Abstract
Objectives
To determine the acceptability of two psychological interventions for depressed adults in the community and their effect on caseness, symptoms, and subjective function.
Design
A pragmatic multicentre randomised controlled trial, stratified by centre.
Setting
Nine urban and rural communities in Finland, Republic of Ireland, Norway, Spain, and the United Kingdom.
Participants
452 participants aged 18 to 65, identified through a community survey with depressive or adjustment disorders according to the international classification of diseases, 10th revision or Diagnostic and Statistical Manual of Mental Disorders, fourth edition.
Interventions
Six individual sessions of problem solving treatment (n=128), eight group sessions of the course on prevention of depression (n=108), and controls (n=189).
Main outcome measures
Completion rates for each intervention, diagnosis of depression, and depressive symptoms and subjective function.
Results
63% of participants assigned to problem solving and 44% assigned to prevention of depression completed their intervention. The proportion of problem solving participants depressed at six months was 17% less than that for controls, giving a number needed to treat of 6; the mean difference in Beck depression inventory score was –2.63 (95% confidence interval –4.95 to –0.32), and there were significant improvements in SF-36 scores. For depression prevention, the difference in proportions of depressed participants was 14% (number needed to treat of 7); the mean difference in Beck depression inventory score was –1.50 (–4.16 to 1.17), and there were significant improvements in SF-36 scores. Such differences were not observed at 12 months. Neither specific diagnosis nor treatment with antidepressants affected outcome.
Conclusions
When offered to adults with depressive disorders in the community, problem solving treatment was more acceptable than the course on prevention of depression. Both interventions reduced caseness and improved subjective function.
Introduction
Depressive disorders are common major sources of personal distress and social disability.1 Most treatment is carried out in primary care, yet many depressed people do not receive health interventions.2,3 Pharmacotherapy is effective in clinical trials, but public opinion favours psychological treatments.4–7
The outcomes of depression international network (ODIN) is a European project studying the prevalence and outcomes of depression in urban and rural communities.8 One objective was to assess the efficacy of psychological interventions. We identified two simple, reproducible interventions that could be delivered in the community without complex healthcare infrastructures or expensive health professionals.
Problem solving treatment has three main steps: patients' symptoms are linked with their problems, problems are defined and clarified, and an attempt is made to solve the problems in a structured way. The treatment involves six individual sessions — less than four hours' therapist time9 — and is easily taught to a range of health professionals. It is as effective as pharmacotherapy for major depression in primary care10,11 but has not yet been tested in community settings.
Group psychoeducation emphasises instruction not therapy and promotes relaxation, positive thinking, pleasant activities, and social skills. The coping with depression course comprises 12 two hour sessions over eight weeks, with class reunions,12 whereas the course on prevention of depression comprises eight sessions.13 Psychoeducation has been used in healthcare and community settings and seems effective in prevention and quality improvement programmes in US primary care.14–16
This arm of the outcomes of depression international network aimed to measure (a) the acceptability of problem solving treatment and the course on prevention of depression to people with depressive disorders identified through a community survey, (b) their impact on depressive caseness, symptoms, and subjective function, and (c) their cost effectiveness. We present findings on acceptability of the two treatments, caseness, symptoms, and subjective function.
Participants and methods
Study sites and populations
The outcomes of depression international network involved nine study sites in Finland, Republic of Ireland, Norway, Spain, and the United Kingdom. Cases of depressive disorders were identified by a two stage community survey between autumn 1996 and spring 1998.17 The Beck depression inventory was used to screen potential cases. This was followed by a standardised diagnostic interview, including the schedule for clinical assessment in neuropsychiatry version 2.0 to assign caseness according to the Diagnostic and Statistical Manual of Mental Disorder, fourth edition or the international classification of diseases, 10th revision, and SF-36 for subjective assessment of function.18–20 Cases were offered follow up interviews six and 12 months later. Ethical approval was obtained according to local protocols. Details of our survey methods, including translation, training, and quality control procedures, have been published.8
Study design
We undertook a pragmatic randomised controlled trial, comparing outcomes of problem solving treatment or the depression prevention course with controls receiving no intervention. Problem solving was offered at a location most suitable to the participant, usually their own home. For group psychoeducation we used a modified course for prevention of depression, with sessions lasting 2.5 hours and with more social support than in the original course on prevention of depression. Each intervention was offered at five sites (table 1) and was delivered by facilitators with qualifications in psychology, nursing, or allied health professions.
