Abstract
Objective
To test the hypotheses that an egg breakfast, in contrast to a bagel breakfast matched for energy density and total energy, would enhance weight loss in overweight and obese participants while on a reduced-calorie weight loss diet.
Subjects
Men and women (n=152), age 25–60 years, body mass index (BMI) ≥25 and ≤50 kg m−2.
Design
Otherwise healthy overweight or obese participants were assigned to Egg (E), Egg Diet (ED), Bagel (B) or Bagel Diet (BD) groups, based on the prescription of either an egg breakfast containing two eggs (340 kcal) or a breakfast containing bagels matched for energy density and total energy, for at least 5 days per week, respectively. The ED and BD groups were suggested a 1000 kcal energy-deficit low-fat diet, whereas the B and E groups were asked not to change their energy intake.
Results
After 8 weeks, in comparison to the BD group, the ED group showed a 61% greater reduction in BMI (−0.95±0.82 vs −0.59±0.85, P<0.05), a 65% greater weight loss (−2.63±2.33 vs −1.59±2.38 kg, P<0.05), a 34% greater reduction in waist circumference (P<0.06) and a 16% greater reduction in percent body fat (P=not significant). No significant differences between the E and B groups on the aforementioned variables were obtained. Further, total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol and triglycerides, did not differ between the groups.
Conclusions
The egg breakfast enhances weight loss, when combined with an energy-deficit diet, but does not induce weight loss in a free-living condition. The inclusion of eggs in a weight management program may offer a nutritious supplement to enhance weight loss.
Keywords: satiety, hunger, proteins, bagels
Introduction
Nearly 7% of the world population is obese1 and about 66% of the adults in the United States are overweight or obese.2 Obesity is associated with a number of adverse medical conditions including increased risk of gallbladder disease, hypertension, type 2 diabetes mellitus, coronary heart disease (CHD), osteoarthritis, cancer death and reduced life expectancy.3–8 Obesity is also associated with adverse social and psychological consequences, including bias, discrimination and decreased quality of life.9,10
More effective treatment strategies are urgently needed for obesity management. The total caloric intake or energy density of one’s diet appears to be associated with obesity11–14 and a diet that induces a negative energy balance continues to be an important part of obesity management. Strategies to achieve the difficult task of eating less than desired include reduction of the energy density of foods by increasing food volume by the addition of fluids,15,16 bulk17–19 or their combination;20 or by increasing satiety by various anorectic drugs or macronutrient combinations of high satiety value.
Satiety is positively associated with the protein, fiber and water content of foods and negatively with fat and palatability ratings.21,22 However, within food groups, there may be as much as a twofold difference in satiety values, suggesting that certain foods promote greater satiety independent of macronutrient content or energy density. An egg is an example of such a food that has a 50% greater satiety index compared to white bread or ready-to-eat breakfast cereal.21 Compared to an isocaloric bagel breakfast of equal weight, an egg breakfast had a greater satiating effect, which translated into a lower caloric intake at lunch.23 The resulting decrease in energy consumption lasted for at least 24 h after the egg breakfast.
This study was undertaken to exploit the short-term satiating benefits of an egg breakfast23 for weight loss in a longer-term trial. The objectives were to determine if the incorporation of an egg breakfast in the diet by overweight or obese subjects would (1) induce reduced energy intake and unintentional weight loss, even when not attempting weight reduction; or (2) enhance weight loss when following a reduced energy diet. We compared the effects of an egg vs isocaloric bagel breakfast of equal weight on weight loss, indices of body size and composition, dietary compliance, food cravings and health-specific quality of life.
Materials and methods
The study was approved by the institutional review boards at Pennington Biomedical Research Center and at Saint Louis University. Written informed consent was obtained from the participants. We certify that all applicable institutional and governmental regulations regarding the ethical use of human volunteers were followed during this research.
Participants
Of the 160 participants enrolled, 8 did not complete the trial. The final study sample included 152 participants (131 women and 21 men; mean age 45.0±9.4 years; black participants 47.7% and white participants 52.3%). Demographic characteristics of the participants are provided in Table 1.
Table 1.
