Abstract
Objective
To compare oxygen supply options for health facilities in the Gambia and develop a decision-making algorithm for choosing oxygen delivery systems in Africa and the rest of the developing world.
Methods
Oxygen cylinders and concentrators were compared in terms of functionality and cost. Interviews with key informants using locally developed and adapted WHO instruments, operational assessments, cost-modelling and cost measurements were undertaken to determine whether oxygen cylinders or concentrators were the better choice. An algorithm and a software tool to guide the choice of oxygen delivery system were constructed.
Findings
In the Gambia, oxygen concentrators have significant advantages compared to cylinders where power is reliable; in other settings, cylinders are preferable as long as transporting them is feasible. Cylinder costs are greatly influenced by leakage, which is common, whereas concentrator costs are affected by the cost of power far more than by capital costs. Only two of 12 facilities in the Gambia were found suitable for concentrators; at the remaining 10 facilities, cylinders were the better option.
Conclusion
Neither concentrators nor cylinders are well suited to every situation, but a simple options assessment can determine which is better in each setting. Nationally this would result in improved supply and lower costs by comparison with conventional cylinders alone, although ensuring a reliable supply would remain a challenge. The decision algorithm and software tool designed for the Gambia could be applied in other developing countries.
Résumé
Objectif
Comparer les options d’approvisionnement en oxygène qui s’offrent aux établissements de soins de Gambie et développer un algorithme de prise de décisions pour guider le choix des systèmes d’approvisionnement en oxygène en Afrique et dans le reste du monde en développement.
Méthodes
Les auteurs ont comparé en termes de fonctionnalité et de coût les bouteilles et les concentrateurs d’oxygène. Ils ont interrogé des informateurs clés en utilisant des instruments d’évaluation OMS mis au point et adaptés localement et réalisé des évaluations opérationnelles, ainsi qu’une modélisation et des mesures des coûts pour déterminer le meilleur choix entre les bouteilles et les concentrateurs d’oxygène. Ils ont élaboré un algorithme et un outil logiciel pour guider la sélection du système d’approvisionnement en oxygène.
Résultats
En Gambie, les concentrateurs d’oxygène présentent des avantages notables par rapport aux bouteilles lorsque l’alimentation électrique est fiable ; dans d’autres contextes, il est préférable de faire appel aux bouteilles dans la mesure où leur transport est praticable. La présence de fuites, phénomène courant, influe fortement sur le coût des bouteilles, tandis que pour les concentrateurs, les coûts énergétiques sont de loin plus importants que les coûts en capital. Sur les 12 établissements gambiens, 2 seulement avaient intérêt d’après l’étude à utiliser des concentrateurs ; pour les 10 autres, les bouteilles constituaient une meilleure option.
Conclusion
Ni les concentrateurs, ni les bouteilles ne conviennent à toutes les situations, mais une évaluation simple des options permet de déterminer pour chaque contexte la meilleure solution. A l’échelle nationale, cette évaluation devrait conduire à une amélioration de l’approvisionnement et à une baisse des coûts par rapport à la situation où l’on utilise uniquement des bouteilles d’oxygène classiques, mais assurer un approvisionnement fiable devrait rester un défi. L’algorithme décisionnel et l’outil logiciel conçus pour la Gambie devraient être applicables dans d’autres pays en développement.
Resumen
Objetivo
Comparar las opciones de suministro de oxígeno para centros de salud en Gambia y desarrollar un algoritmo decisional para elegir los sistemas de suministro de oxígeno en África y en el resto del mundo en desarrollo.
Métodos
Se compararon la funcionalidad y el costo de las bombonas y los concentradores de oxígeno. Se llevaron a cabo entrevistas con informantes clave mediante instrumentos desarrollados localmente o adaptados a partir de otros de la OMS, evaluaciones operacionales, modelizaciones de costos y mediciones de costos a fin de determinar la mejor opción entre las bombonas y los concentradores de oxígeno. Se desarrolló así un algoritmo y un instrumento de software para fundamentar la elección del sistema de suministro de oxígeno.
Resultados
En Gambia, los concentradores de oxígeno presentan ventajas importantes en comparación con las bombonas allí donde el suministro eléctrico es fiable; en caso contrario, la opción preferible son las bombonas, siempre y cuando sea factible transportarlas. El costo de las bombonas depende considerablemente de las fugas, un problema frecuente, mientras que el de los concentradores depende mucho más del costo de la electricidad que de los gastos de infraestructura. Sólo dos de los 12 centros de Gambia analizados reunían las condiciones idóneas para usar concentradores; en los otros diez centros, la mejor opción eran las bombonas.
Conclusión
Ni los concentradores ni las bombonas son soluciones ideales para cualquier situación, pero una simple evaluación de esas dos opciones permite determinar cuál es preferible en cada entorno. A nivel nacional, esa diferenciación se traduciría en mejoras del suministro y menores costos en comparación con el uso exclusivo de las bombonas convencionales, pero seguiría habiendo problemas para garantizar un suministro fiable. El algoritmo decisional y el instrumento de software concebidos para Gambia podrían aplicarse en otros países en desarrollo.
ملخص
الهدف
مقارنة اختيارات إمداد المرافق الصحية بالأكسجين في غامبيا وإعداد خوارزمية لاتخاذ القرار حول اختيار نُظُم توصيل الأكسجين في أفريقيا وبقية البلدان النامية.
