Abstract
Objectives
To obtain reliable estimates of the effects of neuraxial blockade with epidural or spinal anaesthesia on postoperative morbidity and mortality.
Design
Systematic review of all trials with randomisation to intraoperative neuraxial blockade or not.
Studies
141 trials including 9559 patients for which data were available before 1 January 1997. Trials were eligible irrespective of their primary aims, concomitant use of general anaesthesia, publication status, or language. Trials were identified by extensive search methods, and substantial amounts of data were obtained or confirmed by correspondence with trialists.
Main outcome measures
All cause mortality, deep vein thrombosis, pulmonary embolism, myocardial infarction, transfusion requirements, pneumonia, other infections, respiratory depression, and renal failure.
Results
Overall mortality was reduced by about a third in patients allocated to neuraxial blockade (103 deaths/4871 patients versus 144/4688 patients, odds ratio=0.70, 95% confidence interval 0.54 to 0.90, P=0.006). Neuraxial blockade reduced the odds of deep vein thrombosis by 44%, pulmonary embolism by 55%, transfusion requirements by 50%, pneumonia by 39%, and respiratory depression by 59% (all P<0.001). There were also reductions in myocardial infarction and renal failure. Although there was limited power to assess subgroup effects, the proportional reductions in mortality did not clearly differ by surgical group, type of blockade (epidural or spinal), or in those trials in which neuraxial blockade was combined with general anaesthesia compared with trials in which neuraxial blockade was used alone.
Conclusions
Neuraxial blockade reduces postoperative mortality and other serious complications. The size of some of these benefits remains uncertain, and further research is required to determine whether these effects are due solely to benefits of neuraxial blockade or partly to avoidance of general anaesthesia. Nevertheless, these findings support more widespread use of neuraxial blockade.
Introduction
Anaesthesia is commonly classified into two main techniques: general anaesthesia, in which gaseous or intravenous drugs achieve central neurological depression, and regional anaesthesia, in which drugs are administered directly to the spinal cord or nerves to locally block afferent and efferent nerve input.1 Regional anaesthesia for major thoracic, abdominal, or leg surgery relies on neuraxial blockade by injection of local anaesthetic drugs into either the subarachnoid space (spinal anaesthesia) or into the epidural space surrounding the spinal fluid sac (epidural anaesthesia).
The risks of fatal or life threatening events are increased several fold after major surgery, but there is debate about whether the type of anaesthesia has any substantive effect on these risks. Neuraxial blockade has several physiological effects that provide a rationale for expecting to improve outcome with this technique.2 However, the few clinical trials of epidural or spinal anaesthesia that have focused specifically on fatal or life threatening events have generally been too small to detect effects of plausible size reliably. To provide more reliable estimates of the effects of neuraxial blockade on postoperative morbidity and mortality, we conducted a systematic review of all relevant randomised trials.
Methods
Identification of trials and data collection
We sought to identify all trials in which patients were randomised to receive intraoperative neuraxial blockade (with epidural or spinal anaesthesia) or not. We did not exclude trials in adult populations in which the group receiving neuraxial blockade group also received general anaesthesia, the general anaesthesia group received postoperative neuraxial blockade, or there was more than one type of neuraxial blockade or general anaesthesia group (in which case similar groups were combined). Eligibility was not based on whether results were published, the language of publication, or the primary aims of the trial — for example, we included a randomised trial designed to assess the effects of neuraxial blockade on cognitive function.3 Trials were ineligible if they were not randomised or were quasi-randomised (such as assignment according to date of birth) or if data were not available before 1 January 1997.
We conducted a computerised search using the electronic databases Current Contents (1995-6), Embase (Excerpta Medica, 1980-96), Medline (1966-96), and the Cochrane Library (1998). We used the key words “regional anaesthesia,” “regional anesthesia,” “spinal,” or “epidural” and the Cochrane Collaboration search terms for randomised trials.4 Once papers were identified, authors' names and study titles were used as search terms. We scrutinised the reference lists of all identified papers and also hand searched selected conference proceedings.
We developed standard data collection sheets to record details of trial design, interventions, patient characteristics, and events. We did not use quality scores because analyses stratified by specific design characteristics are more informative.5 The definitions of events were those used in the original trials, since patients in one trial were directly compared only with those in the same trial. Two reviewers independently recorded the published findings from each study. This process was not blinded. A third reviewer compared the two sets of data collection sheets and any differences were resolved by discussion. We attempted to contact the authors of all trials to verify the data and obtain additional unpublished data. If there was more than one trial report, authors were also asked whether the patient groups overlapped. Lastly, we asked authors if they knew of any other relevant studies (published or unpublished).
Statistical analysis
Analysis was carried out on an intention to treat basis wherever possible. If no events were reported in the publication or by the authors, we assumed that none occurred. This assumption will generally provide unbiased estimates of proportional effects (the entity typically combined in meta-analysis) but will underestimate absolute effects.6 We calculated odds ratios, 95% confidence intervals, and two sided P values for each outcome of interest using Peto's modification of the Mantel-Haenszel method.7 Homogeneity was assessed by a χ2 test. Whenever possible, we stratified analyses of cause specific outcomes by surgical group and type of anaesthetic to determine whether these factors modified the size or direction of proportional effects. However, there were often too few trials with events for such analyses to be informative, and so subgroup analyses are mostly reported for the crude outcome of total mortality.
Results
Study characteristics
We identified 158 potentially eligible trials. Ten studies were excluded because they were quasi-randomised,8–17 and six were excluded because not all participants were randomised and separate information on the randomised patients was not available.18–23 One trial was excluded because the groups differed with respect to heparin treatment as well as anaesthetic technique.24 The remaining 141 trials that met all the inclusion criteria included a total of 9559 patients.3,25–192 More than one publication was available for 18 studies46–49,59,60,62–65,72,73,84,85 87–92,94–96,99,100,106,107,124–128,134,135,145,146,156–158,161–163,173,174,187,188 but each study was counted only once. No unpublished eligible studies were identified.
The study authors for 107 (76%) eligible trials, including 8290 (87%) patients, verified the data collection sheets. In almost all cases, we obtained additional unpublished information from contacting the authors, mostly about trial design, but also about events (for example 18 deaths were not reported in original publications). Table 1 shows the patient characteristics and anaesthetic methods and tables 2 and 3 provide summary details of outcome events. We defined a neuraxial blockade group and a non-neuraxial blockade group for each trial, which necessitated collapsing similar groups in 15 trials with more than one randomised comparison. The neuraxial blockade group had no general anaesthesia in 79 (56%) trials and the same general anaesthesia as the non-neuraxial blockade group in 37 (26%) trials. In 22 (15%) trials the neuraxial blockade group received a general anaesthesia different from that in the non-neuraxial blockade group; the systemic opioid varied in seven trials,28,34,43,84,120,186,192 the use of inhalational anaesthetic varied in two trials,71,140 the type of inhalational anaesthetic varied in two trials,148,165 the induction drug varied in one trial,191 and more than one aspect varied in 10 trials.42,76,80,81,97,151,161,168,169,189 For three (2%) trials details of the general anaesthesia method were unknown.
Table 1.
Characteristics of included studies
| First author and year of publication | No of patients randomised
|
No without mortality data
|
Mean age (years)
|
No of men
|
No with ASA status I or II
|
Type of NB* | General anaesthesia used in NB group | NB continued after surgery | Mean length of follow up (days) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NB | No NB | NB | No NB | NB | No NB | NB | No NB | NB | No NB | |||||||||
| General | ||||||||||||||||||
| Asoh 1983 | 10 | 10 | — | — | 59 | 57 | 7 | 7 | — | — | Thoracic | No | Yes | — | ||||
| Bottiglieri 1992 | 10 | 10 | — | — | — | — | — | — | — | — | Thoracic | Yes | Yes | — | ||||
| Cuschieri 1985 | 25 | 50 | 0 | 0 | 51 | 52 | 5 | 11 | — | — | Thoracic | Yes | Yes | 4 | ||||
| De Kock 1993 | 20 | 20 | — | — | 34 | 37 | 13 | 13 | — | — | Lumbar | Yes | Yes | — | ||||
| Gelman 1980 | 21 | 17 | — | — | 36 | 39 | — | — | — | — | Thoracic | Yes | Yes | — | ||||
| Godfrey 1981 | 34 | 34 | 0 | 0 | — | — | 34 | 34 | — | — | Lumbar | No | No | 30 | ||||
| Goertz 1993 | 24 | 12 | 0 | 0 | 52 | 44 | — | — | — | — | Thoracic | Yes | Yes | — | ||||
| Hendolin 1987 | 60 | 40 | 0 | 0 | 56 | 55 | 10 | 8 | — | — | Thoracic | Yes | Yes | 7 | ||||
| Hjortso 1985 | 50 | 50 | 6 | 0 | 66 | 69 | 23 | 21 | 42 | 47 | Thoracic | Yes | Yes | 10 | ||||
| Jayr 1988 | 75 | 75 | 1 | 3 | 60 | 59 | 44 | 37 | — | — | Thoracic | Yes | Yes | 5 | ||||
| Jayr 1993 | 82 | 81 | 4 | 6 | 58 | 56 | 43 | 55 | — | — | Thoracic | Yes | Yes | 17 | ||||
| Jensen 1980 | 6 | 6 | 0 | 0 | 51 | 54 | 6 | 6 | 6 | 6 | Lumbar | No | No | — | ||||
| Kausalya 1994 | 25 | 25 | — | — | 39 | 36 | — | — | 10 | 10 | Lumbar | No | No | — | ||||
| Mellbring 1983 | 25 | 25 | 0 | 0 | 62 | 61 | 13 | 19 | — | — | Thoracic | Yes | Yes | — | ||||
| Moiniche 1992 | 15 | 16 | 0 | 0 | 54 | 45 | 3 | 4 | 15 | 16 | Thoracic | Yes | Yes | 2 | ||||
| Naesh 1994 | 7 | 7 | — | — | — | — | 7 | 7 | 7 | 7 | Lumbar | No | No | — | ||||
| Naesh 1994 | 8 | 8 | — | — | 52 | 47 | 0 | 0 | 8 | 8 | Lumbar | Yes | No | 4 | ||||
| Ogata 1985 | 10 | 10 | 0 | 0 | 55 | 50 | — | — | — | — | Thoracic | Yes | — | — | ||||
| Rutberg 1984 | 16 | 8 | 0 | 0 | 43 | 43 | 0 | 0 | 16 | 8 | Thoracic | Yes | Yes | 3 | ||||
| Ryan 1992 | 57 | 43 | 12 | 8 | 65 | 66 | — | — | — | — | Thoracic | Yes | Yes | 14 | ||||
| Scheinin 1982 | 30 | 10 | 0 | 0 | — | — | 13 | 5 | — | — | Thoracic | Yes | Yes | 2 | ||||
| Seeling 1990 | 124 | 123 | 26 | 7 | 61 | 58 | 93 | 88 | 58 | 63 | Thoracic | Yes | Yes | — | ||||
| Seeling 1991 | 223 | 116 | 38 | 9 | 60 | 58 | 134 | 79 | 91 | 60 | Thoracic or lumbar | Yes | Yes | — | ||||