Baseline demographic and body size characteristics
| Variable | Bagel | Egg | Bagel diet | Egg diet | Total |
|---|---|---|---|---|---|
| (mean±s.e.) | (mean±s.e.) | (mean±s.e.) | (mean±s.e.) | (mean±s.e.) | |
| n | 35 | 38 | 40 | 39 | 152 |
| F/M | 30/5 | 33/5 | 34/6 | 34/5 | 131/21 |
| Race (B/W) | 16/19 | 17/20 | 20/20 | 19/20 | 72/79a |
| Age (years) | 44.6±1.6 | 45.2±1.5 | 44.9±1.5 | 45.2±1.5 | 45.0±0.8 |
| BMI (kg m−2) | 35.0±1.2 | 34.0±1.0 | 35.5±1.1 | 33.8±1.0 | 34.6±0.5 |
| Weight (kg) | 94.4±3.1 | 92.9±3.0 | 95.8±3.3 | 92.5±2.7 | 93.9±1.5 |
| Waist (cm) | 103.8±2.6 | 101.7±2.3 | 103.9±2.3 | 100.7±2.4 | 102.5±1.2 |
| Body fat (%) | 41.0±1.2 | 40.6±1.1 | 40.8±1.0 | 40.1±1.1 | 40.6±0.6 |
| Cholesterol (mg/100 ml) | 201.2±7.4 | 193.3±5.7 | 198.1±6.6 | 195.2±6.9 | 196.9±3.3 |
| HDL (mg/100 ml) | 53.7±1.5 | 57.9±2.1 | 55.9±2.1 | 53.1±1.7 | 55.2±0.9 |
| LDL (mg/100 ml) | 123.2±6.4 | 111.9±4.6 | 199.8±5.3 | 117.9±5.4 | 118.2±2.7 |
| Triglycerides (mg/100 ml) | 121.4±11.0 | 116.2±13.2 | 112.1±8.4 | 120.9±10.4 | 117.6±5.4 |
| Restraint | 10.0±0.8 | 9.9±0.9 | 10.7±0.8 | 9.7±0.8 | 10.1±0.4 |
| Disinhibition | 7.1±0.7 | 7.7±0.6 | 8.2±0.6 | 7.4±0.7 | 7.6±0.3 |
| Hunger | 5.4±0.6 | 5.6±0.6 | 5.8±0.6 | 4.5±0.5 | 5.3±0.3 |
| Physical functioning | 83.1±3.6 | 85.8±3.0 | 81.4±3.5 | 85.3±3.1 | 83.8±1.6 |
| Role limits—physical | 87.9±4.5 | 93.4±3.7 | 91.2±3.7 | 91.9±3.5 | 91.2±1.9 |
| Role limits—emotional | 89.2±4.2 | 87.4±4.5 | 91.7±3.5 | 89.5±4.2 | 89.5±2.0 |
| Energy/fatigue | 65.1±3.3 | 65.9±3.4 | 67.3±3.1 | 61.7±2.7 | 65.0±1.6 |
| Emotional well-being | 79.5±2.8 | 82.9±2.4 | 81.4±2.2 | 78.9±1.8 | 80.7±1.2 |
| Pain | 79.1±4.2 | 82.5±2.7 | 82.9±2.8 | 81.1±3.3 | 81.5±1.6 |
| General well-being | 74.3±3.1 | 73.6±3.2 | 72.3±2.9 | 74.7±2.4 | 73.7±1.5 |
| Percent compliance | 87±1.7 | 90±1.1 | 85±2.4 | 87±1.5 | 87±0.9 |
Abbreviations: B, black; BMI, body mass index; F, female; HDL, high-density lipoprotein; LDL, low-density lipoprotein; M, male; W, white.
One person did not provide ethnicity.
Measures
Demographic characteristics
Demographic characteristics were ascertained at the physical examination, including age, height, weight and waist circumference (measured at the iliac crest). Height and weight were measured after removal of shoes and heavy outer garments. Body mass index (BMI) was then calculated (kg m−2). Body fat percent was measured by dual-energy X-ray absorptiometry (DEXA).
Blood chemistry
Serum was separated and used for blood chemistry study, including total cholesterol, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol and triglyceride determinations. Total cholesterol, triglycerides and HDL cholesterol were analyzed on a Beckman Coulter DXC 600 Pro. LDL was calculated using the Friedewald equation. Analyses were conducted by the Clinical Chemistry Core of the Pennington Biomedical Research Center.
Breakfast compliance
The number of days for which participants were compliant was divided by the number of days during which participants were in the program, yielding a percentage.
The RAND 36-item health survey 1.0
The RAND 36-item health survey 1.0 (RAND-36; Stewart et al.24) is a measure of health-specific quality of life that contains eight subscales which measure physical functioning, bodily pain, role limitations due to physical health problems, role limitations due to personal or emotional problems, emotional wellbeing, social functioning, energy/fatigue and general health perceptions. Higher scores are indicative of better functioning. The items comprising the RAND-36 are identical to those of the SF-36,25 both having been developed from longer instruments completed by patients in the Medical Outcomes Study.24,26 In the present study, α coefficients across the subscales ranged from 0.78 to 0.88, with the exception of the social functioning subscale (α=0.55) that was therefore excluded from analyses.
The three-factor eating questionnaire
The three-factor eating questionnaire (TFEQ;27 also known as the Eating Inventory) is a 51-item questionnaire with three subscales that measure cognitive restraint of eating, disinhibition and hunger using a combination of dichotomous questions, four-point Likert scales, and one five-point Likert scale. High cognitive restraint and low disinhibition are predictive of weight loss whereas the opposite is predictive of treatment dropout.28,29 In the present study, α coefficients for the original subscales ranged from 0.83 to 0.84.
