Abstract
Objective
To examine the effects of nurse, infant, and organizational factors on delivery of collaborative and evidence-based pain care by nurses.
Design
Cross sectional.
Setting
Two Level III neonatal intensive care units in 2 large tertiary care centers in Canada.
Participants
A convenience sample of 93 nurses completed survey data on procedures they performed on ill neonates. The 93 nurses performed a total of 170 pain producing procedures on 2 different shifts.
Main Outcome
Nurse use of evidence-based protocols to manage procedure related pain using a scorecard of nurses’ assessment, management, and documentation.
Results
Procedural pain care was more likely to meet evidence-based criteria when nurse participants rated nurse-physician collaboration higher (odds ratio, 1.44; 95% confidence intervals 1.05–1.98), cared for higher care intensity infants (odds ratio, 1.21; 95% confidence intervals, 1.06–1.39), and experienced unexpected increases in work assignments (odds ratio, 1.55; 95% confidence intervals, 1.04–2.30). Nurses’ knowledge about the protocols, educational preparation and experience were not significant predictors of evidence-based care for the most common procedures: heel lance and intravenous initiation.
Conclusion
Nurse-physician collaboration and nurses’ work assignments were more predictive of evidence-based care than infant and nurse factors. Nurses’ knowledge regarding evidence-based care was not a predictor of implementation of protocols. In the final statistical modeling, collaboration with physicians, a variable amenable to intervention and further study, emerged as a strong predictor. The results highlight the complex issue of translating knowledge to practice, however, specific findings related to pain assessment and collaboration provide some direction for future practice and research initiatives.
Keywords: evidenced-based, neonatal procedural pain, nurses, nurse-physician collaboration, knowledge transfer
Collaborative management of pain related to invasive procedures is a key responsibility for nurses caring for hospitalized neonates. However, studies conducted in various clinical settings have consistently demonstrated that nurses underestimated and undermedicated infants’ pain (Elander & Hellstrom, 1992; Foster & Hester, 1990; Johnston, Stremler, Stevens, & Horton, 1997). The stakes are high. Exposure to painful procedures has contributed to the resetting of the human neonate basal arousal systems disorganizing their subsequent stress response (Grunau, Weinberg, & Whitfield, 2004). This increases the potential for negative health outcomes. Hospital accreditation now includes scrutiny of the delivery of optimal pain care.
Health care organizations are now accredited based on evidence-based pain care (Canadian Council of Health Services Accreditation [CCHSA], 2005; Joint Commission on Accreditation of Health Organizations [JCAHO][34], 2001). There is some evidence that possessing knowledge may not be the only factor for providing sound pain care. In two studies, nurses demonstrated acceptable knowledge, but this did not translate to better pain care (Jacob & Puntillo, 1999; Reyes, 2003). Barriers to such care may include insufficient knowledge about evidence or individual or organizational factors that compromise the nurse’s ability to use that knowledge.
Background
Capillary blood sampling by heel lance is the most commonly performed invasive procedure and is reported to be more painful than venipuncture for infants (Larrsson, Tannfeldt, Lagercrantz, & Olsson, 2000; Shah, Taddio, Bennett, & Speidel, 2000). While there is ample evidence to support safe and effective pain care procedures, there are accumulating reports of their underuse in practice. Johnston et al. (1997) found that 45% of all neonatal invasive procedures performed were heel lance for which analgesic was only given 4.9% of the time. In two recent studies, the uptake of pain management strategies does not appear to have increased appreciably. Simons et al. (2003) reported preterm neonates undergo an average of 14 procedures per day with less than 35% given analgesia. Stevens et al. (2003) reported in some cases only 20% of high-risk infants having procedures received appropriate pain care.
Prior research has documented that neonates who experienced pain during the neonatal period displayed a dampened expression to repeated heel lance (Johnston & Stevens, 1996) and exhibited an altered stress response to subsequent painful and nonpainful stimuli (Grunau et al., 2004; Johnston & Stevens, 1996; Taddio, Katz, Ilesrich, & Koren, 1997). The short- and long-term health of these vulnerable neonates is likely negatively impacted by early unmanaged painful experiences. One report indicated they tend to express atypical neurobehavioral responses to pain later in their development (beyond the newborn stage) (Oberlander et al., 2005).
Short-term harmful effects of repeated painful events could include wide fluctuations in intracranial pressures resulting in intraventricular hemorrhage (Anand, Coskun, Thrivikraman, Nemeroff, & Plotsky, 1999; Anand & Scalzo, 2000). In the long term, this may increase the chance of disorders related to anxiety, altered pain sensitivity, stress, attention deficit, and developmental delay (Anand et al., 1999). These outcomes are of concern, particularly as there are several reports showing that analgesics are not used or used infrequently for most procedures (Fernandez & Rees, 1994; Johnston et al., 1997; Reyes, 2003; Simons et al., 2003; Stevens et al., 2003; Van Hulle Vincent, 2005).
Pain Assessment-Organizational and Individual Facilitators and Challenges
Routine pain assessment has been reported to lead to more consistent management of pain (Jacob & Puntillo, 1999; Reyes, 2003). National health care agencies such as the American Academy of Pediatrics (AAP) and Canadian Paediatric Society (CPS) (2006) and national accreditation agencies have established hospital-based standards that include assessment as necessary in pain care (Table 1). In the United States (Reyes, 2003) and in Europe (Gharavi, Schott, Nelle, Reiter, & Linderkemp, 2007), the increase in pain care in neonatal intensive care units (NICU) has been attributed to the implementation of these guidelines. The account-ability for adhering to national policies and accreditation guidelines rests with the organization as well as the individual clinician.
Table 1.
Policy and Accreditation Guidelines
| American Academy of Pediatrics (AAP) and Canadian Pain Society (CPS) (2006) |
| Every health care facility caring for neonates should implement an effective pain-prevention program, which includes strategies for routinely assessing pain, minimizing the number of painful procedures performed, and effectively using pharmacologic and non-pharmacologic therapies for the prevention of pain associated with routine minor procedures. |
| The Canadian Council for Health Services Accreditation (CCHSA) (2005) |
| Each patient receives an appropriate developmental assessment, management and documentation of the pain response to the procedure. |
| Joint Commission on Accreditation of Healthcare Organizations (JCAHO) (2001) |
| Every patient has a right to have his or her pain assessed and treated. |
Some pain experts have suggested that for neonates who are not capable of pain expression, the level of pain care may be mediated by caretakers’ ability to assess pain, especially in younger more acutely ill infants (Breau et al., 2004; Hamers, van den Hout, Halfens, & Kester, 1996). In essence, some caregivers may be more skilled at assessing pain expression in neonates who do not display the typical pain cues of crying, body movement, and facial expression. In two research studies where age was a factor, neonatal nurses performed more pain assessments for older neonates ( ≥ 33 weeks vs. younger) leading to higher pain care (Reyes, 2003). Poorer pain care was reported for older infants not able to display pain cues (Van Hulle Vincent, 2005). From this research it appears there may be a link between neonates’ ability to express pain and the caregiver’s ability to assess pain, especially in groups that do not display typical cues. The nurse’s ability to assess pain irrespective of the child’s age or pain cues requires further exploration.
