Abstract
Background
The purpose of this study was to determine the incidence of and identify risk factors for post-operative hypothyroidism in patients undergoing thyroid lobectomy.
Methods
We retrospectively reviewed patients who underwent a thyroid lobectomy for benign disease from May 2004 to December 2007. Patients with known hypothyroidism or on preoperative thyroid hormone replacement were excluded.
Results
In this study, 14.3% of patients developed hypothyroidism and required thyroid hormone supplementation. These hypothyroid patients had a higher mean pre-operative TSH and lower mean free T4 serum levels compared to euthyroid patients (TSH: 2.12 vs. 1.35 µIU/ml, P=0.006; free T4: 1.03 vs. 1.34 ng/dl, P=0.01, respectively). When stratified into three groups based on their pre-operative TSH measurement (≤ 1.5, 1.51 – 2.5, and ≥ 2.51 µIU/ml), the rate of hypothyroidism increased significantly at each level (13.5%, 20.5%, and 41.3%, respectively, P<0.001). In addition, patients with Hashimoto’s thyroiditis were significantly more likely to become hypothyroid (OR 3.78, 95% CI 2.17 – 6.60).
Conclusion
Following thyroid lobectomy, approximately 1 in 7 patients will experience hypothyroidism requiring thyroid hormone treatment. Patients with pre-operative TSH levels > 1.5 µIU/ml, lower free T4 levels, and Hashimoto’s thyroiditis are at increased risk and should be counseled and followed appropriately.
Keywords: Thyroid lobectomy, hemithyroidectomy, hypothyroidism, risk factors
Background
Thyroid lobectomy or hemithyroidectomy is a frequently performed procedure that is indicated in patients with a variety of thyroid conditions, both benign and malignant (1). Risks and complications following a thyroid lobectomy include among others hypothyroidism, seroma or hematoma formation, injury to the recurrent or superior laryngeal nerves, and rarely infection (2). Traditionally, routine post-operative thyroid hormone replacement with L-thyroxine or levothyroxine was given to suppress the development of additional nodular disease in the thyroid remnant (3–6). However, this customary practice has fallen out of favor at some institutions since many patients will not require supplemental thyroid hormone. While thyroid hormone replacement is required after total thyroidectomy, it is not clear when, and if, thyroid hormone should be administered after unilateral thyroid lobectomy. Theoretically, one thyroid lobe should possess enough functioning thyrocytes for a patient to remain euthyroid. In fact, many surgeons and patients opt for unilateral thyroid resection due to the belief that post-operative thyroid hormone therapy will not be required. However, patients with reduced thyroid function pre-operatively may not have sufficient thyroid tissue remaining after thyroid lobectomy (7).
Patients with hypothyroidism can develop weight gain, fatigue and sleepiness. Patients who develop hypothyroidism following thyroid lobectomy will require life-long thyroid hormone replacement, as well as routine laboratory investigations and medication adjustments. Furthermore, adverse effects of chronic L-thyroxine may occur such as arrythmias (atrial fibrillation) or loss of calcium in the bones resulting osteopenia or osteoporosis. An increased ability to recognize which patients are most at risk for developing hypothyroidism will improve patient care. Therefore, the objectives of this study were to determine the incidence of hypothyroidism in a large cohort and identify risk factors for post-operative thyroid hormone replacement in patients undergoing thyroid lobectomy for benign disease.
Methods
We retrospectively reviewed all patients (n=671) who underwent a thyroid lobectomy from May 2004 to December 2007 at the University of Wisconsin Hospital and Clinics. Patients with a malignancy (n=107) or pre-operative hypothyroidism (n=17) were excluded. Patients with hyperthyroidism were included. Pre-operative hypothyroidism was defined as patients with known diagnosed hypothyroidism, patients on pre-operative thyroid hormone treatment for any reason, or patients with a baseline TSH above the upper limit of normal at our institution (normal TSH range 0.34–4.82 µIU/ml). The number of patients in this group may appear lower because we do not treat patients with nodular disease and normal TSH levels with thyroid hormone. Therefore, the number of patient on pre-operative thyroid hormone replacement is lower than in other series where this is done. Thyroid lobectomy was considered to be the resection of either the right or left thyroid lobe with isthmusectomy. A TSH level was measured in all patients approximately 6 to 8 weeks after surgery during routine follow-up. Post-operative hypothyroidism was defined as a serum TSH level greater than the upper limit of normal (4.82 µIU/ml) measured at least 6 weeks after surgery. Diagnoses of Hashimoto’s thyroiditis and goiter were confirmed by pathology. In addition, thyroid nodule size and resected gland weight were obtained from pathological review. Patients were additionally stratified into three groups based on their pre-operative TSH levels in order to determine the probability of developing hypothyroidism in each group. These groups were defined by TSH levels ≤ 1.5, 1.51 – 2.50, and > 2.5 µIU/ml. The median follow-up was 32 months (range 12–54 months).
