Abstract
The aims of this study were to 1) determine the association between ethnicity and both thoracic and abdominal aortic calcium (TAC and AAC) and 2) investigate associations between cardiovascular disease (CVD) risk factors and both TAC and AAC. Participants were 1,957 men and women enrolled in the Multi-Ethnic Study of Atherosclerosis who had computed tomography scans of both the chest and abdomen. These scans were obtained at the same clinic visit and calcium scores were computed using the Agatston method. Regression analyses were conducted using relative risk regression. The mean age was 65 years and 50% were female. Forty % were White, 26% Hispanic, 21% African American and 13% Chinese. Whites had the highest prevalence of AAC (80%), which was significantly higher than Hispanics (68%, p<0.001), African Americans (63%, p<0.001) and Chinese (74%, p=0.029). Similarly, Whites had the highest prevalence of TAC (42%), which was significantly higher than Hispanics (30%, p < 0.01) and African Americans (27%, p<0.001) but was not significantly different from that in Chinese (38%). Compared to Whites and after adjustment for age, sex, body mass index, hypertension, diabetes, dyslipidemia, smoking and family history of CVD, Hispanics and African Americans, but not Chinese Americans, had a significantly lower risk for the presence of any AAC or any TAC. In these models, diabetes, smoking and dyslipidemia had stronger associations with AAC while hypertension was stronger for TAC. In conclusion, compared to Whites, African-Americans and Hispanics, but not Chinese, have evidence of less atherosclerosis in both the thoracic and abdominal aorta which does not appear to be accounted for by traditional CVD risk factors.
INTRODUCTION
The risk factors for coronary artery calcium (CAC) and thoracic aortic calcium (TAC) appear to be different while calcium due to atherosclerosis in the abdominal aorta has risk factor associations that are distinct from both CAC and TAC.1–3 Although data on the association between abdominal aortic calcium (AAC) and incident CVD events are limited,4 the characteristics of AAC suggest that detection of calcified atherosclerosis in this vascular bed may provide important preventive information.1,3 Furthermore, there is very limited information on the ethnic specific risks for calcium in different segments of the aorta. Accordingly, we conducted this study to test the hypothesis that risks for both TAC and AAC differ by ethnicity.
METHODS
Details about the study design for the Multi-Ethnic Study of Atherosclerosis (MESA) have been published elsewhere.5 In brief, between July 2000 and August 2002, 6,814 men and women who identified themselves as White, African American, Hispanic, or Chinese, were 45 to 84 years old and were free of clinically apparent cardiovascular disease (CVD) were recruited from portions of 6 US communities: Baltimore City and Baltimore County, Maryland; Chicago, Ill; Forsyth County, North Carolina; Los Angeles County, California; Northern Manhattan and the Bronx, New York; and St. Paul, Minn. Each field site recruited from locally available sources, which included lists of residents, lists of dwellings, and telephone exchanges. Individuals with a history of physician-diagnosed heart attack, angina, heart failure, stroke or transient ischemic attack, or having undergone an invasive procedure for cardiovascular disease (coronary artery bypass graft, angioplasty, valve replacement or pacemaker placement) were excluded from participation. The institutional review boards at all participating centers approved the study and all participants gave informed written consent.
Standardized questionnaires were used to obtain demographic information and level of education, annual household income, smoking history, and medication usage for high blood pressure, high cholesterol, or diabetes. Cigarette smoking was defined as current, former, or never. Height and weight were measured with participants wearing light clothing and no shoes. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Resting blood pressure was measured 3 times in seated participants with a Dinamap model Pro 100 automated oscillometric sphygmomanometer (Critikon). The average of the last 2 measurements was used in the analysis. Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥ 90 mm Hg, or current use of an antihypertensive medication.
Blood was collected and stored at −70°F until needed for the appropriate assays. Total and HDL cholesterol, triglycerides, and glucose levels were measured from blood samples obtained after a 12-hour fast. LDL cholesterol was calculated by the Friedewald equation.6 Dyslipidemia was defined as a total-cholesterol/HDL-cholesterol ratio > 5.0 or if the participant used medication to reduce cholesterol. Diabetes was defined as fasting glucose ≥ 126 mg/dL or use of hypoglycemic medication. In addition to the indices listed above, fasting blood was analyzed for selected biomarkers such as C-reactive protein.