| Traynor 1982 | 9 | 9 | — | — | 52 | 49 | 2 | 1 | 9 | 9 | Thoracic | Yes | No | — | ||||
| Tverskoy 1990 | 12 | 24 | — | — | 54 | 56 | 12 | 24 | 12 | 24 | Spinal | No | No | — | ||||
| Watters 1993 | 12 | 8 | — | — | 64 | 65 | 4 | 8 | — | — | Lumbar | Yes | Yes | 2 | ||||
| Worsley 1988 | 47 | 51 | 0 | 0 | 53 | 53 | — | — | — | — | Spinal | Yes | No | 19 | ||||
| Yeager 1987 | 28 | 27 | 0 | 2 | 71 | 72 | — | — | — | — | Thoracic | Yes | Yes | — | ||||
| Subtotal | 1065 | 915 | 87 | 35 | 58 | 56 | 466 | 427 | 274 | 258 | 11 | |||||||
| Obstetrics and gynaecology | ||||||||||||||||||
| Abboud 1985 | 32 | 20 | 0 | 0 | 28 | 29 | 0 | 0 | — | — | Spinal or lumbar | No | No | — | ||||
| Blunnie 1983 | 15 | 30 | — | — | 42 | 41 | 0 | 0 | 15 | 30 | Spinal | Yes | No | — | ||||
| Brandt 1978 | 6 | 6 | — | — | 36 | 40 | 0 | 0 | 6 | 6 | Lumbar | No | Yes | — | ||||
| Buckley 1982 | 6 | 7 | 0 | 0 | 38 | 39 | 0 | 0 | 6 | 7 | Lumbar | Yes | Yes | — | ||||
| Christensen 1982 | 12 | 24 | — | — | — | — | 0 | 0 | — | — | Lumbar | No | — | — | ||||
| Dick 1992 | 23 | 24 | — | — | 27 | 28 | 0 | 0 | 23 | 24 | Lumbar | No | No | — | ||||
| Halevy 1978 | 14 | 18 | — | — | — | — | 0 | 0 | 14 | 18 | Lumbar | No | No | — | ||||
| Holdcroft 1979 | 15 | 37 | 0 | 0 | 32 | 30 | 0 | 0 | 32 | 30 | Lumbar | Yes | No | — | ||||
| Jensen 1977 | 9 | 9 | — | — | 42 | 45 | 0 | 0 | 9 | 9 | Lumbar | Yes | No | — | ||||
| Jordanov 1985 | 27 | 20 | 0 | 0 | 29 | 31 | 0 | 0 | 22 | 20 | Thoracic or lumbar | No | Yes | — | ||||
| Kocknover 1982 | 45 | 45 | — | — | — | — | 0 | 0 | — | — | Lumbar | Yes | No | — | ||||
| Lehtinen 1987 | 11 | 13 | 0 | 0 | 29 | 38 | 0 | 0 | 11 | 13 | Lumbar | No | No | — | ||||
| Licker 1994 | 10 | 9 | 1 | 0 | 51 | 47 | 0 | 0 | 10 | 9 | Lumbar | Yes | Yes | 5 | ||||
| Murakami 1987 | 20 | 17 | 0 | 0 | 41 | 43 | 0 | 0 | — | — | Lumbar | No | — | — | ||||
| Rem 1980 | 6 | 6 | — | — | 38 | 39 | 0 | 0 | 6 | 6 | Lumbar | No | No | — | ||||
| Simpson 1982 | 6 | 30 | 0 | 0 | 44 | 44 | 0 | 0 | 6 | 30 | Lumbar | Yes | No | 8 | ||||
| Wallace 1995 | 54 | 26 | 0 | 0 | — | — | 0 | 0 | — | — | Spinal or lumbar | No | No | — | ||||
| Wattwil 1987 | 20 | 20 | — | — | — | — | 0 | 0 | — | — | Lumbar | Yes | Yes | — | ||||
| Wessen 1994 | 10 | 10 | 0 | 0 | 43 | 45 | 0 | 0 | 10 | 10 | Lumbar | Yes | Yes | 2 | ||||
| Subtotal | 341 | 371 | 1 | 0 | 35 | 36 | 0 | 0 | 170 | 212 | 6 | |||||||
| Orthopaedic | ||||||||||||||||||
| Berggren 1987 | 28 | 29 | — | — | 78 | 77 | 4 | 7 | — | — | Lumbar | No | No | — | ||||
| Bigler 1985 | 20 | 20 | 0 | 0 | 80 | 78 | 2 | 5 | 17 | 16 | Spinal | No | No | 90 | ||||
| Bonnet 1982 | 5 | 14 | — | — | 60 | 58 | 1 | 5 | — | — | Lumbar | No | No | — | ||||
| Brendahl 1991 | 15 | 15 | 0 | 2 | 80 | 79 | 0 | 0 | 15 | 15 | Spinal | No | No | — | ||||
| Brown 1994 | 10 | 10 | 0 | 0 | 75 | 79 | 5 | 5 | 6 | 7 | Spinal | No | No | 2 | ||||
| Chin 1982 | 21 | 21 | 0 | 0 | 73 | 74 | 10 | 9 | 21 | 21 | Lumbar | Yes | No | 6 | ||||
| Christensen 1986 | 6 | 8 | 0 | 0 | 65 | 65 | — | — | — | — | Lumbar | No | Yes | — | ||||
| Couderc 1977 | 50 | 50 | — | — | 86 | 86 | 7 | 7 | — | — | Lumbar | No | No | 90 | ||||
| Dahl 1990 | 50 | 46 | 0 | 4 | 29 | 29 | 38 | 40 | 50 | 46 | Spinal | No | No | 7 | ||||
| Darling 1994 | 10 | 10 | 0 | 0 | 81 | 74 | 1 | 1 | 0 | 0 | Spinal | No | No | 360† | ||||
| Davis 1981 | 64 | 68 | 0 | 0 | 81 | 78 | 11 | 9 | 23 | 24 | Spinal | No | No | 28 | ||||
| Davis 1987 | 265 | 284 | — | — | — | — | — | — | — | — | Spinal | No | No | 28 | ||||
| Davis 1989‡ | 69 | 71 | 0 | 0 | 68 | 67 | 31 | 31 | — | — | Spinal | No | No | 14 | ||||
| Donadoni 1988 | 51 | 29 | 0 | 0 | 62 | 67 | — | — | 0 | 0 | Lumbar | Yes | Yes | 2 | ||||
| Fredin 1986 | 30 | 30 | 2 | 2 | 67 | 66 | 11 | 8 | — | — | Lumbar | No | Yes | — | ||||
| Hedenstierna 1986 | 8 | 8 | 0 | 0 | 64 | 66 | 6 | 4 | — | — | Spinal | No | No | — | ||||
| Hole 1980 | 29 | 31 | 0 | 0 | 70 | 72 | 10 | 11 | 27 | 29 | Lumbar | No | No | 300 | ||||
| Hole 1983 | 13 | 14 | — | — | — | — | — | — | — | — | Lumbar | No | Yes | — | ||||
| Hole 1984 | 10 | 10 | 0 | 0 | 62 | 64 | 4 | 1 | 10 | 9 | Lumbar | No | Yes | 24 | ||||
| Hole 1984 | 10 | 10 | 0 | 0 | 67 | 70 | 3 | 3 | 8 | 8 | Lumbar | No | Yes | — | ||||
| Jakobsen 1986 | 15 | 15 | 0 | 0 | 72 | 72 | — | — | — | — | Lumbar | No | Yes | — | ||||
| Jones 1990 | 76 | 75 | 2 | 3 | — | — | 20 | 19 | — | — | Spinal | No | No | 90 | ||||
| Jorgensen 1991 | 24 | 24 | 0 | 0 | 69 | 64 | 8 | 8 | — | — | Lumbar | No | Yes | 360 | ||||
| Keith 1977 | 10 | 17 | — | — | 61 | 64 | 5 | 3 | — | — | Lumbar | No | No | — | ||||
| Mann 1983 | 30 | 30 | 0 | 0 | 71 | 70 | 18 | 16 | 10 | 12 | Spinal | No | No | 180 | ||||
| Maurette 1988 | 18 | 15 | 0 | 0 | 81 | 85 | — | — | 18 | 15 | Spinal | No | No | — | ||||
| McKenzie 1984 | 75 | 75 | 6 | 2 | 75 | 74 | 8 | 17 | 38 | 34 | Spinal | No | No | 365 | ||||
| McLaren 1982 | 56 | 60 | — | — | — | — | — | — | — | — | Spinal | No | No | 30 | ||||
| Modig 1980 | 15 | 15 | 0 | 0 | 67 | 65 | 8 | 7 | 15 | 15 | Lumbar | No | Yes | 30 | ||||
| Modig 1986 | 50 | 50 | 2 | 4 | 65 | 66 | 27 | 22 | 48 | 46 | Lumbar | No | Yes | 30 | ||||
| Modig 1987 | 14 | 24 | 0 | 0 | 67 | 67 | 5 | 13 | 14 | 24 | Lumbar | No | Yes | 30 | ||||
| Nielsen 1989 | 10 | 20 | — | — | 34 | 38 | 5 | 10 | 5 | 10 | Lumbar | No | No | — | ||||
| Nielsen 1990 | 25 | 39 | — | — | — | — | — | — | — | — | Spinal | No | — | — | ||||
| Pedersen 1986 | 15 | 15 | 0 | 0 | 72 | 72 | 9 | 10 | — | — | Lumbar | No | Yes | — | ||||
| Poll 1988 | 24 | 26 | 0 | 0 | — | — | — | — | — | — | Lumbar | Yes | Yes | — | ||||
| Racle 1986 | 35 | 35 | 0 | 0 | 82 | 82 | 0 | 0 | — | — | Spinal | No | No | 30 | ||||
| Riis 1983 | 20 | 10 | — | — | 70 | 70 | — | — | — | — | Lumbar | Yes | Yes | 90 | ||||
| Seitz 1985 | 10 | 10 | 0 | 0 | — | — | 10 | 10 | — | — | Lumbar | No | No | — | ||||
| Sharrock 1992 | 11 | 10 | — | — | — | — | — | — | — | — | Lumbar | No | Yes | — | ||||
| Stathopoulou 1992 | 26 | 31 | 0 | 0 | 56 | 56 | 11 | 20 | 26 | 31 | Spinal | No | No | — | ||||
| Tulla 1992 | 10 | 10 | 0 | 0 | 61 | 59 | 5 | 5 | 8 | 10 | Spinal | No | No | 4 | ||||
| Valentin 1986§ | 281 | 297 | — | — | 79 | 79 | 58 | 59 | 192 | 182 | Spinal | No | No | — | ||||
| White 1980 | 20 | 40 | 0 | 4 | 78 | 79 | 1 | 7 | 8 | 18 | Spinal | Yes | No | 28 | ||||
| Williams-Russo 1995 | 134 | 128 | 0 | 0 | 69 | 69 | 40 | 38 | — | — | Lumbar | No | Yes | 180 | ||||
| Subtotal | 1768 | 1849 | 12 | 21 | 71 | 71 | 382 | 410 | 559 | 572 | 84 | |||||||
| Urology | ||||||||||||||||||
| Asbjorn 1989§ | 20 | 20 | 0 | 0 | 69 | 69 | 20 | 20 | 20 | 20 | Lumbar | No | Yes | 21 | ||||
| Chung 1987 | 20 | 24 | — | — | 73 | 72 | 9 | 12 | — | — | Spinal | No | No | — | ||||
| Chung 1989 | 22 | 22 | — | — | 72 | 72 | 22 | 22 | 13 | 14 | Spinal | No | No | — | ||||
| Dobson 1994 | 11 | 11 | — | — | 77 | 72 | 11 | 11 | 11 | 11 | Spinal | No | No | — | ||||
| Edwards 1995 | 52 | 48 | — | — | — | — | 52 | 48 | — | — | Spinal | No | No | — | ||||
| Foate 1985 | 8 | 9 | — | — | 69 | 69 | 8 | 9 | — | — | Spinal | No | No | — | ||||
| Frank 1994 | 15 | 15 | 0 | 0 | 61 | 62 | 15 | 15 | 15 | 15 | Lumbar | No | Yes | 0 | ||||
| Hendolin 1981 | 17 | 21 | — | — | 71 | 67 | 17 | 21 | — | — | Lumbar | No | Yes | — | ||||
| Henny 1986 | 10 | 10 | — | — | 62 | 62 | 10 | 10 | — | — | Lumbar | No | Yes | — | ||||
| Jenkins 1983 | 7 | 8 | — | — | 68 | 68 | 7 | 8 | — | — | Lumbar | No | No | — | ||||
| McGowan 1980 | 50 | 100 | 0 | 0 | — | — | 50 | 100 | — | — | Spinal | No | No | 7 | ||||
| Melsen 1987 | 45 | 59 | 0 | 0 | 68 | 64 | 36 | 53 | 45 | 59 | Lumbar | No | No | — | ||||
| Nielsen 1987 | 25 | 20 | 7 | 2 | — | — | — | — | — | — | Lumbar | No | No | — | ||||
| Poikolainen 1983 | 17 | 21 | — | — | — | — | — | — | — | — | Lumbar | No | No | — | ||||
| Rickford 1988 | 53 | 25 | — | — | 45 | 46 | 31 | 13 | 31 | 13 | Spinal or lumbar | No | No | — | ||||
| Shir 1994 | 69 | 34 | — | — | — | — | — | — | — | — | Lumbar | Yes | Yes | — | ||||
| Stjernstrom 1985 | 15 | 10 | — | — | 71 | 66 | 15 | 10 | 15 | 10 | Lumbar | No | No | — | ||||
| Whelan 1982 | 7 | 8 | — | — | 64 | 66 | 7 | 8 | — | — | Spinal | No | No | — | ||||
| Subtotal | 463 | 465 | 7 | 2 | 64 | 65 | 310 | 360 | 150 | 142 | 10 | |||||||
| Vascular | ||||||||||||||||||
| Baron 1991 | 87 | 86 | 6 | 0 | 61 | 62 | 70 | 81 | — | — | Thoracic | Yes | Yes | — | ||||
| Bode 1996 | 285 | 138 | 0 | 0 | 68 | 68 | 40 | 81 | 0 | 0 | Spinal or lumbar | Yes | Yes | — | ||||
| Bonnet 1989 | 10 | 11 | — | — | 63 | 64 | 9 | 11 | — | — | Thoracic | Yes | No | — | ||||
| Borovskikh 1990 | 50 | 50 | 0 | 0 | 56 | 55 | 50 | 50 | — | — | Thoracic | No | Yes | 30 | ||||
| Christopherson 1993 | 49 | 51 | 0 | 0 | 64 | 66 | 30 | 27 | 6 | 6 | Lumbar | No | Yes | 180 | ||||
| Cook 1986 | 50 | 51 | 0 | 0 | 66 | 67 | 35 | 36 | 19 | 20 | Spinal | No | No | 365 | ||||
| Damask 1990 | 9 | 10 | — | — | 71 | 64 | 6 | 8 | — | — | Lumbar | No | No | — | ||||
| Davies 1993 | 25 | 25 | 0 | 0 | 65 | 67 | 23 | 21 | — | — | Thoracic | Yes | Yes | 7 | ||||
| Garnett 1996 | 55 | 56 | 7 | 5 | 68 | 69 | 37 | 43 | 0 | 0 | Lumbar | Yes | Yes | — | ||||
| Gold 1994 | 12 | 12 | 0 | 0 | 73 | 71 | 9 | 9 | 0 | 0 | Lumbar | Yes | Yes | 8 | ||||
| Gottlieb 1988 | 20 | 15 | — | — | — | — | — | — | — | — | Lumbar | Yes | Yes | — | ||||
| Haljamae 1988 | 27 | 28 | — | — | 65 | 60 | 19 | 20 | — | — | Lumbar | Yes | No | — | ||||
| Homann 1984 | 19 | 38 | — | — | 46 | 41 | 8 | 13 | — | — | Lumbar | No | No | — | ||||
| Houweling 1993 | 40 | 20 | 0 | 0 | 65 | 65 | 32 | 15 | — | — | Spinal or lumbar | Yes | Yes | 10 | ||||
| Kossman 1982 | 9 | 10 | — | — | — | — | — | — | — | — | Thoracic | Yes | Yes | — | ||||
| Reinhart 1989 | 35 | 70 | — | — | 63 | 61 | 25 | 52 | 13 | 28 | Thoracic | Yes | Yes | 5 | ||||
| Rosseel 1985 | 9 | 9 | — | — | 67 | 65 | 8 | 8 | 0 | 0 | Thoracic | Yes | No | — | ||||
| Seeling 1985 | 25 | 26 | 1 | 0 | 62 | 62 | 22 | 24 | 11 | 14 | Thoracic | Yes | Yes | — | ||||
| Smeets 1993 | 6 | 5 | 1 | 0 | 62 | 65 | 6 | 5 | — | — | Thoracic | Yes | Yes | — | ||||
| Stenseth 1994 | 20 | 10 | 0 | 0 | 55 | 54 | 20 | 10 | 0 | 0 | Thoracic | Yes | Yes | 6 | ||||
| Truman 1991 | 40 | 40 | 0 | 0 | 70 | 66 | 17 | 15 | 0 | 0 | Thoracic | Yes | Yes | 20 | ||||
| Wust 1980 | 23 | 45 | — | — | 58 | 60 | 20 | 41 | 12 | 18 | Thoracic | Yes | No | — | ||||
| Subtotal | 905 | 806 | 15 | 5 | 65 | 63 | 486 | 570 | 61 | 86 | 94 | |||||||
| Other surgery | ||||||||||||||||||
| Brichon 1994 | 46 | 33 | — | — | 53 | 45 | — | — | — | — | Thoracic | Yes | Yes | — | ||||
| Bromage 1971 | 22 | 22 | — | — | 43 | 48 | — | — | — | — | Thoracic | Yes | Yes | — | ||||
| Ghoneim 1988 | 52 | 53 | — | — | 62 | 60 | 35 | 35 | — | — | Spinal or lumbar | No | No | 90 | ||||
| Hasenbos 1985 | 83 | 80 | 0 | 0 | 42 | 36 | 65 | 60 | 21 | 14 | Thoracic | Yes | Yes | 4 | ||||
| Jia 1985 | 67 | 31 | — | — | — | — | — | — | — | — | — | — | — | — | ||||
| Merhav 1993 | 16 | 15 | — | — | 40 | 46 | 14 | 11 | — | — | Spinal | No | No | — | ||||
| Ogata 1988 | 8 | 13 | — | — | — | — | — | — | — | — | Thoracic | Yes | — | — | ||||
| Ravin 1971 | 10 | 10 | — | — | 71 | 70 | — | — | — | — | Spinal | No | No | — | ||||
| Slinger 1995 | 15 | 15 | — | — | 65 | 62 | 12 | 11 | — | — | Lumbar | Yes | Yes | 3 | ||||
| Zwarts 1989 | 10 | 10 | — | — | 38 | 50 | 5 | 8 | — | — | Thoracic | Yes | Yes | — | ||||
| Subtotal | 329 | 282 | 0 | 0 | 50 | 48 | 131 | 125 | 21 | 14 | 34 | |||||||
| Total | 4871 | 4688 | 122 | 63 | 63 | 62 | 1775 | 1892 | 1235 | 1284 | 62 | |||||||
NB=neuraxial blockade.