Table 1.
Sites for problem solving treatment and course on prevention of depression
| Problem solving | Depression prevention | |
|---|---|---|
| Urban | Finland (Turku) | Ireland (Dublin) |
| Spain (Santander) | Norway (Oslo) | |
| United Kingdom (Liverpool) | United Kingdom (Liverpool) | |
| Rural | Finland (Martilla, Koskitl, Tarvasjoki) | Ireland (Laois) |
| United Kingdom (Vale of Clwyd) | Norway (Rakkestad) |
Assignment—Cases were randomly allocated to one of the trial groups. Inclusion criteria were (a) age 18 to 65, (b) depressive episodes according to the international classification of diseases, 10th revision, dysthymia, or adjustment disorder, or (c) depressive disorders according to the Diagnostic and Statistical Manual of Mental Disorders, fourth edition, dysthymia, adjustment disorder, bereavement, or other depressive disorders. Exclusion criteria were comorbid psychotic condition, current drug or alcohol related disorder, or major suicide risk. Concurrent treatment with antidepressants was not an exclusion criterion. At each study site the unit of randomisation was the participant. Allocation schedules were generated by random number tables and administered by staff not in contact with the participants. Given the nature of the intervention, it was not possible to conceal group allocation from either investigators or participants at follow up.
Statistical methods
The number of participants recruited fell far short of those planned in the original sample size calculations, which were optimistically intended to test the effectiveness of the interventions at each centre separately.8 Here, however, we are concerned with estimation and testing the therapy effects for the centres combined. Revised sample size requirements were calculated on the basis of the outcomes of the Beck depression inventory and schedule for clinical assessment in neuropsychiatry, using a two sided 5% significance level, and assuming a ratio of 1:1:2 for problem solving, depression prevention, and controls. Given the uncertainty of outcome from a study based outside healthcare settings, we made no assumptions concerning the difference in efficacy of problem solving and prevention of depression. Our data have limited power to differentiate the effects of the two forms of therapy. Our trial contained around 200 patients receiving treatment and around 200 controls. These sample sizes are sufficient to have about 85% power to detect a difference between treatment and control groups of 2.5 (8 SD) points on the Beck depression inventory with Student's t test. For the schedule for clinical assessment in neuropsychiatry, with the outcome being “no longer a case,” the trial has about 85% power to detect a 15% difference (35% recovery in controls versus 50% for therapy, odds ratio=0.54) in outcome between interventions and control with a Pearson χ2 test. The corresponding power for comparing individual therapies with the controls (i.e. using 100 patients per group) is about 60%.
The design of the trial is complex, involving nine treatment centres, only one of which used both interventions. It is essential, therefore, in estimating and testing treatment effects that the analysis involves stratification by centre to ensure that each intervention group is being compared with its own control. Quantitative outcomes (scores on the Beck depression inventory and the SF-36 subscales) were analysed with an analysis of covariance. Outcomes at six months and 12 months were analysed separately. Relevant baseline scores, age, and treatment with antidepressants were used as covariates, and treatment group, centre, and diagnostic group were treated as qualitative factors. Centre effects were treated as either random or fixed. Qualitative outcomes (diagnosis of depression) were analysed similarly, but here using logistic regression instead of an analysis of covariance. All analyses of treatment effects were carried out with reg, xtreg (random effects models), logit, and xtlogit (random effects models) from STATA (release 6).
Not all patients provided follow up information. All analyses were carried out by intention to treat but with alternative approaches to dealing with the effects of drop-outs.21 Firstly, analysis of available data (complete case analysis) assumed that data are missing completely at random.22 It was clear, however, that factors such as treatment allocation and the acceptability of the treatment offered influenced drop-out rates. The second approach therefore assumed that data were missing at random, involving calculation of adjustment weights to compensate for missing values.22 Probability of providing a follow up interview was predicted with baseline Beck depression inventory, treatment group, acceptability of treatment, and treatment centre in an unweighted logistic regression (using logit). The reciprocal of this probability was then used as an adjustment (probability) weight using logit in a weighted logistic regression to estimate the treatment effects in the main analyses.
