Abstract
Objective
To examine inter-relationships among stress due to infant appearance and behavior in the NICU, parental role alteration stress in the NICU, depressive symptoms, state anxiety, post-traumatic stress symptoms, and daily hassles exhibited by African American mothers of preterm infants and to determine whether there were sub-groups of mothers based on patterns of psychological distress.
Method
177 African American mothers completed questionnaires on their psychological distress at enrollment during infant hospitalization and 2, 6, 12, 18, and 24 months after term.
Results
Psychological distress measures were inter-correlated. There were four latent classes of mothers: the low distress class with low scores on all measures; the high NICU-related stress class with high infant appearance and parental role stress and moderate scores on other measures; the high depressive symptoms class with high depressive symptoms and state anxiety and moderately elevated scores on NICU-related stress and post-traumatic stress symptoms; the extreme distress class with the highest means on all measures. Infants in the high stress class were sicker than infants in the other classes. The extreme distress class mothers averaged the lowest educational level. The classes differed on distress measures, worry about the child, and parenting stress through 24 months with the extreme distress class having the highest values.
Conclusion
Although different types of maternal psychological distress were substantially related, there were distinct sub-groups of mothers that were identifiable in the NICU. Moreover, these sub-groups continued to differ on trajectories of distress and on their perceptions of the infants and parenting through 24 months after term.
Keywords: Maternal Psychological Distress, Prematurity, Depression, Anxiety, Stress
PATTERNS OF DISTRESS IN AFRICAN AMERICAN MOTHERS OF PRETERM INFANTS
Mothers of preterm infants exhibit high levels of psychological distress during infant hospitalization and after discharge, as shown by high levels of depression, anxiety, stress, and post-traumatic stress symptoms.1-6 African American mothers may be at particular risk for this psychological distress because they not only have about twice the risk of prematurity as Whites7 but also are more distressed in response to prematurity.8-10 The purpose of this study was to examine the inter-relationships of different types of emotional distress--stress due to infant appearance and behavior in the neonatal intensive care unit (NICU), stress due to parental role alteration in the NICU, depressive symptoms, state anxiety, post-traumatic stress symptoms, and daily hassles--occurring in African American mothers of hospitalized preterm infants and to determine whether there were sub-groups of mothers based on patterns of distress.
During infant hospitalization in a NICU, mothers experience high levels of multiple types of psychological distress. Preterm infant hospitalization leads mothers to fear the infant may not survive and grieve over the infant's immaturity and the loss of the expected maternal role.8, 9, 11-13 About 50% of mothers of premature infants have elevated levels of anxiety or depressive symptoms during hospitalization.4, 11, 13, 14-18
Mothers continue to have high levels of emotional distress after their preterm infants are discharged from the hospital. Distressing memories of the NICU continue for 6 months or more,19-21 and some mothers show post-traumatic stress symptoms.2, 3, 5, 22 Further, emotional distress due to prematurity affects maternal perceptions of their children and parenting quality.5, 18, 23-28 For example, mothers of 8-month-old premature infants had more parenting stress than mothers of fullterm infants, even when their infants’ behaviors did not differ.29
Few studies have compared the responses of African American mothers of premature infants to mothers of other racial groups, but African American mothers of premature infants may exhibit somewhat higher levels of distress8-10 although this finding is not universal.30, 31 Similarly, African American mothers of fullterm infants have been found to exhibit higher levels of depression and daily stress than other mothers of fullterms.32 Responses of African American mothers to their premature infants’ health crises may be affected by their cultural backgrounds.33, 34 They often report placing a high value on being a mother.35 Daily hassles associated with economic hardship and being a single parent are additional stressors for these mothers.35, 36 Compared to all mothers of prematures, unmarried mothers and mothers with low education show more emotional distress.15, 18, 37 Low-income, unmarried, African American mothers of children born at term had more depressive symptoms than other African American mothers.38, 39
Although researchers have found correlations among different types of emotional distress in mothers of preterm infants,3, 4, 6, 11, 12, 15, 17 the extent to which there are sub-groups of mothers showing different patterns of distress is unknown. Psychological distress related to prematurity is high during hospitalization and decreases over the first year after birth,4, 6, 14, 17, 40 but most individual mothers do not show this pattern.4 Thus, there may be sub-groups of mothers showing different patterns of distress after premature birth. The purpose of this study, therefore, was to examine the inter-relationship of stress due to infant appearance and behavior in the NICU, stress due to parental role alteration in the NICU, depressive symptoms, state anxiety, post-traumatic stress symptoms, and daily hassles in African American mothers of hospitalized preterms and to determine whether there were sub-groups of mothers based on patterns of distress. We examined whether the sub-groups of mothers differed based on maternal and infant characteristics and infant illness and whether maternal psychological distress and perceptions of their infants and parenting (worry, parenting stress) differed through 2 years after term.
METHODS
Participants
Participants were 177 African American biological mothers of preterm infants weighing less than 1500 gm at birth or requiring mechanical ventilation. The mother-infant dyads were participants in a randomized study testing a nursing support intervention for mothers of prematures. Mothers who lived in rural and small town areas in a southeastern state were recruited from the NICUs of two hospitals when their infants were no longer critically ill. Infants who had congenital neurological problems (such as Down Syndrome or microcephaly), were symptomatic from substance exposure, were hospitalized longer than 2 months post-term, or were triplets or part of a higher order multiples set were excluded. We also excluded mothers who did not have custody or if follow-up for 2 years was unlikely (out-of-state visitors as mothers, maternal HIV), were less than 15 of age, were critically ill, did not speak English, or had mental health problems (history of bipolar disease or psychosis, current diagnosis of major depression, current use of antidepressants). Randomization group was controlled for in all longitudinal analyses, but the groups did not differ significantly on any variable. Table 1 gives the characteristics of the mothers and infants.
Table 1.
Demographic Characteristics of the 177 Rural, African American Mothers and Their Preterm Infants
| Mean (SD) | Percent | |
|---|---|---|
| Maternal Age in Years | 25.9 (6.5) | |
| Percent Married | 26.1% | |
| Maternal Education in Years | 12.6 (1.8) | |
| Percent First-Time Mothers | 25.9% | |
| Delivery: Percent Cesarean Section | 53.7% | |
| Percent on Public Assistance | 52.8% | |
| Percent: Singletons | 91.5% | |
| Twins | 8.4% | |
| Infant Gestational Age in Weeks | 28.3 (2.9) | |
| Infant Birth Weight in Grams | 1107 (394) | |
| Percent Small for Gestational Age | 21.4% | |
| Sex of Child: Male | 42.3% | |
| Infant Medical Complications | ||
| Length of Mechanical Ventilation (days) | 15.6 (26.5) | |
| Intraventricular Hemorrhage: None | 77.3% | |
| Grade I | 14.8% | |
| Grade II | 4.0% | |
| Grade III | 2.3% | |
| Grade IV | 1.7% | |
| Percent Surgery | 24.4% | |
| Percent Patent Ductus Arteriosus | 39.2% | |
| Neurological Insults a | 2.8 (2.7) | |
| Percent with Infections | 60.8% | |
| Number of Infections | 1.9 (4.4) | |
Scored on the NBRS.58
Measures
All data were collected using ages after term. Time points for data collection were enrollment in the hospital, and 2, 6, 12, 18, and 24 months after term.
In this paper, psychological distress is a general term for negative maternal emotional responses. We studied six types of maternal psychological distress: stress in the NICU due to the appearance and behavior of the infant, stress in the NICU due to alterations in the parental role, depressive symptoms, state anxiety, post-traumatic stress symptoms, and minor stresses experienced in daily life. These variables encompass the major psychological responses of mothers of premature infants and are related to child developmental outcomes.3, 4, 10, 13, 41-43 The NICU-related stress variables measured two distinct sources of stress: differences in the appearance and behavior of the infant from that of healthy fullterms and changes in the parental role due to factors in the NICU such as separation from the infant and competition with nurses. Depressive symptoms and state anxiety are mood states that mothers experience because of the infant illness and other life events. Post-traumatic stress symptoms are intrusive thoughts, avoidance or numbing, and increased arousal that mothers may experience after the traumatic event of the birth and hospitalization of a preterm infant. Daily hassles are stresses due to daily life events. Daily hassles have nothing to due with the prematurity but may worsen the emotional distress that mothers experience due to a premature infant. All variables, except the two NICU-related stress variables, were studied through 2 years after term.
