Abstract
Pelvic floor muscle (PFM) dysfunction has been commonly associated with urinary disorders and lumbo-pelvic pain. Transabdominal (TA) ultrasound is currently used by physical therapists to assess PFM function. Controversy exists regarding the correlation between TA ultrasound measurement and vaginal palpation for assessment of PFM contraction, and this relationship has not yet been examined concurrently during the same contraction. The purpose of this study was to determine the correlation of digital palpation and TA ultrasound to assess PFM contraction when recorded 1) simultaneous to digital palpation during one contraction and 2) following digital palpation testing in another contraction. A descriptive correlational design was used to describe the relationship between variables. A total of 19 women (both asymptomatic women and those with incontinence or lumbo-pelvic pain) participated in the study. The modified Oxford scale was used to grade PFM contraction in digital palpation testing. The amount of bladder base movement on ultrasound was measured and considered as an indicator of PFM activity. Two trials were performed for TA ultrasound measurement: 1) simultaneous to digital palpation during one contraction, and 2) following digital palpation testing in another contraction. Spearman's correlation coefficient was used for analysis. There was a significant correlation between digital palpation and TA ultrasound for PFM assessment when measured simultaneously in one contraction (rho=0.62, p=0.01) and separately in a different contraction (rho=0.52, p=0.02), with a stronger correlation found in simultaneous testing. In conclusion, digital palpation and TA ultrasound measurement are significantly correlated and measure comparable parameters in evaluation of PFM contraction.
KEYWORDS: Digital Palpation, Modified Oxford Scale, Pelvic Floor Muscles, Transabdominal Ultrasound
The pelvic floor muscles (PFM) form the floor of the pelvic and abdominal cavity1. PFM are considered to have the dual function of controlling bladder continence and providing stability in the lumbo-pelvic region2,3; i.e., each play an important role in generating, maintaining, and increasing intra-abdominal pressure and maintaining bladder continence. Evidence has confirmed the co-activation of the pelvic floor and abdominal muscles for development of intra-abdominal pressure and trunk load transfer2–6. Consequently, PFM dysfunction has been commonly associated with urinary disorders or lumbo-pelvic pain.
Assessment of PFM function before and after treatment has been generally accepted as an important parameter in clinical and scientific issues to analyze whether the training protocol has been effective7. Various clinical methods have been used to assess PFM function in women attending physical therapy. Manual muscle testing, assessed by vaginal palpation, is one of the most common clinical methods currently used to evaluate PFM contraction1,7–9. However, the digital palpation method may not be appropriate for use in certain populations in which vaginal examination may be against social norms or unpleasant10,11.
More recently, there has been interest in the use of transabdominal (TA) ultrasound to evaluate PFM function1,10–14. TU ultrasound of the TA imaging has several clinical advantages, the method is safe, non-invasive, and comfortable for the patient and the patient does not need to undress. This may be important in specific populations where vaginal assessment may not be desirable or possible. The lifting aspect of the pelvic floor is quantified and measured as an indicator of PFM function in TA ultrasound imaging1,10–14. Although several studies have investigated the comparison of digital palpation to the other measurement tools for PFM evaluation, such as perineometery15,16, vaginal balloon17, electromyography7, and transperineal ultrasound10,11,18,19, few studies have been conducted to determine the association between TA ultrasound measurement and digital muscle testing of PFM action10,12.
With the use of different designs and testing procedures, controversial results have been reported regarding the correlation between TA ultrasound measurement and vaginal palpation. Although Thompson et al10 found significant correlation between TA ultrasound measurements and manual testing for PFM contraction, others have not associated the TA ultrasound and digital palpation measures11. In one study conducted by Sherburn et al12, during the observation of bladder base displacement on ultrasound, digital vaginal examination was simultaneously performed by another examiner to confirm correct muscle activation. In the second study reported by the same researchers, no simultaneous vaginal palpation was performed during the evaluation of PFM contraction using TA ultrasound11. However, in both studies the digital palpation scores and TA ultrasound measurements for PFM contraction were recorded during different contractions. No study has performed digital palpation and TA ultrasound for PFM evaluation during the same contraction. In addition, subjects with lumbo-pelvic pain have not yet been included in such studies.
