Abstract
Objectives
To assess the feasibility and acceptability of studying whole systems of Traditional Chinese Medicine (TCM) and Naturopathic medicine (NM) in the treatment of temporomandibular disorders (TMD), and to determine whether there is indication to support further research.
Design
A pilot study using a randomized controlled clinical trial design of whole system TCM and NM versus state-of-the-art specialty care (SC).
Setting/location
Kaiser Permanente Northwest (KPNW), and practitioner offices in Portland, Oregon.
Subjects
One hundred and sixty (160) women 25–55 years of age attending a KPNW TMD specialty clinic.
Interventions
Whole system TCM and NM, and KPNW TMD clinic SC; the intervention protocols were designed to model the individually tailored type of community care offered in alternative medicine practices in Portland and in the KPNW TMD clinic, using protocols that enhanced similarities among practitioners within each system and permitted full descriptions of the treatments provided.
Outcome measures
TMD was ascertained using the Research Diagnostic Criteria/TMD; outcomes were self-reported worst and average facial pain and interference with activities (scaled 0–10 where 10 is worst).
Results
Of 948 consecutive eligible patients, 160 were randomized to one of three arms; 128 provided endpoint data. TCM and NM demonstrated significantly greater in-treatment reductions for worst facial pain compared to SC (adjusted regression analysis; higher negative values indicate greater improvement, = −1.11 ± 0.43, p = 0.010 and −1.02 ± 0.45, p = 0.025 for TCM and NM, respectively, compared to SC) and at 3 months post-treatment (−1.07 ± 0.51, p = 0.037 and −1.27 ± 0.54, p = 0.019 for TCM and NM versus SC, respectively). Additionally, TCM provided significantly greater decreases in average pain than SC; NM provided significantly greater decreases than SC or TCM in TMD-related psychosocial interference.
Conclusions
These alternative medicine approaches each resulted in significantly greater reduction of pain and psychosocial interference than SC. Further research on the potential benefits of traditional whole systems of medicine for TMD appears warranted.
Introduction
Chronic pain in the temporomandibular joint (TMJ) and/or masticatory muscles affects more than 10% of adults at any one time, and one-third of adults will experience symptoms of temporomandibular joint dysfunction (TMD) over their lifespan.1 Longitudinal data suggest that TMDs are a group of enduring or recurrent conditions that for many patients are resistant to treatment.2,3 TMD affects individuals across all socioeconomic and ethnic groups.4 In a study of TMD patients in Kaiser Permanente Northwest (KPNW) in 1990–1995, the mean age was 40.5 years, and 80% of the patients were female; the TMD patients used 1.6 times the services of other health plan members.5
Pain relief is the primary therapeutic objective of TMD treatments.6–9 Common conventional treatments include anti-inflammatory, analgesic, antidepressant, and other medications used for chronic pain; intra-oral occlusal appliances; physiotherapy; occlusal equilibration and reconstruction; TMJ surgery; arthroscopy; and biobehavioral treatments such as biofeedback, hypnosis, cognitive-behavioral therapy, and education. TMD signs and symptoms, however, have been found to be virtually independent of extent of the treatment sought over a 5-year period.10 Based on findings from several long-term epidemiologic and clinical case studies, TMD, like other chronic pain conditions, seems best characterized as self-limiting or nonprogressive with regard to the physical disease aspects of the condition(s). Thus, no overarching evidence-based rationale for selecting among TMD treatments has emerged.11 Two recent surveys have documented the relatively frequent concurrent use of complementary and alternative medicine (CAM) and conventional therapies by patients with TMD.12,13 In light of the limited successes of usual care in treating TMD, and because TMD is a chronic, recurring, relatively poorly defined group of conditions, it is important to explore the management of these conditions with alternative approaches to health care. One recent paper reporting on a pilot study of shamanic healing for TMD suggests that alternate approaches may have value.14
The goals of this randomized trial pilot study were to evaluate the feasibility and acceptability of randomized trials of whole systems of alternative medicine care for TMD, and to establish whether there was sufficient benefit from these approaches to warrant further research. A further goal was to develop methods for studying complex systems of alternative care for TMD. Two whole systems of care were selected for comparison to standard KPNW specialty care (SC) (see below) on the basis of the proximate location of academic institutions of Traditional Chinese Medicine (TCM) and Naturopathic medicine (NM), skilled practitioners, high local utilization and, for one of the systems (TCM), some existing evidence.
