Abstract
We report the first known case of fungal keratitis caused by Aspergillus nomius. Ocular injury was known as a predisposing factor. The patient was treated with natamycin and econazole eye drops, itraconazole eye ointment, and oral ketoconazole. A therapeutic penetrating keratoplasty was performed 16 days after presentation. A sequence-based approach was used to assign the isolate to a species.
CASE REPORT
A 64-year-old woman with no significant ophthalmic or systemic history presented with a history of pain, redness, and defective vision of the right eye of 4 days’ duration following a minor trauma sustained by mud splashing into the eye. She had been treated elsewhere earlier, and her medications consisted of the use of tobramycin, phenylephrine, natamycin, and moxifloxacin eye drops for 1 day.
On examination, her uncorrected visual acuity was less than 20/800 (<1/60) in the right eye. Slit lamp examination of the right eye was significant for an area of infiltration (6.2 to 7.5 mm) involving the central cornea and extending toward the limbus temporally and superiorly. The infiltrate involved all the layers of the stroma, and there was a dense endothelial plaque. A hypopyon of 1 mm was present. Scrapings obtained from the corneal infiltrate were stained (Gram's stain and 10% KOH) and plated on 5% sheep blood agar, chocolate agar, and potato dextrose agar. Both the Gram stain and the KOH mounts were positive for fungal filaments, and the cultures subsequently grew a fungus which was initially identified as a member of Aspergillus section Flavi.
Given the severity of the infection, the patient was admitted to the hospital, and intensive topical antifungal therapy was initiated. Natamycin (5%) and econazole (2%) eye drops were started on a half-hourly basis, while itraconazole (1%) eye ointment was applied three times a day. This was supplemented with cycloplegics (homatropine) and medication for the relief of pain. Oral antifungal medication in the form of tablets (200 mg ketoconazole twice a day) was also given.
In spite of intensive therapy, the infiltrate continued to progress with thinning and melting of the cornea. Doxycycline tablets were administered to decrease the collagenolytic activity, and amphotericin B (50 μg/ml) eye drops were also added to the medical regimen, but the infiltrate continued to progress to involve the entire cornea with descemetocele formation and finally perforation. A therapeutic penetrating keratoplasty was performed 16 days after presentation. Scleral extension was noted intraoperatively at the superior limbus. The corneal button removed at the time of surgery was also positive for a heavy growth of Aspergillus. Postoperatively the same medical regimen was continued in a tapering fashion, and the patient was discharged on the 10th postoperative day. After an interval of 35 days postoperatively, she once again presented with an area of infiltration at 11 o'clock of the superior sclera; this was treated successfully medically, and the infiltrate healed in a week. She was asked to continue natamycin and econazole (2%) four times a day along with itraconazole (1%) eye ointment three times and homatropine (2%) eye drops twice a day.
The patient was lost to follow-up until 40 days later, when she presented with pain and redness. Examination was remarkable for the presence of a tender nodule involving an area of the sclera from 7 o'clock to 9 o'clock. The patient was once again placed on intensive antifungal therapy with amphotericin B (50 μg/ml) eye drops and econazole (2%) eye drops being administered half-hourly, along with itraconazole (1%) eye ointment three times a day and ketoconazole (200 mg) twice daily. She was once again lost to follow-up and presented intermittently over the next 5 months with scleral involvement, either active scleritis or involvement with ocular congestion. Throughout the follow-up period, her vision in the right eye continued to be perception of light. The graft continued to be edematous.
Her compliance continued to be poor. At each presentation, she was placed on topical and systemic antifungals as well as topical and systemic nonsteroid anti-inflammatory drugs. Therapy always provided symptomatic relief as well as resolution of signs of scleritis. She was last seen 9 months after the initial presentation. Her vision in the right eye was positive for perception of light. An area of scleral thinning extending from 7 to 12 o'clock was noted along with an area of persistent inflammation in the superonasal quadrant.
Mycological study and diagnosis.
