Abstract
Background
Recurrent gliomas have a dismal outcome despite use of multimodality treatment including surgery, radiation therapy and chemotherapy.
Objective
In this article the authors discuss potential applications of oncolytic measles virus strains as novel antitumor agents in the treatment of gliomas.
Methods
Important aspects of measles virus development as an anticancer therapeutic agent including engineering, retargeting and combination studies with other therapeutic modalities are discussed. The translational process that led to the first clinical trial of an engineered measles virus derivative in patients with recurrent glioblastoma multiforme is also described.
Results/conclusions
Oncolytic measles virus strains hold promise as novel antitumor agents in the treatment of gliomas.
Keywords: brain tumor, engineering, measles virus, retargeting, virotherapy
1. Introduction
Malignant gliomas are the most common primary brain tumors with 16,000 deaths each year in the US [1]. Glioblastoma multiforme (GBM) is the most common glioma histology, representing 80% of primary brain tumors in adults. It has a high mortality rate and a median survival of 12 – 16 months [2]. Gliomas are resistant to conventional treatment modalities and they invariably recur despite multimodality treatment including surgery, radiation and chemotherapy. Despite their high propensity for local recurrence, gliomas rarely metastasize and, therefore, represent good candidates for local gene transfer/virotherapy approaches.
Measles virus (MV) is a negative strand RNA virus and belongs in the family of Paramyxoviridae. The MV genome includes six genes translating in eight proteins. MV entry to target cells is mediated by two membrane glycoproteins, the hemagglutin (H) protein and the fusion (F) protein. The H protein is responsible for binding to cellular receptors such as CD46, a regulator of complement activation that is found on all human nucleated cells and frequently overexpressed in tumor cells [3,4], including gliomas [5] and signaling lymphocyte activated molecule (SLAM) which is expressed on T- and B-lymphocytes and macrophages [6]. The F protein causes the virus to fuse with the cell after attachment has taken place. The virus exerts its characteristic cytopathic effect through the formation of syncytia (multinucleated giant cell aggregates), which undergo apoptotic cell death. In contrast to the wild-type virus, vaccine strains of the MV have an excellent safety profile, and have resulted in significant decreases in the measles incidence and mortality worldwide [7].
The authors’ interest in measles as oncolytic agent was fueled by case reports in the 1970s, where natural infection with MV led to spontaneous regression of hematologic malignancies in African children [8,9]. In proof-of-principle studies the authors have also demonstrated that the MV F and H proteins, encoded by non-replicating viral vectors have significant antitumor activity against gliomas [10]. One of the main challenges, however, associated with the use of non-replicating vectors in vivo is limited infection/gene transfer, which can have a negative impact on antitumor efficacy. The authors, therefore, chose to test the natural carriers of these proteins (i.e., replicating attenuated vaccine strains of MV) as antiglioma agents.
2. Measles virus derivatives have in vitro and in vivo antitumor activity against gliomas
One of the great challenges in clinical application of gene transfer using replicating viruses, especially as it pertains to brain tumors, is the limited ability to monitor in vivo the spread and/or elimination of the virus, or to measure the profile of viral gene expression over time. Repeat brain biopsies are typically not feasible or ethically justified and, consequently, additional surgical procedures are usually not a viable option for addressing these concerns. Measurement of these parameters should be an integral component of pharmacokinetic, pharmacodynamic, dose finding and dose scheduling studies and could facilitate the tailoring of virotherapy protocols for individual patients. Without data on virus kinetics, it is not possible to determine whether a failed response to therapy is due to lack of infection, inadequate virus spread, weakened cytopathic effect or premature virus elimination. Also, accurate determination of the timing of virus elimination is needed when deciding on the dose interval between repeat treatment cycles. The authors, therefore, hypothesized that inert soluble marker peptides expressed by the oncolytic vaccine strain of MV could facilitate noninvasive in vivo monitoring of the kinetic profile of viral gene expression. Ideal marker peptides should be non immunogenic, have no biologic function and a constant circulation half-life, and should be efficiently secreted from virus-infected cells into the bloodstream. The concentration of marker peptide in serum should be negligible prior to therapy but easily and accurately measurable thereafter.
The soluble component of the human carcinoembryonic antigen (CEA) fits all the criteria described above for a trackable marker peptide that can be used for noninvasive monitoring of the viral therapy in glioma patients. CEA is a glycoprotein of molecular weight 180 kDa with a circulating half-life of 36 h in humans, and no documented biologic activity [11,12]. Circulating levels are frequently elevated in certain malignancies, such as metastatic colon cancer, in which CEA provides an important nonimmunogenic tumor marker. However, CEA is not expressed in gliomas [13], therefore, elevated levels of CEA in the serum of glioma patients after viral treatment could only be attributed to viral gene expression. Furthermore, as demonstrated in the case of colorectal cancer patients with CNS only metastases, CEA produced in the CNS reaches the systemic circulation and can be detected in the serum [14]. An attenuated strain of the Edmonston’s vaccine lineage (MV-Edm), engineered to express CEA [15,16], was produced.
