Abstract
Background
Despite recent advances in cancer survivorship knowledge and care, most medical schools lack a comprehensive survivorship curriculum, potentially leaving students ill-prepared for caring of survivors.
Methods
A total of 211 students and 22 oncology fellows in three institutions completed a questionnaire assessing knowledge and experience in survivorship care.
Results
Medical students and oncology fellows lack knowledge in key survivorship issues. Students were exposed to cancer survivors frequently in medical school but only half received instruction or practiced critical components of survivorship care.
Conclusions
Improvement of both undergraduate and postgraduate training in survivorship care is urgently warranted.
Introduction
Cancer survival rates have increased dramatically in the last two decades due to improved therapies, earlier detection, more effective maintenance care, and more attention to secondary prevention. For instance, while 5-year relative survival of childhood cancers was less than 50 % in the 1970s, by 2000 the survival rate had improved to 65%i. As of 2003, there were 10.5 million cancer survivors in the United States—more than 3.5% of the population--according to the Office of Cancer Survivorship at the National Cancer Instituteii. Many of these survivors will experience chronic effects of their illness and treatment on their general health statusiii and psychosocial well-beingiv,v. Consequently, they need a survivorship-directed medical historyvi and a team approachvii for their follow-up care.
Undergraduate medical education curricula, however, are only beginning to incorporate lessons on the long-term consequences of cancer treatments. Essential components for survivorship training of future health care providers have been suggestedviii including pain management, prevention of secondary cancers, and long-term consequences of illness and treatment. A recent report from the Institute of Medicine (IOM)7 on cancer survivorship identified only a few institutions where cancer survivorship issues were incorporated into health profession training.
Three institutions, the University of California, Los Angeles (UCLA), the University of California, San Francisco (UCSF), and Drew University of Medicine and Science, are collaborating on a Cancer as a Chronic Disease curriculum spanning the first three years of medical school. Through a Delphi process, a consensus panel of faculty experts developed a comprehensive list of curricular objectives in the attitudinal, knowledge and skill domains, which have been published in the aforementioned IOM report and elsewhere8 and are listed in Table 1 and Table 2. A growing set of new teaching “products” related to cancer survivorship issues are being developed and implemented by the three schools, ranging from a problem based learning (PBL) case of a breast cancer survivor to a self-study module on prostate cancer. All are available onlineix.
Table 1.
Knowledge objectives of the “Cancer as a Chronic Disease Curriculum,” associated number of questions in knowledge test, and performance by senior medical students and oncology fellows.
| Competencies | Number of questions included |
Number of questions answered correctly by students (mean ± SD) |
Number of questions answered correctly by fellows (mean ± SD) |
|---|---|---|---|
| Competency 1 | |||
| Understands that all cancer survivors are at increased risk for other cancers as well as recurrence of the original cancer, and need to avoid tobacco, eat right, and use sunscreen. |
4 | 2.5 ± 1.0 | 2.9 ± 1.2 |
| Competency 2 | |||
| Understands basic mechanisms of genetic contribution to risk of cancer | 5 | 3.5 ± 2.1 | 4.0 ± 1.1 |
| Competency 3 | |||
| Understands common uses of the terms “cure”, “disease free survival”, and “cancer survivor” | 2 | 1.4 ± 0.7 | 1.5 ± 0.7 |
| Competency 4 | |||
| Understands differences in cancer survivorship by gender, ethnicity and socio-economic status | 3 | 1.8 ± 1.0 | 2.1 ± 1.1 |
| Competency 5 | |||
| Understands the variety of social consequences of cancer on su rvivors, including difficulty getting employment and insurance, stigma, and the impact on the family and friendships |
3 | 1.5 ± 0.7 | 1.9 ± 0.6* |
| Competency 6 | |||
| Knows the essential elements to obtain about cancer history, how to get information the patient can’t provide, and how to interpret the health implications of this history. |
3 | 1.5 ± 0.9 | 2.2 ± 1.0** |
| Competency 7 | |||
| Understands consequences of cancer treatment for different developmental stages, including impact on growth, osteoporosis, learning, sexual function and fertility |
5 | 1.6 ± 1.1 | 2.3 ± 1.0** |
|
| |||
| Total | 25 | 14.0 ± 3.7 | 16.8 ± 4.2* |
p < .05
p < .01
p < .01
Table 2.