The Parental Stressor Scale:NICU (PSS:NICU) measured the mother's perception of the amount of stress resulting from the appearance and behavior of the infant in the NICU and from alterations in the parental role during the neonatal hospitalization.12 Mothers rated their responses to the overall experience of the infant's hospitalization on 29 items on a 5-point rating scale ranging from “not at all stressful” to “extremely stressful.” Internal consistency alphas for the infant appearance and behavior sub-scale were .76−.92 and for the parental role alteration sub-scale .83−.92.4, 12, 17, 25 In this study, alphas were .89 for the infant appearance sub-scale and .89 for the parental role alteration sub-scale.
The Center for Epidemiologic Studies Depression Scale (CESD) measured depressive symptoms.44 The frequency of 20 depressive symptoms is rated on a 4-point Likert scale, from “rarely or none of the time (less than 1 day in the past week)” to “most or all of the time (5−7 days).” Scores range from 0 to 60, with higher scores indicating more depressive symptoms. A score of 16 is the critical point for identifying risk for depression, though it does not imply a diagnosis of depression.45, 46 The CESD is correlated with other measures of depression,44, 47 and CESD scores of mothers of high-risk infants were related to other psychological distress measures, such as hospital environmental stress, worry about the child's health, and post-traumatic stress symptoms.17, 48 The CESD has good test-retest reliability.44 Cronbach's alphas were .87−.91 in other studies of mothers of high-risk infants and African American women.4, 17, 49, 50 In this study, internal consistency ranged from .87 at 24 months to .92 at 2 months.
The state anxiety sub-scale of the State-Trait Anxiety Inventory (STAI) measured maternal situational anxiety.51 The state sub-scale includes 20 items and is sensitive to changes in anxiety levels. A score above 47, equal to the 50th percentile for psychiatric patients and the 85th percentile for community dwelling women of 19−39 years of age,51 indicated elevated anxiety in this study. Numerous psychometric studies of the STAI have been conducted.51 Cronbach's alphas were .85 to .95 in studies with African Americans and mothers of prematures.37, 50, 51 In this study, alphas ranged from .90 at 6 and 18 months to .95 at 2 months.
The Perinatal PTSD Questionnaire (PPQ) measured the extent to which mothers experienced post-traumatic stress symptoms in response to the birth and hospitalization of the infant.53, 54 The PPQ has 14 yes-no items measuring intrusive thoughts (e.g., bad dreams of giving birth), avoidance or numbing (e.g., inability to remember parts of the hospitalization), and increased arousal (e.g., increased irritability or anger). The “yes” answers are summed. In White and African American mothers, Cronbach's alpha was .83, and test-retest reliability over 2 to 4 weeks was .92.53 Scores on this tool have been correlated with scores on general PTSD scales (that are not specific to perinatal events) and with the severity of infant perinatal complications.21, 53, 54 Scores of 6 or greater are indicative of elevated PTSD symptoms.21, 53, 54 Internal consistency in this study ranged from .80 at 6 months to .87 at 2 and 24 months.
The daily hassles sub-scale of the Hassles and Uplift Scale measured the stress mothers experience in daily life.55, 56 This sub-scale included 53 items (e.g., time alone, your spouse, your health) rated on the degree to which the item was a hassle today on a 4-point scale, ranging from “none or not applicable” to “a great deal.” The item scores are summed to give the overall severity of hassles, ranging from 0 to 159. Daily hassles severity is related to psychological symptoms and infant development; the tool has been used with African American mothers of prematures.10, 47 Mean day-to-day correlation was .77, and mean monthly correlation was .82.55 Internal consistency in this study ranged from .93 at enrollment to .96 at 6, 12, and 24 months.
Maternal and Infant Characteristics
At each contact, mothers completed a demographic questionnaire. Maternal education, marital status, and public assistance were used to compare sub-groups.
Infant medical records were reviewed weekly until hospital discharge to obtain information on maternal obstetric history and infant medical course. Gestational age was calculated from the obstetric estimated date of confinement, determined either by the date of the mother's last menstrual period or by a first trimester ultrasound examination. When this gestational age did not agree within 2 weeks with the results of a Ballard gestational age examination57 conducted by a clinician on admission to the NICU, the age based on the Ballard examination was used. Age past term was calculated as the number of months past the expected birth date. Maternal characteristics of parity and cesarean section and infant characteristics of gender and twin birth were used to compare sub-groups. Sub-groups were also compared on illness variables: birthweight, gestational age, small for gestational age, mechanical ventilation length, intraventricular hemorrhage, surgery, infections, and patent ductus arteriosis.
To determine the severity of infant neurological insults for sub-group comparisons, the medical record information was scored on the Neurobiologic Risk Scale (NBRS).58 This scale measures insults to the brain through direct injury or inadequate blood flow, oxygenation, or nutrients. Seven insults are scored for severity on a 4-point scale, with higher scores indicating more severe insults. Scores on the NBRS correlated between −.37 and −.65 with developmental scores obtained at 6−24 months and .60 with neurological examinations at 6 and 15 months.58 Inter-rater reliability was reported to be 97%58 but was not assessed in this study.
Perception of Infants and Parenting
The Worry Index26 measured the degree to which mothers worried about their infants in seven areas (eg, medical problems, the infant returning to the hospital, the infant getting enough to eat) at all contacts. Items are rated on a 5-point scale, from “not at all” to “very much.” In previous studies, the internal consistency with African American and white mothers was .75−.90.26, 48 Internal consistency in this study ranged from .77 at 18 months to .89 at enrollment.
The Parental Stress Scale:Prematurely Born Child (PSS:PBC) measured stress related to parenting from 2 through 24 months.59 This scale includes 20 items, such as “getting my baby/child to sleep through the night,” and mothers rated the amount of stress caused by each item on a 5-point scale, ranging from “not at all stressful” to “extremely stressful.” Item scores are summed; possible scores range from 20 to 100. Internal consistency in this study ranged from .91 at 6 months to .93 at 2 and 24 months.
Procedures
The committees for protection of human subjects for the two study sites approved the study. Mothers were enrolled during infant hospitalization when their infants were no longer critically ill. Mothers provided informed consent for themselves and their infants. After enrollment, mothers completed questionnaires about their psychological distress and demographic characteristics. After the infant was discharged from the hospital, mothers completed questionnaires by mail at 2 months after term, during a home visit at 6 and 18 months, and during visits to the neonatal follow-up clinic at 12 and 24 months.
Data Analysis
To determine whether there were sub-groups of mothers based on patterns of psychological distress at enrollment, a latent class analysis (more accurately, a “latent profile analysis” since all indicators were continuous60) was conducted using the six distress measures at enrollment. We determined the number of latent classes by fitting models with different numbers of classes and comparing the Bayesian information criteria (BIC) and conducting Lo-Mendell-Rubin likelihood ratio tests between models;61 smaller absolute BIC values indicate better fit between the models and the observed data. Then, we added demographic and health-related characteristics to the model as covariates to determine whether any characteristic predicted class membership. We only included covariates in the final model if doing so resulted in an improved BIC value. Latent class analysis does not explicitly assign mothers to classes but rather estimates posterior class membership probabilities for each mother. For subsequent analyses, each mother was assumed to belong to the class with the highest posterior probability.