الطريقة
قارن الباحثون مواسير (اسطوانات) ومكثفات الأكسجين من حيث أدائها لوظائفها وتكاليفها، فأجروا مقابلات مع المخبرين الرئيسيين باستخدام استمارة أعدتها منظمة الصحة العالمية مع تكييفها لتلائم الموقع المحلي، مع إجراء تقييمات ميدانية وإعداد نماذج للتكاليف وقياسات للتكاليف للتعرف على ما إذا كانت مواسير (اسطوانات) أو كانت مكثفات الأكسجين هي اختيار أفضل. وبنى الباحثون خوارزمية وبرمجيات لتوجيه اختيار نظام توصيل الأكسجين.
الموجودات
في غامبيا تتمتع مكثفات الأكسجين بمنافع هامة مقارنة بالمواسير (الاسطوانات)، وذلك في المواقع التي يمكن الاعتماد فيها على توافر الطاقة، أما في المواقع الأخرى، فتفضل المواسير (الاسطوانات) حينما يكون نقلها ممكناً. وتتأثر تكلفة المواسير (الاسطوانات) إلى حدٍ كبير بالتسرب، وهو أمر شائع الحدوث، فيما تتأثر تكلفة المكثفات بتكاليف الطاقة أكثر مما تتأثر بتكاليف رأس المال. وقد وجد الباحثون أن مرفق اثنين من أصل 12 مرفقاً في غامبيا ملائمان للمكثفات. أما المرافق العشرة المتبقية فإن المواسير (الاسطوانيات) هي اختيار أفضل .
الاستنتاج
لا تناسب المكثفات ولا المواسير (الاسطوانيات) جميع الأوضاع، ولكن تقييماً بسيطاً للاختيارات يمكن أن يحدد أيهما أفضل في كل موقع. وعلى الصعيد الوطني، سيؤدي ذلك إلى تحسين الإمداد وتخفيض التكاليف بالمقارنة مع الاستخدام المعتاد للمواسير (الاسطوانات) لوحدها، وذلك رغم أن ضمان الإمداد الموثوق سيبقى تحدياً. إن خوارزمية اتخاذ القرار والأداة البرمجية المصممة لغامبيا يمكن تطبيقها في بلدان نامية أخرى.
Introduction
Acute respiratory infection, principally pneumonia, remains the leading cause of death in young children worldwide.1–3 Case management of pneumonia is a key component of the WHO Integrated Management of Childhood Illness strategy and is integral to the achievement of the fourth UN Millennium Development Goal: reducing under-5 mortality by two-thirds by 2015.4 WHO guidelines for the management of pneumonia include antibiotic therapy, appropriate use of oxygen and general supportive care. Oxygen is needed to treat hypoxaemia, a life-threatening feature of very severe pneumonia resulting from impaired lung function.
Medical oxygen, which is potentially life-saving, is in limited supply in the developing world, although the extent and nature of the problem are not well documented.5 A situational analysis has shown that in the Gambia most health facilities have inadequate oxygen availability and that the factors that are important for ensuring oxygen supplies differ between facilities.6
Oxygen concentrators have been proposed as an answer to the high cost and logistical problems associated with oxygen cylinders, the traditional method of supply.7 However, there is a risk that the technology might be misapplied, compromising care.8 The suitability of concentrators for the developing world is still in question, and a realistic appraisal of the role of concentrators in different contexts is needed, along with user-friendly guidance to assist decision-making. In this report, we analyse the options available, suggest a decision-making algorithm and present a software tool we have produced to analyse options and costs in a range of different contexts.
Methods
A health needs assessment framework was used to define issues that surround oxygen treatment in the Gambia and the options for improving it.9–11 In this study we evaluated the two supply options, cylinders and concentrators, in terms of their cost, how well they work and their sustainability.
Functionality assessment
We first analysed the functionality of cylinders and concentrators. Data were collected in 2004–2007 and analysed in 2005–2008. We used semi-structured interviews with two instruments: the first was developed by one of the authors (SEH) specifically for a case study of failed oxygen concentrators in the Gambia,6 and the other was adapted and validated by one of the authors (SEH) for a local study of oxygen use8 from a WHO health facility assessment tool. Interviews were undertaken throughout the Gambia with health-care staff, administrators, policy-makers and others with relevant knowledge. Details of the instruments, interviewees and other aspects of methods used are described elsewhere.6,8 In addition, we collated the international operational experience of our multi-disciplinary team of investigators, assessed the operational experience gained in the Gambia so far and reviewed others’ published experience. The findings of the functional assessment were incorporated, along with the cost analyses described below, into a decision algorithm.
