Abstract
Context:
Whether offspring of parents with bipolar disorder (BP) are at specifically high risk to develop BP and other psychiatric disorders has not been adequately studied.
Objective:
To evaluate lifetime prevalence and specificity of psychiatric disorders in offspring of parents with BP-I and BP-II.
Design:
Offspring aged 6 to 18 years who have parents with BP and community control subjects were interviewed with standardized instruments. All research staff except the statistician were blind to parental diagnoses.
Setting:
Parents with BP were recruited primarily through advertisement and outpatient clinics. Control parents were ascertained by random-digit dialing and were group matched for age, sex, and neighborhood to parents with BP.
Participants:
Three hundred eighty-eight offspring of 233 parents with BP and 251 offspring of 143 demographically matched control parents.
Main Outcome Measures:
Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition) Axis I disorders.
Results:
Adjusting for demographic factors, living with 1 vs both biological parents, both biological parents' non-BP psychopathology, and within-family correlations, offspring of parents with BP showed high risk for BP spectrum disorders (odds ratio [OR]=13.4; 95% confidence interval [CI], 2.9-61.6) and any mood (OR=5.2; 95% CI, 2.3-11.4), anxiety (OR=2.3; 95% CI, 1.3-4.0), and Axis I (OR=2.2; 95% CI, 1.5-3.3) disorders. Off-spring of parents with BP with high socioeconomic status showed more disruptive behavior disorders and any Axis I disorders than offspring of control parents with high socioeconomic status. Families in which both parents had BP had more offspring with BP than families with only 1 parent with BP (OR=3.6; 95% CI, 1.1-12.2). More than 75.0% of offspring who developed BP had their first mood episode before age 12 years, with most of these episodes meeting criteria for BP not otherwise specified and, to a lesser degree, major depression.
Conclusions:
Offspring of parents with BP are at high risk for psychiatric disorders and specifically for early-onset BP spectrum disorders. These findings further support the familiality and validity of BP in youth and indicate a need for early identification and treatment.
Upto 60% of adults with bipolar disorder (BP) experience their first mood symptoms before age 21 years.1-3 Because better outcome may be associated with earlier treatment, it is important for clinicians to identify and treat BP early in life to hopefully be able to prevent the high psychosocial and medical morbidity and mortality associated with this disorder.1 The single best predictive factor associated with the risk of developing BP is high family loading for the disorder.1,3,4 Therefore, carefully evaluating and prospectively following the psychopathology of offspring of parents with BP and comparing them with offspring of parents with and without non-BP psychopathology, are critical for identifying the early clinical presentation of BP.
A meta-analysis and more recent studies have reported rates of BP between 4% and 15% in the offspring of parents with BP and between 0% and 2% in the offspring of healthy parents.5 Bipolar disorder may first manifest in the form of depression,1,3,6,7 and the symptoms of BP overlap and may be confused with symptoms of other common child psychiatric disorders such as attention-deficit/hyperactivity disorder (ADHD) or disruptive behavior disorders (DBDs).3,6-9 Therefore, in addition to BP, it is important to evaluate the rates of non-BP disorders in offspring of parents with BP. In the meta-analysis cited earlier,5 rates of any mood disorders were 26.5% in offspring of parents with BP vs 8.3% in offspring of healthy control parents and the rates of any psychiatric disorder were 52% vs 29%, respectively. More recent studies10-16 also reported high risk for both mood and nonmood disorders in offspring of parents with BP when compared with offspring of parents with and without non-BP psychopathology. However, there is substantial variability in the results.
Discrepancies among the existing studies are likely owing to methodological limitations, including small samples, use of convenience samples, ascertainment bias (eg, recruiting clinically referred children whose parents also have BP), lack of direct interviews with children, differences in the instruments and conceptualization of BP, lack of specification of the BP subtypes studied, method of counting the overlapping symptoms of BP and other disorders, and evaluations by interviewers who were not blinded to parental diagnoses.5,13,15,16 Furthermore, with the exception of a few studies,11,14 most studies included only offspring of healthy parents as a comparison group. Finally, most studies did not take into account the effects of other factors that could have influenced the prevalence of the child's psychopathology such as parents' non-BP psychopathology, demographic characteristics, and family environment.
The main goal of this article is to evaluate the prevalence of lifetime psychiatric disorders in offspring of parents with BP and a random sample of community control parents ascertained through the Bipolar Offspring Study (BIOS). Subsequent reports will focus on other important cross-sectional and longitudinal data collected through BIOS such as rates of potential clinical phenotypes for BP (eg, irritability, sleep patterns), the cosegregation and temporal relation of non-BP and BP disorders, the effects of negative events on the child's outcome, and rates of categorical and dimensional psychopathology in toddlers of parents with BP. Based on the extant literature, it was hypothesized that offspring of parents with BP have higher rates of BP, major depressive disorder (MDD), anxiety disorders, DBDs, and ADHD when compared with offspring of control parents.
METHODS
SUBJECTS
Parents with BP were recruited through advertisement (53.0%), adult BP studies (31.0%), and outpatient clinics (16.0%). There were no differences in BP subtype, age at BP onset, or rates of non-BP disorders on the basis of recruitment source. Parents were required to fulfill DSM-IV17 criteria for BP-I or BP-II. Exclusion criteria included current or lifetime diagnoses of schizophrenia, mental retardation, mood disorders secondary to substance abuse, medical conditions, or medication use, and living more than 200 miles away from Pittsburgh, Pennsylvania.
Control parents consisted of healthy parents or parents with non-BP psychiatric disorders from the community and were group matched by age, sex, and neighborhood using the area code and the first 3 digits of the telephone number and the zip code of the parents with BP. The exclusion criteria for the control parents were the same as those for the parents with BP, with the additional requirements that neither of the biological parents could have BP and they could not have a first-degree relative with BP. Control parents were recruited by the University Center for Social and Urban Research, University of Pittsburgh in an approximate ratio of 1 control parent for every 2 parents with BP.
With the exception of children who were unable to participate (eg, those diagnosed with mental retardation), all offspring aged 6 to 18 years from each family were included in the study.
PROCEDURES
After institutional review board approval and obtaining consent from parents and assent from children, parents were assessed for psychiatric disorders, family psychiatric history, and other variables such as dimensional psychopathology, family environment, and exposure to negative life events. Only instruments directly related to this article will be discussed.
For probands and biological coparents who participated in direct interviews (30.0%), DSM-IV psychiatric disorders were ascertained through the Structured Clinical Interview for DSMIV18 plus the ADHD, DBD, and separation anxiety disorder sections from the Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present and Lifetime Version (K-SADS-PL).19
The family history–research diagnostic criteria method20 plus ADHD and DBD items from the K-SADS-PL were used to ascertain the psychiatric history of second-degree relatives, biological coparents not seen for direct interview, and siblings of offspring who were too old (aged >18 years) to participate at intake.
Parents were interviewed about their children and the children were directly interviewed for the presence of lifetime nonmood psychiatric disorders using the K-SADS-PL. To evaluate the severity of each mood symptom, the K-SADS-PL Mania Rating Scale21,22 and the depression section of the Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present Version were used (for these instruments, see http://www.wpic.pitt.edu/research under “Assessment Instruments”).
As per the instructions for the K-SADS-PL, mood symptoms that were also in common with other psychiatric disorders (eg, hyperactivity) were not rated as present in the mood sections unless they intensified with the onset of abnormal mood. Comorbid diagnoses were not assigned if they occurred exclusively during a mood episode.
All of the diagnoses were made using the DSM-IV criteria. However, to avoid diagnosing youth with “soft” BP symptoms, an operationalized and more strict DSM-IV BP not-otherwise-specified (NOS) diagnosis was used (see the articles by Axelson et al7, Birmaher et al23, and Leibenluft and Rich24 for further details). Youth with this more strict BP-NOS diagnosis have similar but less severe clinical pictures, comorbid disorders, family history, and longitudinal outcomes than the subjects with BP-I.7,23 Moreover, about 25.0% of these youth diagnosed with BP-NOS had their diagnoses converted to BP-I or BP-II.23 With the exception of BP-NOS in children and biological coparents, other NOS and adjustment disorders for children or adults were not included in this study.