Pain Management
The best evidence to inform nurses’ pain management decision making includes studies reviewed for the Cochrane Collaboration. These studies supported the efficacy and safety of oral sucrose for reducing pain from single heel lance and venipuncture in neonates (Stevens, Yamada, & Ohlsson, 2004). This study’s definition of optimal management of tissue damaging procedural pain specifically includes specifically the use of sucrose and pacifier (Fetus and Newborn Committee of Canadian Pediatric Society, 2007). Oral sucrose given two minutes before painful procedures has been shown to decrease infant cry duration, heart rate, facial action, and composite assessments of pain in term and preterm infants (Johnston, Stremler, Horton, & Friedman, 1999; Stevens et al., 2007). In addition, the combination of sucrose and simultaneous swaddling/bundling has been reported as the most effective intervention for infants receiving heel lance (Gibbins et al., 2002; Johnston et al., 1997). These strategies are within the nurse’s scope of practice, yet there may be other factors that influence the use of this evidence.
Effective communication and inter-professional collaboration has not been rigorously examined in the pediatric setting, but numerous research studies have demonstrated that collaborative relationships influence health outcomes in adults. In adult clinical populations, after adjusting for patient comorbidities and age, the presence of better nurse-physician relationships predicted lower 30-day mortality rates (Estabrooks, Midodzi, Cummings, Ricker, Giovannetti, 2005), fewer readmissions to ICU (Baggs, Ryan, Phelps, Richeson, & Johnson, 1992; Miller, 2001) and higher self-report of better pain care (Wild & Mitchell 2000; Willson, 2000). Neonates are unable to self-report, and some have dampened pain display cues, which compromises their ability to communicate pain. As a result, procedures are still performed without pain care. Poor pain care is not the result of lack of evidence; more likely professional and organizational factors limit the use of evidence in practice.
Theoretical Framework
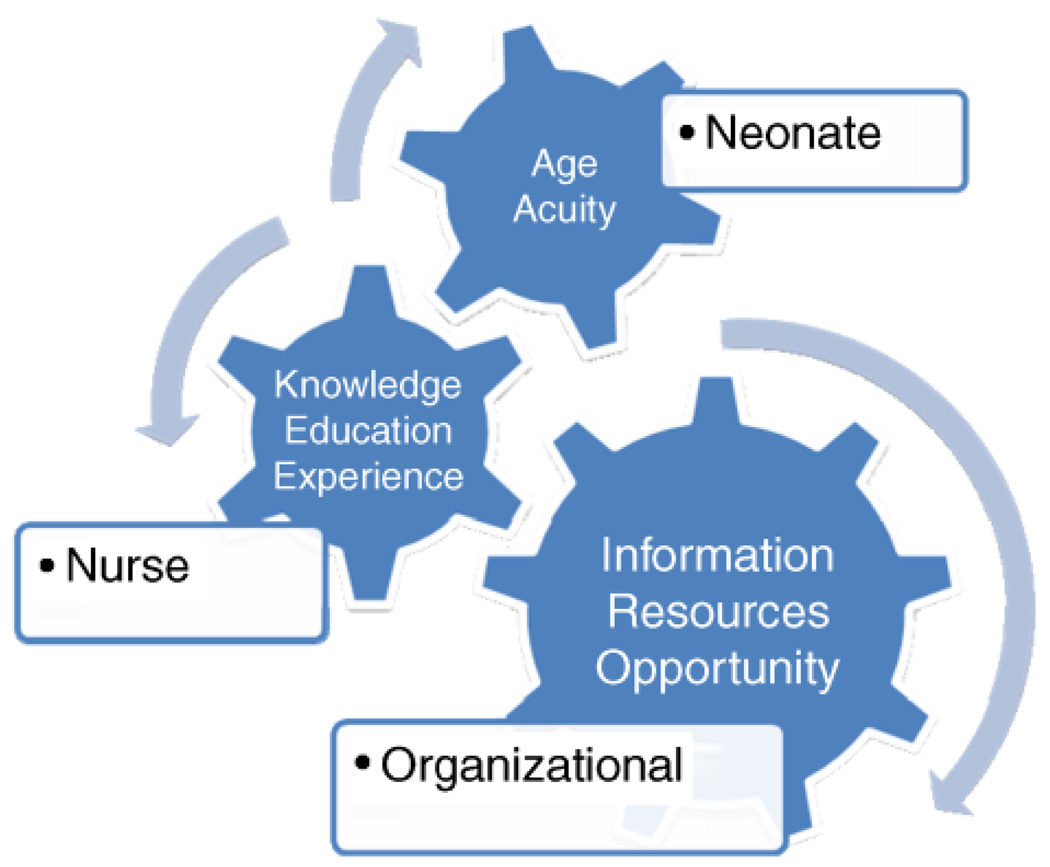
This study was guided by a conceptual framework articulating the interplay between positive work-life components and knowledge translation factors within the context of certain nurse, organizational and infant factors. Before this research no specific framework existed that grouped these concepts together. A diagram is provided to illustrate the conceptual links under study (Figure 1).
Figure 1.
Neonate, nurse and organizational factors influencing knowledge use for optimal pain care.
Specific nurse characteristics such as years of experience and formal nursing education have been associated with better pain care (O’Brien-Pallas et al., 2004). The three organizational variables of interest in the study were drawn from the Theory of Organizational Behavior (Kanter, 1977, 1993): opportunity, information and resources. Opportunity is defined as the existence of available chances to increase knowledge and skills for practice. Opportunities include access to in-services, courses, and conferences to enhance practice knowledge in the area of pain care. Kanter’s work refers to available expertise required to function effectively at work including knowing who to go to for necessary information. Information sources include collaboration and effective communication exchange with physicians. Resources comprise the materials, supplies, equipment and time necessary to do the work. Resources include enough staff with the ability to meet patient care demands. Variations in infant factors, such as age and acuity, have been reported to influence nurses’ pain assessment and management practices (Gadish, Gonzalez, & Hayes, 1988; Reyes, 2003). It was anticipated that higher levels of nurse variables (education and years of experience) may alone increase pain care. Significant increase was anticipated in the presence of a stronger organizational context such as learning opportunities, information exchange with physicians, and resources. Neonate age and acuity had not been extensively studied previously, therefore, the authors explored these variables further while considering all variables together.
The purpose of this cross-sectional descriptive study was to examine the extent to which nurse, organizational, and infant factors predict the likelihood of evidence-based pain care. The primary research question explored the extent to which nurse, organizational, and infant factors predict nurses’ procedural pain care. Nurse factors include pain knowledge, education, and experience; organizational factors include opportunity, information and resources; and infant factors include age and acuity. Seven of these eight were included in the final analysis. Following approval from both institutional ethics boards, the study details were introduced to nurses, neonatologists, and other health care professionals at staff meetings and via memos to electronic work mailboxes.
Methods
Setting and Sample
A convenience sample of 93 registered nurses who performed 170 tissue-damaging procedures participated. The sample of nurses was drawn from two NICUs from two large teaching hospitals in central and eastern Canada. The nursing complement was 77 for Site 1 and 170 for Site 2. Both units were Level III in intensity of care provided to both inborn and outborn neonates. Site 1 had 28 beds and Site 2 had 55. Neonates at both sites were cared for by a complement of nurses, residents, neonatologists, and visiting fellows. In addition, Site 2 had 3 neonatal nurse practitioners practicing in the unit and performing advanced procedures such as central line insertion. Total patient care was the model of care on both units.
