FS.Large effects from small exposures. III. Endocrine mechanisms mediating effects of bisphenol A at levels of human exposure. Endocrinology 2006; 147: S56–S69.. [DOI] [PubMed] [Google Scholar]
- Sheehan DM.Activity of environmentally relevant low doses of endocrine disruptors and the bisphenol A controversy: initial results confirmed. Proc Soc Exp Biol Med 2000; 224: 57–60.. [DOI] [PubMed] [Google Scholar]
- Vandenberg LN, Wadia PR, Schaeberle CM, Rubin BS, Sonnenschein C, Soto AM.The mammary gland response to estradiol: monotonic at the cellular level, non-monotonic at the tissue-level of organization? J Steroid Biochem Mol Biol 2006; 101: 263–274.. [DOI] [PubMed] [Google Scholar]
- Vandenberg LN, Maffini MV, Sonnenschein C, Rubin BS, Soto AM.Bisphenol-A and the great divide: a review of controversies in the field of endocrine disruption. Endocr Rev 2009; 30: 75–95.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyl RW, Myers CB, Marr MC, Thomas BF, Keimowitz AR, Brine DR, Veselica MM, Fail PA, Chang TY, Seely JC, Joiner RL, Butala JH, et al. Three-generation reproductive toxicity study of dietary bisphenol A in CD Sprague-Dawley rats. Toxicol Sci 2002; 68: 121–146.. [DOI] [PubMed] [Google Scholar]
- Ikeda Y, Nagai A, Ikeda MA, Hayashi S.Neonatal estrogen exposure inhibits steroidogenesis in the developing rat ovary. Dev Dyn 2001; 221: 443–453.. [DOI] [PubMed] [Google Scholar]
- Markey CM, Coombs MA, Sonnenschein C, Soto AM.Mammalian development in a changing environment: exposure to endocrine disruptors reveals the developmental plasticity of steroid-hormone target organs. Evol Dev 2003; 5: 67–75.. [DOI] [PubMed] [Google Scholar]
- Lenie S, Cortvrindt R, Eichenlaub-Ritter U, Smitz J.Continuous exposure to bisphenol A during in vitro follicular development induces meiotic abnormalities. Mutat Res 2008; 651: 71–81.. [DOI] [PubMed] [Google Scholar]
- Susiarjo M, Hassold TJ, Freeman E, Hunt PA.Bisphenol A exposure in utero disrupts early oogenesis in the mouse. PLoS Genet 2007; 3: e5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt PA, Koehler KE, Susiarjo M, Hodges CA, Ilagan A, Voigt RC, Thomas S, Thomas BF, Hassold TJ.Bisphenol a exposure causes meiotic aneuploidy in the female mouse. Curr Biol 2003; 13: 546–553.. [DOI] [PubMed] [Google Scholar]
- Patchev AV, Götz F, Rohde W.Differential role of estrogen receptor isoforms in sex-specific brain organization. FASEB J 2004; 18: 1568–1570.. [DOI] [PubMed] [Google Scholar]
- Sar M, Welsch F.Differential expression of estrogen receptor-β and estrogen receptor-α in the rat ovary. Endocrinology 1999; 140: 963–971.. [DOI] [PubMed] [Google Scholar]
- Matsushima A, Teramoto T, Okada H, Liu X, Tokunaga T, Kakuta Y, Shimohigashi Y.ERR gamma tethers strongly bisphenol A and 4-alpha-cumylphenol in an induced-fit manner. Biochem Biophys Res Commun 2008; 373: 408–413.. [DOI] [PubMed] [Google Scholar]
- Okada H, Tokunaga T, Liu XH, Takayanagi S, Matsushima A, Shimohigashi Y.Direct evidence revealing structural elements essential for the high binding ability of bisphenol A to human estrogen-related receptor-gamma. Environ Health Perspect 2008; 116: 32–38.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takayanagi S, Tokunaga T, Liu XH, Okada H, Matsushima A, Shimohigashi Y.Endocrine disruptor bisphenol A strongly binds to human estrogen-related receptor gamma (ERR gamma) with high constitutive activity. Toxicol Lett 2006; 167: 95–105.. [DOI] [PubMed] [Google Scholar]
- Heard DJ, Norby PL, Holloway J, Vissing H.Human ERR gamma, a third member of the estrogen receptor-related receptor (ERR) subfamily of orphan nuclear receptors: tissue-specific isoforms are expressed during development and in the adult. Mol Endocrinol 2000; 14: 382–392.. [DOI] [PubMed] [Google Scholar]