This study was approved by the University of Wisconsin Human Subjects Institutional Review Board. The statistical analysis of the differences between hypothyroid and euthyroid patients was performed by 2-sided Fisher’s exact test and unpaired t tests using the SPSS statistical software version 10.0 (SPSS Corporation, Chicago, IL). Odds ratios (OR) with 95% confidence intervals (CI) were determined and used to assess risk. ANOVA with Bonferroni post-hoc correction was used for sub-analysis of the three pre-operative TSH levels. Statistical significance was defined as a P<0.05. Data are shown as mean ± standard error of the mean (SEM).
Results
We identified 547 patients who underwent a thyroid lobectomy for benign disease at the University of Wisconsin during the study period. Following thyroid lobectomy, 78 of 547 patients (14.3%) required post-operative thyroid hormone replacement. The mean age of the total patients studied was 50 ± 1 years, and the majority (80%) was female (Table 1). No significant differences existed between hypothyroid and euthyroid patients in terms of age (Table 1). More hypothyroid patients tended be female, though this difference was not statistically significance (89% vs. 78%, P= 0.06; OR = 2.03 (95% CI 0.98 – 4.20).
Table 1.
Patient Demographics
| Total | Hypothyroid | Euthyroid | P value | |
|---|---|---|---|---|
| Number (%) | 547 | 78 (14) | 469 (86) | --- |
| Age* | 50 ± 1 | 52 ± 2 | 49 ± 1 | 0.13 |
| Sex, Female (%) | 440 (80) | 69 (89) | 371 (79) | 0.06 |
Data are expressed as mean ± SEM
Analysis of the laboratory values of the patients confirmed that hypothyroid patients had a significantly higher mean pre-operative TSH level compared to euthyroid patients (2.12 vs. 1.35 µIU/ml, P=0.006). Patients who developed hypothyroidism also had a lower mean preoperative T4 level (1.03 vs. 1.34 ng/dl, P=0.01; normal 0.7 – 1.8 ng/dl). Post-operatively we additionally examined the difference in mean calcium levels between these 2 groups of patients which were found to be similar (P=0.56, Table 2).
Table 2.
Comparison of Laboratory Values between Hypo- and Euthyroid Patients
| Hypothyroid (n=78) |
Euthyroid (n=469) |
P value | |
|---|---|---|---|
| Pre-operative | |||
| Serum TSH (µIU/ml) | 2.12 ± 0.26 | 1.35 ± 0.07 | 0.006 |
| Serum free thyroxine (T4, ng/dl) | 1.03 ± 0.07 | 1.34 ± 0.10 | 0.01 |
| Post-operative | |||
| Serum calcium (mg/dl) | 8.9 ± 0.10 | 8.9 ± 0.05 | 0.56 |
Data are expressed as mean ± SEM, TSH: thyroid stimulating hormone
Several patient factors also were analyzed for their prognostic value. Hypothyroid patients had a significantly higher rate of Hashimoto’s thyroiditis than euthyroid patients (32% vs. 11%, P<0.001, Table 3). This relationship was such that patients with Hashimoto’s thyroiditis were nearly four times more likely to require post-operative thyroid hormone replacement therapy (OR = 3.78, 95% CI 2.17 – 6.60). Hypothyroid and euthyroid patients were similar with respect to a history of previous thyroid surgery or neck dissection (Table 3). Furthermore, no statistical differences were observed between the two groups based on the presence of a goiter, the size of the nodule removed, or the resected gland weight (Table 3).
Table 3.
