Abstract
Purpose
This study examined the communicative profiles of children with autism spectrum disorders (ASD) in the second year of life.
Method
Communicative acts were examined in 125 children 18 to 24 months of age: 50 later diagnosed with ASD; 25 with developmental delays (DD); and 50 with typical development (TD). Precise measures of rate, functions, and means of communication were obtained through systematic observation of videotaped Behavior Samples from the Communication and Symbolic Behavior Scales Developmental Profile (Wetherby & Prizant, 2002).
Results
Children with ASD communicated at a significantly lower rate than children with DD and TD. The ASD group used a significantly lower proportion of acts for joint attention and a significantly lower proportion of deictic gestures with a reliance on more primitive gestures compared to DD and TD. Children with ASD who did communicate for joint attention were as likely as other children to coordinate vocalizations, eye gaze, and gestures. Rate of communicative acts and joint attention were the strongest predictors of verbal outcome at age 3.
Conclusions
By 18 to 24 months of age, children later diagnosed with ASD showed a unique profile of communication, with core deficits in communication rate, joint attention, and communicative gestures.
Introduction
By the end of the first year of life typically developing children demonstrate a variety of communicative means and functions to express intentions. Although most children are not yet producing true words at this age, they communicate intentionally using means such as gestures, sounds, and eye gaze to express three major communicative functions: behavior regulation, social interaction, and joint attention (Bates, 1979; Bruner, 1981; Wetherby & Prizant, 2002). Autism spectrum disorders (ASD) are characterized by pervasive impairments in social interaction and communication, including impairments in the use of nonverbal behaviors, a lack of seeking to share enjoyment and interests, and delay in or lack of spoken language and gestures (American Psychiatric Association, 2000). Over the past two decades, major advances have been made in understanding and identifying the social communication impairments in children 2 to 5 years of age with ASD, with substantial research documenting differences in the rate, functions, and means of communication of children with ASD compared to children with other developmental delays (DD) and typical development (TD; Mundy, Sigman, & Kasari, 1990; Stone, Ousley, Yoder, Hogan, & Hepburn, 1997; Wetherby, Prizant, & Hutchinson, 1998). In contrast, research characterizing the communicative profiles of children with ASD younger than 2 years is relatively limited because the usual age of diagnosis is not until at least 3 years.
The second year of life is a critical time to examine the early development and emerging symptoms of ASD because there are implications for early detection leading to early intervention and even the possibility of preemption of significant symptoms. The few studies that have systematically made diagnoses in children under the age of 2 have found that cognitive abilities are impaired (Chawarska, Klin, Paul, & Volkmar, 2007), even in some areas when compared to children with language delays (Landa & Garret-Mayer, 2006). Young children with ASD may also show a different developmental trajectory compared to children with language delays and TD, with a broadening developmental delay and a deceleration of cognitive growth observed across the second year (Landa & Garrett-Mayer), suggesting that the second year of life may be a critical time to examine when and how development goes awry in children with ASD.
Research examining the social communication impairments unique to ASD in children under 2 years of age is emerging from several sources. Studies utilizing home videotapes and parent report provide evidence that impairments in social communication are present in children with ASD prior to the first birthday (Colgan et al., 2006) and early in the second year and that these impairments likely persist, with additional symptoms emerging late in the second year (for review see Wetherby, Watt, Morgan, & Shumway, 2007). However, these studies have been limited by the lack of consistency in sampling procedures as well as small sample sizes and findings are somewhat inconsistent in relation to the specific impairments that may differentiate children with ASD. For example, some research has shown that decreased gaze to people and failing to orient to name may differentiate children with ASD from TD at 12 months of age (Osterling & Dawson, 1994; Osterling, Dawson, & Munson, 2002), while others studies have found no group differences on these behaviors (Werner & Dawson, 2005). There has also been some discrepancy in whether the use of gestures, such as pointing and showing distinguish children with ASD from DD and TD under 2 years of age based on parent report (e.g., Cox et al., 1999; Mitchell et al., 2006) and analyses of home videotapes (Clifford, Young, & Williamson, 2007; Werner & Dawson).
There is now a small body of research using systematic observation of children with ASD under 2 years of age identified prospectively and followed longitudinally to distinguish early characteristics from children with DD and TD. One cohort of children consists of those identified as part of a general population screen as high risk for ASD using the Checklist for Autism in Toddlers (CHAT). Based on CHAT scores, children were invited for a detailed clinical diagnostic assessment and participation in a series of experimental studies. A second major cohort of children under two years of age has been identified from a general population screen using the Communication and Symbolic Behavior Scales Developmental Profile (CSBS DP; Wetherby & Prizant, 2002) and later diagnosed with ASD. Findings from this research provide some preliminary information on early social communication impairments of young children with ASD. For example, an early deficit in shared attention has been well established, with children with ASD in the second year of life showing lack of appropriate gaze and fewer gaze shifts between objects and people compared to DD and TD (Charman et al., 1997; Swettenham et al., 1998; Wetherby et al., 2004; Wetherby et al., 2007). These studies provide evidence of early impairments in eye gaze and highlight the need to investigate eye gaze as a means of communication within the communicative acts of children with ASD in the second year of life, an area of documented impairment in preschool-age children with ASD (Phillips, Gomez, Baron-Cohen, Laa, & Riviere, 1995; Stone et al., 1997).
In addition to deficits in eye gaze, research based on direct observation has documented other social communication impairments in children with ASD in the second year. Using the Systematic Observation of Red Flags of ASD (SORF; Wetherby & Woods, 2002), which employs ratings from 0 to 2 of a standardized behavior sample, Wetherby and colleagues (2004) examined symptoms in the second year of life of children later diagnosed with ASD and identified 13 red flags that correctly classified 18 children with ASD, DD, and TD with 94.4% accuracy. Among these red flags are several items that provide insight into the communicative acts of children with ASD in the second year. For example, in comparison to children with DD and TD, children with ASD showed a lack of sharing interest or enjoyment, which is a measure of communicating for joint attention, as well as a lack of communication involving coordination of at least three of the following: gaze, facial expression, gesture, and sound. In addition, children with ASD were significantly different from children with TD but not DD on a lack of communicative vocalizations with consonants, that is, speech-like vocalizations directed with eye gaze, gesture, or movement toward a person. An impairment in communicative vocalizations was also described by Chawarska et al. (2007) in a recent study of 19 children with autism at a mean age of 21 months, in which a severe deficit in the frequency of vocalizations directed to others was observed on the Autism Diagnostic Observation Schedule (ADOS). These findings indicate that impairments in initiating joint attention and the coordination of communicative means may be evident in children with ASD prior to 24 months. In relation to socially directed gestures, research based on systematic observation indicates deficits in communicative gestures such as pointing and showing in young children with ASD. Wetherby et al. (2004) found that a lack of showing distinguished children with ASD from children with DD and TD, with a lack of pointing distinguishing children with ASD from TD but not DD in the second year. Although the Chawarska et al. (2007) study did not include comparison groups of children with DD and TD, the researchers also found deficits in the use of showing, pointing, and other communicative gestures in the second year. These studies provide valuable information on early social communication impairments observed in children with ASD in the second year of life, but are limited by relatively small sample sizes and restricted scoring ranges on the SORF and ADOS. Research with larger sample sizes in children under 2 years of age is needed to better understand the ontogeny of communication in young children with ASD and to focus on these isolated behaviors such as eye gaze, vocalizations, and gestures within communicative acts of young children with ASD.
Two studies have specifically examined the communicative acts of children with ASD under 2 years of age using direct, systematic observation (Drew, Baird, Taylor, Milne & Charman, 2007; Wetherby et al., 2007). Drew and colleagues (2007) reported on the communicative acts of two samples of children with ASD recruited using the CHAT. Rate of child communicative acts and form, function, and complexity of child communication were assessed using the Social Communication Assessment for Toddlers with Autism (SCATA), a measure of primarily nonverbal social communicative ability during a semi-structured interaction with an unfamiliar adult. The researchers reported that communicative acts had to involve some sense of directedness and child awareness of the adult’s presence to be coded. However, a broad range of communicative acts (forms) and functions were coded. For example, a look to monitor the examiner’s actions, looking at or catching the examiner’s eye, pointing to an object, taking a toy held out by the examiner, and nodding when a new game was suggested were coded as acts if there was some sense of directedness or if the action was done in response to the examiner’s presence. Functions such as monitoring, responding, and naming in addition to requesting and commenting were also coded.
At a mean age of 20.7 months (SD=1.3), Sample 1 (n = 17) communicated at a rate of 3.5 (SD = 1.38) communicative acts per minute. Sample 2, with a mean age of 25.0 months (SD = 5.4), was reported to communicate at a lower rate of 1.87 (SD = .83) acts per minute. This study did not specifically examine whether differences in communicative functions or complexity of acts were significant; however, Sample 1 was reported to communicate most frequently for social purposes or shared pleasure, such as using an affectionate gesture or shifting gaze and smiling when a toy is activated, while Sample 2 communicated most frequently to request. Overall, social communicative acts and requesting were more frequent than commenting in both samples of children. In relation to complexity, acts involving a single form of communication were more frequent than acts with combined or sequential forms in both samples of children. The difference in rate of communicative acts between these two samples was reported to reflect a greater severity of autism in Sample 2, with more children having a diagnosis of autism compared to ASD. To date, the sample of 17 children with a mean age of 21 months is the youngest sample for which precise measures of rate of communicative acts have been studied and reported; however, it did not contribute to the unresolved issues in distinguishing social communication in children with ASD from children with TD and DD under 2 years of age.