Cost modelling
To provide comparative costs in different contexts, we broke down and costed each option by using the ingredients approach and applied a decision-analytic model to frame the alternative components,12,13 taking into account capital and running costs, the scale of consumption and the context. We constructed a decision algorithm to identify the most cost-effective option for a range of circumstances. These results were incorporated into an options analysis tool developed on Microsoft Access software (Microsoft Corporation, Redmond, WA, United States of America), and the tool was applied to data from a previous situational analysis of Gambian health facilities.6 We used costs in 2007 and exchange rates of 22.66 dalasi per United States dollar (US$) and US$ 1.977 per United Kingdom pound on 24 December 2007.14,15
Capital and running costs used in the model are detailed in Table 1. The WHO recommendation of one concentrator to every 10–15 beds (supplying up to four children simultaneously by use of a flow-splitter) was followed, with one backup concentrator added. Costs for five regulator-flowmeter sets per 10–15 beds (for cylinders to supply up to four children at a time plus a backup cylinder) were included. Expected lifespans of 5 years were assumed for concentrators, generators and regulator-flowmeter sets. Where a concentrator would be powered by spare capacity from a facility’s already-operating generator (typically 40 kilovolt-amperes [kVA]) no power cost was included. Where reliable power supplies were of mixed grid and generator origin, the costs were taken as grid-power costs. We rated cylinder leakage at 10% for new well-maintained equipment connected directly to the patient, 50% for old poorly-maintained equipment connected directly to the patient, and 80% for old poorly-maintained equipment connected to a piped delivery system. Oxygen requirements were estimated based on local rates of severe hypoxaemia (oxygen saturation < 90%) among children admitted to hospital (6%)16 and average local durations (3 days) and flow rates (1.5 L/min) of oxygen treatment (unpublished data). We performed sensitivity analyses based on worse-than-expected equipment lifespans, variations in power availability and different levels of cylinder leakage.17,18
Table 1. Detail of capital cost and running cost data used for cost modelling assessment of Gambian health facilities, 2004.
| Category and description | Cost in US$, or power consumption | Notes | ||
|---|---|---|---|---|
| Oxygen concentrator | ||||
| Airsep NewLife Intensity | 1100.00 | 2008 cost direct from manufacturer supplied to Medical Research Council, the Gambia (including shipping) | ||
| 4-way flow-splitter | 175.00 | 2008 cost direct from manufacturer | ||
| Cylinder | ||||
| 6 000 litres | 37.51 | March 2007 cost, Banjul Oxygen | ||
| Delivery | 11.00 per cylinder | 2004 cost to transport to Bansang. Transport to Royal Victoria Teaching Hospital, Banjul, free | ||
| Regulator-flowmeter set | 188.00 | January 2008 cost Oxylitre, United Kingdom | ||
| Hospital piping system | 11 000.00 | 20-bed 6-cylinder bank system based on 2001 costs at Medical Research Council hospital | ||
| Power | ||||
| National grid | 0.40 per kWh | November 2007 cost, NAWEC, the Gambia | ||
| 4-kVA generator | 3000.00 | January 2008 cost, Just Generators, United Kingdom | ||
| Diesel fuela | 1.06 per litre | November 2007 duty-free import price (applicable to government services) |
kVa, kilovolt-ampere; kWh, kilowatt-hour; NAWEC, National Water and Electricity Company; US$, United States dollars. a Fuel consumption of generator: 0.5 litres per 4 kVA output. Power rating of concentrator: 0.4 kW.
To provide directly-measured costing data that could be compared with national modelled data, we undertook a prospective study at the 42-bed Medical Research Council Hospital between 23 January and 4 April 2006. The hospital was supplied mainly with cylinder oxygen through a piped system installed in 2001, with back-up from four concentrators (model DeVilbiss 515, DeVilbiss Healthcare, Somerset, PA, USA). Hospital policy was to give oxygen when oxygen saturation was below 93%, which would be expected to result in higher consumption than if the standard cut-off of < 90% were used. Costs were measured over two consecutive periods: 41 days of supply predominantly by cylinders (period 1) and 45 days of supply predominantly by concentrators (period 2). Costs were taken from payment records. The capital cost of the concentrators was calculated as the proportion of the purchase cost equivalent to the number of hours used divided by the projected 40 000-hour running lifespan (approximately 5 years of continuous use) of an individual unit. The concentrator unit cost was US$ 1763, including shipping; power costs per kilowatt-hour (kWh) were US$ 0.19 from the generator and US$ 0.28 from the grid; oxygen cylinders cost US$ 30.18 per 6000-L cylinder, including delivery; the cylinder piping cost including installation was US$ 16 663. The amount of oxygen consumed was measured by regular recording at the bedside and by the number of cylinders used. The metred running time of the concentrators was also recorded. Costs were represented in US$ based on exchange rates applicable at the time costs were incurred.14,15
Ethical approval for the study was given by the Gambia Government Medical Research Council Joint Ethics Committee (SCC/EC974).
Results
Functionality assessment
The advantages and disadvantages of cylinders and concentrators are shown in Table 2.
Table 2. Comparison of the characteristics of oxygen cylinders and oxygen concentratorsa.
| Characteristics | Cylinders | Concentrators | ||
|---|---|---|---|---|
| Capital cost | High when regulator and flowmeter costs included | High | ||
| Running cost | High, particularly if leakage is significant | Low if power is inexpensive | ||
| High if power is expensive | ||||
| Ease of use | Some training required | Considerable training required | ||
| Reliability | Good | Good on selected models | ||
| Physical robustness | Good | Fair | ||
| Regular maintenance | Needed | Needed | ||
| Technical repairs | Needed (e.g. for regulators, to minimize leakage) | Needed (maintenance staff require specialized training) | ||
| Electricity | Not needed | Needed | ||
| Continuity of oxygen delivery | Liable to run out | Good as long as power is available | ||
| Portability | Poor for large cylinders | Good | ||
| Supply system | Transport needed Ordering needed | Transport not needed | ||
| Ordering not needed |
a Table adapted from the WHO Acute Respiratory Infections Programme oxygen handbook.19
The interview findings have been previously reported.6,8 Cylinders were regarded by most users as relatively simple to operate but hard to move, likely to run out without warning and difficult to resupply. Respondents were generally less familiar with operating oxygen concentrators, although they regarded them as easier to move around. They felt, however, that the need for a continuous power supply and the tendency of concentrators to break down were problematic. Both cylinders and concentrators were regarded as expensive, but cylinders were regarded as especially costly by administrators.