- Sun P, Sehouli J, Denkert C, Mustea A, Konsgen D, Koch I, Wei LH, Lichtenegger W.Expression of estrogen receptor-related receptors, a subfamily of orphan nuclear receptors, as new tumor biomarkers in ovarian cancer cells. J Mol Med 2005; 83: 457–467.. [DOI] [PubMed] [Google Scholar]
- Powell CE, Soto AM, Sonnenschein C.Identification and characterization of membrane estrogen receptor from MCF7 estrogen-target cells. J Steroid Biochem Mol Biol 2001; 77: 97–108.. [DOI] [PubMed] [Google Scholar]
- Watson CS, Bulayeva NN, Wozniak AL, Alyea RA.Xenoestrogens are potent activators of nongenomic estrogenic responses. Steroids 2007; 72: 124–134.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas P, Dong J.Binding and activation of the seven-transmembrane estrogen receptor GPR30 by environmental estrogens: a potential novel mechanism of endocrine disruption. J Steroid Biochem Mol Biol 2006; 102: 175–179.. [DOI] [PubMed] [Google Scholar]
- Jirtle RL, Skinner MK.Environmental epigenomics and disease susceptibility. Nat Rev Genet 2007; 8: 253–262.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolinoy DC, Huang D, Jirtle RL.Maternal nutrient supplementation counteracts bisphenol A-induced DNA hypomethylation in early development. Proc Natl Acad Sci U S A 2007; 104: 13056–13061.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farabollini F, Porrini S, Della Seta D, Bianchi F, Dessi-Fulgheri F.Effects of perinatal exposure to bisphenol A on sociosexual behavior of female and male rats. Environ Health Perspect 2002; 110(suppl 3):409–414.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laessig SA, Auger AP, McCarthy MM, Silbergeld EK.Effects of prenatal chlordecone on sexually differentiated behavior in adult rats. Neurotoxicol Teratol 2007; 29: 255–263.. [DOI] [PubMed] [Google Scholar]
- Gorski RA.Modification of ovulatory mechanisms by postnatal administration of estrogen to the rat. Am J Physiol 1963; 205: 842–844.. [DOI] [PubMed] [Google Scholar]
- Dohler KD.The pre- and postnatal influence of hormones and neurotransmitters on sexual differentiation of the mammalian hypothalamus. Int Rev Cytol 1991; 131: 1–57.. [DOI] [PubMed] [Google Scholar]
- Yanase M, Gorski RA.Sites of estrogen and progesterone facilitation of lordosis behavior in the spayed rat. Biol Reprod 1976; 15: 536–543.. [DOI] [PubMed] [Google Scholar]
- Sun Y, Irie M, Kishikawa N, Wada M, Kuroda N, Nakashima K.Determination of bisphenol A in human breast milk by HPLC with column-switching and fluorescence detection. Biomed Chromatogr 2004; 18: 501–507.. [DOI] [PubMed] [Google Scholar]
- Ye X, Bishop AM, Needham LL, Calafat AM.Automated on-line column-switching HPLC-MS/MS method with peak focusing for measuring parabens, triclosan, and other environmental phenols in human milk. Anal Chimica Acta 2008; 622: 150–156.. [DOI] [PubMed] [Google Scholar]
- Ikezuki Y, Tsutsumi O, Takai Y, Kamei Y, Taketani Y.Determination of bisphenol A concentrations in human biological fluids reveals significant early prenatal exposure. Hum Reprod 2002; 17: 2839–2841.. [DOI] [PubMed] [Google Scholar]
- Padmanabhan V, Siefert K, Ransom S, Johnson T, Pinkerton J, Anderson L, Tao L, Kannan K.Maternal bisphenol-A levels at delivery: a looming problem? J Perinatol 2008; 28: 258–263.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schönfelder G, Wittfoht W, Hopp H, Talsness CE, Paul M, Chahoud I.Parent bisphenol A accumulation in the human maternal-fetal-placental unit. Environ Health Perspect 2002; 110: A703–A707.. [DOI] [PMC free article] [PubMed] [Google Scholar]