TCM practice encompasses acupuncture, herbal therapy, massage (tuina), and breathing and relaxation exercises (qigong and t'ai chi). Among these approaches, acupuncture has received the most attention in the treatment of TMD. Systematic reviews of acupuncture for TMD15,16 each identified the same six reports that met the criteria for randomized controlled trials (RCT), although these represented only three separate trials. Although all three trials demonstrated that acupuncture was at least as effective as usual care (mainly occlusal splint therapy), none was performed with blinded evaluators. More recently, there have been two case series17,18 and two RCTs19,20 assessing effectiveness of acupuncture for TMD, with all four studies favoring acupuncture. Of the RCTs, the study from China reported that acupuncture plus ultrasound therapy outperformed ultra shortwave electrotherapy19 while the UK-based pilot study found verum acupuncture to outperform sham acupuncture for reducing myofascial pain.20
NM is a system of medicine that facilitates the restoration of health and well-being by following a set of principles designed to bring an individual back to a state of balance. The core intent of naturopathic practice is to address the underlying causes of ill health by treating the whole person in a way that supports each individual's own internal power of self-healing. Naturopathic doctors may draw upon several therapeutic modalities, including herbal medicine, nutritional supplements, physical medicine, homeopathy, and bio-identical hormone therapies; and benefit is suggested for some of the components of NM practice.21 Because the goal is to promote lifelong health and well-being, treatments are not prescribed as an end in themselves, but within a framework that fosters the patient's development of optimal lifestyle behaviors such as good nutritional habits, appropriate level and type of exercise, and stress-reduction skills. There are no previous published studies of NM as a whole system of practice for TMD. In fact, there are few treatments designated specifically for TMD within the naturopathic canon because it takes a holistic and individualized approach to patient care.22 Understanding an individual patient's level of stress and patterns of reactivity is considered fundamental to developing a treatment program that supports lifelong health and well-being. Given the potential link between stress-based hypothalamic-pituitary-adrenal (HPA) axis dysregulation and TMD, benefit has been suggested for some constituents of practice in the setting of other chronic pain syndromes. The results of clinical studies that report improved adrenal gland function (i.e., HPA axis function) using nutrient and herbal supplements suggest the potential effectiveness of an NM approach for this group of TMD patients.23,24
The present study was the first National Center for Complementary and Alternative Medicine–funded trial of whole systems of complementary and alternative medicine.25 It aimed to evaluate the appropriateness of and prepare for larger-scale evaluation of whole system TCM and NM including developing recruitment protocols, endpoint assessment tools and protocols, compliance and adherence strategies, details of treatment and resource utilization, as well as characterizing patterns of response. Furthermore, the project evaluated the potential for developing whole system (multicomponent) protocols within TCM and NM that would allow the medicine to be tailored to each individual patient in ways that were faithful to the practice of the medicine and were reproducible. In this way, this project differed from many pragmatic trials in which the practitioner decisions and treatments delivered were essentially treated as a “black box.” The project and all procedures were approved by the KPNW Committee for the Protection of Human Subjects, by the Institutional Review Boards of the Oregon College of Oriental Medicine, and the National College of Natural (formerly Naturopathic) Medicine, and by the center grant Data and Safety Monitoring Board.
Materials and Methods
Setting
The study was based in the Center for Health Research at KPNW, a group model health maintenance organization, which includes a dental plan. KPNW provides coverage for TMD treatment to all health plan members through a TMD referral specialty clinic staffed by two dentists specializing in TMD treatment. TMD patients in this study were treated at the KPNW TMD Clinic or at private practice sites for TCM or NM.
Population, recruitment, and randomization
The study population consisted of women 25–55 years of age. Eligibility criteria included the presence of concomitant diagnoses of multiple chronic systemic health problems and/or chronic fatigue and fibromyalgia as determined through the electronic health record. Exclusion criteria included factors that would prevent full participation in the study, including expecting to move, major psychiatric illness, and life-threatening medical conditions such as cancer. Participants were screened electronically and recruited at the time of referral to the TMD clinic, prior to their first specialty clinic visit, 2001–2003. Those who expressed interest in the study then provided informed consent, and went through a second assessment process, the Research Diagnostic Criteria (RDC/TMD) examination.26 If criteria for a TMD diagnosis were met, patients completed all baseline questionnaires and were then randomized to (1) continued treatment in the SC clinic; (2) TCM; or (3) NM. There was no eligibility criterion for pain level per se. Participants were assigned to their treatment groups based on the values of their balancing factors at baseline, using a design-adaptive allocation program with randomization, which was managed solely by the project biostatistician. Balancing factors were assessed in an initial questionnaire, and included age, depression, smoking, and any prior use of CAM.27,28 Project managers notified participants of their assignments; subsequently, all assessors were blinded to treatment assignment.
Intervention protocols
A whole-systems approach was used in designing the CAM interventions.29 TCM and NM clinicians and investigators collaboratively developed treatment protocols for each CAM intervention arm. These protocols were developed from literature reviews as well as community best practices, based on input from study practitioners and outside experts, with the intention of maintaining the theoretical perspective of each system of care. Next, the protocols were converted to study practitioner written guidelines that specified treatment parameters (see below). Most importantly, in both arms, practitioners were to treat all aspects of the patient, not just the TMD, in a manner consistent with their medical systems. The two complementary and alternative medicine interventions were designed to be matched to each other in total contact time (9–10 hours total) and intervention time frame (3–4 months). In practice, however, the time frame for the TCM arm extended to 5–6 months and for the NM arm to 8 months.
Traditional Chinese Medicine
The TCM arm consisted of an initial 1-hour assessment visit and 19 one-half-hour treatments. Treatment guidelines targeted visits twice per week for 6 weeks, then once per week for 8 weeks. Each treatment included insertion of up to 20 acupuncture needles, an herbal prescription, tuina, and relaxation tapes as appropriate. The two practitioners had both been trained in China at Nanjing University, had both practiced more than 5 years, and were both faculty members at Oregon College of Oriental Medicine. They identified the TCM diagnoses of the patients, and for each diagnosis, acupuncture points, and herbs were specified by protocol (see Appendix 1, columns 1–3). Additional acupuncture points were recommended based on the brief literature on acupuncture treatment for TMD (ST7 and/or ST6, GB20 and/or GB21, yintang, LI4, LV3).16 Finally, optional points and herbs were available for use in common acute conditions, such as allergies, upper respiratory infections, or back strain (see Appendix 1, columns 4–5). Most participants had multiple TCM diagnosis; in these cases, practitioners focused on the primary diagnosis and used the optional points and herbs to address these variations. All needles were 1–2 inches, 32–36 gauge, single-use, disposable needles inserted between 0.25 inch and 1.25 inches depending on the point. Each was inserted using an even method and retained for 20–30 minutes. A maximum of 18 needles were used in any one treatment. All points were inserted perpendicularly unless counterindicated by the point. The practitioner assessed the participant's TCM diagnosis at every visit and was allowed to change diagnoses as the patient presented. Tuina was focused primarily on the neck and shoulders, based on clinical assessment of tightness and patient indication of local pain. Relaxation tapes were provided to all participants.