MV-CEA contains the MV-NSe backbone, which derives from the MV-Edm lineage. The soluble extracellular N terminal domain of CEA (minus the transmembrane C terminal tail) was subcloned as an additional transcription unit before the N gene (Figure 1) [16]. Thus, genes in the infectious clone of p(+) MV-hCEA (MV-CEA) include the extracellular N terminal domain of CEA (soluble marker peptide), followed by the MV genes coding for the nucleocapsid (N), phosphoprotein (P), matrix (M), fusion (F), hemagglutinin (H) and polymerase (L) proteins [16].
Figure 1. A schematic representation of recombinant MV-Edm with soluble human CEA cDNA inserted as an additional transcription unit.
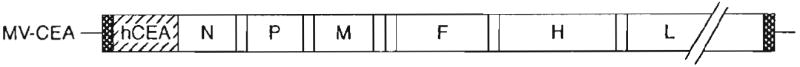
CEA: Carcinoembryonic antigen; F: Fusion; H: Hemagglutinin; L: Polymerase proteins; M: Matrix; MV: Measles virus; N: Nucleocapsid; P: Phosphoprotein.
Expression of viral genes when the virus replicates results in CEA production, and CEA detection can allow monitoring of viral gene expression. MV-CEA is the first measles vaccine derivative tested against gliomas; it resulted in significant cytopathic effect in vitro against essentially all glioma lines tested (both primary and deriving from glioblastoma patients; Figure 2) [17].
Figure 2. A-J, MV-CEA infection results in prominent syncytia formation in U87, U251, and U118 cells and the primary glioma lines GBM5 and 6.

Crystal violet stain, (×200 magnification). A, C, E, G, and I, uninfected U87, U251, U118 cells, GBM5 and 6, respectively. B, D, F, H and J, 72 h after infection of U87, U251, U118, GBM5 and GBM6 cell, respectively, with MV-CEA (MOI 0.1). Extensive syncytia formation is observed preceding cell death.
CEA: Carcinoembryonic antigen; GBM: Glioblastoma multiforme; MV: Measles virus.
One step viral growth curves demonstrated that glioma cells support robust viral replication. CEA levels in the culture supernatants correlated well with viral replication/gene expression in glioma cells. TdT-mediated dUTP neck end labeling (TUNEL) assays demonstrated that glioma cells forming syncytia die by apoptosis [17].
In contrast, MV-CEA had no cytopathic effect against normal cells such as astrocytes and normal human fibroblasts [17]. The selectivity of cytopathic effect of oncolytic MV strains against tumors appears to be at least in part related to CD46 overexpression in tumor cells, the latter representing a mechanism of tumor protection from complement-mediated lysis, and low expression levels in normal cells [17,18]. Indeed, fluorescence-activated cell sorting (FACS) analysis demonstrated high or moderate CD46 expression levels in several primary and established glioma cell lines tested (Allen and Galanis, unpublished data). In a normal brain, CD46 is mainly expressed in endothelial cells, especially at the blood–brain barrier; this observation is consistent with the important role played by the microvasculature in the immune surveillance of the brain [19,20]. CD46 expression in blood-brain barrier should not constitute a safety concern if intratumoral administration of the virus is contemplated. In contrast, CD46 overexpression in gliomas results in a favorable therapeutic index.
In vivo efficacy of the MV-CEA virus was assessed in orthotopic glioma models, including a series of animal models which derive from glioblastoma patients that are then propagated in nude mice. Following orthotopic implantation, they maintain the molecular characteristics and invasiveness of the human tumor they originated from [21].
Treatment with MV engineered vaccine strains resulted in tumor regression and prolongation of survival in all models tested so far, including U87 (p = 0.02, Figure 3), GBM 14 (p = 0.037), GBM39 (p = 0.0079) and GBM6 (p = 0.0049) (Alien and Galanis, unpublished data).
Figure 3. Antitumor effect of MV-CEA, administered intratumorally in an orthotopic U87 tumor model.

Tumors were established by injection of 106 U87 cells into the right caudate nucleus of BALB/c nude mice. Mice were randomly assigned to either MV-CEA treatment (1.8 × 106 TCID50), UV-inactivated MV-CEA treatment, or remained untreated. Significant prolongation of survival was observed in the mice treated with MV-CEA, as compared to mice that received UV-inactivated MV-CEA or no treatment (p = 0.02).
Reproduced with permission from Phuong L, et al. Cancer Res 2003 [17].
CEA: Carcinoembryonic antigen; MV: Measles virus;
TCID50: Tissue culture infective dose.
CEA levels started increasing in the serum of mice treated with the MV-CEA on day 3 after treatment initiation, and peaked at day 10 before gradually declining to baseline (Figure 4) [17].
Figure 4. Serum CEA plotted with U87 subcutaneous tumor volume in BALB/c nude mice treated with intravenous MV-CEA.

The rise and fall of serum CEA parallel the growth and regression of the tumor.
Reproduced with permission from Phuong L, et al. Cancer Res 2003 [17].
CEA: Carcinoembryonic antigen; MV: Measles virus.
3. Toxicology and biodistribution studies
In vitro and in vivo efficacy data supported the potential of MV-CEA as novel antitumor agent against brain tumors. Informative toxicology and biodistribution studies had to be performed, however, prior to this promising approach being translated into a clinical application. In this context, choice of the appropriate toxicology model is crucial. The safety of CNS administration of MV-CEA was tested in two different animal models, Ifnarko CD46 Ge transgenic mice and Rhesus macaques.