On all participants, computed tomography of the chest for CAC and TAC was performed with cardiac-gated electron-beam scanners at 3 field centers (Imatron C-150; Imatron, Inc., San Francisco, California)7 or with a prospectively electrocardiogram triggered scan acquisition at 50 % of the R-R interval with multi-detector scanners at the remaining 3 centers.8 Scans were read centrally at Harbor - University of California Los Angeles (Torrance, California) for quantification of calcium scores using the Agatston method.9
A random subsample of approximately 2,000 subjects was recruited to participate in an ancillary study to MESA. In this study, 1,970 enrolled participants underwent computed tomography scanning of the abdomen to ascertain the presence and extent of calcium due to atherosclerosis in the abdominal aorta. These scans occurred at MESA visits 2 and 3 and were performed concomitant to the chest CT scans for CAC and TAC.
After scanning, images were reconstructed in a 35 cm field of view with 5mm slice thickness. All scan scores were brightness adjusted with a standard phantom. Scans were read centrally by the MESA CT Reading Center, and calcium was scored in an 8 cm segment of the distal abdominal aorta ending at the aortic bifurcation. For all calcium measures (i.e. CAC, TAC and AAC), calcification was identified as a plaque of ≥1mm2 with a density of ≥130 Hounsfield units and quantified using the previously described Agatston scoring method.9
Distributions of demographic and cardiovascular risk factors were compared across ethnic groups. Abdominal and thoracic aorta calcification was dichotomized as present (Agatston score > 0) or absent (= 0). Prevalence of AAC and TAC were compared across gender and race/ethnic groups using χ2 tests for categorical variables. The prevalence of calcification is high in our cohort. Hence odds ratios (ORs) do not approximate the relative risk (RR). Therefore, prevalence ratios estimates (i.e. prevalence rate ratios) are presented from the regression model y = exp(XTβ) with the exponentiated parameter estimated being interpreted as relative risks. We assumed Gaussian error and used robust standard error estimates. Using this method we assessed the relationship between each risk factor and the presence of AAC and TAC, adjusting for all other risk factors in the model. In addition, ordinal logistic regression were also employed to assess the relationship of demographics and risk factors for increasing increments of AAC & TAC ( categories: 0, 1st quartile, 2nd quartile, 3rd quartile and 4th quartile). All statistical analyses were performed with STATA version 10.0 (Stata Corp., Austin, Texas, http://www.stata.com). The level of significance was set at p < 0.05 (2-tailed).
RESULTS
Thirteen subjects who were included in the aortic calcium sub-study did not have computed tomography scans of the chest. Therefore, the study population for this analysis consisted of 1,957 men and women. The mean (standard deviation) age was 65 (10) years and 50% were male. Forty % were non-Hispanic White, 26% Hispanic, 21% African American and 13% Chinese. The characteristics of the cohort stratified by ethnic group are presented in Table 1.
Table 1.
Characteristics by Ethnic Group: The Multi-Ethnic Study of Atherosclerosis (1990 – 2000)
| Variable | African Americans | Chinese | Hispanics | White |
|---|---|---|---|---|
| Age (years) | 64±10 | 65±10 | 63±10 | 65±10 |
| Female | 56% | 47% | 50% | 47% |
| Current smoker | 16% | 4% | 11% | 12% |
| Hypertension | 63% | 41% | 48% | 49% |
| Diabetes Mellitus | 20% | 15% | 21% | 10% |
| Family History of Coronary Heart Disease | 42% | 21% | 42% | 52% |
| Low Density Lipoprotein Cholesterol (mg/dl) | 114±34 | 109±28 | 116±33 | 109±29 |
| High Density Lipoprotein Cholesterol (mg/dl) | 55±16 | 51±14 | 48±13 | 52±16 |
| Body Mass Index (kg/m2) | 30±5 | 24±3 | 30±5 | 28±5 |
| Lipid Lowering Medications | 17% | 25% | 22% | 30% |
| C-Reactive Protein (mg/dl) | 4.3±6.0 | 1.7±3.1 | 4.1±5.1 | 3.5±5.1 |
| Fibrinogen (mg/dl) | 354±74 | 327±58 | 364±74 | 331±67 |
| Homocysteine (µmol/L) | 9.8±3.5 | 9.2±3.0 | 9.0±2.8 | 9.5±5.1 |
Overall, the prevalence of AAC was significantly higher than TAC (73% vs. 35%, p<0.01). The simultaneous presence of calcium in both vascular beds (i.e. thoracic and abdominal aorta) was found in 34% of subjects while the prevalence of calcium limited to the thoracic and abdominal aorta was 1 and 39%, respectively. No calcification was observed in 26% of subjects. The highest prevalence of AAC was observed in non-Hispanic Whites (80%) and was significantly higher than in Chinese (74%, p=0.03), Hispanics (68%, p<0.01) and African Americans (63%, p<0.01). The highest prevalence of TAC was also observed in non-Hispanic Whites (42%) and this was significantly higher than found in Hispanics (30%, p < 0.01) and African Americans (27%, p<0.01) but not Chinese (38%). These relationships were similar in individuals under the age of 65 (Table 2). However, in those over the age of 65, Chinese women had the highest prevalence of calcium in both the thoracic and abdominal aorta.