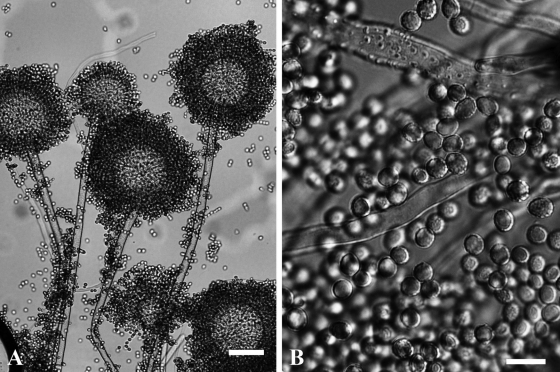
The case isolate was subcultured on Czapek Dox yeast extract and malt extract agar plates for morphological identification. The fungus was identified as Aspergillus species from section Flavi based on colony morphology and microscopic features of the isolate (Fig. 1). Colony surface on Czapek Dox yeast extract was velvety to floccose, consisting of white or light orange-brown vegetative mycelium and sparse to moderately abundant conidial structures. Colony reverse was light yellow or orange-brown. Sclerotia could not be observed. Conidiophores were variable in length (600 to 1,500 mm), uncolored, and echinulate (Fig. 1A). Conidial heads were yellowish green, biseriate, and radiate, often splitting into several columns. Vesicles were globose to subglobose, 45 to 65 μm in diameter. Conidia were globose to subglobose, echinulate, and 4 to 6 μm in diameter (Fig. 1B). Living cultures were deposited at the Department of Microbiology, Aravind Eye Hospital and Postgraduate Institute of Ophthalmology, Coimbatore, India (strain number: 823/07), and at the Centraalbureau voor Schimmelcultures (CBS 123901).
FIG. 1.
Conidial heads (A) and conidia (B) of A. nomius 823/07. Scale bars, 200 μm (A) and 10 μm (B).
For the purposes of molecular identification, mycelia grown in liquid YPG medium (0.5% Bacto yeast extract, 0.5% Bacto peptone, 1% glucose) for 1 day were subjected to DNA isolation by the Masterpure yeast DNA purification kit (Epicentre Biotechnologies, Madison, WI) according to the manufacturer's instructions. The internal transcribed spacer (ITS) region of the rRNA gene complex, incorporating ITS1, the 5.8S rRNA gene, and ITS2, was amplified using primers ITS1 and ITS4 (31). Part of the calmodulin gene was amplified using the primers cmd5 and cmd6 as described by Hong et al. (12), while a segment of the β-tubulin gene was amplified using primers bT2a and bT2b (10). DNA sequences were determined using a BigDye Terminator v3.1 cycle sequencing kit (Applied Biosystems Inc., Foster City, CA) and an ABI 3100 DNA sequencer. Sequence analysis was carried out by BLASTN similarity search at the website of the National Center for Biotechnology Information (http://www.ncbi.nlm.nih.gov/BLAST) (2). Molecular identification based on sequence analysis of ITS, β-tubulin, and calmodulin sequences revealed that the isolate belongs to the species Aspergillus nomius.
Antifungal susceptibility testing.
The Etest method (AB Biodisk, Solna, Sweden) for molds was used to determine the MICs of the isolate to amphotericin B, fluconazole, itraconazole, ketoconazole, voriconazole, and caspofungin. In accordance with the manufacturer's instructions, RPMI 1640 agar (15 g in 1,000 ml) supplemented with 20 g glucose per 1,000 ml medium was used in the tests (1). The MICs of natamycin (Natamet; 5% suspension; Sun Pharmaceutical Ind. Ltd., Halol, India), econazole (Aurozole; 2% suspension; Aurolab, Madurai, India), and clotrimazole (Auroclot; 1% suspension; Aurolab, Madurai, India) were determined by the broth microdilution technique NCCLS M38-A (22). Both the Etest and microdilution plates were incubated at 30°C for 72 h. Candida parapsilosis ATCC 22019 was used as the quality control for econazole, clotrimazole, ketoconazole, and amphotericin B during the susceptibility tests. Results obtained for these strains were in accordance with the quality control ranges published previously for these isolates (11, 24). Results of antifungal susceptibility testing toward the nine antifungal drugs tested are shown in Table 1.
TABLE 1.