Rodents do not normally express the MV receptors CD46 and SLAM; therefore, they cannot be used to assess toxicity of oncolytic MV strains. A very appealing transgenic mouse model of MV pathogenecity has been recently developed, however, by inserting a yeast artificial chromosome containing the human CD46 receptor gene and knocking out the INF-αβ receptor gene [22]. These Ifnarko CD46-Ge transgenic mice express human CD46 in a tissue distribution that replicates human CD46 expression and are susceptible to MV-Edmonston infection. CD46 distribution in the brain of CD46 transgenic mice has been shown to mimic the distribution in humans [22]. Studies of intracerebral inoculation of Ifnarko CD46-Ge mice with MV-Edmonston have demonstrated that this can be a suitable animal model for assessment of measles neurotoxicity [22]. Human patients are not lacking the IFN-αβ receptor gene, nevertheless, in consultation with FDA the authors applied this transgenic mouse model in order to assess the neurotoxicity of MV-CEA, thus mimicking the worst case scenario in the patient population. Test and control articles were administered intracranially in the animals’ caudate nucleus, using the same stereotactic parameters as for the efficacy studies. A total of 120, 6 – 8 week-old measles immune Ifnarko CD46-Ge mice were assigned to three dose groups; one group receiving vehicle control, the second receiving 104 tissue culture infective dose 50 (TCID50) on days 1 and 5, and the third receiving 105 TCID50 on days 1 and 5. By direct brain weight conversion, this is approximately equivalent to 35 × the maximum human dose n i the proposed clinical trial. General appearance, activity level, body weight and key hematologic/biochemical parameters were monitored in all groups of animals, without evidence of abnormality. In order to further assess toxicity, 30 animals from each group were euthanized on early (days 4 and 8), intermediate (day 26) and late (day 90) time points, and tissues from multiple organs were subjected to histologic analysis. Close clinical monitoring revealed no signs of clinical toxicity or neurotoxicity. Histologic examination of ten vital organs: brain, heart, lung, liver, pancreas, kidneys, spleen, ovary, testes, peritoneum and skeletal muscles revealed no significant difference between vehicle-treated animals and MV-CEA treated animals. No CEA elevation was observed and there was no evidence of viral replication outside the CNS (Myers and Galanis, unpublished data).
In addition, safety of the virus following CNS administration was tested in Rhesus macaques. Rhesus macaques are naturally susceptible to MV infection and have been extensively used to study MV pathogenesis. CNS inoculation of MV vaccine strains is die standard method by which the MV vaccine lots are tested for neurotoxicity. Five adult measles immune Rhesus macaques were used in this toxicology study. Immune animals were chosen in order to mimic the study population in the proposed clinical trial. Two macaques received 106 TCID50 on days 1 and 5 to mimic the repeat dose administration schedule in the authors’ trial; two received 105 TCID50 on days 1 and 5, and one animal received vehicle control on die same days. Th e injections were administered in the frontal lobe of the animals, a common location for GBM, using previously established stereotactic coordinates [23]. By direct brain weight conversion die highest dose was 1.5 times higher than maximum human dose in die proposed trial and 3 times higher the maximum dose that the normal brain could be exposed in the clinical study. Animals were monitored closely for clinical signs including rash, fever, conjunctivitis and neurologic status including level of consciousness, motor function, gait, activity level, behavior, posture and facial symmetry. No evidence of neurologic or odier toxicity has been observed to date, at 52 months from viral administration. Hematologic/biochemical parameters were normal at all time points. No CEA elevation was detected pointing to absence of virus propagation. There was no evidence of viremia in peripheral blood mononuclear cells by quantitative-real-time polymerase chain reaction (QRT-PCR), except for a single time point in one of die high-dose animals, and no shedding in buccal mucosa secretions was observed. In addition, there was no laboratory evidence of encephalitis on cerebrospinal fluid (CSF) exam performed on day 9 after administration of the first viral dose. No virus was detected in the CSF by QRT-PCR or Vero cell overlay. MRI imaging revealed no imaging abnormalities and no inflammation [24]. These results in a susceptible transgenic mouse models and primates supported the safety of administration of MV-CEA to primary CNS tumors.
A Phase I clinical trial of MV-CEA in patients with recurrent GBM has been recently activated. Measles-immune, recurrent GBM patients who are candidates for gross total or subtotal resection are eligible for the study. Doses ranging from 105 to 2 × 107 TCID50 will be administered either in the resection cavity following tumor resection (group A) or both into the recurrent tumor and in the resection cavity following resection 5 days after die initial administration (group B). Three patients have been treated and so far tolerated treatment well without evidence of toxicity or CNS inflammation (Galanis E, unpublished data). Patient accrual is ongoing. Extensive correlative analysis is built into this trial to assess receptor expression and correlation with efficacy and toxicity, CEA as a correlate of viral replication in the tumor, viral distribution and shedding.
