Abstract
Previous research has identified a wide range of indicators of social isolation that pose health risks, including living alone, having a small social network, infrequent participation in social activities, and feelings of loneliness. However, multiple forms of isolation are rarely studied together, making it difficult to determine which aspects of isolation are most deleterious for health. Using population-based data from the National Social Life, Health, and Aging Project, we combine multiple indicators of social isolation into scales assessing social disconnectedness (e.g., small social network, infrequent participation in social activities) and perceived isolation (e.g., loneliness, perceived lack of social support). We examine the extent to which social disconnectedness and perceived isolation have distinct associations with physical and mental health among older adults. Results indicate that social disconnectedness and perceived isolation are independently associated with lower levels of self-rated physical health. However, the association between disconnectedness and mental health may operate through the strong relationship between perceived isolation and mental health. We conclude that health researchers need to consider social disconnectedness and perceived isolation simultaneously.
Health risks associated with social isolation have been compared in magnitude to the well-known dangers of smoking cigarettes and obesity (House 2001). Individuals who lack social connections or report frequent feelings of loneliness tend to suffer higher rates of morbidity and mortality (Brummett et al. 2001; Seeman 2000; Uchino, Cacioppo, and Kiecolt-Glaser 1996), as well as infection (Cohen et al. 1997; Pressman et al. 2005), depression (Heikkinen and Kauppinen 2004), and cognitive decline (Barnes et al. 2004; Wilson et al. 2007). Yet, compared to health behaviors such as smoking and obesity, much less is known about how and why social isolation affects health (Cacioppo and Hawkley 2003; House, Landis, and Umberson 1988).
One problem is that most research on social connectedness and health focuses on only one or two measures of social isolation, often due to data limitations (House 2001). Across a range of studies, a number of indicators of isolation have been associated with worse health, such as living alone, having a small social network, low participation in social activities, a perceived lack of social support, and feelings of loneliness (Berkman and Syme 1979; Dean et al. 1992; Hawkley et al. 2006; Krause 1987; Thoits and Hewitt 2001). But when these aspects of social isolation are examined separately, it is difficult to identify the “active ingredient” in social isolation that leads to its deleterious effects on health (House 2001).
A second problem is that disciplinary differences have led to a disjuncture in research on social isolation and health, with psychological research focusing on subjective aspects of isolation (Cacioppo and Hawkley 2003) and sociological research emphasizing social integration (House et al. 1988). As a result, the relative contributions of subjective aspects of isolation, such as loneliness and perceived support, are rarely considered alongside social disconnectedness and social inactivity. This leaves a number of important questions unanswered. For example, does the link between social disconnectedness and health actually reflect the impact of loneliness? Or do social disconnectedness and feelings of loneliness separately diminish health?
This article builds upon the large body of research that has examined the relationship between social isolation and health by considering two forms of isolation at once: social disconnectedness, marked by a lack of social relationships and low levels of participation in social activities, and perceived isolation, defined by loneliness and a perceived lack of social support. We use data from the National Social Life, Health, and Aging Project (NSHAP), a population-based survey of 3,005 community-residing older adults, ages 57 to 85, conducted in 2005−2006. The breadth of data collected in this study allows the combination of a variety of indicators of isolation into two reliable scales capturing social disconnectedness and perceived isolation. Using these scales, we compare the contributions of social disconnectedness and perceived isolation to physical and mental health.
While social isolation has been linked to worse health across all age groups (House et al. 1988), our study focuses on older adults. The health risks posed by social isolation may be particularly severe for older adults (Cacioppo and Hawkley 2003; Tomaka, Thompson, and Palacios 2006), especially as they are likely to face stressful life course transitions, health problems, and disabilities (Brummett et al. 2001). Another reason to examine social disconnectedness and perceived isolation among older adults is the fact that older adults may be uniquely able to optimize social relationships or adjust expectations so that low levels of social connectedness do not precipitate feelings of loneliness or perceived deficits in support (Lang and Carstensen 1994; Schnittker 2007). If social disconnectedness and perceived isolation are especially decoupled among older adults, then the extent to which social disconnectedness and perceived isolation pose unique risks for physical and mental health should be easily observed within this age group.
CONCEPTUALIZING SOCIAL ISOLATION
Social isolation has been a central concern in research on health, but indicators of isolation vary widely both across and within disciplines. Sociologists interested in family and living arrangements have focused on the negative health effects of living alone (Dean et al. 1992; Hughes and Gove 1981) and being unmarried (Lillard and Waite 1995; Ross 1995). Social network research has demonstrated health risks associated with having a small social network (Berkman and Syme 1979; Seeman et al. 1994), infrequent contact with network members (Brummett et al. 2001), and a lack of social network diversity (Barefoot et al. 2005). Sociologists have also identified low participation in social activities, particularly volunteering and religious attendance, as a health risk (Benjamins 2004; Thoits and Hewitt 2001). Perceived social support has been linked to physical and mental health by both sociologists and psychologists (Blazer 1982; Krause 1987; Lin, Ye, and Ensel 1999). Finally, a large body of psychological research has demonstrated a robust association between loneliness and worse health, including cardiovascular disease, inflammation, and depression (Cacioppo et al. 2006; Hawkley et al. 2006; Steptoe et al. 2004). The risks associated with social isolation, in one form or another, are clear. However, the variety and complexity of individuals’ social worlds can scarcely be captured with only one or two measures. It is therefore difficult to determine from previous research whether various aspects of social isolation combine or work separately to influence health outcomes.
In efforts to consolidate multiple measures of isolation, several authors have previously identified central components of isolation (Gierveld and Hagestad 2006; Lin et al. 1999; van Tilburg et al. 1998). For example, van Baarsen et al. (2001) distinguish between social loneliness, as the lack of integration and companionship, and emotional loneliness, as the lack of an attachment figure. Gierveld and Hagestad (2006) similarly contrast isolation (as the opposite of integration) with loneliness (as the opposite of embeddedness). Following these distinctions, and building from the disciplinary approaches of sociology and psychology, we suggest two forms of social isolation: social disconnectedness and perceived isolation.
Social disconnectedness can be characterized by a lack of contact with others. It is indicated by situational factors, like a small social network, infrequent social interaction, and lack of participation in social activities and groups. Perceived isolation, on the other hand, can be characterized by the subjective experience of a shortfall in one's social resources such as companionship and support. Feelings of loneliness and not belonging, for example, indicate a perceived inadequacy of the intimacy or companionship of one's interpersonal relationships compared to the relationships that one would like to have (van Baarsen et al. 2001).
Distinguishing between social disconnectedness and perceived isolation recognizes an important point about how individuals manage their social lives. For some individuals, the perception of social resources is entirely unrelated to the actual amount of time spent alone. Loneliness is only weakly correlated with social network size and frequency of interaction with network members (Fees, Martin, and Poon 1999; Hawkley et al. 2003; Hughes et al. 2004). In fact, the degree to which one perceives himself as isolated is informed by personality and other individual-level characteristics, such as neuroticism (Stokes 1985) and cognitive schemas (Lakey and Cassady 1990). Furthermore, some research suggests that just under half of the variation in loneliness across individuals is heritable (Boomsma et al. 2005). Therefore, we need to assess both concepts together in order to account for the degree to which perceptions of social resources may not reflect actual social situations.
Forms of Social Isolation among Older Adults
Older adults face a number of challenges to remaining socially connected, but recent research indicates great heterogeneity in age-related changes in social connectedness and satisfaction with social life. Life course changes, such as retirement and bereavement, may lead to a loss of social roles (Ferraro 1984; Weiss 2005), and health problems may limit participation in social activities (Li and Ferraro 2006; Thoits and Hewitt 2001). However, social participation and volunteering increase with age, partially due to increased free time brought by retirement (Cornwell, Laumann, and Schumm 2008; Mutchler, Burr, and Caro 2003). Other aspects of social connectedness have nonlinear trajectories with age. Frequency of contact with network members is lowest among the middle-old (Cornwell et al. 2008), and loneliness is greatest among middle-aged adults (Carstensen, Isaacowitz, and Charles 1999).
The variety in age-related trajectories of social relationships means that increasing age does not necessarily bring social isolation. And, social connectedness, support, and loneliness may not be closely linked among older adults. Even when nonkin ties decline, many older adults cultivate closer relationships with those who remain in their networks (Lang and Carstensen 1994), and report relatively high levels of perceived support (Shaw et al. 2007; van Tilburg et al. 1998). Age-related adjustments in expectations may also contribute to older adults’ increasing satisfaction with their relationships despite diminishing network size and frequency of interaction (Schnittker 2007). As a result, older adults’ perceptions of their social resources and relationships may not reflect their actual levels of connectedness (Schnittker 2007; Shaw et al. 2007; van Baarsen et al. 2001; van Tilburg et al. 1998).