The investigators’ operational experience supported local user observations. Some additional observations were relevant. Effective maintenance and monitoring mechanisms are crucial to success. The Gambia is unlike some countries in that all major health facilities are on or near main roads, so cylinder transport is potentially workable if reliable arrangements can be made. For the sake of usability there should be one main method of supply in each facility, with an alternative means of supply as a backup. While solar power has several advantages, including independence from fossil fuels, the careful daily maintenance required for systems powerful enough to run concentrators make the latter currently impractical for most health facilities in the Gambia and other developing countries.20
An engineering assessment of the piped oxygen system at the Medical Research Council Hospital by two of us (DP and KT) showed leakage of around 70% based on the cylinders used and the oxygen delivered over a 4-day period. Most leakage was from the cylinder heads. The cylinder system at the Royal Victoria Teaching Hospital in Banjul also had significant leakage. Cylinder leakage has been repeatedly observed in the Gambia from both free-standing bedside cylinders and piped systems; there are anecdotal reports that problems are greater with older equipment and piped systems. The extent of cylinder leakage was estimated to be 10–80% depending on the kind of system used (piped or direct from the cylinder), the quality of the equipment and the standard of maintenance.
Global experience in comparing the functionality of concentrators and cylinders is summarized in WHO’s oxygen therapy handbook.19 Table 2 represents a refinement of this experience based on the findings of the present study. Notable differences in the table we used compared to the WHO handbook are that cylinder capital costs approach the high costs of concentrators when regulator-flowmeter costs are included; concentrator running costs are high if power costs are high, and training and maintenance are important for cylinders as well as concentrators.
Cost modelling and decision algorithm
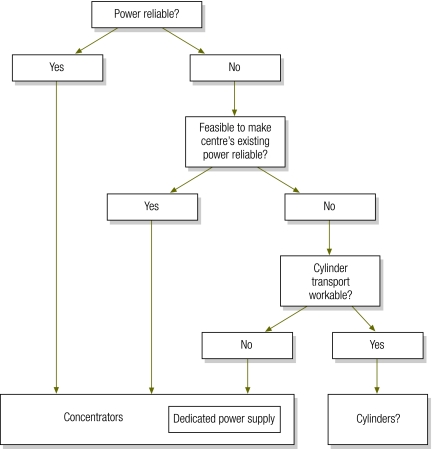
Fig. 1 shows an algorithm for determining the most suitable cost-effective option for the main oxygen supply. Where the power supply is reliable, oxygen concentrators are preferable both in terms of cost and convenience; where creating a reliable power supply is not feasible or cost-effective, the practicality of cylinder transport should be considered. If cylinder transport is workable, then cylinders are preferable. If cylinder delivery is problematic, then a concentrator with a dedicated power supply, such as a small generator, is preferred. If neither option is possible, a reliable oxygen supply cannot be ensured and hypoxaemic patients should be transferred to another facility, if possible.
Fig. 1.
Algorithm for deciding the most suitable main oxygen supply method for health facilities in the Gambia, 2004
Table 3 shows the results of modelling based on 2004 data from health facilities in the Gambia, with costs given for cylinders and for concentrators powered from different sources. With power defined as reliable if available for an average of at least 20 hours daily, two of the 12 facilities were suitable for concentrators, whereas the remaining 10 were better suited to cylinders as the primary source of supply because they had unreliable power supplies and reasonable road access for the delivery of cylinders. The estimated average annual cost of an adequate oxygen supply for all facilities was US$ 152 747 using cylinders, US$ 76 485 using the supply source suggested by the decision algorithm, and US$ 18 742 using concentrators if all facilities had a continuous grid power supply. The costs of running concentrators powered by a small generator compared favourably with the cost of a cylinder supply for all facilities.
Table 3. Decision analysis, estimated oxygen requirements and comparative costs in Gambian health facilities, 2004.
| Health facility | Estimated annual oxygen requirement (million L) | Decision analysis best main supply option | Cost analysis, in US$ |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cost per 1000 L |
Cost per year |
|||||||||
| Concentrators and grid power | Cylinders | Concentrators and large generator (running when existing power not on) | Concentrators and small generator (running when existing power not on) | Best option | Cylinders | 24-hour grid power and concentrators | ||||
| Royal Victoria Teaching Hospital | 2.451 | Concentrators | 1.83 | 31.85 | ND | ND | 4 485 | 78 064 | 4 485 | |
| Basse | 0.216 | Concentrators | 5.32 | 17.74 | ND | ND | 1 149 | 3 832 | 1 149 | |
| Brikama | 1.029 | Cylinders | 1.83 | 16.35 | 15.20 | 2.55 | 16 824 | 16 824 | 1 883 | |
| Bansang | 0.746 | Cylinders | 3.15 | 16.83 | 21.00 | 4.13 | 12 555 | 12 555 | 2 350 | |
| Serekunda | 0.650 | Cylinders | 2.56 | 12.79 | 44.89 | 6.12 | 8 314 | 8 314 | 1 664 | |
| Soma | 0.566 | Cylinders | 3.13 | 16.77 | 45.47 | 6.82 | 9 492 | 9 492 | 1 772 | |
| Essau | 0.472 | Cylinders | 2.86 | 16.57 | 45.17 | 6.76 | 7 821 | 7 821 | 1 350 | |
| AFPRC Hospital | 0.428 | Cylinders | 3.56 | 19.96 | 45.89 | 7.60 | 7 259 | 7 259 | 1 524 | |
| Fajikunda | 0.379 | Cylinders | 3.12 | 16.35 | 45.49 | 7.34 | 4 927 | 4 927 | 1 182 | |
| SJ Bwiam | 0.116 | Cylinders | 6.18 | 17.79 | 48.63 | 13.99 | 2 064 | 2 064 | 717 | |
| Kuntaur | 0.087 | Cylinders | 7.65 | 18.33 | 50.24 | 17.20 | 1 595 | 1 595 | 666 | |
| Total | 76 485 | 152 747 | 18 742 | |||||||
AFPRC, Armed Forces Provisional Ruling Council; ND, not determined (not relevant according to findings from the situational analysis); US$, United States dollars.