Table 2.
Age, Sex and Ethnic Specific Prevalences of Calcium in the Abdominal and Thoracic Aorta: The Multi-Ethnic Study of Atherosclerosis (1990 – 2000)
| Ethnic Group | <65 years (n=981) | ⩾65 years (n=976) | ||||||
|---|---|---|---|---|---|---|---|---|
| Males (n=511) | Females (n=470) | Males (n=476) | Females (n=500) | |||||
| AAC | TAC | AAC | TAC | AAC | TAC | AAC | TAC | |
| Non-Hispanic White (n=782) | 67% | 17% | 60% | 19% | 97% | 65% | 94% | 63% |
| Chinese (n=258) | 55% | 12% | 50% | 16% | 96% | 58% | 95% | 65% |
| Hispanic (n=508) | 53% | 9% | 51% | 13% | 91% | 48% | 85% | 59% |
| African Americans (n=409) | 46% | 7% | 43% | 17% | 80% | 35% | 84% | 45% |
AAC= Abdominal Aorta Calcification, TAC= Thoracic Aorta Calcification
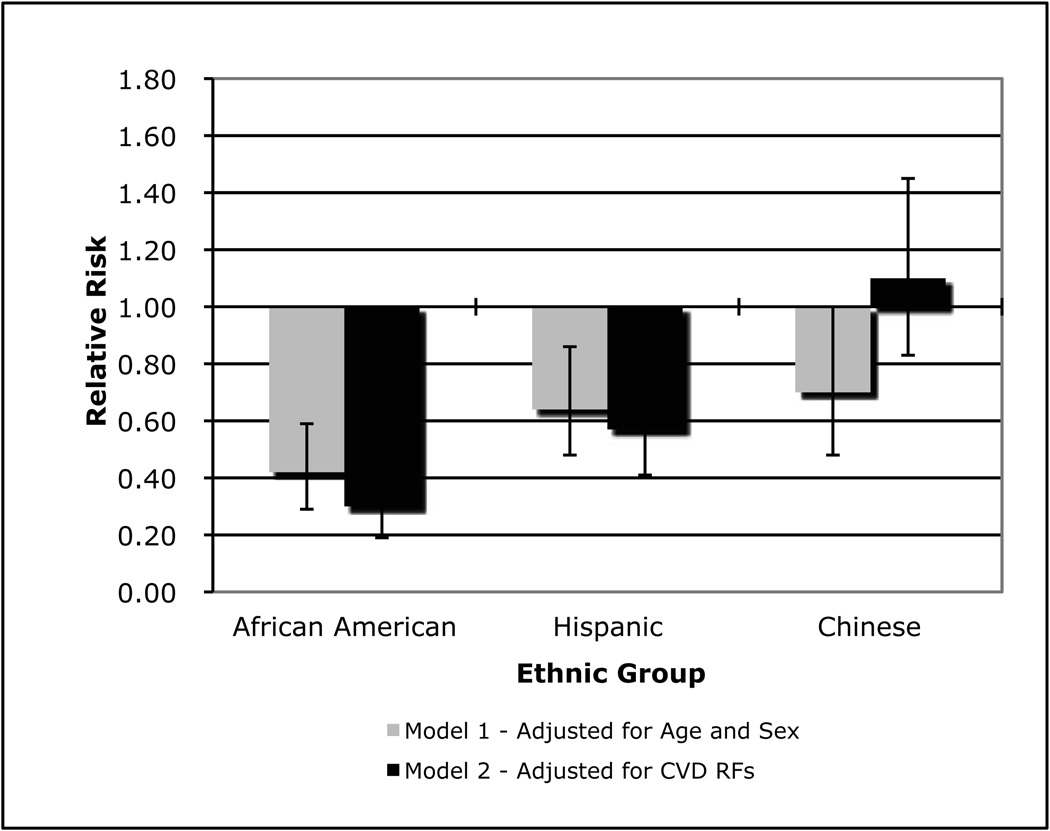
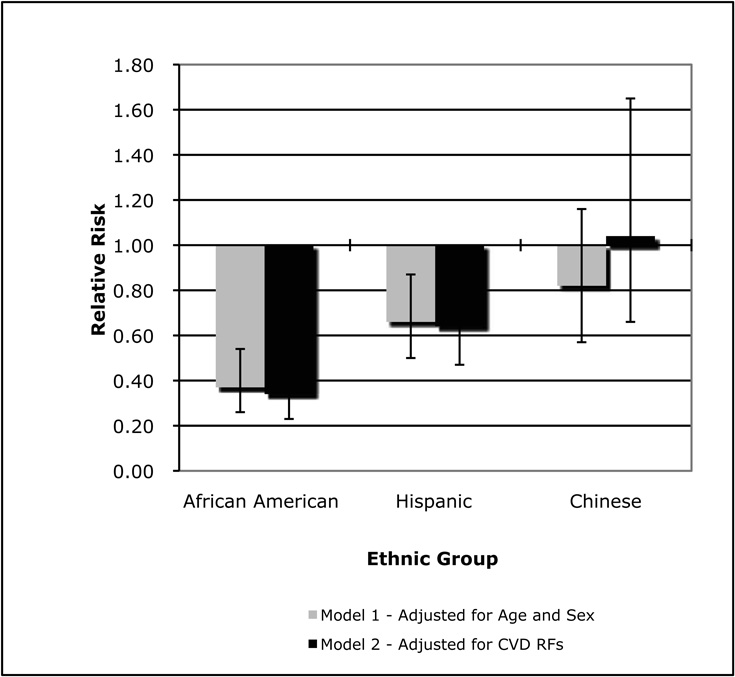
Figure 1 & Figure 2 show the ethnic specific relative risk estimates for AAC and TAC, respectively. With adjustment for age and sex, African Americans (RR: 0.42, p < 0.01), Hispanics (0.64, p < 0.01) and Chinese (0.70, p = 0.05) had significantly lower prevalence of AAC. After further adjustment for smoking, hypertension, diabetes, dyslipidemia and family history of CVD, the relative risk for AAC in African Americans and Hispanics were accentuated (0.30 and 0.57, respectively; p < 0.01 for both), while the risk for Chinese was attenuated and no longer significant (1.1, p = 0.52). The results were similar for TAC. Specifically, both African Americans and Hispanics had reduced risks for the presence of