A second study of communicative acts of children in the second year who were later diagnosed with ASD was recently conducted by Wetherby and colleagues (2007). The researchers compared social communication profiles of 50 children with ASD late in the second year with a mean age of approximately 21 months to children with DD and TD. This group of 50 children with ASD included the 18 children examined using the SORF (Wetherby et al., 2004) and will form the majority of the sample for the present study. Fourteen social communication measures, including communicative acts, were examined using the standard clinical scoring of the CSBS DP. This standard scoring allowed up to 3 communicative acts to be coded for each of the 6 activities in the Behavior Sample, with a maximum of 18 communicative acts possible. Communicative functions (behavior regulation, social interaction, and joint attention) were scored as the number of activities out of 6 during which a child communicated, and inventory of gestures was defined as the number of different conventional gestures displayed out of a total of 8. Based on standard scoring, the ASD group scored significantly lower than the TD group on all 14 social communication measures. In comparison to children with DD, the ASD group scored significantly lower on five social communication measures. Among these were rate of communication, communicating for joint attention, and inventory of conventional gestures. In examining communicative functions, children with ASD were comparable to DD in communicating for behavior regulation, slightly lower on social interaction, and significantly lower on communicating for joint attention. In addition, communicating for behavior regulation and inventory of gestures in the second year were among the strongest predictors of severity of autism symptoms in the fourth year. To date, this is the largest sample of children with ASD examined using direct observation in the second year. Findings from this study provide valuable information about the communicative acts of young children with ASD as measured by a specific instrument, the CSBS DP Behavior Sample. However, this study is limited by the standard scoring of the instrument, which was designed to be a clinical rating, not a precise measure of each communicative act. Thus, results of this study are influenced by the restricted scoring range and the limited number of communicative acts, functions, and means (e.g., gestures and vocalizations) available for data analysis. Results of this study highlight the need to investigate means of communication in relation to communicative functions and to use a descriptive and more precise approach to measurement and analysis of communicative acts in research. This precise measurement will provide information about the utility of the CSBS DP Behavior Sample in children with ASD younger than 2 years of age and will help to describe this young population by offering normative as well as descriptive data for ASD in contrast to the cutoffs obtained through standard scoring. Continued research examining more precise measures of social communication in the second year will also help to better understand the course of development of social communication in young children with ASD.
Purpose of Study
Preliminary research examining the social communication skills of children with ASD under 2 years of age is emerging, with impairments documented in rate of communication, joint attention, and the use of vocalizations, eye gaze, and gestures in communication. However, the methodologies implemented in these studies have been limited by small sample sizes and lack of systematic observation. Investigations that have employed direct observation have relied on restricted rating scales or cutoffs obtained through standard scoring, reducing the precision of measurement of the behaviors under investigation. Given that differences in social communication appear to be among the earliest indicators of ASD, speech-language pathologists (SLPs) play an important role in screening and early detection, as discussed in guidelines recently published by the American Speech-Language-Hearing Association (2006). Research using direct observation with precise measures to describe and quantify social communication skills with a larger sample of children within a narrow age range is needed to provide important information on the core social communication deficits of ASD and improve understanding of the communication profiles of young children with ASD compared to children with DD and TD. Such information is critical in improving screening and early identification and may aid in efforts to provide important intervention targets. The purpose of this study was to compare differences in the communicative acts, including rate, functions, gestures, and coordination of communicative means of children between 18 and 24 months of age later diagnosed with ASD, matched with a group of children with DD and TD. Profile analyses were conducted to determine whether children with ASD exhibit a unique profile of communication at this young age. Predictive relations between communicative acts late in the second year and verbal and nonverbal developmental level at 3 years of age were also examined.
Method
Participants
One hundred twenty five children participated in this study, 50 later diagnosed with ASD, 25 with DD in which ASD had been ruled out, and 50 with TD. Children were recruited through the FIRST WORDS® Project, which conducts screening on a general population sample of children using the CSBS DP (Wetherby & Prizant, 2002) as a measure of prelinguistic communication to identify children younger than 2 years of age at risk for developmental delays. All children in this study had a CSBS DP Behavior Sample when the child was over 18 months of age and a follow-up developmental assessment when the child was over 24 months. The children in this study have previously been reported on by Wetherby et al. (2007), with two additional children with DD recruited by the time of the present study as part of the ongoing longitudinal FIRST WORDS® Project. The Behavior Samples were collected from all children between 1998 and 2005 and children with communication delays were consecutive cases whose family agreed to participate in the follow-up diagnostic evaluation. Standardized protocol was adhered to for all participants, regardless of time of study entry. Recruitment, selection criteria, group assignment, and group matching procedures are described in detail in Wetherby et al. (2004; 2007). Briefly, children in ASD and DD groups showed a communication delay during the second year of life based on performance in the bottom 10th percentile on the Social or Symbolic Composites of the CSBS DP Behavior Sample. Children with communication delay were assigned to the ASD or DD group based on a diagnostic evaluation at three years of age. Children in the ASD group were diagnosed based on information gathered during a multidisciplinary follow-up diagnostic evaluation consisting of a developmental history generally obtained through parent report, the Mullen Scales of Early Learning (MSEL; Mullen, 1995), the Autism Diagnostic Observation Schedule (ADOS; Lord, Rutter, DiLavore, & Risi, 1999), and the Social Communication Questionnaire, Lifetime Version (SCQ; Rutter, Bailey, Berument, Lord, & Pickles, 2001). Children in the DD group scored more than one standard deviation below the mean on at least one of the four scales of the MSEL, and had a diagnosis of ASD ruled out through the same follow-up diagnostic evaluation procedure described for the ASD group. Participants in the TD group were drawn from a pool of children displaying performance above the 25th percentile on the Social and Symbolic Composites of the CSBS DP Behavior Sample during the second year of life and were within normal limits on the MSEL. Additionally, none of the TD children were suspected of having ASD by the clinician during the evaluation or by the parent as measured by the SCQ. The ASD and DD groups were matched group-wise on chronological age and developmental level at the time of the Behavior Sample. Children in the TD group were matched individually to the ASD group on gender and chronological age.
Participant demographics are presented in Table 1. Based on the criterion p-value of >.50 as an index of matching on tests of group differences, with a p-value of <.20 suggesting groups are not matched on a variable (Mervis & Klein-Tasman, 2004), the groups were well-matched on mother’s and father’s education as well as mother’s age. This suggests that the groups were comparable on socioeconomic status. The groups had similar percentages of males. The ASD group had slightly more Hispanic children and Asian children than the TD group, and the DD group had slightly more African American children than both other groups.
Table 1.
Summary of Participant Demographics
|
p value of pairwise differences |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Demographic | ASD (n =50) | DD (n =25) | TD (n =50) | F value | DD-ASD | TD-ASD | |||
| Parent’s education in years completed | |||||||||
| Mother (M, SD ) | 15.48 | 2.08 | 15.22 | 2.47 | 15.19 | 2.25 | 0.24 | .959 | .883 |
| Father (M, SD ) | 15.73 | 2.52 | 15.52 | 2.71 | 15.40 | 2.57 | 0.22 | .986 | .883 |
| Parent’s age at child’s birth in years | |||||||||
| Mother (M, SD ) | 31.19 | 4.93 | 31.94 | 6.37 | 31.24 | 5.56 | 0.13 | .943 | .999 |
| Father (M, SD ) | 32.99 | 6.82 | 35.91 | 5.50 | 33.71 | 6.04 | 1.95 | .162 | .929 |
| Males (%) | 86.0 | 76.0 | 86.0 | ||||||
| First born (%) | 44.0 | 36.0 | 38.0 | ||||||
| Ethnicity (%) | |||||||||
| Caucasian | 72.0 | 68.0 | 84.0 | ||||||
| African American | 16.0 | 20.0 | 14.0 | ||||||
| Hispanic | 8.0 | 8.0 | 2.0 | ||||||
| Asian | 4.0 | 4.0 | 0.0 | ||||||
Note: Degrees of freedom are Welch corrected when necessary for violation of homogeneity of variance as assessed by Levene’s test.
A summary of participant developmental characteristics obtained from the Behavior Sample in the second year and from the MSEL obtained at the follow-up evaluation is presented in Table 2. The children ranged in age from 18.24 to 26.86 months at the time of the Behavior Sample. The ASD group was well-matched on age with the TD group using the Mervis & Klein-Tasman (2004) criterion, and minimally matched with the DD group at the Behavior Sample. The ASD and DD groups were well-matched on the Symbolic Composite of the CSBS DP, indicating they were matched on developmental level in the second year. The ASD group was significantly different than the TD group on all three CSBS DP composites as well as the total score. There were no significant group differences in age across the three groups at the follow-up evaluation. Because several children in this study achieved the lowest possible standard score on the MSEL, a developmental quotient (DQ) based on age equivalent divided by chronological age multiplied by 100, was used to more fully characterize individual variation. Nonverbal DQ was calculated from the average of the Fine Motor and Visual Reception scales, and verbal DQ from the average of the Receptive and Expressive Language scales. The MSEL scores in Table 2 indicate a wide range of functioning in the ASD and DD groups. There were no significant differences between the ASD and DD group on verbal or nonverbal DQ, although the p-values for these differences did not meet the criterion of >.50 for optimal matching. As expected, the ASD group was significantly different than the TD group on verbal and nonverbal DQ. Sixty-two percent of the ASD group had a nonverbal DQ above 70, indicating a relatively higher level of functioning, and 48% had a verbal DQ above 70. In the DD group, 72% had a nonverbal DQ above 70 and 68% had a verbal DQ above 70. At the time of the follow-up evaluation, 27 children in the ASD group (54%) received a best estimate diagnosis of autistic disorder and 23 (46%) received a diagnosis of pervasive developmental disorder not otherwise specified (PDD-NOS). Given the small sample size of the autism and PDD-NOS groups, as well as research indicating diagnoses within the spectrum are not stable in the early years (Charman et al., 2005; Cox et al., 1999; Lord, 1995; Lord et al., 2006; Stone et al., 1999), the present study will examine the sample of children with autism spectrum disorders as one group and will not compare autism and PDD-NOS subgroups.
Table 2.