We examined whether the classes differed on psychological distress (depressive symptoms, state anxiety, post-traumatic stress symptoms, daily hassles), worry, and parenting stress from 2−24 months. To control for correlation between the repeated measurements on each subject, we used separate general linear mixed models with unstructured covariance structures to compare each distress measure between classes over time. The general linear mixed model is a flexible statistical procedure for analyzing continuous longitudinal data that accommodates missing values.62 Each model contained fixed effects for class, contact, and their interaction as well as randomization group. All tests were conducted using pre-specified contrasts at the two-sided 0.05 significance level. The distress variables were dichotomized based on published cut-off scores (depressive symptoms, state anxiety, post-traumatic stress symptoms) or medians at enrollment (daily hassles, worry) or 2 months (parenting stress) if no cut-off scores had been published. Then, the analyses were repeated using generalized estimating equations.63
RESULTS
Table 2 presents the inter-correlations of the six measures of maternal distress at enrollment. All measures were significantly correlated with each other. The highest correlations were for depressive symptoms with both state anxiety and post-traumatic stress symptoms, and the lowest was between infant appearance stress and daily hassles.
Table 2.
Pearson Correlation Coefficients between the Six Maternal Distress Measures for the 177 Mothers at Study Enrollment.
| Mean (SD) | Role Stress | Depr Sympt | State Anxiety | PTS Stress | Daily Hassles | |
|---|---|---|---|---|---|---|
| Infant Appear. Stress | 46.6 (18.9) | .62*** | .48*** | .39*** | .49*** | .33*** |
| Parental Role Stress | 32.5 (10.5) | .56*** | .45*** | .54*** | .36*** | |
| Depressive Symptoms | 19.8 (12.2) | .73*** | .73*** | .49*** | ||
| State Anxiety | 39.8 (13.6) | .55*** | .44*** | |||
| PTS Symptoms | 4.9 (3.6) | .46*** | ||||
| Daily Hassles | 24.7 (20.8) |
Note: Infant Appear. Stress = stress due to infant appearance and behavior in the NICU; PTS Symptoms = post-traumatic stress symptoms
p < .001
Latent Classes Based on Maternal Psychological Distress
The latent class analysis indicated that a model with four classes was most consistent with our data. The four-class model had lower BIC values than models with either three or five classes. A model with three classes would be rejected in favor of a model with four classes (p = .032) but a four-class model would not be rejected in favor of a model with five classes (p = .31) based on Lo-Mendell-Rubin likelihood ratio tests.
We named the latent classes based on the mean distress scores of mothers assigned to each class (Table 3). The 56 mothers assigned to the “low distress” class had, on average, low scores on all measures. The 49 mothers in the “high (NICU-related) stress” class showed high stress due to infant appearance and parental role alteration in the NICU and moderate scores on other measures. The 37 mothers in the “high depressive symptoms” class had high depressive symptoms and state anxiety and moderately elevated infant appearance stress, parental role stress, and post-traumatic stress scores. The 35 mothers in the “extreme distress” class had the highest means on all measures.
Table 3.
Means on the Six Maternal Distress Measures for the Four Classes at Enrollment
| Low Distress N = 56 |
High Stress N = 49 |
High Depress. N = 37 |
Extreme Distress N = 35 |
|
|---|---|---|---|---|
| Distress Measures | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) |
| Infant Appear. Stress | 29.6 (9.7) | 56.6 (13.3) | 40.5 (11.9) | 66.5 (15.3) |
| Parental Role Stress | 21.6 (7.6) | 37.3 (6.2) | 34.3 (7.2) | 41.6 (6.9) |
| Depressive Symptoms | 8.3 (4.8) | 15.7 (6.3) | 27.0 (6.2) | 36.4 (7.3) |
| State Anxiety | 28.1 (6.9) | 34.0 (8.0) | 50.6 (7.2) | 55.2 (9.7) |
| Post-Traumatic Stress | 1.6 (1.7) | 4.6 (3.1) | 6.0 (2.3) | 9.4 (2.0) |
| Daily Hassles | 13.0 (13.5) | 22.2 (14.8) | 24.6 (15.2) | 47.0 (25.4) |
Rate of Elevated Distress in Each Class
The distress variables were dichotomized based on published cut-off scores (depressive symptoms, state anxiety, post-traumatic stress symptoms) or medians at enrollment if no cut-off scores had been published (infant appearance stress, parental role alteration stress, daily hassles). Thirty-two mothers (all in the low distress class) had no elevated scores; 21 had elevated scores on all measures (1 in the high depressive symptoms and 20 in the extreme distress classes). A mean of 5.5 measures were elevated for the extreme distress class, 3.7 for the high depressive symptoms class, 2.9 for the high stress class, and 0.5 for the low distress class.
Table 4 shows the percent of each class with elevated scores on each distress measure. Mothers in the extreme distress class had elevated scores on virtually all measures; every mother had elevated depressive symptoms and post-traumatic stress symptoms. Mothers in the low distress class were unlikely to show elevated scores on any measure. Mothers in the other two classes had intermediate scores with the high depressive symptoms class mothers likely to show elevated scores on depressive symptoms, state anxiety, and post-traumatic stress symptoms. High (NICU-related) stress mothers were likely to show elevated scores on infant appearance stress and parental role alteration stress but were unlikely to show elevated state anxiety or post-traumatic stress symptoms. The differences among the groups on percent of mothers with and without elevated distress scores were significant (p < .001 for each distress measure).
Table 4.
Percent of Each Class Showing Elevated Scores on the Maternal Distress Measures at Enrollment
| Low Distress | High Stress | High Depress. | Extreme Distress | |
|---|---|---|---|---|
| Infant Appearance Stress | 8.9% | 79.5% | 32.4% | 94.2% |
| Parental Role Stress | 5.3% | 75.5% | 54.0% | 88.5% |
| Depressive Symptoms | 10.7% | 53.0% | 94.5% | 100.0% |
| State Anxiety | 1.7% | 4.0% | 70.2% | 74.2% |
| Post-Traumatic Stress Symptoms | 3.5% | 32.6% | 62.1% | 100.0% |
| Daily Hassles | 17.8% | 46.9% | 56.7% | 88.5% |
Class Differences on Maternal and Infant Characteristics
Table 5 shows the class differences on the demographic characteristics and illness variables. Mothers in the extreme distress class had lowest mean educational level. Infants in the high (NICU-related) stress class were the sickest: they averaged smaller birthweights, younger gestational ages, more neurological insults, and longer mechanical ventilation than infants in the other three classes and were more likely to have surgery, infection, and patent ductus arteriosis. The infants in the extreme distress class were the second sickest on these measures. The classes did not differ significantly on maternal age, parity, marital status, cesarean delivery, public assistance, infant gender, twin birth, or intraventricular hemorrhage.
Table 5.
Class Differences on Demographic Characteristics and Infant Illness Variables
| Low Distress Mean (SD) |
High Stress Mean (SD) |
High Depress. Mean (SD) |
Extreme Distress Mean (SD) |
|
|---|---|---|---|---|
| Maternal Age | 26.2 (6.5) | 26.4 (6.7) | 26.2 (6.3) | 24.2 (6.6) |
| Maternal Education In Years** | 12.9 (2.0) | 12.7 (1.9) | 13.0 (1.6) | 11.7 (1.3) |
| Maternal Marital Status | 34.5% | 26.5% | 24.3% | 14.2% |
| First-time Mothers | 33.9% | 22.4% | 16.2% | 28.5% |
| Cesarean Delivery | 48.2% | 46.9% | 62.9% | 62.8% |
| Public Assistance | 42.8% | 52.1% | 54.0% | 68.5% |
| Infant Gender: % Male | 37.5% | 48.9% | 35.1% | 48.3% |
| Twin Birth | 5.3% | 4.0% | 10.8% | 17.1% |
| Birthweight * | 1191 (421) | 1005 (395) | 1204 (367) | 1016 (331) |
| Gestational age * | 28.9 (2.9) | 27.5 (2.9) | 28.9 (2.7) | 28.0 (2.7) |
| Percent SGA | 16.0% | 24.4% | 18.9% | 28.5% |
| Mechanical Ventilation b *** | 7.9 (13.9) | 27.9 (35.8) | 7.4 (21.7) | 19.0 (24.9) |
| Intraventricular Hemorrhage | 21.5% | 22.5% | 19.4% | 28.6% |
| Neurological Insults a *** | 1.9 (2.1) | 4.2 (2.9) | 1.6 (2.3) | 3.3 (2.5) |
| Percent Surgery * | 14.2% | 38.7% | 19.4% | 25.7% |
| Percent Infections ** | 50.0% | 79.5% | 50.0% | 62.8% |
| Patent Ductus Arteriosis * | 28.5% | 48.9% | 27.8% | 54.2% |
Scored on the NBRS.58
Measured in days. Because this variable was highly skewed, it was transformed for analyses using a logarithmic transform.
p < .05.
p < .01.
p < .001.