Nurses were recruited based on infants in their care having a painful procedure on randomly selected data collection days. Sample estimate guidelines for multiple regression were used to determine a robust sample to reduce Type 1 error (Green, 1991). With a power set at .80 and an α of .05, a sample of 160 procedures was estimated as robust enough to detect the highest level of pain care using eight predictor variables. This sample of nurses performed a total of 170 procedures on two different shifts and the delivery of pain care for each of the procedures was the unit of analysis.
Eligibility criteria required that all nurses: (a) understand and read English, (b) work at least half-time on the unit for 6 months, and (c) be caring for an eligible infant. Infants were eligible at any time during their admission to have chart data collected for the study if (a) they were ≥ 28 weeks gestation and (b) had experienced a tissue damaging procedure performed by or with the assistance of a nurse during the data collection shift. The best evidence at the time of the study was sucrose in combination with pacifier and bundling, which were safe and effective to manage procedural pain in neonates 28 weeks and older. All younger infants were excluded. Procedures included heel lance, arterial and intravenous access (central and peripheral), lumbar puncture, oral/nasal/endotracheal suctioning, wound care, and chest tube insertion. Infants who were medically paralyzed were excluded.
Procedures
On data collection shifts, the nurse in charge identified eligible nurses who were caring for an infant meeting the study criteria. Nurses were approached on their work unit by the research assistant and the study details were explained. Once the nurses’ and infants’ eligibility was confirmed and nurses consented to participate, the infants’ parents were provided with information about the study. Parents were provided with an opportunity to request that their infants’ anonymous data not be included. This was acceptable to the Ethics Boards and there were no requests of this nature. Infant age, acuity, and procedural pain care data were collected from charts by the research assistant.
Nurses were provided with a survey package that included a study introduction letter, demographic profile and descriptive data, and the study instruments measuring nurses’ knowledge of pain care, satisfaction with information exchange with physicians, and resources to meet shift complexity. Nurses were recruited and completed surveys after the procedure to reduce bias or changes in their usual care. Nurse participants returned their completed survey packages to an envelope on the units marked “Procedural Pain Study.” Nurses were invited to participate twice, on day shifts 2 weeks apart. Collecting data from the same nurses on two different shifts was anticipated to capture fluctuations in organizational and infant factors while demonstrating that nurse knowledge remained consistent. The nurses’ first responses were linked to the second data set by a code. Data were collected over a 2 months time period at each hospital.
Measures
Nurse: Demographic and Descriptive Data
This included nurses’ work experience, education, in-service attendance, and knowledge of pain management specifically for heel lance and venipuncture.
Nurse: Knowledge
Because nurses’ knowledge of evidence-based pain care was a central component of the study and due to the unavailability of a psychometrically tested instrument in neonatal nurses, the lead investigator developed the Pain Knowledge and Use (PKU) instrument. The items were derived from three sources: existing pain knowledge scales, published literature, and pain experts. Content validity testing of the newly developed instrument was conducted with 15 nurses with greater than 10 years experience working in a hospital setting with ill neonates. Content experts are individuals with the necessary training, experience, and qualifications to judge a measure (Grant & Davis, 1997). Generally 10 or less experts are recommended (Lynn, 1986). More nurses (n = 15) were used to establish the validity of the PKU instrument because it was newly developed and the authors wanted a stringent validity pretesting process. Using Lynn’s (1986) content validity index (CVI) guidelines the, CVI was acceptable at 88%.
This PKU measured nurses’ knowledge of pain assessment (11 items), management (10 items), and documentation practices (4 items) on a 6-point scale. A higher score was indicative of higher knowledge and use. In this sample of nurses, reliability testing was acceptable with a Cronbach’s α coefficient for all 25 items of .84 and test-retest reliability .68 (p < .01).
Organizational-Information Exchange
The Collaboration and Satisfaction about Care Decisions instrument (CSACD) (Baggs, 1994) was originally pilot tested with NICU staff. The nine item survey was scored on a 7-point scale and had acceptable validity (Baggs, 1994) and reliability (Weiss & Davis, 1985). The α coefficients for the current study were .97 (collaboration scale), .91 (satisfaction scale) and the global collaboration (r =.85).
Organizational Resources
The Daily Environmental Complexity Scale (ECS) (O’Brien-Pallas, Irvine, Peereboom, & Murray, 1997) measures nurses’ ratings of how daily unit factors influence their ability to provide required patient care. The 22 items of the ECS top three domains: (1) change in work acuity based on unanticipated increases or decreases in workload, (2) subsequent re-sequencing and coordination of nurses’ work, and (3) the composition of the care team (short staffed, students). Subscales range from 0 to 10 and a higher score implies a more complex shift. O’Brien et al. (1997) reported subscale a reliabilities were .88, .87, and .77. In the current study the coefficients were lower: Change in work acuity (.72), Resequencing of work subscale (.67), and Team Composition subscale (.42). The Team subscale was excluded from the analysis due to low reliability.
Infant Care Acuity
The Neonatal Therapeutic Intervention Score (NTIS) (Gray, Richardson, McCormick, Workman-Daniel, & Goldmann, 1992) measures acuity of illness by examining the frequency and intensity of therapeutic interventions. Eight clinical subscores were used to compute a total score (e.g., respiratory, cardiovascular) and scores ranged from 0 to 47. A higher NTIS implies higher illness severity requiring more care. Validity and internal consistency has been established (Gray et al., 1992).
Outcome Measure: Evidence-Based Pain Care
The Pain Care Data Form developed for this study consists of the recommended standards of pain care for infant procedures (Fetus and Newborn Committee of Canadian Pediatric Society, 2000). Pain care was assessed through chart review and nurses’ report of actual care delivery. Nurses described any pharmacological or nonpharmacological interventions for the procedure. The scores were based on the presence or absence of three evidence-based categories: assessment and documentation (2 points), medication order and administration (2 points), and nonpharmacological interventions such as swaddling and pacifier (1 point). Assessment and documentation were scored with 2 points given their primary importance in communication of the pain. The presence and use of a medication order, equally important, also was scored with 2 points.
The nonpharmacological strategies were scored with 1 point. In pilot testing, nurses’ pain care was not normally distributed across the 5 points so scores were collapsed into three categories: No Pain Care (no evidence of assessment, management, documentation, score = 0), Low Pain Care (Evidence of Nonpharmacological Management, Score = 1) and Evidence-Based Pain Care (medication administration, Score = 2; assessment + medication, score = 3; assessment + medication + documentation, score = 4). Face and content validity were established again using Lynn’s (1986) recommendations with five expert nurses. The number of content experts is generally 10 or less. When five or fewer experts are used, all five must agree on the content validity rating for the instrument to be judged as valid (Lynn, 1986). This occurred with the five experts. In addition, inter-rater reliability was achieved with an agreement rate of 89% with 40% of a randomly selected subset of Pain Care Forms.
Analysis
All data were entered into an SPSS data file for descriptive analyses and multinomial logistic regression analyses predicting the main outcome (No Pain Care, Low Pain Care, and Evidence-Based Pain Care). The SPSS data were converted into a SAS data file for the general estimating equation (GEE) analysis. GEE is a variant of regression accounting for the correlation of repeated measures within the participants over the two collection periods.
The outcome analysis proceeded in three steps: (1) The unique prediction of pain care was estimated from the three theoretical domains separately (nurse, organizational, and neonate factors); (2) the unique prediction of pain care from all predictors in all three domains was estimated simultaneously to see which predictors would survive; and (3) a final, parsimonious predictive model was built including just the strongest and most theoretically important predictors from the first two steps. The significant predictors did not change across these different models.