Comparison of Patient Factors between Hypo- and Euthryoid Patients
| Hypothyroid (n=78) |
Euthyroid (n=469) |
P value | |
|---|---|---|---|
| History of thyroid surgery (%) | 2 (2.5) | 7 (1.5) | 0.62 |
| Previous Neck Dissection (%) | 1 (1.3) | 6 (1.3) | 1.00 |
| Goiter (%) | 27 (35) | 154 (32) | 0.70 |
| Hashimoto’s Thyroiditis (%) | 25 (32) | 52 (11) | 0.001 |
| Nodule Size (cm)* | 3.0 ± 0.2 | 2.8 ± 0.1 | 0.60 |
| Gland Weight (gm)* | 32 ± 5 | 27 ± 2 | 0.21 |
Data are expressed as mean ± SEM
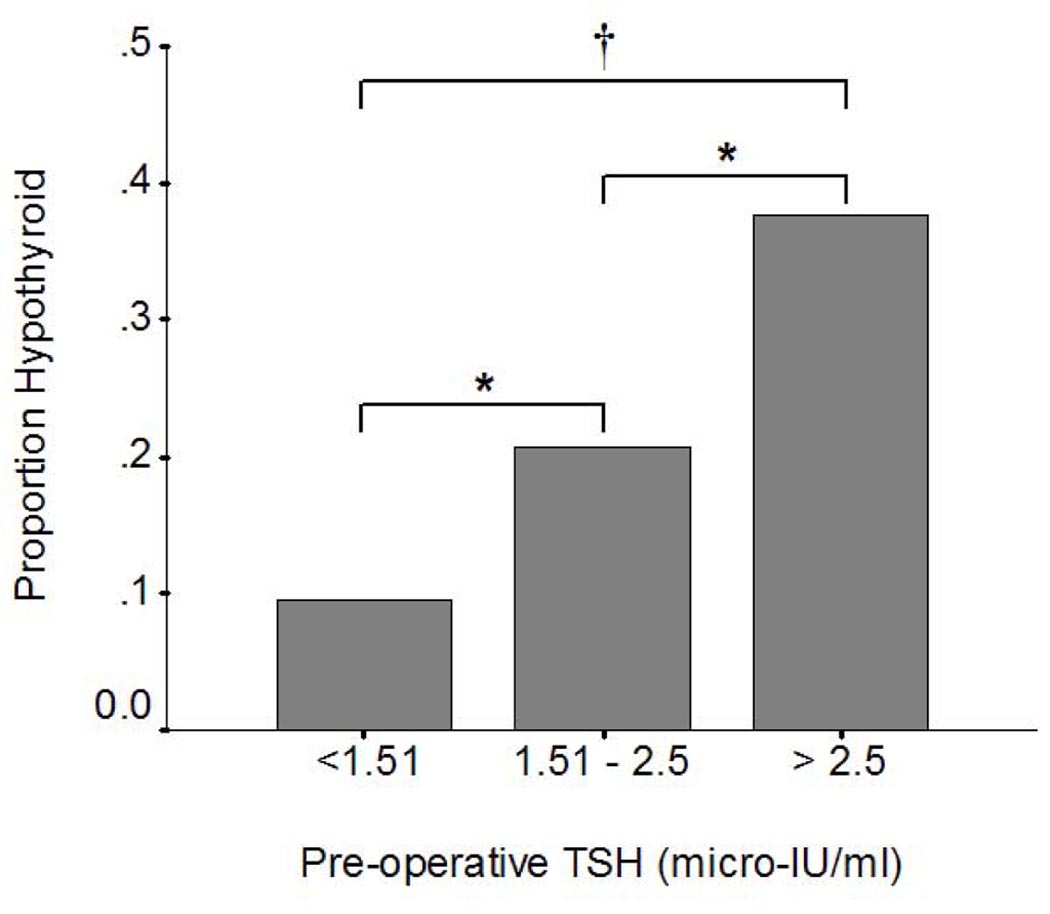
In order to identify a TSH level where the proportion of patients were more likely to require post-operative thyroid hormone replacement, the patients were stratified into three groups based on their pre-operative TSH levels (≤1.5, 1.51 – 2.50, or > 2.5 µIU/ml). When stratified by pre-operative TSH levels, 13.5% patients with TSH levels <1.5 µIU/ml, 20.5% of patients with a TSH between 1.51 – 2.50 µIU/ml, and 41.3% of patients with a TSH >2.5 µIU/ml developed hypothyroidism that required post-operative thyroid hormone replacement (p<0.0001 by ANOVA). Figure 1 demonstrates that the differences in the rate of hypothyroidism between each group of patients were statistically significant. With each increasing level of pre-operative TSH, a significantly larger proportion of patients required thyroid hormone replacement after thyroid lobectomy. For patients with a TSH ≤ 1.5 µIU/ml, the percentage that became hypothyroid (13.5%) was similar to the study population as a whole (14.3%).
Figure 1.