Procedures
Interested persons were screened over the telephone to determine their eligibility including having a BMI greater than 25 kg m−2 and less than 50 kg m−2, being between 20 and 60 years of age, and having lost no more than 5% body weight in the 3 months preceding the study. Those who qualified were invited to orientation sessions where the study was explained and informed consent was obtained. Initial eligibility criteria were confirmed at the baseline evaluation. In addition, persons with unstable cardiac conditions, major systemic illnesses, a history of drug abuse or eating disorders, uncontrolled diabetes or hypothyroidism, familial hyperlipidemias, any condition for which weight loss would be contraindicated, or an allergy to or dislike of eggs were excluded.
Subjects completed baseline measures of health-specific quality of life (SF-36) and dietary restraint, disinhibition and hunger (TFEQ). Body composition was measured by DEXA. A randomized block procedure, to ensure equal gender representation across groups, was used to assign participants to the Bagel (B; 40 randomized, 35 completed), Bagel Diet (BD; 41 randomized, 40 completed), Egg (E; 39 randomized, 38 completed) and Egg Diet (ED; 40 randomized, 39 completed) groups.
A registered dietitian instructed participants in each of the four groups. Subjects in the bagel or the egg groups were instructed to eat a bagel or egg breakfast, respectively (Table 2), between the 0700 and 0800 hours for 8 weeks. The B or the E groups were instructed to continue their routine eating and physical activity patterns, whereas those in BD or ED groups were suggested a 1000-calorie energy-deficit low-fat weight loss diet (1200–1800 kcal per day) based on initial BMI. Participants in all groups were required to return for visits 2, 4 and 8 weeks later for measurement of body weight, waist and hip circumference, and body composition determination.
Table 2.
Nutritional composition of the bagel and egg breakfasts
| Item | Amount | Weight (g) |
Energy (kcal) |
Carbohydrate (g) |
Protein (g) |
Fat (g) |
|---|---|---|---|---|---|---|
| Bagel breakfast | ||||||
| Bagel | 1 | 71 | 195 | 37.9 | 7.5 | 1.1 |
| Cream cheese | 29.6 ml | 28 | 99 | 0.8 | 2.1 | 9.9 |
| Yogurta | 3 oz | 85 | 45 | 7.5 | 3.0 | 0.0 |
| Total | 184 | 339 | 46.2 | 12.6 | 11 | |
| Egg breakfast | ||||||
| Eggs (scrambled) |
2 | 122 | 186 | 1.2 | 12.6 | 14 |
| Toast | 2 | 50 | 134 | 24.8 | 4.0 | 0.18 |
| Jellyb | 14.8 ml | 17 | 20 | 5.0 | 0.0 | 0.0 |
| Total | 189 | 340 | 31.0 | 16.6 | 14.18 |
Yogurt: light, nonfat Yoplait.
Jelly: reduced-calorie Kraft fruit spread.
Analyses
Data for participants completing the study were analyzed with SPSS version 14.0 statistical analysis software. Before conducting statistical analyses, data were cleaned and biologically questionable values were verified according to study records. Two mis-entered values were corrected; a third value that could not be verified was excluded from analyses. Means, standard deviations, percentages, and frequencies were used to describe the sample and study constructs. Differences in dropout according to group assignment, gender and race were examined by χ2-analyses. Differences in dropout according to age and BMI were examined by t-tests. Group differences in the demographic characteristics of gender and race were analyzed by χ2-analyses. Group differences in age and percent compliance were analyzed by two-way analyses of variance. Change scores in anthropometric characteristics, restraint, disinhibition, hunger and health-specific quality of life were analyzed with two-way one-tailed analyses of covariance (ANCOVAs), controlling for gender, with diet (diet vs no diet) and food (egg vs bagel) as main effects and diet by food as the interaction term. Significant main effects were followed by one-way one-tailed ANCOVAs. The level of significance was set at P<0.05.
Results
Preliminary analyses
At baseline, the groups did not differ significantly with regard to gender or racial composition, age or percent compliance with the intake of the designated breakfasts (Table 2). Because men may respond better to weight loss interventions, gender was statistically controlled in subsequent analyses. There were no significant differences in dropout according to group assignment, gender, race, age or BMI. However, there was a trend for participants to be more likely to drop out of the bagel, no-diet condition (P<0.10) with five participants dropping out vs only one participant dropping out of each of the remaining three conditions. There was also a trend for younger (P<0.10) participants to be more likely to drop out of the study.
Anthropometric measurements
Two-way ANCOVAs showed significant main effects of food and diet for the variables of BMI, weight and percent weight loss (Ps<0.001). The interaction term was not statistically significant. Main effects of food showed that participants assigned to the egg condition showed greater improvements in BMI, weight and percent weight loss than participants assigned to the bagel condition (Ps<0.05). Follow-up one-way ANCOVAs showed a significant effect of diet within both the egg and the bagel conditions with dieting participants showing greater improvements in BMI, weight and percent weight loss than non-dieting participants (Ps<0.001). Main effects of diet showed that participants in the diet condition showed significantly greater improvements in BMI, weight and percent weight loss (Ps<0.001) than participants in the no-diet condition. Follow-up one-way ANCOVAs showed that within the diet condition, participants assigned to the egg breakfast showed significantly greater improvements in BMI, weight and percent weight loss (Ps<0.05) than participants assigned to the bagel breakfast. However, among participants in the no-diet condition, no significant differences between participants assigned an egg vs bagel breakfast were obtained.