MICs of antifungal drugs toward Aspergillus nomius strain 823/07
| Assay and antifungal | MIC (μg ml−1) |
|---|---|
| Etest | |
| Amphotericin B | 1 |
| Fluconazole | >256 |
| Ketoconazole | 1 |
| Itraconazole | 4 |
| Voriconazole | 0.125 |
| Caspofungin | 0.25 |
| Broth microdilution | |
| Natamycin | 128 |
| Econazole | 2 |
| Clotrimazole | 1 |
Within the genus Aspergillus, Aspergillus flavus is the predominant etiological agent of keratomycosis (19, 29). A recent paper reported a corneal ulcer due to Aspergillus tamarii (15), suggesting that members of Aspergillus section Flavi other than A. flavus may also be potential causative agents of mycotic keratitis.
Aspergillus nomius Kurtzman, Horn & Hesseltine is morphologically a highly variable species which is difficult to classify by conventional criteria (8, 17). Isolates of this species can produce variously sized sclerotia including the originally described indeterminate ones considered characteristic of this species (18), as well as S-type sclerotia (6).
As an aflatoxin-producing member of Aspergillus section Flavi, A. nomius can convert sterigmatocystin to aflatoxin. While A. flavus normally produces only B-type aflatoxins, A. nomius is able to produce both series B (B1 and B2) and G (G1 and G2) aflatoxins, similarly to Aspergillus parasiticus (5). A recent study of soil samples from Thailand demonstrated that A. nomius is more widespread than may be commonly thought; it can be the predominant aflatoxin-producing Aspergillus species at certain geographic locations and must be considered a potential etiological agent of aflatoxin contamination events due to its ability to produce large quantities of aflatoxins (6).
A. nomius can be distinguished from other members of Aspergillus section Flavi by a number of molecular techniques (3, 4, 7, 8, 16-18, 20, 21, 30), including sequence analysis of the ITS regions (6, 27), as was done in this study. It was hypothesized that A. nomius diverged from a common ancestor prior to the divergence of A. flavus (5, 7). Phylogenetic analyses based on coding sequences of the aflatoxin pathway regulatory gene aflR and the aflJ-aflR intergenic sequence suggested that A. nomius is a diverse paraphyletic assemblage likely to contain several species (7).
A. nomius shows a cosmopolitan distribution (4, 6, 7, 9, 13, 14, 16-18, 23, 25, 26, 28), including previous isolation from red soil in India (20); thus, the mud falling into the eye of the patient can be considered the possible source of the infection. The fact that the patient missed scheduled postoperative follow-up visits possibly contributed to the complications. It is uncertain whether the repeated episodes of scleral involvement were due to the spread of infection from the involved areas as noted during surgery or to recurrence of infection due to poor compliance. However, since this is the first such reported case of A. nomius infection, all possibilities remain hypothetical.
To our knowledge, the presented case of fungal keratitis is the first report on an ocular infection caused by A. nomius and, furthermore, the first known case of human disease with the involvement of this species from Aspergillus section Flavi.
Nucleotide sequence accession numbers.
The GenBank accession numbers for the sequences of the case isolate are GQ221261 (ITS), GQ221262 (β-tubulin), and GQ221263 (calmodulin).
Acknowledgments
This work was supported by the Indian National Science Academy and the Hungarian Academy of Sciences within the frames of the Indo-Hungarian bilateral exchange program No.IA/INSA-HAS Project/2007 and by the intergovernmental project DST-TéT OMFB-00285/2008. L.K. is a grantee of the János Bolyai Research Scholarship.
Footnotes
Published ahead of print on 26 August 2009.
REFERENCES
- 1.AB Biodisk. 1999. Etest technical guide 10. Antifungal susceptibility testing of moulds. AB Biodisk, Solna, Sweden.
