Abstract
Chronic disease (care) management (CDM) is a patient-centered model of care that involves longitudinal care delivery; integrated, and coordinated primary medical and specialty care; patient and clinician education; explicit evidence-based care plans; and expert care availability. The model, incorporating mental health and specialty addiction care, holds promise for improving care for patients with substance dependence who often receive no care or fragmented ineffective care. We describe a CDM model for substance dependence and discuss a conceptual framework, the extensive current evidence for component elements, and a promising strategy to reorganize primary and specialty health care to facilitate access for people with substance dependence. The CDM model goes beyond integrated case management by a professional, colocation of services, and integrated medical and addiction care—elements that individually can improve outcomes. Supporting evidence is presented that: 1) substance dependence is a chronic disease requiring longitudinal care, although most patients with addictions receive no treatment (eg, detoxification only) or short-term interventions, and 2) for other chronic diseases requiring longitudinal care (eg, diabetes, congestive heart failure), CDM has been proven effective.
Keywords: chronic disease management, addiction, primary care, linkage, addiction treatment, chronic care model, recovery
Substance (alcohol and drug) dependence is a chronic disease for which many affected adults receive no intervention or detoxification without subsequent treatment. Like other chronic diseases (eg, diabetes, congestive heart failure), substance dependence has no cure and is characterized by relapses requiring longitudinal care. Medical and psychiatric comorbidities are the rule rather than the exception. As a result, care delivery can be complex both for clinicians and patients. In the United States, systems of care for substance dependence (both alcohol and drug) are rarely integrated with those for medical and psychiatric illnesses. Specialty alcohol and drug treatment is efficacious, but many patients do not access available treatment for substance dependence problems after detoxification or medical care. Others enter specialty addiction treatment but do not receive medical or psychiatric care. Some have called to expand the frame of health services research on addictions to include services outside the specialty treatment sector, including behavioral care integrated into primary care.1-3
Although primary care settings provide the venue for longitudinal, comprehensive, and coordinated care, their potential to effectively treat addiction and related comorbidities has not been realized; medical, mental health, and addiction treatment are not coordinated. Primary care settings, with reorganization and appropriate service elements, hold the promise of simultaneously improving physical and psychiatric health while decreasing substance dependence problems. Although chronic disease management—longitudinal care delivery linking, integrating, and coordinating primary and specialty health care—is effective for other diseases, it has not been described or studied for substance dependence.
CHRONIC DISEASE (CARE) MANAGEMENT
Chronic disease (care) management (CDM) is based on a chronic care model, as described by Wagner et al.4-6 Chronic disease (care) management is a patient-centered model of care, which includes patient and clinician education, explicit evidence-based care plans, and expert care availability (Table 1). In using the term “disease management,” this article is about health services based on Wagner’s model and not about corporate programs that focus primarily on patient self-care and are implemented via telephonic contacts.7
TABLE 1.
Chronic Disease Management (CDM) Conceptual Elements and Potential Elements for Implementation
| CDM Conceptual Element | Potential Implementation Elements |
|---|---|
| Community resources | Case management; address social, legal, financial needs |
| Chronic disease as priority | Focus on substance dependence as a chronic illness; explicit care plans |
| Self-management support | Routine assessment and feedback; patient participation (collaborative care); behavior change; psychosocial support |
| Delivery system design | On-site service delivery (integrated and coordinatedcare); referral agreements; planned visits; use of nonphysicians in multidisciplinary team; patient reminders; collaboration of addiction, medical and psychiatric physicians |
| Decision support | Specialty expertise made accessible |
| Clinical information systems | Electronic medical record; patient registry; monitoring of outcomes |
CDM CONCEPTUAL FRAMEWORK
Many, including the Institute of Medicine (IOM), have recognized the challenge of managing chronic conditions in a health care system designed to treat acute illness.8 In 1996, Wagner et al. proposed a solution—CDM4-6—based on a chronic care model. Chronic disease management is implemented by the following multidisciplinary team members: nurse clinical care managers with disease-specific skills to coordinate referrals, communicate with clinical caregivers, and proactively follow patients; social workers to access community resources; and physician specialists. The U.S. Center for Medicare and Medicaid Services (CMS) and the National Committee for Quality Assurance (NCQA) have recognized the potential of CDM.9-11 Policy analysts have called for CDM to be integrated into primary care settings to avoid fragmented care.12-15
We argue that chronic disease management could be applied to addiction for patients in the primary care setting, particularly those who are out-of-treatment.6 Of U.S. adults, 23 million have substance dependence, costing society almost $300 billion each year, yet 90% of people with addictions are out-of-treatment because of individual barriers and a fragmented treatment system.16-23 Thus, although addictions treatment is effective and reduces health care costs, its benefits are largely unrealized.
In addition to the chronic care model, 2 additional conceptual models support the categories and elements specified in a CDM approach applied to addictions: D’Aunno24 and others’ integrative linkages of health services, and Andersen’s25 behavioral model of health services utilization. D’Aunno and others have proposed that stronger linkages between care systems and clinicians (eg, case management [CM]), “colocated” services, more formal referral arrangements) can increase the likelihood of addictions treatment entry and completion.24 Specialty substance dependence treatment reduces the risk for relapse. Medical and psychosocial services can help to prevent relapse and can help decrease barriers to substance dependence treatment, but patients face substantial systemic and personal barriers to receiving these services, as well as in accessing addiction specialty treatment (eg, insurance problems, personal disorganization, care systems focused on patients with one problem, privacy issues, bureaucracy, motivation).26 Integrative linkages can align these services. Stronger linkage mechanisms increase the probability that patients will obtain needed services. The strongest linkage mechanism is on-site service delivery. To go beyond this structural solution, we conceptualize integrated, professionally delivered case management as a key component of CDM and as a health system-enabling resource as described in Andersen’s model.25 This resource helps the patient to increase recognition of needs (eg, substance dependence treatment, attention to medical and psychosocial needs) and to improve the use of health services (“effective access”) that improve health status. Friedmann et al.27,28 reported that drug use decreased among addiction treatment patients who had comprehensive services matched with identified needs. Thus, effective matching of service to need, one goal of CDM, can be a useful addiction treatment practice. In addition to these common elements that address systems issues and health and social problems, CDM tailored for addiction would include individual addiction-specific interventions. These elements are chosen based on their proven efficacy, their appropriateness for patients who have not entered treatment, their compatibility with health care organization theories, and primary care setting constraints. These addiction treatment components are each supported by their own theoretical frameworks: motivational interviewing by theories of behavior change29,30; case management by therapeutic alliance and enhancing receipt of needed services31,32; medication by theories of neuronal receptor involvement in alcohol and drug dependence33,34; complete health (medical, psychologic, social) and needs assessment, feedback, and advice delivered by an empathic clinician by the biopsychosocial model of addictions requiring pharmacotherapy, psychosocial support and services35; management of detoxification to avoid substance use to relieve withdrawal symptoms36,37; and relapse prevention in primary care.38,39 Based on recent outcomes research, CDM for substance dependence could base recommendations for self-help involvement on an egalitarian model (offer to all regardless of individual need factors) and a need-based model for additional services.40
Finally, researchers have made a case for extended recovery monitoring interventions for alcohol and drug disorders.41 In a randomized trial of patients with alcohol or cocaine dependence, 3 months of weekly telephone monitoring was added to group counseling sessions started after completion of intensive outpatient treatment. Total abstinence was more common 2 years later in the telephone monitoring group.41 Similarly, other researchers have noted benefits from “recovery management check-ups.”42
APPLICATION OF CDM TO ADDICTIONS
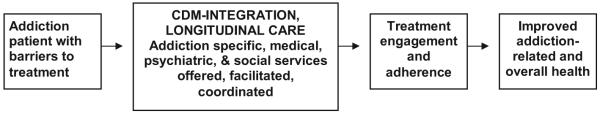
Wagner and colleagues proposed the chronic care model and the elements of effective chronic disease management (Table 1).4-6,43,44 How should these elements work if applied to addiction care? As shown in Figure 1, in CDM, clinicians are expert, identify problems (disease of interest as well as medical, social, emotional), share information with patients and teach problem solving skills. Patients identify problems, set goals, and change behavior based on internal motivation. Multidisciplinary teams, including a nurse care manager, social worker and clinicians with expertise in the disease of interest, and expertise in common comorbidities, can spend time with the patient, coordinate with primary care physicians (PCPs), address necessary releases of information, and facilitate specialist referrals, provide access to community resources, implement evidence-based protocols, encourage self-management, and be proactive about follow-up. Information can be shared across team members, primary care clinicians, and specialists by using electronic records creating virtual colocation of care even when clinicians are in separate physical locations. This same information, when aggregated in a registry, can support the attention of the team to individual patients who have not received needed care and to clinical outcomes. In sum, an informed, motivated patient and a prepared, proactive team and delivery system lead to optimal chronic disease care and improved outcomes.