Results
Characteristics of the sample
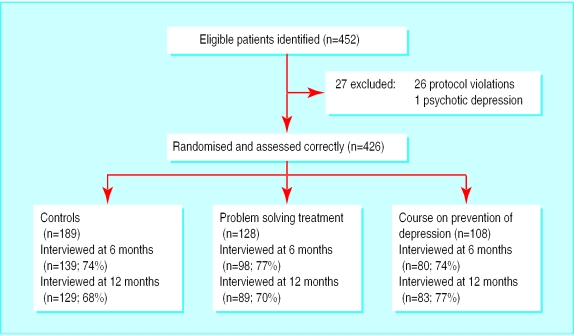
Overall, 452 people were identified as cases through the survey phase of the project of the outcomes of depression international network. Those who responded to the survey were more likely to be female and older than non-responders: the sex difference was significant at three sites.23 Randomisation and assessment were correctly undertaken for 425 people — 26 people recruited in Dublin were excluded post hoc from the analysis, after discovery of a breach in protocol by a former member of the Irish research team, and one participant with a psychotic condition was excluded from the Norwegian sample (figure). Table 2 shows the baseline socioeconomic profiles of participants in each of the three arms. Diagnoses for 412 participants were based on the international classification of diseases, 10th revision: 238 (58%) single depressive episodes and 82 (20%) recurrent depressive episodes, 58 (14%) dysthymia, 21 (5%) adjustment disorder, and 13 (3%) others. Diagnoses for 418 participants were based on the DSM-IV: 216 (52%) single major depressive disorders and 81 (19%) recurrent major depressive disorders, 67 (16%) dysthymia, 18 (4%) adjustment disorders, and 36 (9%) others. Of 394 participants with available data, 102 (26%) reported currently taking antidepressants. There were no significant differences in diagnosis or antidepressant receipt between the study sites or the intervention arms.
Table 2.
Socioeconomic profiles at baseline. Values are numbers (percentages)
| Characteristic | Controls (n=189) | Problem solving (n=128) | Depression prevention (n=108) | Total |
|---|---|---|---|---|
| Sex: | ||||
| Male | 66 (35) | 43 (34) | 39 (36) | 148 (35) |
| Female | 123 (65) | 85 (66) | 69 (64) | 277 (65) |
| Age: | ||||
| 18-25 | 8 (4) | 1 (1) | 10 (9) | 19 (5) |
| 26-45 | 91 (48) | 52 (41) | 51 (47) | 194 (46) |
| 46-65 | 90 (48) | 75 (59) | 47 (44) | 212 (50) |
| Marital status: | ||||
| Single | 28 (14) | 21 (16) | 21 (19) | 70 (16) |
| Married or cohabiting | 117 (62) | 75 (59) | 59 (55) | 251 (60) |
| Separated or divorced | 38 (20) | 23 (18) | 28 (26) | 89 (21) |
| Widowed | 6 (3) | 9 (7) | 0 | 15 (4) |
| Occupation: | ||||
| Employed | 94 (50) | 54 (42) | 57 (53) | 205 (48) |
| Unemployed | 15 (8) | 16 (13) | 10 (9) | 41 (10) |
| Unemployed owing to disability | 40 (21) | 29 (23) | 23 (21) | 92 (22) |
| Housewife | 17 (9) | 16 (13) | 7 (7) | 40 (9) |
| Retired | 10 (5) | 8 (6) | 4 (4) | 22 (5) |
| Other | 13 (7) | 5 (4) | 7 (7) | 25 (6) |
| Accommodation: | ||||
| Owner occupied | 110 (59) | 74 (58) | 49 (46) | 233 (55) |
| Rented | 64 (34) | 41 (32) | 50 (47) | 155 (37) |
| Other | 15 (7) | 13 (10) | 9 (7) | 37 (8) |
Table 3 gives numbers of baseline and follow up interviews completed for participants, at each centre. Differential recruitment between centres reflected differences in the prevalence of depressive disorders in the populations surveyed during the first phase of the outcomes of depression international network.23 We provided 11 courses in depression prevention — three in Ireland, seven in Norway, and one in the United Kingdom.
Table 3.