Naturopathic medicine
Similar to the TCM arm, the NM protocol was designed to be internally consistent with naturopathic philosophy. A total of 9½ hours of contact were scheduled, with the first session 90 minutes, and subsequent visits 1 hour. The original protocol suggested that these be completed in 4 months; in practice, the additional time was needed because the NM protocol involved more lifestyle changes and the practitioners wanted a longer period to assess whether those changes were feasible and/or successful for the participant. The two NM practitioners were trained at NCNM and each had at least 4 years of experience with women's health and pain conditions. The initial visit included an in-depth history focusing on liver function, the adrenal system, the digestive system, and the immune system with particular attention given to the role and impact of stress. The naturopathic physicians then selected appropriate therapies from within practice guidelines they developed based on experience with similar patients, and vetted with clinician faculty at National College of Natural Medicine, with the goal to support healing and restore balance. Treatment for all participants included a Foundational packet consisting of a multimineral/multivitamin supplement, antioxidants, and a liver support formula. In addition, all participants received individualized nutritional and stress reduction recommendations. Physical medicine given by the practitioners was included in every session to provide a “hands-on” experience to partially balance this aspect of the acupuncture intervention. Details are provided in Appendix 2. Exercise recommendations were also emphasized for individual patients, with a view to promoting long-term health and well-being. Standardized protocols and patient handouts were developed for each modality, and all herbal and nutritional supplements were dispensed by a single medicinary. In addition to stress reduction techniques, participants were guided on how to become aware of and better cope with circumstances and thought patterns that triggered their TMD symptoms. When considered clinically necessary, the NM practitioners directly ordered laboratory testing for hormone profiles (e.g., salivary cortisol, DHEA-S, estradiol, progesterone, and testosterone [from ZRT Laboratory, Beaverton, OR]), and recommended participants arrange blood screening tests (e.g., complete blood count, chemistry screens) with their Kaiser Permanente (KP) physicians. Blood screening tests were ordered this way because they were covered by participants' KP benefits, but results were interpreted by the N.D.s. Patients were allocated six months of supplements and herbs, but allowed to stretch their active treatment period to eight months when individual circumstances warranted the extension. Practitioners met monthly to discuss patients and continue to calibrate their treatment decisions.
Specialty care
The SC arm utilized SC provided at the TMD clinic by two dentists who specialized in TMD treatment. All SC participants were provided two 2-hour class sessions on the basics of TMD, including etiology, prognosis, available treatments, and self-care strategies. Bite splints, individual counseling about self-care methods, and pain management strategies were provided by the TMD specialists who delivered care from a strong biopsychosocial perspective. Referrals were possible for physical therapy (including specialized massage), and psychologic and counseling support. Beyond the class, the pace of treatment and number and type of modalities pursued were up to the patient and practitioner. The SC treatment provided was documented after the completion of the study through a review of patient charts in the electronic medical record system.
Measures
Four measures of chronic TMD pain drawn from the RDC/TMD graded chronic pain scale were the basis for the results reported here: 1. Worst facial pain; 2. Average facial pain, when the participant was having pain; 3. effect of pain on activities of daily living; and 4. effect of pain on social activities.25
The original schedule called for measurements at 3, 6, 9, and 12 months. However, as the time frame over which treatments were delivered lengthened, and difficulties in collecting endpoint data were identified and addressed, these time points were revised to occur at the end of treatment, and at two subsequent 3-month intervals. As a result, there was variability in timing of measures from baseline across the study.
Statistical analysis
A procedure was devised to reconcile the revised protocol timing of assessments at end of treatment and 3 months post-treatment with the reality of varying times of endpoint assessments. Each individual's pain scores were linearly interpolated over whatever time points they provided data, and if necessary the final value was carried forward for not more than 1 month to include a few cases in which the final assessment occurred shortly before the last treatment. Thus, the outcomes at the end of treatment and 3 months post-treatment were the linearly interpolated values at those times (which varied across participants). The conditional change model was used for statistical tests.30 Specifically, each change score was regressed on its baseline value, treatment group indicators, and balancing factors (the latter in order to estimate the true standard deviation (SD) of the treatment effects when using design-adaptive randomization). The coefficients of the treatment group indicators, and differences between coefficients, were used to estimate treatment effects and for statistical tests.
Results
Feasibility, acceptability, and adherence to study protocol
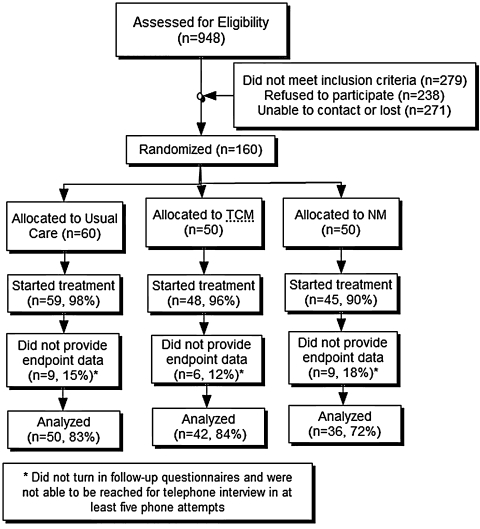
The CONSORT diagram31 for the study is presented in Figure 1. The top box includes all of those individuals who were referred to the TMD clinic during the recruitment period. The category “did not meet inclusion criteria (n = 279, 29%)” includes individuals not eligible through electronic medical record screening and through not having TMD at the diagnostic examination. The category “not able to contact or lost (n = 271, 29%)” refers primarily to individuals who never followed up on their referrals; only a small proportion ever learned of the study activities. Of the 398 who were eligible, 160 (40%) were randomized. Of all potential participants, 17% were randomized, which is slightly above the usual KPNW value of 15%. Once randomized, 1 participant assigned to SC, 2 assigned to TCM, and 5 assigned to NM attended no treatments and did not contribute to the endpoint analysis. After study onset, attempts were made to reach by telephone each participant who never attended or stopped treatment early to learn the reasons.
FIG. 1.
The consort diagram shows the progress of the study using standard guidelines. TCM, Traditional Chinese Medicine; NM, Naturopathic medicine.