4. Retargeting measles virus against tumor-specific receptors
Although based on toxicology data and early human data, locoregional administration of unmodified MV strains appears to be well tolerated, viral retargeting against tumor-specific antigens could be important if systemic administration of the virus is contemplated. Furthermore, retargeting could eliminate the possibility of toxicity due to low CD46 expression levels in the normal brain, and the possible interaction of the virus with the SLAM receptor expressed in B-, T cells and lymphocytes that could result in immunosuppression. In addition, retargeting could allow us co overcome variability in receptor expression in tumor cells [6,25,26]. Development of retargeted MV strains against glioma-specific receptors with ablation of entry through natural receptors could, therefore, improve the therapeutic index in certain clinical settings. Issues that have to be considered when retargeting viral oncolytic agents include maintenance of potency in vitro and in vivo and ability to produce viral liters that allow clinical translation.
Amplification of receptor tyrosine kinases represents one of the hallmarks of GBM and could be exploited to retarget viral entry. EGFR gene amplification occurs in a significant percentage of GBM tumors. EGFR is a 170-kDa trans-membrane tyrosine kinase glycoprotein receptor, amplification of which results in stimulation of a signal transduction cascade that leads to cellular proliferation. Amplification of EGFR is one of the most common oncogenic events in gliomas and is observed in 40% of GBM. The most common type of mutation of EGFR is the vIII mutant, which is characterized by deletion of exons 2 – 7 and is expressed in 40 – 60% of GBM with EGFR amplification. EGFRvIII is not expressed in the normal brain and it is tumor specific. I t therefore represents an excellent candidate for viral retargeting n i gliomas [27,28]. Measles retargeting has become feasible following identification of mutations in the H protein that ablate viral recognition and entry via the natural receptors CD46 and SLAM [29,30]. The authors hypothesized that combining these mutations with ligand display on H could result in effective retargeting. Retargeted recombinant viruses were generated from the measles Edmonston-NSe vaccine strain displaying a single chain antibody against EGFRvIII at the C-terminus of H, and containing the marker green fluorescent protein (GFP) gene in position 1. Two different H mutants were employed: HSNS (V451S, Y481N, A527S)-CD46 blind, and HAA (Y481A, R533A)-CD46 and SLAM blind. The MV-GFP virus was used as a control. Both EGFRvIII retargeted viruses had significant antitumor activity against EGFRvIII-expressing GBMs, which was comparable to the unmodified virus, but no cytopathic effect against normal cells. In an orthotopic model of EGFRvIII-expressing GBM39 xenografts, there was comparable therapeutic efficacy between retargeted strains and unmodified MV-GFP and statistically significant prolongation of survival in treated animals, as compared with the control group, treated with UV-inactivated virus (p = 0.001). Formation of syncytia was observed in tumors treated with retargeted viruses, with a surrounding infiltrate consisting of macrophages and natural killer cells [27].
One of the limitations of this approach is the focal EGFRvIII expression in glioma tissues. In a variation of the EGFRvIII retargeting approach, CD46 and SLAM ablating mutations in H were combined with display of a single-chain antibody that recognizes both EGFR and EGFRvIII. As demonstrated by in vivo and in vitro studies, the retargeted virus can selectively enter the glioma cells via either EGFR or EGFRvIII receptor without losing its oncolytic efficacy, as compared with unmodified MV-GFP strain. The EGFR retargeted strain had significant antitumor activity against primary EGFR amplified and/or EGFRvIII-expressing GBM cell lines in vitro and in vivo. Using primary glioma lines stably transduced to express the luciferase gene to facilitate non-invasive monitoring of intracranial tumors in vivo, significant reduction in tumor growth was demonstrated by chemiluminescent imaging [28].
Recently, viral retargeting was also accomplished by displaying the human IL-13 at the C-terminus of H in combination with the Y481A and R533A CD46 and SLAM ablating mutations. This modification allows viral entry via the IL-13-Rα2 receptor, a decoy receptor present in > 80% of high grade gliomas and further increases the potential applicability of retargeted measles strains [31].
5. Combination of measles virus with conventional therapeutics
Locoregional failure remains a significant problem in glioma treatment with the majority of gliomas recurring in the radiation field. Combining MV with the external beam radiation therapy (RT) is appealing because both treatment modalities can be used in a loco-regional manner to improve local control, the main mode of GBM relapse, and possibly therefore outcome. Given the significant preclinical activity of MV derivatives in glioma models, and the major role of apoptosis in MV and RT induced glioma cell death, we hypothesized that ionizing RT and MV-CEA virotherapy combination treatment would significantly augment the antitumor potential of either modality.