Onset of a mood episode was defined as the first episode of MDD or BP. Onset of BP was defined as the first episode of mania, hypomania, mixed, or operationalized criteria for BP-NOS. Given the controversies of diagnosing BP in very young children, the minimum age at onset for BP spectrum disorders was arbitrarily set at age 4 years.
Bachelors- or masters-level interviewers completed all of the assessments after intensive training for all of the instruments and after 80% agreement or better with a certified rater. The overall Structured Clinical Interview for DSM-IV and K-SADS-PL κ statistics for psychiatric disorders were 0.8 or greater.
About 90.0% of assessments were carried out in the subjects' homes. To ensure blindness to parental diagnoses, the interviewers who met with the parents to assess parental psychopathology were different from the interviewers who assessed their children's psychopathology. All of the data (from the adult, child, and family) were presented to a child psychiatrist for diagnostic confirmation. The child psychiatrists were also blinded to the psychiatric status of the parents. When necessary, subjects' medical and psychiatric records were obtained and reviewed by their respective interviewers. All diagnoses in the parents, children, and relatives were made according to the best-estimate procedure.25
The Petersen Pubertal Developmental Scale26 and respective Tanner stages27,28 were used to evaluate pubertal development. Socioeconomic status (SES) was ascertained using the Hollingshead scale.29
STATISTICAL ANALYSES
The demographic and clinical characteristics between the groups were evaluated using t, χ2, and Fisher exact tests as appropriate. Analyses of the effects of any between-group demographic differences and non-BP psychiatric disorders of both biological parents from the BP and control groups were performed using a series of hierarchical logistic regressions. To account for the presence of within-family correlations, mixed-effects nominal logistic regressions were used.30
The cumulative rates of mood episodes by age at onset between the offspring of parents with BP and control parents were analyzed using the Kaplan-Meier procedure. Because age and pubertal status were highly correlated (ρ=0.88; P<.001), only age effects are included in this article. Effect sizes for continuous and categorical variables (d and h, respectively) were calculated as described by Cohen.31 All of the P values are based on 2-tailed tests with α=.05.
RESULTS
PARENTS
Parents With BP
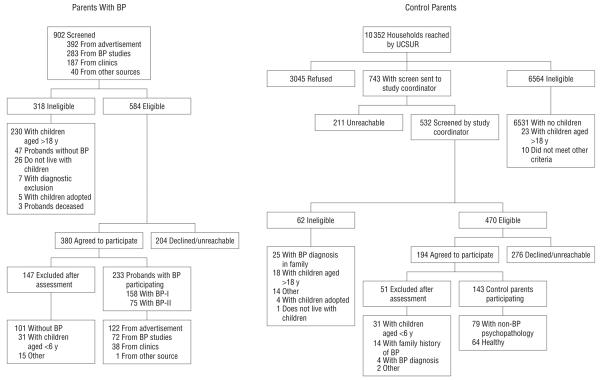
Of the 902 subjects screened by telephone, 584 were qualified for a face-to-face interview with the Structured Clinical Interview for DSM-IV to verify that they had BP (Figure 1). Of these, 204 declined further participation (for reasons of geographic distance, lack of time, custody issues, or not wanting their children to know that they have BP) or were unreachable. Because screening was done over the telephone and prior to obtaining subjects' consent, the institutional review board did not permit the recording of demographic information. Thus, comparisons between subjects who declined and those who agreed to further participation are not available. Of the 380 subjects who agreed to be interviewed, 147 were excluded mainly because they did not fulfill criteria for BP or they only had children younger than 6 years, for a final sample of 233 parents with BP (158 with BP-I and 75 with BP-II). Of the 233 parents with BP, 187 (80.3%) were female. Ten families had 2 parents with BP spectrum disorders (1 family with both parents having BP-I, 1 family with both parents having BP-II, 4 families with 1 parent having BP-I and 1 parent having BP-II, 3 families with 1 parent having BP-I and 1 parent having BP-NOS, and 1 family with 1 parent having BP-II and 1 parent having BP-NOS). About 64.0% of the parents with BP reported that their mood disorder started when they were younger than 20 years, 48.0% when they were younger than 17 years, and 18.0% when they were younger than 13 years.
Figure 1.
Recruitment of parents with bipolar disorder (BP) and community control parents (probands). UCSUR indicates University Center for Social and Urban Research.
Control Parents
Of the 743 community parents referred by the University Center for Social and Urban Research, 532 were reachable and screened by one of the coordinators from BIOS by telephone (Figure 1). Of these, 470 were eligible for face-to-face interviews with the Structured Clinical Interview for DSM-IV; 276 declined participation or were not able to schedule or attend an intake assessment. Owing to institutional review board reasons previously mentioned, demographic information was not available from subjects who declined participation or were unreachable. Fifty-one of the remaining 194 subjects were excluded primarily because of a diagnosis or family history of BP, resulting in a final number of 143 community control parents (79 with non-BP psychiatric disorders and 64 without any psychopathology). Of these cases, none reported BP in their known second-degree relatives.
Demographic Comparisons
Parents with BP were more likely to be white, were less likely to be married at intake, and had slightly lower SES than control parents (Table 1). Compared with the control parents with non-BP psychopathology, parents with BP showed similar demographic characteristics. On average, both groups of parents included 2 children in the study.
Table 1.
Demographic Characteristics and Lifetime Axis I Psychiatric Disorders of Parents With Bipolar Disorder vs Community Control Parents
| Characteristic | Parents With Bipolar Disorder (n=233) |
Community Control Parents (n=143) |
Statistic |
P Value (Effect Size) |
|---|---|---|---|---|
| Demographic | ||||
| Age, mean (SD), y | 39.5 (7.6) | 40.9 (7.4) | t=1.82 | .07 (0.19) |
| Female, % | 80.3 | 77.6 | χ2=0.37 | .50 (0.05) |
| White, % | 88.4 | 75.5 | χ2=10.69 | .001 (0.32) |
| SES, mean(SD)a | 2.9 (1.2) | 3.2 (1.1) | t=2.10 | .04 (0.26) |
| Married at intake, % | 48.5 | 65.7 | χ2=10.64 | .001 (0.37) |
| No. of offspring included, mean (SD) | 1.7 (0.8) | 1.8 (0.8) | t=1.03 | .30 (0.13) |
| Lifetime Axis I psychiatric disorders, % | ||||
| Any Axis I disorders | 100.0 | 54.5 | χ2=128.04 | <.001 (1.50) |
| BP-I | 67.8 | 0.0 | NA | NA |
| BP-II | 32.2 | 0.0 | NA | NA |
| Unipolar MDD | NA | 25.2 | NA | NA |
| Dysthymic disorder | 2.6 | 5.6 | χ2=2.25 | .10(0.15) |
| Any anxiety disorders | 72.5 | 20.3 | χ2=97.05 | <.001 (1.10) |
| Panic disorder | 39.9 | 4.9 | χ2=55.66 | <.001 (0.92) |
| DBDsb | 36.9 | 8.4 | χ2=37.40 | <.001 (0.73) |
| ADHD | 27.5 | 2.8 | χ2=36.41 | <.001 (0.77) |
| Any substance abusec | 63.9 | 28.0 | χ2=45.88 | <.001 (0.72) |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; BP, bipolar disorder; DBDs, disruptive behavior disorders; MDD, major depressive disorder: NA, not applicable; SES, socioeconomic status.
A value of 3 is equivalent to an SES of III, middle class, on the Hollingshead scale.
Includes oppositional defiant disorder and conduct disorder.
Includes alcohol, marijuana, and cocaine.
Axis I Disorders
With the exception of dysthymic disorder, all of the psychiatric disorders were present in higher rates in the parents with BP than in the control parents (all P≤.001; effect size [ES], 0.72-1.50) (Table 1). Within the parents with BP, there were no significant differences in the rates of psychopathology between those recruited through advertisement and those recruited through other means.