A significant main effect of diet was obtained for both waist circumference (P<0.05) and body fat (P<0.01). A follow-up one-way ANCOVA showed that within the diet condition, participants assigned to the egg breakfast showed a trend toward a greater reduction in waist circumference than participants assigned to the bagel breakfast (P<0.06). No such difference was found for body fat. Within the no-diet condition, there was no significant difference between participants assigned to the egg vs bagel breakfast with regard to reduction in waist circumference. However, within the no-diet condition, there was a trend toward a greater reduction in body fat among participants assigned to the bagel breakfast (P<0.07).
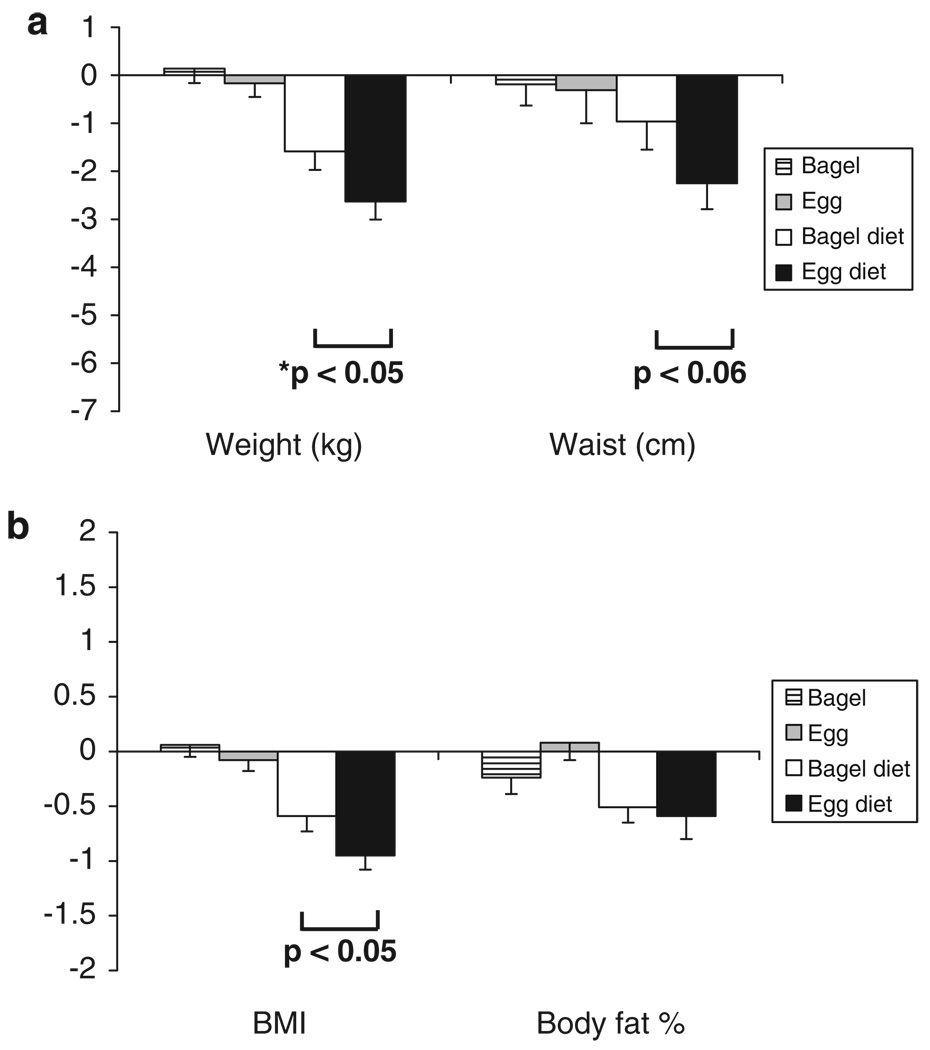
Overall, the ED group showed a 61% greater reduction in BMI (P<0.05), a 65% greater reduction in weight (P<0.05), a 34% greater reduction in waist circumference (P<0.06) and a 16% greater reduction in percent body fat than the BD group (P=not significant, NS; Figures 1a and b). The B and E groups did not differ significantly from one another for these parameters. No significant main effects or interactions were found for changes in total cholesterol, HDL cholesterol, LDL cholesterol or triglycerides (Table 4).
Figure 1.
Changes in body weight, waist circumference (a), body mass index (BMI) and percent body fat (b). Mean±s.d. Changes between the baseline and the final visit at 8 weeks were determined. Analyses of variance showed significant main effects of group for the variables of BMI, weight and percent body fat. Reductions in BMI, body weight, body fat and waist circumference were the greatest for the Egg Diet (ED) group, followed by the Bagel Diet (BD), Egg (E) and Bagel (B) groups. There were no significant differences between the E and B groups. Statistical differences in the ED and BD groups are as indicated.
Table 4.