3-(4,5-Dimethyl-thiazol-2yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium (MTS) and clonogenic assays demonstrated a strong synergistic interaction between MV-CEA and RT in GBM cells including both primary and established glioma lines. Furthermore, significant antitumor efficacy was observed in vivo in a subcutaneous U87 model. There was significant prolongation of survival (p = 0.001) in the combination treatment group as compared to single modality or control treated animals. The synergistic effect of the combination appeared to be due to an increase in viral burst size and increase in apoptotic death: one-step viral growth curves demonstrated increased viral burst size by up to 2 logs in MV/RT combination treated cells, as compared with glioma cells treated with single agent MV-CEA. Changes in CEA levels and expression of viral N and H protein were also consistent with increased viral production. Furthermore, TUNEL assays and western blot analysis demonstrated increase in apoptosis in MV/RT combination treated cells. The pan-caspase inhibitor Z-VAD-FMK and the caspase-8 inhibitor Z-IETD-FMK but not the caspase-9 inhibitor Z-IEHD-FMK protected glioma cells from MV-CEA/RT induced cleavage of poly (ADP-ribose) polymerase (PARP), indicating that the apoptotic death in combination treated cells is mostly mediated via the extrinsic caspase pathway. The Fas–FasL interaction blocking antibody NOK-1 blocked MV/RT-induced PARP cleavage, whereas the Fas agonistic antibody CH11 increased PARP cleavage in MV/RT combination-treated cells. FACS analysis and RT-PCR demonstrated upregulation of Fas in combination-treated cells [32]. Furthermore, increased Fas expression by immunohistochemistry (IHC) was observed in MV/RT combination-treated U87 xenografts. These findings have potential translational implications in glioma treatment. As RT in combination with temozolomide represents the standard of care for newly diagnosed GBM, the authors are in the process of examining the antiglioma activity of measles/temozolomide/RT combination [32].
6. Combination of measles virus derivatives with heat-shock protein inhibitors
Induction of the heat-shock protein 70 (Hsp70) constitutes one of the earliest changes in cellular gene expression following infection with RNA viruses, including MV, and Hsp70 upregulation induced by heat shock has been shown to result in increased MV infection rates and plaque recovery. Hsp90 inhibitors such as geldanamycin (GA) or 17-aminogeldanamycin (17-AAG) result in pharmacologic upregulation of Hsp70 and they are at present in clinical testing as cancer therapeutics. The authors, therefore, investigated the hypothesis that Hsp inhibitors could augment the MV-induced cytopathic effect. The MV-CEA and GA combination was tested in U251 (glioma), MDA-MB231 (breast), SKOV3.IP (ovarian) and TE671 (rhabdomyosarcoma) cancer cell lines. Combination treatment resulted in a statistically significant increase in syncytia formation (p < 0.05 as compared with MV-CEA infection alone) and increase in antitumor activity. Clonogenic assays demonstrated a significant decrease in tumor colony formation in MV-CEA/GA combination treated cells. In addition there was an increase in apoptosis by 4’,6-diamidino-2-phenylindole staining. Western immunoblotting for caspase-9, caspase-8, caspase-3 and PARP, demonstrated increase in cleaved caspase-8, -3 and PARP. The pan-caspase inhibitor Z-VAD-FMK and caspase-8 inhibitor Z-IETD-FMK but not the caspase-9 inhibitor Z-IEHD-FMK protected tumor cells from MV-CEA/GA-induced PARP activation, indicating that apoptosis in combination-treated cells occurs via the extrinsic caspase pathway. Treatment of normal cells, such as normal human fibroblasts, however, with the MV-CEA/GA combination, did not result in cytopathic effect, indicating that GA did not alter the MV-CEA specificity for tumor cells. One-step growth curves, western blot for MV-N protein expression and QRT-PCR quantitation of MV-genome copy number indicate that the difference in cytopathic effect is not due to increased proliferation of MV-CEA in GA-treated tumor cells. Rho activation assays and western blot for total RhoA, a GTPase associated with the actin cytoskeleton, and inactive pRhoA demonstrated decrease in RhoA activation in combination-treated cells, which has been shown to result in an increase in paramyxovirus-induced cell–cell fusion [33].
Identification of RhoA as an important determinant of measles fusogenicity and antitumor effect can be exploited to further increase the efficacy of measles virotherapy. Although the presently available Hsp inhibitors have sub-optimal CNS penetration, additional ongoing experiments are assessing the antitumor activity of combinations or MV derivatives with other cell cycle small-molecule inhibitors, which can affect the cytoskeleton, thus making tumor cells more prone to fusion.
7. Conclusion
The use of oncolytic MV strains represents a novel antitumor strategy in glioma treatment. Following the demonstration of preclinical efficacy after orthotopic administration in several glioma models and safety studies in a transgenic mouse model and primates, the virus presently in Phase I testing in recurrent glioma patients. Safety, efficacy and correlative analysis data deriving from this trial will guide the development of MV derivatives as antiglioma agents. Genetic modification of the virus by engineering the viral H protein to express human CEA could allow real time monitoring by following CEA levels in the serum, a concept tested in the ongoing clinical trial. The virus can be retargeted to bypass its natural receptors and enter target cells via tumor-specific ligands without losing its efficacy, thus increasing tumor selectivity and further improving its safety profile. It can also be combined with conventional treatment modalities such as RT, which represents the standard of care in glioma treatment, significantly increasing the antitumor efficacy of the latter. These results emphasize the potential of MV derivatives as novel antitumor agents in glioma treatment.