Findings
Nurse, Neonate, and Organizational Factors
Across sites nurses had similar education levels (40% Diploma, 60% Baccalaureate) and nearly 50% had more than 10 years of experience. Nurses scored moderately high on the knowledge of pain care instrument (M = 4.57, SD = 0.52) and many nurses accurately identified evidence-based pain care for venipuncture (62%) and heel lance (45%). Yet only a small number actually provided this level of care to study infants for specific procedures (venipuncture, 8%; heel lance, 4%). Major sources of knowledge about pain care included other nurses and/or physicians (38%), journals and the Internet (33%). The nurse characteristics by site were similar however the infant factors were different (Table 2).
Table 2.
Nurse and Neonate Demographic Data Compared between NICU 1 and NICU 2
| Nurse variable | Site 1, n = 31 (f%) | Site 2, n = 62 (f%) | Total, N = 93 |
|---|---|---|---|
| Nurse education | |||
| Diploma | 15 (48) | 32 (54) | 47 (51) |
| Baccalaureate | 16 (51) | 29 (45) | 45 (48) |
| Master Nursing | 0 | 1 (1) | 1 (1) |
| Years experience as neonatal nurse | |||
| 6–12 months | 5 (17) | 1 (1)* | 6 (6) |
| 1–2 years | 4 (13) | 7 (11) | 11 (12) |
| 2–10 years | 6 (19) | 25 (40)* | 31 (33) |
| >10 years | 15 (48) | 29 (48) | 44 (47) |
| Missing | 1 (3) | 0 | 1 (2) |
| Nurse access to pain in-service in the past year | |||
| None | 18 (58) | 42 (68) | 60 (65) |
| 1 | 10 (32) | 17 (27) | 27 (29) |
| 2+ | 3 (10) | 3 (3) | 5 (5) |
| Neonate variable | NICU 1, n = 63 (f%) | NICU 2, n =107 (f%) | Total, N = 170 |
| Neonate age (weeks) | |||
| 28 | 11 (17) | 6 (5)* | 17 (10) |
| 29–32 | 27 (43) | 25 (23)* | 52 (31) |
| 33–36 | 19 (30) | 32 (30) | 51 (30) |
| 37+ | 4 (6) | 44 (41)* | 48 (29) |
| Neonatal intensity score (NTIS) | |||
| Low intensity ( ≤ 3) | 3 (5) | 8 (7) | 11 (6) |
| Moderate intensity (4–7) | 19 (30) | 51 (48) | 70 (41) |
| High intensity (>8) | 40 (63) | 47 (44)* | 87 (53) |
Note.
p < .01.
One site had a higher proportion of younger neonates (28–32 weeks gestation, χ2 = 29.7, p < 05 requiring higher care intensity (higher NTIS scores, χ2 = 6.38, p <.05). The majority of study infants were low birth weight (65% were ≤ 2,000 g, mean weight = 1,880 g). These neonates had an average age of 34 weeks with a mean intensity score of eight (NTIS, Gray et al., 1992). The highest proportions of procedures for both sites were venipuncture (51%) and heel lance (31%). Remaining procedures included central line initiation (9%), immunization and wound care (5%).
For site-based organizational factors, nurses’ perceptions of collaboration were significantly different using independent sample t-test (Site 1: M = 4.15, SD = 1.69; Site 2: M = 4.71; SD = 1.34, p < .05). Two of the shift complexity subscales had similar statistical differences (p < .05) between units (Resequencing of Events and Unanticipated Changes in Acuity). Nurses’ scores from both sites indicated moderately high collaboration with physicians (more at Site 2) and moderately complex environments (higher for Site 2). The organizational factor opportunity, measured by frequency of nurses attendance at an education session with pain care content (Table 2), was not significant by level of pain care delivered (χ2 = 11.07, p = .27); only 34%(n = 32) of the nurses reported session attendance in the previous year.
Preliminary Analysis
To ensure the appropriateness of pooling data across the sites, the results at each site were compared using t- and chi-square tests. There were between site differences on collaboration and complexity of care. However, because there was no statistically different effect for any of the predictors by site using interaction terms (e.g., Site × Collaboration), nurses’ scores from the two sites were pooled. With two exceptions, all correlations between the predictor variables were below the .40 level, suggesting that multicollinearity was not an issue. Two pairs of predictor variables, infant age and acuity (r = −.50, p < .05) and two of the Complexity subscales (Resequencing Work, Unanticipated Changes) were significantly correlated (r = .65, p < .05). To eliminate redundancy neonate acuity was selected as the more accurate representation of care demands and the age predictor was excluded. The Complexity instrument Resequencing subscale was excluded as the reliability coefficients were stronger in the Unanticipated Changes subscale. Nurses’ knowledge and collaboration with physicians were correlated at a level of .27.
Outcome Variable: Evidence-Based Pain Care
Total Pain Care Scores were categorized into three ordinal levels: (1) No Pain Care, (2) Low Pain Care, and (3) Evidence-Based Pain Care. The majority of infants received Low (55%) or No Pain Care (17%), while 28% received Evidence-Based Pain Care. Pain assessments were infrequently performed (8%) for study procedures, and the most common management included nonpharmacological strategies consisting of pacifieralone (15%) or swaddling alone (19%) but more commonly together (36%). Nurses provided pharmacological management for 20% of the procedures, and 10% (n = 17) of infants received sucrose alone or in combination with other strategies.
The descriptive predictor variable results by the three levels of pain care (No Pain, Low Pain, and High Pain Care) can be found in Table 3. Nurses with scores in the High Pain Care level also had the highest mean scores for pain knowledge (M = 4.63, range = 3–5.6), perception of nurse-physician collaboration (M = 5.03, range = 1–7) and all work complexity scales, which was higher in comparison with the nurses who provided Low or No Pain Care.
Table 3.
Descriptive Predictor Variables by Level of Pain Care (N = 170)
| No pain care | Range | Low | Range | Mod-High | Range | |
|---|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | ||||
| Pain knowledge (6 pt) | 4.65 (0.42) | 3.8–5.4 | 4.52(0.54) | 2.7–5.6 | 4.63 (0.53) | 3.0–5.6 |
| Nurse/doctor collaboration (7 pt) | 4.23 (1.39) | 1.3–6.6 | 4.31 (1.42) | 1.0–7.0 | 5.03 (1.63) | 1.0–7.0 |
| Environment complexity (10 pt) | ||||||
| Resequencing of work | 5.23 (.36) | 5.0–6.2 | 5.33 (.51) | 5.0–7.3 | 5.54 (.65) | 5.2–7.1 |
| Change in pt acuity | 5.62 (.67) | 5.0–6.8 | 5.68 (.72) | 5.0–7.8 | 6.09 (1.02) | 5.0–9.6 |
| Team composition | 5.10 (.69) | 3.5–8.0 | 5.06 (.39) | 5.0–8.0 | 5.22 (.94) | 5.0–10 |
Note. Bold numbers denote highest scores.