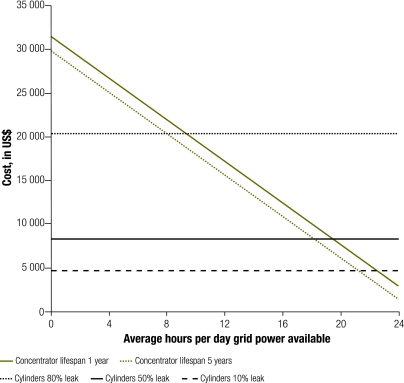
Fig. 2 shows the results of a sensitivity analysis that models the effect of varying lifespans of oxygen concentrators, different levels of cylinder leakage and varying constancy of grid power supply on the cost of oxygen in an average-sized health centre with average oxygen requirements. The amount of cylinder leakage had a large effect on cost, whereas concentrator lifespan had little effect. Furthermore, concentrators were better than cylinders with average leakage in facilities with grid power for more than 18 hours per day (where power gaps are bridged by the facility’s existing generator), and in large facilities with power for more than 12 hours daily (data not shown). The results of the sensitivity analysis for small facilities resembled those obtained for average-sized facilities, the only exception being that early concentrator failure significantly undermined the cost-effectiveness of concentrators because low usage makes capital costs proportionately higher (data not shown). Analysis of the combined use of a concentrator and a small generator showed that for an average-sized facility, the cost advantage compared to cylinders disappeared when concentrator lifespan decreased from 5 years to 1 year (data not shown).
Fig. 2.
Average annual cost of providing oxygen for paediatric patients in an average‑sizeda hospital or major health centre, per daily hours of grid power available,b concentrator lifespan and level of leakage of oxygen cylinders, the Gambia, 2004
kVa, kilovolt-ampere.
a “Average-sized” is defined here as having 15 paediatric beds and an estimated annual oxygen requirement of 0.5 million litres, 1286 patient-years and 5556 concentrator-hours.
b The balance in power requirement was met with a 40-kVA generator (usually present in Gambian facilities).
Costing study
The costs incurred during cylinder and concentrator use are summarized in Table 4. Costs per 1000 litres of oxygen were US$ 4.80 for the cylinder-supplied period and US$ 0.84 for the concentrator-supplied period, compared to US$ 6.56 and US$ 0.86, respectively, for modelled costs in a 42-bed hospital with no cylinder leakage (leakage was fixed before study, see below) and an estimated twice-normal consumption as a result of the Medical Research Council Hospital’s higher treatment cut-offs.16 These costs were broadly similar, and the differences mainly reflected historical differences in item costs, exchange rates and concentrator use in the cylinder-supplied period (Table 4). During the cylinder-supplied period, concentrator backup was required for 2 days (a weekend) because of a delay in cylinder delivery, despite the proximity of the hospital to the supplier (less than 10 km on good roads). Other times, concentrators were used for convenience where piped cylinder supply outlets were not close to the bed. During the concentrator-supplied period, cylinders were used on 1 day because of an oversight. There were no failures of concentrator supply that necessitated the use of cylinders, because the hospital had a reliable power supply sourced 52% of the time from an 850-kVA generator and 48% of the time from the national grid, and there were no concentrator breakdowns. Oxygen usage was twice as high in the concentrator-supplied period because the patients in this period required more oxygen, on average, than in the cylinder-supplied period. The recorded amount of cylinder oxygen delivered to patients at the bedside was similar to the amount measured by cylinder consumption (187 749 L versus 168 000 L, respectively), which indicates successful repair of the cylinder system after the previously mentioned leak was detected.
Table 4. Oxygen delivered and consumed and comparison of costs incurred by delivering oxygen primarily with cylinders (period 1) or concentrators (period 2) at the Medical Research Council Hospital, Fajara, the Gambia, 2004.