In excluded patients only.
11 patients were entered twice into this study.
=The total number randomised was not available.Those presented are the numbers included in the study after exclusions and losses to follow up.
Table 2.
Summary of vascular events and bleeding
| Group | Vascular events
|
Bleeding
|
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Deep vein thrombosis
|
Pulmonary embolism
|
Myocardial infarction
|
Cardiac arrhythmia
|
Other fatal cardiac event
|
Stroke
|
Perioperative transfusion requiring >2 units red cells
|
Postoperative bleed requiring transfusion
|
||||||||||||||||
| NB | No NB | NB | No NB | NB | No NB | NB | No NB | NB | No NB | NB | No NB | NB | No NB | NB | No NB | ||||||||
| General | 26 | 24 | 3 | 5 | 0 | 4 | 3 | 4 | 0 | 0 | 0 | 0 | 61 | 80 | 0 | 0 | |||||||
| Orthopaedics | 117 | 184 | 27 | 59 | 7 | 19 | 36 | 41 | 6 | 3 | 17 | 16 | 81 | 125 | 21 | 57 | |||||||
| Urology | 2 | 11 | 0 | 1 | 3 | 6 | 1 | 0 | 0 | 0 | 0 | 2 | 12 | 32 | 0 | 0 | |||||||
| Vascular | 0 | 0 | 0 | 1 | 35 | 30 | 19 | 31 | 3 | 1 | 2 | 5 | 38 | 41 | 9 | 11 | |||||||
| Other | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 1 | 1 | |||||||
| Total | 145 | 220 | 30 | 66 | 45 | 59 | 59 | 76 | 9 | 4 | 19 | 23 | 193 | 280 | 31 | 69 | |||||||
NB=neuraxial blockade.
Table 3.
Summary of infection, other events, and mortality
| Group | Infection
|
Other events
|
Mortality
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wound infection
|
Pneumonia
|
Death from other infective cause
|
Respiratory depression
|
Renal failure
|
Total mortality
|
No of intraoperative deaths
|
No of deaths between 30 days and 6 months
|
||||||||||||||||
| NB | No NB | NB | No NB | NB | No NB | NB | No NB | NB | No NB | NB | No NB | NB | No NB | NB | No NB | ||||||||
| General | 17 | 13 | 64 | 99 | 2 | 1 | 16 | 14 | 1 | 3 | 18 | 18 | 0 | 0 | 0 | 1 | |||||||
| Orthopaedics | 9 | 14 | 63 | 84 | 0 | 1 | 0 | 1 | 10 | 14 | 58 | 89 | 0 | 1 | 57 | 66 | |||||||
| Urology | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 4 | 6 | 0 | 0 | 0 | 0 | |||||||
| Vascular | 2 | 4 | 22 | 55 | 0 | 8 | 10 | 22 | 7 | 15 | 23 | 31 | 1 | 4 | 3 | 3 | |||||||
| Other | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||||
| Total | 29 | 33 | 149 | 238 | 2 | 10 | 26 | 38 | 18 | 32 | 103 | 144 | 1 | 5 | 60 | 70 | |||||||
NB= neuraxial blockade.
Among the 56 trials for which follow up data were available, the mean duration of follow up was about 62 days. Only 13 trials provided follow up data beyond 30 days postoperatively. No events were recorded in 80 trials involving 2941 participants, which were mostly designed to assess the physiological, biochemical, and endocrine effects of neuraxial blockade. The mean follow up in the first 30 days these trials was 11 days, compared with 21 days in trials in which events were observed.
Overall mortality
A total of 247 deaths within 30 days of randomisation were recorded in 35 trials. Overall mortality was about one third less in the neuraxial blockade group (odds ratio 0.70, 95% confidence interval 0.54 to 0.90, P=0.006; fig 1) with no clear difference between different surgical groups (fig 2). A specific diagnosis was available for 162 of the deaths. Of these, 73 (45%) were due to pulmonary embolism, cardiac events, or stroke, 50 (31%) were due to infective causes, and 39 (24%) were due to other causes. The observed improvement in survival was due to trends towards reductions in deaths from pulmonary embolism, cardiac events, or stroke (0.73, 0.45 to 1.16), deaths from infection (0.68, 0.39 to 1.21), deaths from other causes (0.84, 0.44 to 1.61), and deaths from unknown causes (0.64, 0.41 to 1.01). There was about one fewer death per 100 patients in the 30 days after randomisation in the neuraxial blockade group (103/4871 (2.1%) versus 144/4688 (3.1%)). Only six intraoperative deaths were recorded, one of which was in the neuraxial blockade group (0.28, 0.06 to 1.45). Ten studies, with a total of 1371 patients, recorded 130 deaths between 30 days and six months. All but two of these studies were on orthopaedic patients. Overall, there was no clear effect of neuraxial blockade on deaths during this period (0.89, 0.61 to 1.28).
Figure 1.
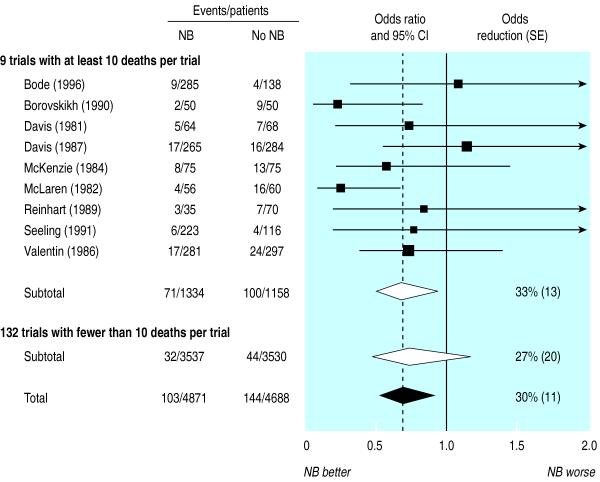
Effect of neuraxial blockade (NB) on postoperative mortality within 30 days of randomisation. Diamonds denote 95% confidence intervals for odds ratios of combined trial results. The vertical dashed line represents the overall pooled result. Size of shaded boxes is proportional to number of events. The overall event rates after adjusting for uneven randomisation193 were 113/5811 (1.9%) versus 158/5667 (2.8%). χ2 test for heterogeneity between individual trials P=0.5
Figure 2.
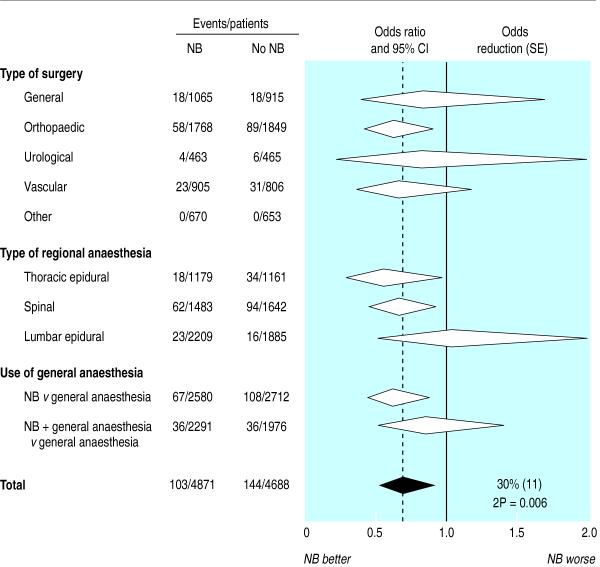
Effect of neuraxial blockade (NB) on postoperative mortality, by surgical group, type of neuraxial blockade, and use of general anaesthesia. Obstetrics and gynaecology trials are included with other surgery. One trial with unknown details of anaesthesia was grouped with lumbar epidural and neuraxial blockade plus general anaesthesia versus general anaesthesia comparisons. Diamonds denote 95% confidence intervals for odds ratios of combined trial results. The vertical dashed line represents the overall pooled result. Size of shaded boxes is proportional to number of events. χ2 test for heterogeneity between different surgical groups, P=0.9
Mortality results by type of anaesthesia
Seven trials (with 826 participants) directly randomised patients to spinal or epidural anaesthesia.25,32,77,104,153,181 Only 13 deaths occurred in these trials, four in the spinal group. However, an indirect comparison between trials of spinal and epidural anaesthesia showed no clear difference between their effects on total mortality (0.68, 0.49 to 0.95 for spinal anaesthesia and 0.68, 0.43 to 1.07 for epidural anaesthesia, P for homogeneity=1.0; fig 2). Mortality was reduced overall whether neuraxial blockade was continued postoperatively (0.68, 0.43 to 1.08) or not (0.70, 0.51 to 0.97). The effect on total mortality was not clearly lower in trials in which neuraxial blockade was combined with general anaesthesia (0.87, 0.53 to 1.41) than in trials in which neuraxial blockade was used alone (0.64, 0.47 to 0.87; P for homogeneity=0.3; fig 2). However, the confidence intervals were wide for the trials that used general anaesthesia. Forty four (18%) deaths occurred in the 22 trials in which the neuraxial blockade group had a different general anaesthesia to that used in the group not allocated neuraxial blockade. The overall effect in this group of trials (0.92, 0.49 to 1.71) was not clearly different (P for homogeneity=0.3) from that in other trials (0.66, 0.49 to 0.88).
Venous thromboembolism, cardiac events, and stroke
A total of 365 deep vein thromboses were reported from 18 trials. Neuraxial blockade reduced the risk of deep vein thrombosis by almost half (0.56, 0.43 to 0.72; fig 3). Since more than 80% of deep vein thromboses were recorded in orthopaedic trials, there was limited power to detect differences between surgical groups. In nine trials all patients were screened for deep vein thromboses by fibrinogen scanning,59,87,129 venography,74,114,132,187 or a combination of methods.62,94 Proportional reductions in deep vein thromboses were similar in the trials with screening (0.56, 0.42 to 0.75) compared with other trials (0.54, 0.30 to 0.96). Therefore, absolute differences were much greater in the trials with screening (121/463 (26%) for neuraxial blockade versus 178/467 (38%) for no neuroaxial blockade) than in other trials (24/4408 (0.5%) versus 42/4221 (1.0%)). Outcome assessments were known to be blinded in only two trials, and deep vein thromboses were also reduced in these studies (0.46, 0.21 to 0.99).66,98 A total of 96 pulmonary emboli were reported from 23 trials, 21 (22%) of which were fatal. Overall, there were about half as many pulmonary emboli in patients allocated to neuraxial blockade (0.45, 0.29 to 0.69; fig 3).
Figure 3.
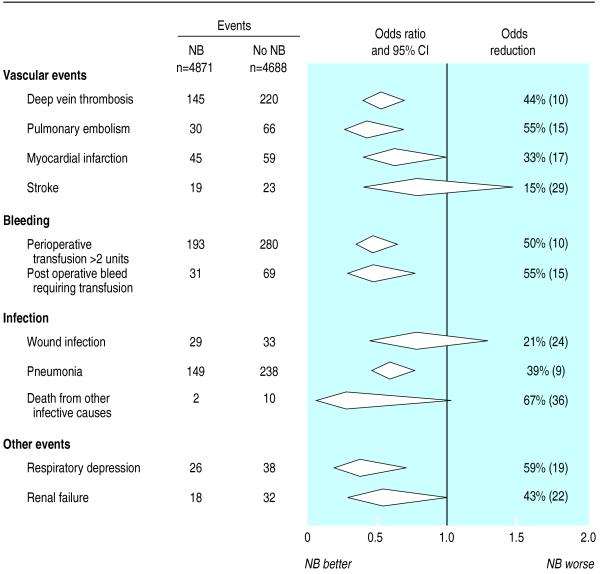
Effects of neuraxial blockade (NB) on postoperative complications. Diamonds denote 95% confidence intervals for odds ratios of combined trial results. The vertical dashed line represents the overall pooled result. Size of shaded boxes is proportional to number of events
A total of 104 myocardial infarctions were reported in 30 trials. Overall, there were about one third fewer myocardial infarctions in patients allocated to neuraxial blockade, but the confidence intervals were compatible with both no effect and a halving in risk (0.67, 0.45 to 1.00; fig 3). Only 42 strokes were reported from eight trials, and the confidence intervals were very wide for this outcome (0.85, 0.46 to 1.57; fig 3).