In both the individual model and the comprehensive model (all predictors together Table 4), infant and organizational factors were more likely to predict evidence-based pain care than the nurse factors. Infant acuity, the unanticipated changes in nurses’ work assignment and nurse-physician collaboration predicted higher pain care. In the regression analysis, nurses’ level of pain knowledge, education level, or access to education had no effect. The variable, nurses’ knowledge level was retained in the final equation based on theoretical importance despite the lack of statistical evidence in the first models. Evidence to support this decision was based on the results of a systematic review by Thompson, Estabrooks, and Degner (2006) indicating the primary source of knowledge utilization is the availability of knowledge. This means if you have access to or possess the knowledge, you are more likely to use it. Therefore, this variable was retained in the model. Consistent with the results in the first two steps of analysis, three predictors contributed significantly to the levels of evidence-based pain care and were retained in the final model along with nurses’ knowledge. These included neonate acuity (95% confidence interval [CI ] 0.008, 0.083], unanticipated changes in nurses’ assignment (95% CI 0.0613, 0.012) and collaboration (95% CI 0.003, 0.140). The presence of higher neonate care acuity, higher nurse-physician collaboration and more unanticipated changes in nurses’ assignment acuity significantly increased the likelihood of pain care.
Table 4.
Predictors of Evidence-Based Pain Care Nurse, Organizational Neonate Factors (Multinomial Logit N = 170)
| Estimate | SE | 95% CI | Z | P > Z | |
|---|---|---|---|---|---|
| Nurse | |||||
| Education | −.0213 | .1106 | −.238, .195 | −0.19 | .84 |
| In-Services | .1241 | .0702 | −.013, .261 | 1.77 | .07 |
| Knowledge | .0400 | .0894 | −.135, .215 | 0.45 | .65 |
| Experience | .0158 | .0385 | −.059, .091 | 0.41 | .68 |
| Organizational | |||||
| Collaboration | .0720 | .0352 | .003, .140 | 2.05 | .04* |
| Resequence events | .0905 | .1058 | −.116, .297 | 0.86 | .39 |
| Team composition | .0567 | .0773 | −.094, .208 | 0.73 | .46 |
| Unanticipated | .1322 | .0613 | .012, .252 | 2.16 | .03* |
| Change in nurse assignment | |||||
| Neonate | |||||
| Neonate acuity | .0461 | .0190 | .008, .083 | 2.42 | .01* |
| Neonate age | .0029 | .0127 | −.022, .027 | 0.23 | .81 |
Note.
p < .05.
These results did not change when the outcome measure was dichotomized into No/Low Pain Care or the highest level of Evidence-Based Pain Care. The odds ratios analysis (Table 5) showed increased probability for optimal pain care, as measured as a two-level variable. This results when nurses care for more acutely ill infants (OR: 1.21; CI: 1.06–1.39), have higher perceived doctor collaboration (OR: 1.44; CI: 1.05–1.98) and unanticipated increases in assignment acuity (OR: 1.55, CI: 1.04–2.30). For example, for each 1-unit increase in collaboration (OR: 1.44), it was 44% more likely that Evidence-Based Pain Care was given. Similarly, for infant acuity, (OR: 1.21) for each 1 unit increase in acuity, it was 21% more likely that high level pain care was given. Those infants with the highest possible level of intensity (score of 17) were 3.57 times more likely to (or three times more likely to) get Evidence-Based Pain Care, compared with those with the lowest possible level of acuity (one).
Table 5.
Logistic Regression Results for No/Low Pain Care Versus Higher Pain Care Delivery (N = 170)
| Variable | OR | 95% CI | p |
|---|---|---|---|
| Nurse-doctor collaboration | 1.44 | 1.05,1.98 | .02* |
| Neonate acuity | 1.21 | 1.06,1.39 | .00* |
| Pain knowledge | 1.07 | 0.50, 2.28 | .86 |
| Change in acuity | 1.55 | 1.04, 2.30 | .00* |
Note. CI = confidence interval; OR = odds ratio.
p<.05.
Discussion
Findings suggested that nurses’ knowledge regarding evidence-based practices was not reflected in the pain care they actually provided. Nurses’ knowledge scores were fairly high and consistent with findings from other research on nurses in pediatric settings (Manworren, 2001; McCaffery & Ferrell, 1997; Reyes, 2003; Van hulle Vincent, 2005). Consistent with other research, nurses accurately identified typical pain display indicators (cry, behavior), but they provided low management in practice (Reyes, 2003; Van hulle Vincent, 2005). There may be other factors, such as recognition of pain or culture of pain management, that have not yet been considered within the context of pain care. Low management may be due to nurses’ lack of ability to recognize ill infants’ subtle expressions of pain (de Rond, de Wit, van Dam, 2001; Reyes, 2003). Researchers have shown that nurses are less adept at recognizing pain expressions in newborns compared with nonhealth professionals (Xavier Balda et al., 2000). This is of considerable concern since children are more likely to have their pain treated in the presence of behavioral indicators (Hamers, Abu-Saad, Halfens, & Schumacher, 1994; Van Hulle Vincent, 2005). Earlier born infants (<32 weeks) have been shown to have less behavioral manifestations during heel lance than older infants (Johnston & Stevens, 1996). Infants in the current study were young (40% ≤ 29 weeks; 30% between 32–36 weeks) and nurses may not have accurately assessed their pain.
The current findings regarding nurses delivering Evidence-Based care to higher intensity infants are different from other research that indicated that sicker (Arts et al., 1994; Hamers et al., 1996) younger children and infants (Johnston et al., 1997; Reyes, 2003) are less likely to receive pain care. For infants not capable of pain expression, pain care may be mediated by nurses’ beliefs. In the absence of pain expression, higher acuity infants may be “assumed” to be in pain and expert nurses may give better care.
Nurses with more work experience or education were no more likely to provide higher pain care. The authors propose that expertise and experience are not the same concept. The Merriam-Webster’s Online Dictionary (2008) defines “expert” as involving or displaying special skill or knowledge as a result of training or experience. Even this definition implies experience alone may define expertise. In this study expertise was not originally defined, only knowledge and adherence to guidelines was examined. Further work explicitly examining this concept of expertise and the influence is required.
In addition, the findings also contrast with other reports that cite nurses’ formal education (Diploma, Baccalaureate) and years of experience predict lower patient mortality rates in infants (Estabrooks, Midodzi et al., 2005; Tourangeau, Cranley, & Jeffs, 2006; Tucker & UK Neonatal Staffing Study Group, 2002) and better pain care (Dougherty & Larson, 2005; Hamers et al., 1996; O’Brien-Pallas et al., 2004; Tibby, Correa-West, Durward, Ferguson, & Murdoch, 2004). Other research contradicts these findings and indicates that more experience has not meant that nurses and physicians used their knowledge about pain to provide better care (Breau et al., 2004; Lebovits et al., 1997) or used research findings in their practice (Profetto-McGrath, Hesketh, Lang, & Estabrooks, 2003). While nurses have cited nursing schools as the fifth source contributing to their level of pain knowledge (Estabrooks, Scott-Findlay, Rutakumwa, Duan, & Rozanova, 2004) more education did not influence better pain care. These discrepant findings may be due to samples, cultures, or measurement differences. Furthermore, opportunities to learn evidence-based pain care at work may be more relevant.
Some have attributed the lack of pain management in children to low access to educational opportunities for physicians and nurses (Karling, Renstrom, & Ljungman, 2002). Attendance at sessions specific to care population can increase pain knowledge and potentially improve pain care (Dahlman, Dykes, & Elander, 1999; de Rond et al., 2001; Estabrooks, Chong, Brigidear, & Profetto-McGrath, 2005; Johnston et al., 2007). This study variable could not be properly examined because few nurses attended an education session on pain. The finding that nurses’ major source of knowledge about pain care was acquired from physicians and nurses has not been reported previously. This may explain why knowledge levels were adequate in the presence of stronger collaboration despite low attendance at educational sessions.