Attitudinal and skills objectives of the of the “Cancer as a Chronic Disease Curriculum.”
| Attitudinal objectives |
| 1. Being comfortable prescribing medications of pain control, including opioids |
| 2. Being comfortable asking new patients routinely about previous cancers |
| 3. Willing to ask oncologists for consultation when appropriate |
| 4. Considering general preventative issues as well as those related to cancer survivorship in cancer survivors |
| Skills objectives |
| 1. Using key screening guidelines to identify people at higher risk for cancer |
| 2. Providing appropriate and individualized recommendations for secondary prevention |
| 3. Tailoring pain medication and other interventions for pain |
| 4. Explaining and helping patients make decisions about advanced healthcare directives, living will |
| 5. Giving bad news about second malignancies or relapse |
| 6. Partnering with patients in decision making |
| 7. Working as primary care provider with a specialty team for continuity of care |
| 8. Providing current cancer inform ation for survivors at the appropriate reading level and language |
Lacking an instrument to measure the efficacy of the new curriculum, a team of content experts drafted outcome measures based on previous work on cancer preventionx. They developed a knowledge testxi that included 25 questions, each of which addressed one of the seven knowledge objectives of the curriculum. Additional questions assessed students’ level of experience with cancer survivors and how competent they felt in providing care.
The present study was conducted as a needs assessment prior to the implementation of the new curriculum and addressed two main questions: (1) What do senior medical students and fellows in oncology training programs know about cancer survivorship? (2) How much exposure and training do medical students receive, and how competent do they feel in caring for cancer survivors? In addition, the authors explored the reliability (internal consistency) and discriminant validity of the knowledge test.
Materials and Methods
We surveyed early fourth-year medical students who had not experienced the Cancer as Chronic Disease curriculum in 2005. The survey instrument consisted of two parts, a knowledge assessment and an experience survey. Students were invited to complete the survey during class time on a voluntary and anonymous basis. Lunch was offered as an incentive. The Institutional Review Boards at UCLA, UCSF and Drew University approved the study.
The knowledge portion of the survey consisted of 25 multiple-choice questions each addressing one of seven cancer survivorship knowledge competencies (Table 1) defined by a panel of experts7. Each competency was addressed by two to five questions. Students were instructed to choose an answer option of “I don’t know” when they had no basis for making an educated guess. Correct answers were scored as +1, incorrect answers as −1, and “I don’t know” as 0. Thus, scores could range from −25 to +25 with negative scores indicating a preponderance of misconceptions. Both total score and a percent correct were calculated.
To determine the discriminant validity of the knowledge assessment instrument, we compared students’ scores to those of twenty-two oncology fellows in medicine, surgery, and pediatrics, three at UCSF and nineteen at UCLA.
The experience survey asked medical students to self-report their exposure to patients with different types of cancer. Furthermore, they rated their self-perceived competence in eight skill areas (listed in Table 2) using a 5-point Likert scale ranging from “very unskilled” to “very skilled”.
They also estimated how often they had observed, received direct instruction in, and practiced the following activities with patients:
Taking a comprehensive cancer history
Counseling on consequences of cancer treatments
Counseling on psychosocial concerns related to cancer
Giving information on secondary prevention of cancer
Working with interdisciplinary teams for continuity of care
All statistical analyses were carried out with SPSS version 14 (SPPS, Inc., Chicago, IL).
Results
Knowledge Test
Of the 238 senior students present in class on the day the survey was distributed, a total of 211 participated in the study—127 at UCLA, 61 at UCSF and 23 at Drew. Response rates were 88.2%, 87.1% and 95.8%. The internal consistency of the knowledge test was modest but acceptable for program evaluation (Chronbach’s alpha = 0.67).
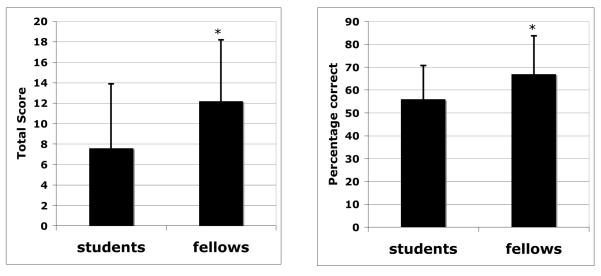
Senior medical students answered on average 56% of the questions correctly, compared to a mean score of 67% for fellows (see Figure 1). Both groups performed particularly poorly in Competency 7 pertaining to long-term treatment consequences. On average, students answered only 1.6 questions (out of 5) correctly on this topic and fellows, only 2.3. In fact, students obtained a negative score, suggesting that they not only lack knowledge, but also may have misconceptions. Also, 42% of the students and 31% of fellows demonstrated no or incorrect knowledge (as indicated by zero or a negative score) about basic survivorship terminology, such as “cure” and “long-term remission” (Competency 3). Furthermore, 37% of the students lacked knowledge on the essential elements of a comprehensive cancer history (Competency 6) compared to 9% of the fellows.
Figure 1.