Number of participants (out of 425) with follow up interviews
| Centre | Country | Site | Treatment | Control group
|
Treatment groups
|
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 6 months | 12 months | Baseline | 6 months | 12 months | |||||
| 1 | Finland | Urban | Problem solving | 24 | 17 | 17 | 23 | 19 | 16 | |
| 2 | Finland | Rural | Problem solving | 22 | 20 | 20 | 28 | 24 | 21 | |
| 3 | Ireland | Urban | Depression prevention | 16 | 6 | 7 | 7 | 5 | 4 | |
| 4 | Ireland | Rural | Depression prevention | 7 | 6 | 6 | 8 | 3 | 5 | |
| 5 | Norway | Urban | Depression prevention | 25 | 17 | 16 | 42 | 31 | 35 | |
| 6 | Norway | Rural | Depression prevention | 25 | 18 | 18 | 36 | 32 | 31 | |
| 7 | Spain | Urban | Problem solving | 11 | 6 | 7 | 19 | 15 | 17 | |
| 8 | United Kingdom | Urban | Problem solving and depression prevention | 37 | 31 | 25 | 32/15* | 22/9* | 19/8* | |
| 9 | United Kingdom | Rural | Problem solving | 23 | 18 | 13 | 26 | 18 | 15 | |
| Total: | 189 | 139 | 129 | 128/108* | 98/80* | 89/83* | ||||
Number receiving problem solving treatment/ number on course for prevention of depression.
Overall, 317 (74%) participants took part in follow up interviews at six months and 301 (71%) at 12 months (figure). There were significant differences between the nine centres in the proportions of participants reinterviewed at six months (χ2=17.52, df=8, P=0.025) and 12 months (χ2=21.47, df=8, P=0.006). No significant differences were found in follow up rates between the three trial groups at either six or 12 months. From a logistic regression analysis for the whole sample the probability of providing a follow up interview decreased with increasing baseline score on the Beck depression inventory: at six months β=−0.017 (0.013 SE); P=0.203 and at 12 months β=−0.025 (0.013 SE), P=0.047.
Acceptability of the interventions
Acceptability was assessed by comparing the proportions of participants who refused or failed to attend an initial session, who discontinued an intervention, and who completed their assigned intervention (table 4). Participants who were randomised to problem solving were significantly more likely than those who were randomised to prevention of depression to complete the intervention (χ2=7.61, df=1, P=0.006).
Table 4.
Acceptability of problem solving treatment and course on prevention of depression. Values are numbers of participants unless stated otherwise
| Centre | Treatment | Offered treatment | Refused treatment | Discontinued treatment | Did not attend | No (%) who completed treatment |
|---|---|---|---|---|---|---|
| 1 | Problem solving | 23 | 0 | 5 | 1 | 17 (74) |
| 2 | Problem solving | 28 | 3 | 4 | 1 | 20 (71) |
| 3 | Depression prevention | 7 | 0 | 2 | 2 | 3 (43) |
| 4 | Depression prevention | 8 | 0 | 1 | 4 | 3 (38) |
| 5 | Depression prevention | 42 | 15 | 5 | 0 | 22 (52) |
| 6 | Depression prevention | 36 | 12 | 5 | 2 | 17 (47) |
| 7 | Problem solving | 19 | 7 | 0 | 0 | 12 (63) |
| 8 | Problem solving | 32 | 5 | 7 | 4 | 16 (50) |
| 8 | Depression prevention | 15 | 5 | 1 | 6 | 3 (20) |
| 9 | Problem solving | 26 | 5 | 6 | 0 | 15 (58) |
| No (%) problem solving (n=128) | 128 | 20 (16) | 22 (17) | 6 (5) | 80 (63) | |
| No (%) depression prevention (n=108) | 108 | 32 (29) | 14 (13) | 14 (13) | 48 (44) |
No significant differences were found in mean scores on the Beck depression inventory between participants completing or refusing to take part in an intervention. Men and single people were least likely to complete. Participants who completed were more likely to take part in follow up interviews: differences were significant at follow up at both six months (χ2=52.71 df=3, P<0.001) and 12 months (χ2=30.78, df=3, P<0.001).
Diagnosis of depression
Table 5 shows the proportions of participants in each centre who were no longer cases at follow up interviews at six and 12 months. It also shows the percentage differences between control and treatment groups in each centre, the percentage and odds ratios for overall differences, and, at six months, the numbers needed to treat to achieve the observed differences.
Table 5.