- 2.Altschul, S. F., W. Gish, W. Miller, E. W. Myers, and D. J. Lipman. 1990. Basic local alignment search tool. J. Mol. Biol. 215:403-410. [DOI] [PubMed] [Google Scholar]
- 3.Chang, P.-K., D. Bhatnagar, T. E. Cleveland, and J. W. Bennett. 1995. Sequence variability in homologs of the aflatoxin pathway gene aflR distinguishes species in Aspergillus section Flavi. Appl. Environ. Microbiol. 61:40-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Egel, D. S., P. J. Cotty, and K. S. Elias. 1994. Relationships among isolates of Aspergillus sect. Flavi that vary in aflatoxin production. Phytopathology 84:906-912. [Google Scholar]
- 5.Ehrlich, K. C., P. K. Chang, J. Yu, and P. J. Cotty. 2004. Aflatoxin biosynthesis cluster gene cypA is required for G aflatoxin formation. Appl. Environ. Microbiol. 70:6518-6524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ehrlich, K. C., K. Kobbeman, B. G. Montalbano, and P. J. Cotty. 2007. Aflatoxin-producing Aspergillus species from Thailand. Int. J. Food Microbiol. 114:153-159. [DOI] [PubMed] [Google Scholar]
- 7.Ehrlich, K. C., B. G. Montalbano, and P. J. Cotty. 2003. Sequence comparison of aflR from different Aspergillus species provides evidence for variability in regulation of aflatoxin production. Fungal Genet. Biol. 38:63-74. [DOI] [PubMed] [Google Scholar]
- 8.Ehrlich, K. C., J. Yu, and P. J. Cotty. 2005. Aflatoxin biosynthesis gene clusters and flanking regions. J. Appl. Microbiol. 99:518-527. [DOI] [PubMed] [Google Scholar]
- 9.Feibelman, T. P., P. J. Cotty, M. A. Doster, and T. Michailides. 1998. A morphologically distinct strain of Aspergillus nomius. Mycologia 90:618-623. [Google Scholar]
- 10.Glass, N. L., and G. C. Donaldson. 1995. Development of primer sets designed for use with the PCR to amplify conserved genes from filamentous ascomycetes. Appl. Environ. Microbiol. 61:1323-1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guinet, R., D. Nerson, F. de Closets, J. Dupouy-Camet, L. Kures, M. Marjollet, J. L. Poirot, A. Ros, J. Texier-Maugein, and P. J. Volle. 1988. Collaborative evaluation in seven laboratories of a standardized micromethod for yeast susceptibility testing. J. Clin. Microbiol. 26:2307-2312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hong, S. B., H. S. Cho, H. D. Shin, J. C. Frisvad, and R. A. Samson. 2006. Novel Neosartorya species isolated from soil in Korea. Int. J. Syst. Evol. Microbiol. 56:477-486. [DOI] [PubMed] [Google Scholar]
- 13.Ito, Y., S. W. Peterson, and T. Goto. 1998. Isolation and characterization of Aspergillus nomius from Japanese soil and silk worm excrement. Mycotoxins 46:9-15. [Google Scholar]
- 14.Kenjo, T., Y. Ishide, K. Aoyama, and M. Ichinoe. 2007. Fungal population and distribution of aflatoxigenic fungi in commercial almond powder products. Shokuhin Eiseigaku Zasshi 48:90-96. (In Japanese.) [DOI] [PubMed] [Google Scholar]
- 15.Kredics, L., J. Varga, S. Kocsubé, I. Dóczi, R. A. Samson, R. Rajaraman, V. Narendran, M. Bhaskar, C. Vágvölgyi, and P. Manikandan. 2007. Case of keratitis caused by Aspergillus tamarii. J. Clin. Microbiol. 45:3464-3467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kumeda, Y., and T. Asao. 1996. Single-strand conformation polymorphism analysis of PCR-amplified ribosomal DNA internal transcribed spacers to differentiate species of Aspergillus section Flavi. Appl. Environ. Microbiol. 62:2947-2952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumeda, Y., and T. Asao. 2001. Heteroduplex panel analysis, a novel method for genetic identification of Aspergillus section Flavi strains. Appl. Environ. Microbiol. 67:4084-4090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kurtzman, C. P., B. W. Horn, and C. W. Hesseltine. 1987. Aspergillus nomius, a new aflatoxin-producing species related to Aspergillus flavus and Aspergillus tamarii. Antonie van Leeuwenhoek 53:147-158. [DOI] [PubMed] [Google Scholar]
- 19.Manikandan, P., I. Dóczi, S. Kocsubé, J. Varga, T. M. Németh, Z. Antal, C. Vágvölgyi, M. Bhaskar, and L. Kredics. 2008. Aspergillus species in human keratomycosis, p. 293-328. In J. Varga and R. Samson (ed.), Aspergillus in the genomic era. Wageningen Academic Publishers, Wageningen, The Netherlands.