Psychopathology in the Biological Coparent
There was no difference in the proportion of direct assessments used to obtain the nonproband biological parent's psychiatric disorders between parents with BP and control parents (26.3% vs 27.8%, respectively). The biological coparents of the offspring of parents with BP as compared with the biological coparents of the offspring of control parents showed higher rates of any Axis I psychiatric disorders (48.2% vs 29.1%, respectively), BP (3.9% [3 subjects with BP-I, 3 subjects with BP-II, and 3 subjects with BP-NOS] vs 0%, respectively), substance abuse (30.2% vs 16.6%, respectively), and DBDs (5.9% vs 1.3%, respectively) (all P≤.03). No other differences were found.
OFFSPRING
Demographic Comparisons
Three hundred eighty-eight offspring of parents with BP and 251 offspring of control parents (161 from parents with ≥1 parent with non-BP psychopathology and 90 from healthy parents) were recruited (Table 2). No families were rejected if 1 of the children refused to participate. Only 7 children of parents with BP and 4 children of control parents were not eligible or refused to participate. The diagnoses of these children were captured in the family history.
Table 2.
Demographic Characteristics and Axis I Lifetime Psychiatric Disorders of Offspring of Parents With Bipolar Disorder
| Characteristic | Offspring of Parents With BP (n=388) |
Offspring of Community Control Parents (n=251) |
Statistic |
P Value (Effect Size) |
|---|---|---|---|---|
| Demographic | ||||
| Age, mean (SD), y | 11.9 (3.6) | 11.8 (3.5) | t=0.54 | .60 (0.03) |
| Female, % | 48.5 | 54.6 | χ2=2.29 | .10 (0.14) |
| White, % | 81.4 | 74.1 | χ2=4.88 | .03 (0.17) |
| Tanner stage, %a | ||||
| I, II, or II | 65.6 | 66.4 | χ2=0.04 | .80 (0.00) |
| IV or V | 34.4 | 33.6 | ||
| Living with both biological parents, % | 42.5 | 60.2 | χ2=18.96 | <.001 (0.36) |
| Lifetime Axis I psychiatric disorders, % | ||||
| Any Axis I disorders | 52.1 | 29.1 | χ2=32.82 | <.001 (0.47) |
| Any mood disorder | 21.1 | 4.4 | χ2=34.39 | <.001 (0.55) |
| BP spectrum disorders | 10.6 | 0.8 | χ2=23.18 | <.001 (0.48) |
| BP-I | 2.1 | 0.0 | FET | .03 (0.28) |
| BP-II | 1.3 | 0.4 | FET | .40 (0.10) |
| BP-NOS | 7.2 | 0.4 | χ2=16.35 | <.001 (0.44) |
| Any depression | 10.6 | 3.6 | χ2=10.30 | .001 (0.27) |
| Dysthymic disorder | 1.5 | 0.4 | FET | .26 (0.15) |
| MDD | 9.1 | 3.2 | χ2=8.26 | .004 (0.26) |
| Any anxiety disorders | 25.8 | 10.8 | χ2=21.58 | <.001 (0.39) |
| SAD, GAD, and/or SP | 22.2 | 7.6 | χ2=23.64 | <.001 (0.40) |
| Panic disorder | 1.0 | 1.6 | FET | .70 (0.08) |
| OCD | 2.6 | 0.4 | FET | .06 (0.25) |
| PTSD | 4.6 | 3.6 | χ2=0.42 | .50 (0.05) |
| DBDs | 19.1 | 8.0 | χ2=14.98 | <.001 (0.33) |
| ODD | 17.0 | 6.4 | χ2=15.41 | <.001 (0.36) |
| CD | 3.6 | 2.4 | χ2=0.74 | .40 (0.12) |
| ADHD | 24.5 | 16.7 | χ2=5.44 | .02 (0.17) |
| Any substance abuse | 3.9 | 2.8 | χ2=0.53 | .50 (0.06) |
| Alcohol | 1.8 | 1.6 | FET | >.99 (0.00) |
| Drugs | 3.6 | 1.6 | χ2=2.26 | .10 (0.12) |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; BP, bipolar disorder; CD, conduct disorder; DBDs, disruptive behavior disorders; FET, Fisher exact test; GAD, generalized anxiety disorder; MDD, major depressive disorder; NOS, not otherwise specified; OCD, obsessive-compulsive disorder; ODD, oppositional defiant disorder; PTSD, posttraumatic stress disorder; SAD, separation anxiety disorder; SP, social phobia.
A Tanner stage of I indicates prepubertal; II to III, midpubertal; and IV to V, postpubertal.
Offspring of parents with BP were more likely to be white and less likely to be living with both biological parents than offspring of control parents. There were no other between-group demographic differences.
Axis I Disorders
With the exceptions of BP-II and dysthymic, panic, obsessive-compulsive, posttraumatic stress, conduct, and substance use disorders, all psychiatric disorders were present in higher rates in the offspring of parents with BP than in the offspring of control parents (all P≤.02; ES, 0.17-0.55) (Table 2).
Specifically for BP spectrum disorders, offspring of parents with BP showed significantly more BP spectrum disorders (41 of 388 children [10.6%]; 8 with BP-I, 5 with BP-II, and 28 with BP-NOS) than offspring of control parents (2 of 251 children [0.8%]) (P<.001; ES, 0.48). This increased rate of BP was accounted for by significantly higher rates of BP-I (P = .03; ES, 0.28) and BP-NOS (P<.001; ES, 0.44). Nearly all of the BP-NOS cases were not given the diagnosis of BP-I or BP-II because they did not meet the DSM-IV duration criteria. In addition to elation and/or irritability, all of the children with BP-NOS had an average of 4 clinically significant DSM-IV BP symptoms (range, 3-9 symptoms), whereas children with BP-I or BP-II had an average of 5 symptoms (range, 2-9 symptoms). Within the 41 children with BP spectrum disorders who have parents with BP, 31 (75.6%) had onset of their BP prior to age 12 years and 10 (24.4%) had onset at or after age 12 years, with most of these first episodes being NOS (19 vs 4 subjects, respectively), followed by MDD (8 vs 4 subjects, respectively), mania (3 subjects vs 1 subject, respectively), and hypomania (1 subject each) (all P>.05). Of the 41 subjects, 35 (85.4%) had a co-morbid disorder (51.0% had any anxiety disorder, 53.0% had DBD, and 39.0% had ADHD).
Offspring of families with 2 parents with BP spectrum disorders had BP significantly more often when compared with families with 1 parent with BP (4 of 14 subjects [28.6%] vs 37 of 374 subjects [9.9%], respectively; Fisher exact test, P=.05; odds ratio [OR]=3.6; 95% confidence interval [CI], 1.1-12.2). There were no other differences in child psychopathology between offspring of families with 1 or 2 parents with BP.
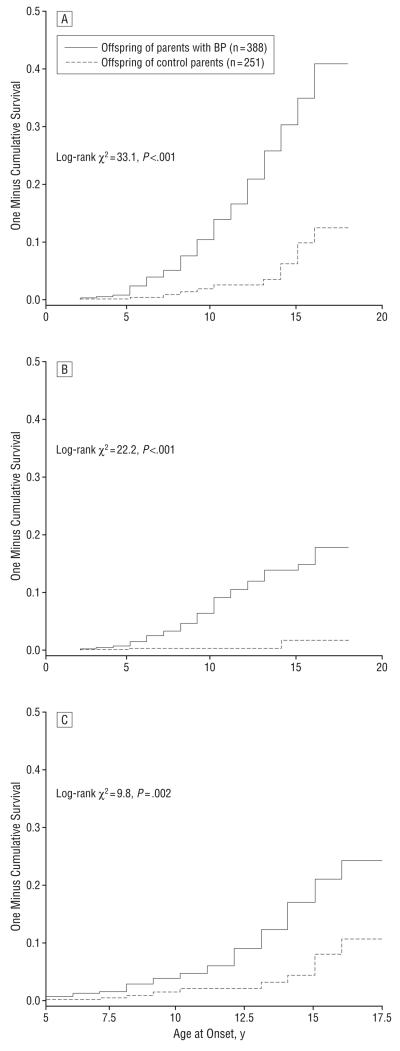
As shown in Figure 2A, offspring of parents with BP had higher morbid risk of any mood episodes with a cumulative risk of approximately 20.9% by age 12 years and 40.8% by age 18 years (hazard ratio=5.1; 95% CI, 2.7-9.6). Offspring of parents with BP also had a significantly higher risk of BP and depressive episodes. For BP (Figure 2B), the cumulative risk was 12.0% by age 12 years and 17.8% by age 18 years (hazard ratio=3.0; 95% CI, 1.4-6.1). For MDD (Figure 2C), the cumulative risk was 9.1% by age 12 years and 24.3% by age 18 years (hazard ratio=13.5%; 95% CI, 3.3-55.8). For all of the earlier-noted comparisons, there were no age×group interactions.