When stratified by pre-operative TSH levels, patients with a TSH > 2.5 µIU/mL (41%) were most likely to need post-operative thyroid hormone replacement followed by patients with a TSH from 1.51 – 2.5 µIU/mL (21%). Compared to patients with TSH levels ≤ 1.5 µIU/mL of whom 14% became hypothyroid this increased incidence was significant (*P<0.05; †P<0.0001 by ANOVA Bonferroni post-hoc correction).
Discussion
This study was designed to assess the rate of and identify factors for the development of hypothyroidism following thyroid lobectomy. While all patients undergoing total thyroidectomy require life-long thyroid hormone replacement, only a proportion of patients will have the same need after a lobectomy. Defining the risks of hypothyroidism development is crucial in order to develop better pre-operative counseling, management strategies, and follow-up for patients undergoing this procedure. We found that 14.3% of patients required thyroid hormone replacement after undergoing a thyroid lobectomy for benign disease. The variables that were significantly increased in hypothyroid patients were a higher mean pre-operative TSH, a lower pre-operative T4 level, and the presence of Hashimoto’s thyroiditis. Specifically, patients with a pre-operative TSH level > 1.5 µIU/mL had a higher proportion of hypothyroidism development. Furthermore, female sex may also be potential risk factors for hypothyroidism post-thyroid lobectomy, although this factor only trended toward statistical significance.
Previously reported rates of hypothyroidism after thyroid lobectomy or hemithyroidectomy range from 5% to 49%, with most between 15% and 30% (7–14). In the largest reported study with 1051 patients who underwent hemithyroidectomy, 28% of patients required thyroid hormone supplementation post-operatively, but 6% of the patients included were hypothyroid prior to surgery (13). This incidence varies largely depending upon how hypothyroidism was defined and the length follow-up (2, 9, 12, 14–16). The incidence of hypothyroidism requiring post-operative thyroid hormone replacement in our study of 14% falls within this reported range, but at the lower end. Our data may have underestimated the true incidence of post-operative hypothyroidism in this patient population because participants were screened at 6 to 8 weeks after lobectomy. With our median follow-up of 32 months, it is likely that more patients will develop hypothyroidism with time. The incidence of hypothyroidism increases with age in the normal population. In other studies, the mean time to the diagnosis of hypothyroidism has been 5 to 7 months and up to 38% of patients have taken 6 or more months to develop this complication (9, 11, 14). On the other hand, Piper et al. reported that 92% of patients were diagnosed by 8 weeks (12). Another reason that our incidence of hypothyroidism following thyroid lobectomy may be lower than other reports is that our biochemical definition of hypothyroidism only identified those patients with a TSH that was elevated as opposed to patients who were treated with thyroid hormone in the absence of laboratory abnormalities. In a study by Koh et al., of the 43% of patients with hypothyroidism, 19% had overt hypothyroidism, whereas 81% had subclinical disease (9).
When we examined the pre-operative laboratory values of the patients, those patients who developed hypothyroidism after thyroid lobectomy had higher TSH levels and lower free T4 levels than their euthyroid counterparts (Table 2). Of note, these levels were still within the normal reference ranges of our laboratory. Several studies also have reported that patients who become hypothyroid have “higher normal” pre-operative TSH levels (8–11, 14, 16, 17). However, to the best of our knowledge, the result of lower free T4 levels in hypothyroid patients has not been previously shown, perhaps because this laboratory value is not routinely measured. Due to the inverse relationship of TSH and T4 levels, the finding that the hypothyroid group had lower free T4 levels before surgery is not surprising. Other pre-operative measurements that may be increased in patients who are hypothyroid following lobectomy are thyroglobulin and thyroperoxidase (microsomal) antibodies (8, 9, 15).
Further examination of TSH values in this study revealed a significantly increased rate of hypothyroidism in patients with pre-operative TSH levels from 1.51 to 2.5 µIU/ml and an even higher rate in patients with TSH levels >2.5 µIU/L when evaluated against patients with levels ≤1.5 µIU/ml. Recently both Moon and Wormald described that an elevated TSH level was an independent risk factor for the development of hypothyroidism following thyroid lobectomy (14, 16). In addition, studies that have used one cutoff value such as a TSH level >1.6 or >2.0 µIU/ml have found that patients are 7–10 times more likely to develop hypothyroidism following surgery (8, 14). When these results are considered together, “normal elevated” pre-operative TSH levels >1.5 µIU/ml, especially when seen with lower pre-operative T4 levels or specific antibodies, should alert the surgeon to a potential increased risk of hypothyroidism following thyroid lobectomy with appropriate pre-operative counseling of patients.