8. Expert opinion
Despite several clinical trials involving both non-replicating (retroviruses, adenoviruses) [34-36] and replicating (E1B attenuated adenovirus Onyx-015, HSV-1 mutant G207, NDV, reovirus) [37-40] viral vectors and a variety of transgenes (p53, HSV-tk), neither gene therapy nor virotherapy have yet fulfilled their promise as antiglioma agents. MV derivatives have potential advantages in this setting: they have significant preclinical activity against gliomas, potent bystander effect with 80 – 100 tumor cells fusing to form syncytia for each cell infected, and tumor specificity because of overexpression of the MV receptor CD46 in tumor cells. They can also be effectively engineered and retargeted. Furthermore, the synergistic activity of the virus when combined with other therapeutic modalities such as RT creates opportunities that could allow incorporation of the virus in the existing therapeutic armamentarium against gliomas.
Results from the ongoing clinical trial of intratumoraJ administration of escalating doses of MV-CEA in patients with GBM will guide future translational efforts. Engineering the virus to express the soluble marker peptide CEA could allow us to monitor viral gene expression real-time and individualize treatment. If this hypothesis is proven, it could greatly facilitate monitoring of viral replication, the latter representing a real challenge in glioma trials, as repeat biopsies are not always safe or ethically justified. Tumor resection five days after viral administration, as planned in the ongoing trial, will also allow us to address tumor distribution following viral administration, a key determinant of efficacy.
As with other viral systems, ongoing research and possible further modification of the virus based on clinical trial feedback may be necessary in order to fully realize the therapeutic potential of this approach. Better understanding of viral biology and the mechanism of measles-induced fusion as well as cell membrane fusogenicity could be exploited to further increase viral potency. Synergistic combinations with chemotherapy, RT and small molecules represent directions worth exploring. Virus strains armed with therapeutic transgenes, such as MV-NIS (expressing the sodium iodine symporter gene) [41] are also being tested as antiglioma agents. Patients’ immune response and the extent of intratumoral spread are possible limitations, which could decrease the antitumor efficacy of oncolytic viruses. Use of cell carriers such as endothelial cells could represent a possible solution to this problem [42,43]. In addition, combination with immunosuppressive agents and novel delivery methods such as convection-enhanced delivery could address some of these limitations. Ongoing experiments will investigate the translational applicability of these approaches, with the ultimate goal being systemic delivery of measles derivatives that can reach and specifically replicate in CNS tumors.
Acknowledgments
Declaration of interest Supported by P50 CA 108961 and R21 CA 123839.
Bibliography
Papers of special note have been highlighted as either of interest (•) or of considerable interest (••) to readers.
- 1.Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2006. CA Cancer J Clin. 2006;56(2):106–30. doi: 10.3322/canjclin.56.2.106. [DOI] [PubMed] [Google Scholar]
- 2.Galanis E, Buckner JC. Diffuse cerebral gliomas in adults. In: Noseworthy JH, editor. Neurological Therapeutics: Principles and Practice. Abingdon: Informa Healthcare; 2006. pp. 832–53. [Google Scholar]
- 3.Dorig RE, Marcil A, Chopra A, Richardson CD. The human CD46 molecule is a receptor for measles virus (Edmonston strain) Cell. 1993;75(2):295–305. doi: 10.1016/0092-8674(93)80071-l. [DOI] [PubMed] [Google Scholar]
- 4.Naniche D, Varior-Krishnan G, Cervoni F, et al. Human membrane cofactor protein (CD46) acts as a cellular receptor for measles virus. J Virol. 1993;67(10):6025–32. doi: 10.1128/jvi.67.10.6025-6032.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ulasov IV, Tyler MA, Zheng S, Han Y, Lesniak MS. CD46 represents a target for adenoviral gene therapy of malignant glioma. Hum Gene Ther. 2006;17:556–64. doi: 10.1089/hum.2006.17.556. [DOI] [PubMed] [Google Scholar]
- 6.Tatsuo H, Ono N, Tanaka K, Yanagi Y. SLAM (CDw150) is a cellular receptor for measles virus. Nature. 2000;406(6798):893–7. doi: 10.1038/35022579. [DOI] [PubMed] [Google Scholar]
- 7.Cutts FT, Markowitz LE. Successes and failures in measles control. J Infect Dis. 1994;170(Suppl 1):s32–41. doi: 10.1093/infdis/170.supplement_1.s32. [DOI] [PubMed] [Google Scholar]
- 8.Greentree LB. Hodgkin’s disease: therapeutic role of measles vaccine. Am J Med. 1983;75(6):928. doi: 10.1016/0002-9343(83)90865-3. [DOI] [PubMed] [Google Scholar]
- 9.Schattner A. Therapeutic role of measles vaccine in Hodgkin’s disease. Lancet. 1984;1(8369):171. doi: 10.1016/s0140-6736(84)90112-0. [DOI] [PubMed] [Google Scholar]
- 10.Galanis E, Bateman A, Johnson K, et al. Use of viral fusogenic membrane glycoproteins as novel therapeutic transgenes in gliomas. Hum Gene Ther. 200l;12(7):811–21. doi: 10.1089/104303401750148766. [DOI] [PubMed] [Google Scholar]
- 11.Collatz E, Von Kleist S, Burtin P. Further investigations of circulating antibodies in colon cancer patients: on the autoantigenicity of the carcinoembryonic antigen. Int J Cancer. 1971;8(2):298–303. doi: 10.1002/ijc.2910080215. [DOI] [PubMed] [Google Scholar]
- 12.Ura Y, Ochi Y, Hamazu M, et al. Studies on circulating antibody against carcinoembryonic antigen (CEA) and CEA-like antigen in cancer patients. Cancer Lett. 1985;25(3):283–95. doi: 10.1016/s0304-3835(15)30008-2. [DOI] [PubMed] [Google Scholar]
- 13.Dabbs DJ. Diagnostic lmmunohistochemistry. Churchill Livingstone; Philadelphia, PA: 2002. [Google Scholar]
- 14.Ishikura A, Hunaki N, Watanabe K. Brain metastases of colorectal cancer – a case report. Gan No Rinsho. 1987;33(2):188–92. [PubMed] [Google Scholar]
- 15.Peng KW, Teneyck CJ, Galanis E, et al. Intraperitoneal therapy of ovarian cancer using an engineered measles virus. Cancer Res. 2002;62(16):4656–62. [PubMed] [Google Scholar]
- 16.Peng KW, Facteau S, Wegman T, O’Kane D, Russell SJ. Non-invasive in vivo monitoring of trackable viruses expressing soluble marker peptides. Nat Med. 2002;8(5):527–31. doi: 10.1038/nm0502-527. •• First demonstration that oncolytic measles virus Edmonston-vaccine strains can be engineered to express trackable peptides.