Figure 2.
Cumulative rates by age at onset of any mood episodes (A), bipolar disorder (BP) episodes (mania, hypomania, mixed, or operationalized BP not-otherwise-specified episodes) (B), and depressive episodes (major depressive episodes excluding youth with BP) (C).
Mixed-Effects Logistic Regression
After adjusting for offspring's age, race, SES, living with both biological parents, both biological parents having non-BP disorders, and within-family correlations, when compared with the offspring of control parents, the offspring of parents with BP showed significantly higher risk for any Axis I disorders (OR=2.2; 95% CI, 1.5-3.3), any mood disorder (OR=5.2; 95% CI, 2.3-11.4), BP spectrum disorders (OR=13.4; 95% CI, 2.9-61.6), and any anxiety disorders (OR=2.3; 95% CI, 1.3-4.0) (OR=3.0 for separation anxiety disorder, generalized anxiety disorder, and/or social phobia) (Table 3).
Table 3.
Adjusted Odds Ratios for Bipolar and Other Psychiatric Disorders in Offspring of Parents With Bipolar Disorder
| OR (95% CI) |
|||
|---|---|---|---|
| Disorders | Offspring of Parents With BP vs Offspring of All Control Parentsa |
Offspring of Parents With BP vs Offspring of Control Parents With Non-BP Psychopathologyb |
Offspring of Parents With BP vs Offspring of Healthy Control Parentsb |
| Any Axis I disorders | 2.2 (1.5-3.3)c | 2.0 (1.3-3.1)c | 4.0 (1.3-12.1)c |
| Any mood disorder | 5.2 (2.3-11.4)c | 4.3 (1.9-9.7)c | 18.3 (1.7-200.0)c |
| BP spectrum disorders | 13.4 (2.9-61.6)c | 9.1 (2.0-41.7)c | 15.1 (2.7-∞))c,d |
| Depressive disorderse | 2.1 (0.9-4.9) | 1.9 (0.8-4.6) | 4.8 (0.3-68.6) |
| Any anxiety disorders | 2.3 (1.3-4.0)c | 2.2 (1.2-3.9)c | 3.8 (0.5-27.5) |
| SAD, GAD, and/or SP | 3.0 (1.5-5.9)c | 2.9 (1.5-5.9)c | 4.1 (0.4-46.5) |
| DBDs | 2.1 (0.9-4.4) | 2.1 (0.9-4.6) | 1.9 (0.2-22.6) |
| ODD | 1.9 (0.9-4.0) | 2.0 (0.9-4.3) | 1.3 (0.1-19.3) |
| CD | 1.3 (0.2-8.2) | 1.2 (0.2-8.9) | 2.8 (0.1-220.7) |
| ADHD | 1.4 (0.9-2.3) | 1.2 (0.7-2.1) | 3.5 (1.1-11.4)c |
| Substance abuse | 0.7 (0.1-6.1) | 0.7 (0.3-2.3) | 2.1 (0.2-17.5) |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; BP, bipolar disorder; CD, conduct disorder; CI, confidence interval; DBDs, disruptive behavior disorders; GAD, generalized anxiety disorder; ODD, oppositional defiant disorder; OR, odds ratio; SAD, separation anxiety disorder; SP, social phobia
Adjusting for offspring's age, race, socioeconomic status, living with both biological parents, and within-family correlations.
Adjusting for offspring's age, race, socioeconomic status, living with both biological parents, both biological parents' non-BP psychopathology, and within-family correlations.
Results are significant, with P≤.04.
The upper 95% confidence limit to ∞ is owing to no BP in offspring of healthy control parents
Includes major depressive disorder and dysthymic disorder.
Offspring of parents with BP and SES higher than the median (34, which corresponds to class III) showed significantly more DBDs and any Axis I disorders than offspring of control parents with higher SES (DBDs: 15.2% vs 2.1%, respectively; χ2=15.9; OR=5.6; 95% CI, 1.6-19.0; Axis I disorders: 49.1% vs 17.5%, respectively; χ2=34.4; OR=3.6; 95% CI, 2.1-6.3). In contrast, in parents with SES of 34 or lower, there were no between-group differences in the rates of DBDs and Axis I disorders between offspring of parents with BP and control parents (DBDs: 22.1% vs 15.7%, respectively; Axis I disorders: 54.4% vs 44.4%, respectively). There were no effects of race or sex. Similar results were observed when oppositional defiant disorder and conduct disorder were analyzed separately, after excluding offspring with DBDs from the analyses of any Axis I disorders, or after adjusting for multiple comparisons.
For comparison with the existing literature, in addition to showing the adjusted ORs for all of the offspring of the control parents, Table 3 shows the adjusted ORs for the offspring of the control parents stratified by the presence of parental non-BP psychopathology.
COMMENT
As compared with offspring of control parents, offspring of parents with BP showed a 14-fold increase in the rates of BP spectrum disorders and approximately a 2- to 3-fold increase in any mood and anxiety disorders after adjusting for both biological parents' non-BP psychiatric disorders, significant between-group demographic variables, and within-family correlations. Also, the offspring of parents with BP and higher SES showed 4- and 6-fold increases in the rates of any Axis I disorders and DBDs, respectively. Families in which both parents had BP had more offspring with BP spectrum disorders than families in which only 1 parent had BP. Most of the offspring's BP episodes started during childhood, with most first episodes being of the NOS type and, to a lesser degree, depression episodes. As expected, about 85.0% of children with BP had other comorbid disorders, mainly anxiety disorders, DBDs, and ADHD.
Before discussing each of the earlier-noted findings, the limitations of the study deserve comment. First, because most children have not reached the age of highest risk to develop BP, the rate of BP in these children is likely to continue to increase with further follow-up. Second, as in any pediatric study, the probands for both the BP and control groups were much more likely to be the mothers rather than the fathers. In addition, the psychopathology in the biological coparents was mainly ascertained by interviewing the probands. However, there were no between-group differences in rates of mothers serving as the probands and no differences in the proportion of direct and indirect interviews of the co-biological parents with BP and control parents. Third, because the diagnosis of BP-II in adults appears to be low even with direct interviews,32 it is possible that in using indirect interviews we could have missed some of these diagnoses in relatives of both groups. Nevertheless, the rates of BP-II found in the study are similar to those reported in epidemiological studies.33,34 Fourth, although there are contradictory results in the literature and the effects seem to be small,35-38 parents with psychopathology could have been more interested in having their children evaluated through the study and may have had greater knowledge of the disorder, possibly inflating the rate of disorders in their offspring. However, at least for the control parents (of whom 50% had psychopathology), the rates of lifetime psychiatric disorders in their offspring were similar to those described in other community studies.39-41 Finally, although the literature is controversial,42,43 parents who participated in BIOS could have had more psychopathology than those who did not participate. However, the rates of psychiatric disorders in parents with BP and their age at BP onset were similar to those reported in the adult BP literature.1,33,34,44,45 Moreover, parents with BP and control parents with non-BP psychopathology were comparable in demographic characteristics and recruitment origin. Finally, taking into consideration the age and sex of the control parents recruited in BIOS, the lifetime prevalence of psychiatric disorders found in these parents is similar to that reported in a recent large epidemiological study in the United States.46
Both biological parents of the offspring of parents with BP showed considerably higher rates of Axis I psychiatric disorders than the control parents. Thus, it is not surprising that their offspring showed more psychopathology than the offspring of control parents. However, together with prior “top-down”5,10-16 and “bottom-up” BP family studies,1,3,47-51 BIOS provides further evidence that offspring of parents with BP are at specifically high risk to develop early-onset BP. Noticeably and similar to BIOS, in a review of the adult BP literature, the average age-adjusted lifetime prevalence for BP spectrum disorders in first-degree relatives was 10.7%, compared with 1.0% for the relatives of healthy control subjects.1
In BIOS, most of the children diagnosed with BP fulfilled the operationalized criteria for BP-NOS7,24 and 56.0% of the first episodes were of the NOS type. As in another investigation,7 most of these youth did not meet criteria for BP-I or BP-II because they lacked the current DSM-IV episode duration requirements for the diagnosis of these disorders. Thus, it appears that early-onset BP with genetic loading may often present with subthreshold manic symptoms before reaching full DSM-IV criteria for BP-I or BP-II. Because youth with the stricter definition of BP-NOS are at high risk for diagnoses converting to BP-I or BP-II,23 follow-up of the subjects with BP-NOS in BIOS will provide an additional test of the validity of the BP-NOS phenotype in a nonreferred high-risk sample.