When about one quarter of participants had reached the end of treatment, the follow-up questionnaire completion rate was found to be unacceptably low. The original follow-up questionnaires were lengthy with qualitative questions, and these questionnaires were substantially streamlined to decrease participant burden. Additionally, questionnaire return was more closely monitored and a plan of rapid response was implemented to improve the questionnaire response rate. Of the 24 participants who attended visits but provided no follow-up data (from a total of 160), 22 were recruited prior to this protocol revision; subsequently, only 2 participants did not provide endpoint data.
There was considerable variability in number of visits completed per treatment arm. The mode for SC was one to three visits, which generally represented the class, and provision of a bite splint. Individuals receiving more visits in SC (about half) were those needing further bite splint adjustments, and those referred for massage within KPNW. The mode for TCM was 20 visits (the number called for in the protocol); 33 participants received 19 or more treatments. Among those 6 who completed between 16 and 18 visits, the main reasons for not completing all visits were sufficient improvement, and difficulty in scheduling or transportation. Among the 9 who began treatment and received 12 or fewer treatments, the main reasons for stopping treatment were pain from needling, and lack of relief from TMD symptoms. The mode for NM was 9 visits (9 visits was the protocol); 31 participants received 7 or more treatments. Among the 14 who began treatment and received fewer than 7 treatments, the main reasons were dissatisfaction with group assignment, unwillingness to make lifestyle changes, and lack of improvement.
Baseline characteristics of study sample
Table 1 provides demographic and other characteristics of the study population, as distributed among the three arms at randomization. P values are not provided because balance was guaranteed by the allocation program. Overall, the group of women was predominantly middle-aged, with a median education level of “some college.” Household income for most was between $25,000 and $75,000. The 13.75% proportion of nonwhite and/or Hispanic participants is typical of Portland and KPNW. The level of depression as measured by the SCL-90-R embedded in the RDC was relatively high; 47–54% of participants were severely depressed, and an additional one third were moderately depressed.
Table 1.
Baseline Characteristics of Women Participating in alternative Medicine Approaches for Temporomandibular Joint Dysfunction Study (Mean ± Standard Deviation, or Count)
| Intervention group | Specialty care | Traditional Chinese Medicine | Naturopathic medicine |
|---|---|---|---|
| Sample size | 60 | 50 | 50 |
| Age (yrs) | 40.5 ± 9.4 | 40.1 ± 8.5 | 40.6 ± 9.2 |
| Education | |||
| Some HS | 2 | 0 | 1 |
| HS grad | 11 | 5 | 13 |
| Some college | 25 | 24 | 19 |
| College graduate | 8 | 8 | 7 |
| Post college | 14 | 13 | 10 |
| Income | |||
| <$25,000 | 12 | 8 | 7 |
| <$50,000 | 15 | 18 | 17 |
| <$75,000 | 20 | 13 | 13 |
| <$100,000 | 5 | 6 | 6 |
| >$100,000 | 5 | 4 | 1 |
| Race | |||
| Native American | 1 | 1 | 4 |
| Asian/Pacific Is | 3 | 1 | 0 |
| Black | 1 | 0 | 2 |
| White | 52 | 47 | 39 |
| Other | 3 | 1 | 5 |
| Hispanic | |||
| Yes | 2 | 1 | 6 |
| No | 58 | 49 | 44 |
| Depressiona | |||
| Moderately depressed % (n) | 35% (21) | 32% (16) | 32% (16) |
| Severely depressed % (n) | 47% (28) | 52% (26) | 54% (27) |
| Current smoker | 18% | 18% | 22% |
| Expectancyb | |||
| Acupuncture | 3.55 ± 1.05 | 3.83 ± 1.01 | 3.38 ± 1.09 |
| Herbs | 3.34 ± 0.90 | 3.30 ± 0.9 | 3.09 ± 0.83 |
| NM | 3.31 ± 0.84 | 3.52 ± 0.89 | 3.35 ± 0.98 |
| Duration of facial pain (yrs) | 7.3 ± 8.2 | 8.8 ± 8.3 | 5.4 ± 6.9 |
| Quality of pain | |||
| Persistent | 29 | 22 | 18 |
| Recurrent | 28 | 26 | 30 |
| Number who have ever used CAM | |||
| Acupuncturec | 17 | 12 | 6 |
| Biofeedback | 6 | 10 | 8 |
| Chiropractic | 34 | 30 | 21 |
| Herbs from practitioner | 10 | 7 | 7 |
| Herbs from store | 18 | 21 | 18 |
| Homeopathy | 10 | 5 | 8 |
| Massage | 27 | 23 | 25 |
| Naturopathyc | 6 | 7 | 7 |
| Percent who have tried any CAM modality | 72% | 74% | 72% |
CAM, complementary and alternative medicine; NM, naturopathic medicine.
SCL-90-R from the Research Diagnostic Criteria (range 0–4).
Subjects prospectively scored expectancies about each treatment type as (1) very unhelpful, (2) somewhat unhelpful, (3) not sure, (4) somewhat helpful, (5) very helpful.
Individuals who had tried these therapies for temporomandibular joint dysfunction were excluded from the study.