- 17.Phuong LK, Allen C, Peng KW, et al. Use of a vaccine strain of measles virus genetically engineered to produce carcinoembryonic antigen as a novel therapeutic agent against glioblastoma multiforme. Cancer Res. 2003;63(10):2462–9. •• First in vitro and in vivo demonstration of significant antitumor activity of oncolytic measles virus strains against gliomas.
- 18.Anderson BD, Nakamura T, Russell SJ, Peng KW. High CD46 receptor density determines preferential killing of tumor cells by oncolytic measles virus. Cancer Res. 2004;64(14):4919–26. doi: 10.1158/0008-5472.CAN-04-0884. [DOI] [PubMed] [Google Scholar]
- 19.Mcquaid S, Cosby SL. An immunohistochemical study of the distribution of the measles virus receptors, CD46 and SLAM, in normal human tissues and subacute sclerosing panencephalitis. Lab Invest. 2002;82(4):403–9. doi: 10.1038/labinvest.3780434. [DOI] [PubMed] [Google Scholar]
- 20.Shusta EV, Zhu C, Boado RJ, Pardridge WM. Subtractive expression cloning reveals high expression of CD46 at the blood–brain barrier. J Neuropathol Exp Neurol. 2002;61(7):597–604. doi: 10.1093/jnen/61.7.597. [DOI] [PubMed] [Google Scholar]
- 21.Giannini C, Sarkaria JN, Saito A, et al. Patient rumor EGFR and PDGFRA gene amplifications retained in an invasive intracranial xenograft model of glioblastoma multiforme. Neuro Oncol. 2005;7(2):164–76. doi: 10.1215/S1152851704000821. • Development of orthocopic glioma models deriving from GBM patients, which maintain the molecular characteristics and invasiveness of the original human tumor.
- 22.Mrkic B, Pavlovic J, Rulicke T, et al. Measles virus spread and pathogenesis in genetically modified mice. J Virol. l998;72(9):7420–7. doi: 10.1128/jvi.72.9.7420-7427.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Driesse MJ, Vincent AJ, Sillevis Smitt PA, et al. Intracerebral injection of adenovirus harboring the HSVtk gene combined with ganciclovir administration: toxicity study in nonhuman primates. Gene Ther. 1998;5(8):1122–9. doi: 10.1038/sj.gt.3300695. [DOI] [PubMed] [Google Scholar]
- 24.Myers R, Harvey ME, Greiner SM, et al. Safety of repeat intracerebral administration of MV-CEA in Rhesus macaques in support of a Phase I/II clinical trial for patients with recurrent gliomas. Mol Ther. 2006;13(Suppl 1):s113. doi: 10.1089/hum.2008.035. Abstract 297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maenpaa A, Junnikkaia S, Hakulinen J, et al. Expression of complement membrane regulators membrane cofactor protein (CD46), decay accelerating factor (CD55), and protectin (CD59) in human malignant gliomas. Am J Pathol. 1996;148:1139–52. [PMC free article] [PubMed] [Google Scholar]
- 26.Shinoura N, Heffelfinger SC, Miller M, et al. RNA expression of complement regulatory proteins in human brain tumors. Cancer Lett. 1994;86:143–9. doi: 10.1016/0304-3835(94)90072-8. [DOI] [PubMed] [Google Scholar]
- 27.Allen C, Vongpunsawad S, Nakamura T, et al. Retargeted oncolytic measles strains entering via the EGFRvIII receptor maintain significant antitumor activity against gliomas with increased tumor specificity. Cancer Res. 2006;66(24):11840–50. doi: 10.1158/0008-5472.CAN-06-1200. • A study demonstrating that MV retargeting against glioma-specific antigens is feasible without loss of potency, but with increased specificity.