Consistent with the literature,2,45,52-54 most parents with BP recollected that their illness started before age 20 years and about 20.0% had illness that started before age 13 years. In contrast, most of their children developed their first BP episode before age 12 years, suggesting the possibility that parents were more perceptive of their children's symptoms early in life or perhaps that BP has more penetrance and manifests earlier in new generations.45,52,55
Offspring of families in which both parents had BP were 3.6 times more likely to have BP, without being at higher risk for any other psychiatric disorders as compared with families with only 1 parent with BP. One child study and other adult family studies reported similar findings,1,56 giving further evidence to the specificity of the family transmission of BP. Future articles will examine the earlier-noted results in greater depth and analyze other important issues such as the parent-of-origin effect and the effects of second-degree family psychopathology.
Similar to a meta-analysis of studies of pediatric high risk for BP5 and other recent studies,14 after adjusting for confounding factors, there were no between-group differences in the rates of MDD in the offspring. Bottom-up family studies have also shown that the first-degree relatives of youth with BP have significantly more depression when compared with first-degree relatives of healthy children48-50 but not when compared with the first-degree relatives of children with non-BP disorders.49,50,57 As expected,11,12,14,58,59 rates of depression increased during adolescence. Because BP may manifest its first symptoms with depression (30.0% in BIOS),3,60-63 particularly if there is family history of BP,61,64-66 it is likely that a significant proportion of the depressed children of parents with BP included in this study will eventually develop BP.
After adjusting for confounding factors, the offspring of parents with BP showed significantly higher rates of anxiety disorders, particularly generalized anxiety disorder, social phobia, and/or separation anxiety disorder, when compared with the offspring of control parents. There were no differences in the rates of other anxiety disorders, but the base rate of these disorders was low. Other studies of high risk for BP and studies of adults and youth with BP have also reported high rates of anxiety disorders.7,9,67-73 Also, high rates of anxiety disorders have been consistently observed in adults with early-onset BP when compared with adults with late-onset BP,1,70,71 and anxiety disorders appear to be associated with increased risk of developing BP during adulthood.44,74,75 Ongoing prospective follow-up of children recruited into BIOS will help to address this question.
High rates of DBDs and ADHD have been reported in offspring of parents with BP when compared with offspring of healthy parents5,9,16 and parents with non-BP disorders.11 Because some of the symptoms of these disorders overlap with the symptoms of BP69 and because mood disorders in youth are often manifested by severe irritability, ADHD-like symptoms, and oppositional behaviors, the earlier-noted findings have suggested that these symptoms may be one of the ways BP is manifested early in life or may be prodromal symptoms of BP.14,76-78 In BIOS, initial analyses also showed significant differences in the rates of DBDs, oppositional defiant disorder, and ADHD between the offspring of parents with BP and control parents. However, after adjusting for confounding variables, there were differences only in the rate of DBDs between offspring of parents with BP and healthy parents but not between offspring of parents with BP and control parents with non-BP psychopathology (Table 3). Thus, the presence of DBDs in the offspring of parents with BP seems to be related to general parental psychopathology or other related factors.
Of note, offspring of parents with BP with high SES showed more DBDs and any Axis I disorders than offspring of control parents with high SES. Because low SES has been associated with higher risk for childhood psychopathology, particularly behavior disorders,79 it is possible that higher SES is not protective in offspring of parents with BP. Alternatively, low SES may be such a strong predictor of DBDs that having a parent with BP confers no further risk of DBDs among subjects with low SES. Follow-up of the BIOS sample will further clarify whether early symptoms of ADHD and DBDs in offspring of parents with BP are early indicators for BP, particularly if these symptoms are severe.80
The rates of substance abuse for all of the offspring groups were relatively low, but most of the youth had not yet reached the age of highest risk for substance abuse. Youth with BP appear to be at higher risk for developing substance abuse than youth with other psychopathology.81,82 Moreover, substance use may lower the threshold for BP.83 Thus, early detection and treatment of these children are warranted before they develop substance use or abuse.
Taken together, our findings from BIOS have several potential clinical implications. Clinicians who treat adults with BP should question those who are parents about their children's psychopathology to offer prompt identification and early interventions for any psychiatric problems that may be affecting the children's functioning, particularly early-onset BP. Some of the psychopathology presenting in offspring of parents with BP, particularly depression and anxiety, could be associated with the development of BP. However, it is not clear what the optimal treatment would be, given the possible risk of antidepressants inducing the onset of BP in these high-risk children. Also, clinicians who treat offspring of parents with BP should be alerted to parental psychopathology because as shown in this and other studies,1 their parents may have other comorbid disorders besides BP that could convey negative implications for the children's longitudinal outcomes. Effective treatment of these parents may diminish and perhaps prevent psychopathology in their children.84,85
Because nearly half of the offspring of parents with BP have not yet manifested any diagnosable psychiatric illness, there is a great need and opportunity for primary prevention in this high-risk population. Thus, it is critical to have prospective longitudinal studies of the offspring of parents with BP that include comparisons with offspring of parents with and without non-BP disorders to evaluate clinical and biological phenotypes and genetic polymorphisms that can help determine who is at risk to develop BP.
Acknowledgments
Funding/Support: This work was supported by grant MH60952 from the National Institute of Mental Health.
Footnotes
Financial Disclosure: Dr Birmaher has participated in forums sponsored by some pharmaceutical companies (Solvay, Abcomm, Inc, and Jazz Pharmaceuticals, Inc). Dr Kupfer has served on the advisory boards of Pfizer, Inc, Eli Lilly and Co, Forest Pharmaceuticals, Inc, F. Hoff-man-La Roche Ltd, and Solvay/Wyeth Pharmaceuticals and has been a consultant to Servier Amérique.
Publisher's Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
Additional Contributions: We dedicate this article to Editha Nottelmann, PhD, Chief, Affective and Regulatory Disorders Branch, Division of Developmental Translational Research, on her retirement from the National Institute of Mental Health. Her support, insight, and guidance played an important role in this study. Carol Kostek, BS, and Mary Kay Gill, MSN, provided assistance with manuscript preparation, University Center for Social and Urban Research staff and Amy Broz, AS, Jill Calkins, BA, Holly Donovan, BS, Elizabeth Picard, BS, Jeffrey Ryan, BA, and Lindsay Virgin, BA, were previous interviewers, and Scott Turkin, MD, and the Dubois Regional Medical Center Behavioral Health Services staff collaborated on this work.