| Period 1a | Period 2b | |||
|---|---|---|---|---|
| No. of patients | 20 | 18 | ||
| Oxygen consumed, in L | ||||
| Oxygen delivered from cylinders | 181 896 | 2 880 | ||
| Oxygen delivered from concentrators | 37 575 | 443 746 | ||
| Total | 219 471 | 446 626 | ||
| Concentrator hours | 325 | 1 885 | ||
| Costs, in US$ | ||||
| Concentrator capital costsc | 14.32 | 83.08 | ||
| Concentrator running costsd | 30.31 | 175.84 | ||
| Cylinder piping capital costse | 93.35 | 102.46 | ||
| Cylinder running costsf | 914.94 | 14.49 | ||
| Total | 1052.92 | 375.87 | ||
| Cost per 1000 L | 4.80 | 0.84 | ||
| Adjusted cost per average patient during each period (41 days in Period 1, 45 days in Period 2)g | 74.54 | 13.04 | ||
US$, United States dollars. a In period 1 (41 days) cylinders were the principal source of oxygen, although concentrators were occasionally used. b In period 2 (45 days) concentrators were the principal source of oxygen, although cylinders were occasionally used. c Formula: Running cost = unit cost × (hours used/40 000). Projected lifespan of 40 000 hours running time (approximately 5 years). Unit cost: US$ 1763. d Formula: [Power cost per kilowatt-hour (kWh) from generator × power rating of concentrator × hours spent running concentrator from generator] + [power cost per kWh from grid × power rating of concentrator × hours spent running concentrator from grid]. Power cost from generator: US$ 0.19/kWh; power cost from grid: US$ 0.28/kWh; power rating of concentrators: 0.4 kW; hours of generator versus grid power: Period 1, generator 169 hours, grid 156 hours; Period 2, generator 980 hours, grid 905 hours. e Formula: Piping cost = Piping original cost × (duration study/lifespan of piping). Projected lifespan of piping 20 years. Original cost of piping including installation: US$ 16 633. f Formula: Cylinder running cost = cylinder unit supply cost × (litres used/6000). Cost of one 6000-L cylinder: US$ 30.18. g The average oxygen consumption per patient in each period among the 38 patients in the study was 15 529 L. This average consumption was multiplied by the cost per litre to obtain the adjusted cost per average patient.
Discussion
In this article we analyse options for oxygen provision in Gambian health facilities and propose a decision algorithm to guide the choice between concentrators and cylinders as the main supply source at the facility level. We have developed an options assessment tool that allows detailed comparisons of the costs of currently available options, and have used this to model costs in health facilities throughout the Gambia. We have shown that these costs are consistent with full direct cost measurements in one facility. Concentrators have cost advantages where the power supply is reliable, whereas cylinders currently appear to be the most workable cost-effective choice where power is not reliable and where cylinder transport is workable. Cylinder leakage, a potentially fixable drawback, significantly affects overall costs, whereas premature concentrator failure or other causes of inflated capital costs modestly affect costs in average-sized and large facilities. Data from all 12 government hospitals and major health centres in the Gambia indicated that concentrators were probably the better main supply source for just two of them, the largest hospital being one such centre, whereas cylinders were likely to be better for the rest. We estimated the cost of an improved oxygen supply at all facilities to be one-half the cost of conventional cylinders alone.
Published reports on the benefits of oxygen concentrators are positive.7,20–29 Nevertheless, the limitations of this body of literature should be considered. The most comprehensive work in this area has been led by MB Dobson.7,23,25,26 His careful 1991 report, which modelled costs in three sizes of hospital in Papua New Guinea, predicted a saving of 25%–75% with concentrators compared to cylinders, but did not include transport costs and did not address operational feasibility issues in much detail.25 A seminal 1996 paper on a field trial in Egypt showed that concentrators could succeed on a large scale when introduced with an appropriate programme of technical support and staff training.23 The limitations of this study were its short duration (1 year) and the questionable generalizability of its findings, given Egypt’s atypically good infrastructure. No report of the long-term outcome of this project has been published. The largest-scale introduction of concentrators reported to date, for use in anaesthesia, occurred in Malawi in 1987.29 The report notes that all units “worked according to specification” over 26 months, though it is not clear how much need there was for the comprehensive technical back-up that had been put in place. Dobson reported that in a 10-year audit in Malawi, 90% of concentrators were “still in use”.7 Four publications reported experiences, all essentially positive, of portable concentrator use for periods ranging from 3 to 6 years, although on a small scale.21,22,27,30 All but one of these studies were confined to a single facility, the exception being a recent report from Malawi in which one concentrator was supplied to each of five district hospitals.30 We found only one report of a single large oxygen concentrator and piping system supplying an entire hospital. The system, in a Ghanaian teaching hospital, incorporated an oxygen reservoir and backup cylinders, and broke down only twice in 4 years.31 We know of only one report of concentrator failure on a significant scale (a donation of over 20 second-hand units electrically incompatible with the local power supply), but it is likely that publication bias has prevented other negative findings from coming to light.8 On the basis of this literature it would be unwise to assume that concentrators will do well in every situation. Although few studies have identified or quantified the problem of cylinder leakage in the developing world,32 the experience in this study, borne out by what we have observed in other settings, suggests that this problem should not be ignored. The extent of this problem in different settings and with different equipment combinations should be the focus of future studies.
This study has not dealt with the important issue of the efficient use of oxygen, which will affect service costs regardless of the supply method used. Training and monitoring are needed to ensure that all who need oxygen receive it, and that it is not wasted on those who do not. Pulse oximetry is the best available means of detecting hypoxaemia, and the more widespread use of this diagnostic technique is important to assist efficient oxygen usage.33 The costs associated with initiation, training and monitoring, which are important components of any oxygen delivery programme, have not been included in this analysis. Recent work in Papua New Guinea showed that these costs amounted to an additional sum representing approximately 50% of start-up costs.34 The costs for high-level engineering maintenance of either supply source have not been included, as is pragmatically consistent with a context where repairs tend to be done inexpensively with locally-available expertise, or not at all.8
No matter what oxygen delivery system is implemented, in a resource-limited setting like the Gambia it will be vulnerable to breakdown and interruption of supply. Making an appropriate choice between cylinders and concentrators is important but does not, on its own, ensure a sustainable supply. To succeed, a programme must have the support of key decision-makers, fit well with local health policy and have a secure funding mechanism. Important factors such as the reliability of the power supply and cylinder transport can fluctuate markedly over time, so reliable operational arrangements must be made for backup supplies, effective monitoring and coping with situational changes. The vulnerability of available methods of supply underlines the potential, as well as the need, for robust new technology to transform the field. In the Gambian context as in many others, the financial sustainability of both sources of oxygen is subject to fluctuations in the cost of energy, chiefly of fossil fuels, which are necessary for power production both for the national grid and for generators. The development of reliable power sources that are not dependent on fossil fuel would be a significant advance. Although refrigerators have been successfully solar-powered in developing countries, the output required for concentrators is of a much higher order and the technology is not sufficiently robust for this at present.