any TAC after adjustment for age and sex (0.37 and 0.66, respectively; p < 0.01 for both) that was modestly attenuated with additional adjustment for the CVD risk factors listed above. The risk for TAC among Chinese was not significantly different from non-Hispanic Whites regardless of the adjustment. Of note, for all ethnic groups, replacing dyslipidemia with the individual cholesterol fractions or additional adjustment for C-reactive protein, fibrinogen and homocysteine did not change the magnitude or significance of the associations for the presence of AAC or TAC.
Figure 1.
Relative Risk Estimates for the Presence of Any Calcium Due to Atherosclerosis in the Abdominal Aorta: (2000 – 2006)
Reference Group = Non-Hispanic White
Figure 2.
Relative Risk Estimates for the Presence of Any Calcium Due to Atherosclerosis in the Thoracic Aorta: The Multi-Ethnic Study of Atherosclerosis (2000 – 2006)
Reference Group = Non-Hispanic White
In the models just described, there were differences in the associations between the traditional CVD risk factors and both AAC and TAC. For example, the associations between current and former smoking and AAC (RR: 5.8, 95% CI: 3.5 – 9.5; 2.4, 1.7 – 3.3; respectively) were larger than the associations between these smoking variables and TAC (2.4, 1.6 – 3.8; 1.7, 1.3 – 2.3; respectively). The risk for AAC associated with diabetes was 1.9 (1.1 – 2.1) compared to 1.2 (0.8 – 1.7) for TAC. Conversely, the presence of hypertension was stronger for TAC than AAC (2.6, 2.0 – 3.4 vs. 1.7, 1.1 – 3.1).