REFERENCES
- 1.Goodwin FK, Jamison K. Manic-Depressive Illness: Bipolar Disorders and Recurrent Depression. 2nd ed. Oxford University Press; New York, NY: 2007. [Google Scholar]
- 2.Leboyer M, Henry C, Paillere-Martinot M-L, Bellivier F. Age at onset in bipolar affective disorders: a review. Bipolar Disord. 2005;7(2):111–118. doi: 10.1111/j.1399-5618.2005.00181.x. [DOI] [PubMed] [Google Scholar]
- 3.Pavuluri MN, Birmaher B, Naylor MW. Pediatric bipolar disorder: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2005;44(9):846–871. doi: 10.1097/01.chi.0000170554.23422.c1. [DOI] [PubMed] [Google Scholar]
- 4.Birmaher B, Axelson D, Pavaluri M. Bipolar disorder. In: Martin A, Volkmar FR, Lewis M, editors. Lewis's Child and Adolescent Psychiatry: A Comprehensive Textbook. 4th ed. Lippincott Williams & Wilkins; London, England: 2007. [Google Scholar]
- 5.Lapalme M, Hodgins S, LaRoche C. Children of parents with bipolar disorder: a metaanalysis of risk for mental disorders. Can J Psychiatry. 1997;42(6):623–631. doi: 10.1177/070674379704200609. [DOI] [PubMed] [Google Scholar]
- 6.McClellan J, Kowatch R, Findling RL. Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with bipolar disorder [published correction appears in J Am Acad Child Adolesc Psychiatry. 2007;46(6):786] J Am Acad Child Adolesc Psychiatry. 2007;46(1):107–125. doi: 10.1097/01.chi.0000242240.69678.c4. [DOI] [PubMed] [Google Scholar]
- 7.Axelson D, Birmaher B, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan N, Leonard H, Hunt J, Iyengar S, Bridge J, Keller M. Phenomenology of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006;63(10):1139–1148. doi: 10.1001/archpsyc.63.10.1139. [DOI] [PubMed] [Google Scholar]
- 8.Kowatch RA, Fristad M, Birmaher B, Wagner KD, Findling RL, Hellander M. Child Psychiatric Workgroup on Bipolar Disorder. Treatment guidelines for children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2005;44(3):213–235. doi: 10.1097/00004583-200503000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Duffy A, Alda M, Kutcher S, Cavazzoni P, Robertson C, Grof E, Grof P. A prospective study of the offspring of bipolar parents responsive and nonresponsive to lithium treatment. J Clin Psychiatry. 2002;63(12):1171–1178. doi: 10.4088/jcp.v63n1213. [DOI] [PubMed] [Google Scholar]
- 10.Chang KD, Steiner H, Ketter TA. Psychiatric phenomenology of child and adolescent bipolar offspring. J Am Acad Child Adolesc Psychiatry. 2000;39(4):453–460. doi: 10.1097/00004583-200004000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Henin A, Biederman J, Mick E, Sachs GS, Hirshfeld-Becker DR, Siegel RS, McMurrich S, Grandin L, Nierenberg AA. Psychopathology in the offspring of parents with bipolar disorder: a controlled study. Biol Psychiatry. 2005;58(7):554–561. doi: 10.1016/j.biopsych.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 12.Hillegers MH, Reichart CG, Wals M, Verhulst FC, Ormel J, Nolen WA. Five-year prospective outcome of psychopathology in the adolescent offspring of bipolar parents. Bipolar Disord. 2005;7(4):344–350. doi: 10.1111/j.1399-5618.2005.00215.x. [DOI] [PubMed] [Google Scholar]
- 13.Wals M, Hillegers MH, Reichart CG, Ormel J, Nolen WA, Verhulst FC. Prevalence of psychopathology in children of a bipolar parent. J Am Acad Child Adolesc Psychiatry. 2001;40(9):1094–1102. doi: 10.1097/00004583-200109000-00019. [DOI] [PubMed] [Google Scholar]
- 14.Hirshfeld-Becker DR, Biederman J, Henin A, Faraone SV, Dowd ST, De Petrillo LA, Markowitz SM, Rosenbaum JF. Psychopathology in the young offspring of parents with bipolar disorder: a controlled pilot study. Psychiatry Res. 2006;145(23):155–167. doi: 10.1016/j.psychres.2005.08.026. [DOI] [PubMed] [Google Scholar]
- 15.Singh MK, DelBello MP, Stanford KE, Soutullo C, McDonough-Ryan P, McElroy SL, Strakowski SM. Psychopathology in children of bipolar parents. J Affect Disord. 2007;102(13):131–136. doi: 10.1016/j.jad.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 16.DelBello MP, Geller B. Review of studies of child and adolescent offspring of bipolar parents. Bipolar Disord. 2001;3(6):325–334. doi: 10.1034/j.1399-5618.2001.30607.x. [DOI] [PubMed] [Google Scholar]
- 17.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- 18.Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID), I: history, rationale, and description. Arch Gen Psychiatry. 1992;49(8):624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 19.Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 20.Andreasen NC, Endicott J, Spitzer RL, Winokur G. The family history method using diagnostic criteria: reliability and validity. Arch Gen Psychiatry. 1977;34(10):1229–1235. doi: 10.1001/archpsyc.1977.01770220111013. [DOI] [PubMed] [Google Scholar]
- 21.Axelson D, Birmaher BJ, Brent D, Wassick S, Hoover C, Bridge J, Ryan N. A preliminary study of the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children mania rating scale for children and adolescents. J Child Adolesc Psychopharmacol. 2003;13(4):463–470. doi: 10.1089/104454603322724850. [DOI] [PubMed] [Google Scholar]
- 22.Frazier TW, Demeter CA, Youngstrom EA, Calabrese JR, Stansbrey RJ, McNamara NK, Findling RL. Evaluation and comparison of psychometric instruments for pediatric bipolar spectrum disorders in four age groups. J Child Adolesc Psychopharmacol. 2007;17(6):853–866. doi: 10.1089/cap.2007.0057. [DOI] [PubMed] [Google Scholar]
- 23.Birmaher B, Axelson D, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan N, Leonard H, Hunt J, Iyengar S, Keller M. Clinical course of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006;63(2):175–183. doi: 10.1001/archpsyc.63.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leibenluft E, Rich BA. Pediatric bipolar disorder. Annu Rev Clin Psychol. 2008;4:163–187. doi: 10.1146/annurev.clinpsy.4.022007.141216. [DOI] [PubMed] [Google Scholar]
- 25.Leckman JF, Sholomskas D, Thompson WD, Belanger A, Weissman MM. Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch Gen Psychiatry. 1982;39(8):879–883. doi: 10.1001/archpsyc.1982.04290080001001. [DOI] [PubMed] [Google Scholar]
- 26.Petersen AC, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: reliability, validity, and initial norms. J Youth Adolesc. 1988;17(2):117–133. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- 27.Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969;44(235):291–303. doi: 10.1136/adc.44.235.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in boys. Arch Dis Child. 1970;45(239):13–23. doi: 10.1136/adc.45.239.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hollingshead AB. Index of social status. In: Mangen DJ, Peterson WA, editors. Research Instruments in Social Gerontology, Vol 2: Social Roles and Social Participation. University of Minnesota Press; Minneapolis: 1982. [Google Scholar]
- 30.Hedeker D. MIXNO: a computer program for mixed-effects nominal logistic regression. J Stat Softw. 1999;4(5):1–92. [Google Scholar]
- 31.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. [Google Scholar]
- 32.Rice JP, McDonald-Scott P, Endicott J, Coryell W, Grove WM, Keller MB, Altis D. The stability of diagnosis with an application to bipolar II disorder. Psychiatry Res. 1986;19(4):285–296. doi: 10.1016/0165-1781(86)90121-6. [DOI] [PubMed] [Google Scholar]