Average total score and percentage correct in knowledge on survivorship issues for senior medical students and fellows. Asterisk denotes a significant difference between fellows and students at p<.001. Bars indicate standard deviations.
To determine the discriminant validity of the knowledge test, we contrasted performance by students against oncology fellows using a t-test for independent samples. Although there were no differences in variance between groups, we confirmed the analysis using the non-parametric Mann-Whitney test to account for the large difference in sample size (211 vs. 22). As depicted in Figure 1, both approaches indicated that fellows had higher percentage scores and total scores (p<.001).
Experience Survey
Most students reported having seen survivors of breast (90%), colorectal (85%), prostate (82%) and gynecologic cancers (93%). In contrast, less than half (48%) had encountered a survivor of leukemia or other childhood cancers.
By the end of the third year of medical school, most students had observed others caring for survivors. As shown in Table 3, about half of the students, however, reported that they had never received direct instruction on these topics (median: 53%) or practiced these skills (median: 46%) , with the exception of taking a cancer history. Most students (79%) were given the opportunity to take a patient’s cancer history at least once.
Table 3.
Percentage of students who reported never having observed, received instruction in, or practiced caring for cancer survivors.
| Never observed someone else |
Never received direct instruction |
Never practiced | |
|---|---|---|---|
| Asking cancer survivors about cancer history |
13% | 40% | 21% |
| Helping cancer survivors deal with treatment consequences |
25% | 53% | 46% |
| Counseling cancer survivors with psychosocial concerns |
37% | 56% | 51% |
| Providing information on secondary prevention to cancer survivors |
28% | 49% | 44% |
| Being involved in interdisciplinary team to provide continuity of care |
29% | 53% | 50% |
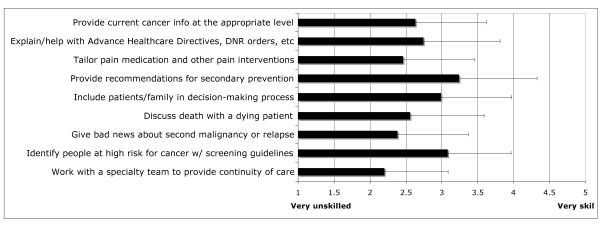
Using a Likert rating scale, students reported overall low competence levels in caring for survivors (Figure 2). Students felt the least competent in working with a specialty team for continuity of care, giving bad news about a malignancy, and tailoring pain medication.
Figure 2.
Senior students’ self-reported level of competence in caring for cancer survivors. Bars indicate standard deviations.
Discussion
In this study, we introduced a new instrument designed for the evaluation of a Cancer As Chronic Disease curriculum and determined its psychometric properties. A panel of experts determined the crucial skills and knowledge needed for survivorship care and subsequently drafted questions related to one of seven competency domains, resulting into an instrument with inherent content validity. In addition, we found evidence for its discriminant validity. Specifically, oncology fellows, who presumably had better knowledge of cancer survivorship, outperformed medical students albeit at an unsatisfactory level. The internal consistency of our instrument was modest (0.67) but adequate for program evaluation.
Senior medical students in three institutions demonstrated limited knowledge about cancer as a chronic disease. On average, students answered about half of the questions correctly while oncology fellows performed only slightly better. In fact, we found a negative score for Competency 7 suggesting that students may have misconceptions, and not just lack of knowledge, about the consequences of cancer treatment on growth, osteoporosis, learning, sexual function, and fertility. Furthermore, students were exposed to cancer survivors frequently in medical school (with the exception of childhood cancer survivors). Nonetheless, about half of the student never received direct instruction or practiced critical components of survivorship care. In addition, and perhaps consequently, students reported low confidence in all cancer survivorship-related patient care activities, such as giving bad news, tailoring pain medication, and working with a specialty team. The latter is particularly disconcerting given the multidisciplinary nature of survivorship care.
Our study has several limitations. First, a relatively low number of oncology fellows participated (compared to the number of medical students). Thus, they may not have represented fellows nationally. Furthermore, our study relied on students’ self-reported experience and competence in survivorship care. Previous studies (e.g.,xii ) have shown that self-reported competence may lack validity. Finally, the level of reliability of our knowledge test precludes its use for assessment of individual students. Future studies involving larger samples could conduct item-item correlations and Exploratory Factor Analysis to identify items that do not fit and may lower the internal consistency. These items could be replaced or removed all together to improve the reliability of the knowledge test.