- 20.Moody, S. F., and B. M. Tyler. 1990. Restriction enzyme analysis of mitochondrial DNA of the Aspergillus flavus group: A. flavus, A. parasiticus, and A. nomius. Appl. Environ. Microbiol. 56:2441-2452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moody, S. F., and B. M. Tyler. 1990. Use of nuclear DNA restriction fragment length polymorphism to analyze the diversity of the Aspergillus flavus group: A. flavus, A. parasiticus, and A. nomius. Appl. Environ. Microbiol. 56:2453-2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Committee for Clinical Laboratory Standards. 2002. Reference method for broth dilution antifungal susceptibility testing of filamentous fungi; approved standard. NCCLS document M38-A. NCCLS, Wayne, PA.
- 23.Olsen, M., P. Johnsson, T. Möller, R. Paladino, and M. Lindblad. 2008. Aspergillus nomius, an important aflatoxin producer in Brazil nuts? World Mycotoxin J. 1:123-126. [Google Scholar]
- 24.Pfaller, M. A. M. Bale, B. Buschelman, M. Lancaster, A. Espinel-Ingroff, J. H. Rex, and M. G. Rinaldi. 1994. Selection of candidate quality control isolates and tentative quality control ranges for in vitro susceptibility testing of yeast isolates by National Committee for Clinical Laboratory Standards proposed standard methods. J. Clin. Microbiol. 32:1650-1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pitt, J. I., A. D. Hocking, K. Bhudhasamai, B. F. Miscamble, K. A. Wheeler, and P. Tanboon-Ek. 1993. The normal mycoflora of commodities from Thailand. 1. Nuts and oilseeds. Int. J. Food Microbiol. 20:211-226. [DOI] [PubMed] [Google Scholar]
- 26.Razzaghi-Abyaneh, M., M. Shams-Ghahfarokhi, A. Allameh, A. Kazeroon-Shiri, S. Ranjbar-Bahadori, H. Mirzahoseini, and M. B. Rezaee. 2006. A survey on distribution of Aspergillus section Flavi in corn field soils in Iran: population patterns based on aflatoxins, cyclopiazonic acid and sclerotia production. Mycopathologia 161:183-192. [DOI] [PubMed] [Google Scholar]
- 27.Rigó, K., J. Varga, B. Tóth, J. Téren, Á. Mesterházy, and Z. Kozakiewicz. 2002. Evolutionary relationships within Aspergillus section Flavi based on sequences of the intergenic transcribed spacer regions and the 5.8S rRNA gene. J. Gen. Appl. Microbiol. 48:9-16. [DOI] [PubMed] [Google Scholar]
- 28.Saito, M., O. Tsuruta, P. Siriacha, S. Kawasugi, and M. Manabe. 1989. Atypical strains of Aspergillus flavus isolated in maize fields. Jpn. Agric. Res. Q. 23:151-154. [Google Scholar]
- 29.Thomas, P. A. 2003. Current perspectives on ophthalmic mycoses. Clin. Microbiol. Rev. 16:730-797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang, L., K. Yokoyama, H. Takahasi, N. Kase, Y. Hanya, K. Yashiro, M. Miyaji, and K. Nishimura. 2001. Identification of species in Aspergillus section Flavi based on sequencing of the mitochondrial cytochrome b gene. Int. J. Food Microbiol. 71:75-86. [DOI] [PubMed] [Google Scholar]
- 31.White, T. J., T. Bruns, S. Lee, and J. Taylor. 1990. Amplification and direct sequencing of fungal ribosomal RNA genes for phylogenetics, p. 315-322. In M. H. Innes, D. H. Gelfand, J. J. Sninsky, and T. J. White (ed.), PCR protocols. Academic Press, San Diego, CA.