These study findings are consistent with previous research regarding the influence of higher nurse-physician collaboration predicting better care (Baggs et al., 1992; O’Brien-Pallas et al., 2004; Tourangeau et al., 2006) and better use of research (Hansen, Biros, Delaney, & Schug, 1999). In this study, the small, but significant correlation between nurses’ knowledge and collaboration with physicians suggests that the quality of clinician information exchange may facilitate evidence-based pain care. Nurses with low knowledge would not be likely to engage in discussions with physicians. De Rond et al. (2001) found that most physicians (69%) believed they had sufficient knowledge to relieve pain, but only 25% thought that the nurses with whom they worked had the same capabilities.
Researchers are examining the link between inter-professional collaboration and knowledge utilization (Hansen et al., 1999; Thompson et al., 2006). Thompson et al.’s review identified the primary theme in knowledge transfer was the increase in availability of knowledge. However, increasing interpersonal contact, where information was exchanged, enhanced the likelihood of behavioral change. Consistent with Thompson’s work, the findings in the current study indicated collaboration predicts evidence-based pain care.
The findings indicated that both increases in infant acuity and nurses’ work assignment significantly predicted evidence-based pain care. While it was reassuring to learn that infants with higher care intensity receive better pain care, questions remain as to why. Nurses with more expertise are typically assigned to medically unstable infants with a higher probability of unanticipated increases in their acuity. Hamers et al. (1996) reported that nurse’s expertise did not influence assessment, yet more expert nurses were more confident in their pain care decisions and more inclined to administer analgesics to children. Nurse’s expertise, while not examined here, may explain why infants cared for by nurses with increasing assignment work received higher care. While there may have been variability in the nurse’s level of expertise, none of the nurses were at the lowest level of knowledge and ability. Busier nurses did not use research less. This is consistent with the Estabrooks et al. (2004) report indicating no significant relationships between high workload and low research use.
Implications for Practice
Nurses’ knowledge levels did not directly predict higher pain care; however, low knowledge may have resulted in higher frequencies of substandard pain care. While nurses scored moderately high on their knowledge of optimal pain care for procedures, there were gaps in what they said they knew to be pain expression and the frequency they treated pain. This evidence may provide some answers as to how nurses assess pain cues in ill neonates. Nurses may not recognize the more complex pain display indicators in a large proportion of the infants in their care. Implications for neonatal nurses in practice would include specific training and demonstrated understanding on neonate pain display cues.
Nurses identified learning from their colleagues as a major source of knowledge. This finding provides direction for practice and educational training changes. Increasing chances for all disciplines to learn about pain care, together, and then providing the opportunities to exchange that knowledge may improve evidence-based pain care. Discrepancies in accurate knowledge of assessment, treatment and perceptions of intensity caused by procedures may explain why physicians may not consider nurse input in care; resulting in low information exchange.
The finding that more acutely ill neonates were more likely to receive better pain care indicates links may occur between severity of diagnosis and level of pain care. Or it may be an indication that nurses who provide care for more acutely ill neonates are better able to use their knowledge in practice.
Strengths and Limitations
In this study the use of nonprobability sampling was a limitation even though all nurses had an equal chance to participate and were randomly recruited based on infants in their care. Selection bias appeared not to be a factor because 99% of the nurses who were eligible for the study consented to participate and of those, 90% did participate. A potential limitation is that the pain knowledge instrument may not have discriminated levels of knowledge and this could explain the findings regarding knowledge-practice gap. While the instrument has good theoretical and psychometric properties, further testing is required. The strengths of the design expedited data collection and provided an opportunity to examine diversity in work conditions. While the objective of this study was to examine the factors that may increase the likelihood of evidence-based pain care delivery one study limitation is that the neonate’s actual pain expression was not measured. Future research linking nurses’ actual assessment of neonates’ pain expression in the context of organizational factors will further contribute to understanding of this issue.
Conclusion
In summary, in this study of 170 neonate procedures across two NICUs, organizational and infant variables were more likely to predict nurse delivery of evidence-based pain care. No nurse factors significantly predicted evidence-based pain care, and nurses’ knowledge level as an individual predictor did not show significant impact. However, it is not reasonable to conclude that knowledge does not influence better care. Nurses with moderate levels of knowledge provided some pain care and nurses with moderate knowledge and collaborative nurse-physician relationships provided higher pain care. The discrepancies between nurses’ knowledge and pain care practices were perplexing. However, some nurses, despite increasing workload of their assignment, still provided higher levels of pain care. Enhancing pain care may result from creating workplaces where nurses have specific opportunities such as learning pain assessment and management tailored to the population in their care and where the routine is to exchange this information with other professionals. The results indicate exploration of the modifiable factors that influence practice in terms of pain care is required.
Acknowledgments
Funded by Canadian Health Services Research Foundation/Canadian Institutes of Health Research, Formation et expertise en recherche en administration des services infirmiers (FERASI) Center; Canadian Institutes of Health Research, Pain in Child Health Program; Nova Scotia Health Research Foundation; Canadian Nurses Foundation; Nursing Research Fund, Dalhousie University; and Izaak Walton Killam Health Centre. The authors thank Marlene Furlong, RN.
Contributor Information
Margot A. Latimer, Dalhousie University and IWK Health Centre, Halifax, Nova Scotia, Canada..
Celeste C. Johnston, McGill University, Montreal, Quebec, Canada..
Judith A. Ritchie, McGill University Health Centre, Montreal, Quebec, Canada..
Sean P. Clarke, University of Toronto, Toronto, Ontario, Canada..
Debra Gilin, Department of Psychology, St Mary’s University, Halifax, Nova Scotia, Canada..
REFERENCES
- American Academy of Pediatrics Committee and Canadian Paediatric Society. Prevention and management of pain in the neonate: An update. 2006 Retrieved May 15, 2008, from http://aappolicy.aappublications.org/cgi/content/abstract/pediatrics;118/5/2231.
- Anand KJS, Coskun V, Thrivikraman KV, Nemeroff CB, Plotsky PM. Long term behavioral effects of repetitive pain in neonatal rat pups. Physiological Behavior. 1999;66:627–637. doi: 10.1016/s0031-9384(98)00338-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anand KJS, Scalzo FM. Can adverse neonatal experiences alter brain development and subsequent behavior? Biological Neonate. 2000;77:69–82. doi: 10.1159/000014197. [DOI] [PubMed] [Google Scholar]
- Arts SE, Abu-Saad HH, Champion GD, Crawford MR, Fischer RJ, Juniper KH, et al. Age-related response to lidocaine-prilocaine (EMLA) emulsion and effect of music distraction on the pain of intravenous cannulation. Pediatrics. 1994;93(5):797–801. [PubMed] [Google Scholar]
- Baggs JG. Development of an instrument to measure collaboration and Satisfaction about care decisions. Journal of Advanced Nursing. 1994;20:176–182. doi: 10.1046/j.1365-2648.1994.20010176.x. [DOI] [PubMed] [Google Scholar]
- Baggs JG, Ryan SA, Phelps CE, Richeson JF, Johnson JE. The association between interdisciplinary collaboration and patient outcomes in a medical intensive care unit. Heart Lung. 1992;21(1):18–24. [PubMed] [Google Scholar]
- Breau LM, McGrath P, Stevens B, Beyene J, Camfield C, Finley A, et al. Healthcare professionals’ perceptions of pain in infants at risk for neurological impairment. BioMed Central Pediatrics. 2004;4(23) doi: 10.1186/1471-2431-4-23. Retrieved February 4, 2009, from http://www.biomedcentral.com/1471-2431/4/23/ [DOI] [PMC free article] [PubMed]
- Canadian Council of Health Services Accreditation. Inclusion of pain management in the AIM standards. 2005 Retrieved May 15, 2008, from http://www.canadianpainsociety.ca/Standards-Statement-CCHSA.pdf.