- 28.Paraskevakou G, Allen C, Nakamura T, et al. Epidermal growth factor receptor (EGFR)-retargetcd measles virus strains effectively target EGFR-or EGFRvIII expressing gliomas. Mol Ther. 2007;15(4):677–86. doi: 10.1038/sj.mt.6300105. [DOI] [PubMed] [Google Scholar]
- 29.Nakamura T, Peng KW, Harvey M, et al. Rescue and propagation of fully retargeted oncolytic measles viruses. Nat Biotechnol. 2005;23:209–14. doi: 10.1038/nbt1060. • Important reference describing technology allowing measles retargeting.
- 30.Vongpunsawad S, Oezgun N, Braun W, Cattanco R. Selectively receptor-blind measles viruses: identification of residues necessary for SLAM- or CD46-induced fusion and their localization on a new hemagglutinin structural model. J Virol. 2004;78(1):302–13. doi: 10.1128/JVI.78.1.302-313.2004. • Identification of mutations in measles H protein that ablate entry via the natural receptors CD46 or SLAM.
- 31.Allen C, Paraskevakou G, Iankov I, et al. IL13 displaying retargeted oncolytic measles virus (MV) strains have significant activity and improved therapeutic index against gliomas. Mol Ther. 2007;15(Suppl 1):s22. Abstract 51. [Google Scholar]
- 32.Liu C, Sarkaria JN, Allen C, et al. Combination of oncolytic measles virus strains and radiation therapy has synergisitic activity in the treatment of glioblastoma multiforme. Clin Cancer Res. 2007;13(23):7155–65. doi: 10.1158/1078-0432.CCR-07-1306. [DOI] [PubMed] [Google Scholar]
- 33.Schowalter RM, Wurth MA, Aguilar HC, et al. Rho GTPase activity modulates paramyxovirus fusion protein-mediated cell–cell fusion. Virology. 2006;350(2):323–34. doi: 10.1016/j.virol.2006.01.033. [DOI] [PubMed] [Google Scholar]
- 34.Immonen A, Vapalahti M, Tyynela K, et al. AdvHSV-tk gene therapy with intravenous ganciclovir improves survival in human malignant glioma: a randomised, controlled study. Mol Ther. 2004;10(5):967–72. doi: 10.1016/j.ymthe.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 35.Lang FF, Bruner JM, Fuller GN, et al. Phase I trial of adenovirus-mediated p53 gene therapy for recurrent glioma: biological and clinical results. J Clin Oncol. 2003;21(13):2508–18. doi: 10.1200/JCO.2003.21.13.2508. [DOI] [PubMed] [Google Scholar]
- 36.Ram Z, Culver KW, Oshiro EM, et al. Therapy of malignant brain tumors by intratumoral implantation of retroviral vector-producing cells. Nat Med. 1997;3(12):1354–61. doi: 10.1038/nm1297-1354. [DOI] [PubMed] [Google Scholar]
- 37.Chiocca EA, Abbed KM, Tatter S, et al. A Phase I open-label, dose-escalation, multi-institutional trial of injection with an E1B-attenuated adenovirus, ONYX-015, into the peritumoral region of recurrent malignant gliomas, in the adjuvant setting. Mol Ther. 2004;10(5):958–66. doi: 10.1016/j.ymthe.2004.07.021. [DOI] [PubMed] [Google Scholar]
- 38.Freeman AI, Zakay-Rones Z, Gomori JM, et al. Phase I/II trial of intravenous NDV-HUJ oncolytic virus in recurrent glioblastoma multiforme. Mol Ther. 2006;13(1):221–8. doi: 10.1016/j.ymthe.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 39.Markert JM, Medlock MD, Rabkin SD, et al. Conditionally replicating herpes simplex virus mutant, G207 for the treatment of malignant glioma: results of a Phase I trial. Gene Ther. 2000;7(10):867–74. doi: 10.1038/sj.gt.3301205. [DOI] [PubMed] [Google Scholar]
- 40.Forsyth PA, Roldan G, George D, et al. A Phase I trial of intratumoral (i.t.) administration of reovirus in patients with histologically confirmed recurrent malignant gliomas (MGs) ASCO Ann Meeting Proc Part I. 2006;24(18s):1563. doi: 10.1038/sj.mt.6300403. [DOI] [PubMed] [Google Scholar]
- 41.Dingli D, Peng KW, Harvey ME, et al. Image-guided radiovirotherapy for multiple myeloma using a recombinant measles virus expressing the thyroidal sodium iodide symporter. Blood. 2004;103(5):1641–6. doi: 10.1182/blood-2003-07-2233. [DOI] [PubMed] [Google Scholar]
- 42.Iankov ID, Blechacz B, Liu C, et al. Infected cell carriers: a new strategy for systemic delivery of oncolytic measles viruses in cancer virotherapy. Mol Ther. 2007;15(1):114–22. doi: 10.1038/sj.mt.6300020. [DOI] [PubMed] [Google Scholar]
- 43.Wei J, Wahl J, Nakamura T, et al. Targeted release of oncolytic measles virus by blood outgrowth endothelial cells in situ inhibits orthotopic gliomas. Gene Ther. 2007;14(22):1573–86. doi: 10.1038/sj.gt.3303027. [DOI] [PubMed] [Google Scholar]