FIGURE 1.
How chronic disease management (CDM) can improve health for people with addiction.
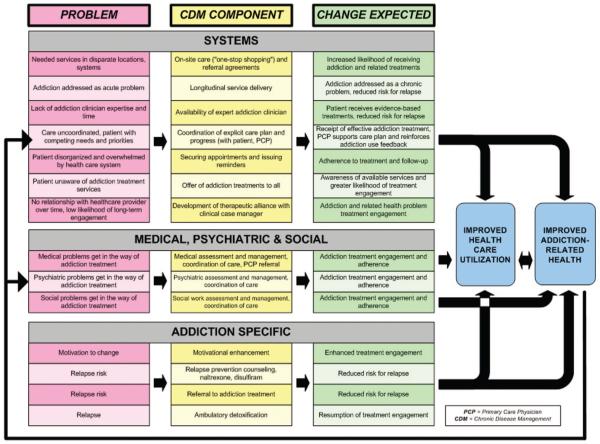
How could CDM elements be implemented in primary care for addiction? Figure 2 categorizes the specific elements of a proposed CDM intervention for substance (alcohol or drug) dependence into 3 areas: systems; medical, psychiatric and social problems; and addiction specific components and related outcomes. The systems changes follow directly from the elements in Table 1.
FIGURE 2.
How chronic disease management (CDM) components address specific problems to lead to improved health.
This approach is needed in part because of the current fragmentation of the treatment system, a system that only infrequently incorporates efficacious treatment elements. Although addiction treatment services often exist, and may be available in the sense that services are covered by insurance or grant funded, many barriers still prevent most patients from accessing these services. In fact, specialty services are not truly accessible at the time or in the settings in which patients are present. Chronic disease management, involving strong linkages within and between systems of care, integrated case management, and known effective addictions treatment components delivered under one roof, is hypothesized to increase the likelihood that patients will access and receive effective treatment for substance dependence problems, re-engage in care when they drop out, improve utilization of medical and other health services, and be less likely to suffer consequences of alcohol and drug use. These hypotheses are based on a careful review of the literature that we present in the section that follows regarding the chronic nature of addiction, fragmentation of care, suboptimal access to effective addiction care, and evidence for the individual components of the proposed CDM model.
ADDICTION: A CHRONIC DISEASE WITH PSYCHIATRIC AND MEDICAL COMORBIDITY
Whereas current care utilization is episodic (ie, detoxification only), the course of substance dependence often is chronic, particularly in people who seek and receive treatment. In a population-based sample, not a treatment sample, the mean duration of an episode of alcohol dependence was 3.7 years, and 28% of people had more than 1 episode (average, 5 episodes).45 As with chronic medical illnesses, addiction is associated with chronic physiologic changes, a relapsing course, no “cure,” variable adherence to care, and the need for ongoing care.46,47 In addition to social, legal and family consequences, medical, and psychiatric disorders (eg, depression) are common (ie, 30-50%) and can be triggers for relapse.38,48-54 When patients seek care for substance dependence, they are more likely than others to have myriad conditions: injury/overdose, anxiety, depression, psychosis, low back pain, headache, arthritis, asthma, acid-related peptic disorders, chronic obstructive pulmonary disease, hepatitis C, hypertension, alcoholic gastritis, diseases of the pancreas, and cirrhosis.55,56 Because addiction can decrease medication adherence and other self-care, the care of these other medical and psychiatric conditions becomes more complex.57
FRAGMENTED ADDICTION TREATMENT
Elements of the proposed model of CDM provide strategies to reduce entry barriers to effective addiction treatment and to promote continuous patient engagement in some level of care. The current treatment system is fragmented among acute medical and specialty alcohol and drug services with little coordination.58-60 Furthermore, few patients in recovery report having ever had formal treatment61 and only 18% of adults with addiction report seeking mental health or addictions treatment annually.19 Detoxification is a possible entry point to the treatment system but the missing linkage from detoxification, not a treatment itself, to treatment is recognized at the national level.62 Privacy protection may interfere with coordinating linkage between treatment systems. However, the period after detoxification is a time of crisis during which mortality is substantial.63 Barriers to treatment entry and continuous care include patient, treatment program, and systems factors. True accessibility64 or “effective access”25 is frequently missing, and only half of individuals entering treatment complete care episodes even though current programs are generally short-term.65 Low rates occur despite the fact that financial barriers may be low, addiction treatment often is available without health insurance,66 and persons with addictions generally live close to treatment programs, an average of 3.2 miles, although this availability is not consistent.67 The treatment system may not be offering what the patient wants or can use. Patient factors include motivation, employment issues, attitudes, and beliefs,68-71 and other comorbid medical and psychiatric problems can interfere with access to care. For example, a treatment program may preclude patients from concomitant use of psychiatric medication. These barriers can make “usual care,” effectively no care, or, at best, suboptimal care for alcohol and drug dependence. Elements of CDM have the potential to address many of these barriers (Table 1; Figs. 1 and 2).
UNDERUTILIZED EFFICACIOUS TREATMENTS
Case management, pharmacotherapy (eg, naltrexone and buprenorphine), brief interventions, social skills training, community reinforcement approaches, behavior contracting, motivational interviewing, motivational incentives, and marital therapy are effective treatment elements that are currently underutilized for which use could be increased by CDM.52,72-80 Pharmacological treatments are underused in the addiction system, which emerged outside of medical care settings. The orientation of the system is toward short-term interventions.81 Treatment philosophy, particularly 12-step orientation, may run counter to any psychotropic drug use.82,83 Health professionals have varied medical skills and qualifications (eg, ability to prescribe or administer medication84), and many lack both familiarity with addiction medications and ancillary support for its management.85 Nevertheless, new interventions for addiction treatment particularly well suited to medical settings include “medical management” as tested in the COMBINE study86 and used in the BRENDA (Biopsychosocial evaluation, Report, Empathy, Needs, Direct advice, Assessment) approach. BRENDA has primarily been used to support pharmacotherapy of alcoholism. Although not yet tested in a randomized trial nor used for patients with drug dependence, controlled studies have found use of BRENDA to be associated with improved medication adherence, retention in treatment, and improved clinical outcomes.35,87,88 Preliminary data from primary care studies suggest that training to use such guidelines leads to clinician-based discussions about relapse risk.38,89
INSUFFICIENT LINKAGE OF ADDICTION TREATMENT AND PRIMARY MEDICAL CARE
Options for linkage of addiction and primary medical care treatment have primarily included distributive approaches, in which patients in one system are referred to another resulting in tenuous links.59 Few patients with addictions access medical care and informal referrals from addictions treatment do not increase access.24,90 Conversely, patients in medical settings are often not identified or referred to addiction treatment.91-93 In 1991, a Federal conference concluded that better linkage should be pursued by colocating services and improving the effectiveness of referrals.94 This conclusion remains relevant today.
A parallel problem exists for primary care providers accessing mental health services, an element of care also in short supply and often comorbid with substance dependence.92,95 Primary care physicians have been challenged to play a larger role in addressing patients’ mental health needs.96-100 Some clinical models use a mental health team in the primary care clinic to rapidly evaluate and stabilize patients, and educate the primary care clinical staff.99,100 In these integrated approaches receipt of mental health services increase, referrals decrease, patients benefit by continuing to be treated by their primary care physicians, and physicians benefit from additional support and training from mental health professionals. A quality improvement initiative for depression care management in primary care practices enhanced effectiveness and outcomes, leading an editorialist to conclude that “Evidence that depression outcomes can be improved through systematic changes in delivery of care is now compelling.”101,102 In another model, a Veterans Affairs mental health clinic103 successfully integrated medical care emphasizing preventive measures, patient education, and close collaboration with mental health providers and patients had significant improvements in quality and outcomes of medical care. Mechanic104 notes that although few systems successfully integrate care at the clinical level, simply having a clinician meet a community provider to whom patients with schizophrenia would be linked improved continuity of care and symptom improvement.105 These mental health studies demonstrate the importance of discrete systemic innovations to improve access and clinical and utilization outcomes. Thus, although interorganizational integration and coordination of care has been difficult to achieve, when achieved, outcomes are improved.106-108
Intraorganizational interventions, such as CDM, have been proven feasible and effective and form the basis of the proposed model of CDM for addictions. Chronic disease management improves patient adherence to treatments and disease control compared with usual care and relies on patient education and reminders, and clinician education and feedback.109-111 Compared with usual care, CDM interventions focus on a disease but attend to comorbidity. A major strength and promise of such interventions is improvement in the disease of focus as well as comorbidities.101-103,112-115
Although no trials of CDM for addiction appear in the literature, systematic reviews have identified numerous controlled studies of CDM for psychiatric illnesses and inform the choice of effective elements for addictions. For example, a large randomized trial of a depression CDM intervention found that CDM patients were more likely to receive depression treatments and have a significant reduction in depressive symptoms and functional impairment116 and improved arthritis pain and functional outcomes.117 In this CDM intervention, patients received a 20-minute educational video and booklet about depression, a visit with a trained depression nurse or psychologist care manager in primary care, underwent medical and psychosocial assessment, and were asked about their treatment preferences. The team suggested antidepressant medication (80% had 1 trial of medication) or brief psychotherapy adapted for the primary care setting delivered by the case manager (30% received this counseling). Thus, the team offered services tailored to patients’ needs and preferences rather than attempting to provide a specific treatment to all subjects regardless of preference or need. Patients were contacted by telephone (mean, 6 times) or visited the clinic every other week (mean, 9 visits). When symptoms persisted, the team, including a specialist (psychiatrist), intervened. The depression CDM intervention included focus on a medical condition if the patient wished.