Diagnosis of depressive disorders at 6 and 12 months
| Centre | Proportion not depressed (%)
|
Difference | Proportion not depressed (%)
|
Difference | ||
|---|---|---|---|---|---|---|
| 6 months
|
12 months
|
|||||
| Control group | Treatment group | Control group | Treatment group | |||
| 1 Problem solving | 8/19 (42) | 11/19 (58) | 16 | 9/17 (53) | 11/16 (69) | 16 |
| 2 Problem solving | 12/20 (60) | 20/24 (83) | 23 | 13/20 (65) | 13/22 (59) | −6 |
| 3 Depression prevention | 3/6 (50) | 5/5 (100) | 50 | 5/7 (71) | 4/4 (100) | 29 |
| 4 Depression prevention | 4/6 (67) | 2/3 (67) | 0 | 4/6 (67) | 3/5 (60) | −7 |
| 5 Depression prevention | 9/17 (53) | 18/31 (58) | 5 | 8/16 (50) | 18/35 (51) | −1 |
| 6 Depression prevention | 6/18 (33) | 12/32 (38) | 4 | 10/18 (56) | 14/31 (45) | −10 |
| 7 Problem solving | 2/6 (33) | 8/15 (53) | 20 | 5/7 (71) | 11/17 (68) | −7 |
| 8 Problem solving | 10/31 (32) | 12/22 (55) | 22 | 16/25 (64) | 12/19 (63) | −1 |
| 8 Depression prevention | 10/31 (32) | 7/9 (78) | 46 | 16/25 (64) | 5/8 (63) | −2 |
| 9 Problem solving | 8/18 (44) | 7/18 (39) | −6 | 8/13 (62) | 8/15 (53) | −8 |
| Total for problem solving | 40/94 (43) | 58/98 (59) | 17* | 50/82 (61) | 55/89 (62) | 1† |
| Total for depression prevention | 32/78 (41) | 44/80 (55) | 14‡ | 43/72 (60) | 44/83 (53) | −7§ |
Odds ratio 1.39, number needed to treat 6.
Odds ratio 1.01.
Odds ratio 1.31, number needed to treat 7.
Odds ratio 0.89.
At six months there was a 17% difference in the proportions of cases between participants assigned to problem solving and controls, giving a number needed to treat of 6, and a 14% difference between participants assigned to prevention of depression and controls, giving a number needed to treat of 7. At 12 months there were no differences between the three treatment arms.
Table 6 gives logistic regression estimates of treatment effects on the diagnosis of depression using two computational methods — unweighted (complete case analysis) and weighted (to adjust for drop-out). In both analyses the centre effects were treated as fixed as a straightforward weighted analysis was not possible using xtlogit in STATA. Baseline data for the Beck depression inventory, age, concurrent treatment with antidepressants (yes or no), and diagnostic category (single, recurrent, dysthymia, adjustment, or other) were also included in the analysis. Using odds ratios with 95% confidence limits, at six months the first method shows a significant treatment effect for problem solving and an almost significant effect for prevention of depression, whereas the weighted analysis yields similar therapy effects, both falling just short of significance (α=0.05). These analyses indicate a treatment effect, with similar outcomes of the two therapies. The estimated common therapy effect odds ratios are 0.50 (95% confidence interval 0.30 to 0.85) and 0.54 (0.32 to 0.91) for the unweighted and weighted analyses, respectively. Ignoring drop-outs does not significantly bias estimates of treatment effects. At 12 months, neither method shows any differences between the two interventions and controls.
Table 6.
Logistic regression estimates of treatment effects on diagnosis of depressive disorders. Values are odds ratios (95% confidence intervals), with controls as reference group*
| 6 months | 12 months | |
|---|---|---|
| Unweighted (complete case analysis) | ||
| Problem solving | 0.51 (0.27 to 0.97) | 0.92 (0.48 to 1.77) |
| Depression prevention | 0.50 (0.21 to 1.15) | 1.02 (0.46 to 2.23) |
| Weighted (to allow for missing outcomes) | ||
| Problem solving | 0.58 (0.34 to 1.09) | 0.87 (0.45 to 1.70) |
| Depression prevention | 0.47 (0.20 to 1.12) | 1.07 (0.46 to 2.48) |
Adjusted for Beck depression inventory score, age, diagnostic category, and use of antidepressants at baseline, and for centre effects.
Depressive symptoms and subjective function
Depressive symptoms were measured at each interview by the Beck depression inventory, with lower figures indicating less depressive symptoms. Subjective function was measured with the SF-36, with higher scores indicating better subjective function. We present data on three SF-36 domains, mental role, social function, and mental health, as these are most relevant to a depression oriented intervention.