- Dahlman GB, Dykes AK, Elander G. Patients’ evaluation of pain and nurses’ management of analgesics after surgery. Journal of Advance Nursing. 1999;30(4):866–874. doi: 10.1046/j.1365-2648.1999.01153.x. [DOI] [PubMed] [Google Scholar]
- de Rond ME, deWit R, van Dam FS. The implementation of a pain monitoring programme for nurses in daily clinical practice: Results of a follow-up study in five hospitals. Journal of Advanced Nursing. 2001;35:590–598. doi: 10.1046/j.1365-2648.2001.01875.x. [DOI] [PubMed] [Google Scholar]
- Dougherty MB, Larson E. A review of instruments measuring nurse-physician collaboration. Journal of Nursing Administration. 2005;35:244–253. doi: 10.1097/00005110-200505000-00008. [DOI] [PubMed] [Google Scholar]
- Elander G, Hellstrom G. Analgesic administration in children and adults following heart surgery. Scandinavian Journal of Caring in Science. 1992;6:17–21. doi: 10.1111/j.1471-6712.1992.tb00117.x. [DOI] [PubMed] [Google Scholar]
- Estabrooks CA, Chong H, Brigidear K, Profetto-McGrath J. Profiling Canadian nurses’ preferred knowledge sources for clinical practice. Canadian Journal of Nursing Research. 2005a;7:118–140. [PubMed] [Google Scholar]
- Estabrooks CA, Midodzi W, Cummings G, Ricker K, Giovannetti P. The impact of hospital nursing characteristics on 30-day mortality. Nursing Research. 2005b;54(2):74–84. doi: 10.1097/00006199-200503000-00002. [DOI] [PubMed] [Google Scholar]
- Estabrooks CA, Scott-Findlay S, Rutakumwa W, Duan Q, Rozanova J. The determinants of research utilization in acute care: Pain management in adult and pediatric settings (No.04-01-TR) Edmonton, AB: Faculty of Nursing, University of Alberta; 2004. [Google Scholar]
- Fernandez CV, Rees EP. Pain management in Canadian level 3 neonatal intensive care units. Canadian Medical Association Journal. 1994;150:499–504. [PMC free article] [PubMed] [Google Scholar]
- Fetus and Newborn Committee, Canadian Paediatric Society. Prevention and management of pain in the neonate: An update. A joint statement with the American Academy of Pediatrics and the Fetus and Newborn Committee, Canadian Paediatric Society. Paediatrics & Child Health. 2007;12(2):137–138. Reaffrmed May, 2007. Retrieved February 3, 2009 from http://www.cps.ca/english/statements/fn/fn07-01.htm.
- Foster RL, Hester NO. The relationship between pain ratings and pharmacological interventions for children in pain. Advances in Pain Research and Therapy. 1990;15:31–37. [Google Scholar]
- Gadish HS, Gonzalez JL, Hayes JS. Factors affecting nurses’ decisions to administer pediatric pain medication postoperatively. Journal of Pediatric Nursing. 1988;3:383–390. [PubMed] [Google Scholar]
- Gharavi B, Schott C, Nelle M, Reiter G, Linderkemp O. Pain management and the effect of guidelines in neonatal units in Austria, Germany and Switzerland. Pediatric International. 2007;49:652–658. doi: 10.1111/j.1442-200X.2007.02453.x. [DOI] [PubMed] [Google Scholar]
- Gibbins S, Stevens BJ, Hodnett E, Pinelli J, Ohlsson A, Darlington G. Effcacy and safety of sucrose for procedural pain relief in preterm and term neonates. Nursing Research. 2002;51:375–382. doi: 10.1097/00006199-200211000-00005. [DOI] [PubMed] [Google Scholar]
- Grant JS, Davis LL. Focus on quantitative methods: Selection and use of content experts for instrument development. Research in Nursing and Health. 1997;20:269–274. doi: 10.1002/(sici)1098-240x(199706)20:3<269::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Gray JE, Richardson DK, McCormick MC, Workman-Daniel K, Goldmann DA. Neonatal therapeutic intervention scoring system: A therapy based severity of illness index. Pediatrics. 1992;90:561–567. [PubMed] [Google Scholar]
- Green SB. How many subjects does it take to do a regression analyses? Multivariate Behavioral Research. 1991;26:449–510. doi: 10.1207/s15327906mbr2603_7. [DOI] [PubMed] [Google Scholar]
- Grunau RE, Weinberg J, Whitfield MF. Neonatal procedural pain and preterm infant cortisol response to novelty at 8 months. Pediatrics. 2004;114:77–84. doi: 10.1542/peds.114.1.e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen HE, Biros MH, Delaney NM, Schug VL. Research utilization and interdisciplinary collaboration in emergency care. Academy of Emergency Medicine. 1999;6:271–279. doi: 10.1111/j.1553-2712.1999.tb00388.x. [DOI] [PubMed] [Google Scholar]
- Hamers JPH, Abu-Saad HH, Halfens RJ, Schumacher JN. Factors influencing nurses’ pain assessment and interventions in children. Journal of Advanced Nursing. 1994;20:853–860. doi: 10.1046/j.1365-2648.1994.20050853.x. [DOI] [PubMed] [Google Scholar]
- Hamers JPH, van den Hout MA, Halfens RJG, Kester AD. The influence of children’s vocal expressions, age, medical diagnosis and information obtained from parents on nurses’ pain assessments and decisions regarding interventions. Pain. 1996;65:53–61. doi: 10.1016/0304-3959(95)00147-6. [DOI] [PubMed] [Google Scholar]
- Jacob E, Puntillo KA. A survey of nursing practice in the assessment and management of pain in children. Pediatric Nursing. 1999;25:278–286. [PubMed] [Google Scholar]
- Johnston CC, Stevens BJ. Experience in a neonatal intensive care unit affects pain response. Pediatrics. 1996;98:925–930. [PubMed] [Google Scholar]
- Johnston CC, Stremler R, Horton L, Friedman A. Effect of repeated doses of sucrose during heel stick procedure in preterm neonates. Biology of the Neonate. 1999;75:160–166. doi: 10.1159/000014092. [DOI] [PubMed] [Google Scholar]
- Johnston CC, Stremler R, Stevens B, Horton L. Effectiveness of oral sucrose and simulated rocking on pain response in preterm neonates. Pain. 1997;72:193–199. doi: 10.1016/s0304-3959(97)00033-x. [DOI] [PubMed] [Google Scholar]
- Johnston CJ, Gagnon A, Ritchie JR, Rennick J, Bournaki H, Patenaude M, et al. Coaching one-to-one for pain practices of pediatric nurses. Journal of Pediatric Nursing. 2007;22(6):467–478. doi: 10.1016/j.pedn.2007.07.004. [DOI] [PubMed] [Google Scholar]
- Joint Commission on Accreditation of Healthcare Organizations. Pain management standards. 2001 Retrieved October 10, 2007, from http://www.jointcommission.org/NewsRoom/health_care_issues.htm#9.