Older adults are more likely to experience bereavement and encounter health problems that increase their need for social support and companionship, so the health-damaging aspects of social isolation can be particularly deleterious at older ages (Cacioppo et al. 2006; Heikkinen and Kauppinen 2004; House et al. 1988). Older adults who experience one or another aspect of social isolation are at greater risk for all-cause mortality, increased morbidity, diminished immune function, depression, and cognitive decline (Barnes et al. 2004; Brummett et al. 2001; House 2001; Seeman 2000; Uchino et al. 1996). Therefore, it is important that we understand the mechanisms through which aspects of isolation may present health risks for older adults, in particular.
HEALTH-RELATED CONSEQUENCES OF SOCIAL DISCONNECTEDNESS AND PERCEIVED ISOLATION
Previous research on social isolation across age groups points to a variety of mechanisms through which various aspects of isolation may affect health. Some mechanisms link social disconnectedness and perceived isolation to worse health outcomes in similar ways. For example, both social connectedness and the perception of available support buffer the deleterious effects of stress exposure (Thoits 1995). Socially connected individuals may receive instrumental support from network members or co-residents, which may assist in active coping and ultimately reduce stress (Waite and Hughes 1999). Similarly, individuals who rarely experience loneliness and those who perceive high levels of social support tend to have more active coping strategies and greater self-esteem and sense of control (Cornman et al. 2003; Ernst and Cacioppo 1999), each of which can diminish the effects of stress (Pearlin 1989; and see Steptoe et al. 2004).
However, evidence of other mechanisms that link one or the other form of isolation to health outcomes suggests that social disconnectedness and perceived isolation may separately affect health. For example, social connectedness, indicated by one's social network and level of social participation, can provide access to material resources such as information, transportation, financial loans, or emotional support (Ellison and George 1994; Haines and Hurlbert 1992; Lin 2001). Aspects of social connectedness such as integration within dense social networks may also promote healthy behaviors, leading to better health outcomes (Kinney et al. 2005; Rook and Ituarte 1999; Umberson 1987), although stressful relationships have been linked to worse health outcomes (Umberson et al. 2006; Wickrama et al. 2001), and health-risk behaviors such as smoking, risky sexual behavior, and poor diet can be diffused through social networks (Christakis and Fowler 2007; Latkin et al. 2003). Nevertheless, on average, the positives of social connectedness seem to outweigh the negatives.
Aspects of perceived isolation are often linked to health outcomes through different mechanisms. The modification of health-related behaviors has not been found to account for the link between loneliness or the perception of a lack of social support and worse health outcomes (Hawkley et al. 2003; Seeman 2000; Steptoe et al. 2004). However, a large body of research suggests a potentially strong correlation between perceived isolation and mental health problems, especially depression (Weeks et al. 1980). Loneliness is a key predictor of depression among older adults, in particular (Cacioppo et al. 2006; Heikkinen and Kauppinen 2004). Similarly, perceived social support is more important for mental health outcomes than indicators of social connectedness, such as received support (Krause 1987) and network size (Brummett et al. 2001). To the extent that mental health problems put individuals at risk for physical health problems (Mehta, Yaffe, and Covinsky 2002; Sorkin, Rook, and Lu 2002), perceived isolation may affect physical health through its impact on mental health.
Another possibility is that perceived isolation mediates the relationship between social disconnectedness and health. Social connectedness and social participation may directly influence loneliness and perceived social support. Although many aspects of social connectedness are only weakly or moderately correlated with loneliness (Hawkley et al. 2003), some losses of social ties, such as widowhood, are associated with increased loneliness among older adults (Koropeckyj-Cox 1998). Little research has examined whether the relationship between social disconnectedness and health can be attributed to perceived isolation.
Overall, separate strands of work focusing on aspects of social disconnectedness and perceived isolation suggest the possibility of different mechanisms through which these two forms of social isolation affect health. We develop and test two overarching hypotheses about these relationships.
Hypothesis 1: Social disconnectedness and perceived isolation are independently associated with health.
The reasoning and mechanisms underlying this hypothesis are outlined above. Alternatively, one might hypothesize that social disconnectedness presents a risk for health only when it results in perceived isolation, which increases stress, decreases self-efficacy, and predicts mental health problems (Cohen 1988; Cornman et al. 2003; Ernst and Cacioppo 1999; Pearlin 1989; Weeks et al. 1980). Thus, our second hypothesis:
Hypothesis 2: Perceived isolation mediates the relationship between social disconnectedness and health.
Evidence in support of either hypothesis would imply that these two forms of isolation are not interchangeable with respect to health. From a practical standpoint, this would suggest that individuals who do not feel isolated at any given level of connectedness fare better than those who are equally connected but perceive themselves as isolated. This would suggest that future research on the health consequences of social isolation could be strengthened by including indicators of both social disconnectedness and perceived isolation.
DATA AND METHODS
We use data from the National Social Life, Health, and Aging Project (NSHAP), a nationally representative population-based study of community-residing older adults. The NSHAP sample was selected from a multi-stage area probability design screened by the Institute for Social Research for the Health and Retirement Study (HRS). The HRS design oversampled by race-ethnicity; NSHAP retained this design and also oversampled by age and gender. From summer 2005 to spring 2006, NSHAP interviewed 3,005 individuals, age 57 to 85, achieving a weighted response rate of 75.5 percent.
Most of the data for the NSHAP study were collected during a two-hour in-home interview. Respondents were also given a questionnaire to complete and return by mail. The study was modularized so that some items were always included in the interview, while other items were included in either the interview or the questionnaire for a randomly-selected subset of respondents. The return rate for the questionnaire was 84 percent. After accounting for questionnaire and item-level non-response, our effective sample size includes 2,910 respondents who have valid data on the self-reported health dependent variables, measures of social isolation, and covariates. Table 1 summarizes the variables included in our analyses.
TABLE 1.
Summary Statistics for Indicators Included in the Social Disconnectedness and Perceived Isolation Scales and Covariates
| Mean or Proportiona | Standard Deviation | N | |
|---|---|---|---|
| Social Disconnectedness (Cronbach's alpha = .73) | −.024 | .625 | 2,910 |
| Social Network Characteristics | |||
| Social network size (range = 0−5, 6 or more) | 3.578 | 1.591 | 2,906 |
| Social network range (number of types of relationships in the network; range = 0,5) | 2.419 | 1.064 | 2,910 |
| Proportion of social network members who live in the household (range = 0,1) | .296 | .306 | 2,843 |
| Average frequency of interaction with network members (range = 0,1 where 0 = the respondent does not contact any alters and 1 = respondent contacts all alters every day) | .578 | .261 | 2,842 |
| Number of Friends | |||
| How many friends would you say you have?” (0 = “none,” 1 = “1 friend,” 2 = “2−3 friends,” 3 = “4−9 friends,” 4 = “10−20 friends,” 5 = “more than 20“) | 3.312 | 1.298 | 2,779 |
| Social Participation | |||
| Frequency of . . . | |||
| Attending meetings of an organized group (from 1 = “never” to 7 = “several times a week“) | 3.662 | 2.150 | 2,431 |
| Socializing with friends and relatives (from 1 = “never” to 7 = “several times a week“) | 5.392 | 1.301 | 2,449 |
| Volunteering (from 1 = “never” to 7 = “several times a week“) | 3.202 | 2.084 | 2,430 |
| Perceived Isolation (Cronbach's alpha = .70) | −.006 | .591 | 2,910 |
| Loneliness | |||
| How often do you . . . (1 = “hardly ever (or never),” 2 = “some of the time,” 3 = “often“) | |||
| Feel that you lack companionship? | 1.406 | .614 | 2,392 |
| Feel left out? | 1.321 | .534 | 2,387 |
| Feel isolated from others? | 1.262 | .507 | 2,394 |
| Perceived Social Support | |||
| How often can you . . . (1 = “often,” 2 = “some of the time,” 3 = “hardly ever (or never)“) | |||
| Open up to members of your family? | 1.682 | .711 | 2,769 |
| Rely on members of your family? | 1.411 | .654 | 2,765 |
| Open up to your friends? | 1.978 | .729 | 2,677 |
| Rely on your friends? | 1.680 | .709 | 2,653 |
| Open up to your spouse or partner? | 1.272 | .539 | 1,999 |
| Rely on your spouse or partner? | 1.160 | .448 | 1,994 |
| Covariates and Dependent Variables | |||
| Age (in decades) | 6.798 | .784 | 2,910 |
| Attended college (1 = at least some college; 0 = no college attendance) | .509 | .499 | 2,910 |
| Co-morbidities (number of chronic conditions ever diagnosed, range = 0, 16)b | 2.163 | 1.526 | 2,910 |
| Depressive symptoms (CES-D-ml) | 9.428 | 3.582 | 2,866 |
| Female | .514 | .500 | 2,910 |
| Married or partnered | .741 | .464 | 2,910 |
| Non-white | .192 | .454 | 2,910 |
| Self-rated mental healthc | |||
| Poor | .017 | – | 49 |
| Fair | .095 | – | 275 |
| Good | .278 | – | 807 |
| Very good | .369 | – | 1,073 |
| Excellent | .243 | – | 706 |
| Self-rated physical healthc | |||
| Poor | .074 | – | 214 |
| Fair | .193 | – | 561 |
| Good | .300 | – | 874 |
| Very good | .311 | – | 905 |
| Excellent | .122 | – | 356 |
Survey-adjusted and weighted to account for the probability of selection, with post-stratification adjustments for non-response.