Nonetheless, our assessment instrument could be used to evaluate educational interventions designed to improve knowledge of long-term effects of cancer or to conduct a needs assessment as described in this study. Our short assessment tool could function as a benchmark against which subsequent curricular innovations can be evaluated. In this survey, senior students who had not been exposed to a survivorship curriculum, had limited knowledge about cancer as a chronic disease, experienced inadequate training, and reported low confidence levels in related clinical skills, underscoring the need for a dedicated survivorship curriculum. Since then, the three participating institutions have been implementing a comprehensive survivorship curriculum using the survey instrument to monitor its effect. Evidence was recently presented that the new curriculum improved knowledge and self-rated competency.xiii
We also found that oncology fellows showed a surprising lack of knowledge in this domain. As Ferrel and Winn8 pointed out, improvement of both undergraduate and postgraduate training in survivorship care is urgently warranted. Additional efforts are needed to ensure that knowledge and experience gained during undergraduate training transfer into subsequent phases of the educational continuum. A thorough understanding of the special needs of cancer survivors, including psychosocial functioning and long-term effects of treatment, is of paramount concern for both primary care and specialty physicians who will be providing quality care for this special populationxiv.
Acknowledgments
This research study has been made possible by a grant from the National Cancer Institute, R25 CA096075, 2002-2007, (PI: LuAnn Wilkerson).
Footnotes
This study was presented in part during the annual meeting of the American Association of Cancer Education, San Diego, October, 12-14.
References
- i.American Cancer Society . Cancer facts and figures 2006. American Cancer Society; Atlanta, GA: http://www.cancer.org. [Google Scholar]
- ii.National Cancer Institute Cancer Survivorship Research Website. http://dccps.nci.nih.gov/ocs.
- iii.Hudson MM, Mertens AC, Yasui Y, Hobbie W, Chen H, Gurney JG, Yeazel M, Recklitis CJ, Marina N, Robison LR, Oeffinger KC. Health status of adult long-term survivors of childhood cancer. A report from the childhood cancer survivor study. JAME. 2003;290:1583–1592. doi: 10.1001/jama.290.12.1583. [DOI] [PubMed] [Google Scholar]
- iv.Langeveld NE, Grootenhuis MA, Voute PA, de Haan RJ. Posttraumatic stress symptoms in adult survivors of childhood cancer. Pediatr Blood Cancer. 2004;42:604–610. doi: 10.1002/pbc.20024. [DOI] [PubMed] [Google Scholar]
- v.Zebrack BJ, Zevon MA, Turk N, Nagarajan R, Whitton J, Robison LL, Zelter LK. Psychological distress in long-term survivors of solid tumors diagnosed in childhood: A report from the childhood cancer survivor study. Pediatr Blood Cancer. 2006 Jun 5; doi: 10.1002/pbc.20914. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- vi.Ganz PA. Monitoring the physical health of cancer survivors: A survivorship-focused medical history. J Clin Oncol. 2006;24:5105–5111. doi: 10.1200/JCO.2006.06.0541. [DOI] [PubMed] [Google Scholar]
- vii.Hewitt M, Greenfield S, Stovall E. From Cancer Patient to Cancer Survivor: Lost in Transition. Institute of Medicine. National Academies Press; Washington, DC: 2006. [Google Scholar]
- viii.Ferrell BR, Winn R. Medical and nursing education and training opportunities to improve survivorship care. J Clin Oncol. 2006;24:5142–5148. doi: 10.1200/JCO.2006.06.0970. [DOI] [PubMed] [Google Scholar]
- ix.David Geffen School of Medicine, UCLA Cancer Education Projects. Online at: http://apps.medsch.ucla.edu/cancer/materials.htm.
- x.Wilkerson L, Lee M, Hodgson C. Evaluating curricular effects on medical students’ knowledge and self-perceived skills in cancer prevention. Acad Med. 2002;77:S51–S53. doi: 10.1097/00001888-200210001-00017. [DOI] [PubMed] [Google Scholar]
- xi.Wilkerson L, Go VL, Stuber M, Uijtdehaage S. Developing instruments to measure knowledge and experience related to cancer survivorship. J Cancer Educ. 2005;3(supplement):16. [Google Scholar]
- xii.Albanese M, Dottl S, Mejicano G, Zakowski L, Seibert C, Van Eyck S, Prucha C. Distorded perceptions of competence and incompetence are more than regression effects. Adv in Health Sci Edu. 2006;11:267–278. doi: 10.1007/s10459-005-2400-7. [DOI] [PubMed] [Google Scholar]
- xiii.Uijtdehaage S, Hauer K, Rajagopalan S, Wilkerson L. Improving knowledge and experience with cancer survivors: effects of a dedicated curriculum. J Cancer Educ. 2007;4(supplement):38. [Google Scholar]
- xiv.Rowland JH, Hewitt M, Ganz PA. Cancer survivorship: a new challenge in delivering quality cancer care. J Clin Oncol. 2006;24:5101–5104. doi: 10.1200/JCO.2006.09.2700. [DOI] [PubMed] [Google Scholar]