Using a calcium score of zero (referent) and quartiles for the presence of AAC and TAC, Table 3 provides odds ratios for increasing increments of AAC & TAC. The results of these ordinal logistic regression analyses are very similar to those for the presence and absence of AAC and TAC. That is, after adjustment for the age, sex and the CVD risk factors, African Americans had a 60% lower odds for increasing increments of AAC while Hispanics had 35% lower odds. The odds in Chinese was not significantly different from non-Hispanic Whites. After the same adjustment, African Americans again had a 60% lower odds for increasing TAC, Hispanics had nearly a 40% lower odds and Chinese were not significantly different from non-Hispanic Whites.
Table 3.
Odds for Increasing Increments of Abdominal Aortic Calcium (AAC) and Thoracic Aortic Calcium (TAC): The Multi-Ethnic Study of Atherosclerosis (1990 – 2000)
| Variable | AAC* | TAC* | ||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Age (per 10 years) | 3.36 | 3.00–3.75 | 4.14 | 3.59–4.76 |
| Male vs. Female | 1.11 | 0.91–1.34 | 0.61 | 0.48–0.77 |
| Ethnic Group | ||||
| White | 1.00 (ref) | -- | 1.00 (ref) | -- |
| Chinese | 0.95 | 0.71–1.28 | 1.12 | 0.78–1.60 |
| Black | 0.41 | 0.32–0.53 | 0.39 | 0.29–0.54 |
| Hispanic | 0.66 | 0.53–0.83 | 0.62 | 0.47–0.83 |
| Smoking | ||||
| Never Smoker | 1.00 (ref) | -- | 1.00 (ref) | -- |
| Former Smoker | 2.31 | 1.90–2.81 | 1.60 | 1.26–2.03 |
| Current Smoker | 4.42 | 3.25–6.01 | 2.93 | 1.98–4.34 |
| Hypertension | 1.82 | 1.50–2.21 | 2.69 | 2.11–3.41 |
| Diabetes Mellitus | 1.54 | 1.18–2.00 | 1.52 | 1.12–2.06 |
| Family History of Coronary Heart Disease | 1.39 | 1.16–1.67 | 1.44 | 1.15–1.80 |
| Low Density Lipoprotein Cholesterol (per SD=31) | 1.26 | 1.15–1.38 | 1.09 | 0.97–1.23 |
| High Density Lipoprotein Cholesterol (per SD=15) | 0.83 | 0.75–0.92 | 0.82 | 0.73–0.93 |
| Body Mass Index (per SD=5 ) | 1.01 | 0.91–1.1 | 0.94 | 0.83–1.06 |
| Cholesterol Medication | 2.08 | 1.67–2.59 | 1.35 | 1.04–1.73 |
For both AAC and TAC, all listed independent variables are in the same model
To determine if there were differences in the associations between CVD risk factors and both AAC and TAC by ethnic group, we conducted relative risk regression analyses stratified by ethnicity (Table 4). Increasing age was strongly associated with both AAC and TAC in all ethnic groups but the association was strongest for Chinese women and AAC. Male gender was associated with twice the risk for AAC in Non-Hispanic Whites. Current smoking was a strong risk factor for AAC in Non-Hispanic Whites and African Americans. Otherwise and in general, the risks for AAC and TAC associated with hypertension, diabetes, family history of CVD, cholesterol fractions and cholesterol medication use were similar across all ethnic groups.
Table 4.