Tables 7 and 8 give overall mean scores for each of the four quantitative measures, comparing controls, problem solving, and prevention of depression at baseline and at six and 12 months. The second part indicates the treatment effects for each variable, taking into account relevant baseline scores and random centre effects. On this basis, at six months problem solving had a significant effect on the score on the Beck depression inventory and all three SF-36 scores, whereas prevention of depression had a significant effect on the SF-36 scores but not on the Beck depression inventory score. At 12 months there was evidence of a residual effect of problem solving on SF-36 domains of mental role and social function.
Table 7.
Outcomes for Beck depression inventory and SF-36 at baseline and 6 and 12 months. Values are overall means (SD)
| Baseline | 6 months | 12 months | |||
|---|---|---|---|---|---|
| Beck depression inventory | |||||
| Controls | 22.51 (8.01) | 14.97 (10.23) | 12.60 (9.50) | ||
| Problem solving | 23.11 (7.65) | 12.48 (9.95) | 11.15 (9.20) | ||
| Depression prevention | 22.41 (9.08) | 14.26 (9.71) | 14.60 (8.75) | ||
| SF-36 | |||||
| Mental role: | |||||
| Controls | 34.05 (38.26) | 51.71 (42.70) | 63.62 (41.90) | ||
| Problem solving | 34.36 (37.63) | 63.91 (42.13) | 70.53 (37.38) | ||
| Depression prevention | 38.87 (38.53) | 64.90 (40.70) | 61.43 (40.48) | ||
| Social function: | |||||
| Controls | 59.46 (29.23) | 64.90 (32.46) | 70.39 (30.09) | ||
| Problem solving | 50.48 (29.69) | 73.39 (28.81) | 75.42 (29.28) | ||
| Depression prevention | 48.62 (28.23) | 68.31 (29.07) | 66.89 (27.33) | ||
| Mental health: | |||||
| Controls | 43.51 (17.73) | 53.71 (23.58) | 60.51 (22.39) | ||
| Problem solving | 40.97 (19.26) | 60.08 (21.09) | 62.79 (22.00) | ||
| Depression prevention | 42.98 (16.39) | 59.54 (21.41) | 57.11 (20.33) | ||
Table 8.
Outcomes for treatment effects at 6 and 12 months
| Treatment v control | Outcome |
6 months
|
12 months
|
||||
|---|---|---|---|---|---|---|---|
| Mean (95% CI) | P value | Mean (95% CI) | P value | ||||
| Problem solving | Beck depression inventory* | −2.63 (−4.95 to −0.32) | 0.026 | −1.00 (−3.31 to 1.31) | 0.398 | ||
| Problem solving | SF-36 (mental role)† | 12.09 (1.17 to 23.01) | 0.030 | 8.31 (−2.06 to 18.68) | 0.116 | ||
| Problem solving | SF-36 (social function)‡ | 9.57 (2.12 to 17.02) | 0.012 | 6.96 (−0.74 to 14.59) | 0.077 | ||
| Problem solving | SF-36 (mental health)§ | 7.59 (2.26 to 12.92) | 0.005 | 4.14 (−0.99 to 9.28) | 0.114 | ||
| Depression prevention | Beck depression inventory* | −1.50 (−4.16 to 1.17) | 0.272 | 1.11 (−1.30 to 3.52) | 0.901 | ||
| Depression prevention | SF-36 (mental role)† | 12.70 (0.46 to 24.94) | 0.042 | −4.02 (−14.53 to 6.49) | 0.454 | ||
| Depression prevention | SF-36 (social function)‡ | 8.66 (0.07 to 17.25) | 0.048 | 2.36 (−6.10 to 10.83) | 0.584 | ||
| Depression prevention | SF-36 (mental health)§ | 6.95 (0.76 to 13.14) | 0.028 | −3.25 (−8.47 to 1.97) | 0.223 | ||
After controlling for baseline Beck depression inventory score and random centre effects.
After controlling for baseline Beck depression inventory score, mental role scores, and random centre effects.
After controlling for baseline Beck depression inventory score, social function scores, and random centre effects.
After controlling for baseline Beck depression inventory score, mental health scores, and random centre effects.
Discussion
Implications
Our study design breaks new ground in mental health research in community settings by combining a population survey with a randomised controlled trial. The outcomes of depression international network is the first international multicentre randomised controlled trial of psychological interventions for depression undertaken among the general population. It is the largest trial to date of problem solving treatment and the largest and most rigorously designed trial of the course on prevention of depression.
Our results indicate that problem solving was more acceptable than the course on prevention of depression when offered to people identified with depression in the community through a random sampling procedure. Almost two thirds of participants assigned to problem solving completed the intervention compared with less than half of those offered the course on prevention of depression.