Worst facial pain
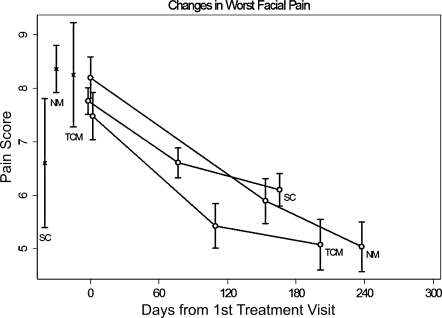
Table 2 shows the unadjusted values for worst facial pain and average facial pain scale scores and the interference of TMD with social function (all scaled from 0 to 10, where 10 is worst) at baseline, end of treatment (ET), and 3 months post-treatment (ET+ 3) among participants providing outcome data. Figure 2 illustrates these results for worst pain; baseline values are plotted at the time of first treatment for convenience. The vertical lines at the left edge of the figure indicate the baseline mean ± SD worst facial pain scores for individuals not providing endpoint data, for comparison purposes. Data are more sparse after the endpoints shown; however, there is no indication of changes in the trajectories shown from ET to ET+ 3 after the last points (data not shown). Using regression analysis adjusted for age, depression, smoking, and any prior CAM use (the balancing factors), both TCM and NM provided significantly more relief from worst pain than Specialty Care at end of treatment (difference by regression analysis from SC = −1.11 ± 0.43 points, p = 0.010 and −1.02 ± 0.45 points, p = 0.025 for TCM and NM, respectively, where negative means less pain) and at 3 months beyond the end of treatment (difference = −1.07 ± 0.51 points, p = 0.037 and −1.27 ± 0.54 points, p = 0.019 for TCM and NM versus SC, respectively), with no significant differences between alternative medicine arms. Overall, reductions in worst pain at end of treatment and 3 months post-treatment were 13% and 22% for SC, 29% and 33% for TCM, and 28% and 39% for NM. The percent of individuals achieving clinically meaningful pain reduction in worst facial pain (30% or more reduction in baseline pain) by end of treatment and 3 months post-treatment were 18% and 27% for SC, 32% and 46% for TCM, and 28% and 34% for NM.
Table 2.
Unadjusted Temporomandibular Joint Dysfunction Outcomes at Baseline, End of Treatment, and 3-Month Follow-up by Treatment Group (Mean ± Standard Deviation)
| Group | Specialty care | Traditional Chinese Medicine | Naturopathic medicine | pb | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Timea | BL | BS | ET | ET +3 | BL | BS | ET | ET +3 | BL | BS | ET | ET +3 | |
| N | 60 | 50 | 50 | 49 | 50 | 42 | 42 | 40 | 50 | 36 | 36 | 34 | |
| Worst FP | 7.6 ± 2.2 | 7.8 ± 1.8 | 6.6 ± 2.0 | 6.1 ± 2.1 | 7.5 ± 2.8 | 7.6 ± 2.9 | 5.4 ± 2.7 | 5.1 ± 3.0 | 8.2 ± 2.2 | 8.2 ± 2.3 | 5.9 ± 2.5 | 5.0 ± 2.7 | ≤0.04 (A) |
| Avg FP | 5.4 ± 2.5 | 5.5 ± 2.3 | 4.6 ± 2.0 | 4.0 ± 1.8 | 5.6 ± 2.5 | 5.5 ± 2.6 | 3.6 ± 2.1 | 3.2 ± 2.1 | 5.7 ± 2.4 | 5.8 ± 2.7 | 4.2 ± 2.5 | 3.5 ± 2.4 | ≤0.02 (B) |
| Impact on social life | 3.0 ± 3.0 | 2.9 ± 2.9 | 2.4 ± 2.2 | 2.0 ± 1.8 | 3.2 ± 3.0 | 3.0 ± 2.9 | 2.4 ± 2.4 | 2.0 ± 2.2 | 3.7 ± 2.6 | 3.7 ± 2.6 | 2.5 ± 2.1 | 1.9 ± 2.2 | ≤0.02(C) |
BL, baseline for everyone; BS, baseline for those who had treatments and outcomes and were included in analyses; ET, end of treatment; ET+3, 3 months post ET; FP, facial pain.
Minimum significance level of bolded treatment intervention improvement compared to improvement in specialty care group; details provided below.
A: ET v. BS: T-S p = 0.010, N-S p = 0.025, N-T p = 0.840; ET+3 v. BS: T-S p = 0.037, N-S p = 0.019; N-T p = 0.725.
B: ET v. BS: T-S p = 0.004, N-S p = 0.145; N-T p = 0.225; ET+3 v. BS: T-S p = 0.017, N-S p = 0.118; N-T p = 0.495.
C: ET v. BS: T-S p = 0.758, N-S p = 0.012; N-T p = 0.034; ET+3 v. BS: T-S p = 0.927, N-S p = 0.099; N-T p = 0.099.
FIG. 2.
Trajectories of the average of worst facial pain are shown by group for the individuals who provided endpoint data, plotted at baseline, end of treatment, and 3 months post-treatment. The end of treatment and 3 months post-treatment time points vary by treatment group because of different protocols between groups. Standard errors of the means are also shown. The vertical lines at the far left show the mean and standard error for the baseline worst facial pain among those participants in each group who contributed no subsequent outcome assessments. Baseline values are centered at the time of the first intervention visit. TCM, Traditional Chinese Medicine; NM, Naturopathic medicine; SC, specialty care.
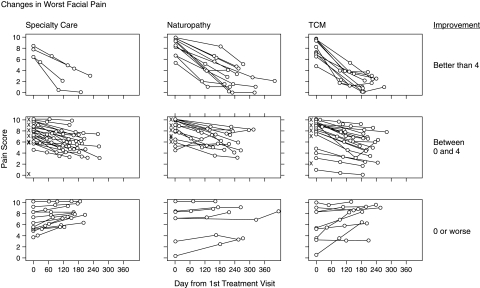
The individual outcomes for worst facial pain in each of three groups are presented in Figure 3. For ease of viewing, the individuals have been grouped based on their outcomes at 3 months after the end of treatment into 3 groups: substantial improvement (4 or more points on the 10-point scale); some improvement (between 0 and 4 points on the 10-point scale); or no improvement (0 or worsening). The two alternative medicine arms each have about twice the number with substantial improvement compared to the SC arm, and fewer than the SC arm with no improvement or with worsening; there are both greater overall pain reductions and higher response rates in the alternative medicine arms compared to SC.
FIG. 3.
Individual trajectories of worst facial pain are shown for all individuals who provided endpoint data. The columns represent treatment groups. The rows represent the degree of improvement: substantial improvement (more than a 4-point decline on a 0–10 scale); modest improvement (from more than 0 points to a 4-point decline on a 0–10 scale); no improvement or worsening (no decline or pain increase). Baseline values are centered at the time of the first intervention visit.