Rost et al.118 randomized 211 adults with major depression to usual primary medical care or to a CDM intervention group. An “initial intervention” was a visit with a trained office nurse to assess depressive symptoms, provide education about treatment options, address readiness to engage in treatment, and arrange follow-up. In the “continuing intervention,” nurse care managers phoned patients to encourage adherence and to advise them to raise problems with their physicians. The content was tailored to whether the patient was symptomatic. Nurse care managers provided physicians with reports of patients’ symptoms and treatments, and a psychiatrist provided treatment guidelines. Chronic disease management increased remission of depression and improved emotional and physical functioning.
Simon et al.119 compared CDM with usual medical care for depression. Chronic disease management included telephone assessments of depressive symptoms and treatments, calls to those who discontinued treatments, assistance with appointments, reports to primary care physicians on patient progress with depression treatment recommendations, and suggestions to contact patients to schedule follow-up visits as needed. A psychiatrist supervised the CDM team. Chronic disease management improved prescription of appropriate doses of medication and decreased depressive symptoms and the incidence of major depression compared with usual care.
Hedrick et al.120 tested CDM for depression compared with usual primary care, in which psychiatrists were available for referrals in primary care. Care was by a multidisciplinary team in primary care consisting of a psychologist, psychiatrist, social workers, and a psychology technician. The team implemented evidence-based care (antidepressants and 6 sessions of cognitive behavioral therapy), communicated with primary care physicians, took patient preferences into account, proactively monitored patient symptoms and treatment barriers, and provided patient education. Chronic disease management increased the proportion of patients receiving effective therapies for depression and was associated with improved depressive symptoms and mental health-related quality of life.
Because substance dependence is associated with significant medical illness and cost consequences, the evidence regarding CDM for medical illnesses also is relevant. Chronic disease management for heart failure, diabetes, arthritis and asthma, in randomized, controlled studies121-126 and in systematic reviews of more than 100 trials43,44,127 leads to clinical and functional improvement, decreased hospitalizations, treatment adherence, and patient satisfaction. Health systems adopting these programs report improved outcomes.44 Of note, Whellan et al.’s126 intervention, in addition to addressing the target chronic disease of heart failure directly, also included “other strategies targeted at optimizing the control of concomitant illnesses that may worsen” heart failure. A lesson for addictions care might be to include care for common comorbid medical and psychiatric illnesses in substance dependence CDM.
Evidence for effectiveness of CDM for psychiatric and medical illnesses is strong. Because addiction has similarities with these chronic illnesses, CDM has potential for improving addiction outcomes.
ELEMENTS OF CDM FOR ADDICTION PROVEN EFFECTIVE
A Medline search from 1966 through late 2007 for “disease management” and “alcoholism” or “drug dependence” yielded few results, none of which included controlled trial evidence for the effectiveness of CDM for addiction. Given the lack of relevant published studies, we reviewed the evidence for 2 key components, which when combined would reflect on the potential benefit of CDM when studied in patients with addiction: a) integrated case management delivered by professionals, and b) integrative linkage of medical, psychosocial, and alcohol and drug dependence care.
Case management coordinates and links patients with appropriate services to address specific needs across systems of care,32,128,129 and in this model is delivered by a skilled nurse or social worker. Case management includes patient assessment, care planning and coordination, linkage to services, outcome monitoring, and advocacy for patients, in a single point of contact, for addiction, medical, and other services (eg, family services, self-help groups, insurance, food, housing, transportation, and employment). In alcohol and drug treatment practice, the CM definition is quite varied,32,130,131 may be delivered by paraprofessionals or peers, and not all models are effective. When CM and addiction treatment are delivered by one clinician, the approach is more effective than case management alone.32 One key ingredient is therapeutic alliance.132 This alliance impacts homelessness,31 treatment participation, drinking,133 and drug treatment retention and outcome,134,135 particularly for those with more severe psychiatric problems.136
Case management can increase linkage from substance abuse treatment to primary medical care.48 Case management also can decrease relapse and increase retention in addictions treatment.137 McLellan et al. compared outpatient group counseling twice per week with counseling and case management in a quasi-experimental study in patients admitted to addiction treatment.15-20 Case management was associated with greater receipt of alcohol, medical, psychiatric, employment, and family services, and with less alcohol intoxication (and lower severity), and fewer days of psychiatric and medical problems.75 In a similar study,52 Case management improved alcohol use, medical, employment, legal, and family status. Stout et al.130 compared case monitoring aftercare delivered by skilled clinicians (case management plus reassessment and ongoing advice) for patients with alcohol abuse or dependence discharged from day hospital to standard referrals to outpatient follow-up. Case monitors met with subjects for 30 minutes and then by telephone monthly or less for 2 years. The interactions included constant reassessment, were supportive and nonjudgmental, and addressed substance use and other major life problems by referral. Recommendations depended on patient needs. Preliminary results were a 50% decrease in heavy drinking and fewer emergency visits in the CM group.41,138 Dennis et al.42 found that quarterly case management delivered by phone for patients in early recovery led to more appropriate treatment utilization.
A second element involves organizational restructuring: integration and “colocation” of services to achieve integration and continuity of care.139-142 Studies of colocation have found that patients with addictions who receive both regular addiction and medical care were less likely to be hospitalized than those who received one or neither service,143 and on-site medical service provision, transportation, and CM increased receipt of medical services.144-150 Friedmann et al.151 found that provision of primary medical care by off-site referral or on-site at drug treatment programs, compared with no such mechanism, reduced emergency, and hospital utilization.
Furthermore, on-site primary care at addiction programs has been associated with reduced addiction severity.152 In a randomized trial, patients receiving on-site medical, psychiatric, employment, and family services had less opiate use, and improved medical, employment, legal and psychiatric outcomes.74 Women with psychiatric problems were more likely to complete outpatient addictions care when offered psychiatric care.153 In a trial that randomized veterans without primary care who were entering substance abuse treatment with a chronic medical condition to receive primary medical care either on-site or off-site, on-site care increased access to primary care and addiction treatment retention.154
On-site alcohol and drug treatment in primary care also can improve alcohol and drug use outcomes and be safe and effective.155-159 In clinical trials, naltrexone for alcoholism was efficacious when given with primary care management.160 Similar findings of success of acamprosate in primary care have been reported.161 Furthermore, one study reported that 78% of patients receiving office-based buprenorphine for opiate dependence remained in care compared with 52% of patients in a traditional drug treatment center.158
In a unique model, Weisner et al.162 randomized 592 adults to usual, separate primary care, or integrated primary care at an addictions treatment program by 3 primary care physicians with specialty addictions training, a medical assistant, and 2 nurses. There were no overall differences in abstinence, but in a subgroup of patients with substance abuse-related medical conditions (57%), on-site care was associated with increased abstinence at 6 months. In a randomized trial in a special alcohol clinic for veterans,163 the integrated care group was more likely to be abstinent than a usual care group (74% versus 49% 30-day abstinence).164 The study intervention was focused on alcoholism but included substantial attention to comorbidity. The intervention was an initial thorough inpatient evaluation by a multidisciplinary team who developed a care plan to reduce alcohol severity and remission of related medical conditions. The plan included monthly primary care visits to review drinking and medical problems at a frequency indicated by clinical status and feedback of blood test results to encourage abstinence. Mental health and social services and more intensive alcohol treatment were provided on-site when necessary. Patients were contacted when they missed appointments. In a recent prospective study,165 patients with alcohol dependence were referred to Alcoholics Anonymous; when most refused to attend, the study provided monthly extensive visits with a medical nurse who was available for telephone consults, and brief visits with a gastroenterologist. Drinking decreased from 16 to 2.5 drinks per day.