Outcomes at six months were positive for both treatment arms, with results consistent across most measures. Compared with the controls, participants who were assigned to problem solving and the course on prevention of depression were less likely to remain cases of depression and more likely to report improved subjective mental and social functioning. Participants assigned to problem solving were less likely to report depressive symptoms. These differences were unrelated to diagnostic category or concurrent treatment with antidepressants. The benefits of problem solving at six months are comparable with previous studies in primary care,10,11 whereas a smaller effect size might have been expected in a community sample not seeking healthcare interventions. We confirm that non-doctors can deliver the problem solving intervention effectively11 and note its relevance across a range of depressive disorders.
Limitations
The differential in acceptability between problem solving and prevention of depression may reflect differential accessibility. Problem solving was usually delivered in the participants' homes. Participants who were assigned to prevention of depression had to travel, which may have reduced their likelihood of taking part. There were greater time delays in organising group events, and the didactic nature of the course on prevention of depression may have discouraged participation by those with previous negative experiences of education. Depressed patients may have felt stigmatised by their condition and less inclined to participate in group activity than a private individual process, particularly in close-knit rural areas such as the Norwegian rural site.
The positive outcomes for the course on prevention of depression at six months were less substantial than those in the studies cited earlier.14–16 This could reflect differences in study design or variations in internal coherence between the study groups. The course with eight sessions could be less effective than the one with 12 sessions.
By 12 months no significant effects were retained in either treatment arm, although there was evidence of a residual advantage from the problem solving treatment in two domains of subjective function. Booster sessions might sustain treatment benefits.
Our methods of analysis allowed us to account for the effects of conducting a set of linked trials in different centres but not for the possible constituents of centre effects. Cost effectiveness data will be reported separately.
Conclusions
Problem solving treatment and the course on prevention of depression may be recommended as effective interventions for people with depressive conditions in urban and rural community settings. This is because they reduce severity and duration of depressive disorders and improve subjective mental and social functioning. Our results should influence psychological services in primary care, emphasising treatments that are specific, brief, and easy to learn, with specific implications for practice counsellors. They also provide encouragement for depressed people who have not previously benefited from healthcare interventions.
What is already known on this topic
Psychological interventions for depression are popular with the public, but evidence for their efficacy in community settings is limited
Problem solving is an effective treatment for depression in primary care
Group psychoeducation may be effective in healthcare and community settings
What this study adds
It is feasible to undertake psychological interventions for depressive disorders in the context of community based surveys in a range of urban and rural settings across Europe
Problem solving treatment seems more acceptable than the course on prevention of depression to depressed people in community settings
Both problem solving treatment and the course on prevention of depression reduce the severity and duration of depressive disorders and improve subjective mental and social functioning
Figure.
Flow of participants through trial
Acknowledgments
The Outcome of Depression International Network Group is composed of academic colleagues and research and administrative staff who have worked on this part of the network's project. They are Gail Birkbeck, Trygve Børve, Maura Costello, Pim Cuijpers, Ioana Davies, Nicholas Fenlon, Mette Finne, Fiona Ford, Andres Gomes del Barrio, Claire Hayes, Ann Horgan, Tarja Koffert, Nicola Jones, Lourdes Lasa, Marja Lehtilä, Catherine McDonough, Erin Michalak, Christine Murphy, Anna Nevra, Teija Nummelin, and Britta Sohlman.
Footnotes
Funding: The project for the outcomes of depression international network was supported by the EC Biomed 2 programme (contract No BMH4-CT-1681), the English National Health Service Executive north west research and development office (contract No RDO/18/31), Spanish Fondo de Investigacion Sanitaria (contract No 96/1798), the Wales office of research and development (contract No RC092), the Norwegian Research Council, the Council for Mental Health, the Department of Health and Social Welfare, and the Finnish Pensions Institute of Agricultural Entrepreneurs (contract No 0339).
Competing interests: None declared.