Average facial pain
TCM provided better relief for average facial pain when the participants were having pain than did SC at end of treatment (ET) and at 3 months post end of treatment (ET+ 3) (adjusted difference by regression analysis = −0.96 ± 0.34 points, p = 0.004 and −0.92 ± 0.38 points, p = 0.017 for TCM at ET and ET+ 3 respectively; unadjusted values are shown in Table 2).Changes in the NM arm were not significantly different from SC or TCM. Overall, the average pain reductions at end of treatment and ET+ 3 were, respectively, 16% and 27% in SC, 35% and 42% in TCM, and 28% and 40% in NM. The percent of individuals achieving clinically meaningful average facial pain reduction (30% or more reduction in baseline pain) by ET and ET+ 3 were 17% and 38% for SC, 44% and 48% for TCM, and 28% and 38% for NM.
Interference of facial pain with activities
None of the arms showed significant differences compared to any other arm for the amount of change in the impact of TMD-related pain on activities of daily living (data not shown). However, the NM arm provided more relief than either other arm in relation to the impact of TMD-related pain on social activities at end of treatment (adjusted difference by regression analysis NM compared to SC = −0.59 ± 0.23 points, p = 0.012; NM versus TCM = −0.52 ± 0.24 points, p = 0.034; unadjusted values shown in Table 2).Participants reported reductions in social dysfunction due to TMD-related pain at ET and ET+ 3 of 17% and 31% in SC, 20% and 33% in TCM, and 32% and 49% in NM.
Of the 24 comparisons provided by comparing each group with both other groups at each time point across four variables (Table 2; interference with activities of daily living not shown), 8 of the 24 comparisons showed significant differences at the p < 0.05 level, whereas 1–2 would have been expected by chance at the p < 0.05 level. SC did not provide more benefit, whether significant or not, in any comparison. As a pilot trial designed to identify whether there was evidence for continuing research, correction for multiple comparisons was not warranted.
Safety and side effects
No serious adverse events were reported that were in any way related to the intervention. Minor side effects were mainly reported as self-limiting localized pain and bruising from the acupuncture needles, or minor gastrointestinal discomfort with herbs in both TCM and NM arms, which were resolved by the practitioners by reducing dosage.
Discussion
The results from this pilot trial suggest that TCM and NM, when delivered as whole systems of care, can be as effective as or more effective than high-quality specialty dental care for individuals suffering from TMD with systemic co-morbidities. Results suggest that although patients may achieve more rapid improvement of facial pain with TCM, over the course of treatment both NM and TCM result in significantly more improvement in facial pain than specialty dental care. The interventions were also safe, with no serious adverse events that were related to the interventions. Side effects of the treatments, as managed by the practitioners, were mild and limited. It is important to note that clinical trial protocols were designed to reflect what would be common best practice in community treatment.
The study was designed to have a strong control arm for comparison. The improvement seen in the participants assigned to the SC arm are similar to that recently reported for bite splint and nonsplint care9 and similar to the improvements demonstrated in RCTs comparing cognitive–behavioral interventions and a tailored self-care intervention to standard SC.32,33 These comparable improvements shown in the SC arm compared to the experimental interventions in trials suggest that the SC arm consistently provided positive TMD care. The differences achieved by the CAM interventions thus may be beyond current standard treatment for TMD, and these interventions appear to merit further research.
Participants who joined the study were interested in trying alternative medicine approaches, and thus the results of this study can only be generalized to those individuals who are interested in trying these approaches. The present trial was unique from a TCM perspective in that no prior clinical trials have offered TCM as a system of care with acupuncture point prescriptions and Chinese herbal therapy individualized to each participant. In a trial approaching the present design, patients with seasonal allergic rhinitis randomly assigned to a TCM arm received a standardized acupuncture protocol and a basic herbal formula with practitioners allowed to use additional acupoints and an additional herbal formula tailored to the patient's individualized TCM diagnosis.34 Compared to patients assigned to receive superficial needling at standardized nonacupuncture points and a nonspecific herbal formula, patients in the TCM group showed significantly greater improvement on a symptom severity Visual Analogue Scale and a rhinitis quality-of-life scale.
No other studies have reported on the outcomes of whole systems naturopathic interventions for pain. NM involves lifestyle changes, and NM study practitioners were initially concerned about adherence and retention among participants who had no knowledge of NM. This lack of familiarity with NM by study participants stood in marked contrast to their private practices where most individuals seeking NM treatment were already somewhat familiar with what to expect, and arrived ready to make lifestyle changes. In this study, participants were naãve to NM interventions and philosophy. Practitioners reported that the first session was largely an orientation to the medicine, but within one or two sessions, most participants began to understand what was expected. This arm had a higher percentage of participants not completing treatment than the TCM arm, possibly because of the degree to which this medicine calls for changes in lifestyle practices. The study SC dentists concurred that improvement in TMD pain requires changes in lifestyle, and they speculated that these results suggest that the SC approach may be less successful than NM in fostering such changes. The ability of the NM practitioners to achieve lifestyle change may also explain the better outcomes on social functioning achieved with NM as compared with TCM.
Limitations to this study include short follow-up times, some loss of endpoints in the early stages of the study, and variability in the timing of measures in relation to the interventions, which future studies should address. We should also note some limitations to generalizability as only 40% of those who were eligible accepted randomization into the trial. However, enrollment rates in the trial compare favorably with other similar studies, particularly when considering the need to accept the study questionnaire burden and randomization to treatment modality arm. Surveillance of those ending participation in the study prematurely also allowed us to adjust our assessment procedures to ensure better retention, thus building a stronger foundation for future studies of this type.
Conclusions
While methods for study of whole medical systems remain in development, this study demonstrates the feasibility and potential for developing greater understanding of traditional whole-systems approaches in a manner that can simultaneously provide guidance to community CAM practitioners. Results suggest that both TCM and NM may provide greater improvement for some patients with TMD than state-of-the-art SC. Knowledge gained in protocol design and implementation, and these results, suggest that further research is warranted. Future research may also seek to determine which patients are most likely to respond to the specific CAM whole-system approaches.