Conditions included: 1) arthritis; 2) stomach or peptic ulcers; 3) emphysema, bronchitis, or lung disease; 4) asthma; 5) stroke, blood clot, or bleeding in the brain; 6) high blood pressure or hypertension; 7) diabetes or high blood sugar; 8) Alzheimer's disease or other form of dementia; 9) cirrhosis, or serious liver damage; 10) HIV/AIDS; 11) leukemia or polycythemia vera; 12) lymphoma; 13) skin cancer (including melanoma, basal cell carcinoma, and squamous cell carcinoma; 14) cancer, other than skin cancer, leukemia, or lymphoma; 15) poor kidney function; and 16) thyroid problems.
Response proportions and frequencies presented are unweighted.
Social Disconnectedness Scale
Previous research has employed indicators of numerous aspects of isolation, but no single indicator captures the complex nature of social isolation. One of the strengths of the NSHAP data is its variety of social connectedness measures. We construct a social disconnectedness scale based on eight items assessing respondents’ lack of connectedness to other individuals and social groups. The scale has acceptable internal consistency, with an alpha of .73 and moderate to strong item-rest correlations. Two components—social network characteristics (eigenvalue = 2.75) and social participation (eigenvalue = 1.55)—account for about 54 percent of the variance.
Social network characteristics comprise four of the scale items. Social network measures included in NSHAP allow the characterization of respondents’ relationships with other individuals and the networks within which respondents are embedded (see Cornwell et al. 2008). To capture respondents’ social networks, respondents were asked the following question:
From time to time, most people discuss things that are important to them with others. For example, these may include good or bad things that happen to you, problems you are having, or important concerns you may have. Looking back over the last 12 months, who are the people with whom you most often discussed things that were important to you?
First, social network size indicates the number of network members identified by the respondent. Second, the proportion of social network members who live in the household is also considered. A high proportion of network members in the home results in relatively fewer connections with individuals outside the home. Third, social network range indicates the extent to which the respondent is connected to a variety of types of individuals (e.g., spouse, friend, co-worker). Fourth, frequency of contact with network members indicates an individual's exposure to his network members.
The social disconnectedness scale also incorporates the number of friends reported by each respondent. Excluding their spouses and family members, respondents indicated how many “people you consider to be your friends, both your closest friends and people with whom you are pretty good friends.” This question was modularized, so that a random two-thirds of respondents answered the question during the in-person interview, and one-third encountered it in the questionnaire. Mean response does not differ according to the collection mode.
Items assessing the lack of participation in social activities outside of the home are also included in the scale. Respondents were asked how often they volunteer, attend meetings of an organized group, and socialize with friends and family. Each of these items was included in the questionnaire.
The eight variables are standardized, their values are averaged, and the computed scores are reversed so that they indicate disconnectedness rather than connectedness. Scores on the social disconnectedness scale range from −1.30 to 2.34, with a weighted mean of −.02 and standard deviation of .63.
Perceived Isolation Scale
We measured perceived isolation using a scale combining nine items that assess loneliness and perceived (lack of) social support. The perceived isolation scale has acceptable internal consistency (α = .70) and moderate to strong item-rest correlations. About 46 percent of the variance is comprised of two components: loneliness (eigenvalue = 2.02) and perceived social support (eigenvalue = 1.20).
Six of the nine items in the scale are indicators of perceived social support. Regarding social support from one's family, respondents were asked, “How often can you open up to members of your family if you need to talk about your worries?” and “How often can you rely on them for help if you have a problem?” The same two questions were asked about the respondent's friends and spouse or current partner. Questions about social support from family members and friends were modularized so that about two-thirds of respondents were asked the questions during the in-person interview and one-third responded to the questions in the questionnaire. Mean responses do not differ according to collection mode.
Finally, we also include the three-item loneliness scale developed by Hughes et al. (2004). In the questionnaire, respondents were asked, “How often do you feel that you lack companionship?” “How often do you feel left out?” and “How often do you feel isolated from others?”
The perceived isolation scale is constructed by standardizing each of these items and then averaging the scores. Note that 66 respondents do not have scores for perceived isolation because they had missing data on every scale item. Seven of the nine scale items were included in the questionnaire. The two remaining items, asked during the interview, assessed support from a spouse or partner. Therefore, scale scores are missing in cases where a respondent did not return the questionnaire and did not have a spouse or partner. Scores on the scale range from −.98 to 3.63, with a weighted mean of −.01 and a standard deviation of .59. Higher scores indicate greater perceived isolation.
Dependent Variables
Our dependent variables include self-rated measures of physical and mental health status, as well as an indicator of depressive symptoms. Self-rated physical health was assessed using a standard question: “Would you say your health is excellent, very good, good, fair, or poor?” This question is widely used in epidemiological and population-based survey research. Although it does not directly define health, individuals’ self-ratings of their overall health have been shown in numerous studies to be predictive of mortality (Idler and Benyamini 1997). The effectiveness of the self-rated health measure may stem, in part, from the fact that it reflects physical health status, symptoms, function, and health behaviors (Fayers and Sprangers 2002), as well as emotional, spiritual, or psychological characteristics that may be important for health trajectories (Idler, Hudson, and Leventhal 1999; Molarius and Janson 2002). The measure is reliable across age, gender, and racial and ethnic groups (Finch et al. 2002; Johnson and Wolinsky 1994).
We also use a single item capturing self-rated mental health. Following the self-rated physical health question, respondents were asked, “What about your emotional or mental health? Is it excellent, very good, good, fair, or poor?” This measure has not been validated against clinical assessments of mental health disorders, but the distribution of NSHAP responses mirrors that found in recent research (Mulvaney-Day, Alegria, and Sribney 2007). Both self-rated physical health and self-rated mental health are coded so that higher values indicate better health.
Finally, we perform analyses predicting depressive symptomatology using a shortened 11-item version of the Center for Epidemiological Studies Depression Scale (CES-D) (Radloff 1977) to assess the presence of depressive symptoms.1 Respondents were asked to indicate how often they experienced a number of feelings during the past week, including (1) “I did not feel like eating; my appetite was poor”; (2) “I felt depressed”; (3) “I felt that everything I did was an effort”; (4) “My sleep was restless”; (5) “I was happy”; (6) “I felt lonely”; (7) “People were unfriendly”; (8) “I enjoyed life”; (9) “I felt sad”; (10) “I felt that people disliked me”; and (11) “I could not get ‘going.’” Responses ranged from “rarely or none of the time” to “some of the time,” “occasionally,” and “most of the time.”
One item on the shortened CES-D asks whether respondents felt lonely during the past week, and loneliness is a component of the perceived isolation scale. In order to decrease the overlap between these two scales, we remove the loneliness item from the CES-D scale. Following Cacioppo et al. (2006), we refer to this revised CES-D, minus the loneliness item, as the CES-D-ml. This nominally decreases the scale's internal consistency reliability (from α = .80 to α = .78). Scale scores represent a sum of the responses (ranging from 0 to 3) to each item, so the scale ranges from 0 to 30, with higher scores indicating more depressive symptoms.2
Covariates
In predicting physical and mental health outcomes, we control for respondent's age and, using a series of dummy variables, gender (1 = female), minority status (1 = nonwhite), college attendance (1 = completed at least some college), and marital/partnership status (1 = married or in a current romantic partnership). In analyses of mental health, we also control for prior diagnosis of physical health problems since poor physical health is a key risk factor for depression in older adults (Geerlings et al. 2000). To control for physical condition, we employ a single-item indicator based on a modified, questionnaire-appropriate format of the Charlson Co-morbidity Index (Charlson et al. 1987). Respondents were asked whether a doctor has ever told them that they have any of a number of conditions, including hypertension, diabetes, lung disease, Alzheimer's disease, and cancer. The total number of conditions reported provides a rough measure of physical health status.