Ethnic Specific Risk Factor Associations for Abdominal Aortic Calcium (AAC) and Thoracic Aortic Calcium (TAC): The Multi-Ethnic Study of Atherosclerosis (1990 – 2000)
| Abdominal Aortic Calcium (AAC) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Non-Hispanic White | Hispanic | Chinese | African American | ||||
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |
| Age (per 10 years) | 5.4 | 3.6–8.1 | 5.6 | 2.9–10.7 | 9.0 | 3.1–25.5 | 3.2 | 2.3–4.5 |
| Male vs. Female | 2.0 | 1.1–3.7 | 1.1 | 0.6–2.1 | 0.6 | 0.2–2.0 | 0.7 | 0.3–1.3 |
| Smoking | ||||||||
| Never Smoker | 1.00 (ref) | -- | 1.00 (ref) | -- | 1.00 (ref) | -- | 1.00 (ref) | -- |
| Former Smoker | 3.4 | 1.7–6.6 | 3.3 | 1.5–7.1 | 2.2 | 0.5–9.2 | 2.5 | 1.3–4.9 |
| Current Smoker | 11.6 | 5.6–29.1 | 3.9 | 1.5–10.1 | 2.2 | 0.4–24.8 | 7.8 | 2.8–21.6 |
| Hypertension | 1.9 | 1.0–3.5 | 1.4 | 0.8–2.5 | 2.4 | 0.2–34.5 | 1.9 | 1.1–3.3 |
| Diabetes Mellitus | 1.3 | 0.5–3.5 | 2.2 | 0.8–5.9 | 10.4 | 0.1–2456.7 | 1.6 | 0.7–3.8 |
| Family history of Coronary Heart Disease | 1.0 | 0.6–1.8 | 1.6 | 0.9–2.9 | 1.3 | 0.3–4.8 | 0.8 | 0.4–1.5 |
| Low Density Lipoprotein Cholesterol (per SD=31) | 1.1 | 0.8–1.4 | 1.4 | 1.1–1.8 | 3.4 | 0.2–1.0 | 1.2 | 0.9–1.6 |
| High Density Lipoprotein Cholesterol (per SD=15) | 0.9 | 0.7–1.2 | 0.8 | 0.5–1.0 | 0.3 | 0.1–1.8 | 0.8 | 0.6–1.0 |
| Body Mass Index (per SD=5) | 1.1 | 0.7–1.6 | 1.1 | 0.8–1.5 | 1.0 | 0.1–10.0 | 1.0 | 0.7–1.3 |
| Cholesterol Medication | 3.6 | 1.3–10.1 | 2.0 | 0.9–4.4 | Undef | Undef | 1.5 | 0.7–2.9 |
| Thoracic Aortic Calcium (TAC) | ||||||||
| Variable | Non-Hispanic White | Hispanic | Chinese | African American | ||||
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |
| Age (per 10 years) | 4.5 | 3.4–5.9 | 5.9 | 3.1–11.4 | 4.2 | 1.8–9.6 | 3.0 | 2.2–4.2 |
| Male vs. Female | 1.0 | 0.6–1.6 | 0.3 | 0.1–0.8 | 0.3 | 0.1–0.9 | 0.5 | 0.3–0.9 |
| Smoking | ||||||||
| Never Smoker | 1.00 (ref) | -- | 1.00 (ref) | -- | 1.00 (ref) | -- | 1.00 (ref) | -- |
| Former Smoker | 1.4 | 0.9–2.2 | 3.3 | 1.7–6.5 | 3.6 | 1.1–11.6 | 1.6 | 0.8–2.9 |
| Current Smoker | 3.1 | 1.6–6.0 | 4.5 | 1.3–15.2 | Undef | Undef | 2.1 | 0.7–6.1 |
| Hypertension | 2.9 | 1.9–4.6 | 3.9 | 1.9–7.8 | 3.0 | 1.0–8.9 | 1.6 | 0.8–3.0 |
| Diabetes Mellitus | 1.4 | 0.6–3.2 | 2.0 | 0.8–4.6 | 2.1 | 0.7–7.1 | 0.9 | 0.5–1.8 |
| Family History of Coronary Heart Disease | 1.5 | 0.9–2.2 | 1.3 | 0.7–2.2 | 1.3 | 0.3–5.2 | 1.2 | 0.7–2.1 |
| Low Density Lipoprotein Cholesterol (per SD=31) | 1.2 | 0.9–1.5 | 1.3 | 1.0–1.7 | 0.8 | 0.4–1.6 | 1.1 | 0.8–1.6 |
| High Density Lipoprotein Cholesterol (per SD=15) | 0.8 | 0.6–1.03 | 0.8 | 0.5–1.2 | 0.8 | 0.4–1.5 | 0.8 | 0.6–1.0 |
| Body Mass Index (per SD=5 ) | 0.9 | 0.7–1.1 | 0.9 | 0.6–1.30 | 0.3 | 0.2–0.7 | 1.0 | 0.7–1.4 |
| Cholesterol Medication | 1.2 | 0.7–2.0 | 1.0 | 0.5–2.2 | 1.2 | 0.4–3.8 | 1.5 | 0.8–2.9 |
For both AAC and TAC, as well as the different ethnic groups, all listed independent variables are in the same model Undef = Undefined (due to small cell size)
DISCUSSION
Previous results from the MESA indicate ethnic specific differences in the prevalence of calcified atherosclerosis in the coronary arteries. Specifically, compared to non-Hispanic Whites (where the prevalence of CAC was 70% in men and 45% in women), the prevalence of any CAC was lower in African (52% and 36%, respectively), Hispanic (56% and 35%, respectively) and Chinese Americans 59% and 42%, respectively).10 These results are similar to those for the current analysis on thoracic and aortic calcium and suggest either ethnic specific differences in the rates of developing atherosclerosis or in the propensity to calcify atherosclerotic plaques or both. In this regard and compared to Whites, African Americans were found to have higher prevalences of atherosclerosis in all 3 vascular beds studied in the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study.11 Other research, including that derived from CT scans,12 suggests that atherosclerosis is calcified less frequently in African Americans.13 Unfortunately, similar studies comparing Whites with either Chinese or Hispanic Americans are not available and indicate an important gap that should be pursued in future research efforts.