In addition to an elevated pre-operative TSH and a decreased T4 measurement, we found that Hashimoto’s thyroiditis was another factor that increased the need for thyroid hormone supplementation. This diagnosis resulted in patients being almost four times more likely to develop hypothyroidism after thyroid lobectomy. Hashimoto’s thyroiditis is an inflammatory disease that is the most common cause of hypothyroidism in the United States, and is found more frequently in females (18). Additionally, Hashimoto’s thyroiditis is characterized by intense lymphocytic infiltration of the thyroid and the presence of thyroid auto-antibodies. Other investigations have found a similar relationship between either Hashimoto’s thyroiditis, the degree of lymphocytic infiltration, the presence of chronic inflammation, or detectable thyroid auto-antibodies and hypothyroidism following lobectomy (9, 11, 12, 14, 15, 17). The association among the presence of Hashimoto’s thyroiditis, a “normal elevated” TSH, a low free T4, and thyroid auto-antibodies is likely due to the underlying pathologic disease process. When we retrospectively compared the pre-operative labs of patients with and without Hashimoto’s thyroidits, we discovered that patients with this diagnosis had significantly higher mean TSH levels and lower free T4 levels (TSH: 2.25 ± 0.31 vs 1.19 ± 0.06 µIU/ml, P<0.001; free T4: 0.53 ± 0.08 vs 1.57 ± 0.01 ng/dl, P=0.29). Awareness that Hashimoto’s thyroiditis and these additional factors significantly increase the risk of developing post-operative hypothyroidism following thyroid lobectomy is an important tool in counseling patients regarding their chances of needing thyroid hormone replacement therapy in the future.
While patients with hypothyroidism had equivalent resected gland weights in this and other studies, a smaller remnant volume as measured by ultrasound has been recognized as a risk factor for hypothyroidism (14, 16, 17). Of the other patient variables that we investigated that were not related to the development of hypothyroidism (age, history of thyroid surgery or neck dissection, goiter presence, and nodule size), only patients with the diagnosis of a multinodular goiter have been shown to have a higher risk for the occurrence of hypothyroidism (11). The results of the present study are limited by the retrospective design and the lack of analysis of certain factors such as thyroid auto-antibodies and remnant volume. In addition, our definition of and screening for hypothyroidism after lobectomy may have excluded some patients with subclinical disease or a longer time course to the development of disease. Adequate postoperative screening for hypothyroidism may need to continue for at least 12 months post-surgery with a heightened awareness for patients reporting symptoms consistent with an underactive thyroid.
Interpretation of these results and the related literature has several practical implications in the clinical setting. A pre-operative TSH level >1.5 µIU/ml, a lower pre-operative free T4 level, and/or known Hashimoto’s thyroiditis, especially in a female patient, should alert the clinician that the likelihood of developing hypothyroidism requiring thyroid hormone supplementation after a thyroid lobectomy is significantly increased. The incidence of hypothyroidism is not negligible following thyroid lobectomy, but may not be as high as previously reported. Patients with an increased potential for post-operative hypothyroidism must be made aware of their risk factors and undergo more intensive follow-up.