- Kanter RM. Men and women of the corporation. New York: Basic Books; 1977 1993. [Google Scholar]
- Karling M, Renstrom M, Ljungman G. Acute and post operative pain in children: A Swedish nationwide survey. Acta Paediatrica. 2002;91:660–666. doi: 10.1080/080352502760069070. [DOI] [PubMed] [Google Scholar]
- Larrsson BA, Tannfeldt G, Lagercrantz H, Olsson GL. Alleviation of pain of venepuncture in neonates. Acta Paediatrica. 2000;87:774–779. doi: 10.1080/080352598750013879. [DOI] [PubMed] [Google Scholar]
- Lebovits AH, Florence I, Bathina R, Hunko V, Fox MT, Bramble CY. Pain knowledge and attitudes of healthcare providers: Practice characteristic differences. Clinical Journal of Pain. 1997;13:237–243. doi: 10.1097/00002508-199709000-00009. [DOI] [PubMed] [Google Scholar]
- Lynn MR. Determination and quantification of content validity. Nursing Research. 1986;35(6):382–385. [PubMed] [Google Scholar]
- Manworren R. Development and testing of the pediatric nurses’ knowledge and attitudes survey regarding pain. Pediatric Nurse. 2001;27(2):151–158. [PubMed] [Google Scholar]
- McCaffery M, Ferrell BR. Nurses’ knowledge of pain assessment and management: How much progress have we made? Journal of Pain and Symptom Management. 1997;14:175–188. doi: 10.1016/s0885-3924(97)00170-x. [DOI] [PubMed] [Google Scholar]
- Merriam-Webster online dictionary. 2008 Retrieved October 7, from http://www.merriam-webster.com/dictionary/expert.
- Miller PA. Nurse-physician collaboration in an intensive care unit. American Journal of Critical Care. 2001;10(5):341–350. [PubMed] [Google Scholar]
- Oberlander T, Grunau RE, Fitzgerald C, Papsdorf M, Rurak D, Riggs W. Pain reactivity in 2-month-old infants after prenatal and postnatal serotonin reuptake inhibitor medication exposure. Pediatrics. 2005;115(2):411–425. doi: 10.1542/peds.2004-0420. [DOI] [PubMed] [Google Scholar]
- O’Brien-Pallas L, Irvine D, Peereboom E, Murray M. Measuring nursing workload: Understanding variability. Nursing Economics. 1997;15(4):172–182. [PubMed] [Google Scholar]
- O’Brien-Pallas L, Thomson D, McGillis-Hall L, Pink G, Kerr M, Wang S, et al. Evidence-based Standards for Measuring Nurse Staffing and Performance. 2004 Retrieved December 1, 2004, from www.chsrf.ca/final_research/ogc/pdf/o’brien_e.pdf.
- Profetto-McGrath J, Hesketh K, Lang S, Estabrooks C. A study of critical thinking and research utilization among nurses. Western Journal of Nursing Research. 2003;25(3) doi: 10.1177/0193945902250421. 322-237. [DOI] [PubMed] [Google Scholar]
- Reyes S. Nursing assessment of infant pain. Journal of Perinatology and Neonatological Nursing. 2003;17(4):291–303. doi: 10.1097/00005237-200310000-00008. [DOI] [PubMed] [Google Scholar]
- Shah VS, Taddio A, Bennett S, Speidel BD. Neonatal pain response to heelsticks vs venepuncture for routine blood sampling. Archives of Disease Child and Fetal Neonatal Education. 2000;77:F143–F144. doi: 10.1136/fn.77.2.f143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons SHP, van Dijk M, Anand KS, Roofthooft D, vanLingren RA, Tibboel D. Do we still hurt newborn babies? Archives of Pediatrics and Adolescent Medicine. 2003;157:1058–1064. doi: 10.1001/archpedi.157.11.1058. [DOI] [PubMed] [Google Scholar]
- Stevens B, McGrath P, Gibbins S, Beyene J, Breau L, Camfield C, et al. Procedural pain in newborns at risk for neurologic impairment. Pain. 2003;105(1–2):27–35. doi: 10.1016/s0304-3959(03)00136-2. [DOI] [PubMed] [Google Scholar]
- Stevens B, Yamada J, Ohlsson A. Sucrose for analgesia in newborn infants undergoing painful procedures. Cochrane Database Systematic Review. 2004;(3):CD001069. doi: 10.1002/14651858.CD001069.pub2. [DOI] [PubMed] [Google Scholar]
- Taddio A, Katz J, Ilesrich AL, Koren E. Effect of neonatal circumcision on pain response during subsequent routine vaccination. Lancet. 1997;349(9052):599–603. doi: 10.1016/S0140-6736(96)10316-0. [DOI] [PubMed] [Google Scholar]
- Thompson GN, Estabrooks CA, Degner L. Clarifying the concepts in knowledge transfer: A literature review. Journal of Advanced Nursing. 2006;53(6):691–701. doi: 10.1111/j.1365-2648.2006.03775.x. [DOI] [PubMed] [Google Scholar]
- Tibby SM, Correa-West J, Durward A, Ferguson L, Murdoch I. Adverse events in a pediatric intensive care unit: Relationship to workload, skill mix and staff supervision. Intensive Care Medicine. 2004;1(16):1160–1166. doi: 10.1007/s00134-004-2256-y. Retrieved January 25, 2005, from Pubmed database. [DOI] [PubMed]
- Tourangeau AE, Cranley LE, Jeffs L. Impact of nursing on hospital patient mortality: A focused review and related policy implications. Journal of Quality and Safety in Health Care. 2006;15:4–8. doi: 10.1136/qshc.2005.014514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JUK Neonatal Staffing Study Group. Patient volume, staffing, and workload in relation to risk adjusted outcomes in a random stratified sample of UK neonatal intensive care units: A prospective evaluation. Lancet. 2002;359(9301):99–107. doi: 10.1016/s0140-6736(02)07366-x. [DOI] [PubMed] [Google Scholar]
- Weiss SJ, Davis HP. Validity and reliability of the collaborative practice scales. Nursing Research. 1985;34(5):299–305. [PubMed] [Google Scholar]
- Wild LR, Mitchell PH. Quality pain management outcomes: The power of place. Outcomes Management for Nursing Practice. 2000;4(3):136–143. [PubMed] [Google Scholar]
- Willson H. Factors affecting the administration of analgesia to patients following repair of fractured hip. Journal of Advanced Nursing. 2000;31(5):1145–1154. doi: 10.1046/j.1365-2648.2000.01425.x. [DOI] [PubMed] [Google Scholar]
- Van Hulle Vincent C. Nurses knowledge, attitudes and practices: Regarding children’s pain. The American Journal of Maternal Child Nursing. 2005;30(3):177–183. doi: 10.1097/00005721-200505000-00005. [DOI] [PubMed] [Google Scholar]
- Xavier Balda R, Guinsburg R, de Almeida MF, Peres C, Miyoshi MH, Kopelman MI. The recognition of facial expression of pain in full-term newborns by parents and health professionals. Archives of Pediatrics and Adolescent Medicine. 2000;154(10):1009–1016. doi: 10.1001/archpedi.154.10.1009. [DOI] [PubMed] [Google Scholar]