- 33.Kessler RC, Merikangas KR, Wang PS. Prevalence, comorbidity, and service utilization for mood disorders in the United States at the beginning of the twenty-first century. Annu Rev Clin Psychol. 2007;3:137–158. doi: 10.1146/annurev.clinpsy.3.022806.091444. [DOI] [PubMed] [Google Scholar]
- 34.Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, Kessler RC. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication [published correction appears in Arch Gen Psychiatry. 2007;64(9):1039] Arch Gen Psychiatry. 2007;64(5):543–552. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Angold A, Weissman MM, John K, Merikangas KR, Prusoff BA, Wickramaratne P, Gammon GD, Warner V. Parent and child reports of depressive symptoms in children at low and high risk of depression. J Child Psychol Psychiatry. 1987;28(6):901–915. doi: 10.1111/j.1469-7610.1987.tb00678.x. [DOI] [PubMed] [Google Scholar]
- 36.Kiss E, Gentzler AM, George C, Kapornai K, Tamás Z, Kovacs M, Vetró A. Factors influencing mother-child reports of depressive symptoms and agreement among clinically referred depressed youngsters in Hungary. J Affect Disord. 2007;100(13):143–151. doi: 10.1016/j.jad.2006.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Najman JM, Williams GM, Nikles J, Spence S, Bor W, O'Callaghan M, Le Brocque R, Andersen MJ. Mothers' mental illness and child behavior problems: cause-effect association or observation bias? J Am Acad Child Adolesc Psychiatry. 2000;39(5):592–602. doi: 10.1097/00004583-200005000-00013. [DOI] [PubMed] [Google Scholar]
- 38.Youngstrom E, Loeber R, Stouthamer-Loeber M. Patterns and correlates of agreement between parent, teacher, and male adolescent ratings of externalizing and internalizing problems. J Consult Clin Psychol. 2000;68(6):1038–1050. doi: 10.1037//0022-006x.68.6.1038. [DOI] [PubMed] [Google Scholar]
- 39.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60(8):837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 40.Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorder during adolescence and young adulthood in a community sample. Bipolar Disord. 2000;2(3 pt 2):281–293. doi: 10.1034/j.1399-5618.2000.20309.x. [DOI] [PubMed] [Google Scholar]
- 41.Weissman MM, Gammon GD, John K, Merikangas KR, Warner V, Prusoff BA, Sholomskas D. Children of depressed parents: increased psychopathology and early onset of major depression. Arch Gen Psychiatry. 1987;44(10):847–853. doi: 10.1001/archpsyc.1987.01800220009002. [DOI] [PubMed] [Google Scholar]
- 42.Low NC, Cui L, Merikangas KR. Community vs clinic sampling: effect on the familial aggregation of anxiety disorders. Biol Psychiatry. 2008;63(9):884–890. doi: 10.1016/j.biopsych.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 43.Goldstein RB, Weissman MM, Adams PB, Horwath E, Lish JD, Charney D, Woods SW, Sobin C, Wickramaratne PJ. Psychiatric disorders in relatives of probands with panic disorder and/or major depression. Arch Gen Psychiatry. 1994;51(5):383–394. doi: 10.1001/archpsyc.1994.03950050043005. [DOI] [PubMed] [Google Scholar]
- 44.Kessler RC, Rubinow DR, Holmes C, Abelson JM, Zhao S. The epidemiology of DSM-III-R bipolar I disorder in a general population survey. Psychol Med. 1997;27(5):1079–1089. doi: 10.1017/s0033291797005333. [DOI] [PubMed] [Google Scholar]
- 45.Perlis RH, Miyahara S, Marangell LB, Wisniewski SR, Ostacher M, DelBello MP, Bowden CL, Sachs GS, Nierenberg AA. STEP-BD Investigators. Long-term implications of early onset in bipolar disorder: data from the first 1000 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD) Biol Psychiatry. 2004;55(9):875–881. doi: 10.1016/j.biopsych.2004.01.022. [DOI] [PubMed] [Google Scholar]
- 46.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication [published correction appears in Arch Gen Psychiatry. 2005;62(7):768] Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 47.Neuman RJ, Geller B, Rice JP, Todd RD. Increased prevalence and earlier onset of mood disorders among relatives of prepubertal vs adult probands. J Am Acad Child Adolesc Psychiatry. 1997;36(4):466–473. doi: 10.1097/00004583-199704000-00008. [DOI] [PubMed] [Google Scholar]
- 48.Kutcher S, Marton P. Affective disorders in first-degree relatives of adolescent onset bipolars, unipolars, and normal controls. J Am Acad Child Adolesc Psychiatry. 1991;30(1):75–78. doi: 10.1097/00004583-199101000-00011. [DOI] [PubMed] [Google Scholar]
- 49.Wozniak J, Biederman J, Mundy E, Mennin D, Faraone SV. A pilot family study of childhood-onset mania. J Am Acad Child Adolesc Psychiatry. 1995;34(12):1577–1583. doi: 10.1097/00004583-199512000-00007. [DOI] [PubMed] [Google Scholar]
- 50.Geller B, Tillman R, Bolhofner K, Zimerman B, Strauss NA, Kaufmann P. Controlled, blindly rated, direct-interview family study of a prepubertal and early-adolescent bipolar I disorder phenotype: morbid risk, age at onset, and comorbidity. Arch Gen Psychiatry. 2006;63(10):1130–1138. doi: 10.1001/archpsyc.63.10.1130. [DOI] [PubMed] [Google Scholar]
- 51.Strober M, Morrell W, Burroughs J, Lampert C, Danforth H, Freeman R. A family study of bipolar I disorder in adolescence: early onset of symptoms linked to increased familial loading and lithium resistance. J Affect Disord. 1988;15(3):255–268. doi: 10.1016/0165-0327(88)90023-7. [DOI] [PubMed] [Google Scholar]
- 52.Chengappa KN, Kupfer DJ, Frank E, Houck PR, Grochocinski VJ, Cluss PA, Stapf DA. Relationship of birth cohort and early age at onset of illness in a bipolar disorder case registry. Am J Psychiatry. 2003;160(9):1636–1642. doi: 10.1176/appi.ajp.160.9.1636. [DOI] [PubMed] [Google Scholar]
- 53.Lish JD, Dime-Meenan S, Whybrow PC, Price RA, Hirschfeld RM. The National Depressive and Manic-depressive Association (DMDA) survey of bipolar members. J Affect Disord. 1994;31(4):281–294. doi: 10.1016/0165-0327(94)90104-x. [DOI] [PubMed] [Google Scholar]
- 54.Kraepelin E. Manic Depressive Insanity and Paranoia. E & S Livingstone; London, England: 1921. [Google Scholar]
- 55.O'Donovan M, Jones I, Craddock N. Anticipation and repeat expansion in bipolar disorder. Am J Med Genet C Semin Med Genet. 2003;123C(1):10–17. doi: 10.1002/ajmg.c.20009. [DOI] [PubMed] [Google Scholar]
- 56.Chang K, Steiner H, Ketter T. Studies of offspring of parents with bipolar disorder. Am J Med Genet C Semin Med Genet. 2003;1;123C:26–35. doi: 10.1002/ajmg.c.20011. [DOI] [PubMed] [Google Scholar]
- 57.Brotman MA, Kassem L, Reising MM, Guyer AE, Dickstein DP, Rich BA, Towbin KE, Pine DS, McMahon FJ, Leibenluft E. Parental diagnoses in youth with narrow phenotype bipolar disorder or severe mood dysregulation. Am J Psychiatry. 2007;164(8):1238–1241. doi: 10.1176/appi.ajp.2007.06101619. [DOI] [PubMed] [Google Scholar]
- 58.Costello EJ, Pine DS, Hammen C, March JS, Plotsky PM, Weissman MM, Biederman J, Goldsmith HH, Kaufman J, Lewinsohn PM, Hellander M, Hoagwood K, Koretz DS, Nelson CA, Leckman JF. Development and natural history of mood disorders. Biol Psychiatry. 2002;52(6):529–542. doi: 10.1016/s0006-3223(02)01372-0. [DOI] [PubMed] [Google Scholar]
- 59.Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Natural course of adolescent major depressive disorder in a community sample: predictors of recurrence in young adults. Am J Psychiatry. 2000;157(10):1584–1591. doi: 10.1176/appi.ajp.157.10.1584. [DOI] [PubMed] [Google Scholar]