Bleeding
In total, 473 patients from 16 trials required transfusion of two or more units of blood and 100 patients from 12 trials had a postoperative bleed requiring a transfusion. The requirement for a transfusion of two or more units of blood was reduced by about half in patients allocated neuraxial blockade (0.50, 0.39 to 0.66; fig 3). A similar proportional reduction was found for postoperative bleeds requiring a transfusion (0.45, 0.29 to 0.70; fig 3). There was no clear difference in the proportional effects on either outcome across surgical groups.
Postoperative infection
In total, 62 wound infections were reported from 14 trials. There were fewer wound infections in those allocated to neuraxial blockade, although the confidence intervals were wide (0.79, 0.47 to 1.33; fig 3). Three hundred and eighty seven cases of pneumonia were recorded in 28 trials, of which 38 (10%) were fatal. The risk of developing pneumonia was less in patients randomised to neuraxial blockade (0.61, 0.48 to 0.76; fig 3). There was no clear difference in the proportional effects with the use of concomitant general anaesthesia (neuraxial blockade versus general anaesthesia: 0.63, 0.46 to 0.87; neuraxial blockade plus general anaesthesia versus general anaesthesia: 0.59, 0.42 to 0.81). However, there was some evidence (P for homogeneity=0.05) that the proportional reduction in pneumonia was greater after thoracic epidural anaesthesia (0.48, 0.35 to 0.67) than after lumbar epidural or spinal anaesthesia (0.76, 0.55 to 1.04). Twelve deaths due to an infective cause other than pneumonia were recorded in six trials, of which two occurred in patients allocated to neuraxial blockade (0.33, 0.10 to 1.07; fig 3).
Other postoperative events
A total of 64 cases of respiratory depression were reported from eight trials. The odds of respiratory depression were reduced by 59% in patients allocated to neuraxial blockade (0.41, 0.23 to 0.73; fig 3). The effect was present in trials with and without concomitant general anaesthesia (neuraxial blockade alone versus general anaesthesia 0.37, 0.11 to 1.21; neuraxial blockade plus general anaesthesia versus general anaesthesia 0.43, 0.22 to 0.81). Fifty cases of renal failure were recorded in 10 trials. Although the risk of renal failure was reduced in patients randomised to neuraxial blockade, the confidence intervals were wide and compatible with both no effect and a two thirds reduction (0.57, 0.32 to 1.00; fig 3).
Sensitivity analyses
We conducted several analyses to assess whether the effects on total mortality were dependent on trials with methodological problems or affected by the type of anaesthesia. However, all these tests lacked power to detect moderate sized differences.
An overall reduction in mortality was still evident after we excluded studies for which the total number of patients originally randomised was not available (0.68, 0.51 to 0.91)26,180; original authors could not be contacted (0.69, 0.53 to 0.90)36,38,40,82,83,86,103,115,118,131,137–144,147,150,153,155,166,171,172,179,181,185,190; more than 5% of all patients were lost to follow up or excluded after randomisation (0.69, 0.51 to 0.91) 3,14,32,38,57,62,71,74,75,94,108,113,114,120,129,130,140,159,164,165,171,173,181,187; or more than 5% of the neuraxial blockade group were excluded after randomisation (0.68, 0.51 to 0.91).28,32,57,75,94,113,120,129,130,140,159,164,165,171,173 The reduction in mortality was also evident after exclusion of two trials that were stopped before scheduled completion (0.70, 0.53 to 0.91) and exclusion of unpublished data (0.67, 0.51 to 0.88).28,46,94,109,130,165 Finally, there was no clear evidence of publication bias from tests for trend across groups defined by trial size.
Discussion
Our overview shows improved survival in patients randomised to neuraxial blockade. Additionally, we found reductions in risk of venous thromboembolism, myocardial infarction, bleeding complications, pneumonia, respiratory depression, and renal failure. There was no clear evidence that these effects, in proportional terms, differed by the type of surgical group or the type of neuraxial blockade, although there was limited power to assess subgroup effects reliably. Furthermore, there was no evidence of “catch up” mortality in the neuraxial blockade group between 30 days and 6 months.
The benefits seen for neuraxial blockade may be conferred by multifactorial mechanisms, including altered coagulation, increased blood flow, improved ability to breathe free of pain, and reduction in surgical stress responses.2 In particular, major surgery induces a “stress response” that is substantially altered by neuraxial blockade but not by general anaesthesia.2 This observation, together with the subgroup comparisons shown here, suggests that these benefits are principally due to the use of neuraxial blockade rather than avoidance of general anaesthesia. Thus the key issue seems to be whether neuraxial blockade is used or not, and the way in which this is achieved is less relevant.
Validity of findings
It is unlikely that bias could explain much of the reduction in mortality. We included all randomised trials, irrespective of their initial aims or reported findings. Most trials were not designed to assess major events, but it is unlikely that we missed many deaths or major non-fatal events because we contacted the authors of trials involving 87% of patients and few patients had no outcome data. However, incidence will have been underestimated for non-fatal events that often go undiagnosed, such as deep vein thrombosis. This finding will not bias relative risk estimates6 unless information is selectively available from trials with extreme results. For deep vein thrombosis, at least, the proportional effect of neuraxial blockade in trials designed to assess this outcome was similar to that in other trials. With regard to other potential biases, lack of blinding may have caused some selective misdiagnosis of non-fatal events, but analyses did not indicate publication bias and the overall reduction in mortality was not dependent on inclusion of trials with unconfirmed data or trials for which intention to treat analyses were not possible. Lastly, even though these data represent most of the randomised evidence potentially available, the confidence intervals were wide for many outcomes and relatively little information was available about cause of death.
If the proportional effects of neuraxial blockade are consistent in different patient populations, neuraxial blockade would be expected to result in about one fewer postoperative death and several fewer major complications for every 100 patients at similar risk to those in the studies. However, even though such benefits would be widely regarded as clinically important, the largest individual trial to date180 did not have the power to reliably detect effects of this size. Lack of statistical power may therefore be the principal reason why previous individual trials, editorials,194 and meta-analyses of trials in hip fracture patients195,196 have concluded that neuraxial blockade had no important effect on mortality.
Implications
Our overview indicates that neuraxial blockade reduces major postoperative complications in a wide range of patients. However, uncertainty about the net benefits of neuraxial blockade is likely to remain among some clinicians and for some patient groups. For example, opinion is divided about whether neuraxial blockade is indicated or contraindicated in patients at risk of cardiac complications,197 and it is unclear whether the differences that we observed reflect the benefits of neuraxial blockade alone or are partly due to the avoidance of the adverse effects of general anaesthesia. Such uncertainties provide the rationale for large randomised trials, such as the ongoing multicentre Australian study of epidural anaesthesia and analgesia in major surgery.198 However, since serious complications associated with neuraxial blockade, such as spinal haematoma, are very rare199–201 and more common side effects, such as headache or urinary retention, are not life threatening, our data support recent trends towards increased use of neuraxial blockade. Furthermore, although we focused on intraoperative anaesthetic techniques, postoperative neuraxial blockade has been shown to have additional benefits, at least for pulmonary complications.202 Overall, therefore our data should result in more widespread use of spinal or epidural anaesthesia.
What is already known on this topic
Neuraxial blockade with epidural or spinal anaesthesia reduces the incidence of deep vein thrombosis and one month mortality in hip fracture patients
Insufficient evidence exists for other postoperative outcomes in this surgical group
What this study adds
Mortality was reduced by one third in patients allocated neuraxial blockade
Reductions in mortality did not differ by surgical group, type of blockade, or in trials in which neuraxial blockade was combined with general anaesthesia
Neuraxial blockade also reduced the risk of deep vein thrombosis, pulmonary embolism, transfusion requirements, pneumonia, respiratory depression, myocardial infarction, and renal failure
Acknowledgments
We thank all trialists who confirmed data and provided extra information for this overview: T K Abboud, A R Aitkenhead, T Asoh, J F Baron, A Bayer, D Berggren, P Berthelsen, D Bigler, P K Bithal, W P Blunnie, R Bode, F Bonnet, N A Borovskikh, M R Brandt, S Bredbacka, M J Breslow, F P Buckley, K S Channer, S P Chin, R Christopherson, F Chung, E Couderc, R J Cuschieri, J B Dahl, F M Davies, M J Davies, M Davis, M De Kock, J Devulder, W Dick, N D Edwards, S M Frank, R L Garnett, S Gelman, S P Gerrish, M M Ghoneim, M S Gold, A Gottlieb, E Hakansson, M Hasenbos, H Hendolin, S W Henneberg, A Holdcroft, A Hole, R Hosoda, P L Houweling, A O Hughes, C Jayr, J Jenkins, N Jia, R D M Jones, L N Jorgensen, J Kanto, H Kehlet, A Lehtinen, M Licker, R A M Mann, P Maurette, S McGowan, P J McKenzie, A D McLaren, G Mellbring, N Melsen, I Milsom, J Modig, S Moiniche, I Murat, J M Murray, J A Odoom, M S J Pathy, J Pedersen, J S Poll, A V Pollock, J P Racle, S Raja, K Reinhart, H Renck, B Rosberg, B A Rosenfeld, H Rutberg, P Ryan, B Scheinin, W Seeling, N Sharrock, I Smilov, T Stathopoulou, R Stenseth, V I Strashnov, J Takala, J Takeda, M V Tseshinsky, H Tsuji, K J Tuman, N Valentin, J M Watters, L G Welborn, A Wessen, I W C White, C Wiessman, P Williams-Russo, M P Yeager, and O N Zabrodin. We thank Iain Chalmers, Rory Collins, Mike Davis, Konrad Jamrozik, John McCall, Tom Pedersen, John Rigg, and Charles Warlow for their helpful comments and Gary Whitlock, Xin-Hua Zhang, Philippa Day, and Valentine Kravtsov for help with translating papers.
Footnotes
Funding: Health Research Council of New Zealand and Astra Pain, New Zealand. NW undertook this research during the tenure of a training fellowship from the Health Research Council of New Zealand. AR is a senior research fellow of the National Heart Foundation of New Zealand.
Competing interests: HK has received fees for consulting and speaking at meetings from AstraZeneca.
References
- 1.Cousins M, Bridenbaugh P, editors. Neural blockade in clinical anesthesia and management of pain. 2nd ed. Philadelphia: J B Lippincott; 1988. [Google Scholar]
- 2.Kehlet H. Modification of responses to surgery by neural blockade: clinical implications. In: Cousins M, Bridenbaugh P, editors. Neural blockade in clinical anesthesia and management of pain. 2nd ed. Philadelphia: J B Lippincott; 1988. pp. 145–188. [Google Scholar]
- 3.Jones M, Piggott S, Vaughan R, Bayer A, Newcombe R, Twining T, et al. Cognitive and functional competence after anaesthesia in patients aged over 60: controlled trial of general and regional anaesthesia for elective hip or knee replacement. BMJ. 1990;300:1683–1687. doi: 10.1136/bmj.300.6741.1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dickersin K, Larson K. Establishing and maintaining an international register of RCTs. Oxford: Cochrane Collaboration; 1995. [Google Scholar]
- 5.Greenland S. Quality scores are useless and potentially misleading. Am J Epidemiol. 1994;140:300–301. [Google Scholar]
- 6.Rodgers A, MacMahon S. Systematic underestimation of treatment effects as a result of diagnostic test inaccuracy: implications for the interpretation and design of thromboprophylaxis trials. Thromb Haemost. 1995;73:167–171. [PubMed] [Google Scholar]
- 7.Yusuf S, Peto R, Lewis J, Collins R, Sleight P. Beta blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis. 1985;27:335–371. doi: 10.1016/s0033-0620(85)80003-7. [DOI] [PubMed] [Google Scholar]
- 8.Bredbacka S, Blomback M, Hagnevik K, Irestedt L, Raabe N. Per-and postoperative changes in coagulation and fibrinolytic variables during abdominal hysterectomy under epidural or general anaesthesia. Acta Anaesthesiol Scand. 1986;30:204–210. doi: 10.1111/j.1399-6576.1986.tb02397.x. [DOI] [PubMed] [Google Scholar]
- 9.Gregoretti S. Comparison of water, electrolyte and nitrogen balance in the postoperative period after epidural or general anesthesia: a randomised study of patients undergoing hysterectomy. Minerva Anestesiol. 1985;51:87–91. [PubMed] [Google Scholar]
- 10.Jia N, Guo H, San Y, Liu L. Comparison of changes in plasma catecholamines between general anesthesia and general anesthesia plus epidural block. Acta Acad Med Sinicae. 1991;13:112–114. [PubMed] [Google Scholar]
- 11.Konishi M, Yamada M, Yamada T, Noguchi J, Takeda J. The effects of halothane and epidural anesthesia on the gastric intramural pH and the pH of the gastric juice. Masui. 1989;38:329–333. [PubMed] [Google Scholar]
- 12.Mitchell D, Friedman RJ, Baker JD, Cooke JE, Darcy MD, Miller MC. Prevention of thromboembolic disease following total knee arthroplasty. Epidural versus general anesthesia. Clin Orthop. 1991;269:109–112. [PubMed] [Google Scholar]
- 13.Modig J, Malmberg P, Karlstrom G. Effect of epidural versus general anaesthesia on calf blood flow. Acta Anaesthesiol Scand. 1980;24:305–309. doi: 10.1111/j.1399-6576.1980.tb01553.x. [DOI] [PubMed] [Google Scholar]
- 14.Modig J, Hjelmstedt A, Sahlstedt B, Maripuu E. Comparative influences of epidural and general anaesthesia on deep venous thrombosis and pulmonary embolism after total hip replacement. Acta Chir Scand. 1981;147:125–130. [PubMed] [Google Scholar]
- 15.Modig J, Borg T, Karlstrom G, Maripuu E, Sahlstedt B. Thromboembolism after total hip replacement: role of epidural and general anesthesia. Anesth Analg. 1983;62:174–180. [PubMed] [Google Scholar]
- 16.Perhoniemi V, Linko K. Hemodynamics of the legs and clinical symptoms following regional blocks for transurethral surgery. Eur Urol. 1986;12:244–248. doi: 10.1159/000472628. [DOI] [PubMed] [Google Scholar]
- 17.Wickstrom I, Holmberg I, Stefansson T. Survival of female geriatric patients after hip fracture surgery. A comparison of 5 anesthetic methods. Acta Anaesthesiol Scand. 1982;26:607–614. doi: 10.1111/j.1399-6576.1982.tb01825.x. [DOI] [PubMed] [Google Scholar]
- 18.Asoh T, Tsuji H. Post-operative complications of gastrectomy in patients with gastric cancer. (Unpublished.)