Appendix 1.
Traditional Chinese Medicine Protocol
| Syndrome diagnosis | Points | Base herbal formula(s) | Symptoms | Points |
|---|---|---|---|---|
| Liver qi stagnation | GB41, GB40, GB34, LV14, LV13 | Xiao yao san or chai ju shu gan tang | Headache | GV20, taiyang, GB41, ST41, TW5 |
| Liver blood xu | GB39, BL18, BL20 | Jia wei si wu tang | Insomnia | HT7 or PC6, anmian |
| Liver yin xu | SP6 | Yi guan jian | Ear pain | TW3, TW17 |
| Liver Wind, liver yang, or liver Fire rising | LV2, GB40 | Zheng gan xi feng tang or tianma gouteng yin | Fibromyalgia | SP21, scalp points: upper, middle, and lower jiao |
| Qi and blood stagnation due to injury | Ah shi | Xiao huo luo dan or tong qiao hue xue tang | Depression and/or anxiety | GV24, GV20, CV17, CV12, CV6 |
| Heart blood xu | BL15 | Tian wang bu xin dan, zhi gan cao tang, sheng mai san, gan mai da zao tang or ding zhi wan | Neck/shoulder pain or tightness | BL43, BL12, SI3 |
| Spleen qi xu and Damp retention | ST36, SP9 | Bu zhong yi qi tang, shen ling bai zhu san, jiu jun zi tang, or wu ling san | Low back pain | BL23, shiqizhui, BL40 |
| Kidney qi xu | BL23, KD3 | Jin gui shen qi tang | Difficulty moving the jaw | During last 5 minutes remove all local points and stimulate LI4 while patient attempts to move her jaw |
| Kidney jing xu | BL52 | Zuo gui yin | ||
| Kidney yin xu | SP6, KD6 | Zhi dai di huang tang, or liu wei di huang tang | ||
| Kidney yang xu | GV4, CV4 | You gui wan | ||
| Wind-Cold invasion | TW5 | Juan bi tang, Yi yi ren tang, or Gui zhi wu tou tang |
Appendix 2.
Naturopathic Medicine Protocol
| Nutritional recommendations | Study-specific handouts for: |
| Blood type diet | Peter J. D. Adamo, N.D. (Eat Right 4 Your Type); |
| Anti-inflammatory diet | Eliminate foods likely to provoke an inflammatory reaction in the body such as red meat, sugar, coffee, chocolate, processed grains, and milk |
| Hypo-allergenic | Eliminate foods most likely to provoke specific allergic reaction |
| Cleansing/detoxification | Remove foods hard for the body to digest and include foods that promote the process of detoxification |
| TMD specific diet | Avoiding hard and chewy foods, changing diet when pain is present |
| Supplements | |
| Foundational packet | Multivitamin/mineral tablet, essential fatty acids and liver support (a lipotropic supplement that supports the function and health of the liver), and a tea composed of the following herbs: Arctium lappa, Silybum marianum, Mahonia spp, Taraxacum off., and Glycyrrhiza glabra, Zingiver off. |
| Additional supplements available | Supplements in formulary for inflammatory bowel syndrome, hormone imbalance, fibromyalgia, adrenal fatigue, and blood sugar imbalance |
| Stress management | Breathing techniques, visualization/guided imagery, and stress journaling |
| Physical medicine | Somatic re-education; NM manipulation; trigger point therapy; NM massage; heat packs; castor oil packs |
TMD, temporomandibular joint dysfunction; NM, naturopathic medicine.
Acknowledgments
The project was one of three main projects in the Oregon Center for Complementary and Alternative Medicine Research in Craniofacial Disorders, funded by the National Institutes of Health, National Center for Complementary and Alternative Medicine grant number P50AT00076 to Kaiser Permanente Center for Health Research, Portland OR, 1999–2005. None of the authors have any conflicts of interest.
References
- 1.Von Korff M. Dworkin SF. Le Resche L. Kruger A. An epidemiologic comparison of pain complaints. Pain. 1988;32:173–183. doi: 10.1016/0304-3959(88)90066-8. [DOI] [PubMed] [Google Scholar]
- 2.Laskin D. Greene CS. Hylander W. TMDs: An Evidence-Based Approach to Diagnosis and Treatment. Chicago: Quintessence; 2005. [Google Scholar]
- 3.Dworkin SF. LeResche L. Von Korff M. Studying the natural history of TMD: Epidemiologic perspectives on physical and psychological findings. In: Vig KD, editor; Vig PS, editor. Clinical Research as the Basis for Clinical Practice. Ann Arbor, MI: University of Michigan; 1989. pp. 39–60. [Google Scholar]
- 4.Smith JA. Syrop S. TMD incidence and socioeconomic standing: Eradicating the myth of the upper class patient. N Y State Dent J. 1994;60:36–39. [PubMed] [Google Scholar]
- 5.White BA. Williams LA. Leben JR. Health care utilization and cost among health maintenance organization members with temporomandibular disorders. J Orofac Pain. 2001;15:158–169. [PubMed] [Google Scholar]
- 6.Greene CS. Managing TMD patients: Initial therapy is the key. J Am Dent Assoc. 1992;123:43–45. doi: 10.14219/jada.archive.1992.0188. [DOI] [PubMed] [Google Scholar]
- 7.LeResche L. Drangsholt M. Temporomandibular disorders. In: Goldman MB, editor; Hatch MC, editor. Women and Health. San Diego: Academic Press; 2000. pp. 1120–1128. [Google Scholar]
- 8.Dworkin SF. Truelove EL. Temporomandibular Disorders. In: Rakel RE, editor. Conn's Current Therapy. New York: W.B. Saunders; 1997. [Google Scholar]
- 9.Truelove E. Huggins KH. Mancl L. Dworkin SF. The efficacy of traditional, low-cost and nonsplint therapies for temporomandibular disorder: A randomized controlled trial. J Am Dent Assoc. 2006;137:1099–1107. doi: 10.14219/jada.archive.2006.0348. [DOI] [PubMed] [Google Scholar]