Andersen et al.166 studied 45 adults cared for by a nurse care manager who addressed both their HIV and substance abuse, accompanying patients to physician visits and facilitating integration of medical and substance abuse treatment recommendations. Addiction severity and health-related quality of life improved significantly in this sample during 6 months. Bartels et al.167 studied 2022 elderly patients with a mental health disorder and/or at-risk drinking, randomizing them to integration and colocation of mental health and substance abuse services in primary care, or to facilitated referral, including scheduling and payment, and transportation, to specialty mental health, or substance abuse clinics. The integrated model was associated with greater attendance at mental health and substance abuse treatment. This body of research, both randomized controlled trials and cohort studies, supports the concept that integration of addiction, mental health, and medical services yields improvements in adherence to care, severity of substance use, and appropriate utilization of services.
CONCLUSIONS
Substance dependence is a common and costly chronic illness associated with medical and psychiatric comorbidity. Treatment can be efficacious when it is actually received by patients. But the current system of care is fragmented, not coordinated, and does not always include proven efficacious treatments. Patient motivation and coexisting health and social problems are barriers to receipt of effective treatment. Integrated and coordinated care, which simultaneously addresses patient motivation and needs across health domains, provides efficacious addiction treatments and facilitates effective access to other treatment. This integrated care may increase the likelihood that care is received and that addiction-related and other clinical outcomes improve. The World Health Organization called the management of chronic conditions “one of the greatest challenges facing health care systems throughout the world” and recommended building integrated health care as an essential part of the solution.168
Chronic disease management is a relatively new model to care for chronic psychiatric and medical illnesses and has not been fully applied or disseminated for alcohol or drug dependence. In fact, the leading and latest literature on the topic, prompted by calls from the Institute of Medicine, is silent regarding addictions.169 More recently, the Institute of Medicine has again, and more specifically, called for improvements in the quality of care for substance use conditions.170 Chronic disease management is one way to advance this agenda.
Chronic disease management shows promise as an effective strategy for managing substance dependence. It is critical to test the effectiveness of CDM integrated in a primary care setting for substance dependent patients, because this approach can take advantage of the fact that many patients with addictions attend primary care yet do not receive specialty care for their addictions. The current fragmented health service delivery models are limited in many ways for patients with the chronic illness of substance dependence. While we await studies of the effectiveness of CDM in primary care, elements of CDM could be implemented now.
In 1996, we judged from a review of the literature that linking people with addictions with primary medical care59 held promise, and later we detailed the potential benefits.58 In a randomized trial, we demonstrated that multidisciplinary assessment and referral increased linkage of people with addictions to primary medical care but found that simple linkage was not enough to improve health.171 Based on review of the latest literature, the evidence suggests that services delivery models that include case management and integrated care and are modeled on chronic disease (care) management hold promise for improving the care received by people with substance dependence.
ACKNOWLEDGMENTS
The authors thank the Health Evaluation and Linkage to Primary care (HELP) and the Addiction Health Evaluation and Disease management (AHEAD) study teams for their assistance in thinking broadly about the issues covered in this paper.
Drs. Saitz, Samet, and Larson were supported in this work by grants from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) (R-01 AA 10870) and the National Institute on Drug Abuse (NIDA) (R-01 DA 10019). In addition, Dr. Saitz is supported by grants from the NIAAA (R-01s AA. 13216, AA 14258, AA 14713, R25, AA 13822, and P60 AA 13759), the Substance Abuse and Mental Health Services Administration (SAMHSA) UT 9 TI018311, and the National Center for Research Resources (NCRR) (K30 RR 22252). Dr. Samet is supported by grants from NIAAA (R-01 AA 016059, K-24 AA 015674, and R-21 AA 014821), NIDA (R-01 DA 019841 and R-25 DA 13582), and (SAMHSA) (1 U79T8 018311), and Dr. Larson is supported by a grant from the NIDA (R01 DA 016929).
Footnotes
This work was presented in part at the annual meeting of the Research Society on Alcoholism, July 7-12, 2007, Chicago, IL.
REFERENCES
- 1.Humphreys K, Tucker JA. Toward more responsive and effective intervention systems for alcohol-related problems. Addiction. 2002;97:126–132. doi: 10.1046/j.1360-0443.2002.00004.x. [DOI] [PubMed] [Google Scholar]
- 2.Trask PC, Schwartz SM, Deaner SL, et al. Behavioral medicine: the challenge of integrating psychological and behavioral approaches into primary care. Eff Clin Pract. 2002;5:75–83. [PubMed] [Google Scholar]
- 3.Weisner C, Schmidt LA. Expanding the frame of health services research in the drug abuse field. Health Serv Res. 1995;30:707–726. [PMC free article] [PubMed] [Google Scholar]
- 4.Von Korff M, Gruman J, Schaefer J, et al. Collaborative management of chronic illness. Ann Intern Med. 1997;127:1097–1102. doi: 10.7326/0003-4819-127-12-199712150-00008. [DOI] [PubMed] [Google Scholar]
- 5.Wagner EH. The role of patient care teams in chronic disease management. BMJ. 2000;320:569–572. doi: 10.1136/bmj.320.7234.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511–544. [PubMed] [Google Scholar]
- 7.Disease Management Association of America [Accessed July 14, 2007]; Available at: http://www.dmaa.org/dm_definition.asp.
- 8.Institute of Medicine. Committee on Quality of Health Care in America . Crossing the Quality Chasm: A New Health System for the 21st Century. National Academy Press; Washington, DC: 2001. [Google Scholar]
- 9.Hunter DJ, Fairfield G. Disease management. BMJ. 1997;315:50–53. doi: 10.1136/bmj.315.7099.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Department of Health Services Medicare program; voluntary chronic care improvement under traditional fee-for-service Medicare. Federal Register. 2004;69:22065–22079. [Google Scholar]
- 11.National Committee for Quality Assurance [Accessed July 17, 2007];Disease management standards and guidelines for accreditation. Draft standards for public comment. Available at: http://www.NCQA.org.
- 12.Bodenheimer T. Disease management: promises and pitfalls. N Engl J Med. 1999;340:1202–1205. doi: 10.1056/NEJM199904153401511. [DOI] [PubMed] [Google Scholar]
- 13.Bodenheimer T. Disease management in the American market. BMJ. 2000;320:563–566. doi: 10.1136/bmj.320.7234.563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DeBusk RF, West JA, Miller NH, et al. Chronic disease management: treating the patient with disease(s) vs treating disease(s) in the patient. Arch Intern Med. 1999;159:2739–2742. doi: 10.1001/archinte.159.22.2739. [DOI] [PubMed] [Google Scholar]
- 15.Kendrick T. Depression management clinics in general practice? Some aspects lend themselves to the mini-clinic approach. BMJ. 2000;320:527–528. doi: 10.1136/bmj.320.7234.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- 17.Substance Abuse and Mental Health Services Administration. Office of Applied Studies . Results from the 2005 National Survey on Drug Use and Health: National Findings. Rockville, MD: [3 Accessed July 17, 2007]. Office of Applied Studies, NSDUH Series H-30, DHHS Publication No. SMA 06-4194. Available at: http://oas.samhsa.gov/NSDUH/2k5NSDUH/2k5results.htm#7. [Google Scholar]
- 18.Cartwright WS. Economic costs of drug abuse in the United States. J Mental Health Policy Econ. 1999;2:133–134. doi: 10.1002/(sici)1099-176x(199909)2:3<133::aid-mhp53>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 19.Green-Hennessey S. Factors associated with receipt of behavioral health services among persons with substance dependence. Psychiatr Serv. 2002;53:1592–15798. doi: 10.1176/appi.ps.53.12.1592. [DOI] [PubMed] [Google Scholar]
- 20.Harwood HJ, Fountain D, Livermore G. The economic costs of alcohol and drug abuse in the United States-1992. National Institute on Drug Abuse, National Institute on Alcohol Abuse and Alcoholism; Washington, DC: 1998. [Google Scholar]
- 21.Harwood HJ. Updating estimates of the economic costs of alcohol abuse in the United States. National Institute on Alcohol Abuse and Alcoholism; Washington, DC: 2000. [Google Scholar]