When these characteristics were added as covariates to the latent class analysis, only maternal education, length of mechanical ventilation, and number of neurological insults improved the model fit. However, mechanical ventilation length and number of neurological insults were highly correlated (r = 0.70). Thus, the final model only included as covariates maternal education and mechanical ventilation length, but the latter is a proxy for overall infant health. Lower maternal education predicted membership in the extreme distress class, with an estimated odds ratio of 1.5 (95% CI 1.1−2.0) of belonging to the extreme distress class relative to the low distress class for every year less of education. Longer mechanical ventilation predicted membership in both the high stress and extreme distress classes relative to the low distress class, with each doubling in the number of days of ventilation (odds ratios of 1.6 [95% CI 1.2−2.1] and 1.3 [95% CI 1.0−1.6] for the high stress and extreme distress classes, respectively).
Class Differences in Maternal Distress over Time
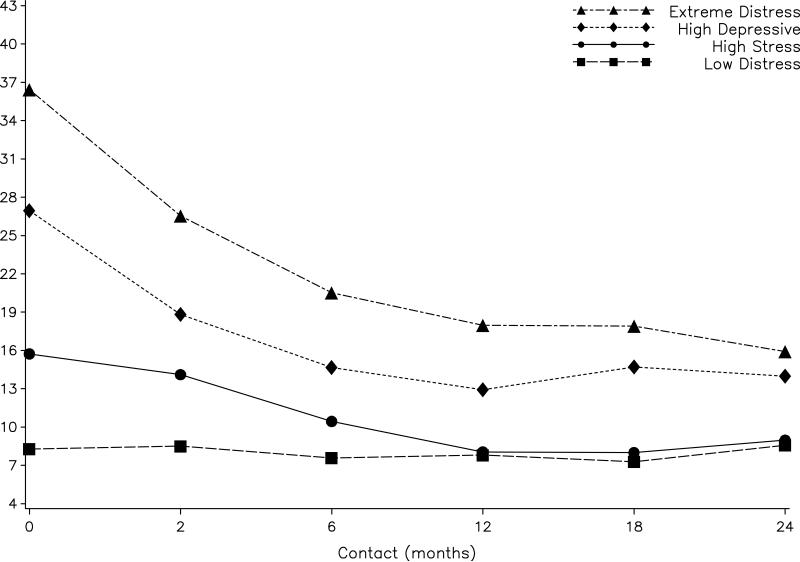
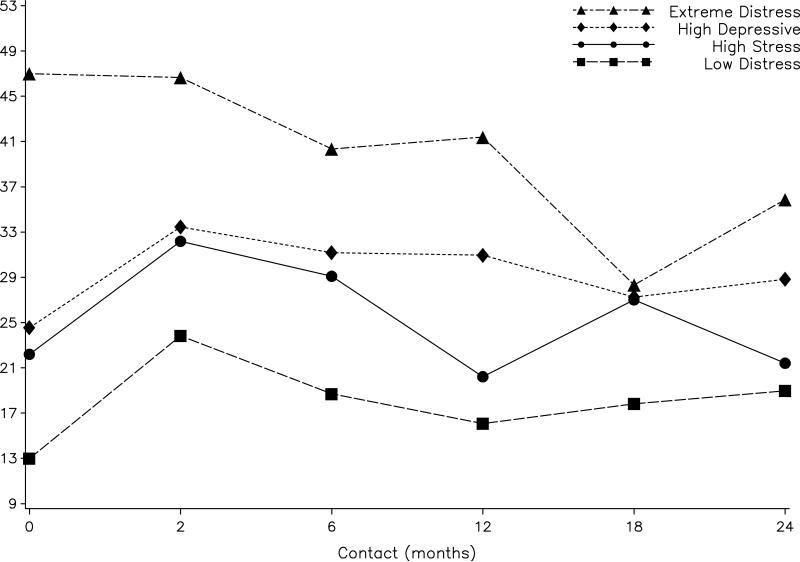
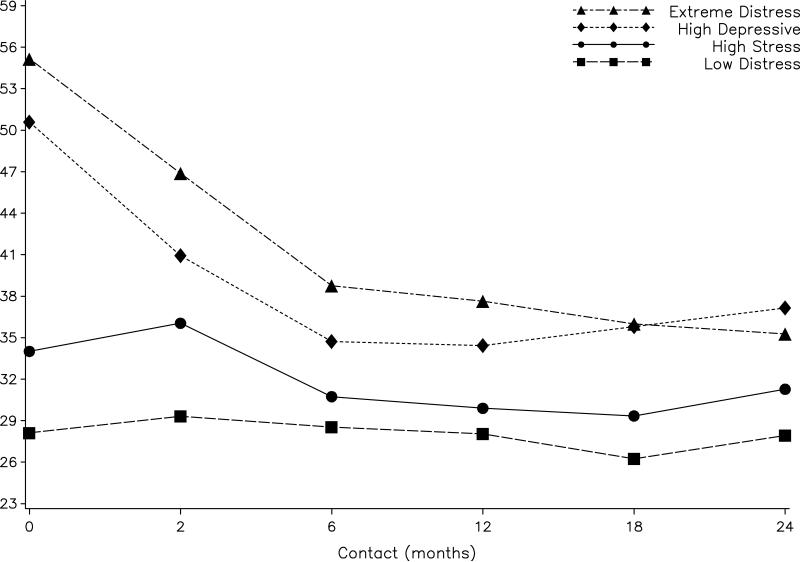
The classes significantly differed on all psychological distress variables, worry, and parenting stress from 2 to 24 months after term (see Figures 1, 2, 3, 4, 5, and 6). All classes, except the low distress, showed significant decreases in depressive symptoms and state anxiety over time (see Figures 1-2). Depressive symptoms averaged a decrease from enrollment to 24 months of almost 20 points for the extreme distress class (p < .001), 13 points for the high depressive class (p < .001), and 7 points for the high stress class (p < .001). State anxiety decreased from enrollment to 24 months an average of 19 points for the extreme distress class (p < .001) and 13 points for the high depressive class (p < .001). State anxiety decreased from enrollment to 12 months an average of 4 points in the high stress class (p = .037) but stabilized thereafter. The mean of the extreme distress class on depressive symptoms remained above 16 indicating high risk for depression at all contacts. From 6−24 months, the mean depressive symptoms and state anxiety of the low distress and high (NICU-related) stress classes did not differ significantly.
Figure 1.
Mean depression scores for the four classes of mothers over time.
Figure 2.
Mean state anxiety scores for the four classes of mothers over time.