Analytic Strategy
Because self-rated physical and mental health are both ordinal, we use ordered logistic regression analysis to examine the effects of disconnectedness and perceived isolation on these outcomes. Both variables consist of j ordered categories, represented by the integers 1, 2, ... , j. Ordered logistic regression models the cumulative probability of being above a given category, as a linear function of the predictors. If β is the vector of ordered-logit regression coefficients, then exp[βK] is a vector of odds ratios, or proportionate changes associated with a one-unit increase in χik, the kth explanatory variable, in the odds of being above category j. One can interpret the coefficients in conventional terms; a positive regression coefficient means that an increase in the value of an independent variable is associated with better self-rated health. Coefficients can be used to assess statistical significance, but they are not directly interpretable on the self-rated health scale. In the analysis of depressive symptoms, we use OLS regression to estimate the effects of disconnectedness and perceived isolation because the CES-D scale is typically analyzed as an interval-ratio variable. All regression models are survey-adjusted and weighted to account for probability of selection and nonresponse.
Because the NSHAP data are cross-sectional, causal inference from regression analyses should be made with caution. It is possible, and perhaps likely, that social disconnectedness and perceived isolation are caused by physical and mental health conditions. Individuals in poor health may be less likely than healthy individuals to maintain social ties (Li and Ferraro 2006; Litwin 2003) and to positively assess their relationships and available social support (Cornman et al. 2003). To the extent that reverse causation exists, regression analysis will produce biased estimates of the effects of isolation on health. Our models are not intended to provide conclusive evidence of the magnitude of the effects of objective and subjective isolation, but to assess whether these two forms of social isolation have distinct linkages with various health outcomes.
RESULTS
A lack of social connectedness is not always accompanied by feelings of loneliness and isolation. In fact, the correlation between social disconnectedness and perceived isolation is only weak to moderate in strength (r = .25, p < .001) within this population-based sample of older adults. Since objective and subjective isolation are conceptually distinct and are not strongly correlated, it is possible that they are independently associated with health. We next examine our two hypotheses regarding their independent associations with, and relative importance for, three different health outcomes.
Self-Rated Physical Health
Table 2 presents results from ordered logistic regression analyses predicting self-rated physical health. Significant associations between sociodemographic characteristics and self-rated health presented in the first model are consistent with previous research (Johnson and Wolinsky 1994). Social disconnectedness and perceived isolation are introduced in models 2 and 3, respectively. As expected, both forms of isolation are associated with worse health.
TABLE 2.
Ordered Logistic Regressions of Self-Rated Physical Healtha on Social Disconnectedness, Perceived Isolation, and Covariatesb
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Age (in decades) | −.165** | −.169** | −.144* | −.152* |
| (.056) | (.056) | (.059) | (.060) | |
| Attended college | .627*** | .511*** | .604*** | .515*** |
| (.101) | (.105) | (.104) | (.107) | |
| Female | .147 | .066 | .084 | .030 |
| (.080) | (.083) | (.075) | (.079) | |
| Non-white | −.568*** | −.462*** | −.518*** | −.443*** |
| (.111) | (.108) | (.114) | (.110) | |
| Spouse/partner | .435*** | .454*** | .381*** | .406*** |
| (.090) | (.090) | (.090) | (.090) | |
| Social disconnectedness | −.415*** | −.335*** | ||
| (.070) | (.073) | |||
| Perceived isolation | −.434*** | −.359*** | ||
| (.068) | (.070) | |||
| Intercepts | ||||
| 1 | 3.263*** | 3.376*** | 3.226*** | 3.323*** |
| 2 | 1.697*** | 1.798*** | 1.642** | 1.732** |
| 3 | .337 | .420 | .263 | .343 |
| 4 | −1.467** | −1.401** | −1.555** | −1.488** |
| Unweighted N | 2910 | 2910 | 2910 | 2910 |
| F | 19.15*** | 23.33*** | 16.32*** | 18.49*** |
| (df) | (5,46) | (6,45) | (6,45) | (7,44) |
p < .05
p < .01
p < .001 (two-tailed tests)
Self-rated health is coded so that higher values indicate better health.
Estimates presented are survey-adjusted and weighted for the probability of selection with post-stratification adjustments for non-response. Standard errors are presented in parentheses.
Model 4 considers both social disconnectedness and perceived isolation simultaneously.3 Results support our first hypothesis that both disconnectedness and perceived isolation are independently associated with poorer self-rated health.4 An increment of one standard deviation in social disconnectedness is associated with about 30 percent lower odds of rating one's health above a given category (e−.335 = .715). Similarly, older adults whose perceived isolation score is one standard deviation above average face 30 percent lower odds of being above any category of self-rated health (e−.359 = .698).
It is worth noting that disconnectedness and perceived isolation account for part of the health-related advantages of college attendance and marriage. Partnered individuals report better health partially because they perceive themselves to be less isolated (t = 4.13, p < .001), and older adults who attended college may fare better with respect to physical health because they are more socially connected (t = 15.06, p < .001) and perceive themselves as less isolated (t = 5.25, p < .001) than those who did not attend college. Additionally, over 20 percent of minorities’ health disadvantage in model 1 may be attributed to their higher levels of disconnectedness (t = 12.70, p < .001) and perceived isolation (t = 5.28, p < .001).
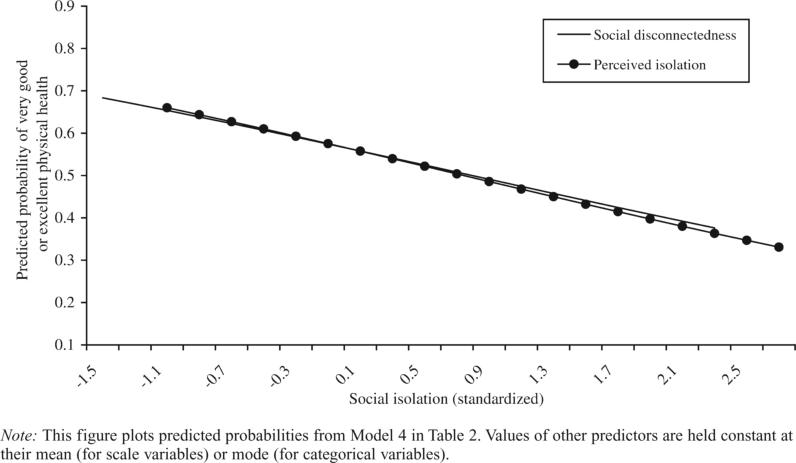
The relationships between social disconnectedness and physical health and between perceived isolation and physical health seem to be distinct and additive. As Figure 1 illustrates, higher levels of both social disconnectedness and perceived isolation are associated with worse physical health, based on the fourth model in Table 2. Older adults who are socially connected or perceive high levels of support and companionship from others have a nearly 70 percent chance of reporting very good or excellent health (see Figure 1). However, those who report extreme social disconnectedness or perceived isolation have only a 40 percent chance of reporting very good or excellent health.
FIGURE 1.
Predicted Probabilities of Very Good or Excellent Physical Health, According to Levels of Social Disconnectedness and Perceived Isolation
Self-Rated Mental Health
Table 3 presents ordered logistic regression analyses predicting self-rated mental health. Net of a number of sociodemographic covariates, social disconnectedness and perceived isolation are each negatively related to self-rated mental health, as shown in the second and third models. Perceived isolation, however, has a decidedly stronger association than social disconnectedness with mental health.
TABLE 3.
Ordered Logistic Regressions of Self-Rated Mental Healtha on Social Disconnectedness, Perceived Isolation, and Covariatesb
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Age (in decades) | −.078 | −.079 | −.047 | −.048 |
| (.056) | (.055) | (.060) | (.060) | |
| Attended college | .620*** | .526*** | .598*** | .552*** |
| (.098) | (.100) | (.106) | (.108) | |
| Female | −.186* | −.259** | −.304** | −.335*** |
| (.078) | (.079) | (.083) | (.083) | |
| Non-white | −.430** | −.341* | −.357* | −.316* |
| (.148) | (.143) | (.161) | (.156) | |
| Spouse/partner | .167 | .175 | .042 | .052 |
| (.095) | (.098) | (.107) | (.108) | |
| Co-morbidities | −.189*** | −.192*** | −.192*** | −.194*** |
| (.024) | (.025) | (.025) | (.025) | |
| Social Disconnectedness | −.359*** | −.187* | ||
| (.079) | (.079) | |||
| Perceived Isolation | −.800*** | −.755*** | ||
| (.059) | (.062) | |||
| Intercepts | ||||
| 1 | 4.906*** | 4.996*** | 4.973*** | 5.013*** |
| 2 | 2.987*** | 3.067*** | 3.008*** | 3.046*** |
| 3 | 1.304** | 1.367** | 1.255* | 1.288* |
| 4 | −.439 | −.390 | −.555 | −.525 |
| Unweighted N | 2910 | 2910 | 2910 | 2910 |
| F | 20.19*** | 19.00*** | 47.05*** | 43.07*** |
| (df) | (6,45) | (7,44) | (7,44) | (8,43) |
Note:
p < .05
p < .01
p < .001 (two-tailed tests)
Higher values indicate better mental health.