Between-group comparisons in change in biochemical measurements
| Variable | Bagel | Egg | Bagel diet | Egg diet | F-values |
|---|---|---|---|---|---|
| (mean±s.e.) | (mean±s.e.) | (mean±s.e.) | (mean±s.e.) | ||
| Total cholesterol (mg/100 ml) | −5.4±4.1 | −1.8±4.2 | 1.0±3.7 | −0.3±4.3 | 0.1, 0.9, 0.4 |
| HDL cholesterol (mg/100 ml) | −0.4±1.2 | −0.4±1.1 | −1.8±1.0 | −0.1±1.1 | 0.6, 0.2, 0.6 |
| LDL cholesterol (mg/100 ml) | −4.7±3.6 | −1.4±3.7 | 1.6±2.9 | 0.2±3.2 | 0.1, 1.4, 0.5 |
| Triglycerides (mg/100 ml) | −0.7±6.4 | −4.21±8.1 | 6.0±6.6 | −5.5±9.8 | 0.9, 0.1, 0.3 |
Abbreviations: HDL, high-density lipoprotein; LDL, low-density lipoprotein.
F-values are listed in order of a main effect of food (bagel vs diet), diet (no diet vs diet) and their interaction.
Dietary restraint, disinhibition and hunger
Results from two-way ANCOVAs showed significant main effects of diet for the variables of restraint and hunger (Ps<0.001; Table 3). Participants in the diet condition showed significantly greater improvements in dietary restraint and reductions in hunger than did participants in the no-diet condition. Follow-up one-way ANCOVAs showed no significant differences between participants assigned to the egg vs bagel breakfasts within either of the two diet conditions (Ps=NS). No other main effects or interactions were statistically significant, although there was a trend toward a main effect of diet on disinhibition with greater reductions in disinhibited eating among those in the diet vs no-diet condition (P<0.07).
Table 3.
Between-group comparisons in weight change mechanisms
| Variable | Bagel | Egg | Bagel diet | Egg diet | F |
|---|---|---|---|---|---|
| (mean±s.e.) | (mean±s.e.) | (mean±s.e.) | (mean±s.e.) | ||
| TFEQ | |||||
| Restraint | 0.6±0.6a | 0.8±0.5a | 3.7±0.7b | 5.2±0.8b | 0.1, 33.2***, 0.1 |
| Disinhibition | −0.3±0.4a | −0.6±0.3a,b | −2.0±0.5c | −1.50±0.5b,c | 0.0, 2.2, 0.2 |
| Hunger | −0.03±0.3a | −0.6±0.4a | −2.0±0.5b | −0.8±0.3a | 0.2, 6.4**, 0.1 |
| RAND-36 | |||||
| Physical functioning | −3.0±1.5b | −1.3±1.4b,c | 2.9±1.9a | 1.7±1.6a,c | 1.1, 0.8, 0.0 |
| Role limits—physical | −4.3±3.9 | −7.2±4.4 | −3.1±4.8 | 2.70±3.8 | 1.2, 2.5, 0.2 |
| Role limits—emotional | −7.8±5.3 | 0.9±4.9 | −5.0±4.4 | 4.5±3.7 | 2.7, 1.4, 0.0 |
| Energy/fatigue | −3.1±6.3a | 2.4±2.4a,b | 3.4±3.0b | 10.1±2.8c | 1.3, 3.7*, 0.6 |
| Emotional well-being | −0.1±11.9 | 0.5±2.0 | 1.2±2.1 | 4.9±2.3 | 1.2, 0.5, 0.4 |
| Pain | −0.8±3.9 | 0.7±1.7 | 2.8±2.8 | 6.2±3.0 | 1.0, 3.2*, 0.2 |
| General well-being | −3.5±2.2 | 1.4±2.2 | 2.0±2.3 | 3.9±2.3 | 1.9, 1.4, 0.0 |
Abbreviations: RAND-36, RAND 36-item health survey 1.0; TFEQ, three-factor eating questionnaire.
*P<0.05; **P<0.01; ***P<0.001; means with differing superscripts are significantly different. *F-values are listed in order of a main effect of food (bagel vs diet), diet (no diet vs diet) and their interaction.
Health-specific quality of life
Results of two-way ANCOVAs showed significant main effects of diet on the variables of energy (less fatigue) and pain (Ps<0.05), with participants in the diet condition showing greater improvements on these variables than participants in the no-diet condition. Follow-up ANCOVAs showed no significant differences between participants assigned to the egg vs bagel breakfasts within either the diet or no-diet conditions. Main effects also showed a trend for a main effect of diet on physical role limitations (P<0.06) with participants in the diet condition showing greater improvements than those in the no-diet condition. Main effects also showed trends for main effects of food on emotional role limitations (P<0.06), and general well-being (P<0.09) with participants in the egg condition showing marginally greater improvements in emotional role limitations and general well-being than participants in the bagel condition.