The purpose of this study was to investigate the association between digital palpation and TA ultrasound measurement for the assessment of PFM contraction when recorded simultaneously during the same contraction and in separate contractions in a mixed population (asymptomatic women and women with urinary disorders or lumbo-pelvic pain).
Methods
Subjects
A total of 19 women between the ages of 22 and 40 years (mean = 30.63, SD = 5.68) participated in the study. To have a wide range of manually graded muscle strength, the subject population in this study was a mixed population including 7 asymptomatic women, 3 women with urinary incontinence, and 9 women with chronic low back pain. Subjects with low back pain or urinary incontinence were selected among the individuals seen in the physical therapy clinics. The asymptomatic women were selected from among those who accompanied a patient or from staff at the University of Social Welfare and Rehabilitation Sciences. All the subjects signed an informed consent approved by the Human Subjects Committee at the University of Social Welfare and Rehabilitation Sciences before participating.
The asymptomatic subjects had no complaint of pain or dysfunction in the low back, pelvis, or lower extremities and no symptoms of incontinence. Low back pain patients were included if they had a history of low back pain for more than six weeks before the study or had intermittent pain and had experienced at least three episodes of pain, each lasting more than one week, during the year before the study. Exclusion criteria were pregnancy, history of spinal surgery and spinal or pelvic fracture, urinary tract infection, vaginal infection, and known neurological disorders. The physical characteristics of the subjects are shown in Table 1.
TABLE 1.
Demographic data of the subjects (N = 19).
| Variables | Mean (SD) | Min | Max |
|---|---|---|---|
| Age (years) | 30.6 (5.7) | 22 | 40 |
| Weight (kg) | 65.2 (10.01) | 50 | 85 |
| Height (cm) | 160.2 (5.3) | 151 | 171 |
| BMI (kg/m2) | 25.4(3.9) | 19.7 | 33.3 |
| Number of pregnancies∗ | 1(5) | 0 | 5 |
The number of pregnancies: Data are median (range)
Procedures
Two examiners blinded to the subjects' health status tested the subjects. One measured PFM contraction on TA ultrasound and the other performed digital palpation. Two trials were performed for TA ultrasound measurement: during the first trial first examiner performed manual muscle testing by vaginal palpation and simultaneously the second examiner measured the displacement that occurred on TA ultrasound during the same contraction. During the second trial, the second examiner performed TA ultrasound measurement following the digital palpation testing in another contraction. The examiners and their results were blinded from each other. All testing procedures were performed in the biomechanics laboratory of the physical therapy department at the University of Social Welfare and Rehabilitation Sciences.
Transabdominal Ultrasound Measurement
The transabdominal ultrasound used in this study was an imaging unit set in B-mode (Ultrasonix-ES500, Canada) with a 3.5 MHz curved array transducer. The procedure described by others10–14 was followed to measure the amount of bladder base movement as an indicator of PFM contraction. All women were assessed by the same examiners. A standardized bladder filling protocol was used prior to imaging. One hour before the measurement, the women were asked to fill their bladder by consuming 600–750 ml of water within half an hour (completed half an hour prior to testing), without voiding until after the ultrasound assessment. The subject's position was crook-lying supine with one pillow under the head. The ultrasound probe was transversely placed in the midline on the supra-pubic region and was angled in a caudal/posterior direction to obtain a clear image of the inferior-posterior aspect of the bladder. A marker was placed at the bladder base on the junction of the hyper- and hypo-echoic areas in the region of the greatest displacement visualized during a PFM contraction. The marker was first placed on the bladder base at the rest. The participants were instructed to draw in and lift the PFM to perform a voluntary PFM contraction, and the marker was then placed on the bladder base at the point of maximal displacement during the PFM contraction. The amount of bladder base displacement from resting position at the end of each contraction was measured in millimeters (mm). If the bladder base was found to descend during PFM contraction, the displacement was given a negative value. The ultrasound transducer was not moved during the testing procedure.