- 10.Ohrbach R. Dworkin SF. Five-year outcomes in TMD: Relationship of changes in pain to changes in physical and psychological variables. Pain. 1998;74:315–326. doi: 10.1016/s0304-3959(97)00194-2. [DOI] [PubMed] [Google Scholar]
- 11.Suvinen TI. Reade PC. Kemppainen P, et al. Review of aetiological concepts of temporomandibular pain disorders: Towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur J Pain. 2005;9:613–633. doi: 10.1016/j.ejpain.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 12.DeBar LL. Vuckovic N. Schneider J. Ritenbaugh C. Use of complementary and alternative medicine for temporomandibular disorders. J Orofacial Pain. 2003;17:224–236. [PubMed] [Google Scholar]
- 13.Raphael KG. Klausner JJ. Nayak S. Marbach JJ. Complementary and alternative therapy use by patients with myofascial temporomandibular disorders. J Orofac Pain. 2003;17:36–41. [PubMed] [Google Scholar]
- 14.Vuckovic NH. Gullion CM. Williams LA, et al. Feasibility and short-term outcomes of a shamanic treatment for temporomandibular joint disorders. Altern Ther Health Med. 2007;13:18–29. [PubMed] [Google Scholar]
- 15.Ernst E. White AR. Acupuncture as a treatment for temporomandibular joint dysfunction: A systematic review of randomized trials. Arch Otolaryngol Head Neck Surg. 1999;125:269–272. doi: 10.1001/archotol.125.3.269. [DOI] [PubMed] [Google Scholar]
- 16.Rosted P. Practical recommendations for the use of acupuncture in the treatment of temporomandibular disorders based on the outcome of published controlled studies. Oral Dis. 2001;7:109–115. [PubMed] [Google Scholar]
- 17.Wong YK. Cheng J. A case series of temporomandibular disorders treated with acupuncture, occlusal splint and point injection therapy. Acupunct Med. 2003;21:138–149. doi: 10.1136/aim.21.4.138. [DOI] [PubMed] [Google Scholar]
- 18.Goddard G. Short term pain reduction with acupuncture treatment for chronic orofacial pain patients. Med Sci Monit. 2005;11:CR71–CR74. [PubMed] [Google Scholar]
- 19.Zhou FH. Zhao HY. Acupuncture and ultrasound therapy for temporomandibular disorders [in Chinese] Di Yi Jun Yi Da Xue Xue Bao. 2004;24:720–721. [PubMed] [Google Scholar]
- 20.Smith P. Mosscrop D. Davies S, et al. The efficacy of acupuncture in the treatment of temporomandibular joint myofascial pain: A randomized controlled trial. J Dent. 2007;35:259–267. doi: 10.1016/j.jdent.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 21.Pizzorno JE. Murray MT. Textbook of Natural Medicine. 3rd. St. Louis: Churchill-Livingstone Elsevier; 2006. [Google Scholar]
- 22.Myers CD. White BA. Heft MW. A review of complementary and alternative medicine use for treating chronic facial pain. J Am Dent Assoc. 2002;133:1189–1196. doi: 10.14219/jada.archive.2002.0360. [DOI] [PubMed] [Google Scholar]
- 23.Barros L. Pileggi F. The anti-adrenergic effects of hypermagnesemia: An experimental study. Brazil J Med Biol Res. 1991;24:29–33. [PubMed] [Google Scholar]
- 24.Wagner H. Norr HM, et al. Drugs with adaptogenic effects for strengthening the powers of resistance [in German] Z Phytother. 1992;13:42–54. [Google Scholar]
- 25.Nahin RL. Straus SE. Research into complementary and alternative medicine: Problems and potential. BMJ. 2001;322:161–164. doi: 10.1136/bmj.322.7279.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dworkin SF. Ohrbach R. Assessment of orofacial pain. In: Turk DC, editor; Melzack R, editor. Handbook of Pain Assessment. 2nd. New York: Guilford Press; 2001. pp. 475–498. [Google Scholar]
- 27.Aickin M. Randomization, balance, and the validity and efficiency of design-adaptive allocation methods. J Stat Planning Inference. 2001;94:97–119. [Google Scholar]
- 28.Aickin M. Beyond randomization. J Altern Complement Med. 2002;8:765–772. doi: 10.1089/10755530260511775. [DOI] [PubMed] [Google Scholar]
- 29.Ritenbaugh C. Verhoef M. Fleishman S, et al. Whole systems research: A discipline for studying complementary and alternative medicine. Altern Ther Health Med. 2003;9:32–36. [PubMed] [Google Scholar]
- 30.Plewis I. Analysing Change. Chichester, UK: John Wiley & Sons; 1985. [Google Scholar]
- 31.Altman DG. Schulz KF. Moher D, et al. for the CONSORT Group. The revised CONSORT statement for reporting randomized trials: Explanation and elaboration. Ann Intern Med. 2001;134:663–694. doi: 10.7326/0003-4819-134-8-200104170-00012. [DOI] [PubMed] [Google Scholar]
- 32.Dworkin SF. Huggins KH. Wilson L, et al. A randomized clinical trial using Research Diagnostic Criteria for Temporomandibular Disorders-Axis II to target clinic cases for a tailored self-care TMD treatment program. J Orofacial Pain. 2002a;16:48–63. [PubMed] [Google Scholar]
- 33.Dworkin SF. Turner JA. Mancl L, et al. A randomized clinical trial of a tailored comprehensive care treatment program for temporomandibular disorders. J Orofacial Pain. 2002b;16:259–276. [PubMed] [Google Scholar]
- 34.Brinkhaus B, et al. Acupuncture and Chinese herbal medicine in the treatment of patients with seasonal allergic rhinitis: A randomized-controlled clinical trial. Allergy. 2004;59:953–960. doi: 10.1111/j.1398-9995.2004.00540.x. [DOI] [PubMed] [Google Scholar]