Discussion
Effect on weight loss
Long-term adherence to a reduced energy weight loss diet is difficult, and compliance and consequential weight loss outcomes may be improved by supplementing efforts with strategies to reduce hunger and/or increase satiety. Although anorectic drugs have been used successfully to increase weight loss, a potentially safer alternative would be to use foods with a higher satiety value. Holt et al.22 showed that increasing satiety values of isocaloric breakfast breads were associated with decreased energy intake at a test meal 2 h later. Considering the high satiety value of eggs,21 we previously hypothesized and showed that in overweight and obese subjects, a breakfast consisting of eggs would induce greater satiety and reduce lunchtime energy intake compared to a bagel-breakfast matched for energy density and total energy.23 As an extension of these findings, this study compared the effects of an egg vs bagel breakfast intake for 2 months on weight loss, indices of body size and composition, food cravings and health-specific quality of life. A longer-term study is required to further confirm the utility of this regimen for weight management.
The two breakfasts were designed for palatability and acceptability in addition to nutritional and other considerations. Bagels were selected as a commonly used breakfast food and other accompaniments were included for palatability and for providing a breakfast of sizable energy value. As the satiety value of equicaloric foods is associated with their serving weight,21 we matched the total energy as well as energy density of the two breakfasts. The two breakfasts were left unmatched for other nutrients as the focus of the study was to compare the weight loss effect of an egg breakfast with another popular breakfast, which may not necessarily match for nutrients. Although the effects of various macronutrients and their combinations on satiety and weight loss have been extensively studied, using this information about various nutrients to actually select food items in a diet is often challenging for the lay population. Instead of investigating macronutrient effects, this study determined the role of a specific food in supporting weight loss efforts.
The results clearly demonstrated that when not following a diet, the egg breakfast did not induce weight loss. However, eating an egg breakfast while on a reduced energy diet does enhance weight loss. For a broader application outside a well-structured clinical trial setting, we attempted to simulate a weight loss effort undertaken with little or no medical supervision. Except suggesting a low-energy diet at the baseline, various components of a typical weight loss program in clinical setting such as compliance monitoring, food intake determination, group sessions or dietary counseling were not offered. This lack of intensity is reflected in relatively modest weight loss in 8 weeks in the ED and BD groups. Despite the modest weight loss, the results suggest that much better weight loss is possible if the reduction in energy intake, the most common weight loss approach in the United States,30 is supplemented by an egg breakfast. Scrambled eggs were used in the study. Although the effect of other preparations is unknown, it is unlikely that the results would significantly differ.
Although the mechanism involved is unclear, results are consistent with previous literature documenting the satiating effects of eggs,21 or a high-protein breakfast in comparison to a high-carbohydrate breakfast.31 Although the additional protein content of an egg breakfast may contribute to the effect, its contribution relative to the total daily protein intake should be considered. It is uncertain if the additional protein intake of 4 g from egg breakfast would enhance weight loss. The subjects could not be blinded to the study groups and some placebo effect of egg consumption is potentially possible, but unlikely to remain for 8 weeks.
Effect of on plasma cholesterol
In this study, subjects consumed two eggs five times per week. Given that one egg contains 213 mg cholesterol, this averages out to an additional cholesterol intake of 304 mg per day ((213 × 2 × 5)/7). Assuming that the baseline cholesterol intake is typical for Americans—307 mg per day for men and 225 mg per day for women,32 this represents average total cholesterol intakes of 611 mg per day for the men and 529 mg per day for women. Increased plasma LDL cholesterol concentrations are a risk factor for premature CHD. Several studies in animal models have shown that dietary cholesterol raises LDL cholesterol and produces atherosclerosis. As eggs are a concentrated source of cholesterol, they have also been subjected to intense scrutiny in terms of their ability to influence LDL cholesterol and CHD risk. However, at the end of 2 months, changes in plasma total, HDL and LDL cholesterol and triglycerides did not differ significantly between the groups (Table 4). Our data strongly confirm several recent reports published over the past decade. Several meta-analyses as well as a highly publicized epidemiology study strongly suggest that daily egg consumption does not adversely affect plasma lipoproteins with regard to the risk for CHD or stroke among healthy individuals.33–40
Effect on dietary restraint, disinhibition, hunger and health-specific quality of life
Results showed that the two diet groups reported greater improvements in dietary restraint than did the two no-diet groups, a finding consistent with their greater weight loss. Surprisingly, the two diet groups showed greater reductions in hunger than did the no-diet groups. Although concerns about the potential deleterious effects of dieting on hunger and subsequent overeating have been expressed, controlled studies of monitored dieting have shown improvements in problematic eating attitudes and behaviors.41
Only two differences were found with regard to health-specific quality of life. The diet groups reported greater improvements in energy, or a decrease in fatigue, as well as greater improvements in pain. The greater weight loss achieved by these two groups may be reflected in these modest improvements in health-specific quality of life.
Conclusions
Dietary management of obesity is sound in theory, but difficult to practice and help is required to increase compliance and the consequential enhancement of weight loss. In addition to other treatment considerations such as reduced kcal intake and improved nutrient composition and adequacy, simple changes in familiar daily foods may enhance weight loss. This study uniquely demonstrates how weight loss could be enhanced by a commonly available low-cost food such as eggs, which is favorably exploited for its properties not explained by its energy density.