Digital Palpation Testing
Digital muscle testing is one of the most common clinical methods used by physical therapists to assess PFM strength and the woman's ability to perform correct PFM contractions1,7–9. The PFM contraction was assessed by digital palpation testing using a modified Oxford muscle grading scale. The detailed procedure for this test has been described by Sapsford et al8. The modified Oxford scale is a 6-point measurement scale: 0 = nothing, 1= flicker, 2 = weak squeeze, 3 = moderate squeeze and lift, 4 = good squeeze and lift, 5 = strong squeeze and lift. All the subjects were assessed by the same examiner. The subject's position and the instructions for performing the PFM contraction were the same as those used during the ultrasound measurement.
Data Analysis
MedCalc® statistical software was used for data analysis. The association between TA ultrasound measurement and digital palpation testing (modified Oxford scale) to evaluate PFM contraction was assessed using Spearman's coefficient of correlation.
Results
The demographic data for the subjects is presented in Table 1. The measurements taken using TA ultrasound and digital palpation for PFM contraction are summarized in Table 2. The presented data are mean (SD) for TA ultrasound measurements and median (range) for vaginal palpation testing, which was considered ordinal.
TABLE 2.
Descriptive statistics for digital palpation andTA ultrasound measurements.
| Variables | Mean (SD) Median (range) | Lowest value | Highest value | 95% CI for mean/median |
|---|---|---|---|---|
| TA ultrasound measurement in trial 1 (mm)∗ | 4.9 (6.9) | −6.2 | 23.8 | 1.6–8.3 |
| TA ultrasound measurement in trial 2 (mm)∗ | 7.4 (6.5) | 0.1 | 23.8 | 4.3–10.6 |
| Digital palpation testing (modified Oxford scale)∗∗ | 3(3) | 2 | 5 | 3–4 |
Trial 1 = Ultrasound measurement simultaneous with digital palpation testing in same contraction
Trial 2 = Ultrasound measurement following digital palpation testing in separate contraction
TA = Transabdominal, = Data are mean (SD),
= Data are median (range), 95% CI = 95% confidence interval
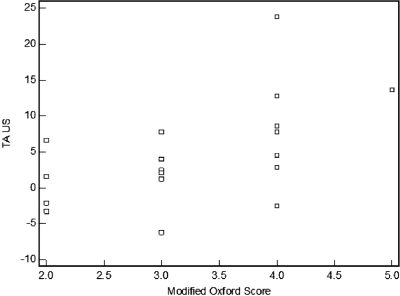
Table 3 presents the correlation between the TA ultrasound measurements and digital palpation testing (modified Oxford scale). There was a significant correlation between manually graded PFM strength and TA ultrasound measurement when simultaneously performed (rho=0.62, p=0.01, 95% CI for rho: 0.23 – 0.83) (Table 3, Figure 1).
TABLE 3.
Correlation between digital palpation testing andTA ultrasound measurements.
| Variables | Digital palpation testing (modified Oxford scale) | ||
|---|---|---|---|
| rho | P-value | 95% CI for rho | |
| TA ultrasound measurement simultaneous with digital palpation | 0.62 | <0.01 | 0.23–0.83 |
| TA ultrasound measurement following digital palpation | 0.52 | 0.02 | 0.08–0.78 |
TA = Transabdominal, CI = confidence interval
FIGURE 1.
Correlation between digital palpation testing and TA ultrasound measurement when simultaneously performed. TA = transabdominal.