- 22.National Institute on Alcohol Abuse and Alcoholism . Drinking in the United States: main findings from the 1992 National Longitudinal Alcohol Epidemiologic Survey (NLAES) U.S. Department of Health and Human Services; Bethesda, MD: 1998. [Google Scholar]
- 23.Grant BF, Dawson DA, Stinson FS, et al. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991-1992 and 2001-2002. Drug Alcohol Depend. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 24.D’Aunno T. Linking substance-abuse treatment and primary health Care. In: V Egertson JA, Fox DM, Leshner AI, editors. Treating Drug Abusers Effectively. Blackwell; Cambridge, MA: 1997. pp. 311–331. [Google Scholar]
- 25.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 26.Teitelbaum MA, Walker M, Gabay M, et al. Barriers to the delivery of integrated primary care services and substance abuse treatment: case studies of nine linkage program projects. Health Resources and Services Administration and ABT Associates, Inc.; Washington, DC: 1992. [Google Scholar]
- 27.Friedmann PD, Hendrickson JC, Gerstein D, et al. The effect of matching comprehensive services to patients’ needs on drug use improvement in addiction treatment. Addiction. 2004;99:962–972. doi: 10.1111/j.1360-0443.2004.00772.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saitz R, Horton NJ, Larson MJ, et al. Primary medical care and reductions in addiction severity: a prospective cohort study. Addiction. 2005;100:70–78. doi: 10.1111/j.1360-0443.2005.00916.x. [DOI] [PubMed] [Google Scholar]
- 29.Miller WR, Rollnick S. Motivational Interviewing. Preparing People to Change Addictive Behavior. The Guilford Press; New York: 1991. [Google Scholar]
- 30.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47:1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 31.Chinman MJ, Rosenheck R, Lam JA. The case management relationship and outcomes of homeless persons with serious mental illness. Psychiatr Serv. 2000;51:1142–1147. doi: 10.1176/appi.ps.51.9.1142. [DOI] [PubMed] [Google Scholar]
- 32.Ridgely SM, Willenbring ML. Application of case management to drug abuse treatment: overview of models and research issues. In: Ashery R, editor. Progress and Issues in Case Management. National Institute on Drug Abuse; Rockville, MD: 1992. pp. 12–33. [PubMed] [Google Scholar]
- 33.Litten RZ, Allen JP. Advances in development of medications for alcoholism treatment. Psychopharmacology (Berl) 1998;139:20–33. doi: 10.1007/s002130050686. [DOI] [PubMed] [Google Scholar]
- 34.Dole VP. Implications of methadone maintenance for theories of narcotic addiction. JAMA. 1988;260:3025–3029. [PubMed] [Google Scholar]
- 35.Volpicelli JR, Pettinati HM, McLellan AT, et al. Combining Medication and Psychosocial Treatments for Addictions. The BRENDA Approach. The Guilford Press; New York: 2001. [Google Scholar]
- 36.Edwards G. Withdrawal symptoms and alcohol dependence: fruitful mysteries. Br J Addict. 1990;85:447–461. doi: 10.1111/j.1360-0443.1990.tb01665.x. [DOI] [PubMed] [Google Scholar]
- 37.Kosten TR, O’Connor PG. Management of drug and alcohol withdrawal. N Engl J Med. 2003;348:1786–1795. doi: 10.1056/NEJMra020617. [DOI] [PubMed] [Google Scholar]
- 38.Friedmann PD, Saitz R, Samet JH. Management of adults recovering from alcohol or other drug problems: relapse prevention in primary care. JAMA. 1998;279:1227–1231. doi: 10.1001/jama.279.15.1227. [DOI] [PubMed] [Google Scholar]
- 39.Friedmann PD, Rose J, Hayaki J, et al. Training primary care clinicians in maintenance care for moderated alcohol use. J Gen Intern Med. 2006;21:1269–1275. doi: 10.1111/j.1525-1497.2006.00611.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moos RH, Moos BS. The interplay between help-seeking and alcohol-related outcomes: divergent processes for professional treatment and self-help groups. Drug Alcohol Depend. 2004;75:155–164. doi: 10.1016/j.drugalcdep.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 41.McKay JR. Is there a case for extended interventions for alcohol and drug use disorders? Addiction. 2005;100:1594–1610. doi: 10.1111/j.1360-0443.2005.01208.x. [DOI] [PubMed] [Google Scholar]
- 42.Dennis M, Scott CK, Funk R. An experimental evaluation of recovery management checkups (RMC) for people with chronic substance use disorders. Eval Program Planning. 2003;26:339–352. doi: 10.1016/S0149-7189(03)00037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bodenheimer T, Lorig K, Holman H, et al. Patient self-management of chronic disease in primary care. JAMA. 2002;288:2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 44.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288:1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 45.Hasin DS, Stinson FS, Ogburn E, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 46.McLellan AT. Have we evaluated addiction treatment correctly? Implications from a chronic care perspective. Addiction. 2002;97:249–252. doi: 10.1046/j.1360-0443.2002.00127.x. [DOI] [PubMed] [Google Scholar]
- 47.McLellan AT, Lewis DC, O’Brien CP, et al. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 48.Brindis C, Pfeffer R, Wolfe A. A case management program for chemically dependent clients with multiple needs. J Case Manag. 1995;4:22–28. [PubMed] [Google Scholar]
- 49.Brooner RK, King VL, Kidorf M, et al. Psychiatric and substance use comorbidity among treatment-seeking opioid abusers. Arch Gen Psychiatry. 1997;54:71–80. doi: 10.1001/archpsyc.1997.01830130077015. [DOI] [PubMed] [Google Scholar]
- 50.Hasin D, Liu X, Nunes E, et al. Effects of major depression on remission and relapse of substance dependence. Arch Gen Psychiatry. 2002;59:375–380. doi: 10.1001/archpsyc.59.4.375. [DOI] [PubMed] [Google Scholar]
- 51.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 52.McLellan AT, Hagan TA, Levine M, et al. Does clinical case management improve outpatient addiction treatment. Drug Alcohol Depend. 1999;55:91–103. doi: 10.1016/s0376-8716(98)00183-5. [DOI] [PubMed] [Google Scholar]
- 53.Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- 54.Ziedonis D, Brady K. Dual diagnosis in primary care. Detecting and treating both the addiction and mental illness. Med Clin North Am. 1997;81:1017–1036. doi: 10.1016/s0025-7125(05)70561-7. [DOI] [PubMed] [Google Scholar]
- 55.Mertens JR, Lu YW, Parthasarathy S, et al. Medical and psychiatric conditions of alcohol and drug treatment patients in an HMO: comparison with matched controls. Arch Intern Med. 2003;163:2511–2517. doi: 10.1001/archinte.163.20.2511. [DOI] [PubMed] [Google Scholar]
- 56.Compton WM, Thomas YF, Stinson FS, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- 57.Golin CE, Liu H, Hays RD, et al. A prospective study of predictors of adherence to combination antiretroviral medication. J Gen Intern Med. 2002;17:756–765. doi: 10.1046/j.1525-1497.2002.11214.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Samet JH, Friedmann P, Saitz R. Benefits of linking primary medical care and substance abuse services: patient, provider, and societal perspectives. Arch Intern Med. 2001;161:85–91. doi: 10.1001/archinte.161.1.85. [DOI] [PubMed] [Google Scholar]
- 59.Samet JH, Saitz R, Larson MJ. A case for enhanced linkage of substance abusers to primary medical care. Subst Abuse. 1996;17:181–192. [Google Scholar]
- 60.Weisner C, McCarty D, Schmidt L. New directions in alcohol and drug treatment under managed care. Am J Managed Care. 1999;5:SP57–SP69. [PubMed] [Google Scholar]
- 61.Brown RL, Saunders LA, Bobula JA, et al. Remission of alcohol disorders in primary care patients. Does diagnosis matter? J Fam Pract. 2000;49:522–528. [PubMed] [Google Scholar]
- 62.Mark T, Dilionardo J, Chalk M, Coffey R. Substance abuse detoxification: improvements needed in linkage to treatment (SMA-02-3728) Substance Abuse and Mental Health Services Administration; Rockville, MD: 2002. [Google Scholar]
- 63.Saitz R, Gaeta J, Cheng DM, et al. Risk of mortality during four years after substance detoxification in urban adults. J Urban Health. 2007;84:272–282. doi: 10.1007/s11524-006-9149-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Institute of Medicine . Broadening the Base of Treatment for Alcohol Problems. National Academy Press; Washington, DC: 1990. [PubMed] [Google Scholar]
- 65.Substance Abuse and Mental Health Services Administration. Office of Applied Studies. The Drug and Alcohol Services Information System (DASIS) Treatment completion in the Treatment Episode Data Set (TEDS) Rockville, MD: Jan 30, 2003. [Accessed July 17, 2007]. Available at: http://www.oas.samhsa.gov/2k3/TXcompleters/TXcompleters.cfm. [Google Scholar]
- 66.Substance Abuse and Mental Health Services Administration [Accessed July 17, 2007];Health insurance status of admissions for substance abuse treatment: 1999. Available at: http://www.oas.samhsa.gov/2k2/insuranceTX/insuranceTX.cfm. [PubMed]
- 67.Substance Abuse and Mental Health Services Administration. Office of Applied Studies. The National Household Survey on Drug Abuse (NHSDA) Drug and Alcohol Services Information System (DASIS) [Accessed July 17, 2007];Distance to substance abuse treatment facilities among those with alcohol dependence or abuse. Available at: http://www.oas.samhsa.gov/2k2/distance/distance.htm.