- 19.Rosberg B, Fredin H, Gustafson C. Anaesthetic techniques and surgical blood loss in total hip arthroplasty. Acta Anaesthesiol Scand. 1982;26:189–193. doi: 10.1111/j.1399-6576.1982.tb01751.x. [DOI] [PubMed] [Google Scholar]
- 20.Shirasaka C, Tsuji H, Asoh T, Takeuchi Y. Role of splanchnic nerves in endocrine and metabolic response to abdominal surgery. Br J Surg. 1986;73:142–145. doi: 10.1002/bjs.1800730224. [DOI] [PubMed] [Google Scholar]
- 21.Tsuji H, Asoh Y, Takeuchi Y, Shirasaka C. Attenuation of adrenocortical response to upper abdominal surgery with epidural blockade. Br J Surg. 1983;70:122–124. doi: 10.1002/bjs.1800700223. [DOI] [PubMed] [Google Scholar]
- 22.Tsuji H, Shirasaka C, Asoh T, Takeuchi Y. Influences of splanchnic nerve blockade on endocrine-metabolic responses to upper abdominal surgery. Br J Surg. 1983;70:437–439. doi: 10.1002/bjs.1800700716. [DOI] [PubMed] [Google Scholar]
- 23.Uchida I, Asoh T, Shirasaka C, Tsuji H. Effect of epidural analgesia on postoperative insulin resistance as evaluated by insulin clamp technique. Br J Surg. 1988;75:557–562. doi: 10.1002/bjs.1800750618. [DOI] [PubMed] [Google Scholar]
- 24.Planes A, Vochelle N, Fagola M, Feret J, Bellaud M. Prevention of deep vein thrombosis after total hip replacement: the effect of low molecular weight heparin with spinal and general anaesthesia. J Bone Joint Surg Br. 1991;73B:418–422. doi: 10.1302/0301-620X.73B3.1670442. [DOI] [PubMed] [Google Scholar]
- 25.Abboud TK, Nagappala S, Murakawa K, David S, Haroutunian S, Zakarian M, et al. Comparison of the effects of general and regional anesthesia for cesarean section on neonatal nuerologic and adaptive capacity scores. Anesth Analg. 1985;64:996–1000. [PubMed] [Google Scholar]
- 26.Asbjorn J, Jakobsen B, Pilegaard H, Blom L, Ostergaard A, Brandt M. Mental function in elderly men after surgery during epidural analgesia. Acta Anaesthesiol Scand. 1989;33:369–373. doi: 10.1111/j.1399-6576.1989.tb02925.x. [DOI] [PubMed] [Google Scholar]
- 27.Asoh T, Tsuji H, Shirasaka C, Takeuchi Y. Effect of epidural analgesia on metabolic response to major upper abdominal surgery. Acta Anaesthesiol Scand. 1983;27:233–237. doi: 10.1111/j.1399-6576.1983.tb01942.x. [DOI] [PubMed] [Google Scholar]
- 28.Baron J, Bertrand M, Barre E, Godet G, Mundler O, Coriat P, et al. Combined epidural and general anesthesia versus general anesthesia for abdominal aortic surgery. Anesthesiology. 1991;75:611–618. doi: 10.1097/00000542-199110000-00010. [DOI] [PubMed] [Google Scholar]
- 29.Berggren D, Gustafson Y, Eriksson B, Bucht G, Hansson LI, Reiz S, et al. Postoperative confusion after anesthesia in elderly patients with femoral neck fractures. Anesth Analg. 1987;66:497–504. [PubMed] [Google Scholar]
- 30.Bigler D, Adelhoj B, Petring O, Pederson N, Busch P, Kalhke P. Mental function and morbidity after acute hip surgery during spinal and general anaesthesia. Anaesthesia. 1985;40:672–676. doi: 10.1111/j.1365-2044.1985.tb10949.x. [DOI] [PubMed] [Google Scholar]
- 31.Blunnie W, McIlroy A, Merrett J, Dundee J. Cardiovascular and biochemical evidence of stress during major surgery associated with different techniques of anaesthesia. Br J Anaesth. 1983;55:611–617. doi: 10.1093/bja/55.7.611. [DOI] [PubMed] [Google Scholar]
- 32.Bode R, Lewis K, Zarich S, Pierce E, Roberts M, Kowalchuk G, et al. Cardiac outcome after peripheral vascular surgery: comparison of general and regional anesthesia. Anesthesiology. 1996;84:3–13. doi: 10.1097/00000542-199601000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Bonnet F, Harari A, Thibonnier M, Viars P. Suppression of antidiuretic hormone hypersecretion during surgery by extradural anaesthesia. Br J Anaesth. 1982;54:29–35. doi: 10.1093/bja/54.1.29. [DOI] [PubMed] [Google Scholar]
- 34.Bonnet F, Touboul C, Picard A, Vodinh J, Becquemin J. Neuroleptanesthesia versus thoracic epidural anesthesia for abdominal aortic surgery. Ann Vasc Surg. 1989;3:214–219. doi: 10.1016/S0890-5096(07)60026-0. [DOI] [PubMed] [Google Scholar]
- 35.Borovskikh N, Lebedev L, Strashkov V, Vinogradov A. Comparative evaluation of the effectiveness of epidural anesthesia with spontaneous respiration and general anesthesia in aorto-femoral bifurcation shunt. Vestn Khir Im I I Grek. 1990;145:95–98. [PubMed] [Google Scholar]
- 36.Bottiglieri T, Petros A, Smith D, Ronzoni G, Carli F. The effect of extradural bupivacaine on CSF monoamine metabolites in surgical patients. Reg Anesth. 1992;17(Suppl):95. [Google Scholar]
- 37.Brandt M, Fernandes A, Mordhorst R, Kehlet H. Epidural analgesia improves postoperative nitrogen balance. BMJ. 1978;i:1106–1108. doi: 10.1136/bmj.1.6120.1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bredahl C, Hindsolm KB, Frandsen PC. Changes in body heat during hip fracture surgery: a comparison of spinal analgesia and general anaesthesia. Acta Anaesthesiol Scand. 1991;35:548–552. doi: 10.1111/j.1399-6576.1991.tb03346.x. [DOI] [PubMed] [Google Scholar]
- 39.Brichon P, Pison C, Chaffanjon P, Fayot P, Buchberger M, Neron L, et al. Comparison of epidural analgesia and cryoanalgesia in thoracic surgery. Eur J Cardiothorac Surg. 1994;8:482–486. doi: 10.1016/1010-7940(94)90019-1. [DOI] [PubMed] [Google Scholar]
- 40.Bromage P, Shibata H, Willoughby R. Influence of prolonged epidural blockade on blood sugar and cortisol responses to operations upon the upper part of the abdomen and the thorax. Surg Gynecol Obstet. 1971;132:1051–1056. [PubMed] [Google Scholar]
- 41.Brown A, Visram A, Jones R, Irwins M, Bacon-Shone J. Preoperative and postoperative oxygen saturation in the elderly following spinal or general anaesthesia — an audit of current practice. Anaesth Intensive Care. 1994;22:150–154. doi: 10.1177/0310057X9402200205. [DOI] [PubMed] [Google Scholar]
- 42.Buckley F, Kehlet H, Brown N, Scott D. Postoperative glucose tolerance during extradural analgesia. Br J Anaesth. 1982;54:325–331. doi: 10.1093/bja/54.3.325. [DOI] [PubMed] [Google Scholar]
- 43.Chin S, Abou Madi M, Eurin B, Witvoet J, Montagne J. Blood loss in total hip replacement: extradural v. phenoperidine analgesia. Br J Anaesth. 1982;54:491–495. doi: 10.1093/bja/54.5.491. [DOI] [PubMed] [Google Scholar]
- 44.Christensen P, Brandt M, Rem J, Kehlet H. Influence of extradural morphine on the adrenocortical and hyperglycaemic response to surgery. Br J Anaesth. 1982;54:23–26. doi: 10.1093/bja/54.1.23. [DOI] [PubMed] [Google Scholar]
- 45.Christensen T, Waaben J, Lindeburg T, Vesterberg K, Vinnars E, Kehlet H. Effect of epidural analgesia on muscle amino acid pattern after surgery. Acta Chir Scand. 1986;152:407–411. [PubMed] [Google Scholar]
- 46.Christopherson R, Beattie C, Frank S, Norris E, Meinert C, Gottlieb S, et al. Perioperative morbidity in patients randomized to epidural or general anesthesia for lower extremity vascular surgery. Anesthesiology. 1993;79:422–434. doi: 10.1097/00000542-199309000-00004. [DOI] [PubMed] [Google Scholar]
- 47.Breslow M, Parker S, Frank S, Norris E, Yates H, Raff H, et al. Determinants of catecholamine and cortisol responses to lower extremity revascularization. Anesthesiology. 1993;79:1202–1209. doi: 10.1097/00000542-199312000-00010. [DOI] [PubMed] [Google Scholar]
- 48.Frank S, Beattie C, Christopherson R, Norris E, Rock P, Parker S, et al. Epidural versus general anesthesia, ambient operating room temperature, and patient age as predictors of inadvertent hypothermia. Anesthesiology. 1992;77:252–257. doi: 10.1097/00000542-199208000-00005. [DOI] [PubMed] [Google Scholar]
- 49.Rosenfeld B, Beattie C, Christopherson R, Norris E, Frank S, Breslow M, et al. The effects of different anesthetic regimes on fibrinolysis and the development of postoperative arterial thrombosis. Anesthesiology. 1993;79:435–443. doi: 10.1097/00000542-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 50.Chung F, Meier R, Lautenschlager E, Carmichael F, Chung A. General or spinal anesthesia: which is better in the elderly? Anesthesiology. 1987;67:422–427. doi: 10.1097/00000542-198709000-00026. [DOI] [PubMed] [Google Scholar]
- 51.Chung F, Chung A, Meier R, Lautenshlaeger E, Seyone C. Comparison of perioperative mental function after general anaesthesia and spinal anaesthesia with intravenous sedation. Can J Anaesth. 1989;36:382–387. doi: 10.1007/BF03005334. [DOI] [PubMed] [Google Scholar]
- 52.Cook P, Davies M, Cronin K, Moran P. A prospective randomised trial comparing spinal anaesthesia using hyperbaric cinchocaine with general anaesthesia for lower limb vascular surgery. Anaesth Intensive Care. 1986;14:373–380. doi: 10.1177/0310057X8601400409. [DOI] [PubMed] [Google Scholar]
- 53.Couderc E, Mauge F, Duvaldestin P, Desmonts J. Resultats comparatifs de l'anesthesie generale et peridurale chez le grand vieillard dans la chirurgie de la hanche. Anesth Anal Reanim. 1977;34:987–998. [PubMed] [Google Scholar]
- 54.Cuschieri R, Morran C, Howie J, McArdle C. Postoperative pain and pulmonary complications: comparison of three analgesic regimens. Br J Surg. 1985;72:495–498. doi: 10.1002/bjs.1800720631. [DOI] [PubMed] [Google Scholar]
- 55.Dahl J, Schultz P, Anker-Moller E, Christensen E, Staunstrup H, Carlsson P. Spinal anaesthesia in young patients using a 29-gauge needle: technical considerations and an evaluation of postoperative complaints compared with general anaesthesia. Br J Anaesth. 1990;64:178–182. doi: 10.1093/bja/64.2.178. [DOI] [PubMed] [Google Scholar]
- 56.Damask MC, Weissman C, Todd G. General versus epidural anesthesia for femoral-popliteal bypass surgery. J Clin Anesth. 1990;2:71–75. doi: 10.1016/0952-8180(90)90056-9. [DOI] [PubMed] [Google Scholar]
- 57.Darling J, Murray J, Hainsworth A, Trinick T. The effect of isoflurane or spinal anesthesia on indocyanine green disappearance rate in the elderly. Anesth Analg. 1994;78:706–709. doi: 10.1213/00000539-199404000-00016. [DOI] [PubMed] [Google Scholar]
- 58.Davies M, Silbert B, Mooney P, Dysart R, Meads A. Combined epidural and general anaesthesia versus general anaesthesia for abdominal aortic surgery: a prospective randomised trial. Anaesth Intensive Care. 1993;21:790–794. doi: 10.1177/0310057X9302100607. [DOI] [PubMed] [Google Scholar]
- 59.Davis F, Laurenson V. Spinal anaesthesia or general anaesthesia for emergency hip surgery in elderly patients. Anaesth Intensive Care. 1981;9:352–358. doi: 10.1177/0310057X8100900406. [DOI] [PubMed] [Google Scholar]
- 60.Davis F, Quince M, Laurenson V. Deep vein thrombosis and anaesthetic technique in emergency hip surgery. BMJ. 1980;281:1528–1529. doi: 10.1136/bmj.281.6254.1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Davis F, Woolner D, Frampton C, Wilkinson A, Grant A, Harrison R, et al. Prospective, multi-centre trial of mortality following general or spinal anaesthesia for hip fracture surgery in the elderly. Br J Anaesth. 1987;59:1080–1088. doi: 10.1093/bja/59.9.1080. [DOI] [PubMed] [Google Scholar]
- 62.Davis F, Laurenson V, Gillespie W, Wells J, Foate J, Newman E. Deep vein thrombosis after total hip replacement: a comparison between spinal and epidural anaesthesia. J Bone Joint Surg Br. 1989;71B:181–185. doi: 10.1302/0301-620X.71B2.2925731. [DOI] [PubMed] [Google Scholar]
- 63.Davis F, McDermott E, Hickton C, Wells E, Heaton D, Laurenson V, et al. Influence of spinal and general anaesthesia on haemostasis during total hip arthroplasty. Br J Anaesth. 1987;59:561–571. doi: 10.1093/bja/59.5.561. [DOI] [PubMed] [Google Scholar]