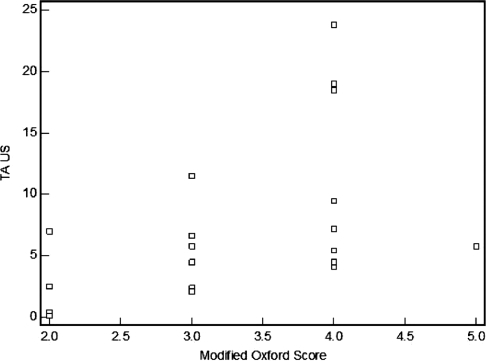
A significant association was also found between TA ultrasound measurement and digital palpation testing when tested in separate contractions (rho= 0.52, p=0.02, 95% CI for rho: 0.08 – 0.78) (Table 3, Figure 2).
FIGURE 2.
Correlation between digital palpation testing and TA ultrasound measurement when tested in separate contractions. TA = transabdominal.
Discussion
The modified Oxford muscle grading scale, used in this study, is a frequently used digital assessment of PFM contraction. Digital examination is a straightforward and clinically practical means of PFM assessment and requires no special equipment. It has been often compared with other measurement approaches for evaluation of the PFM contraction such as perineometery15,16, vaginal balloon17, electromyography7, and transperineal ultrasound10,11,18,19. However, vaginal palpation is inappropriate for use in certain populations10,11.
Real-time ultrasound imaging is a reliable and valid method used by physical therapists to evaluate muscle structure, function, and activation patterns. The value of ultrasound imaging in a clinical rehabilitation setting is that it allows for real-time study of the muscles as they contract20. It provides direct feedback to the therapist and patient and assists them in the correct activation of the muscles. This is especially important when the activation pattern of deep muscles such as deep trunk and pelvic floor, which are difficult to access, is investigated.
Transperineal ultrasound has been previously used to assess the PFM contraction by measuring the amount of bladder neck elevation during PFM contraction10,11,18,19. However, the transperineal method may be unsuitable for use in certain populations where placing the ultrasound transducer on the perineum is unpleasant. The location of the probe on the perineum can also limit some functional maneuvers.
More recently, TA ultrasound has been used by therapists to assess the lifting aspect of the pelvic floor by observing movement of the bladder base during PFM contraction. This technique is comfortable for the patient, quick, and easy to apply. The patient does not need to get undressed and the probe is not placed at the perineum. This makes TA ultrasound a valuable tool for PFM evaluation in specific populations where vaginal palpation or perineal examination may not be possible or desirable, e.g. children, adolescents, men, victims of sexual abuse, and some ethnic groups. The reliability of TA ultrasound for measurement of bladder base movement during PFM contraction has been established previously10,12.
The result of this study showed a significant association between TA ultrasound measurement and digital palpation testing for PFM evaluation when simultaneously or separately tested (Table 3, Figures 1, 2). Similar findings have been reported elsewhere10,12. Dietz et al18 also reported a positive correlation between the measurements taken using transperineal ultrasound and manual muscle testing. In contrast, Sherburn et al12 found no significant relationship between ultrasound measures and digital palpation. This difference could arise from the fact that different approaches have been used in the previous studies. In the study conducted by Sherburn et al12, during the observation of bladder base displacement on ultrasound, vaginal examination was simultaneously performed by another examiner. But in the study of Thompson et al10, no simultaneous vaginal examination was carried out during ultrasound measurement. The subject population was also different in the earlier studies. However, in both studies the strength of PFM was manually graded separately from ultrasound measurement.
The significance of this study was in assessing and comparing the relationship between digital palpation and TA ultrasound when recorded simultaneously during the same contraction or in separate contractions. Our data indicate stronger correlation between the measures when they are evaluated simultaneously (Table 3, Figures 1, 2). We think vaginal palpation gives better feedback as to PFM contraction. Thus, a stronger association was found between the measures when they were performed simultaneously during the same contraction.