A recent study in Papua New Guinea showed a 35% reduction in inpatient mortality from pneumonia after the introduction of reliable oxygen supplies used appropriately.34 This is the only such measurement of impact available. Although we do not know if these findings would apply in the Gambian setting, it is informative to consider the benefit and cost that would result if it did. According to local health centre data, in 2004 only 79 pneumonia deaths were recorded, a likely underestimate resulting from misclassification and incomplete recording. Some of the patients probably received oxygen, although even in centres where oxygen supplies were reliable, pulse oximetry was rarely available to confirm the need for treatment. If we assume that the number of deaths not recorded offsets the number of deaths among patients who died despite having received oxygen, a 35% reduction in mortality would save 28 lives at a cost of US$ 1800 per life saved, or US$ 54 per disability-adjusted life-year (DALY) averted. This is less than the cost of other interventions intended to prevent deaths from pneumonia, such as administering the conjugate pneumococcal vaccine (US$ 100 per DALY averted).35,36 The annual cost of saving these lives was estimated to be approximately US$ 76 000 for all health facilities combined, only 50% more than the amount spent on oxygen at the Royal Victoria Teaching Hospital alone in 2004.6
Having a reliable oxygen supply is an important goal for health facilities where cases of severe pneumonia are managed. Neither concentrators nor cylinders are well suited to every situation, and a simple options assessment can determine which is the preferable primary supply source in each setting. Options assessment is likely to lead to improvements in oxygen supply and reductions in costs compared with the costs associated with conventional cylinders. To facilitate this exercise we have produced a computer-based tool based on the present study (available from corresponding author). The challenge of then sustaining the supply should not be underestimated, and much work remains to be done to fully meet this challenge. Nevertheless, it is precisely this type of health service development that will be needed to achieve sustained reductions in child mortality worldwide. ■
Footnotes
Competing interests: None declared.
References
- 1.Revised global burden of disease (GBD) 2002 estimates Geneva: World Health Organization; 2005. Available from: http://www.who.int/healthinfo/global_burden_disease/estimates_regional_2002_revised/en/ [accessed on 21 July 2009].
- 2.Black RE, Morris SS, Bryce J. Child survival series: where and why are 10 million children dying every year? Lancet. 2003;361:2226–34. doi: 10.1016/S0140-6736(03)13779-8. [DOI] [PubMed] [Google Scholar]
- 3.Jaffar S, Leach A, Greenwood A. Changes in the pattern of infant and childhood mortality in Upper River Division, The Gambia, from 1989 to 1993. Trop Med Int Health. 1997;2:28–37. doi: 10.1046/j.1365-3156.1997.d01-131.x. [DOI] [PubMed] [Google Scholar]
- 4.Management of the child with serious infection or severe malnutrition Geneva: World Health Organization; 2000 (WHO/FCH/CAH/00.1).
- 5.Report of WHO informal consultation on clinical use of oxygen Geneva: World Health Organization; 2003. Available from: http://www.who.int/surgery/collaborations/Oxygen_Meeting_Report_Geneva_2003.pdf [accessed on 21 July 2009].
- 6.Hill SE, Njie O, Sanneh M, Jallow M, Peel D, Njie M, et al. Oxygen for treatment of severe pneumonia in The Gambia, West Africa: a situational analysis. Int J Tuberc Lung Dis. 2009;13:587–93. [PubMed] [Google Scholar]
- 7.Dobson MB. Oxygen concentrators and cylinders. Int J Tuberc Lung Dis. 2001;5:520–3. [PubMed] [Google Scholar]
- 8.Howie SR, Hill SE, Peel D, Sanneh M, Njie M, Hill PC, et al. Beyond good intentions: lessons on equipment donation from an African hospital. Bull World Health Organ. 2008;86:52–6. doi: 10.2471/BLT.07.042994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wright J. Health needs assessment in practice London: BMJ Books; 1998. [Google Scholar]
- 10.Stevens A, Raftery J. Health care needs assessment London: Radcliffe Medical Press; 1997. [Google Scholar]
- 11.Coster G. Health needs assessment for New Zealand [background paper and literature review]. Wellington: Ministry of Health; 2000. [Google Scholar]
- 12.McPake B, Kumaranayake L, Normand C. Health economics: an international perspective London: Routledge; 2002. [Google Scholar]
- 13.Consensus Conference on Guidelines on Economic Modelling in Health Technology Assessment. Decision analytic modelling in the economic evaluation of health technologies. A consensus statement. Pharmacoeconomics. 2000;17:443–4. doi: 10.2165/00019053-200017050-00003. [DOI] [PubMed] [Google Scholar]
- 14.Central Bank of The Gambia. Official exchange rates for valuation purposes Available from: http://www.cbg.gm/archives/previous-rates.html [accessed on 4 February 2008].