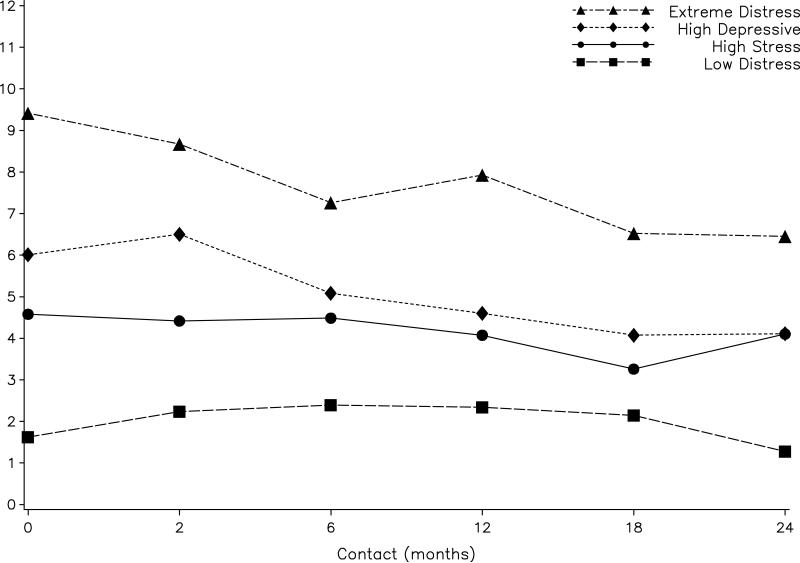
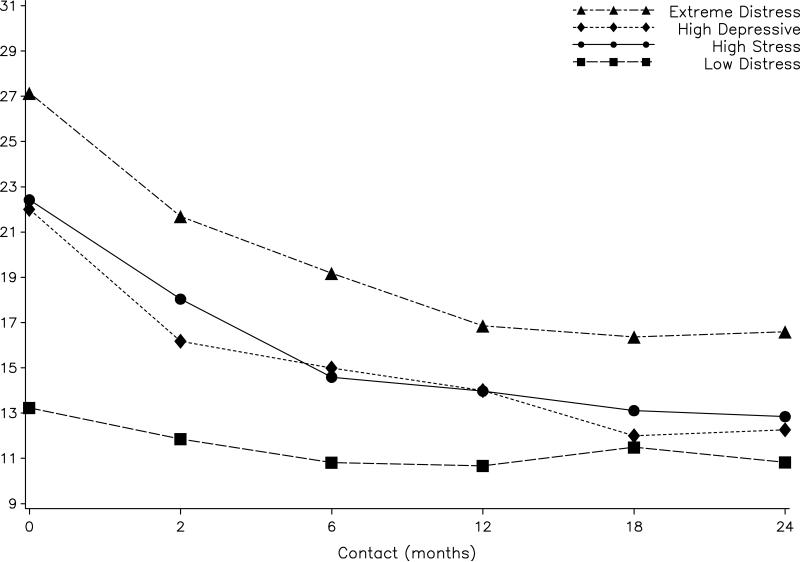
Figure 3.
Mean post-traumatic stress scores for the four classes of mothers over time.
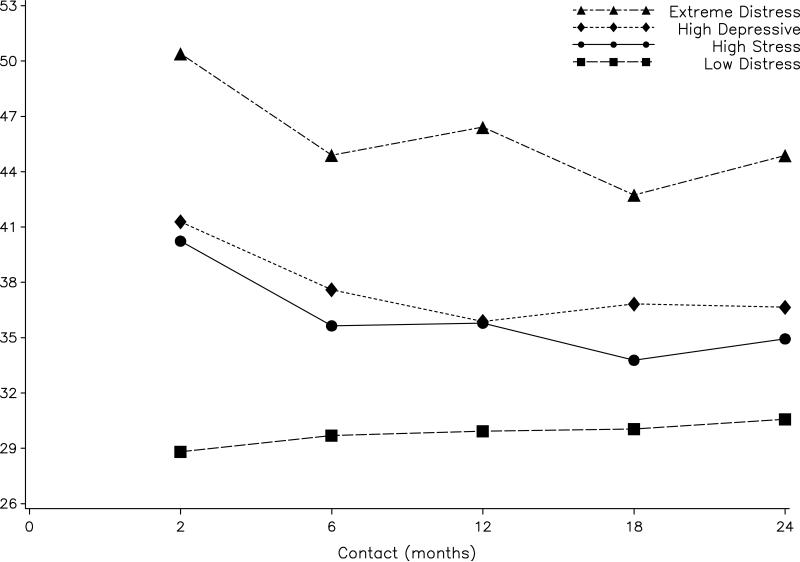
Figure 4.
Mean daily hassles scores for the four classes of mothers over time.
Figure 5.
Mean worry about the child for the four classes of mothers over time.
Figure 6.
Mean parenting stress scores for the four classes of mothers over time.
When analyses were repeated using the dichotomous depressive symptom variables, 44−57% of the extreme distress group had elevated depressive symptoms from 6−24 months as compared to 37−44% of the high depressive symptom class, 4−25% of the high stress class, and 10−18% of the low distress class (p = .002). In the dichotomous anxiety analyses, about 18−31% of the extreme distress group had elevated state anxiety scores from 6−24 months as compared to 6−16% of the high depressive symptom class and less than 5% of the other classes (p < .001).
Post-traumatic stress scores decreased significantly over age only for the high depressive symptom and extreme distress classes (see Figure 3). Post-traumatic stress averaged a decrease from enrollment to 24 months of almost 3 points in the extreme distress class (p < .001) and 2 points in the high depressive class (p = .005). However, the means of the extreme distress class remained above the cut-off point of 6 at all contacts. The low distress and high stress classes differed on post-traumatic stress symptoms at all ages (p < .003), but the high stress and high depressive symptoms classes did not differ significantly (p = .11). The dichotomous post-traumatic stress analysis indicated that 65% or more of the extreme distress class had elevated post-traumatic stress symptoms at each age; whereas the percent of the high depressive symptom class with elevated post-traumatic stress symptoms decreased from 59% at 2 months to 37% at 24 months, and roughly 25% of the high stress class and 11% or less of the low distress class had elevated post-traumatic stress symptoms at each age (p < .001).
Only the extreme distress class showed a significant decline over age in daily hassles (p = .023), but mean daily hassles scores of this class remained higher than the other three classes (p < .001; see Figure 4). From 2 to 24 months, mean daily hassles of the low distress and high (NICU-related) stress classes did not differ (p = .35); the high stress and high depressive symptoms classes also did not differ (p = .14). In the dichotomous daily hassles analyses, the percent of extreme distress mothers with elevated daily hassles scores decreased from 96% at enrollment to 72−77% at 6−24 months compared to about 50−69% of the high depressive symptom class and 25−50% of the other classes having elevated daily hassles scores (p < .001).
All classes showed significant decreases in worry about child health over time: an average decrease of 11 points for the extreme distress class (p < .001), 10 points for the high depressive class (p < .001), 9 points for the high stress class (p < .001), and 3 points for the low distress class (p = .008; see Figure 5). From 2−24 months, the high stress and high depressive symptoms classes did not differ (p = .82). In the dichotomous worry analyses, about 70−80% of the extreme distress group had elevated worry scores from 6 to 24 months as compared to 46−64% of the high depressive symptoms class, 17−41% of the high stress class, and about 16−27% of the low distress classes (p < .001).
Parenting stress showed a significant decrease for the extreme distress class (p < .01), but remained stable for the other three classes (all p < .20; see Figure 6). From 2−24 months, the mean parenting stress of the low distress and high stress classes did not differ (p = .20); the high stress and high depressive symptoms classes also did not differ (p = .90). In the dichotomous parenting stress analyses, about 70−85% of the extreme distress group had elevated parenting stress from 12 to 24 months as compared to 58−67% of the high depressive symptoms class and about 35% of the other two classes (p < .001).
DISCUSSION
We found that the six types of psychological distress experienced by African American mothers of preterm infants during hospitalization were inter-correlated. The patterns of distress, as represented by our four classes, differed primarily on degree of distress. However, the high NICU-related stress and high depressive symptoms classes had similar amounts of distress, but the mothers in the high stress class had greater stress due to infant appearance and parental role alteration probably because their infants were sicker than those in the high depressive class. These classes differed on types of distress experienced, rather than the amount of distress.
Importantly, we found that class membership determined in the NICU predicted psychological distress levels and perception of the infants and parenting over the first 24 months after term. Ours is the first study to show that there are distinct sub-groups of mothers with differing trajectories of distress in response to the hospitalization of a preterm infant. The extreme distress class had the highest mean scores on all variables through 24 months, the low distress class had the lowest mean scores, and the high depressive symptoms class had intermediate scores. The scores of the high (NICU-related) stress class started out similar to those of the high depressive symptoms class during hospitalization but rapidly declined as infant health improved so that by 6 months the depressive symptoms and state anxiety scores of this class did not differ from those of the low distress class. On the other hand, emotional responses more directly related to infant health--post-traumatic stress symptoms, worry, and parenting stress--remained similar to those of the high depressive symptoms cluster.