Estimates are survey-adjusted and weighted for probability of selection with post-stratification adjustments for non-response. Standard errors are presented in parentheses.
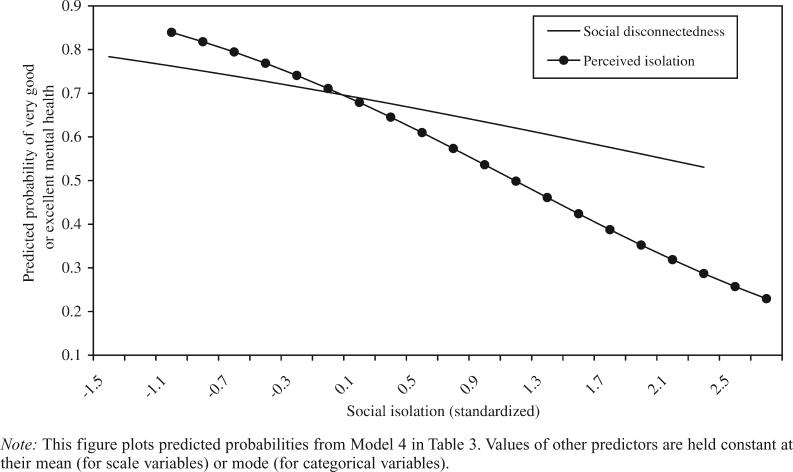
Model 4 assesses the roles of social disconnectedness and perceived isolation together. These results deserve attention for a couple of reasons. The strong relationship between perceived isolation and mental health is in line with previous research suggesting that loneliness is particularly deleterious for mental health (Cacioppo et al. 2006; Heikkinen and Kauppinen 2004). An increase of one standard deviation on the perceived isolation scale is associated with about a one-half reduction in the odds of having better mental health (e−.755 = .470).
However, the relationship between social disconnectedness and mental health in model 4 is noticeably reduced from that in model 2. The health risks of disconnectedness appear to operate through the strong, negative association between perceived isolation and mental health. This provides evidence in support of our second hypothesis that perceived isolation may mediate the relationship between social disconnectedness and health.
Figure 2, estimated from model 4, illustrates that when we control for perceived isolation, social disconnectedness has only a slight association with the probability of having very good or excellent mental health. Individuals who do not perceive themselves to be isolated have a nearly 85 percent chance of having very good or excellent mental health. But those who feel extremely isolated have only about a 25 percent chance of claiming very good or excellent mental health.
FIGURE 2.
Predicted Probabilities of Very Good or Excellent Mental Health, According to Levels of Social Disconnectedness and Perceived Isolation
Two details related to the analysis of self-rated mental health are worth noting here. First, when we control for both social disconnectedness and perceived isolation, women's mental health disadvantage nearly doubles. Previous research suggests a stronger link between loneliness and mental illness among women compared with men (Cacioppo et al. 2006). Following this, we added multiplicative terms for interactions between gender and social disconnectedness and perceived isolation, but they were not significant. Further work is needed to examine the reasons for the stronger relationship between gender and mental health that emerges after we account for perceived isolation.
Supplementary analyses testing the proportional odds assumption suggest that the relationship between social disconnectedness and mental health may be more complex than that which is shown in Table 3. In fact, the relationship between social disconnectedness and self-rated mental health in model 4 varies across the levels of self-rated mental health, so ordered logistic regression may be too restrictive for this analysis. To observe the differences in the parameterizations for social disconnectedness, we constructed a partial proportional odds model constraining all independent variables, except disconnectedness, to meet the parallel lines assumption across the five categories of self-rated mental health (Williams 2006). The negative relationship between social disconnectedness and self-rated mental health is significantly stronger when we examine worse levels of mental health (e.g., for better than “poor” mental health, (b = −.81, p < .01), compared to better than “good” (b = −.16, p < .05) or better than “very good” (b = .12, p > .05) mental health). Social disconnectedness may not make a difference for mental health within the higher categories, but both disconnectedness and perceived isolation are associated with mental health at the lower extreme.
Depressive Symptoms
Because self-rated mental health is a new measure, we look for support for the previous results using OLS regression analysis of the modified CES-D-ml scale of depressive symptoms, shown in Table 4. The first model reflects well-established relationships between sociodemographic characteristics and depression among older adults (Heikkinen and Kauppinen 2004). In models 2 and 3, only perceived isolation is associated with depressive symptomatology.
TABLE 4.
Ordinary Least-Squares Regressions of Depressive Symptomsa on Social Disconnectedness, Perceived Isolation, and Covariatesb
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Age (in decades) | −.186* | −.185* | −.229* | −.229* |
| (.088) | (.090) | (.090) | (.091) | |
| Attended college | −.578** | −.502** | −.504** | −.502** |
| (.175) | (.173) | (.173) | (.170) | |
| Female | .383* | .438** | .567** | .568** |
| (.159) | (.155) | (.155) | (.153) | |
| Non-white | .234 | .165 | .083 | .081 |
| (.195) | (.210) | (.205) | (.218) | |
| Spouse/partner | −.496** | −.500** | −.300 | −.300 |
| (.179) | (.179) | (.198) | (.197) | |
| Co-morbidities | .490*** | .492*** | .487*** | .487*** |
| (.048) | (.049) | (.049) | (.049) | |
| Social disconnectedness | .279 | −.007 | ||
| (.157) | (.145) | |||
| Perceived isolation | 1.185*** | 1.183*** | ||
| (.148) | (.141) | |||
| Constant | 10.052*** | 10.004*** | 10.113*** | 10.111*** |
| Unweighted n | 2866 | 2866 | 2866 | 2866 |
| F | 29.91*** | 28.40*** | 41.53*** | 35.80*** |
| (df) | (6,45) | (7,44) | (7,44) | (8,43) |
| R2 | .067 | .070 | .104 | .104 |
Notes:
p < .05
p < .01
p < .001 (two-tailed tests)
Higher values indicate more depressive symptoms, based on the CES-D-ml.
Estimates presented are survey-adjusted and weighted for the probability of selection with post-stratification adjustments for non-response. Standard errors are presented in parentheses.
Model 4 considers social disconnectedness and perceived isolation together. The results are similar to those observed for self-rated mental health. Perceived isolation has a much stronger relationship than social disconnectedness with both self-rated mental health and depression. An increase of one standard deviation on the perceived isolation scale is associated with an increase of slightly more than one point on the CES-D-ml scale. After we account for this relationship between perceived isolation and depression, social disconnectedness is not associated with depressive symptoms.
The association between social disconnectedness and depressive symptoms is reduced in magnitude with the inclusion of perceived isolation, as was observed with respect to self-rated mental health. This provides further support for our second hypothesis that perceived isolation may mediate the relationship between disconnectedness and health, with respect to mental health in particular. Although the cross-sectional nature of our data limits our ability to make causal inferences, the evidence here suggests that the relationship between social disconnectedness and mental health works at least in part through perceived isolation. No such evidence was observed in the analysis of self-rated physical health.5
DISCUSSION
Our findings that two distinct forms of social isolation are both associated with worse physical and mental health should not come as a surprise. However, the variety of operationalizations of social isolation in previous research has made it difficult to determine whether particular aspects of isolation are more or less consequential for health. We build from this research by consolidating multiple aspects of social isolation within two larger forms: social disconnectedness and perceived isolation. Our findings demonstrate that social disconnectedness and perceived isolation are not interchangeable indicators. Instead, they have separate and distinct associations with physical and mental health.
Social disconnectedness is associated with worse physical health, regardless of whether it prompts feelings of loneliness or a perceived lack of social support. On the other hand, at all levels of social disconnectedness (or connectedness), the perception that one lacks social resources may take a toll on physical health. With respect to physical health outcomes, then, both situational and perceived isolation matter.