- 68.Grant BF. Barriers to alcoholism treatment: reasons for not seeking treatment in a general population sample. J Stud Alcohol. 1997;58:365–371. doi: 10.15288/jsa.1997.58.365. [DOI] [PubMed] [Google Scholar]
- 69.Joe GW, Simpson DD, Broome KM. Effects of readiness for drug abuse treatment on client retention and assessment of process. Addiction. 1998;93:1177–1190. doi: 10.1080/09652149835008. [DOI] [PubMed] [Google Scholar]
- 70.Joe GW, Simpson DD, Greener JM, et al. Integrative modeling of client engagement and outcomes during the first 6 months of methadone treatment. Addict Behav. 1999;24:649–659. doi: 10.1016/s0306-4603(99)00024-6. [DOI] [PubMed] [Google Scholar]
- 71.Weisner C, Mertens J, Tam T, et al. Factors affecting the initiation of substance abuse treatment in managed care. Addiction. 2001;96:705–716. doi: 10.1046/j.1360-0443.2001.9657056.x. [DOI] [PubMed] [Google Scholar]
- 72.Miller WR, Wilbourne PL. Mesa Grande: a methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction. 2002;97:265–277. doi: 10.1046/j.1360-0443.2002.00019.x. [DOI] [PubMed] [Google Scholar]
- 73.Johnson RE, Chutuape MA, Strain EC, et al. A comparison of levomethadyl acetate, buprenorphine, and methadone for opioid dependence. N Engl J Med. 2000;343:1290–1297. doi: 10.1056/NEJM200011023431802. [DOI] [PubMed] [Google Scholar]
- 74.McLellan AT, Arndt IO, Metzger DS, et al. The effects of psychosocial services in substance abuse treatment. JAMA. 1993;269:1953–1959. [PubMed] [Google Scholar]
- 75.McLellan AT, Hagan TA, Levine M, et al. Supplemental social services improve outcomes in public addiction treatment. Addiction. 1998;93:1489–1499. doi: 10.1046/j.1360-0443.1998.931014895.x. [DOI] [PubMed] [Google Scholar]
- 76.Higgins ST, Petry NM. Contingency management. Incentives for sobriety. Alcohol Res Health. 1999;23:122–127. [PMC free article] [PubMed] [Google Scholar]
- 77.Rawson RA. [Accessed July 17, 2007];Treatment for stimulant use disorders, Treatment Improvement Protocol (TIP) Series 33. Available at: http://ncadi.samhsa.gov/govpubs/BKD289/33f.aspx.
- 78.Burke BL, Arkowitz H, Dunn C. The efficacy of motivational interviewing and its adaptations. What we know so far. In: Miller W, Rollnick S, editors. Motivational Interviewing. Preparing People for Change. 2nd ed. Guilford Press; New York: 2002. pp. 217–250. [Google Scholar]
- 79.Zweben A, Zuckoff A. Motivational interviewing and treatment adherence. In: Miller W, Rollnick S, editors. Motivational Interviewing. Preparing People for Change. 2nd ed. Guilford Press; New York: 2002. pp. 299–319. [Google Scholar]
- 80.Fiellin DA, O’Connor PG. Clinical practice. Office-based treatment of opioid-dependent patients. N Engl J Med. 2002;347:817–823. doi: 10.1056/NEJMcp013579. [DOI] [PubMed] [Google Scholar]
- 81.Thomas C, Wallack S, Swift D, et al. Barriers to adoption of naltrexone in alcoholism treatment: a three-state study. Alcohol Clin Exp Res. 2000;24:38A. [Google Scholar]
- 82.Knudsen HK, Ducharme LJ, Roman PM, et al. Buprenorphine diffusion: the attitudes of substance abuse treatment counselors. J Subst Abuse Treat. 2005;29:95–106. doi: 10.1016/j.jsat.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 83.Thomas CP, Wallack SS, Lee S, et al. Research to practice: adoption of naltrexone in alcoholism treatment. J Subst Abuse Treat. 2003;24:1–11. [PubMed] [Google Scholar]
- 84.Garbutt JC, Kranzler HR, O’Malley SS, et al. Efficacy and tolerability of long-acting injectable naltrexone for alcohol dependence: a randomized controlled trial. JAMA. 2005;293:1617–1625. doi: 10.1001/jama.293.13.1617. [DOI] [PubMed] [Google Scholar]
- 85.Ward LD, Shea JA, Laine C, et al. Willingness to provide primary care office-based methadone maintenance (PCOM): a qualitative study of clinic directors. J Gen Intern Med. 2003;18:277. abstract. [Google Scholar]
- 86.Miller WR, Moyers TB, Arciniega L, et al. Training, supervision and quality monitoring of the COMBINE Study behavioral interventions. J Stud Alcohol Suppl. 2005:188–195. doi: 10.15288/jsas.2005.s15.188. [DOI] [PubMed] [Google Scholar]
- 87.Pettinati HM, Volpicelli JR, Pierce JD, Jr, et al. Improving naltrexone response: an intervention for medical practitioners to enhance medication compliance in alcohol dependent patients. J Addict Dis. 2000;19:71–83. doi: 10.1300/J069v19n01_06. [DOI] [PubMed] [Google Scholar]
- 88.Kaempf G, O’Donnell C, Oslin DW. The BRENDA model: a psychosocial addiction model to identify and treat alcohol disorders in elders. Geriatr Nurs. 1999;20:302–304. doi: 10.1053/gn.1999.v20.103922001. [DOI] [PubMed] [Google Scholar]
- 89.Friedmann PD, Ramsey S, Herman D, et al. Maintenance care for alcohol problems in remission in primary care; Presented at the 2002 National Meeting of the Association for Medical Education and Research on Substance Abuse; Washington, DC. 2002. [Google Scholar]
- 90.Laine C, Newschaffer C, Zhang D, et al. Models of care in New York State Medicaid substance abuse clinics. Range of services and linkages to medical care. J Subst Abuse. 2000;12:271–285. doi: 10.1016/s0899-3289(00)00054-7. [DOI] [PubMed] [Google Scholar]
- 91.Buchsbaum DG, Buchanan RG, Poses RM, et al. Physician detection of drinking problems in patients attending a general medicine practice. J Gen Intern Med. 1992;7:517–521. doi: 10.1007/BF02599456. [DOI] [PubMed] [Google Scholar]
- 92.Saitz R, Mulvey KP, Plough A, et al. Physician unawareness of serious substance abuse. Am J Drug Alcohol Abuse. 1997;23:343–354. doi: 10.3109/00952999709016881. [DOI] [PubMed] [Google Scholar]
- 93.Saitz R, Mulvey KP, Samet JH. The substance abusing patient and primary care: linkage via the addiction treatment system? Substance Abuse. 1997;18:187–195. [Google Scholar]
- 94.Kunnes R, Niven R, Gustafson T, et al. Financing and payment reform for primary health care and substance abuse treatment. J Addict Dis. 1993;12:23–42. doi: 10.1300/J069v12n02_03. [DOI] [PubMed] [Google Scholar]
- 95.Trude S, Stoddard JJ. Referral gridlock: primary care physicians and mental health services. J Gen Intern Med. 2003;18:442–449. doi: 10.1046/j.1525-1497.2003.30216.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Arboleda-Florez J, Saraceno B. Mental health and primary care. Can Med Assoc J. 2001;164:1013–1014. [PMC free article] [PubMed] [Google Scholar]
- 97.Dodds S, Blaney NT, Nuehring EM, et al. Integrating mental health services into primary care for HIV-infected pregnant and non-pregnant women: whole life- a theoretically derived model for clinical care and outcomes assessment. Gen Hosp Psychiatry. 2000;22:251–260. doi: 10.1016/s0163-8343(00)00090-6. [DOI] [PubMed] [Google Scholar]
- 98.Feingold A, Slammon WR. A model integrating mental health and primary care services for families with HIV. Gen Hosp Psychiatry. 1993;15:290–300. doi: 10.1016/0163-8343(93)90021-f. [DOI] [PubMed] [Google Scholar]
- 99.Felker BL, Barnes RF, Greenberg DM, et al. Preliminary outcomes from an integrated mental health primary care team. Psychiatr Serv. 2004;55:442–444. doi: 10.1176/appi.ps.55.4.442. [DOI] [PubMed] [Google Scholar]
- 100.Kates N, Craven M, Crustolo AM, et al. Integrating mental health services within primary care. Gen Hosp Psychiatry. 1997;19:324–332. doi: 10.1016/s0163-8343(97)00051-0. [DOI] [PubMed] [Google Scholar]
- 101.Von Korff M. Can care management enhance integration of primary and specialty care? BMJ. 2004;329:605. doi: 10.1136/bmj.329.7466.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Dietrich A, Oxman TE, Williams JW, et al. Re-engineering systems for the treatment of depression in primary care: cluster randomised controlled trial. BMJ. 2004;329:602–605. doi: 10.1136/bmj.38219.481250.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Druss BG, Rohrbaugh RM, Levinson CM, et al. Integrated medical care for patients with serious psychiatric illness: a randomized trial. Arch Gen Psychiatry. 2001;58:861–868. doi: 10.1001/archpsyc.58.9.861. [DOI] [PubMed] [Google Scholar]