Thus, class membership provided information about the emotional responses of mothers in each class. For example, the class with the greatest distress, the extreme distress class, also had marked life stress due to high daily hassles and low educational levels. Other studies have found that mothers with low education show more emotional distress than other mothers of preterms.15, 18, 37 Even at 24 months, 56% of mothers in the extreme distress class had elevated depressive symptoms, 65% had elevated post-traumatic stress symptoms, 77% had elevated daily hassle scores, 76% had elevated worry scores, and 70% had elevated parenting stress scores. This prolonged emotional distress is concerning because chronically distressed mothers have been found to be more bothered by infant behaviors, to have poorer perceptions of their children, to be less responsive to their children, and to report less attachment to them.18, 23, 24, 28, 64-68 As a result, elevated maternal distress is related to poor child development in both prematures and fullterms.6, 10, 23, 41, 68-70 Given the chronicity of the distress in extreme distress class of mothers and despite the fact their infants were the second sickest, their distress is likely to be due as much to ongoing, but undiagnosed, mental health issues as to responses to prematurity. Mothers with combination of high levels of psychological distress and high daily hassles may need a more intensive mental health intervention than standard NICU parental support.
By contrast, the mothers in the low distress class showed low levels of distress at all time points that were similar to levels found in the general population.44-46, 51 Thus, the responses to prematurity of the mothers in this class did not appear to have long-lasting consequences.
Overall, the trajectories of maternal psychological distress in our study were similar to those found in previous studies. Most classes showed significant declines over time in distress measures except for the low distress class, which already had low scores. Previous studies have found that maternal psychological distress is highest during hospitalization and then decreases over the first year after birth,4, 6, 14, 17, 40 probably due to decreasing maternal distress as infant medical conditions improve. Our finding of four distinct classes of mothers with different trajectories of distress probably explains the finding that despite group trends indicating that maternal distress is high during hospitalization, decreases over time, and returns to normal by 6 months, most individual mothers do not show this pattern.4
An exception to the finding of decreasing distress over time was the daily hassles score, which only showed declines over time for the extreme distress class. This lack of change in daily hassles for most classes was not surprising since daily hassles are part of the mother's ongoing lives55, 56 and are not likely to be affected by improvements in infant medical condition. Interestedly, both daily hassles and parenting stress showed a slight peak at 2 months for most classes. This is similar to findings that mothers show increased distress when they take premature infants home and assume responsibility for their care.14, 71-73 Thus, both future research and clinical interventions need to focus on maternal support needs in the immediate post-hospital discharge period.
Several factors may limit the generalizability of this study. First, the mothers in our study represented a sample of convenience, as is typically the case in randomized studies. Thus, the statistical inferences should not be generalized beyond the study population. We are the first to identify specific latent classes of African American mothers, and this finding needs to be replicated. Also, we excluded the sickest infants, those hospitalized for longer than 2 months after term so the trajectory of distress for the mothers of these infants is unknown. However, these infants make up only a very small percentage of preterm infants treated in NICUs. Finally, we only studied African American mothers from rural and small town areas in one southeastern state. Future research is needed to determine whether mothers of other ethnicities and from other localities show similar patterns of distress because studies have sometimes found that African American mothers of premature infants show higher levels of distress than mothers of other ethnicities8-10 and depression rates are higher in women living in rural states.74 However, because African American mothers’ distress in response to prematurity has generally been found to be similar to that of White mothers,8-10, 30, 31 similar sub-groups will most likely be identified in other ethnicities though the proportion of mothers classified into each may vary.
In conclusion, despite significant inter-correlations among different types of maternal psychological distress in the NICU, we found there were four distinct classes of African American mothers of premature infants who differed both on the severity of their initial distress in the hospital and on their trajectories of distress over the first 24 month after term. Mothers in these four classes would probably respond differently to interventions to reduce their distress. Importantly, mothers in these sub-groups can be identified while their infants are still hospitalized in the NICU based on current psychological distress levels, maternal education, and infant illness severity. Mothers with sick infants, low educational elves, and high distress--especially depressive symptoms, post-traumatic stress symptoms, and daily hassles--are at high risk for chronic distress and need intensive mental health interventions that continue after infant discharge. By contrast, the distress of mothers of equally sick infants without socioeconomic risks or elevated state anxiety or post-traumatic stress symptoms should decrease as infants’ medical conditions improve. These mothers primarily need supportive interventions. The needs of mothers with less ill infants depend on their levels of distress. Mothers with low levels of distress in the NICU should continue to have low distress after their infants leave the hospital; whereas mothers with elevated depressive symptoms may need more active interventions to prevent them from becoming part of the more than third of the high depressive symptoms group that had chronically elevated depressive symptoms. Professionals conducting mental health or supportive interventions with African American mothers of preterm infants need to consider not only the severity of the distress experienced by the mothers but also their patterns of distress.
Acknowledgments
This study was supported by Grant R01 NR035962 from the National Institute for Nursing Research, NIH.
We wish to thank Janice Werezczak, Carol Hubbard, Michael Belyea, Paula Anderson, Martha Ferebee, Donna Harris, Zhaowei Hua, James Gregory Lewis, HyeKyun Rhee, Donna Smart, William Wooten, and Tara Wright for technical assistance.
Contributor Information
Diane Holditch-Davis, School of Nursing, Duke University, Durham, NC, USA.
Margaret Shandor Miles, School of Nursing, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
Mark A. Weaver, Family Health International, Durham, NC, USA.
Stephen Engelke, Division of Neonatology, Department of Pediatrics, School of Medicine, East Carolina University, Greenville, NC, USA.