Summary of Developmental Characteristics
| ASD (n = 50) |
DD (n = 25) |
TD (n =50) |
p value of pairwise differences |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | M | SD | M | SD | M | SD | F value | DD-ASD | TD-ASD |
| CSBS DP behavior sampled | |||||||||
| Age in months | 21.29a | 1.92 | 20.64a | 1.56 | 21.07a | 1.75 | 1.23 | .321 | .911 |
| Social composite | 5.00a | 2.36 | 7.92b | 3.21 | 11.38c | 2.57 | 82.77*** | .001 | .000 |
| Speech composite | 5.82a | 2.62 | 7.16a | 2.59 | 10.26b | 2.43 | 39.86*** | .116 | .000 |
| Symbolic composite | 5.82a | 3.07 | 6.52a | 2.60 | 10.96b | 2.56 | 48.77*** | .661 | .000 |
| Total | 73.88a | 12.62 | 81.64b | 11.86 | 102.54c | 11.26 | 75.77*** | .035 | .000 |
| Mullen scales of early learning e | |||||||||
| Age in months | 38.98a | 9.83 | 35.85a | 6.11 | 35.45a | 5.42 | 1.23 | .258 | .085 |
| Nonverbal DQ | 76.00a | 25.81 | 84.48a | 20.12 | 114.08b | 17.48 | 44.45*** | .325 | .000 |
| Verbal DQ | 68.00a | 31.11 | 77.26a | 21.04 | 108.93b | 15.52 | 46.96*** | .345 | .000 |
Note: Means in the same row with different subscripts differ significantly at p <.05 on the post-hoc Dunnet T3 comparison; Degrees of freedom are Welch corrected when necessary for violation of homogeneity of variance as assessed by Levene’s test.
Standard Scores based on a M of 10 and SD of 3 for the Composite and M of 100 and SD of 15 for the Total.
Developmental Quotients (DQ) based on age equivalent divided by chronological age multiplied by 100
p <.05
p <.01
p <.001
Communication Measures from the Behavior Samples
Communication measures were obtained from the videotaped CSBS DP Behavior Sample collected between 18 and 24 months of age. The Behavior Sample is a face-to-face evaluation of the child interacting with a parent and a clinician during a series of communicative temptations designed to entice or tempt the child to communicate spontaneously, including a wind-up toy, balloon, bubbles, bag of toys, and a jar of cheerios. In addition, book sharing, comprehension probes, and opportunities for symbolic and constructive play are presented. Communication measures for this study were coded during all Behavior Sample activities with the exception of the comprehension probes and constructive play, which are at the end of the sample. These two activities were not included because they consist primarily of giving verbal instructions for the child to follow, thus minimizing opportunities for communicative acts. The child’s caregiver was present during the evaluation and encouraged to participate and respond to the child naturally but not direct the child’s behavior. All videotaped Behavior Samples were re-coded using the Observer® Video-Pro 5.0 software by Noldus Information Technology, allowing for measurement of the frequency, duration, and co-occurrence of operationally defined behaviors. Coders blind to participant diagnoses and the purpose of the study were trained on the coding definitions. Children representative of those in this investigation, but not included in the data analyses, were used to train the coders on the various coding parameters. Prior to coding data to be analyzed, coders were trained to the criterion level of kappa > .6. Behavior Samples were re-coded on the following parameters, with the CSBS (Wetherby & Prizant, 1993) as the basis for the coding definitions for communicative acts and functions.
Communicative acts
A communicative act is an interactive behavior that consists of a gesture, vocalization, or verbalization that is directed toward another person and that serves a communicative function. The decision to code an act was based on three criteria: 1) the act was a gesture, vocalization or verbalization; 2) the act was directed to another person; and 3) the act served a communicative purpose (function). A vocal/verbal act was directed by either a gesture or eye gaze. A gestural act was directed by the movement toward the person, touching the person, or using either a vocalization or eye gaze with the gesture. Thus, a simple contact gesture or motor movement, such as touching another person, giving an object, or pushing an object away, met the criterion of being directed toward another person by the movement or touch and did not have to be used with eye gaze or a vocalization. The onset and offset were coded for each communicative act to allow for other behaviors (e.g., eye gaze) to be coded and analyzed within communicative acts. The coding of communicative acts differed from that of Wetherby et al. (2007) in that every communicative act was coded for the present study compared to the more restricted CSBS DP standard scoring used by Wetherby et al. which is capped at three acts per activity.
Communicative functions
Once a communicative act was identified, the function of the act was coded using three major categories (Bruner, 1981; Wetherby & Prizant, 2002).
Behavior regulation: acts used to regulate the behavior of another person to obtain a specific result. The child’s goal was to get another person to do something (i.e., request) or stop doing something (i.e., protest).
Social interaction: acts used to attract or maintain another’s attention to oneself. The child’s goal was to get another person to look at or notice him or her.
Joint attention: acts used to direct another’s attention to an object, event, or topic. The child’s goal was to get another person to look at or notice something. This involved commenting on an object/action or requesting information.
Judgments about communicative function were inferred from the context based on the child’s communicative goal or purpose (Wetherby & Prizant, 2002). If it was clear that the child was communicating for one of the three communicative functions described above, but there was insufficient information to determine which function category was most appropriate, the communicative act was coded as unclear.
Communicative gestures
A communicative gesture is a nonvocal action directed to another person that serves a communicative function. For each communicative act, it was determined whether the child used a gesture during the act. It was possible for more than one gesture to be coded within a single communicative act. Gestures were coded within the following three categories.
Deictic: gestures used to establish reference to indicate or call attention to an object or event (Iverson & Thal, 1998). The following deictic gestures were coded: give, push/pull away, reach, show, tap, point, indicative, throw/drop/hit, moving object toward adult, and using another’s hand as a tool.
Representational: gestures used to establish reference and carry some fixed semantic content (Iverson & Thal, 1998). Representational gestures included: head shake, wave, clap, head nod, and depictive gesture or sign.
Contact without objects: gestures used to direct communication but not involving objects or carrying fixed semantic contact. This category was mutually exclusive with deictic or representational gestures. Contact without objects included: reaching toward or touching an adult or self injury (e.g., slapping or hitting self).
Communicative vocalizations
For each communicative act, it was determined whether the child produced a vocalization during the act. Transcribable vocalizations, those that contain a recognizable vowel sound, as well as nontranscribable vocalizations, such as a laugh, cry, raspberry, or squeal were counted as vocalizations. Verbalizations (e.g., single and multi-word spoken utterances) also were counted as vocalizations. Noncommunicative vocalizations, that is, vocalizations that were not directed to another person, were not coded as part of the present study.
Eye gaze
Eye gaze was coded independent of and within communicative acts. Coders determined where the child was directing his/her gaze based on the following categories: (a) a person’s face, (b) body, or (c) hand, (d) an object, (e) an object in a person’s hand, and (f) other. Eye gaze alone was not considered a communicative act but could be used to direct an act if the child looked at the person’s face immediately before, during, or after the act. Gaze to a person’s face was coded any time the child was looking toward another’s face (i.e., from the chin upward), including the caregiver, clinician, or another visible person.
Interrater Reliability
Interrater reliability for communicative acts and associated measures was calculated using Cohen’s kappa coefficients, percent agreement, and generalizability (g) or intraclass correlation coefficients for approximately 25% of the data. Cohen’s kappa has values ranging from 0 to 1, with values between .40 and .60 indicating fair agreement, .60 to .75 indicating good agreement, and values over .75 indicating excellent agreement (Fleiss, 1981). The g coefficient is a measure of the source and magnitude of variance accounted for by the subjects and the raters. A g coefficient approaches 1 as the variance accounted for by the subjects is large in comparison with the variance accounted for by raters (Bakeman & Gottman, 1997). G coefficients of .6 or greater are considered acceptable for demonstrating inter-rater reliability (Mitchell, 1979).
For communicative acts, agreement was calculated for the state of communicative acts (i.e., the onset and offset) and communicative function. A kappa of .78 was obtained for the state of total communicative acts, with percent agreement at 88.7%, indicating excellent agreement. Reliability measures for communicative function for total acts indicate excellent agreement overall, with a kappa of .86 and 91.4% agreement. Percent agreement and g coefficients calculated for each communicative function indicate good agreement for behavior regulation, social interaction, and joint attention, with g coefficients of .85, .94, and .96 respectively, and percent agreement of 88% for behavior regulation and joint attention, and 75% for social interaction. Percent agreement for unclear acts was low, at 32%. However, there were very few unclear acts coded. That, in combination with the .70 g coefficient suggests adequate agreement.
To determine agreement between raters on total gestures, percent agreement was calculated from a 2 × 2 confusion matrix that included gesture and no gesture. Percent agreement of 85% and a g coefficient of .95 were obtained, indicating good agreement on identifying the presence of a gesture. Agreement was also calculated on overall gesture type, with deictic, representational, and contact without object gestures combined. A kappa of .72 was obtained, with 77% agreement. The percent agreement calculated individually for deictic, representational, and contact without object gestures indicate high interrater reliability, with agreement of 97% for deictic, and 100% for representational and contact without object gestures. The g coefficients for these gesture categories ranged from .97 to .98.
Interrater reliability was also calculated for communicative vocalizations and eye gaze. When a communicative act was coded, the coder decided whether the act contained a vocalization. A kappa of .85, percent agreement of 94%, and a g coefficient of .94 were obtained on vocalizations within acts, indicating excellent agreement on this measure. For eye gaze, a kappa of .70 was obtained for total eye gaze, indicating good agreement overall. Percent agreement was calculated for eye gaze to face, with 64% agreement and a g coefficient of .97.
Results
A series of one-way analyses of variance (ANOVA) were used to examine group differences on rate of total communicative acts and the proportion of acts for the three communicative functions, differences on the rate of total gestures and the proportion of gestures for the three gesture categories, and differences on the coordination of communicative means. Significant effects were followed-up with pair-wise comparisons to evaluate differences among the three groups using the Dunnett T3. Profile analyses were conducted to compare group profiles on communicative functions and gestures using a mixed ANOVA, with one between-subjects factor of group (ASD, DD, TD) and one within-subjects factor of function (behavior regulation, social interaction, joint attention) or gesture (deictic, representational, and contact without object). Prior to conducting profile analyses, scores for all variables were converted to z-scores to standardize the data set, putting the relative differences in the same metric (Tabachnick & Fidell, 2007). Partial eta squared (η2) was used as a measure of effect size. Values of .01, .06, and .14 are by convention interpreted as small, medium, and large effect sizes, respectively (Green & Salkind, 2003).