- 64.Davis F, Laurenson V, Lewis J, Wells J, Gillespie W. Metabolic response to total hip arthroplasty under hypobaric subarachnoid or general anaesthesia. Br J Anaesth. 1987;59:725–729. doi: 10.1093/bja/59.6.725. [DOI] [PubMed] [Google Scholar]
- 65.Davis F, Larenson V, Gillespie W, Foate J, Seagar A. Leg blood flow during total hip replacement under spinal or general anaesthesia. Anaesth Intensive Care. 1989;17:136–143. doi: 10.1177/0310057X8901700203. [DOI] [PubMed] [Google Scholar]
- 66.De Kock M, Crochet B, Morimont C, Scholtes J. Intravenous or epidural clonidine for intra- and postoperative analgesia. Anesthesiology. 1993;79:525–531. doi: 10.1097/00000542-199309000-00016. [DOI] [PubMed] [Google Scholar]
- 67.Dick W, Traub E, Kraus H, Tollner U, Burghard R, Muck J. General anaesthesia versus epidural anaesthesia for primary caesarean section — a comparative study. Eur J Anaesthesiol. 1992;9:15–21. [PubMed] [Google Scholar]
- 68.Dobson P, Caldicott L, Gerrish S, Cole J, Channer K. Changes in haemodynamic variables during transurethral resection of the prostate: comparison of general and spinal anaesthesia. Br J Anaesth. 1994;72:267–271. doi: 10.1093/bja/72.3.267. [DOI] [PubMed] [Google Scholar]
- 69.Donadoni R, Baele G, Rolly G, Devulder M. Influence of epidural anesthesia on coagulation factors in patients undergoing total hip replacement. Reg Anesth. 1988;13:55. doi: 10.1111/j.1399-6576.1989.tb02972.x. [DOI] [PubMed] [Google Scholar]
- 70.Edwards N, Callaghan L, White T, Reilly C. Perioperative myocardial ischaemia in patients undergoing transurethral surgery: a pilot study comparing general with spinal anaesthesia. Br J Anaesth. 1995;74:368–372. doi: 10.1093/bja/74.4.368. [DOI] [PubMed] [Google Scholar]
- 71.Foate J, Horton H, Davis F. Lower limb blood flow during transurethral resection of the prostate under spinal or general anaesthesia. Anaesth Intensive Care. 1985;13:383–386. doi: 10.1177/0310057X8501300409. [DOI] [PubMed] [Google Scholar]
- 72.Frank S, Shir Y, Raja S, Fleisher L, Beattie C. Core hypothermia and skin surface temperature gradients. Anesthesiology. 1994;80:502–507. doi: 10.1097/00000542-199403000-00005. [DOI] [PubMed] [Google Scholar]
- 73.Fleisher L, Frank S, Shir Y, Estafanous M, Kelly S, Raja S. Cardiac sympathovagal balance and peripheral sympathetic vasoconstriction: epidural versus general anesthesia. Anesth Analg. 1994;79:165–171. doi: 10.1213/00000539-199407000-00031. [DOI] [PubMed] [Google Scholar]
- 74.Fredin H, Rosberg B. Anaesthetic techniques and thromboembolism in total hip arthroplasty. Eur J Anaesthesiol. 1986;3:273–281. [PubMed] [Google Scholar]
- 75.Garnett R, MacIntyre A, Lindsay P, Barber G, Cole C, Hajjar G, et al. Perioperative ischaemia in aortic surgery: combined epidural/general anaesthesia and epidural analgesia vs general anaesthesia and iv analgesia. Can J Anaesth. 1996;43:769–777. doi: 10.1007/BF03013027. [DOI] [PubMed] [Google Scholar]
- 76.Gelman S, Laws H, Potzick J, Strong S, Smith L, Erdemir H. Thoracic epidural vs balanced anesthesia in morbid obesity: an intraoperative and postoperative hemodynamic study. Anesth Analg. 1980;59:902–908. [PubMed] [Google Scholar]
- 77.Ghoneim M, Hinrichs JV, O'Hara MW, Mehta MP, Pathak D, Kumar V, et al. Comparison of psychologic and cognitive functions after general or regional anesthesia. Anesthesiology. 1988;69:507–515. doi: 10.1097/00000542-198810000-00010. [DOI] [PubMed] [Google Scholar]
- 78.Godfrey P, Greenan J, Ranasinghe D, Shabestary S, Pollock A. Ventilatory capacity after three methods of anaesthesia for inguinal hernia repair: a randomized controlled trial. Br J Surg. 1981;68:587–589. doi: 10.1002/bjs.1800680820. [DOI] [PubMed] [Google Scholar]
- 79.Goertz A, Seeling W, Heinrich H, Lindner K, Schirmer U. Influence of high thoracic epidural anesthesia on left ventricular contractility assessed using the end-systolic pressure-length relationship. Acta Anaesthesiol Scand. 1993;37:38–44. doi: 10.1111/j.1399-6576.1993.tb03595.x. [DOI] [PubMed] [Google Scholar]
- 80.Gold M, DeCrosta D, Rizzuto C, Ben-Harari R, Ramanathan S. The effect of lumbar epidural and general anesthesia on plasma catecholamines and hemodynamics during abdominal aortic aneurysm repair. Anesth Analg. 1994;78:225–230. doi: 10.1213/00000539-199402000-00006. [DOI] [PubMed] [Google Scholar]
- 81.Gottlieb A, McCoy C, Augereau P, Beven E. Hemodynamics of aortic clamping: a comparison between general and lumbar epidural anesthesia. Reg Anesth. 1988;13:69. [Google Scholar]
- 82.Halevy S, Liu-Barnett M, Ross P, Roginsky M. Serum thyroid hormones changes in patients undergoing caesarean section under general or regional anaesthesia. Br J Anaesth. 1978;50:1053–1057. doi: 10.1093/bja/50.10.1053. [DOI] [PubMed] [Google Scholar]
- 83.Haljamae H, Frid I, Holm J, Akerstrom G. Epidural vs general anaesthesia and leg blood flow in patients with occlusive atherosclerotic disease. Eur J Vasc Surg. 1988;2:395–400. doi: 10.1016/s0950-821x(88)80018-5. [DOI] [PubMed] [Google Scholar]
- 84.Hasenbos M, van Egmond J, Gielen M, Crul J. Post-operative analgesia by epidural versus intramuscular nicomorphine after thoracotomy. Part 1. Acta Anaesthesiol Scand. 1985;29:572–576. doi: 10.1111/j.1399-6576.1985.tb02256.x. [DOI] [PubMed] [Google Scholar]
- 85.Hasenbos M, van Egmond J, Gielen M, Crul J. Post-operative analgesia by epidural versus intramuscular nicomorphine after thoracotomy. Part 2. Acta Anaesthesiol Scand. 1985;29:577–582. doi: 10.1111/j.1399-6576.1985.tb02257.x. [DOI] [PubMed] [Google Scholar]
- 86.Hedenstierna G, Lofstrom J. Effect of anaesthesia on respiratory function after major lower extremity surgery. Acta Anaesthesiol Scand. 1985;29:55–60. doi: 10.1111/j.1399-6576.1985.tb02159.x. [DOI] [PubMed] [Google Scholar]
- 87.Hendolin H, Mattila M, Poikolainen E. The effect of lumbar epidural analgesia on the development of deep vein thrombosis of the legs after open prostatectomy. Acta Chir Scand. 1981;147:425–429. [PubMed] [Google Scholar]
- 88.Hendolin H, Lansimies E. Skin and central temperatures during continuous epidural analgesia and general anaesthesia in patients subjected to open prostatectomy. Ann Clin Research. 1982;14:181–186. [PubMed] [Google Scholar]
- 89.Hendolin H, Alhava E. Effect of epidural versus general anaesthesia on peroperative blood loss during retropubic prostatectomy. Int Urol Nephrol. 1982;14:399–405. doi: 10.1007/BF02081981. [DOI] [PubMed] [Google Scholar]
- 90.Hendolin H, Lahtinen J, Lansimies E, Tuppurainen T. The effect of thoracic epidural analgesia on postoperative stress and morbidity. Ann Chir Gynaecol. 1987;76:234–240. [PubMed] [Google Scholar]
- 91.Hendolin H, Tuppurainen T, Lahtinen J. Thoracic epidural analgesia and deep vein thrombosis in cholecystectomized patients. Acta Chir Scand. 1982;48:405–409. [PubMed] [Google Scholar]
- 92.Hendolin H, Lahtinen J, Lansimies E, Tuppurainen T, Partanen K. The effect of thoracic epidural analgesia on respiratory function after cholecystectomy. Acta Anaesthesiol Scand. 1987;31:645–651. doi: 10.1111/j.1399-6576.1987.tb02637.x. [DOI] [PubMed] [Google Scholar]
- 93.Henny C, Oddoom J, Ten Cate H, Ten Cate J, Oosterhoff R, Dabhoiwala N, et al. Effects of extradural bupivacaine on the haemostatic system. Br J Anaesth. 1986;58:301–305. doi: 10.1093/bja/58.3.301. [DOI] [PubMed] [Google Scholar]
- 94.Hjortso N, Neumann P, Frosig F, Anderson T, Lindhard A, Rogon E, et al. A controlled study on the effect of epidural analgesia with local anaesthetics and morphine on morbidity after abdominal surgery. Acta Anaesthesiol Scand. 1985;29:790–796. doi: 10.1111/j.1399-6576.1985.tb02302.x. [DOI] [PubMed] [Google Scholar]
- 95.Hjortso N, Andersen T, Frosig F, Neumann P, Rogon E, Kehlet H. Failure of epidural analgesia to modify postoperative depression of delayed hypersensitivity. Acta Anaesthesiol Scand. 1984;28:128–131. doi: 10.1111/j.1399-6576.1984.tb02027.x. [DOI] [PubMed] [Google Scholar]
- 96.Hjortso N, Christensen N, Andersen T, Kehlet H. Effects of the extradural administration of local anaesthetic agents and morphine on the urinary excretion of cortisol, catecholamines and nitrogen following abdomial surgery. Br J Anaesth. 1985;57:400–406. doi: 10.1093/bja/57.4.400. [DOI] [PubMed] [Google Scholar]
- 97.Holdcroft A, Hall G, Cooper G. Redistribution of body heat during anaesthesia. Anaesthesia. 1979;34:758–764. doi: 10.1111/j.1365-2044.1979.tb06408.x. [DOI] [PubMed] [Google Scholar]
- 98.Hole A, Terjesen T, Breivik H. Epidural versus general anaesthesia for total hip arthroplasty in elderly patients. Acta Anaesthesiol Scand. 1980;24:279–287. doi: 10.1111/j.1399-6576.1980.tb01549.x. [DOI] [PubMed] [Google Scholar]
- 99.Hole A, Unsgaard G. The effect of epidural and general anaesthesia on lymphocyte functions during and after major orthopaedic surgery. Acta Anaesthesiol Scand. 1983;27:135–141. doi: 10.1111/j.1399-6576.1983.tb01923.x. [DOI] [PubMed] [Google Scholar]
- 100.Hole A, Unsgaard G, Breivik H. Monocyte functions are depressed during and after surgery under general anaesthesia but not under epidural anaesthesia. Acta Anaesthesiol Scand. 1982;26:301–307. doi: 10.1111/j.1399-6576.1982.tb01771.x. [DOI] [PubMed] [Google Scholar]
- 101.Hole A. Per- and postoperative monocyte and lymphocyte functions: effects of sera from patients operated under general or epidural anaesthesia. Acta Anaesthesiol Scand. 1984;84:287–291. doi: 10.1111/j.1399-6576.1984.tb02062.x. [DOI] [PubMed] [Google Scholar]
- 102.Hole A, Bakke O. T-lymphocytes and the subpopulations of T-helper and T-suppressor cells measured by monoclonal antibodies (T11,T4 and T8) in relation to surgery under epidural and general anaesthesia. Acta Anaesthesiol Scand. 1984;28:296–300. doi: 10.1111/j.1399-6576.1984.tb02064.x. [DOI] [PubMed] [Google Scholar]
- 103.Homann B, Blumenberg D, Lerner H. The influence of anaesthesia on plasma levels of factor XIII. Anaesthesist. 1984;33:145–148. [PubMed] [Google Scholar]
- 104.Houweling P, Ionescu T, Leguit P, Van Der Tweel I, Smalhout B. Comparison of the cardiovascular effects of intravenous, epidural and intrathecal sufentanil analgesia as a supplement to general anaesthesia for abdominal aortic aneurysm surgery. Eur J Anesthesiol. 1993;10:403–411. [PubMed] [Google Scholar]
- 105.Jakobsen BW, Pederson J, Egeberg BB. Postoperative lymphocytopenia and leucocytosis after epidural and general anaesthesia. Acta Anaesthesiol Scand. 1986;30:668–671. doi: 10.1111/j.1399-6576.1986.tb02498.x. [DOI] [PubMed] [Google Scholar]
- 106.Jayr C, Mollie A, Bourgain J, Truffa Bachi J, Treich G. Postoperative pulmonary complications after abdominal surgery: epidural compared with parenteral morphine analgesia. Reg Anesth. 1988;13:6. [PubMed] [Google Scholar]
- 107.Jayr C, Mollie A, Bourgain J, Alarcon J, Masselot J, Lasser P, et al. Postoperative pulmonary complications: general anesthesia with postoperative parenteral morphine compared with epidural analgesia. Surgery. 1988;104:57–63. [PubMed] [Google Scholar]
- 108.Jayr C, Thomas H, Rey A, Farhat F, Lasser P, Bourgain J. Postoperative pulmonary complications: epidural analgesia using bupivacaine and opioids versus parenteral opioids. Anesthesiology. 1993;78:666–676. doi: 10.1097/00000542-199304000-00009. [DOI] [PubMed] [Google Scholar]