This is not the case with respect to mental health. The relationship between social disconnectedness and mental health appears to operate through the strong association between perceived isolation and mental health. These findings support research noting robust links between aspects of subjective isolation, particularly loneliness, and mental health (Cacioppo et al. 2006; Heikkinen and Kauppinen 2004). However, the role of perceived isolation as a mediator in the relationship between social disconnectedness and mental health has not been demonstrated so clearly in prior work. Our results suggest that socially disconnected older adults have worse mental health only to the extent that they feel isolated. This is an interesting finding that deserves more attention.
Since social disconnectedness and perceived isolation are more likely to be decoupled among older adults (Schnittker 2007; Shaw et al. 2007; van Baarsen et al. 2001; van Tilburg et al. 1998), the present study provides a liberal test of our hypothesis that these two forms of isolation have separate and distinct associations with health. We can find no theoretical reason that social disconnectedness and perceived isolation should be differentially related to health among younger adults. However, further research examining the contributions of these two forms of isolation within other age groups would advance our understanding of how changes in connectedness affect health across the life course.
From the standpoint of health promotion, our results may suggest that older adults who are able to withstand socially isolating circumstances or adjust their expectations so that they do not develop a subjective sense of isolation may fare better, with respect to physical and mental health, than those who feel isolated. This is an important issue because aging typically involves profound challenges to social connectedness, such as retirement and bereavement (Ferraro 1984; Weiss 2005). We need to better understand how older adults adapt to changes in their social relationships, and how psychological, environmental, and perhaps even genetic factors may affect older adults’ appraisals of their social support and companionship (Boomsma et al. 2005; Lakey and Cassady 1990). This could direct policy-related efforts to increase both social connectedness and the perceived availability of social resources among older adults.
We view this article as an early step toward the examination of the relative effects of social disconnectedness and perceived isolation on health and well-being. The present study has several limitations. First, reliance on self-reported measures of social connectedness restricts our ability to measure objective social disconnectedness apart from perceived isolation. Second, we are limited by reliance on cross-sectional data. We have approached these analyses with a theoretical focus on social isolation as a health risk. However, physical and mental health problems may create asymmetries in primary social relationships (see Horwitz, Reinhard, and Howell-White 1996) and limit individuals’ abilities and desires to develop and maintain social relationships (Li and Ferraro 2006; Thoits and Hewitt 2001). Therefore, causal relationships implied by our findings should be interpreted with caution. Longitudinal data will be useful for sorting out these processes and identifying specific mechanisms linking social disconnectedness and perceived isolation to particular health outcomes. We hope that further research will refine these concepts, reveal causal mechanisms, and help researchers and policymakers to better understand the health risks of social isolation.
Biography
Erin York Cornwell is a postdoctoral research associate in the Department of Sociology at Cornell University. She was the project coordinator for the first wave of the National Social Life, Health, and Aging Project (NSHAP), which provided the data for this article. She is interested in how social context and social relationships shape individuals’ life chances. Her dissertation research used NSHAP data to examine how household disorder affects older adults’ health and social connectedness. A forthcoming article in Sociological Perspectives examines differential access to experts through personal networks, and other work focuses on how social status shapes aspects of the legal process, such as participation and influence during jury trials.
Linda J. Waite is Lucy Flower Professor of Sociology and Director of the Center on Aging at the University of Chicago. She was the principal investigator for the National Social Life, Health and Aging Study. She is co-author, with Frances Goldscheider, of New Families, No Families?: The Transformation of the American Home (University of California Press, 1991), winner of the Duncan Award from the American Sociological Association. She is also author, with Maggie Gallagher, of The Case for Marriage: Why Married People are Happier, Healthier and Better Off Financially (Doubleday, 2000), which won the 2000 Outstanding Book Award from the Coalition for Marriage, Family and Couples Education. She is past president of the Population Association of America.
Footnotes
The National Health, Social Life, and Aging Project (NSHAP) is supported by the National Institutes of Health, including the National Institute on Aging, the Office of Women's Health Research, the Office of AIDS Research, and the Office of Behavioral and Social Sciences Research (grant 5R01AG021487). We are grateful for comments and suggestions from Benjamin Cornwell, Louise Hawkley, Edward Laumann, Martha McClintock, Phil Schumm, Peggy Thoits, and four anonymous reviewers.
The National Social Life, Health, and Aging Project employed a shortened version of the CES-D scale similar to the Iowa form (Kohout et al. 1993), but it included four, rather than three, response categories.
Twelve respondents have missing data on self-rated physical health, and 10 respondents have missing data on self-rated mental health. Those cases are omitted from all analyses. An additional 44 respondents have missing data on at least one CES-D-ml item. Those cases are excluded from the analysis of depressive symptoms.
Tests of the proportional odds assumption indicate that none of the coefficients differs across the five levels of self-rated health within any of the self-rated physical health models (Williams 2006).
Negative affect may predict lower self-rated health (Benyamini, Leventhal, and Leventhal 1999) and social isolation, so we conducted supplementary analyses controlling for depressive symptoms. This reduces the coefficient for perceived isolation in model 4 by roughly one-third, but other coefficients do not markedly change. We do not present that model because of concerns about reverse causation between depressive symptoms and self-rated health.
An interaction term crossing social disconnectedness and perceived isolation was included in analyses predicting physical and mental health, but it was not significant and resulted in little change in the other predictors.
Contributor Information
ERIN YORK CORNWELL, Cornell University.
LINDA J. WAITE, University of Chicago
REFERENCES
- Barefoot John C., Gronbaek Morten, Jensen Gorm, Schnohr Peter, Prescott Eva. Social Network Diversity and Risks of Ischemic Heart Disease and Total Mortality: Findings from the Copenhagen City Heart Study. American Journal of Epidemiology. 2005;161:960–67. doi: 10.1093/aje/kwi128. [DOI] [PubMed] [Google Scholar]
- Barnes Lisa L., Mendes de Leon Carlos F., Wilson Robert S., Bienias Julia L., Evans Denis A. Social Resources and Cognitive Decline in a Population of Older African Americans and Whites. Neurology. 2004;63:2322–26. doi: 10.1212/01.wnl.0000147473.04043.b3. [DOI] [PubMed] [Google Scholar]
- Benjamins Maureen Reindl. Religion and Functional Health Among the Elderly: Is There a Relationship and Is It Constant? Journal of Aging and Health. 2004;16:355–74. doi: 10.1177/0898264304264204. [DOI] [PubMed] [Google Scholar]
- Benyamini Yael, Leventhal Elaine A., Leventhal Howard. Self-Assessments of Health: What Do People Know that Predicts Their Mortality? Research on Aging. 1999;21:477–500. [Google Scholar]