Rate of Communicative Acts
The mean length of the Behavior Sample, excluding comprehension probes and constructive play, was 18 minutes and 22 seconds (SD=04:27) for the ASD group, 17 minutes and 46 seconds (SD=02:55) for the DD group, and 18 minutes and 28 seconds (SD=03:03) for the TD group, which was not significantly different across groups, F = 0.29, p= .746. Prior to deriving rate of acts, unclear communicative acts, which were acts used for a communicative purpose but with insufficient information to determine which function category, were examined. The total number of unclear acts was 26 (2.3%) for the ASD group, 16 (2.0%) for the DD group, and 43 (1.9%) for the TD group, which was not significantly different, F = 0.96, p= .385. Given the small percentage of unclear acts and the nonsignificant difference across groups, unclear acts were excluded from all analyses.
A summary of mean scores, standard deviations, and effect sizes of group differences for rate of total communicative acts are presented in Table 3. The ASD group communicated at a rate of 1.23 acts per minute (SD=.83), which was significantly lower than the DD group at 1.81 acts per minute (SD=.83) and the TD group at 2.40 (SD=.78). A large effect size was observed for the ASD-TD comparison and a medium effect size for ASD-DD. Because the significant group difference on rate of total communicative acts alone could account for subsequent group differences on rate measures, proportion measures were used in all subsequent analyses of acts.
Table 3.
Group Differences in Rate of Total Acts and Gestures, and Proportion of Acts and Gestures for Each Communicative Function/Category
| Pairwise group differences |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ASD (n = 50) |
DD (n = 25) |
TD (n = 50) |
DD-ASD |
TD-ASD |
|||||||
| Measure | M | SD | M | SD | M | SD | F value | p value | Effect sized | p value | Effect sized |
| Rate of Total Acts | 1.23a | 0.83 | 1.81b | 0.83 | 2.40c | 0.78 | 26.17*** | .019 | 0.70 | .000 | 1.45 |
| Functions (%) | |||||||||||
| Behavior Regulation | 65.16a | 22.12 | 52.80ab | 19.81 | 49.62b | 18.26 | 7.92** | .052 | −0.59 | .001 | −0.77 |
| Social Interaction | 19.71a | 20.39 | 13.19ab | 16.13 | 11.51b | 9.90 | 3.24* | .354 | −0.36 | .037 | −0.54 |
| Joint Attention | 15.12a | 15.13 | 34.01b | 19.89 | 38.86b | 17.56 | 25.67*** | .000 | 1.08 | .000 | 1.45 |
| Rate of Total Gestures | 1.16a | 0.77 | 1.73b | 0.85 | 2.09b | 0.75 | 17.99*** | .021 | 0.70 | .000 | 1.22 |
| Proportion of Gestures (%) | |||||||||||
| Deictic | 66.10a | 25.46 | 84.36b | 12.22 | 83.44b | 11.85 | 10.39*** | .000 | 0.97 | .000 | 0.93 |
| Representational | 8.92a | 16.43 | 8.71a | 10.18 | 12.34a | 10.51 | 1.06 | 1.000 | −0.02 | .519 | 0.25 |
| Contact without objects | 24.98a | 25.43 | 6.93b | 9.24 | 4.22b | 8.20 | 15.00*** | .000 | −1.04 | .000 | −1.23 |
Note: Means in the same row with different subscripts differ significantly at p <.05. Rate reflects number of acts/gestures per minute.
Proportion is the number of acts/gestures for each function/category divided by the total number of acts/gestures.
Degrees of freedom are Welch corrected when necessary for violation of homogeneity of variance as assessed by Levene’s test.
Effect size based on Cohen’s d = .20 is small, .50 is medium, and .80 is large
p <.05
p <.01
p <.001
Communicative Functions
The proportion of acts for each communicative function (i.e., behavior regulation, social interaction, joint attention) was calculated using the number of communicative acts for each function divided by the total number of acts. As shown in table 3, results indicate that children with ASD used a significantly greater proportion of acts for both behavior regulation and social interaction compared to the TD group. Compared to the DD group, children with ASD used a marginally greater proportion of acts for behavior regulation, which was a nonsignificant trend with a medium effect size, but no significant difference on acts for social interaction. Children with ASD used a significantly lower proportion of acts for joint attention compared to children with DD and TD.
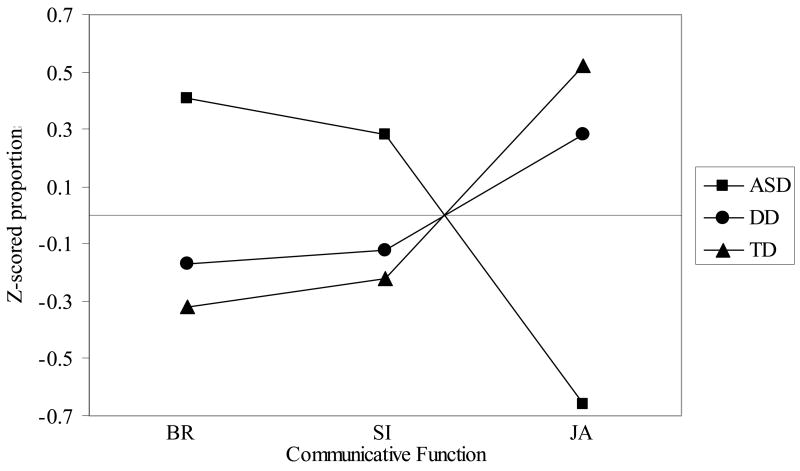
Figure 1 shows the profile plot of the mean proportion of total acts for behavior regulation, social interaction, and joint attention for the three groups. The profile analysis revealed a significant group by function interaction, [F(2, 122) = 11.26, p = .000; η2 = .156]. After examining the profile plot, interaction contrasts were conducted to examine the difference between behavior regulation and joint attention in the ASD group compared to the difference in behavior regulation and joint attention in the TD and DD groups, to determine whether the difference between these two communicative functions was different for different diagnostic groups. The interaction contrast was significant [F(2,122) = 18.30, p = .000; η2 = .231], with follow-up tests revealing a significant difference between the ASD and TD groups [F(1,122) = 34.21, p = .000; η2=.219] and the ASD and DD groups [F(1,122) = 14.43, p = .000; η2 = .106]. The ASD group was higher on behavior regulation and lower on joint attention compared to the DD and TD groups, who were lower on behavior regulation and higher on joint attention. Simple contrasts examining differences in means between behavior regulation and joint attention within group revealed that the ASD group was significantly lower on proportion of joint attention compared to behavior regulation [F(1,49) = 24.18, p = .000; η2 = .330]. In contrast, children with TD were significantly higher on proportion of joint attention than behavior regulation [F(1,49) = 12.80, p = .001; η2 = .207]. The within group contrast between behavior regulation and joint attention was not significantly different for the DD group [F(1,24) = 1.65, p = .211; η2 = .064].
Figure 1.
Profile plot of the mean proportion of communicative acts for behavior regulation, social interaction, and joint attention for children with ASD, DD, and TD.
Communicative Gestures
A summary of mean scores, standard deviations, and effect sizes of group differences for rate of total communicative gestures are presented in Table 3. Significant group differences were found for rate of total communicative gestures, with a mean rate of 1.16 per minute (SD=.77) for the ASD group, 1.73 (SD=.85) for the DD group, and 2.09 (SD=.75) for the TD group. Post hoc tests revealed that the ASD group was significantly lower than both the DD and TD groups, with medium to large effect sizes observed. The pattern of rate of communicative gestures across groups was similar to that observed for total communicative acts, with a large correlation (r = .98) observed between rate of gestures and acts. The proportion of gestures for each gesture category (i.e., deictic, representational, contact without object) was calculated by dividing the number of communicative gestures for each category by total gestures. As shown in Table 3, the ASD group was significantly lower than DD and TD on proportion of deictic gestures, with large effect sizes observed. In contrast, children with ASD showed a significantly higher proportion of contact without object gestures than both other groups. Differences were not observed on the proportion of representational gestures. It should be noted that of the 17 gestures coded in this study, self-injury was the only gesture not observed in any children in this sample. Thus, reach/touch adult was the only gesture coded in the category of contact without object gestures.
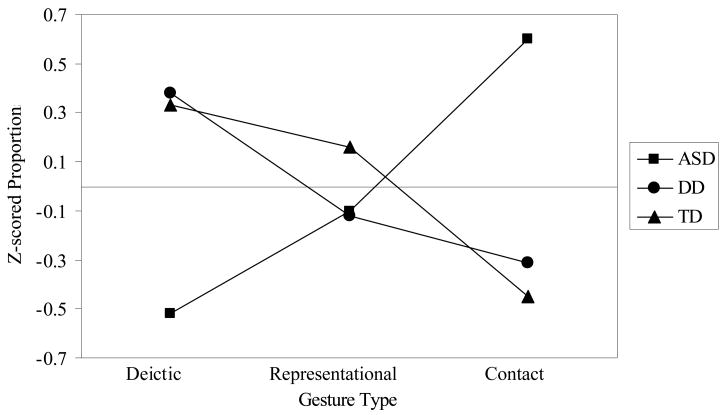
Figure 2 shows the profile plot of the mean proportion of deictic, representational, and contact without object gestures for the three groups. The profile analysis revealed a significant group by gesture interaction, F(2, 122) = 10.71, p = .000; η2 = .149). After examining the profile plot, three interaction contrasts were conducted. The first contrast, which examined the difference between deictic and representational gestures in the ASD group compared to the difference in the TD and DD groups, was significant [F(2,122) = 3.09, p = .049; η2 = .048]. Follow-up tests revealed a significant difference between the ASD and DD groups [F(1,122) = 5.20, p = .024; η2 = .041], with the ASD group using a lower proportion of deictic gestures and a higher proportion of representational gestures in contrast to the DD group, who showed the reverse pattern. The ASD and TD groups were not significantly different [F(1,122) = 3.31, p = .071; η2=.026]. Simple contrasts revealed no significant within group differences for the ASD [F(1,49) = 2.12, p = .152; η2 = .041], DD [F(1,24) = 3.84, p = .062; η2 = .138], or TD [F(1,22) = .89, p = .350; η2=.018] groups.