REFERENCES
- 1.Black BP, Holditch-Davis D, Miles MS. Life Course Theory as a framework to examine becoming a mother of a medically fragile preterm infant. Res Nursing Health. doi: 10.1002/nur.20298. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Callahan JL, Hynan MT. Identifying mothers at risk for postnatal emotional distress: Further evidence for the validity of the perinatal posttraumatic stress disorder questionnaire. J Perinatol. 2002;22(6):448–454. doi: 10.1038/sj.jp.7210783. [DOI] [PubMed] [Google Scholar]
- 3.Holditch-Davis D, Bartlett TR, Blickman A, et al. Post-traumatic stress symptoms in mothers of premature infants. J Obstetr Gynecol Neonatal Nurs. 2003;32:161–171. doi: 10.1177/0884217503252035. [DOI] [PubMed] [Google Scholar]
- 4.Miles MS, Holditch-Davis D, Scher M, et al. A longitudinal study of depressive symptoms in mothers of prematurely born infants. J Dev Behav Pediatr. 2007;28(1):36–44. doi: 10.1097/01.DBP.0000257517.52459.7a. [DOI] [PubMed] [Google Scholar]
- 5.Pierrehumbert B, Nicole A, Muller-Nix C, et al. Parental post-traumatic reactions after premature birth: Implications for sleeping and eating problems in the infant. Arch Dis Child Fetal Neonatal Ed. 2003;88:F400–F404. doi: 10.1136/fn.88.5.F400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singer LT, Salvatore A, Guo S, et al. Maternal psychological distress and parenting stress after the birth of a very low-birth-weight infant. JAMA. 1999;281:799–805. doi: 10.1001/jama.281.9.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ashton D. Prematurity--infant mortality: The scourge remains. Ethn Dis. 2006;16(2 Suppl 3):S3–S58. S62. [PubMed] [Google Scholar]
- 8.Miles MS, Holditch-Davis D, Brunssen S, et al. Perceptions of stress, worry, and support in Black and White mothers of hospitalized medically fragile infants. J Pediatr Nurs. 2002;17:82–88. doi: 10.1053/jpdn.2002.124125. [DOI] [PubMed] [Google Scholar]
- 9.Miles MS, Wilson S, Docherty S. African American mothers’ response to a chronically ill infant. Neonatal Netw. 2000;18(8):17–25. doi: 10.1891/0730-0832.18.8.17. [DOI] [PubMed] [Google Scholar]
- 10.Thompson RJ, Gustafson KE, Oehler JM, et al. Developmental outcome of very low birth weight infants at four years of age as a function of biological risk and psychosocial risk. J Dev Behav Pediatr. 1997;18:91–96. doi: 10.1097/00004703-199704000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Franck LS, Cox S, Allen A, et al. Measuring neonatal intensive care unit-related parental stress. J Adv Nurs. 2005;49(6):608–615. doi: 10.1111/j.1365-2648.2004.03336.x. [DOI] [PubMed] [Google Scholar]
- 12.Miles MS, Funk SG, Carlson J. Parental Stressor Scale: Neonatal Intensive Care Unit. Nurs Res. 1993;42:148–152. [PubMed] [Google Scholar]
- 13.Miles MS, Funk S, Kasper MA. The stress response of mothers and fathers of preterm infants. Res Nurs Health. 1992;15:261–269. doi: 10.1002/nur.4770150405. [DOI] [PubMed] [Google Scholar]
- 14.Brooten D, Gennaro S, Brown LP, et al. Anxiety, depression, and hostility in mothers of preterm infants. Nurs Res. 1988;37:213–216. [PubMed] [Google Scholar]
- 15.Davis L, Edwards H, Mohay H, et al. The impact of very premature birth on the psychological health of mothers. Early Hum Dev. 2003;73(1−2):61–70. doi: 10.1016/s0378-3782(03)00073-2. [DOI] [PubMed] [Google Scholar]
- 16.Feldman R, Eidelman AI. Maternal postpartum behavior and the emergences of infant-mother and infant-father synchrony in preterm and fullterm infants: The role of neonatal vagal tone. Dev Psychobiol. 2007;49:290–302. doi: 10.1002/dev.20220. [DOI] [PubMed] [Google Scholar]
- 17.Mew AM, Holditch-Davis D, Belyea M, et al. Correlates of depressive symptoms in mothers of preterm infants. Neonatal Netw. 2003;22(5):51–60. doi: 10.1891/0730-0832.22.5.51. [DOI] [PubMed] [Google Scholar]
- 18.Zelkowitz P, Bardin C, Papageorgiou A. Anxiety affects the relationship between parents and their very low birth weight infants. Infant Mental Health J. 2007;28(3):296–313. doi: 10.1002/imhj.20137. [DOI] [PubMed] [Google Scholar]
- 19.Garel M, Dardennes M, Blondel B. Mothers’ psychological distress 1 year after very preterm childbirth. Results of the EPIPAGE qualitative study. Child Care Health Dev. 2007;33(2):137–143. doi: 10.1111/j.1365-2214.2006.00663.x. [DOI] [PubMed] [Google Scholar]
- 20.Reichman SRF, Miller AC, Gordon RM, et al. Stress appraisal and coping in mothers of NICU infants. Child Health Care. 2000;29:279–293. [Google Scholar]
- 21.Holditch-Davis D, Miles MS. Mothers’ stories about their experiences in the neonatal intensive unit. Neonatal Netw. 2000;19(3):13–21. doi: 10.1891/0730-0832.19.3.13. [DOI] [PubMed] [Google Scholar]
- 22.DeMier RL, Hynan MT, Hatfield RF, et al. A measurement model of perinatal stressors: Identifying risk for postnatal emotional distress in mothers of high-risk infants. J Clin Psychol. 2000;56:89–100. doi: 10.1002/(sici)1097-4679(200001)56:1<89::aid-jclp8>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 23.Allen EC, Manuel JC, Legault C, et al. Perception of child vulnerability among mothers of former premature infants. Pediatrics. 2004;113(2):267–273. doi: 10.1542/peds.113.2.267. [DOI] [PubMed] [Google Scholar]
- 24.Feeley N, Gottlieb L, Zelkowitz P. Infant, mother, and contextual predictors of mother-very low birth weight infant interaction at 9 months of age. J Dev Behav Pediatr. 2005;26:24–33. [PubMed] [Google Scholar]
- 25.Holditch-Davis D, Schwartz T, Black B, et al. Correlates of mother-premature infant interactions. Res Nurs Health. 2007;30:333–346. doi: 10.1002/nur.20190. [DOI] [PubMed] [Google Scholar]
- 26.Miles MS, Holditch-Davis D. Compensatory parenting: How mothers describe parenting their 3-year-old prematurely born children. J Pediatr Nurs. 1995;10:243–253. doi: 10.1016/s0882-5963(05)80021-1. [DOI] [PubMed] [Google Scholar]
- 27.Muller-Nix C, Forcada-Guex M, Pierrehumbert B, et al. Prematurity, maternal stress and mother-child interactions. Early Hum Dev. 2004;79:145–158. doi: 10.1016/j.earlhumdev.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 28.Singer LT, Fulton S, Davillier M, et al. Effects of infant risk status and maternal psychological distress on maternal-infant interactions during the first year of life. J Dev Behav Pediatr. 2003;24:233–241. doi: 10.1097/00004703-200308000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moran G, Pederson DR. Proneness to distress and ambivalent relationships. Infant Behav Dev. 1998;21:493–503. [Google Scholar]
- 30.Doering LV, Moser DK, Dracup K. Correlates of anxiety, hostility, depression, and psychosocial adjustment in parents of NICU infants. Neonatal Netw. 2000;19(5):15–23. doi: 10.1891/0730-0832.19.5.15. [DOI] [PubMed] [Google Scholar]
- 31.Lau C, Hurst NM, Smith EO, et al. Ethnic/racial diversity, maternal stress, lactation and very low birthweight infants. J Perinatol. 2007;27(7):399–408. doi: 10.1038/sj.jp.7211770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mandl KD, Tronick EZ, Brennan TA, et al. Infant health care use and maternal depression. Arch Pediatr Adolesc Med. 1999;153:808–813. doi: 10.1001/archpedi.153.8.808. [DOI] [PubMed] [Google Scholar]
- 33.Sawyer L, Regev H, Proctor S, et al. Matching versus cultural competence in research: Methodological considerations. Res Nurs Health. 1995;18:557–567. doi: 10.1002/nur.4770180611. [DOI] [PubMed] [Google Scholar]
- 34.Yoos HL, Kitzman H, Olds DL, et al. Child rearing beliefs in the African-American community: Implications for culturally competent pediatric care. J Pediatr Nurs. 1995;10:343–353. doi: 10.1016/S0882-5963(05)80031-4. [DOI] [PubMed] [Google Scholar]
- 35.Dickerson BJ. Black Single Mothers: Understanding Their Lives and Families. Sage; Thousand Oaks, CA: 1995. [Google Scholar]
- 36.Wilson MN. The context of the African American family. In: Everett JE, Chipungu SS, Leashore BR, editors. Child Welfare: An Afrocentric Perspective. Rutgers University; New Brunswick, NJ: 1991. pp. 85–118. [Google Scholar]