- Berkman Lisa F., Syme Leonard. Social Networks, Host Resistance, and Mortality: A Nine-Year Follow-Up Study of Alameda County Residents. American Journal of Epidemiology. 1979;109:186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- Blazer Dan G. Social Support and Mortality in an Elderly Community Population. American Journal of Epidemiology. 1982;115:684–94. doi: 10.1093/oxfordjournals.aje.a113351. [DOI] [PubMed] [Google Scholar]
- Boomsma Dorret I., Willemsen Gonneke, Dolan Conor V., Hawkley Louise C., Cacioppo John T. Genetic and Environmental Contributions to Loneliness in Adults: The Netherlands Twin Register Study. Behavior Genetics. 2005;35:745–52. doi: 10.1007/s10519-005-6040-8. [DOI] [PubMed] [Google Scholar]
- Brummett Beverly H., Barefoot John C., Siegler Ilene C., Clapp-Channing Nancy E., Lytle Barbara L., Bosworth Hayden B., Williams Redford B., Mark Daniel B. Characteristics of Socially Isolated Patients with Coronary Artery Disease Who are at Elevated Risk for Mortality. Psychosomatic Medicine. 2001;63:267–272. doi: 10.1097/00006842-200103000-00010. [DOI] [PubMed] [Google Scholar]
- Cacioppo John T., Hawkley Louise C. Social Isolation and Health, with an Emphasis on Underlying Mechanisms. Perspectives in Biology and Medicine. 2003;46:S39–S52. [PubMed] [Google Scholar]
- Cacioppo John T., Hughes Mary Elizabeth, Waite Linda J., Hawkley Louise C., Thisted Ronald A. Loneliness as a Specific Risk Factor for Depressive Symptoms: Cross-Sectional and Longitudinal Analyses. Psychology and Aging. 2006;21:140–51. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- Carstensen Laura L., Isaacowitz Derek M., Charles Susan T. Taking Time Seriously: A Theory of Socioemotional Selectivity. American Psychologist. 1999;54:165–81. doi: 10.1037//0003-066x.54.3.165. [DOI] [PubMed] [Google Scholar]
- Charlson Mary E., Pompei Peter, Ales Kathy L., McKenzie CR. A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation. Journal of Chronic Disease. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Christakis Nicholas A., Fowler James H. The Spread of Obesity in a Large Social Network over 32 Years. New England Journal of Medicine. 2007;357:370–79. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- Cohen Sheldon. Psychosocial Models of the Role of Social Support in the Etiology of Physical Disease. Health Psychology. 1988;7:269–97. doi: 10.1037//0278-6133.7.3.269. [DOI] [PubMed] [Google Scholar]
- Cohen Sheldon, Doyle William J., Skoner David P., Rabin Bruce S., Gwaltney Jack M., Jr. Social Ties and Susceptibility to the Common Cold. Journal of the American Medical Association. 1997;277:1940–44. [PubMed] [Google Scholar]
- Cornman Jennifer C., Goldman Noreen, Glei Dana A., Weinstein Maxine, Chang Ming-Cheng. Social Ties and Perceived Support: Two Dimensions of Social Relationships and Health Among the Elderly in Taiwan. Journal of Aging and Health. 2003;15:616–44. doi: 10.1177/0898264303256215. [DOI] [PubMed] [Google Scholar]
- Cornwell Benjamin, Laumann Edward O., Schumm L. Philip. The Social Connectedness of Older Adults: A National Profile. American Sociological Review. 2008;73:185–203. doi: 10.1177/000312240807300201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean Alfred, Kolody Bohdan, Wood Patricia, Matt George E. The Influence of Living Alone on Depression in Elderly Persons. Journal of Aging and Health. 1992;4:3–18. [Google Scholar]
- Ellison Christopher G., George Linda K. Religious Involvement, Social Ties, and Social Support in a Southeastern Community. Journal for the Scientific Study of Religion. 1994;33:46–61. [Google Scholar]
- Ernst John M., Cacioppo John T. Lonely Hearts: Psychological Perspectives on Loneliness. Applied & Preventative Psychology. 1999;8:1–22. [Google Scholar]
- Fayers Peter M., Sprangers Mirjam A.G. Understanding Self-Rated Health. The Lancet. 2002;359:187–88. doi: 10.1016/S0140-6736(02)07466-4. [DOI] [PubMed] [Google Scholar]
- Fees BS, Martin P, Poon LW. A Model of Loneliness in Older Adults. Journal of Gerontology: Psychological Sciences and Social Sciences. 1999;54:P231–P239. doi: 10.1093/geronb/54b.4.p231. [DOI] [PubMed] [Google Scholar]
- Ferraro Kenneth F. Widowhood and Social Participation in Later Life: Isolation or Compensation? Research on Aging. 1984;6:451–68. [Google Scholar]
- Finch Brian Karl, Hummer Robert A., Reindl Maureen, Vega William A. Validity of Self-Rated Health among Latino(a)s. Journal of Epidemiology. 2002;155:755–59. doi: 10.1093/aje/155.8.755. [DOI] [PubMed] [Google Scholar]
- Geerlings Sandra W., Beekman Aartjan T.F., Deeg Dorly J.H., Van Tilburg Willem. Physical Health and the Onset and Persistence of Depression in Older Adults: An Eight-Wave Prospective Community-Based Study. Psychological Medicine. 2000;30:369–80. doi: 10.1017/s0033291799001890. [DOI] [PubMed] [Google Scholar]
- Gierveld Jenny de Jong, Hagestad Gunhild O. Perspectives on the Integration of Older Men and Women. Research on Aging. 2006;28:627–37. [Google Scholar]
- Haines Valerie A., Hurlbert Jeanne S. Network Range and Health. Journal of Health and Social Behavior. 1992;33:254–66. [PubMed] [Google Scholar]
- Hawkley Louise C., Burleson Mary H., Berntson Gary G., Cacioppo John T. Loneliness in Everyday Life: Cardiovascular Activity, Psychosocial Context, and Health Behaviors. Journal of Personality and Social Psychology. 2003;85:105–20. doi: 10.1037/0022-3514.85.1.105. [DOI] [PubMed] [Google Scholar]
- Hawkley Louise C., Masi Christopher M., Berry Jarett D., Cacioppo John T. Loneliness is a Unique Predictor of Age-Related Differences in Systolic Blood Pressure. Psychology and Aging. 2006;21:152–64. doi: 10.1037/0882-7974.21.1.152. [DOI] [PubMed] [Google Scholar]
- Heikkinen Riitta-Liisa, Kauppinen Markku. Depressive Symptoms in Late Life: A 10-Year Follow-Up. Archives of Gerontology and Geriatrics. 2004;38:239–50. doi: 10.1016/j.archger.2003.10.004. [DOI] [PubMed] [Google Scholar]
- Horwitz Allan V., Reinhard Susan C., Howell-White Sandra. Caregiving as Reciprocal Exchange in Families with Seriously Mentally Ill Members. Journal of Health and Social Behavior. 1996;37:149–62. [PubMed] [Google Scholar]
- House James S. Social Isolation Kills, But How and Why? Psychosomatic Medicine. 2001;63:273–74. doi: 10.1097/00006842-200103000-00011. [DOI] [PubMed] [Google Scholar]
- House James S., Landis Karl R., Umberson Debra. Social Relationships and Health. Science. 1988;241:540–45. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Hughes Mary Elizabeth, Waite Linda J., Hawkley Louise C., Cacioppo John T. A Short Scale for Measuring Loneliness in Large Surveys: Results from Two Population-Based Studies. Research on Aging. 2004;26:655–72. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes Michael, Gove Walter R. Living Alone, Social Integration, and Mental Health. American Journal of Sociology. 1981;87:48–74. doi: 10.1086/227419. [DOI] [PubMed] [Google Scholar]
- Idler Ellen, Benyamini Yael. Self-Rated Health and Mortality: A Review of Twenty-Seven Community Studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Idler Ellen L., Hudson Shawna V., Leventhal Howard. The Meanings of Self-Rated Health: A Qualitative and Quantitative Approach. Research on Aging. 1999;21:458–76. [Google Scholar]
- Johnson Robert J., Wolinsky Fredric D. Gender, Race, and Health: The Structure of Health Status Among Older Adults. Gerontologist. 1994;34:24–35. doi: 10.1093/geront/34.1.24. [DOI] [PubMed] [Google Scholar]
- Kinney Anita, Yeomans Lindsey E., Martin Bloor Christopher, Sandler Robert S. Social Ties and Colorectal Cancer Screening among Blacks and Whites in North Carolina. Cancer Epidemiology, Biomarkers and Prevention. 2005;14:182–89. [PubMed] [Google Scholar]
- Kohout Frank J., Berkman Lisa F., Evans Denis A., Cornoni-Huntley Joan. Two Shorter Forms of the CES-D Depression Symptoms Index. Journal of Aging and Health. 1993;5:179–93. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- Koropeckyj-Cox Tanya. Loneliness and Depression in Middle and Old Age: Are the Childless More Vulnerable? Journal of Gerontology: Psychological Sciences and Social Sciences. 1998;53:S303–S312. doi: 10.1093/geronb/53b.6.s303. [DOI] [PubMed] [Google Scholar]
- Krause Neil. Satisfaction with Social Support and Self-Rated Health in Older Adults. The Gerontologist. 1987;27:301–08. doi: 10.1093/geront/27.3.301. [DOI] [PubMed] [Google Scholar]
- Lakey Brian, Bennett Cassady Patricia. Cognitive Processes in Perceived Social Support. Journal of Personality and Social Psychology. 1990;59:337–43. [Google Scholar]