Acknowledgements
We acknowledge the contribution of our study coordinator, Ms Natalie Currier, in outpatient visits and follow-up of the study participants.
Performance site: Pennington Biomedical Research Center, Baton Rouge, LA 70808, USA.
Funding source: American Egg Board.
Presented at: Experimental Biology 2007.
References
- 1.World Health Organization. Geneva: WHO; World Health Report—Life in the 21st Century: A Vision for All. 1998
- 2.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 3.Allison DB, Fontaine KR, Manson JE, Stevens J, VanItallie TB. Annual deaths attributable to obesity in the United States. JAMA. 1999;282:1530–1538. doi: 10.1001/jama.282.16.1530. [DOI] [PubMed] [Google Scholar]
- 4.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Over-weight, obesity, and mortality from cancer in a prospectively studied cohort of US adults. N Engl J Med. 2003;348:1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 5.Fontaine KR, Redden DT, Wang C, Westfall MS, Allison DB. Years of life lost due to obesity. JAMA. 2003;289:187–193. doi: 10.1001/jama.289.2.187. [DOI] [PubMed] [Google Scholar]
- 6.Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 7.Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med. 2003;138:24–32. doi: 10.7326/0003-4819-138-1-200301070-00008. [DOI] [PubMed] [Google Scholar]
- 8.Thompson D, Edelsberg J, Colditz GA, Bird AP, Oster G. Lifetime health and economic consequences of obesity. Arch Intern Med. 1999;159:2177–2183. doi: 10.1001/archinte.159.18.2177. [DOI] [PubMed] [Google Scholar]
- 9.Kolotkin RL, Meter K, Williams GR. Quality of life and obesity. Obes Rev. 2001;2:219–229. doi: 10.1046/j.1467-789x.2001.00040.x. [DOI] [PubMed] [Google Scholar]
- 10.Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9:788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 11.Drewnowski A. Energy density, palatability, and satiety: implications for weight control. Nutr Rev. 1998;56:347–353. doi: 10.1111/j.1753-4887.1998.tb01677.x. [DOI] [PubMed] [Google Scholar]
- 12.Poppitt SD. Energy density of diets and obesity. Int J Obes. 1995;19:S20–S23. [PubMed] [Google Scholar]
- 13.Rolls BJ, Bell EA. Dietary approaches to the treatment of obesity. Med Clin North Am. 2000;84:401–418. doi: 10.1016/s0025-7125(05)70228-5. [DOI] [PubMed] [Google Scholar]
- 14.Stubbs J, Ferres S, Horgan G. Energy density of foods: effects on energy intake. Crit Rev Food Sci Nutr. 2000;49:481–515. doi: 10.1080/10408690091189248. [DOI] [PubMed] [Google Scholar]
- 15.Rolls BJ, Bell EA, Thorwart ML. Water incorporated into a food but not served with a food decreases energy intake in lean women. Am J Clin Nutr. 1999;70:448–455. doi: 10.1093/ajcn/70.4.448. [DOI] [PubMed] [Google Scholar]
- 16.Rolls BJ, Castellaos VH, Halford JC, Kilara A, Panyam D, Pelkman CL, et al. Volume of food consumed affect satiety in men. Am J Clin Nutr. 1998;67:1170–1177. doi: 10.1093/ajcn/67.6.1170. [DOI] [PubMed] [Google Scholar]
- 17.Burton-Freeman B. Dietary fiber and energy regulation. J Nutr. 2000;130 suppl:272–275. doi: 10.1093/jn/130.2.272S. [DOI] [PubMed] [Google Scholar]
- 18.Howarth NC, Huang TTK, Roberts SB, McCrory MA. Dietary fiber and fat are associated with excess weight in young and middle-aged US adults. J Am Diet Assoc. 2005;105:1365–1372. doi: 10.1016/j.jada.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 19.Howarth NC, Saltzman E, Roberts SB. Dietary fiber and weight regulation. Nutr Rev. 2001;59:129–139. doi: 10.1111/j.1753-4887.2001.tb07001.x. [DOI] [PubMed] [Google Scholar]
- 20.Rolls BJ, Roe LS, Meengs JS. Salad and satiety: energy density and portion size of a first-course salad affect energy intake at lunch. J Am Diet Assoc. 2004;104:1570–1576. doi: 10.1016/j.jada.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 21.Holt SHA, Brand Miller JC, Petocz P, Farmakalidis E. A satiety index of common foods. Eur J Clin Nutr. 1995;49:675–690. [PubMed] [Google Scholar]
- 22.Holt SHA, Brand Miller JC, Stitt PA. The effects of equal-energy portions of different breads on blood glucose levels, feelings of fullness and subsequent energy intake. J Am Diet Assoc. 2001;101:767–773. doi: 10.1016/S0002-8223(01)00192-4. [DOI] [PubMed] [Google Scholar]