- 37.Blanchard LW, Blalock SJ, DeVellis RF, et al. Social comparisons among mothers of premature and full-term infants. Child Health Care. 1999;28:329–348. [Google Scholar]
- 38.Beeghly M, Olson K, Weinberg MK, et al. Prevalence, stability, and socio-demographic correlates of depressive symptoms in Black mothers during the first 18 months postpartum. Matern Child Health J. 2003;7(3):157–168. doi: 10.1023/a:1025132320321. [DOI] [PubMed] [Google Scholar]
- 39.Brody GH, Murry VM, Kim S, et al. Longitudinal pathways to competence and psychological adjustment among African American children living in rural single-parent households. Child Dev. 2002;73(5):1505–1516. doi: 10.1111/1467-8624.00486. [DOI] [PubMed] [Google Scholar]
- 40.O'Brien M, Asay JH, McCluskey-Fawcett K. Family functioning and maternal depression following premature birth. J Reprod Infant Psychol. 1999;17:175–188. [Google Scholar]
- 41.Liaw FR, Brooks-Gunn J. Cumulative familial risks and low-birthweight children's cognitive and behavioral development. J Clin Child Psychol. 1994;23:360–372. [Google Scholar]
- 42.Miles MS, Funk SG, Kasper MA. The neonatal intensive care unit environment: Sources of stress for parents. AACN Clin Iss Crit Care Nurs. 1991;2:346–354. doi: 10.4037/15597768-1991-2022. [DOI] [PubMed] [Google Scholar]
- 43.Nadeau L, Boivin M, Tessier R, et al. Mediators of behavioral problems in 7-year-old children born after 24 to 28 weeks of gestation. J Dev Behav Pediatr. 2001;22:1–10. doi: 10.1097/00004703-200102000-00001. [DOI] [PubMed] [Google Scholar]
- 44.Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 45.Myers JK, Weissman MM. Psychiatric disorders and their treatment: A community survey. Med Care. 1980;18(1):117–123. doi: 10.1097/00005650-198001000-00009. [DOI] [PubMed] [Google Scholar]
- 46.Roberts RE, Vernon SW. The Center for Epidemiologic Studies Depression Scale: Its use in a community sample. Am J Psychiatry. 1983;140(1):41–46. doi: 10.1176/ajp.140.1.41. [DOI] [PubMed] [Google Scholar]
- 47.Weissman MM, Sholomskas D, Pottenger M, et al. Assessing depressive symptoms in five psychiatric populations: A validation study. Am J Epidemiol. 1977;106:203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- 48.Miles MS, Holditch-Davis D, Burchinal M, et al. Distress and growth in mothers of medically fragile infants. Nurs Res. 1999;48:129–140. doi: 10.1097/00006199-199905000-00003. [DOI] [PubMed] [Google Scholar]
- 49.Holditch-Davis D, Miles MS, Burchinal M, et al. Parental caregiving and developmental outcomes in infants of mothers with HIV. Nurs Res. 2001;50:5–14. doi: 10.1097/00006199-200101000-00003. [DOI] [PubMed] [Google Scholar]
- 50.Miles MS, Burchinal P, Holditch-Davis D, et al. Personal, family, and health related correlates of depressive symptoms in mothers with HIV. J Fam Psychol. 1997;11:23–34. [Google Scholar]
- 51.Spielberger CD, Gorusch RL, Lushene R, et al. Manual for the State/Trait Anxiety Inventory (Form Y) Consulting Psychologist; Palo Alto: 1983. [Google Scholar]
- 52.Miles MS, Carlson J, Funk S. Sources of support reported by mothers and fathers of infants hospitalized in a neonatal intensive care unit. Neonatal Netw. 1996;15(3):45–54. [PubMed] [Google Scholar]
- 53.DeMier RL, Hynan MT, Harris HB, et al. Perinatal stressors as predictors of symptoms of posttraumatic stress disorder in mothers of infants at high risk. J Perinatal. 1996;16:276–280. [PubMed] [Google Scholar]
- 54.Quinnell FA, Hynan MT. Convergent and discriminant validity of the Perinatal PTSD Questionnaire (PPQ): A preliminary study. J Trauma Stress. 1999;12:193–199. doi: 10.1023/A:1024714903950. [DOI] [PubMed] [Google Scholar]
- 55.Delongis A, Folkman S, Lazarus RS. Hassles, health and mood: A prospective study with repeated daily assessments. J Pers Soc Psychol. 1988;54:486–495. doi: 10.1037//0022-3514.54.3.486. [DOI] [PubMed] [Google Scholar]
- 56.Kanner AD, Coyne JC, Schaefer C, et al. Comparison of two modes of stress measurement: Daily hassles and uplifts versus major life events. J Behav Med. 1981;4:1–39. doi: 10.1007/BF00844845. [DOI] [PubMed] [Google Scholar]
- 57.Ballard JL, Khoury JC, Wedig K, et al. New Ballard Score expanded to included extremely premature infants. J Pediatr. 1991;119:417–23. doi: 10.1016/s0022-3476(05)82056-6. [DOI] [PubMed] [Google Scholar]
- 58.Brazy J, Goldstein R, Oehler JM, et al. Nursery Neurobiologic Risk Score: Levels of risk and relationships with nonmedical factors. J Dev Behav Pediatr. 1993;14:375–380. [PubMed] [Google Scholar]
- 59.Holditch-Davis D, Miles MS. Grant # NR01894 Report to the National Institute for Nursing Research, NIH. 2003. Assessment of biological and social risk in preterm infants. [Google Scholar]
- 60.Muthén BO. Beyond SEM: General latent variable modeling. Behaviormetrika. 2002;29:81–117. [Google Scholar]
- 61.Lo YT, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. [Google Scholar]
- 62.Holditch-Davis D, Edwards L, Helms R. Modeling development of sleep-wake behaviors: I. Using the mixed general linear model. Physiol Behav. 1998;63(3):311–318. doi: 10.1016/s0031-9384(97)00459-9. [DOI] [PubMed] [Google Scholar]
- 63.Zeger SL, Liang KY, Albert PS. Models for longitudinal data: A generalized estimating equation approach. Biometrics. 1988;44:1049–1060. [PubMed] [Google Scholar]
- 64.Donovan WL, Leavitt LA, Walsh RO. Conflict and depression predict maternal sensitivity to infant cries. Infant Behav Dev. 1998;21:505–517. [Google Scholar]
- 65.Feldman R, Weldman J, Leckman JF, et al. The nature of the mother's tie to her infant: Maternal bonding under conditions of proximity, separation, and potential loss. J Child Psychol Psychiatr. 1999;40:929–939. [PubMed] [Google Scholar]
- 66.Kaplan P, Bachorowski JA, Zarlengo-Strose P. Child-directed speech produced by mothers with symptoms of depression fails to promote associative learning in 4-month-old infants. Child Dev. 1999;70:560–570. doi: 10.1111/1467-8624.00041. [DOI] [PubMed] [Google Scholar]
- 67.McLearn KT, Minkowitz CS, Strobino DM, et al. Maternal depressive symptoms at 2 to 4 months post partum and early parenting practices. Arch Pediatr Adolesc Med. 2006;160(3):279–284. doi: 10.1001/archpedi.160.3.279. [DOI] [PubMed] [Google Scholar]
- 68.Wong ST. The relationship between parent emotion, parent behavior, and health status of young African American and Latino children. J Pediatr Nurs. 2006;21(6):434–442. doi: 10.1016/j.pedn.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 69.National Institute of Child and Human Development Early Child Care Network Chronicity of maternal depressive symptoms, maternal sensitivity, and child functioning at 36 weeks. Dev Psychol. 1999;35:1297–1310. doi: 10.1037//0012-1649.35.5.1297. [DOI] [PubMed] [Google Scholar]
- 70.Onufrak B, Saylor CF, Taylor MJ, et al. Determinants of responsiveness of mothers of children with intraventricular hemorrhage. J Pediatr Psychol. 1995;20:587–599. doi: 10.1093/jpepsy/20.5.587. [DOI] [PubMed] [Google Scholar]
- 71.Butts PA, Brooten D, Brown L, et al. Concerns of parents of low birthweight infants following hospital discharge: a report of parent-initiated telephone calls. Neonatal Netw. 1988;7(2):37–42. [PubMed] [Google Scholar]
- 72.Pederson DR, Bento S, Chance GW, et al. Maternal emotional responses to preterm birth. Am J Orthopsychiatr. 1987;57:15–21. doi: 10.1111/j.1939-0025.1987.tb03504.x. [DOI] [PubMed] [Google Scholar]
- 73.Thompson RJ, Oehler JM, Catlett AT, et al. Maternal psychological adjustment to the birth of an infant weighing 1,500 grams or less. Infant Behav Dev. 1993;16:471–485. [Google Scholar]
- 74.Lanzi RG, Pascoe JM, Keltner B, et al. Correlates of maternal depression symptoms in a national Head Start program sample. Arch Pediatr Adolesc Med. 1999;153:801–807. doi: 10.1001/archpedi.153.8.801. [DOI] [PubMed] [Google Scholar]