Figure 2.
Profile plot of the mean proportion of deictic, representational, and contact without object gestures for children with ASD, DD, and TD.
The second interaction contrast examined the difference between deictic and contact without object gestures in the ASD group compared to the difference in these gestures in the TD and DD groups, and was significant [F(2,122) = 18.81, p = .000; η2 = .236]. Follow-up tests revealed a significant difference between the ASD and TD groups [F(1,122) = 32.34, p = .000; η2=.210] and the ASD and DD groups [F(1,122) = 19.53, p = .000; η2 = .138], with the ASD group using a lower proportion of deictic gestures and a higher proportion of contact without object gestures in contrast to the DD and TD groups, who showed the reverse pattern. Simple contrasts revealed a significant within group difference for all three groups, with the ASD group significantly lower on proportion of deictic gestures compared to contact without object gestures [F(1,49) = 10.93, p = .002; η2 = .182] in comparison to the TD [F(1,49) = 40.30, p = .000; η2 = .451] and DD [F(1,24) = 13.06, p = .001; η2=.352] groups, who were significantly higher on proportion of deictic compared to contact without object gestures.
The third interaction contrast examined the difference between representational and contact without object gestures. This contrast was significant [F(2,122) = 9.64, p = .000; η2 = .136], with follow-up tests showing a significant difference between ASD and TD [F(1,122) = 18.78, p = .000; η2 = .133] as well as ASD and DD [F(1,122) = 5.86, p = .017; η2 = .046]. Simple contrasts revealed a significant within group difference for the ASD and TD groups, with the ASD group significantly lower on proportion of representational gestures compared to contact without object [F(1,49) = 5.81, p = .020; η2 = .106]. In contrast, the TD group was significantly higher on proportion of representational compared to contact without object gestures [F(1,49) = 19.21, p = .000; η2 = .282]. This within group contrast was not significant for the DD group [F(1,24) = .96, p = .338; η2 = .038].
Coordination of Vocalization, Eye Gaze, and Gesture
Proportions for acts directed with a vocalization, acts directed with eye gaze, and acts coordinated with vocalization, eye gaze, and gesture were computed using the number of communicative acts directed with each of these communicative means divided by the number of total acts for each communicative function. Proportion measures for coordinated acts could not be calculated for children who had no communicative acts coded for a particular communicative function; therefore, the sample size was smaller for analyses examining group differences in proportion of coordinated acts for social interaction and joint attention.
As shown in Table 4, the ASD group used a significantly lower proportion of total acts and behavior regulation acts with vocalizations compared to the TD group. No significant differences were observed between the ASD and DD groups on proportion of acts directed with a vocalization. In addition, no group differences were observed for the proportion of acts with eye gaze for any function. However, large variances were observed on the proportion of acts directed with eye gaze, which may have masked group differences. No group differences were observed for the proportion of total acts coordinated with a vocalization, eye gaze, and gesture, but a significant difference with a medium effect size was observed between ASD and TD on proportion of coordinated behavior regulation acts. Analyses conducted to examine profiles across functions for acts directed with a vocalization, acts with eye gaze, and acts coordinated with a vocalization, eye gaze, and gesture revealed no significant group by function interaction for acts directed with a vocalization [F(2, 90) = 1.25, p = .292; η2 = .027], acts with eye gaze [F(2, 90) = 1.11, p = .352; η2 = .024], or acts coordinated with a vocalization, eye gaze, and gesture [F(2, 90) = .62, p = .651; η2 = .014].
Table 4.
Group Differences in Proportion of Acts with a Vocalization, Eye Gaze, and Coordinated with Vocalization, Gaze, and Gesture
| Pairwise group differences |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ASD (n = 50) |
DD (n = 25) |
TD (n = 50) |
DD-ASD |
TD-ASD |
|||||||
| Measure | M | SD | M | SD | M | SD | F value | p value | Effect sized | p value | Effect sized |
| Acts with Vocalization (%) | |||||||||||
| Total Acts | 54.46a | 27.01 | 59.36a | 31.40 | 76.74b | 18.96 | 12.39*** | .879 | 0.17 | .000 | 0.97 |
| Behavior Regulation | 47.30a | 31.03 | 52.34ab | 34.94 | 67.62b | 24.90 | 6.92** | .903 | 0.15 | .001 | 0.73 |
| Social Interaction | 50.14a | 36.36 | 59.96a | 36.70 | 64.74a | 31.23 | 1.94 | .679 | 0.27 | .149 | 0.43 |
| Joint Attention | 85.08a | 27.47 | 72.63a | 31.77 | 87.64a | 16.97 | 2.16 | .350 | −0.42 | .945 | 0.12 |
| Acts with Gaze (%) | |||||||||||
| Total Acts | 42.26a | 27.30 | 49.87a | 16.93 | 51.96a | 17.16 | 2.25 | .368 | 0.34 | .105 | 0.44 |
| Behavior Regulation | 22.39a | 26.53 | 27.47a | 29.88 | 30.61a | 30.70 | 1.02 | .853 | 0.18 | .395 | 0.29 |
| Social Interaction | 54.79a | 46.69 | 73.69a | 31.31 | 63.25a | 31.16 | 1.80 | .180 | 0.48 | .707 | 0.22 |
| Joint Attention | 60.60a | 38.65 | 51.86a | 30.07 | 53.18a | 20.42 | 0.61 | .709 | −0.25 | .650 | −0.25 |
| Acts Coordinated with Vocalization, Gaze, and Gesture (%) | |||||||||||
| Total Acts | 17.17a | 14.69 | 20.62a | 15.84 | 22.94a | 10.88 | 2.47 | .742 | 0.23 | .081 | 0.45 |
| Behavior Regulation | 14.80a | 13.05 | 20.93ab | 22.93 | 24.16b | 15.29 | 5.45 | .525 | 0.34 | .004 | 0.66 |
| Social Interaction | 23.79a | 25.77 | 27.86a | 29.29 | 23.19a | 23.98 | 0.26 | .929 | 0.15 | .999 | −0.02 |
| Joint Attention | 13.52a | 20.29 | 18.62a | 18.20 | 20.83a | 12.52 | 1.82 | .690 | 0.27 | .170 | 0.45 |
Note: Means in the same row with different subscripts differ significantly at p <.05.
Proportion is the total number of coordinated acts for each function divided by the total number of acts for that function.
Degrees of freedom are Welch corrected when necessary forviolation of homogeneity of variance as assessed by Levene’s test.
Effect size based on Cohen’s d = .20 is small, .50 is medium, and .80 is large
p <.05
p <.01
p <.001
Predictive Relations with Verbal and Nonverbal Developmental Level
Correlations between communicative acts in the second year of life and verbal and nonverbal DQ on the MSEL completed at 36 month of age or older (n = 40) were computed for children in the ASD group. After controlling for the effects of age, moderate to large significant correlations were observed between rate of communicative acts and verbal DQ (r = .51, p = .019) and between rate and nonverbal DQ (r = .47, p = .031). A moderate significant relation was observed between the proportion of joint attention acts and verbal DQ (r = .47, p = .03). Moderate marginally significant correlations were observed between the following communication measures in the second year and verbal DQ: proportion of behavior regulation acts with a vocalization (r = .38, p = .086), and proportion of joint attention acts coordinated with a vocalization, eye gaze, and gesture (r = .40, p = .077).
Discussion
The purpose of this study was to precisely examine the communicative acts of children between 18 and 24 months of age later diagnosed with ASD (referred to as ASD). Although major advances have been made in understanding communication impairments, including differences in rate, functions, and means of communication of children 2 to 5 years of age with ASD (e.g., Charman et al., 2005; Dawson et al., 2004; Mundy et al., 1990; Stone et al., 1997; Wetherby et al., 1998), relatively little is known about the communicative profiles of children with ASD younger than 2 years. Findings from this study provide important information on the core communication deficits of children with ASD in the second half of the second year of life and offer insight into how young children with ASD are similar and different in their communication compared to children with DD and TD. This discussion will highlight findings on communicative rate, functions, and means, including the unique profile of communication exhibited by children with ASD late in the second year.
Rate of Communicative Acts
Children with ASD in this sample communicated at a significantly lower rate than children with DD and TD. The mean rate of 1.23 (SD=.83) acts per minute in the present ASD sample is lower than that found for the two samples of children reported on by Drew et al. (2007) who were recruited using the CHAT and assessed using sampling procedures similar to those used in the present study. Nonverbal functioning was quite similar across the samples of children, ranging from 74.8 (SD = 19.4) for Sample 1 (mean age = 20.7 months) and 79.6 (SD = 10.2) for Sample 2 (mean age = 25.0 months) in the Drew et al. study and 76.0 (SD = 25.81) in the present sample. The nonverbal measures used across these studies were similar, with Drew et al. reporting a nonverbal developmental quotient obtained from two scales of the Griffiths Scale of Infant Development that measure similar skills to the Visual Reception and Fine Motor scales of the MSEL used to measure nonverbal functioning in the present study. In comparing the severity of the samples, 54% of the present ASD sample met criteria for a diagnosis of autistic disorder, which was much lower than the 87% reported for Sample 2, but nearly identical to that reported for Sample 1 (53%). It is likely that the differences in rate of communication between these studies may be accounted for by differences in the definition and identification of communicative acts, which were more stringent in the present study. Communicative acts had to be a gesture and/or vocalization and directed toward another person using a gesture, vocal/verbalization, or eye gaze to be coded in the present study. In comparison, isolated behaviors such as eye gaze toward a person, vocalizing/verbalizing, and pointing were coded as communicative acts in the Drew et al. (2007) study. In the present study, although eye gaze, vocalizing, or pointing could be used to direct a communicative act to another person, these isolated behaviors were not coded as communicative acts. Drew et al. (2007) also noted that during their adult-child interaction, the clinician provided as much adult scaffolding as necessary to help the child display communicative abilities and that the researchers included more early forms of communication than previous studies, stating, “One risk of ‘generously’ coding potentially communicative behaviors as communication is that we were ascribing competence where it was not present” (p. 658).