Acknowledgments
This study was funded in part by the American College of Surgeons Resident Research Scholarship, and NIH grants T32 CA009614 and T35 DK062709-03.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented at the 66th Annual Meeting of the Central Surgical Association, Sarasota FL, March 5–7, 2009
References
- 1.Mittendorf E, McHenry C. Thyroidectomy for selected patients with thyrotoxicosis. Arch Otolaryngol Head Neck Surg. 2001 Jan;127(1):61–65. doi: 10.1001/archotol.127.1.61. [DOI] [PubMed] [Google Scholar]
- 2.Fewins J, Simpson C, Miller F. Complications of thyroid and parathyroid surgery. Otolaryngol Clin North Am. 2003 Feb;36(1):189–206. doi: 10.1016/s0030-6665(02)00129-9. x. [DOI] [PubMed] [Google Scholar]
- 3.Bergfelt G, Risholm L. Postoperative thyroid hormone therapy in nontoxic goitre. Acta Chir Scand. 1963 Dec;126:531–537. [PubMed] [Google Scholar]
- 4.Berglund J, Bondesson L, Christensen S, Larsson A, Tibblin S. Indications for thyroxine therapy after surgery for nontoxic benign goitre. Acta Chir Scand. 156(6–7):433–438. [PubMed] [Google Scholar]
- 5.Hedman I, Jansson S, Lindberg S. Need for thyroxine in patients lobectomised for benign thyroid disease as assessed by follow-up on average fifteen years after surgery. Acta Chir Scand. 152:481–486. [PubMed] [Google Scholar]
- 6.Hegedüs L, Hansen J, Veiergang D, Karstrup S. Does prophylactic thyroxine treatment after operation for non-toxic goitre influence thyroid size? Br Med J (Clin Res Ed) 1987 Mar;294(6575):801–803. doi: 10.1136/bmj.294.6575.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Farkas E, King T, Bolton J, Fuhrman G. A comparison of total thyroidectomy and lobectomy in the treatment of dominant thyroid nodules. Am Surg. 2002 Aug;68(8):678–682. discussion 82-3. [PubMed] [Google Scholar]
- 8.De Carlucci DJ, Tavares M, Obara M, Martins L, Hojaij F, Cernea C. Thyroid function after unilateral total lobectomy: risk factors for postoperative hypothyroidism. Arch Otolaryngol Head Neck Surg. 2008 Oct;134(10):1076–1079. doi: 10.1001/archotol.134.10.1076. [DOI] [PubMed] [Google Scholar]
- 9.Koh Y, Lee S, Choi E, Lee J, Mok J, Kim H, et al. Prediction of hypothyroidism after hemithyroidectomy: a biochemical and pathological analysis. Eur Arch Otorhinolaryngol. 2000 Apr;265(4):453–457. doi: 10.1007/s00405-007-0513-8. [DOI] [PubMed] [Google Scholar]
- 10.McHenry C, Slusarczyk S. Hypothyroidisim following hemithyroidectomy: incidence, risk factors, and management. Surgery. 2000 Dec;128(6):994–998. doi: 10.1067/msy.2000.110242. [DOI] [PubMed] [Google Scholar]
- 11.Miller F, Paulson D, Prihoda T, Otto R. Risk factors for the development of hypothyroidism after hemithyroidectomy. Arch Otolaryngol Head Neck Surg. 2006 Jan;132(1):36–38. doi: 10.1001/archotol.132.1.36. [DOI] [PubMed] [Google Scholar]
- 12.Piper H, Bugis S, Wilkins G, Walker B, Wiseman S, Baliski C. Detecting and defining hypothyroidism after hemithyroidectomy. Am J Surg. 2005 May;189(5):587–591. doi: 10.1016/j.amjsurg.2005.01.038. discussion 91. [DOI] [PubMed] [Google Scholar]
- 13.Vaiman M, Nagibin A, Hagag P, Kessler A, Gavriel H. Hypothyroidism following partial thyroidectomy. Otolaryngol Head Neck Surg. 2008 Jan;138(1):98–100. doi: 10.1016/j.otohns.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 14.Wormald R, Sheahan P, Rowley S, Rizkalla H, Toner M, Timon C. Hemithyroidectomy for benign thyroid disease: who needs follow-up for hypothyroidism? Clin Otolaryngol. 2008 Dec;33(6):587–591. doi: 10.1111/j.1749-4486.2008.01794.x. [DOI] [PubMed] [Google Scholar]
- 15.Buchanan M, Lee D. Thyroid auto-antibodies, lymphocytic infiltration and the development of post-operative hypothyroidism following hemithyroidectomy for non-toxic nodular goitre. J R Coll Surg Edinb. 2001 Apr;46(2):86–90. [PubMed] [Google Scholar]
- 16.Moon H, Jung E, Park S, Jung T, Jeong C, Ju Y, et al. Thyrotropin level and thyroid volume for prediction of hypothyroidism following hemithyroidectomy in an Asian patient cohort. World J Surg. 2008 Nov;32(11):2503–2508. doi: 10.1007/s00268-008-9717-3. [DOI] [PubMed] [Google Scholar]
- 17.Seiberling K, Dutra J, Bajaramovic S. Hypothyroidism following hemithyroidectomy for benign nontoxic thyroid disease. Ear Nose Throat J. 2007 May;86(5):295–299. [PubMed] [Google Scholar]
- 18.Repplinger D, Bargren A, Zhang Y, Adler J, Haymart M, Chen H. Is Hashimoto's thyroiditis a risk factor for papillary thyroid cancer? J Surg Res. 2008 Nov;150(1):49–52. doi: 10.1016/j.jss.2007.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]