In the context of a higher atherosclerotic burden, the lower rate of calcification in African Americans suggests that there may be ethnic differences in certain components of the atherosclerotic process. To this end, calcium is deposited in arteries and other vascular areas as part of the chronic inflammatory process of atherosclerosis14,15 and these calcified plaques are histologically similar to those from enchondral bone. Indeed, atherosclerotic plaques have been found to contain tissue similar to bone marrow.16 In 2 separate studies, we have reported significant inverse associations between lumbar bone mineral density and calcified atherosclerosis in the abdominal aorta and coronary arteries.17,18 Furthermore, cell-culture studies have demonstrated that oxidized low-density lipoprotein cholesterol inhibits the differentiation of osteoblasts in bone while promoting the calcification of smooth muscle vascular cells.19 However, oxidized LDL levels are higher in both African Americans and Hispanics than in Whites and Chinese,20 which is opposite of what one would expect if this type of cholesterol was associated with decreased bone mineral density and increased atherosclerotic calcification. Clearly, more research is needed to better understand the links between calcified atherosclerosis and ethnicity.
The strengths of our study include use of understudied minority groups, a large well-characterized sample, measures of calcium from vascular beds for which there is a limited literature, and a standardized assessment of vascular calcium. Our study has limitations, and thus our conclusions are drawn with caution. First, although the selection of subjects for the MESA study was population-based, it was not random. Second, in some of the analytic cells, the number of Chinese and Hispanics was relatively small. Therefore, the relative risk estimates in Figure 1 & Figure 2 for these ethnic groups (especially Chinese Americans) should be viewed with caution. Also, the power to detect significant differences in the ethnic specific analyses for risk factors is likely marginal. This may have also contributed to the unexpectedly higher prevalences of calcium in Chinese participants over the age of 65. Finally, residual confounding due to misclassification and non-perfect ascertainment of risk factors may have resulted in slightly inflated effect estimates for the different ethnic groups.
ACKNOWLEDGEMENTS
This research was supported by a grant from the American Heart Association (Allison), a grant from the NIH (R01 HL071739) and contracts N01-HC-95159 through N01-HC-95165 and N01-HC-95169 from the National Heart, Lung, and Blood Institute. The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Allison MA, Criqui MH, Wright CM. Patterns and risk factors for systemic calcified atherosclerosis. Arterioscler Thromb Vasc Biol. 2004;24:331–336. doi: 10.1161/01.ATV.0000110786.02097.0c. [DOI] [PubMed] [Google Scholar]
- 2.Kuller LH, Matthews KA, Sutton-Tyrrell K, Edmundowicz D, Bunker CH. Coronary and aortic calcification among women 8 years after menopause and their premenopausal risk factors : the healthy women study. Arterioscler Thromb Vasc Biol. 1999;19:2189–2198. doi: 10.1161/01.atv.19.9.2189. [DOI] [PubMed] [Google Scholar]
- 3.Wong ND, Sciammarella M, Arad Y, Miranda-Peats R, Polk D, Hachamovich R, Friedman J, Hayes S, Daniell A, Berman DS. Relation of thoracic aortic and aortic valve calcium to coronary artery calcium and risk assessment. Am J Cardiol. 2003;92:951–955. doi: 10.1016/s0002-9149(03)00976-7. [DOI] [PubMed] [Google Scholar]
- 4.Wilson PWF, Kauppila LI, O'Donnell CJ, Kiel DP, Hannan M, Polak JM, Cupples LA. Abdominal Aortic Calcific Deposits Are an Important Predictor of Vascular Morbidity and Mortality. Circulation. 2001;103:1529–1534. doi: 10.1161/01.cir.103.11.1529. [DOI] [PubMed] [Google Scholar]