- Lang Frieder R., Carstensen Laura L. Close Emotional Relationships in Late Life: Further Support for Proactive Aging in the Social Domain. Psychology and Aging. 1994;9:315–24. doi: 10.1037//0882-7974.9.2.315. [DOI] [PubMed] [Google Scholar]
- Latkin Carl A., Forman Valerie, Knowlton Amy, Sherman Susan. Norms, Social Networks, and HIV-related Risk Behaviors among Urban Disadvantaged Drug Users. Social Science and Medicine. 2003;56:465–76. doi: 10.1016/s0277-9536(02)00047-3. [DOI] [PubMed] [Google Scholar]
- Li Yunqing, Ferraro Kenneth F. Volunteering in Middle and Later Life: Is Health a Benefit, Barrier or Both? Social Forces. 2006;85:497–519. [Google Scholar]
- Lillard Lee A., Waite Linda J. Til Death Do Us Part:’ Marital Disruption and Mortality. American Journal of Sociology. 1995;100:1131–56. [Google Scholar]
- Lin Nan. Social Capital: A Theory of Social Structure and Action. Cambridge University Press; Cambridge, England: 2001. [Google Scholar]
- Lin Nan, Ye Xiaolan, Ensel Walter M. Social Support and Depressed Mood: A Structural Analysis. Journal of Health and Social Behavior. 1999;40:344–59. [PubMed] [Google Scholar]
- Litwin Howard. The Association of Disability, Sociodemographic Background, and Social Network Type in Later Life. Journal of Aging and Health. 2003;15:391–408. doi: 10.1177/0898264303015002004. [DOI] [PubMed] [Google Scholar]
- Mehta Kala M., Yaffe Kristine, Covinsky Kenneth E. Cognitive Impairment, Depressive Symptoms, and Functional Decline in Older People. Journal of the American Geriatrics Society. 2002;50:1045–50. doi: 10.1046/j.1532-5415.2002.50259.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molarius Anu, Janson Staffan. Self-Rated Health, Chronic Diseases, and Symptoms Among Middle-Aged and Elderly Men and Women. Journal of Clinical Epidemiology. 2002;55:364–70. doi: 10.1016/s0895-4356(01)00491-7. [DOI] [PubMed] [Google Scholar]
- Mulvaney-Day Norah E., Alegria Margarita, Sribney William. Social Cohesion, Social Support, and Health among Latinos in the United States. Social Science and Medicine. 2007;64:477–95. doi: 10.1016/j.socscimed.2006.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutchler Jan E., Burr Jeffrey A., Caro Francis G. From Paid Worker to Volunteer: Leaving the Paid Workforce and Volunteering in Later Life. Social Forces. 2003;81:1267–93. [Google Scholar]
- Pearlin Leonard I. The Sociological Study of Stress. Journal of Health and Social Behavior. 1989;20:241–56. [PubMed] [Google Scholar]
- Pressman Sarah D., Cohen Sheldon, Miller Gregory E., Barkin Anita, Rabin Bruce S., Treanor John J. Loneliness, Social Network Size, and Immune Response to Influenza Vacci-nation in College Freshmen. Health Psychology. 2005;24:297–306. doi: 10.1037/0278-6133.24.3.297. [DOI] [PubMed] [Google Scholar]
- Radloff Lenore Sawyer. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rook Karen S., Ituarte Philip H.G. Social Control, Social Support, and Companionship in Older Adults’ Family Relationships and Friendships. Personal Relationships. 1999;6:199–211. [Google Scholar]
- Ross Catherine E. Reconceptualizing Marital Status as a Continuum of Social Attachment. Journal of Marriage and the Family. 1995;57:129–40. [Google Scholar]
- Schnittker Jason. Look (Closely) at All the Lonely People: Age and the Social Psychology of Social Support. Journal of Aging and Health. 2007;19:659–82. doi: 10.1177/0898264307301178. [DOI] [PubMed] [Google Scholar]
- Seeman Teresa E. Health Promoting Effects of Friends and Family on Health Outcomes in Older Adults. American Journal of Health Promotion. 2000;14:362–70. doi: 10.4278/0890-1171-14.6.362. [DOI] [PubMed] [Google Scholar]
- Seeman Teresa E., Berkman Lisa F., Blazer Dan G., Rowe John W. Social Ties and Support and Neuroendocrine Function: The MacArthur Studies of Successful Aging. Annals of Behavioral Medicine. 1994;16:95–106. [Google Scholar]
- Shaw Benjamin A., Krause Neal, Liang Jersey, Bennett Joan. Tracking Changes in Social Relations Throughout Late Life. Journal of Gerontology: Social Sciences. 2007;62B:S90–S99. doi: 10.1093/geronb/62.2.s90. [DOI] [PubMed] [Google Scholar]
- Sorkin Dara, Rook Karen S., Lu John L. Loneliness, Lack of Emotional Support, Lack of Companionship, and the Likelihood of Having a Heart Condition in an Elderly Sample. Annals of Behavioral Medicine. 2002;24:290–98. doi: 10.1207/S15324796ABM2404_05. [DOI] [PubMed] [Google Scholar]
- Steptoe Andrew, Owen Natalie, Kunz-Ebrecht Sabine R., Brydon Lena. Loneliness and Neuroendocrine, Cardiovascular, and Inflammatory Stress Responses in Middle-Aged Men and Women. Psychoneuroendocrinology. 2004;29:593–611. doi: 10.1016/S0306-4530(03)00086-6. [DOI] [PubMed] [Google Scholar]
- Stock James H., Wright Jonathan H., Yogo Motohiro. A Survey of Weak Instruments and Weak Identification in Generalized Method of Moments. Journal of Business and Economic Statistics. 2002;20:518–29. [Google Scholar]
- Stokes Joseph P. The Relation of Social Network and Individual Difference Variables to Loneliness. Journal of Personality and Social Psychology. 1985;48:981–90. [Google Scholar]
- Thoits Peggy. Stress, Coping, and Social Support Processes: Where Are We? What Next? Journal of Health and Social Behavior. 1995;35:53–79. [PubMed] [Google Scholar]
- Thoits Peggy A., Hewitt Lyndi N. Volunteer Work and Well-Being. Journal of Health and Social Behavior. 2001;42:115–31. [PubMed] [Google Scholar]
- Tomaka Joe, Thompson Sharon, Palacios Rebecca. The Relation of Social Isolation, Loneliness, and Social Support to Disease Outcomes Among the Elderly. Journal of Aging and Health. 2006;18:359–84. doi: 10.1177/0898264305280993. [DOI] [PubMed] [Google Scholar]
- Uchino Bert N., Cacioppo John T., Kiecolt-Glaser Janice K. The Relationship Between Social Support and Physiological Processes: A Review with Emphasis on Underlying Mechanisms and Implications for Health. Psychological Bulletin. 1996;119:488–531. doi: 10.1037/0033-2909.119.3.488. [DOI] [PubMed] [Google Scholar]
- Umberson Debra. Family Status and Health Behaviors: Social Control as a Dimension of Social Integration. Journal of Health and Social Behavior. 1987;28:306–19. [PubMed] [Google Scholar]
- Umberson Debra, Williams Kristi, Powers Daniel A., Liu Hui, Needham Belinda. You Make Me Sick: Marital Quality and Health Over the Life Course. Journal of Health and Social Behavior. 2006;47:1–16. doi: 10.1177/002214650604700101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Baarsen Berna, Snijders Tom A.B., Smit Johannes H., van Duijn Marijtje A. Lonely but Not Alone: Emotional Isolation and Social Isolation as Two Distinct Dimensions of Loneliness in Older People. Educational and Psychological Measurement. 2001;61:119–35. [Google Scholar]
- van Tilburg Theo G., Gierveld Jenny de Jong, Lecchini Laura, Marsiglia D. Social Integration and Loneliness: A Comparative Study among Older Adults in the Netherlands and Tuscany, Italy. Journal of Social and Personal Relationships. 1998;15:740–54. [Google Scholar]
- Waite Linda J., Hughes Mary Elizabeth. At Risk on the Cusp of Old Age: Living Arrangements and Functional Status Among Black, White, and Hispanic Adults. Journal of Gerontology. 1999;54B:S136–S144. doi: 10.1093/geronb/54b.3.s136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weeks David G., Michela John L., Peplau Letitia A., Bragg Martin E. Relation between Loneliness and Depression: A Structural Equation Analysis. Journal of Personality and Social Psychology. 1980;39:1238–44. doi: 10.1037/h0077709. [DOI] [PubMed] [Google Scholar]
- Weiss Robert S. Retirement, Marriage, and Social Isolation. Illness, Crisis, and Loss. 2005;13:75–84. [Google Scholar]
- Wickrama KAS, Lorenz Frederick O., Wallace Lora Ebert, Peiris Laknath, Conger Rand D., Elder Glen H., Jr. Family Influences on Physical Health During the Middle Years: The Case of Onset of Hypertension. Journal of Marriage and the Family. 2001;63:527–39. [Google Scholar]
- Williams Richard. Generalized Ordered Logit/Partial Proportional Odds Models for Ordinal Dependent Variables. The Stata Journal. 2006;6:58–82. [Google Scholar]
- Wilson Robert S., Krueger Kristin R., Arnold Steven E., Schneider Julie A., Kelly Jeremiah F., Barnes Lisa L., Tang Yuxiao, Bennett David A. Loneliness and Risk of Alzheimer Disease. Archives of General Psychiatry. 2007;64:234–40. doi: 10.1001/archpsyc.64.2.234. [DOI] [PubMed] [Google Scholar]