- 109.Jenkins J, Fox J, Sharwood Smith G. Changes in body heat during transvesical prostatectomy. Anaesthesia. 1983;38:748–753. doi: 10.1111/j.1365-2044.1983.tb12197.x. [DOI] [PubMed] [Google Scholar]
- 110.Jensen B, Berthelsen P, Brochner-Mortensen J. Glomerular filtration rate during halothane anaesthesia and epidural analgesia in combination with halothane anaesthesia. Acta Anaesthesiol Scand. 1977;21:395–399. doi: 10.1111/j.1399-6576.1977.tb01238.x. [DOI] [PubMed] [Google Scholar]
- 111.Jensen CH, Berthelsen P, Kuhl C, Kehlet H. Effect of epidural analgesia on glucose tolerance during surgery. Acta Anaesthesiol Scand. 1980;24:472–474. doi: 10.1111/j.1399-6576.1980.tb01586.x. [DOI] [PubMed] [Google Scholar]
- 112.Jia N, Luo L, Zhao J, Yan W, Liu B, Zhang Y, et al. Influence of epidural and general anesthesia on human plasma cAMP. Chin Med J. 1985;65:30–33. [PubMed] [Google Scholar]
- 113.Jordanov K, Smilov I, Ninio A, Mincheva-Saeva M. A comparative study on epidural and general anaesthesia in elective caesarian section. Akush Ginekol (Sofiia) 1985;24:31–40. [PubMed] [Google Scholar]
- 114.Jorgensen L, Rasmussen L, Nielsen P, Leffers A, Albrecht Beste E. Antithrombotic efficacy of continuous extradural analgesia after knee replacement. Br J Anaesth. 1991;66:8–12. doi: 10.1093/bja/66.1.8. [DOI] [PubMed] [Google Scholar]
- 115.Kausalya R, Jacob R. Efficacy of low-dose epidural anaesthesia in surgery of the anal canal — a randomised controlled trial. Anaesth Intensive Care. 1994;22:161–164. doi: 10.1177/0310057X9402200207. [DOI] [PubMed] [Google Scholar]
- 116.Keith I. Anaesthesia and blood loss in total hip replacement. Anaesthesia. 1977;32:444–450. doi: 10.1111/j.1365-2044.1977.tb09981.x. [DOI] [PubMed] [Google Scholar]
- 117.Kokhnover S, Manevich L, Molchanova G. Comparative study of prolonged peridural anesthesia and combined general anesthesia in operative gynecology. Akush Ginekol (Sofiia) 1982;6:48–52. [PubMed] [Google Scholar]
- 118.Kossman B, Volk E, Spilker E, Maier V, Fehm H. Influence of thoracic epidural analgesia on glucose, cortisol, insulin and glucagon responses to surgery. Reg Anesth. 1982;7:107–109. [Google Scholar]
- 119.Lehtinen AM, Laatikainen T, Koskimies AI, Hovorka J. Modifying effects of epidural analgesia or general anesthesia on the stress hormone response to laparoscopy for in vitro fertilization. J In Vitro Fert Embryo Transf. 1987;4:23–29. doi: 10.1007/BF01555431. [DOI] [PubMed] [Google Scholar]
- 120.Licker M, Suter P, Krauer F, Rifat N. Metabolic response to lower abdominal surgery: analgesia by epidural blockade compared with intravenous opiate infusion. Eur J Anaesthesiol. 1994;11:193–199. [PubMed] [Google Scholar]
- 121.Mann R, Bisset W. Anaesthesia for lower limb amputation: a comparison of spinal analgesia and general analgesia in the elderly. Anaesthesia. 1983;38:1185–1191. doi: 10.1111/j.1365-2044.1983.tb12523.x. [DOI] [PubMed] [Google Scholar]
- 122.Maurette P, Castagnera L, Vivier C, Erny P. Psychological assessment in the elderly after general and spinal anaesthesia. Ann Fr Anesth Reanim. 1988;7:305–308. doi: 10.1016/s0750-7658(88)80033-9. [DOI] [PubMed] [Google Scholar]
- 123.McGowan S, Smith G. Anaesthesia for transurethral prostatectomy: a comparison of spinal intradural analgesia with two methods of general anaesthesia. Anaesthesia. 1980;35:847–853. doi: 10.1111/j.1365-2044.1980.tb03941.x. [DOI] [PubMed] [Google Scholar]
- 124.McKenzie P, Wishart H, Smith G. Long-term outcome after repair of fractured neck of femur. Comparison of subarachnoid and general anaesthesia. Br J Anaesth. 1984;56:581–584. doi: 10.1093/bja/56.6.581. [DOI] [PubMed] [Google Scholar]
- 125.McKenzie P, Wishart H, Dewar K, Gray I, Smith G. Comparison of the effects of spinal anaesthesia and general anaesthesia on postoperative oxygenation and perioperative mortality. Br J Anaesth. 1980;52:49–54. doi: 10.1093/bja/52.1.49. [DOI] [PubMed] [Google Scholar]
- 126.McKenzie P, Wishart H, Gray I, Smith G. Effects of anaesthetic technique on deep vein thrombosis: a comparison of subarachnoid and general anaesthesia. Br J Anaesth. 1985;57:853–857. doi: 10.1093/bja/57.9.853. [DOI] [PubMed] [Google Scholar]
- 127.McLaren A. Mortality studies. A review. Reg Anesth. 1982;7:S172–S174. [Google Scholar]
- 128.McLaren A, Stockwell M, Reid V. Anaesthetic techniques for surgical correction of fractured neck of femur: a comparative study of spinal and general anaesthesia in the elderly. Anaesthesia. 1978;33:10–14. doi: 10.1111/j.1365-2044.1978.tb08270.x. [DOI] [PubMed] [Google Scholar]
- 129.Mellbring G, Dahlgren S, Reiz S, Sunnnegardh O. Thromboembolic complications after major abdominal surgery: effect of thoracic epidural analgesia. Acta Chir Scand. 1983;149:263–268. [PubMed] [Google Scholar]
- 130.Melsen N, Thorshauge H. Patients experience of epidural anaesthesia and general anaesthesia. Ugeskr Laeger. 1987;149:150–152. [PubMed] [Google Scholar]
- 131.Merhav H, Rothstein H, Eliraz A, Hana R, Pfeffermann R. A comparison of pulmonary function and oxygenation following local, spinal or general anaesthesia in patients undergoing inguinal hernia repair. Int Surg. 1993;78:257–261. [PubMed] [Google Scholar]
- 132.Modig J, Malmberg P, Saldeen T. Comparative effects of epidural and general anesthesia on fibrinolysis function, lower limb rheology and thromboembolism after total hip replacement. Anesthesiology. 1980;53:S34. [Google Scholar]
- 133.Modig J, Maripuu E, Sahlstedt B. Thromboembolism following total hip replacement: a prospective investigation of 94 patients with emphasis on the efficacy of lumbar epidural anaesthesia in prophylaxis. Reg Anesth. 1986;11:72–79. [Google Scholar]
- 134.Modig J, Karlstrom G. Intra- and post-operative blood loss and haemodynamics in total hip replacement when performed under lumbar epidural versus general anaesthesia. Eur J Anaesthesiol. 1987;4:345–355. [PubMed] [Google Scholar]
- 135.Modig J. Beneficial effects on intraoperative and postoperative blood loss in total hip replacement when performed under lumbar epidural anesthesia. Acta Chir Scand Suppl. 1988;550:95–103. [PubMed] [Google Scholar]
- 136.Moiniche S, Hjortso N, Blemmer T, Dahl J, Kehlet H. BP and heart rate during postoperative orthostatic stress and continuous epidural analgesia. Reg Anesth. 1992;17(Suppl):2. [Google Scholar]
- 137.Murakami M. Effect of anaesthesia on endocrine metabolic response to lower abdominal surgery. Masui. 1987;36:583–591. [PubMed] [Google Scholar]
- 138.Naesh O, Hindberg I, Friis J, Christiansen C. General versus regional anaesthesia and platelet aggregation in minor surgery. Eur J Anaesthesiol. 1994;11:169–173. [PubMed] [Google Scholar]
- 139.Naesh O, Hindberg I, Friis J, Christiansen C, Pedersen T, Trap-Jensen J, et al. Platelet activation in major surgical stress: influence of combined epidural and general anaesthesia. Acta Anaesthesiol Scand. 1994;38:820–825. doi: 10.1111/j.1399-6576.1994.tb04012.x. [DOI] [PubMed] [Google Scholar]
- 140.Nielsen KK, Andersen K, Asbjorn J, Vork F, Ohrt Nissen A. Blood loss in transurethral prostatectomy: epidural versus general anaesthesia. Int Urol Nephrol. 1987;19:287–292. doi: 10.1007/BF02549865. [DOI] [PubMed] [Google Scholar]
- 141.Nielsen T, Nielsen H, Husted S, Hansen S, Olsen K, Fjeldborg N. Stress response and platelet function in minor surgery during epidural bupivacaine and general anaesthesia: effect of epidural morphine addition. Eur J Anaesthesiol. 1989;6:409–417. [PubMed] [Google Scholar]
- 142.Nielson WR, Gelb AW, Casey JE, Penny FJ, Merchant RN, Manninen PH. Long-term cognitive and social sequelae of general versus regional anesthesia during arthroplasty in the elderly. Anesthesiology. 1990;73:1103–1109. doi: 10.1097/00000542-199012000-00006. [DOI] [PubMed] [Google Scholar]
- 143.Ogata M, Takara H, Tanaka T, Nakamura S, Shigematsu A. The effect of anesthesia on plasma renin and aldosterone: comparison between nitrous oxide-halothane and nitrous oxide epidural anesthesia. Masui. 1985;34:1358–1363. [PubMed] [Google Scholar]
- 144.Ogata M, Yanagida K, Takenaka I, Shimozawa K, Shigematsu A. The effect of anesthesia and partial hepatectomy on plasma renin and aldosterone: comparison between nitrous oxide-enflurane anesthesia and nitrous oxide epidural anesthesia. Masui. 1988;37:163–168. [PubMed] [Google Scholar]
- 145.Pedersen J, Jakobsen B, Egeberg B. Comparison between epidural analgesia and general anaesthesia. Ugeskr Laeger. 1986;148:1819–1822. [PubMed] [Google Scholar]
- 146.Pedersen J, Jakobsen B, Egeberg B. Thromboembolic complications after hip replacement. Ugeskr Laeger. 1987;149:1463–1466. [PubMed] [Google Scholar]
- 147.Poikolainen E, Hendolin H. Effects of lumbar epidural analgesia and general anaesthesia on flow velocity in the femoral vein and postoperative deep vein thrombosis. Acta Chir Scand. 1983;149:361–364. [PubMed] [Google Scholar]
- 148.Poll J, van Kleef J, Moolenaar A. The influence of epidural anaesthesia on the cortisol response to surgery. A comparison between minor and major surgery in orthopaedic patients. Reg Anesth. 1988;13:4. [Google Scholar]
- 149.Racle J, Benkhadra A, Poy J, Gleizal B, Gaudray A. Comparative study of general and spinal anesthesia in the elderly female patient undergoing hip surgery. Ann Fr Anesth Reanim. 1986;5:24–30. doi: 10.1016/s0750-7658(86)80118-6. [DOI] [PubMed] [Google Scholar]
- 150.Ravin M. Comparison of spinal and general anaesthesia for lower abdominal surgery in patients with chronic obstructive pulmonary disease. Anesthesiology. 1971;35:319–322. doi: 10.1097/00000542-197109000-00018. [DOI] [PubMed] [Google Scholar]
- 151.Reinhart K, Foehring U, Kersting T, Schaefer M, Bredle D, Hirner A, et al. Effects of thoracic epidural anesthesia on systemic hemodynamic function and systemic oxygen supply-demand relationship. Anesth Analg. 1989;69:360–369. [PubMed] [Google Scholar]
- 152.Rem J, Brandt M, Kehlet H. Prevention of postoperative lymphopenia and granulocytosis by epidural analgesia. Lancet. 1980;i:283–284. doi: 10.1016/s0140-6736(80)90780-1. [DOI] [PubMed] [Google Scholar]
- 153.Rickford JK, Speedy HM, Tytler JA, Lim M. Comparative evaluation of general, epidural and spinal anaesthesia for extracorporeal shockwave lithotripsy. Ann R Coll Surg Engl. 1988;70:68–73. [PMC free article] [PubMed] [Google Scholar]
- 154.Riis J, Lomholt B, Haxholdt O, Kehlet H, Valentin N, Danielsen U, et al. Immediate and long-term mental recovery from general versus epidural anesthesia in elderly patients. Acta Anaesthesiol Scand. 1983;27:44–49. doi: 10.1111/j.1399-6576.1983.tb01903.x. [DOI] [PubMed] [Google Scholar]
- 155.Rosseel P, Marichal P, Lauwers L, Baute L, Hanegreefs G. A hemodynamic study of epidural versus intravenous anesthesia for aortofemoral bypass surgery. Acta Anesthesiol Belg. 1985;36:345–363. [PubMed] [Google Scholar]
- 156.Rutberg H, Hakanson E, Anderberg B, Jorfeldt L, Martensson J, Schildt B. Effects of the extradural administration of morphine, or bupivacaine, on the endocrine response to upper abdominal surgery. Br J Anaesth. 1984;56:233–237. doi: 10.1093/bja/56.3.233. [DOI] [PubMed] [Google Scholar]
- 157.Hakansson E, Anderberg B, Jorfeldt L, Martensson J, Rutberg H, Schildt B. Extradural morphine can suppress the endocrine response to upper abdominal surgery. Acta Anaesthesiol Scand Suppl. 1983;78:78. [Google Scholar]