References
- 1.Ormel J, von Korff M, Ustun T, Pini S, Korten A, Oldehinkel T. Common mental disorders and disability across cultures. JAMA. 1994;272:1741–1748. doi: 10.1001/jama.272.22.1741. [DOI] [PubMed] [Google Scholar]
- 2.Paykel ES, Priest RG. Recognition and management of depression in general practice: consensus statement. BMJ. 1992;161:633–637. doi: 10.1136/bmj.305.6863.1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldberg D, Huxley P. Common mental disorders: a biosocial model. London: Routledge; 1992. [Google Scholar]
- 4.Freemantle N, Long A, Mason A, Song F, Sheldon T, Watson P, et al. The treatment of depression in primary care. York: NHS Centre for Reviews and Dissemination; 1993. [Google Scholar]
- 5.Eccles M, Freemantle N, Mason J. North of England evidence-based guideline development project: summary version of guidelines for the choice of antidepressants for depression in primary care. Fam Pract. 1999;16:103–111. doi: 10.1093/fampra/16.2.103. [DOI] [PubMed] [Google Scholar]
- 6.Frank E. Enhancing patient outcomes: treatment adherence. J Clin Psychiatry. 1998;58(s1):11–14. [PubMed] [Google Scholar]
- 7.Paykel ES, Hart D, Priest RG. Changes in public attitudes to depression during the defeat depression campaign. Br J Psychiatry. 1998;173:519–522. doi: 10.1192/bjp.173.6.519. [DOI] [PubMed] [Google Scholar]
- 8.Dowrick C, Casey P, Dalgard O, Hosman C, Lehtinen V, Vazquez-Barquero J-L, et al. Outcomes of Depression International Network (ODIN): background, methods and field trials. Br J Psychiatry. 1998;172:359–363. doi: 10.1192/bjp.172.4.359. [DOI] [PubMed] [Google Scholar]
- 9.Hawton K, Kirk J. Problem-solving. In: Hawton K, Salkovskis PM, Kirk JW, Clark DM, editors. Cognitive behaviour therapy for psychiatric problems: a practical guide. Oxford: Oxford Medical; 1989. pp. 406–427. [Google Scholar]
- 10.Mynors-Wallis L, Gath D, Lloyd-Thomas A, Tomlinson D. Randomised controlled trial comparing problem solving treatment with amitriptyline and placebo for major depression in primary care. BMJ. 1995;310:441–445. doi: 10.1136/bmj.310.6977.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mynors-Wallis L, Gath D, Day A, Baker F. Randomised controlled trial of problem solving treatment, antidepressant medication, and combined treatment for major depression in primary care. BMJ. 2000;320:26–30. doi: 10.1136/bmj.320.7226.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lewinsohn P. The coping with depression course: review and future directions. Can J Behav Sci. 1989;21:470–493. [Google Scholar]
- 13.Muñoz R. The depression prevention course (revised edition 1998). Unpublished manual. Available from the author: University of California, San Francisco, Department of Psychiatry.
- 14.Cuijpers P. A psychoeducational approach to the treatment of depression: a meta-analysis of Lewinsohn's ‘coping with depression’ course. Behav Ther. 1998;29:521–533. [Google Scholar]
- 15.Muñoz R, Ying Y, Bernal G, Perez-Stable E, Sorensen J, Hargreaves W, et al. Prevention of depression with primary care patients: a randomized controlled trial. Am J Community Psychol. 1995;23:199–222. doi: 10.1007/BF02506936. [DOI] [PubMed] [Google Scholar]
- 16.Wells K, Sherbourne C, Schoenbaum M, Duan N, Meredith L, Unutzer J, et al. Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA. 2000;283:212–220. doi: 10.1001/jama.283.2.212. [DOI] [PubMed] [Google Scholar]
- 17.Dunn G, Pickles A, Tansella A, Vazquez-Barquero J. Two-phase epidemiological surveys in psychiatric research. Br J Psychiatry. 1999;174:95–100. doi: 10.1192/bjp.174.2.95. [DOI] [PubMed] [Google Scholar]
- 18.Beck A, Ward C, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization. Schedule for clinical assessment in neuropsychiatry: version 2.0. Geneva: WHO (Division of Mental Health); 1994. [Google Scholar]
- 20.Stewart A, Hays R, Ware J. The MOS short-form general health survey: reliability and validity in the patient population. Med Care. 1998;26:724–732. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ. 1999;319:670–674. doi: 10.1136/bmj.319.7211.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Little R, Rubin D. Statistical analysis with missing data. New York: Wiley; 1987. [Google Scholar]
- 23.Ayuso-Mateos J, Vazquez-Barquero J, Dowrick C, Lehtinen V, Dalgard O, Casey P, et al. Depressive disorders in Europe: prevalence figures from the ODIN study. Br J Psychiatry 2000 (in press). [DOI] [PubMed]