Results of the present study, indicating that rate of communication is a core deficit of ASD at 18 to 24 months of age, confirm and extend the findings of Wetherby et al. (2007), who recently examined the social communicative skills of 123 of the 125 participants recruited for the present investigation using the standard scoring of the CSBS DP. Although rate was calculated differently across the two studies, coding definitions of communicative acts for the present investigation were developed based on the CSBS DP (Wetherby & Prizant, 2002); therefore, it seems logical that findings from these two studies would be in agreement. Results from the present study also extend the findings of Wetherby et al. by providing a more precise measure of communicative rate in this sample of children. Specifically, in contrast to Wetherby et al. (2007), in which cutoffs were obtained through standard scoring, the present study systematically measured every communicative act during the Behavior Sample, providing a precise rate per minute of communicative acts in this sample of children. This precise measurement helps to describe this young population by offering normative as well as descriptive data for ASD.
The importance of measuring communicative rate is highlighted by recent findings in which rate of communication between 18 and 24 months of age was correlated with all other social communication skills measured in the second year, predicted nonverbal cognitive level, and was moderately correlated with communication symptoms of autism at approximately 3 years of age (Wetherby et al., 2007). Findings from the present study also showed that rate of communication late in the second year was the strongest predictor of verbal and nonverbal outcome at 3 years of age. Communicative rate in children with ASD at age 2 has also been shown to be significantly associated with outcome in several domains at age 7, while standard measures of cognitive and language ability collected at age 2 did not predict outcome (Charman et al., 2005). In contrast, findings from a recent study of a large sample of children with autism followed from age 2 to 5 indicated that nonverbal cognitive ability at age 2 was the strongest predictor of language at age 5. At age 3, communication scores were a stronger predictor of language at 5 years (Thurm, Lord, Lee, & Newschaffer, 2007). However, Thurm et al. reported on slightly older children than those in the present sample and did not include a measure of communication rate, making direct comparison of predictors difficult. Overall, research suggests that predictors of language may vary over time. Charman et al. (2005) suggested that assessing early social communication skills, such as communicative acts, may be more important than measuring IQ and formal language abilities in very young children with ASD. The findings of this study support the importance of communicative rate late in the second year as a predictor of developmental level and autism symptoms at 3 years of age, and underscore the important role of the SLP in assessing social communication skills in young children.
Given that rate of communication appears to be a core deficit of ASD as early as 18 to 24 months of age and is likely to help distinguish ASD from other developmental delays, it is useful to consider what rate of communication is reflecting. Charman et al. (2005) suggested that rate may be an index of an intrinsic social motivation and thus a measure of autism severity associated with better outcomes. Rate has also been described as a reflection of a child’s repertoire of social communication skills and a useful index of initiating and responding to social bids, with predictive relations between rate and outcome reflecting a transactional process, such that children with higher communication rates have a better likelihood of impacting the social environment by creating a greater number of opportunities for interaction (Wetherby et al., 2007). The data from the present study provide further support that by 18 to 24 months of age, children with ASD show a discrepancy in rate of communication. This disturbance, or decreased tendency to initiate interactions, may exacerbate subsequent social symptoms and atypical neurodevelopmental outcomes (Mundy & Burnette, 2005). As suggested by Mundy and Burnette, it will be particularly important to understand the way in which “the early onset of impairments in major milestones of social development potentially contributes to the subsequent unfolding of the full syndrome of autism across the first years of life” (p. 656).
Communicative Functions
Findings for the three communicative functions point to a core deficit in communicating for joint attention in children with ASD between 18 and 24 months of age, such that a deficit in joint attention is more specific to ASD rather than being more generally associated with other developmental delays. This extends downward a consistent finding on preschoolers with ASD (Sigman et al., 1986; Stone & Caro-Martinez, 1990; Stone et al., 1997; Wetherby et al., 1998) and extends those of previous studies of children with ASD under 2 years (Drew, 2007; Werner and Dawson, 2005; Wetherby et al., 2004; 2007), providing precise information on the proportion of acts used for different communicative functions in children with ASD between 18 and 24 months. The profile of communication observed in the ASD group, with a pattern of deficit in communicating for joint attention compared to communication used to regulate the behavior of another person, also appears to be specific to ASD rather than being characteristic of general developmental delay. These findings demonstrate that young children with ASD do communicate, but communicate predominately for behavior regulation rather than for the purpose of commenting or sharing attention on an object or event of interest.
In considering findings on the three communicative functions, it is useful to consider the types of acts coded within each function. Behavior regulation involves requesting or protesting, and serves a less social, imperative or instrumental function (Mundy & Burnette, 2005; Wetherby, 2006; Wetherby & Prizant, 2002). In contrast, communicating for joint attention involves social sharing, with the child directing another person’s attention to comment or get the other person to look at or notice something. Social interaction generally involves objects less and relies more on dyadic face-to-face interaction between the adult and child. Thus, it may be easier for children with ASD to communicate for social interaction than joint attention because the former generally does not involve the use of objects or the triadic coordination between an object and another person. The profiles of communication observed in this young ASD sample have implications for early intervention. For example, the relative strengths in behavior regulation and social interaction may be used to bootstrap other skills or enhance skills in other areas, including joint attention (Wetherby et al., 2007). Communicating for social interaction may help young children with ASD connect with people and may be an easier place to start than joint attention, because communicating for social interaction does not require the coordination of gaze with an object. Dawson and colleagues (2004) recently reported on joint attention deficits in a group of 3- to 4-year old children with ASD and suggested a social orienting impairment in which the failure to attend to and find social stimuli inherently rewarding may contribute to impairments in joint attention. The researchers discussed the inherent reward that typically developing children experience during affective exchanges that often occur within communicative acts, particularly acts for joint attention. Such early successful exchanges can provide an opportunity for developing communication skills and learning the inherent value of communication to share experiences. Thus, engaging in communicative exchanges for any purpose, including behavior regulation and social interaction, may help children with ASD attend to others and in so doing, build communication for a variety of intentions (Dawson et al., 2004; Wetherby et al., 2007).
Communicative Gestures
Findings from this study suggest that children with ASD between 18 and 24 months exhibit a core deficit in rate of communicative gestures, a finding that is consistent with previous research (Cox et al., 1999; Werner et al., 2005; Wetherby et al., 2007). The rate of gestures observed across groups reflected the pattern observed for rate of total communicative acts, suggesting that many of the communicative acts included a gesture. Findings on gestures in children with ASD younger than 18 months have been somewhat mixed. Using home videotapes from first birthday parties of children later diagnosed with ASD, researchers found no significant differences between ASD and DD groups on overall use of gestures (Osterling et al., 2002), suggesting that at 12 months of age the decreased use of gestures appeared to be associated with developmental delay rather than ASD. In contrast, as reported by parents on the MacArthur Communicative Developmental Inventories – Words and Gestures, at 12 months of age siblings of children with ASD who were later diagnosed with autism were reported to have fewer gestures compared to siblings who received no diagnosis at 2 years and a control group of low-risk infants with no family history of ASD (Zwaigenbaum et al., 2005). Overall, combined research findings suggest that for children with ASD, deficits in gesture use emerge over the first two years of life, with the present study suggesting that by 18 to 24 months, impairment in the use of gestures is not only associated with developmental delay, but is a core deficit of ASD.
This study extends previous research by providing information on the specific types or categories of gestures that may help distinguish children with ASD at this young age. A distinct profile of strengths and weaknesses in communicative gestures was found, with a core deficit in deictic gestures used to establish reference, to indicate or call attention to an object or event, in combination with a higher proportion of contact without object gestures. As discussed by Iverson and Thal (1998), researchers have suggested a close relationship between eye gaze behaviors and the development of deictic gestures. In typical development, infants learn that following the gaze of another person provides valuable information regarding the focus of the other person’s attention, and that others can obtain information by following their line of regard. Understanding that the focus of attention or line of regard is identifiable and can be used to establish reference is important in the development of deictic gestures. Infants between 8 and 14 months of age generally begin to use deictic gestures to establish reference to indicate their focus of attention. This relationship between the development of deictic gestures and early eye gaze behaviors seems particularly interesting for children with ASD, given early impairments in the use of eye gaze. That is, if children with ASD are experiencing impairments in the use of eye gaze in early development, such as following the gaze or focus of attention of another person, this may impede the development of the use of deictic gestures to establish reference. Limited research has been conducted to examine individual deictic gestures, such as pointing and showing, in children with ASD under 24 months of age and has resulted in mixed findings. It will be important for future research to examine the development of individual deictic gestures in children with ASD over the first years of life and to examine these gestures relative to communicative functions.
This is the first study to directly observe and report on representational gestures in children with ASD under 2 years. All groups were observed to use a similar proportion of representational gestures, suggesting that the use of these gestures alone, as conceptualized and measured in this study, may not differentiate children with ASD under 2 years. However, research has shown that children with ASD show deficits in acquiring symbolic aspects of communication including the use of symbolic gestures (Wetherby, 2006). Several factors may have contributed to this finding on representational gestures. For example, the TD group used few representational gestures, indicating that typically developing children have likely moved into the use of words to represent ideas symbolically by this age. Also, a range of gestures were coded in this category, including those that generally emerge early (e.g., clapping) as well as later in development (e.g., head nod). This range, along with the low frequency observed in all groups may have made it difficult to detect differences. Also, these gestures were not examined relative to communicative functions and it may be that children with ASD have difficulty using representational gestures for a variety of communicative functions. In addition, the children with ASD in this study were identified prospectively, leading to a referral for early intervention services. Several children in the ASD group were observed to use sign gestures to communicate, which may be related to early intervention services. Continued research is needed to sort out these methodological limitations and examine the development of representational gestures.
In contrast to deictic and representational gestures, the ASD group showed a significantly higher proportion of contact without object gestures compared to children with DD and TD. This finding may suggest a possible reliance on a more primitive gesture and supports findings indicating a core deficit in the use of deictic gestures. One gesture that was observed and coded in the contact without object category was reach/touch adult. This gesture was not used to establish reference, and thus did not qualify as deictic or representational. Although this gesture was not examined in relation to communicative function, by definition it did not involve an object and thus was used for behavior regulation or social interaction to request comfort, which may provide additional evidence of a core deficit in communicating for joint attention but not behavior regulation and social interaction in children with ASD between 18 and 24 months.