- 23.Vander Wal JS, Marth JM, Khosla P, Jen C, Dhurandhar NV. Short-term effect of eggs on satiety in overweight and obese subjects. J Am Coll Nutr. 2005;24:510–515. doi: 10.1080/07315724.2005.10719497. [DOI] [PubMed] [Google Scholar]
- 24.Stewart AL, Sherbourne CD, Hays RD, Wells KB, Nelson EC, Kamberg CJ, et al. Summary and discussion of MOS measures. In: Stewart AL, Ware JE Jr, editors. Measuring Functioning and Well-Being: The Medical Outcome Study Approach. Durham, NC: Duke University Press; 1992. pp. 345–371. [Google Scholar]
- 25.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 26.Hays RD, Shapiro MF. An overview of generic health-related quality of life measures for HIV research. Qual Life Res. 1992;1:91–97. doi: 10.1007/BF00439716. [DOI] [PubMed] [Google Scholar]
- 27.Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29:71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- 28.Laporte DJ, Stunkard AJ. Predicting attrition and adherence to a very low calorie diet: a prospective investigation of the eating inventory. Int J Obes. 1990;14:197–206. [PubMed] [Google Scholar]
- 29.Westenhoefer J, Stunkard AJ, Pudel V. Validation of the flexible and rigid control dimensions of dietary restraint. Int J Eat Disord. 1999;26:53–64. doi: 10.1002/(sici)1098-108x(199907)26:1<53::aid-eat7>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 30.Bish CL, Blank HM, Maynard LM, Serdula MK, Thompson NJ, Khan LK. Health related quality of life and weight loss practices among overweight and obese US adults 2003: behavioral risk factor surveillance system. Med Gen Med. 2007;9:35. [PMC free article] [PubMed] [Google Scholar]
- 31.Teff KL, Young SN, Blundell JE. The effect of protein or carbohydrate breakfasts on subsequent plasma amino acid levels, satiety, and nutrient selection in males. Pharmacol Biochem Behav. 1989;34:829–837. doi: 10.1016/0091-3057(89)90282-7. [DOI] [PubMed] [Google Scholar]
- 32.Wright JD, Wang CY, Kennedy-Stephenson J, Bethene ER. Dietary intake of ten key nutrients for public health, United States: 1999–2000 Advance Data from Vital and Health Statistics. Centers for Disease Control and Prevention. No: 334. 2003. Apr 17, [PubMed] [Google Scholar]
- 33.Clarke RFC, Collins R, Appleby P, Peto R. Dietary lipids and blood cholesterol: quantitative meta-analysis of metabolic ward studies. BMJ. 1997;314:112–117. doi: 10.1136/bmj.314.7074.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Herron KL, Fernandez ML. Are the current dietary guidelines regarding egg consumption appropriate? J Nutr. 2004;134:187–190. doi: 10.1093/jn/134.1.187. [DOI] [PubMed] [Google Scholar]
- 35.Herron KL, Vega-Lopez S, Conde K, Ramjiganesh T, Shachter NS, Fernandez ML. Men classified as hypo- or hyperresponders to dietary cholesterol feeding exhibit differences in lipoprotein metabolism. J Nutr. 2003;133:1036–1042. doi: 10.1093/jn/133.4.1036. [DOI] [PubMed] [Google Scholar]
- 36.Howell WJ, McNamara DJ, Tosca MA, Smith BT, Gaines JA. Plasma lipid and lipoprotein responses to dietary fat and cholesterol: a meta-analysis. Am J Clin Nutr. 1997;65:1747–1764. doi: 10.1093/ajcn/65.6.1747. [DOI] [PubMed] [Google Scholar]
- 37.Hu FB, Stampfer MJ, Rimm EB, Manson J, Ascherio A, Colditz G, et al. A prospective study of egg consumption and risk of cardiovascular disease in men and women. JAMA. 1999;281:1387–1394. doi: 10.1001/jama.281.15.1387. [DOI] [PubMed] [Google Scholar]
- 38.Knopp RH, Retzlaff B, Fish B, Walden C, Wallick S, Anderson M, et al. Effects of insulin resistance and obesity on lipoproteins and sensitivity to egg feeding. Arterioscler Thromb Vasc Biol. 2003;23:1437–1443. doi: 10.1161/01.ATV.0000082461.77557.C7. [DOI] [PubMed] [Google Scholar]
- 39.McNamara DJ. The impact of egg limitations on coronary heart disease risk: do the numbers add up? J Am Coll Nutr. 2000;19:540S–548S. doi: 10.1080/07315724.2000.10718978. [DOI] [PubMed] [Google Scholar]
- 40.McNamara DJ. Eggs and heart disease risk: perpetuating the misperception. Am J Clin Nutr. 2002;75:333–335. doi: 10.1093/ajcn/75.2.333. [DOI] [PubMed] [Google Scholar]
- 41.Presnell K, Stice E, Tristan J. Experimental investigation of the effects of naturalistic dieting on bulimic symptoms: moderating effects of depressive symptoms. Appetite. 2008;50:91–101. doi: 10.1016/j.appet.2007.06.002. [DOI] [PubMed] [Google Scholar]