- 60.DelBello MP, Hanseman D, Adler CM, Fleck DE, Strakowski SM. Twelve-month outcome of adolescents with bipolar disorder following first hospitalization for a manic or mixed episode. Am J Psychiatry. 2007;164(4):582–590. doi: 10.1176/ajp.2007.164.4.582. [DOI] [PubMed] [Google Scholar]
- 61.Strober M, Carlson G. Bipolar illness in adolescents with major depression: clinical, genetic, and psychopharmacologic predictors in a three- to four-year prospective follow-up investigation. Arch Gen Psychiatry. 1982;39(5):549–555. doi: 10.1001/archpsyc.1982.04290050029007. [DOI] [PubMed] [Google Scholar]
- 62.Strober M, Lampert C, Schmidt S, Morrell W. The course of major depressive disorder in adolescents, I: recovery and risk of manic switching in a follow-up of psychotic and nonpsychotic subtypes. J Am Acad Child Adolesc Psychiatry. 1993;32(1):34–42. doi: 10.1097/00004583-199301000-00006. [DOI] [PubMed] [Google Scholar]
- 63.Geller B, Zimerman B, Williams M, Bolhofner K, Craney JL. Adult psychosocial outcome of prepubertal major depressive disorder. J Am Acad Child Adolesc Psychiatry. 2001;40(6):673–677. doi: 10.1097/00004583-200106000-00012. [DOI] [PubMed] [Google Scholar]
- 64.Kovacs M. Presentation and course of major depressive disorder during childhood and later years of the life span. J Am Acad Child Adolesc Psychiatry. 1996;35(6):705–715. doi: 10.1097/00004583-199606000-00010. [DOI] [PubMed] [Google Scholar]
- 65.Geller B, Fox LW, Clark KA. Rate and predictors of prepubertal bipolarity during follow-up of 6- to 12-year-old depressed children. J Am Acad Child Adolesc Psychiatry. 1994;33(4):461–468. doi: 10.1097/00004583-199405000-00003. [DOI] [PubMed] [Google Scholar]
- 66.Akiskal HS. Developmental pathways to bipolarity: are juvenile-onset depressions pre-bipolar? J Am Acad Child Adolesc Psychiatry. 1995;34(6):754–763. doi: 10.1097/00004583-199506000-00016. [DOI] [PubMed] [Google Scholar]
- 67.Biederman J, Faraone SV, Marrs A, Moore P, Garcia J, Ablon S, Mick E, Gershon J, Kearns ME. Panic disorder and agoraphobia in consecutively referred children and adolescents. J Am Acad Child Adolesc Psychiatry. 1997;36(2):214–223. doi: 10.1097/00004583-199702000-00012. [DOI] [PubMed] [Google Scholar]
- 68.Birmaher B, Kennah A, Brent D, Ehmann M, Bridge J, Axelson D. Is bipolar disorder specifically associated with panic disorder in youths? J Clin Psychiatry. 2002;63(5):414–419. doi: 10.4088/jcp.v63n0507. [DOI] [PubMed] [Google Scholar]
- 69.Kowatch RA, Youngstrom EA, Danielyan A, Findling RL. Review and meta-analysis of the phenomenology and clinical characteristics of mania in children and adolescents. Bipolar Disord. 2005;7(6):483–496. doi: 10.1111/j.1399-5618.2005.00261.x. [DOI] [PubMed] [Google Scholar]
- 70.Frank E, Cyranowski JM, Rucci P, Shear MK, Fagiolini A, Thase ME, Cassano GB, Grochocinski VJ, Kostelnik B, Kupfer DJ. Clinical significance of lifetime panic spectrum symptoms in the treatment of patients with bipolar I disorder. Arch Gen Psychiatry. 2002;59(10):905–911. doi: 10.1001/archpsyc.59.10.905. [DOI] [PubMed] [Google Scholar]
- 71.Henry C, Van den Bulke D, Bellivier F, Etain B, Rouillon F, Leboyer M. Anxiety disorders in 318 bipolar patients: prevalence and impact on illness severity and response to mood stabilizer. J Clin Psychiatry. 2003;64(3):331–335. [PubMed] [Google Scholar]
- 72.Dickstein DP, Rich BA, Binstock AB, Pradella AG, Towbin KE, Pine DS, Leibenluft E. Comorbid anxiety in phenotypes of pediatric bipolar disorder. J Child Adolesc Psychopharmacol. 2005;15(4):534–548. doi: 10.1089/cap.2005.15.534. [DOI] [PubMed] [Google Scholar]
- 73.Goldstein BI, Levitt AJ. Prevalence and correlates of bipolar I disorder among adults with primary youth-onset anxiety disorders. J Affect Disord. 2007;103(13):187–195. doi: 10.1016/j.jad.2007.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry. 2003;60(7):709–717. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- 75.Johnson JG, Cohen P, Brook JS. Associations between bipolar disorder and other psychiatric disorders during adolescence and early adulthood: a community-based longitudinal investigation. Am J Psychiatry. 2000;157(10):1679–1681. doi: 10.1176/appi.ajp.157.10.1679. [DOI] [PubMed] [Google Scholar]
- 76.Kovacs M, Pollock M. Bipolar disorder and comorbid conduct disorder in childhood and adolescence. J Am Acad Child Adolesc Psychiatry. 1995;34(6):715–723. doi: 10.1097/00004583-199506000-00011. [DOI] [PubMed] [Google Scholar]
- 77.Tillman R, Geller B, Bolhofner K, Craney JL, Williams M, Zimerman B. Ages of onset and rates of syndromal and subsyndromal comorbid DSM-IV diagnoses in a prepubertal and early adolescent bipolar disorder phenotype. J Am Acad Child Adolesc Psychiatry. 2003;42(12):1486–1493. doi: 10.1097/00004583-200312000-00016. [DOI] [PubMed] [Google Scholar]
- 78.Biederman J, Faraone SV, Milberger S, Jetton JG, Chen L, Mick E, Greene RW, Russell RL. Is childhood oppositional defiant disorder a precursor to adolescent conduct disorder? findings from a four-year follow-up study of children with ADHD. J Am Acad Child Adolesc Psychiatry. 1996;35(9):1193–1204. doi: 10.1097/00004583-199609000-00017. [DOI] [PubMed] [Google Scholar]
- 79.Costello EJ, Compton SN, Keeler G, Angold A. Relationships between poverty and psychopathology: a natural experiment. JAMA. 2003;290(15):2023–2029. doi: 10.1001/jama.290.15.2023. [DOI] [PubMed] [Google Scholar]
- 80.Biederman J, Faraone SV, Wozniak J, Mick E, Kwon A, Aleardi M. Further evidence of unique developmental phenotypic correlates of pediatric bipolar disorder: findings from a large sample of clinically referred preadolescent children assessed over the last 7 years. J Affect Disord. 2004;82(suppl 1):S45–S58. doi: 10.1016/j.jad.2004.05.021. [DOI] [PubMed] [Google Scholar]
- 81.Wilens TE, Biederman J, Millstein RB, Wozniak J, Hahesy AL, Spencer TJ. Risk for substance use disorders in youths with child- and adolescent-onset bipolar disorder. J Am Acad Child Adolesc Psychiatry. 1999;38(6):680–685. doi: 10.1097/00004583-199906000-00014. [DOI] [PubMed] [Google Scholar]
- 82.Goldstein BI, Strober MA, Birmaher B, Axelson DA, Esposito-Smythers C, Goldstein TR, Leonard H, Hunt J, Gill MK, Iyengar S, Grimm C, Yang M, Ryan ND, Keller MB. Substance use disorders among adolescents with bipolar spectrum disorders. Bipolar Disord. 2008;10(4):469–478. doi: 10.1111/j.1399-5618.2008.00584.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Winokur G, Coryell W, Akiskal HS, Maser JD, Keller MB, Endicott J, Mueller T. Alcoholism in manic-depressive (bipolar) illness: familial illness, course of illness, and the primary-secondary distinction [published correction appears in Am J Psychiatry. 1995;152(7):1106] Am J Psychiatry. 1995;152(3):365–372. doi: 10.1176/ajp.152.3.365. [DOI] [PubMed] [Google Scholar]
- 84.Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, Hughes CW, Garber J, Malloy E, King CA, Cerda G, Sood AB, Alpert JE, Trivedi MH, Rush AJ. STAR*D-Child Team. Remissions in maternal depression and child psychopathology: a STAR*D-child report. JAMA. 2006;295(12):1389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- 85.Beardslee WR, Bemporad J, Keller MB, Klerman GL. Children of parents with major affective disorder: a review. Am J Psychiatry. 1983;140(7):825–832. doi: 10.1176/ajp.140.7.825. [DOI] [PubMed] [Google Scholar]