Coordination of Communicative Means
Overall, examination of communicative means revealed somewhat surprising findings, with the ASD group not significantly different from DD on the proportion of total acts directed with a vocalization, eye gaze, and coordinated with vocalization, eye gaze, and gesture. Also, the proportions of acts with these different means were generally not significantly different across groups for each of the functions. For example, although the ASD group used a significantly lower proportion of joint attention acts, the groups were similar on the proportion of joint attention acts directed with a vocalization, eye gaze, and coordinated with vocalization, eye gaze, and gesture. However, not all children communicated for all functions. Thus, children with ASD who did communicate were as likely as other children to direct that communication using coordinated means, suggesting that coordination of communicative means may not be a core deficit in children with ASD between 18 and 24 months of age who are communicating.
In considering factors that may have masked group differences on communicative means, it may be that children with ASD between 18 and 24 months do not show differences in frequency or proportion of means, but rather the type or quality. For example, Wetherby et al. (2004) found that children with ASD in the second year were not significantly different from children with DD on the lack of communicative vocalizations with consonants. However, significantly more unusual prosody was reported in the ASD group, suggesting the need to examine not only the quantity but the quality of vocalizations in young children with ASD. Results of the present study on acts directed with eye gaze were surprising given that eye gaze deficits have been well established in individuals with ASD, including those under 2 years (Charman et al., 1997; Osterling et al., 2002; Swettenham et al., 1998). However, the similarity across groups on proportion of acts directed with gaze in this study does not necessarily equate to the ASD group exhibiting typical gaze behavior. Watt (2006) recently examined eye gaze and repetitive and stereotyped behaviors in 123 of the children this sample and found that the ASD group looked significantly less at others’ faces compared to children with DD and TD, being lower both on rate per minute of eye gaze to face episodes as well as proportion of eye gaze to face, the percentage of time across the Behavior Sample spent looking at another’s face.
It is also possible that children with ASD may show a deceleration in skills/growth across the first years of life. This plateauing or deceleration may be characteristic of the unfolding of the diagnostic features of ASD and continue over the second and into the third year (Landa & Garrett-Mayer, 2006; Ozonoff, 2006). For example, it may be that children with ASD are more able to coordinate communicative means or direct communication with eye gaze in the second half of the second year of life than slightly later. This hypothesis is supported by research on preschool-age children with ASD that has documented core impairments in the ability to coordinate means and direct communicative acts with eye gaze (Phillips et al., 1995; Stone et al., 1997; Wetherby et al., 1998). It is possible that the contrasting findings between preschool-age children with ASD and those obtained in this study relate to the larger sample size or the more precise measures. Although the relative use of coordinated means of communication did not distinguish groups, there was large variance observed in many of the proportion measures. Thus, some children coordinated means of communication better than others, and it may have been that children with ASD who communicated for joint attention were the children who were able to coordinate communicative means. Continued research is needed to further clarify understanding of the communicative means and coordination of communication in young children with ASD to examine possible changes across the first years of life. However, findings from this study on the coordination of communicative means suggest that it will be important for clinicians not to rule out ASD if a child coordinates means of communication.
Limitations and Future Research Directions
Several limitations must be considered in interpreting the results of this study. This study reflects profiles of children between 18 and 24 months who were later diagnosed with ASD. It is not known if these children met diagnostic criteria for ASD in the second year of life and it is possible that the diagnoses could have changed over time. In addition, this ASD sample consisted of a very heterogeneous group of children, with variation on developmental level as well as social communication skills. To match the wide range of cognitive functioning in the ASD group, the DD group also consisted of children with a wide range of functioning, which may have masked the detection of group differences. Although this heterogeneity is characteristic of the ASD population, future research with larger samples divided based on cognitive level will be important. In addition, the ASD group consisted of children with autistic disorder and PDD-NOS. Previous studies have suggested that young children with PDD-NOS show more social interest than children with autism (e.g., Mars, Mauk, & Dowrick, 1998). Thus, it may have been those with PDD-NOS that were more likely to communicate and coordinate means of communication. Also, because the children with ASD in this sample had been identified in the second year, some prior to 18 months, as having a social communication delay, many had been receiving early intervention services. Social communication skills are generally one of the main targets of early intervention for children with ASD, which may have impacted the communication of the children in this sample in a positive direction.
It is also important to consider the impact of the sampling procedures. One of the strengths of this study was the use of direct and systematic observation. However, the Behavior Sample is designed to provide a supportive sampling context, with scaffolding provided as needed to elicit communication. The supportive procedures as well as the semi-structured clinical setting may have impacted the communication of the children in this study, such that children were communicating with a greater frequency and in different ways compared to everyday natural environments. Examination of parent-child interactions in a natural setting would provide information on the effects of the sampling procedures on the communicative profiles of children with ASD. In addition, to aid in early screening and detection, it would be useful to examine the different activities within the Behavior Sample to determine potential activities that are most likely to distinguish children with ASD. Longitudinal research is also needed to further explore how the communication of children with ASD unfolds over the first years of life, examining changes in skills and symptomatology at smaller intervals of time as well as predictive relations of communicative acts to later outcome. In addition, it will be important to separate out the effects of initial differences in cognitive ability as well as the impact of early intervention on the presentation of ASD in young children.
Clinical Implications
Findings from this study provide greater understanding of the communication of children with ASD under 2 years of age and have important clinical implications. The precise measures obtained in this study provide support for the validity of the systematic sampling procedures used in the CSBS DP Behavior Sample in assessing the early social communication skills that may help to identify and distinguish children with ASD late in the second year of life. That is, given the congruency in findings between the precise and detailed measurement of communicative acts obtained in the present study and results obtained in the recent study using the standard scoring of the CSBS DP (Wetherby et al., 2007), this standardized measure may serve as a useful clinical tool for SLPs in assessing and identifying young children with social communication delays.
Recent guidelines from the American Academy of Pediatrics (AAP) recommend screening children for ASD at 18 and 24 months of age. Findings from this study provide information on the skills that may contribute to screening and early detection. The important role of the SLP in early detection was also highlighted in the AAP report, which stated that most children later diagnosed with ASD initially present to their primary care pediatricians with speech delays (Johnson et al., 2007). In addition, parents, care providers, and clinicians may base concerns about the development of communication and language on words. Findings from this study indicate that impairments in the use of prelinguistic social communication behaviors, such as communicative gestures, are also important early indicators of ASD. As suggested by Landa & Garrett-Mayer (2006), continued efforts are needed to provide training and increase awareness of “typical development, normal variation, and red flags indicating the need for developmental screening” (p. 635).
Acknowledgments
Stacy Shumway is associated with the Pediatric & Developmental Neuropsychiatry Branch, National Institute of Mental Health, Bethesda, Maryland. Amy M. Wetherby is associated with the Department of Communication Disorders, Florida State University. This study is based on the first author’s dissertation completed at Florida State University.
This research was supported in part by a grant from the National Institutes of Health, National Institute on Deafness and Other Communication Disorders (1R01DC007462) and a grant from the U.S. Department of Education, Office of Special Education and Rehabilitation Services (H324C030112). This work was written while Dr. Shumway was working at NIMH and was not written as part of the Contributor’s official duties as a Government employee. The views expressed in this article are solely the responsibility of the authors and do not necessarily represent the views of the USDOE, the NIH, or the United States Government. The authors would like to thank the families who gave their time to participate in this project.
Contributor Information
Stacy Shumway, Pediatric & Developmental Neuropsychiatry Branch – National Institute of Mental Health, Bethesda, MD.