The significant correlation between the measures in separate tests, (rho=0.52, P=0.02), complements the results of the previous studies. Peschers et al7 and B⊘ and Finckenhagen17 believed that digital palpation was the only way to ensure a correct PFM contraction and considered it a gold standard. Although digital examination is important for palpating components of pelvic floor dysfunction, it is not the only method to assess PFM action. The result of the study conducted by Sherburn et al12 demonstrated that the bladder base elevation observed on TA ultrasound confirms whether correct PFM muscle contraction has been performed. Concomitant digital palpation may therefore not be necessary in assessing PFM contraction.
The value of the TA view is that it allows for evaluation of both sides of the pelvic floor at once. Another advantage of using the TA ultrasound is that any pressures by the transducer against the abdominal wall, and movement of the abdominal wall, are dissipated by the fluid-filled bladder and so do not affect the PFM displacement values. Additionally, the probe placement in TA ultrasound method does not restrict movement of the lower limbs, which is important in the assessment of the subjects with lumbo-pelvic pain.
Limitations
TA ultrasound may be criticized because of the lack of a fixed bony landmark as a reference point. Measures of displacement are only expressed relative to a chosen starting point rather than an anatomical landmark. In this study similar to the others, a distinct edge of the endopelvic fascia in the region of its greatest observed displacement that was clearly observable during the movement was selected for measurement.
Another area of concern in this study is the sample population. The participants in previous similar studies were mainly asymptomatic or incontinent women. Patients with lumbo-pelvic pain were not included in those studies. With regard to the dual function of PFM in controlling continence and providing trunk stability, the sample population in this study was a mixed population of asymptomatic women and those with urinary incontinence or chronic low back pain.
Conclusion
This study investigated the association between digital palpation and TA ultrasound for the assessment of PFM contraction when measured simultaneously during the same contraction and during separate contractions. Our data indicate a significant correlation between vaginal palpation and TA ultrasound measurement when simultaneously or separately tested. Stronger correlation was found between the measures when performed simultaneously. This suggests that these two methods of evaluation measure comparable parameters. TA ultrasound can be used as a valuable tool for measuring PFM function.
Footnotes
This research was reviewed and was approved by the Human Subjects Committee at the University of Social Welfare and Rehabilitation Sciences.
REFERENCES
- 1.B⊘ K, Sherburn M. Evaluation of female pelvic-floor muscle function and strength. Phys fler. 2005;85:269–282. [PubMed] [Google Scholar]
- 2.Richardson CA, Jull GA, Hodges PW, Hides JA. flerapeutic Exercise for Spinal Segmental Stabilization in Low Back Pain: Scientific Basis and Clinical Approach. Edinburgh, UK: Churchill Livingstone; 1999. [Google Scholar]
- 3.Sapsford R. Rehabilitation of pelvic floor muscles utilizing trunk stabilization. Man fler. 2004;9:3–12. doi: 10.1016/s1356-689x(03)00131-0. [DOI] [PubMed] [Google Scholar]
- 4.Neumann P, Gill V. Pelvic floor and abdominal muscle interaction: EMG activity and intra-abdominal pressure. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13:125–132. doi: 10.1007/s001920200027. [DOI] [PubMed] [Google Scholar]
- 5.Hodges PW, Eriksson AEM, Shirley D, Gandevia SC. Intra-abdominal pressure increases stiffness of the lumbar spine. J Biomech. 2005;38:1873–1880. doi: 10.1016/j.jbiomech.2004.08.016. [DOI] [PubMed] [Google Scholar]