- 104.Mechanic D. Policy challenges in improving mental health services: some lessons from the past. Psychiatr Serv. 2003;54:1227–1232. doi: 10.1176/appi.ps.54.9.1227. [DOI] [PubMed] [Google Scholar]
- 105.Olfson M, Mechanic D, Boyer CA, et al. Linking inpatients with schizophrenia to outpatient care. Psychiatr Serv. 1998;49:911–917. doi: 10.1176/ps.49.7.911. [DOI] [PubMed] [Google Scholar]
- 106.Glisson C, Hemmelgarn A. The effects of organizational climate and interorganizational coordination on the quality and outcomes of children’s service systems. Child Abuse Negl. 1998;22:401–421. doi: 10.1016/s0145-2134(98)00005-2. [DOI] [PubMed] [Google Scholar]
- 107.Goldman HH, Morrissey JP, Ridgely MS. Evaluating the Robert Wood Johnson Foundation program on chronic mental illness. Milbank Q. 1994;72:37–47. [PubMed] [Google Scholar]
- 108.Bickman L. Implications of a children’s mental health managed care demonstration evaluation. J Ment Health Adm. 1996;23:107–117. doi: 10.1007/BF02518647. [DOI] [PubMed] [Google Scholar]
- 109.Mueser KT, Corrigan PW, Hilton DW, et al. Illness management and recovery: a review of the research. Psychiatr Serv. 2002;53:1272–1284. doi: 10.1176/appi.ps.53.10.1272. [DOI] [PubMed] [Google Scholar]
- 110.Weingarten SR, Henning JM, Badamgarav E, et al. Interventions used in disease management programmes for patients with chronic illness-which ones work? Meta-analysis of published reports. BMJ. 2002;325:925. doi: 10.1136/bmj.325.7370.925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Badamgarav E, Weingarten SR, Henning JM, et al. Effectiveness of disease management programs in depression: a systematic review. Am J Psychiatry. 2003;160:2080–2090. doi: 10.1176/appi.ajp.160.12.2080. [DOI] [PubMed] [Google Scholar]
- 112.Katon W, Russo J, Von Korff M, et al. Long-term effects of a collaborative care intervention in persistently depressed primary care patients. J Gen Intern Med. 2002;17:741–748. doi: 10.1046/j.1525-1497.2002.11051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Katon WJ, Roy-Byrne P, Russo J, et al. Cost-effectiveness and cost offset of a collaborative care intervention for primary care patients with panic disorder. Arch Gen Psychiatry. 2002;59:1098–1104. doi: 10.1001/archpsyc.59.12.1098. [DOI] [PubMed] [Google Scholar]
- 114.Roy-Byrne PP, Katon W, Cowley DS, et al. A randomized effectiveness trial of collaborative care for patients with panic disorder in primary care. Arch Gen Psychiatry. 2001;58:869–876. doi: 10.1001/archpsyc.58.9.869. [DOI] [PubMed] [Google Scholar]
- 115.Schoenbaum M, Unutzer J, Sherbourne C, et al. Cost-effectiveness of practice-initiated quality improvement for depression: results of a randomized controlled trial. JAMA. 2001;286:1325–1330. doi: 10.1001/jama.286.11.1325. [DOI] [PubMed] [Google Scholar]
- 116.Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 117.Lin EH, Katon W, Von Korff M, et al. Effect of improving depression care on pain and functional outcomes among older adults with arthritis: a randomized controlled trial. JAMA. 2003;290:2428–2429. doi: 10.1001/jama.290.18.2428. [DOI] [PubMed] [Google Scholar]
- 118.Rost K, Nutting P, Smith JL, et al. Managing depression as a chronic disease: a randomised trial of ongoing treatment in primary care. BMJ. 2002;325:934. doi: 10.1136/bmj.325.7370.934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Simon GE, VonKorff M, Rutter C, et al. Randomised trial of monitoring, feedback, and management of care by telephone to improve treatment of depression in primary care. BMJ. 2000;320:550–554. doi: 10.1136/bmj.320.7234.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hedrick SC, Chaney EF, Felker B, et al. Effectiveness of collaborative care depression treatment in Veterans’ Affairs primary care. J Gen Intern Med. 2003;18:9–16. doi: 10.1046/j.1525-1497.2003.11109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Blonde L. Disease management approaches to type 2 diabetes. Manag Care. 2000;9:18–23. [PubMed] [Google Scholar]
- 122.McAlister FA, Lawson FM, Teo KK, et al. A systematic review of randomized trials of disease management programs in heart failure. Am J Med. 2001;110:378–384. doi: 10.1016/s0002-9343(00)00743-9. [DOI] [PubMed] [Google Scholar]
- 123.Rich MW, Beckham V, Wittenberg C, et al. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995;333:1190–1195. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- 124.Riegel B, Carlson B, Kopp Z, et al. Effect of a standardized nurse case-management telephone intervention on resource use in patients with chronic heart failure. Arch Intern Med. 2002;162:705–712. doi: 10.1001/archinte.162.6.705. [DOI] [PubMed] [Google Scholar]
- 125.Vrijhoef HJ, Diederiks JP, Spreeuwenberg C. Effects on quality of care for patients with NIDDM or COPD when the specialised nurse has a central role: a literature review. Patient Educ Couns. 2000;41:243–250. doi: 10.1016/s0738-3991(99)00104-4. [DOI] [PubMed] [Google Scholar]
- 126.Whellan DJ, Gaulden L, Gattis WA, et al. The benefit of implementing a heart failure disease management program. Arch Intern Med. 2001;161:2223–2228. doi: 10.1001/archinte.161.18.2223. [DOI] [PubMed] [Google Scholar]
- 127.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA. 2002;288:1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 128.National Institute on Drug Abuse . Progress and Issues in Case Management. National Institute on Drug Abuse; Rockville, MD: 1992. [Google Scholar]
- 129.Siegal HA. Comprehensive case management for substance abuse treatment. U.S. Department of Health and Human Services; Rockville, MD: 2001. [Google Scholar]
- 130.Stout RL, Rubin A, Zwick W, et al. Optimizing the cost-effectiveness of alcohol treatment: a rationale for extended case monitoring. Addict Behav. 1999;24:17–35. doi: 10.1016/s0306-4603(98)00029-x. [DOI] [PubMed] [Google Scholar]
- 131.Willenbring ML, Ridgely MS, Stinchfield R, et al. Application of case management in alcohol and drug dependence: matching techniques and populations. U.S. Department of Health and Human Services; Washington, DC: 1991. [Google Scholar]
- 132.Horvath A, Symonds B. Relation between working alliance and outcome in psychotherapy: a meta-analysis. J Counsel Psychol. 1991;38:139–149. [Google Scholar]
- 133.Connors GJ, Carroll KM, DiClemente CC, et al. The therapeutic alliance and its relationship to alcoholism treatment participation and outcome. J Consult Clin Psychol. 1997;65:588–598. doi: 10.1037//0022-006x.65.4.588. [DOI] [PubMed] [Google Scholar]
- 134.Barber JP, Luborsky L, Gallop R, et al. Therapeutic alliance as a predictor of outcome and retention in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study. J Consult Clin Psychol. 2001;69:119–124. doi: 10.1037//0022-006x.69.1.119. [DOI] [PubMed] [Google Scholar]
- 135.Luborsky L, Barber JP, Siqueland L. The revised Helping Alliance Questionnaire (HA-II): psychometric properties. J Psychotherap Res. 1996;5:260–271. [PMC free article] [PubMed] [Google Scholar]
- 136.Petry NM, Bickel WK. Therapeutic alliance and psychiatric severity as predictors of completion of treatment for opioid dependence. Psychiatr Serv. 1999;50:219–227. doi: 10.1176/ps.50.2.219. [DOI] [PubMed] [Google Scholar]
- 137.Shwartz M, Baker G, Mulvey KP, et al. Improving publicly funded substance abuse treatment: the value of case management. Am J Public Health. 1997;87:1659–1664. doi: 10.2105/ajph.87.10.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hilton ME, Maisto SA, Conigliaro J, et al. Improving alcoholism treatment across the spectrum of services. Alcohol Clin Exp Res. 2001;25:128–135. [PubMed] [Google Scholar]
- 139.Bachrach LL. Continuity of care for chronic mental patients: a conceptual analysis. Am J Psychiatry. 1981;138:1449–1456. doi: 10.1176/ajp.138.11.1449. [DOI] [PubMed] [Google Scholar]