Amy M. Wetherby, Florida State University
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: APA; 2000. [Google Scholar]
- American Speech-Language-Hearing Association. Guidelines for Speech-Language Pathologists in Diagnosis, Assessment, and Treatment of Autism Spectrum Disorders Across the Life Span. Rockville, MD: 2006. Available from http://www.asha.org/about/publications/reference-library/ [Google Scholar]
- Bakeman R, Gottman JM. Observing interaction: An introduction to sequential analysis. 2. New York: Cambridge University Press; 1997. [Google Scholar]
- Bates E. The emergence of symbols: Cognition and communication in infancy. New York: Academic Press; 1979. [Google Scholar]
- Bruner J. The social context of language acquisition. Language and Communication. 1981;1:155–178. [Google Scholar]
- Charman T, Swettenham J, Baron-Cohen S, Cox A, Baird G, Drew A. Infants with autism: An investigation of empathy, pretend play, joint attention, and imitation. Developmental Psychology. 1997;33:781–789. doi: 10.1037//0012-1649.33.5.781. [DOI] [PubMed] [Google Scholar]
- Charman T, Taylor E, Drew A, Cockerill H, Brown J, Baird G. Outcome at 7 years of children diagnosed with autism at age 2: Predictive validity of assessments conducted at 2 and 3 years of age and pattern of symptom change over time. Journal of Child Psychology and Psychiatry. 2005;46:500–513. doi: 10.1111/j.1469-7610.2004.00377.x. [DOI] [PubMed] [Google Scholar]
- Chawarska K, Klin A, Paul R, Volkmar F. Autism spectrum disorder in the second year: Stability and change in syndrome expression. Journal of Child Psychology and Psychiatry. 2007;48:128–138. doi: 10.1111/j.1469-7610.2006.01685.x. [DOI] [PubMed] [Google Scholar]
- Clifford S, Young R, Williamson P. Assessing the early characteristics of autistic disorder using video analysis. Journal of Autism and Developmental Disorders. 2007;37:301–313. doi: 10.1007/s10803-006-0160-8. [DOI] [PubMed] [Google Scholar]
- Colgan SE, Lanter E, McComish C, Watson LR, Crais ER, Baranek GT. Analysis of social interaction gestures in infants with autism. Child Neuropsychology. 2006;12:307–319. doi: 10.1080/09297040600701360. [DOI] [PubMed] [Google Scholar]
- Cox A, Klein K, Charman T, Baird G, Baron-Cohen S, Swettenham J, Wheelright S, Drew A. Autism spectrum disorders at 20 and 42 months of age: stability of clinical and ADI-R diagnosis. Journal of Child Psychology and Psychiatry. 1999;40:719–732. [PubMed] [Google Scholar]
- Dawson G, Toth K, Abbott R, Osterling J, Munson J, Estes A, Liaw J. Early social attention impairments in autism: Social orienting, joint attention, and attention to distress. Developmental Psychology. 2004;40:271–283. doi: 10.1037/0012-1649.40.2.271. [DOI] [PubMed] [Google Scholar]
- Drew A, Baird G, Taylor E, Milne E, Charman T. The social communication assessment for toddlers with autism (SCATA): An instrument to measure the frequency, form and function of communication in toddlers with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2007;37:648–666. doi: 10.1007/s10803-006-0224-9. [DOI] [PubMed] [Google Scholar]
- Fleiss JL. Statistical methods for rates and proportions. 2. New York: Wiley; 1981. [Google Scholar]
- Green SB, Salkind NJ. Using SPSS for windows and macintosh: Analyzing and understanding data. 3. New Jersey: Prentice Hall; 2003. [Google Scholar]
- Johnson CP, Myers SM the Council on Children with Disabilities. Identification and evaluation of children with autism spectrum disorders. Pediatrics. 2007;120:1183–1215. doi: 10.1542/peds.2007-2361. [DOI] [PubMed] [Google Scholar]
- Iverson J, Thal D. Communicative transitions: There’s more to the hand than meets they eye. In: Wetherby A, Warren S, Reichle J, editors. Transitions in prelinguistic communication. Baltimore: Paul H. Brookes; 1998. pp. 59–86. [Google Scholar]
- Landa R, Garrett-Mayer E. Development in infants with autism spectrum disorders: A prospective study. Journal of Child Psychology and Psychiatry. 2006;47:629–638. doi: 10.1111/j.1469-7610.2006.01531.x. [DOI] [PubMed] [Google Scholar]
- Lord C. Follow-up of two year-olds referred for possible autism. Journal of Child Psychology and Psychiatry. 1995;36:1365–1382. doi: 10.1111/j.1469-7610.1995.tb01669.x. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, DiLavore PS, Shulman C, Thurm A, Pickles A. Autism from 2 to 9 years of age. Archives of General Psychiatry. 2006;63:694–701. doi: 10.1001/archpsyc.63.6.694. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore P, Risi S. Autism Diagnostic Observation Schedule-Generic. Los Angeles, CA: Western Psychological Services; 1999. [Google Scholar]
- Mars AE, Mauk JE, Dowrick PW. Symptoms of pervasive developmental disorders as observed in prediagnostic home videos of infants and toddlers. Journal of Pediatrics. 1998;132:500–504. doi: 10.1016/s0022-3476(98)70027-7. [DOI] [PubMed] [Google Scholar]
- Mervis CB, Klein-Tasman BP. Methodological issues in group-matching designs: Alpha levels for control variable comparisons and measurement characteristics of control and target variables. Journal of Autism and Developmental Disorders. 2004;34(1):7–17. doi: 10.1023/b:jadd.0000018069.69562.b8. [DOI] [PubMed] [Google Scholar]
- Mitchell SK. Interobserver agreement, reliability, and generalizability of data collected in observational studies. Psychological Bulletin. 1979;86:376–390. [Google Scholar]
- Mitchell S, Brian J, Zwaigenbaum L, Roberts W, Szatmari P, Smith I, et al. Early language and communication developmental of infants later diagnosed with autism spectrum disorder. Journal of Developmental and Behavioral Pediatrics. 2006;27:69–78. doi: 10.1097/00004703-200604002-00004. [DOI] [PubMed] [Google Scholar]
- Mullen E. The Mullen Scales of Early Learning. Circle Pines, MN: American Guidance; 1995. [Google Scholar]
- Mundy P, Burnette C. Joint attention and neurodevelopmental models of autism. In: Volkmar FR, Paul R, Klin A, Cohen D, editors. Handbook of Autism and Developmental Disorders. 3. New Jersey: Wiley; 2005. [Google Scholar]
- Mundy P, Sigman M, Kasari C. A longitudinal study of joint attention and language development in autistic children. Journal of Autism and Developmental Disorders. 1990;20:115–128. doi: 10.1007/BF02206861. [DOI] [PubMed] [Google Scholar]
- Osterling JA, Dawson G. Early recognition of children with autism: A study of first birthday home videotapes. Journal of Autism and Developmental Disorders. 1994;24:247–257. doi: 10.1007/BF02172225. [DOI] [PubMed] [Google Scholar]
- Osterling JA, Dawson G, Munson JA. Early recognition of 1-year-old infants with autism spectrum disorder versus mental retardation. Development and Psychopathology. 2002;14:239–251. doi: 10.1017/s0954579402002031. [DOI] [PubMed] [Google Scholar]
- Ozonoff S. Studying autism in the first year of life: Constructs and caution. 2006, June; Paper presented at the International Meeting for Autism Research (IMFAR); Montreal, Canada. [Google Scholar]
- Phillips W, Gomez JC, Baron-Cohen S, Laa V, Riviere A. Treating people as objects, agents, or “subjects”: How young children with and without autism make requests. Journal of Child Psychology and Psychiatry. 1995;36:1383–1398. doi: 10.1111/j.1469-7610.1995.tb01670.x. [DOI] [PubMed] [Google Scholar]
- Rutter M, Bailey A, Berument S, Lord C, Pickles A. Social communication questionnaire research edition. Los Angeles, CA: Western Psychological Corporation; 2001. [Google Scholar]
- Sigman M, Mundy P, Sherman T, Ungerer J. Social interactions of autistic, mentally retarded, and normal children and their caregivers. Journal of Child Psychology and Psychiatry. 1986;27:647–656. doi: 10.1111/j.1469-7610.1986.tb00189.x. [DOI] [PubMed] [Google Scholar]
- Stone WL, Caro-Martinez LM. Naturalistic observations of spontaneous communication in autism children. Journal of Autism and Developmental Disorders. 1990;20:437–453. doi: 10.1007/BF02216051. [DOI] [PubMed] [Google Scholar]
- Stone WL, Lee E, Ashford L, Brissie J, Hepburn S, Coonrod E, Weiss B. Can autism be diagnosed accurately in children under three years? Journal of Child Psychology and Psychiatry. 1999;40:219–226. [PubMed] [Google Scholar]
- Stone WL, Ousley OY, Yoder PJ, Hogan KL, Hepburn SL. Nonverbal communication in two- and three-year old children with autism. Journal of Autism and Developmental Disorders. 1997;27:677–696. doi: 10.1023/a:1025854816091. [DOI] [PubMed] [Google Scholar]
- Swettenham J, Baron-Cohen S, Charman T, Cox A, Baird G, Drew A, et al. The frequency and distribution of spontaneous attention shifts between social and nonsocial stimuli in autistic, typically developing, and nonautistic developmentally delayed infants. Journal of Child Psychology and Psychiatry. 1998;39:747–753. [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 5. Boston: Allyn & Bacon; 2007. [Google Scholar]
- Thurm A, Lord C, Lee L, Newschaffer C. Predictors of language acquisition in preschool children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2007;37:1721–1734. doi: 10.1007/s10803-006-0300-1. [DOI] [PubMed] [Google Scholar]
- Watt NJ. Repetitive and stereotyped behaviors in children with autism spectrum disorders in the second year of life. Unpublished doctoral dissertation. Florida State University; Tallahassee: 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner E, Dawson G. Validation of the phenomenon of autistic regression using home videotapes. Archives of General Psychiatry. 2005;62:889–895. doi: 10.1001/archpsyc.62.8.889. [DOI] [PubMed] [Google Scholar]
- Werner E, Dawson G, Munson J, Osterling J. Variation in early developmental course in autism and its relation with behavioral outcome at 3–4 years of age. Journal of Autism and Developmental Disorders. 2005;35:337–350. doi: 10.1007/s10803-005-3301-6. [DOI] [PubMed] [Google Scholar]
- Wetherby AM. Understanding and measuring social communication in children with autism spectrum disorders. In: Charman T, Stone W, editors. Social and communication development in autism spectrum disorders: Early identification, diagnosis, and intervention. N.Y: Guilford Publications; 2006. pp. 3–34. [Google Scholar]
- Wetherby A, Prizant B. Communication and Symbolic Behavior Scales Developmental Profile- First Normed Edition. Baltimore, MD: Paul H. Brookes; 2002. [Google Scholar]
- Wetherby A, Prizant B. Communication and Symbolic Behavior Scales - Normed Edition. Chicago, IL: Applied Symbolix; 1993. [Google Scholar]
- Wetherby AM, Prizant BM, Hutchinson TA. Communicative, social/affective, and symbolic profiles of young children with autism and pervasive developmental disorders. American Journal of Speech-Language Pathology. 1998;7:79–91. [Google Scholar]
- Wetherby A, Watt N, Morgan L, Shumway S. Social communication profiles of children with autism spectrum disorders late in the second year of life. Journal of Autism and Developmental Disorders. 2007;37:960–975. doi: 10.1007/s10803-006-0237-4. [DOI] [PubMed] [Google Scholar]
- Wetherby A, Woods J. Systematic observation of red flags for autism spectrum disorders in young children, Unpublished manual. Florida State University; Tallahassee, FL: 2002. [Google Scholar]
- Wetherby A, Woods J, Allen L, Cleary J, Dickinson H, Lord C. Early indicators of autism spectrum disorders in the second year of life. Journal of Autism and Developmental Disorders. 2004;34(5):473–493. doi: 10.1007/s10803-004-2544-y. [DOI] [PubMed] [Google Scholar]
- Zwaigenbaum L, Bryson S, Rogers T, Roberts W, Brian J, Szatmari P. Behavioral manifestations of autism in the first year of life. International Journal of Developmental Neuroscience. 2005;23:143–152. doi: 10.1016/j.ijdevneu.2004.05.001. [DOI] [PubMed] [Google Scholar]