- 158.Hesselvik F, Brodin B, Hakanson E, Rutberg H, von SH. Influence of epidural blockade on postoperative plasma fibronectin concentrations. Scand J Clin Lab Invest. 1987;47:435–440. [PubMed] [Google Scholar]
- 159.Ryan P, Schweitzer S, Woods R. Effect of epidural and general anesthesia compared with general anaesthesia alone in large bowel anastomoses: a prospective study. Eur J Surg. 1992;158:45–49. [PubMed] [Google Scholar]
- 160.Scheinin B, Rosenberg P. Effect of prophylactic epidural morphine or bupivacaine on postoperative pain after upper abdominal surgery. Acta Anaesthesiol Scand. 1982;26:474–478. doi: 10.1111/j.1399-6576.1982.tb01802.x. [DOI] [PubMed] [Google Scholar]
- 161.Seeling W, Ahnefeld F, Rosenberg G, Heirich H, Spilker D. Cardiovascular changes associated with epidural combined with general anaesthesia as compared to neuroleptanaesthesia. Anaesthesist. 1985;34:217–228. [Google Scholar]
- 162.Seeling W, Ahnefeld F, Hamann H, Heinrich H, Hutschenreiter S, Rosenberg G. Intrarenal aortic bypass operations: influence of neuroleptanaesthesia and continuous epidural anaesthesia on cardiovascular responses during surgery. Anaesthesist. 1985;34:417–428. [Google Scholar]
- 163.Seeling W, Ahnefeld F, Grunert A, Heinrich H, Lotz P, Rosenberg G, et al. Influence of neuroleptanaesthesia compared with continous epidural plus general anaesthesia on homeostasis and oxygen transport during infrarenal aortic bypass surgery. Anaesthesist. 1986;35:80–92. [PubMed] [Google Scholar]
- 164.Seeling W, Bruckmooser K, Hufner C, Kneitinger E, Rigg C, Rockemann M. Continuous thoracic epidural analgesia does not diminish postoperative complications after abdominal surgery in patients at risk. Anaesthesist. 1990;39:33–40. [PubMed] [Google Scholar]
- 165.Seeling W, Bothner U, Eifert B, Rockemann M, Schreiber M, Schurmann W, et al. Patient-controlled analgesia versus epidural analgesia with bupivacaine or morphine after major abdominal operations. No difference in postoperative outcome. Anaesthesist. 1991;40:614–623. [PubMed] [Google Scholar]
- 166.Seitz W, Lubbe N, Bechstein W, Fritz K, Kirchner E. Effects of anaesthesia and surgery on the hypothalamic hypophyseal adrenocortical system. Anasthesiol Intensivther Notfallmed Scherzther. 1985;20:119–124. [PubMed] [Google Scholar]
- 167.Sharrock N, Go G. Fibrinolytic activity following total knee arthroplasty under epidural or general anesthesia. Reg Anesth. 1992;17(suppl):94. [Google Scholar]
- 168.Shir Y, Raja S, Frank S. The effect of epidural versus general anesthesia on postoperative pain and analgesic requirements in patients undergoing radical prostatectomy. Anesthesiology. 1994;80:49–56. doi: 10.1097/00000542-199401000-00011. [DOI] [PubMed] [Google Scholar]
- 169.Simpson PJ, Radford SG, Forster SJ, Cooper GM, Hughes AO. The fibrinolytic effects of anaesthesia. Anaesthesia. 1982;37:3–8. doi: 10.1111/j.1365-2044.1982.tb00985.x. [DOI] [PubMed] [Google Scholar]
- 170.Slinger P, Shennib H, Wilson S. Post-thoracotomy pulmonary function: a comparison of epidural versus intravenous meperidine infusions. J Cardiothorac Vasc Anesth. 1995;9:128–134. doi: 10.1016/S1053-0770(05)80182-X. [DOI] [PubMed] [Google Scholar]
- 171.Smeets H, Kievit J, Dulfer F, van Kleef J. Endocrine-metabolic response to abdominal aortic surgery: a randomized trial of general anesthesia versus general plus epidural anesthesia. World J Surg. 1993;17:601–607. doi: 10.1007/BF01659119. [DOI] [PubMed] [Google Scholar]
- 172.Stathopoulou T, Melissaki A, Fountoulaki T, Pagouni H, Giala M. Systemic haemodynamic, enzymatic and acid-base changes with the use of tourniquet after general and spinal anaesthesia. Reg Anesth. 1992;17(suppl):181. [Google Scholar]
- 173.Stenseth R, Bjella L, Berg E, Christensen O, Levang O, Gisvold S. Thoracic epidural analgesia in aortocoronary bypass surgery 1: haemodynamic effects. Acta Anaesthesiol Scand. 1994;38:826–833. doi: 10.1111/j.1399-6576.1994.tb04013.x. [DOI] [PubMed] [Google Scholar]
- 174.Stenseth R, Bjella L, Berg E, Christensen O, Levang O, Gisvold S. Thoracic epidural analgesia in aortocoronary bypass surgery II: effects on the endocrine metabolic response. Acta Anaesthesiol Scand. 1994;38:834–839. doi: 10.1111/j.1399-6576.1994.tb04014.x. [DOI] [PubMed] [Google Scholar]
- 175.Stjernstrom H, Henneberg S, Eklund A, Tabow F, Arturson G, Wiklund L. Thermal balance during transurethral resection of the prostate. Acta Anaesthesiol Scand. 1985;29:743–749. doi: 10.1111/j.1399-6576.1985.tb02293.x. [DOI] [PubMed] [Google Scholar]
- 176.Traynor C, Paterson L, Ward ID, Morgan M, Hall GM. Effects of extradural analgesia and vagal blockade on the metabolic and endocrine response to upper abdominal surgery. Br J Anaesth. 1982;54:319–323. doi: 10.1093/bja/54.3.319. [DOI] [PubMed] [Google Scholar]
- 177.Tulla H, Takala J, Alhava E, Hendolin H, Manninen H, Kari A, et al. Does the anaesthetic method influence the postoperative breathing pattern and gas exchange in surgery? A comparison between general and spinal anaesthesia. Acta Anaesthesiol Scand. 1992;36:101–105. doi: 10.1111/j.1399-6576.1992.tb03431.x. [DOI] [PubMed] [Google Scholar]
- 178.Tuman K, McCarthy R, March R, DeLaria G, Patel R, Ivankovich A. Effects of epidural anesthesia and analgesia on coagulation and outcome after major vascular surgery. Anesth Analg. 1991;73:696–704. doi: 10.1213/00000539-199112000-00005. [DOI] [PubMed] [Google Scholar]
- 179.Tverskoy M, Cozacov C, Ayache M, Bradley E, Kissin I. Postoperative pain after inguinal herniorrhaphy with different types of anesthesia. Anesth Analg. 1990;70:29–35. doi: 10.1213/00000539-199001000-00006. [DOI] [PubMed] [Google Scholar]
- 180.Valentin N, Lomholt B, Jensen JS, Hejgaard N, Kreiner S. Spinal or general anaesthesia for surgery of the fractured hip? A prospective study of mortality in 578 patients. Br J Anaesth. 1986;58:284–291. doi: 10.1093/bja/58.3.284. [DOI] [PubMed] [Google Scholar]
- 181.Wallace D, Leveno K, Cunningham F, Giesecke A, Shearer V, Sidawi J. Randomized comparison of general and regional anesthesia for cesarean delivery in pregnancies complicated by severe pre-eclampsia. Obstet Gynecol. 1995;86:193–199. doi: 10.1016/0029-7844(95)00139-i. [DOI] [PubMed] [Google Scholar]
- 182.Watters J, March R, Desai D, Monteith K, Hurtig J. Epidural anaesthesia and analgesia do not affect energy expenditure after major abdominal surgery. Can J Anaesth. 1993;40:314–319. doi: 10.1007/BF03009628. [DOI] [PubMed] [Google Scholar]
- 183.Wattwil M, Sundberg A, Olsson J, Nordstrom S. Thoracolumbar epidural anaesthesia blocks the circulatory response to laryngoscopy and intubation. Acta Anaesthesiol Scand. 1987;31:529–531. doi: 10.1111/j.1399-6576.1987.tb02616.x. [DOI] [PubMed] [Google Scholar]
- 184.Wessen A, Persson P, Nilsson A, Hartvig P. Clinical pharmacokinetics of propofol given as a constant-rate infusion and in combination with epidural blockade. J Clin Anesth. 1994;6:193–198. doi: 10.1016/0952-8180(94)90058-2. [DOI] [PubMed] [Google Scholar]
- 185.Whelan P, Morris P. Immunological responsiveness after transurethral resection of the prostate: general versus spinal anaesthetic. Clin Exp Immunol. 1982;48:611–618. [PMC free article] [PubMed] [Google Scholar]
- 186.White I, Chappell W. Anaesthesia for surgical correction of fractured femoral neck: a comparison of three techniques. Anaesthesia. 1980;35:1107–1100. doi: 10.1111/j.1365-2044.1980.tb05053.x. [DOI] [PubMed] [Google Scholar]
- 187.Williams-Russo P, Sharrock N, Mattis S, Szatrowski T, Charlson M. Cognitive effects after epidural vs general anesthesia in older adults: a randomized trial. JAMA. 1995;274:44–50. [PubMed] [Google Scholar]
- 188.Williams-Russo P, Sharrock N, Haas S, Insall J, Windsor R, Laskin R, et al. Randomized trial of epidural versus general anesthesia: outcomes after primary total knee replacement. Clin Orthop. 1996;331:199–208. doi: 10.1097/00003086-199610000-00028. [DOI] [PubMed] [Google Scholar]
- 189.Worsley M, Wishart H, Peebles Brown D, Aitkenhead A. High spinal nerve block for large bowel anastomosis: a prospective study. Br J Anaesth. 1988;60:836–840. doi: 10.1093/bja/60.7.836. [DOI] [PubMed] [Google Scholar]
- 190.Wust H, Spirgatis WD, Sandmann W, Krian A, Richter O. The effects of different anaesthesic techniques on lactate under the course of aorto-femoral bypass operation. Anasthesiol Intensivmed Notfallmed Schmerzther. 1980;15:87–98. [PubMed] [Google Scholar]
- 191.Yeager M, Glass D, Neff R, Brinck Johnsen T. Epidural anesthesia and analgesia in high-risk surgical patients. Anesthesiology. 1987;66:729–736. doi: 10.1097/00000542-198706000-00004. [DOI] [PubMed] [Google Scholar]
- 192.Zwarts S, Hasenbos M, Gielen M, Kho H. The effect of continuous epidural analgesia with sufentanil and bupivacaine during and after thoracic surgery on the plasma cortisol concentration and pain relief. Reg Anesth. 1989;14:183–188. [PubMed] [Google Scholar]
- 193.Antiplatelet Trialists' Collaboration. Collaborative overview of randomised trials of antiplatelet therapy. 1. Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. BMJ. 1994;308:81–106. [PMC free article] [PubMed] [Google Scholar]
- 194.Go A. Cardiac outcomes after regional or general anesthesia: do we have the answer? Anesthesiology. 1996;84:1–2. doi: 10.1097/00000542-199601000-00001. [DOI] [PubMed] [Google Scholar]
- 195.Sorenson R, Pace N. Anesthestic techniques during surgical repair of femoral neck fractures. Anesthesiology. 1992;77:1095–1104. doi: 10.1097/00000542-199212000-00009. [DOI] [PubMed] [Google Scholar]
- 196.Parker M, Urwin S, Handoll H, Griffiths R. Cochrane Collaboration. Cochrane Library. Issue 1. Oxford: Update Software; 2000. General versus spinal/epidural anaesthesia for surgery for hip fractures in adults. [Google Scholar]
- 197.Rodgers A, Sage D, Futter M, MacMahon S. Attitudes and practices of New Zealand anaesthetists with regard to epidural and subarachnoid anaesthesia. Anaesth Intensive Care. 1996;24:79–86. doi: 10.1177/0310057X9602400114. [DOI] [PubMed] [Google Scholar]
- 198.Rigg J, Jamrozik K, Myles P, Silbert B, Peyton P, Parsons R, et al. Design of the multicenter Australian study of epidural anesthesia and analgesia in major surgery: The MASTER trial. Controlled Clin Trials. 2000;21:244–256. doi: 10.1016/s0197-2456(00)00045-3. [DOI] [PubMed] [Google Scholar]
- 199.Tarkkila P, Kaukinen S. Complications during spinal anesthesia: a prospective study. Reg Anesth. 1991;16:101–106. [PubMed] [Google Scholar]
- 200.Tanaka K, Watanabe R, Harada T, Dan K. Extensive application of epidural anesthesia and analgesia in a university hospital: incidence of complications related to technique. Reg Anesth. 1993;18:34–38. [PubMed] [Google Scholar]
- 201.Horlocker T, McGregor D, Matsushige D, Schroeder D, Besse J. A retrospective review of 4767 consecutive spinal anesthetics: central nervous system complications. Anesth Analg. 1997;84:578–584. doi: 10.1097/00000539-199703000-00021. [DOI] [PubMed] [Google Scholar]
- 202.Ballantyne J, Carr D, deFerranti S, Suarez T, Lau J, Chalmers T, et al. The comparitive effects of postoperative analgesia therapies on pulmonary outcome: cumulative meta-analysis of randomized, controlled trials. Anesth Analg. 1998;86:598–612. doi: 10.1097/00000539-199803000-00032. [DOI] [PubMed] [Google Scholar]