- 15.xe.com. Current and historical rate tables Available from: http://www.xe.com/ict/ [accessed on 15 February 2008].
- 16.Junge S, Palmer A, Greenwood BM, Kim Mulholland E, Weber MW. The spectrum of hypoxaemia in children admitted to hospital in The Gambia, West Africa. Trop Med Int Health. 2006;11:367–72. doi: 10.1111/j.1365-3156.2006.01570.x. [DOI] [PubMed] [Google Scholar]
- 17.American Hospital Association. Estimated useful lives of depreciable hospital assets Chicago, IL: American Hospital Publishing; 1998. [Google Scholar]
- 18.Emergency Care Research Institute. Oxygen concentrators Plymouth Meeting, PA: ECRI, 2004. [Google Scholar]
- 19.Oxygen therapy for acute respiratory infections in young children in developing countries Geneva: World Health Organization; 1993 (ARI/93.28). Available from: http://www.who.int/child-adolescent-health/New_Publications/CH.../WHO_ARI_93.28.html [accessed on 29 July 2009].
- 20.Schneider G. Oxygen supply in rural Africa: a personal experience. Int J Tuberc Lung Dis. 2001;5:524–6. [PubMed] [Google Scholar]
- 21.Shrestha BM, Singh BB, Gautam MP, Chand MB. The oxygen concentrator is a suitable alternative to oxygen cylinders in Nepal. Can J Anaesth. 2002;49:8–12. doi: 10.1007/BF03020412. [DOI] [PubMed] [Google Scholar]
- 22.Mokuolu OA, Ajayi OA. Use of an oxygen concentrator in a Nigerian neonatal unit: economic implications and reliability. Ann Trop Paediatr. 2002;22:209–12. doi: 10.1179/027249302125001499. [DOI] [PubMed] [Google Scholar]
- 23.Dobson M, Peel D, Khallaf N. Field trial of oxygen concentrators in upper Egypt. Lancet. 1996;347:1597–9. doi: 10.1016/S0140-6736(96)91080-6. [DOI] [PubMed] [Google Scholar]
- 24.Perrelet A, Zellweger JP, Talla I, Ndiaye Y, Gautier E, Gehri M. The oxygen concentrator: an appropriate technology for treating hypoxaemic children in developing countries. Int J Tuberc Lung Dis. 2004;8:1138–41. [PubMed] [Google Scholar]
- 25.Dobson MB. Oxygen concentrators offer cost savings for developing countries. Anaesthesia. 1991;46:217–9. doi: 10.1111/j.1365-2044.1991.tb09413.x. [DOI] [PubMed] [Google Scholar]
- 26.Dobson MB. Oxygen concentrators for the smaller hospital — a review. Trop Doct. 1992;22:56–8. doi: 10.1177/004947559202200204. [DOI] [PubMed] [Google Scholar]
- 27.Litch JA, Bishop RA. Oxygen concentrators for the delivery of supplemental oxygen in remote high-altitude areas. Wilderness Environ Med. 2000;11:189–91. doi: 10.1580/1080-6032(2000)011[0189:ocftdo]2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 28.Wood PB. Oxygen concentrator in a remote hospital in Zaire. Trop Doct. 1985;15:26–7. doi: 10.1177/004947558501500113. [DOI] [PubMed] [Google Scholar]
- 29.Pedersen J, Nyrop M. Anaesthetic equipment for a developing country. Br J Anaesth. 1991;66:264–70. doi: 10.1093/bja/66.2.264. [DOI] [PubMed] [Google Scholar]
- 30.Enarson P, La Vincente S, Gie R, Maganga E, Chokani C. Implementation of an oxygen concentrator system in district hospital paediatric wards throughout Malawi. Bull World Health Organ. 2008;86:344–8. doi: 10.2471/BLT.07.048017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oduro KA. Trends in the supply of oxygen in hospital — oxygen concentrators — Korle Bu experience. West Afr J Med. 1992;11:244–6. [PubMed] [Google Scholar]
- 32.Singh V, Kothari K, Khandelwal R. Adequacy assessment of oxygen therapy. J Assoc Physicians India. 2000;48:701–3. [PubMed] [Google Scholar]
- 33.Weber MW, Mulholland EK. Pulse oximetry in developing countries. Lancet. 1998;351:1589. doi: 10.1016/S0140-6736(05)61160-9. [DOI] [PubMed] [Google Scholar]
- 34.Duke T, Wandi F, Jonathon M, Matai S, Kaupa M, Saavu M, et al. Impact of improved oxygen systems on child deaths from pneumonia: a multi-hospital effectiveness study in Papua New Guinea. Lancet. 2008;372:1328–33. doi: 10.1016/S0140-6736(08)61164-2. [DOI] [PubMed] [Google Scholar]
- 35.Disability adjusted life years (DALY) Geneva: World Health Organization. Available from: http://www.who.int/healthinfo/boddaly/en/ [accessed on 17 May 2008].
- 36.Sinha A, Levine O, Knoll M, Muhib F, Lieu T. Cost-effectiveness of pneumococcal conjugate vaccination in the prevention of child mortality: an international economic analysis. Lancet. 2007;369:389–96. doi: 10.1016/S0140-6736(07)60195-0. [DOI] [PubMed] [Google Scholar]