- 140.Baker F. Coordination of alcohol, drug abuse, and mental health services. U.S. Department of Health and Human Services; Rockville, MD: 1991. [Google Scholar]
- 141.Intagliata J. Improving the quality of community care for the chronically mentally disabled: the role of case management. Schizophr Bull. 1982;8:655–674. doi: 10.1093/schbul/8.4.655. [DOI] [PubMed] [Google Scholar]
- 142.Willenbring M. Psychiatric care management for chronic addictive disorders: conceptual framework. Am J Addict. 2001;10:242–248. doi: 10.1080/105504901750532120. [DOI] [PubMed] [Google Scholar]
- 143.Laine C, Hauck WW, Gourevitch MN, et al. Regular outpatient medical and drug abuse care and subsequent hospitalization of persons who use illicit drugs. JAMA. 2001;285:2355–2362. doi: 10.1001/jama.285.18.2355. [DOI] [PubMed] [Google Scholar]
- 144.Des Jarlais DC, Fisher DG, Newman JC, et al. Providing hepatitis B vaccination to injection drug users: referral to health clinics vs on-site vaccination at a syringe exchange program. Am J Public Health. 2001;91:1791–1792. doi: 10.2105/ajph.91.11.1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Friedmann PD, Alexander JA, Jin L, et al. On-site primary care and mental health services in outpatient drug abuse treatment units. J Behav Health Serv Res. 1999;26:80–94. doi: 10.1007/BF02287796. [DOI] [PubMed] [Google Scholar]
- 146.Friedmann PD, D’Aunno TA, Jin L, et al. Medical and psychosocial services in drug abuse treatment: do stronger linkages promote client utilization? Health Serv Res. 2000;35:443–465. [PMC free article] [PubMed] [Google Scholar]
- 147.Friedmann PD, Lemon SC, Stein MD, et al. Linkage to medical services in the Drug Abuse Treatment Outcome Study. Med Care. 2001;39:284–295. doi: 10.1097/00005650-200103000-00008. [DOI] [PubMed] [Google Scholar]
- 148.Mezzelani P, Venturini L, Turrina G, et al. High compliance with a hepatitis B virus vaccination program among intravenous drug users. J Infect Dis. 1991;163:923. doi: 10.1093/infdis/163.4.923. [DOI] [PubMed] [Google Scholar]
- 149.Perlman DC, Perkins MP, Solomon N, et al. Tuberculosis screening at a syringe exchange program. Am J Public Health. 1997;87:862–863. [PubMed] [Google Scholar]
- 150.Stancliff S, Salomon N, Perlman DC, et al. Provision of influenza and pneumococcal vaccines to injection drug users at a syringe exchange. J Subst Abuse Treat. 2000;18:263–265. doi: 10.1016/s0740-5472(99)00064-1. [DOI] [PubMed] [Google Scholar]
- 151.Friedmann PD, Hendrickson JC, Gerstein DR, et al. Do mechanisms that link addiction treatment patients to primary care influence subsequent utilization of emergency and hospital care? Med Care. 2006;44:8–15. doi: 10.1097/01.mlr.0000188913.50489.77. [DOI] [PubMed] [Google Scholar]
- 152.Friedmann P, Zhang Z, Hendrickson J, et al. Effects of primary medical care on addiction and medical severity in substance abuse treatment programs. J Gen Intern Med. 2003;18:1–8. doi: 10.1046/j.1525-1497.2003.10601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Magura S, Horgan CM, Mertens JR, et al. Effects of managed care on alcohol and other drug (AOD) treatment. Alcohol Clin Exp Res. 2002;26:416–422. [PubMed] [Google Scholar]
- 154.Saxon AJ, Malte CA, Sloan KL, et al. Randomized trial of onsite versus referral primary medical care for veterans in addictions treatment. Med Care. 2006;44:334–342. doi: 10.1097/01.mlr.0000204052.95507.5c. [DOI] [PubMed] [Google Scholar]
- 155.O’Connor PG, Carroll KM, Shi JM, et al. Three methods of opioid detoxification in a primary care setting. A randomized trial. Ann Intern Med. 1997;127:526–530. doi: 10.7326/0003-4819-127-7-199710010-00004. [DOI] [PubMed] [Google Scholar]
- 156.Basu S, Smith-Rohrberg D, Bruce RD, et al. Models for integrating buprenorphine therapy into the primary HIV care setting. Clin Infect Dis. 2006;42:716–721. doi: 10.1086/500200. [DOI] [PubMed] [Google Scholar]
- 157.O’Connor PG, Farren CK, Rounsaville BJ, et al. A preliminary investigation of the management of alcohol dependence with naltrexone by primary care providers. Am J Med. 1997;103:477–482. doi: 10.1016/s0002-9343(97)00271-4. [DOI] [PubMed] [Google Scholar]
- 158.O’Connor PG, Oliveto AH, Shi JM, et al. A randomized trial of buprenorphine maintenance for heroin dependence in a primary care clinic for substance users versus a methadone clinic. Am J Med. 1998;105:100–105. doi: 10.1016/s0002-9343(98)00194-6. [DOI] [PubMed] [Google Scholar]
- 159.O’Connor PG, Waugh ME, Carroll KM, et al. Primary care-based ambulatory opioid detoxification: the results of a clinical trial. J Gen Intern Med. 1995;10:255–260. doi: 10.1007/BF02599882. [DOI] [PubMed] [Google Scholar]
- 160.O’Malley SS, Rounsaville BJ, Farren C, et al. Initial and maintenance naltrexone treatment for alcohol dependence using primary care vs specialty care: a nested sequence of 3 randomized trials. Arch Intern Med. 2003;163:1695–1704. doi: 10.1001/archinte.163.14.1695. [DOI] [PubMed] [Google Scholar]
- 161.Kiritze-Topor P, Huas D, Rosenzweig C, et al. A pragmatic trial of acamprosate in the treatment of alcohol dependence in primary care. Alcohol Alcohol. 2004;39:520–527. doi: 10.1093/alcalc/agh088. [DOI] [PubMed] [Google Scholar]
- 162.Weisner C, Mertens J, Parthasarathy S, et al. Integrating primary medical care with addiction treatment: a randomized controlled trial. JAMA. 2001;286:1715–1723. doi: 10.1001/jama.286.14.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Willenbring M, Olson D, Bielinski J. Integrated outpatients treatment for medically ill alcoholic men: results from a quasi-experimental study. J Stud Alcohol. 1995;56:337–343. doi: 10.15288/jsa.1995.56.337. [DOI] [PubMed] [Google Scholar]
- 164.Willenbring M, Olson D. A randomized trial of integrated outpatient treatment for medically ill alcoholic men. Arch Intern Med. 1999;159:1946–1952. doi: 10.1001/archinte.159.16.1946. [DOI] [PubMed] [Google Scholar]
- 165.Lieber CS, Weiss DG, Groszmann R, et al. I. Veterans Affairs Cooperative Study of polyenylphosphatidylcholine in alcoholic liver disease: effects on drinking behavior by nurse/physician teams. Alcohol Clin Exp Res. 2003;27:1757–1764. doi: 10.1097/01.ALC.0000093744.12232.34. [DOI] [PubMed] [Google Scholar]
- 166.Andersen M, Paliwoda J, Kaczynski R, et al. Integrating medical and substance abuse treatment for addicts living with HIV/AIDS: evidence-based nursing practice model. Am J Drug Alcohol Abuse. 2003;29:847–859. doi: 10.1081/ada-120026264. [DOI] [PubMed] [Google Scholar]
- 167.Bartels SJ, Coakley EH, Zubritsky C, et al. Improving access to geriatric mental health services: a randomized trial comparing treatment engagement with integrated versus enhanced referral care for depression, anxiety, and at-risk alcohol use. Am J Psychiatry. 2004;161:1455–1462. doi: 10.1176/appi.ajp.161.8.1455. [DOI] [PubMed] [Google Scholar]
- 168.World Health Organization [Accessed July 17, 2007];Executive summary and global report. Innovative care for chronic conditions: building blocks for action. Noncommunicable diseases and mental health. Available at: http://www.who.int/chp/en/
- 169.Casalino L, Gillies RR, Shortell SM, et al. External incentives, information technology, and organized processes to improve health care quality for patients with chronic diseases. JAMA. 2003;289:434–441. doi: 10.1001/jama.289.4.434. [DOI] [PubMed] [Google Scholar]
- 170.Institute of Medicine . Improving the Quality of Health Care for Mental and Substance-Use Conditions: Quality Chasm Series. The National Academies Press; Washington, DC: 2005. [PubMed] [Google Scholar]
- 171.Samet JH, Larson M, Horton NJ, et al. Linking alcohol and drug dependent adults to primary medical care: a randomized controlled trial of a multidisciplinary health intervention in a detoxification unit. Addiction. 2003;98:509–516. doi: 10.1046/j.1360-0443.2003.00328.x. [DOI] [PubMed] [Google Scholar]