- 5.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR, Jr, Kronmal R, Liu K, Nelson JC, O'Leary D, Saad MF, Shea S, Szklo M, Tracy RP. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 6.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 7.Breen J, Sheedy P, Schwartz R. Coronary artery calcification detected with ultrafast CT as an indication of coronary artery disease. Radiology. 1992;185:435–439. doi: 10.1148/radiology.185.2.1410350. [DOI] [PubMed] [Google Scholar]
- 8.Carr J, Crouse J, Goff D. Evaluation of sub-second gated helical CT for quantification of coronary artery calcium and comparison with electron beam CT. Am J Radiol. 2000;174:915–921. doi: 10.2214/ajr.174.4.1740915. [DOI] [PubMed] [Google Scholar]
- 9.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 10.Bild DE, Detrano R, Peterson D, Guerci A, Liu K, Shahar E, Ouyang P, Jackson S, Saad MF. Ethnic Differences in Coronary Calcification: The Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2005;111:1313–1320. doi: 10.1161/01.CIR.0000157730.94423.4B. [DOI] [PubMed] [Google Scholar]
- 11.Zieske AW, Malcom GT, Strong JP. Natural history and risk factors of atherosclerosis in children and youth: the PDAY study. Pediatr Pathol Mol Med. 2002;21:213–237. doi: 10.1080/15227950252852104. [DOI] [PubMed] [Google Scholar]
- 12.Wagenknecht LE, Langefeld CD, Freedman BI, Carr JJ, Bowden DW. A Comparison of Risk Factors for Calcified Atherosclerotic Plaque in the Coronary, Carotid, and Abdominal Aortic Arteries: The Diabetes Heart Study. Am. J. Epidemiol. 2007;166:340–347. doi: 10.1093/aje/kwm091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burke APFA, Kutys R, Zieske A, Weber D, Virmani R. Atherosclerotic coronary plaques in African Americans are less likely to calcify than coronary plaques in Caucasian Americans. Circulation. 2002;106 S:481. [Google Scholar]
- 14.Stary HC. The development of calcium deposits in atherosclerotic lesions and their persistence after lipid regression. Am J Cardiol. 2001;88:16E–19E. doi: 10.1016/s0002-9149(01)01713-1. [DOI] [PubMed] [Google Scholar]
- 15.Stary HC, Chandler AB, Dinsmore RE, Fuster V, Glagov S, Insull W, Jr, Rosenfeld ME, Schwartz CJ, Wagner WD, Wissler RW. A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Arterioscler Thromb Vasc Biol. 1995;15:1512–1531. doi: 10.1161/01.atv.15.9.1512. [DOI] [PubMed] [Google Scholar]
- 16.Demer LL, Tintut Y. Mineral exploration: search for the mechanism of vascular calcification and beyond: the 2003 Jeffrey M. Hoeg Award lecture. Arterioscler Thromb Vasc Biol. 2003;23:1739–1743. doi: 10.1161/01.ATV.0000093547.63630.0F. [DOI] [PubMed] [Google Scholar]
- 17.Hyder JA, Allison MA, Criqui MH, Wright CM. Association between systemic calcified atherosclerosis and bone density. Calcif Tissue Int. 2007;80:301–306. doi: 10.1007/s00223-007-9004-6. [DOI] [PubMed] [Google Scholar]
- 18.Hyder JA, Allison MA, Wong N, Papa A, Lang TF, Sirlin C, Gapstur SM, Ouyang P, Carr JJ, Criqui MH. Association of Coronary Artery and Aortic Calcium With Lumbar Bone Density: The MESA Abdominal Aortic Calcium Study. Am J Epidemiol. 2008 doi: 10.1093/aje/kwn303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parhami F, Morrow AD, Balucan J, Leitinger N, Watson AD, Tintut Y, Berliner JA, Demer LL. Lipid oxidation products have opposite effects on calcifying vascular cell and bone cell differentiation. A possible explanation for the paradox of arterial calcification in osteoporotic patients. Arterioscler Thromb Vasc Biol. 1997;17:680–687. doi: 10.1161/01.atv.17.4.680. [DOI] [PubMed] [Google Scholar]
- 20.Holvoet P, Jenny NS, Schreiner PJ, Tracy RP, Jacobs DR. The relationship between oxidized LDL and other cardiovascular risk factors and subclinical CVD in different ethnic groups: The Multi-Ethnic Study of Atherosclerosis (MESA) Atherosclerosis. 2007;194:245–252. doi: 10.1016/j.atherosclerosis.2006.08.002. [DOI] [PubMed] [Google Scholar]