- 6.Sapsford R, Hodges PW, Richardson CA, et al. Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neurourol Urodyn. 2001;20:31–42. doi: 10.1002/1520-6777(2001)20:1<31::aid-nau5>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 7.Peschers UM, Gingelmaier A, Jundt K, et al. Evaluation of pelvic floor muscle strength using four different techniques. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12:27–30. doi: 10.1007/s001920170090. [DOI] [PubMed] [Google Scholar]
- 8.Sapsford R, Bullock-Saxton J, Markwell S. Women's Health. A Textbook for Physiotherapists. London, UK: WB Saunders; 1998. [Google Scholar]
- 9.Devreese A, Staes F, De Weerdt W, et al. Clinical evaluation of pelvic floor muscle function in continent and incontinent women. Neurourol Urodyn. 2004;23:190–197. doi: 10.1002/nau.20018. [DOI] [PubMed] [Google Scholar]
- 10.Thompson JA, O'Sullivan PB, Briffa NK, et al. Assessment of pelvic floor movement using transabdominal and transperineal ultrasound. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:285–292. doi: 10.1007/s00192-005-1308-3. [DOI] [PubMed] [Google Scholar]
- 11.Thompson JA, O'Sullivan PB, Briffa NK, Neumann P. Comparison of transperineal and transabdominal ultrasound in the assessment of voluntary pelvic floor muscle contractions and functional manoeuvres in continent and incontinent women. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:779–786. doi: 10.1007/s00192-006-0225-4. [DOI] [PubMed] [Google Scholar]
- 12.Sherburn M, Murphy CA, Carroll S, et al. Investigation of transabdominal real-time ultrasound to visualize the muscles of the pelvic floor. Aust J Physiother. 2005;51:167–170. doi: 10.1016/s0004-9514(05)70023-4. [DOI] [PubMed] [Google Scholar]
- 13.Kelly M, Tan BK, Thompson J, et al. Healthy adults can more easily elevate the pelvic floor in standing than in crook-lying: An experimental study. Aust J Physiother. 2007;53:187–191. doi: 10.1016/s0004-9514(07)70026-0. [DOI] [PubMed] [Google Scholar]
- 14.B⊘ K, Sherburn M, Allen T. Transabdominal ultrasound measurement of pelvic floor muscle activity when activated directly or via a transversus abdominis muscle contraction. Neurourol Urodyn. 2003;22:582–588. doi: 10.1002/nau.10139. [DOI] [PubMed] [Google Scholar]
- 15.Hundley AF, Wu JM, Visco AG. A comparison of perineometer to brink score for assessment of pelvic floor muscle strength. Am J Obstet Gynecol. 2005;192:1583–1591. doi: 10.1016/j.ajog.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 16.Isherwood PJ, Rane A. Comparative assessment of pelvic floor strength using a perineometer and digital examination. BJOG. 2000;107:1007–1011. doi: 10.1111/j.1471-0528.2000.tb10404.x. [DOI] [PubMed] [Google Scholar]
- 17.B⊘ K, Finckenhagen HB. Vaginal palpation of pelvic floor muscle strength: Inter-test reproducibility and comparison between palpation and vaginal squeeze pressure. Acta Obstet Gynecol Scand. 2001;80:883–887. doi: 10.1034/j.1600-0412.2001.801003.x. [DOI] [PubMed] [Google Scholar]
- 18.Dietz HP, Jarvis SK, Vancaillie TG. The assessment of levator muscle strength: A validation of three ultrasound techniques. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13:156–159. doi: 10.1007/s192-002-8346-5. [DOI] [PubMed] [Google Scholar]
- 19.Thompson JA, O'Sullivan PB, Briffa NK, Neumann P. Assessment of voluntary pelvic floor muscle contraction in continent and incontinent women using transperineal ultrasound, manual muscle testing and vaginal squeeze pressure measurements. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:624–630. doi: 10.1007/s00192-006-0081-2. [DOI] [PubMed] [Google Scholar]
- 20.Whittaker JL, Thompson JA, Teyhen DS, Hodges P. Rehabilitative ultrasound imaging of pelvic floor muscle function. J Orthop Sports Phys fler. 2007;37:487–498. doi: 10.2519/jospt.2007.2548. [DOI] [PubMed] [Google Scholar]