Prion diseases are uniformly fatal, often rapidly progressive, neurodegenerative diseases resulting from the transformation and accumulation of a native protein, the prion protein, into an abnormally shaped protein, called the prion. Human prion diseases, such as Creutzfeldt-Jakob disease (CJD), come in three forms: sporadic, genetic, and acquired (such as variant CJD).1 Many therapeutic strategies have been tested as potential treatments for prion diseases in cell cultures and in animals.2 Unfortunately, drugs that work in cell culture have generally not worked as well in animals, and the few drugs reported to work in animal models were beneficial only in the early, preclinical phase of the disease. When assessed in human beings in case series or case reports, these drugs showed no clear long-term clinical efficacy.3,4 So far, only one randomised controlled trial of human prion disease, with the opioid-like analgesic flupirtine, has been published.5 However, no significant benefit was seen for either the primary outcome (cognitive function) or the secondary outcome (survival).5 In 2001, a paper reported on the effectiveness of the antimalarial drug quinacrine (also known as mepacrine) in eliminatation of prions from a cell-culture model of prion disease.4 Because quinacrine has been used for many decades and has a well described safety and tolerability profile, the UK Medical Research Council designed a trial of quinacrine for the treatment of prion disease, known as PRION-1. In this issue of The Lancet Neurology, Collinge and co-workers6 present the results of this first UK trial to treat human prion diseases with quinacrine.
PRION-1 was initially intended to be a partially randomised, patient-preference treatment trial, but ultimately this trial was only an observational study—albeit an important and well designed one. This trial offered patients with any form of prion disease the choice of entering one of three arms of an unblinded study: randomisation to receive quinacrine immediately or after 6 months; immediate quinacrine; or no quinacrine. Some patients chose to change group during the study. Primary endpoints were death and treatment response.
Collinge and co-workers present data from 107 pa tients with prion disease in both the main PRION-1 study (84 patients) and an earlier pilot study (23 patients; six were offered open-label quinacrine and 17 were offered either quinacrine or no quinacrine). Because only one patient chose the randomisation arm at enrolment, the study is effectively an observational study that compared patients who chose quinacrine with those who did not. Patients who chose to receive quinacrine differed from those who chose to not receive the study treatment. More than twice as many patients chose not to receive quinacrine as chose to receive it, and patients with the least cognitive impairment (based on the mini-mental state examination) and best level of function (based on clinical dementia rating and Barthel index) tended to choose the quinacrine arm. Additionally, more patients with genetic forms of prion disease chose the quinacrine arm and more patients with the sporadic form of the disease chose no quinacrine compared with patients with other forms of the disease (although disease severity might have accounted for this; the more severe the disease, the less likely the patients were to choose quinacrine). These differences make a fair comparison of the two cohorts impractical.
After adjusting for several confounding factors, no significant difference in survival was seen between those who chose quinacrine at enrolment and those who did not. The fact that the only patients who had “transient response” (ie, improvements) received quinacrine is encouraging, but whether this response was due to a quinacrine-related side-effect, such as hypomania,7 or to a possible anti-prion effect is not clear. Another unanswered question is whether quinacrine prolongs survival: although some patients had a transient improvement, quinacrine did not notably reverse the disease, similar to findings of other published reports.8,9
Despite the limitations of the overall trial design (essentially being an observational study and therefore similar to an earlier, smaller French study8), PRION-1 was a well planned, detailed, and thorough prospective study. Perhaps the most important part of PRION-1 was the extensive neurological assessments with standardised neurological, cognitive, functional, and behavioural data collected at regular intervals. Notably, the results of this study show that treatment trials for rare, rapidly progressive, and fatal diseases are possible. The most important outcome from PRION-1 might be the forthcoming quantitative clinical data on secondary endpoints prospectively quantifying the course of human prion diseases, which will help researchers to design better clinical treatment trials for patients with prion disease.
Although randomised, double-blinded, placebo-controlled studies are the preferred gold standard for trial design, patients with a rapidly fatal disease commonly want whatever treatment is available and might be reluctant to participate in placebo-controlled trials. Observational studies, however, are fraught with confounding factors, and the results are often disproven when the studies are repeated in a more controlled manner. In the USA, our centre at the University of California, San Francisco, CA, recently completed enrolment in a randomised, double-blinded, placebo-controlled study of quinacrine in sporadic CJD.4,10 Another similarly designed study, with the antibiotic doxycycline, is underway in Italy for all forms of prion disease. Whatever the findings of these studies, quinacrine and doxycycline are unlikely to be the “penicillin” for CJD and more effective treatments are needed for prion diseases.2
Future studies will need a design (ie, fully randomised, double blinded, and placebo controlled) that provides unequivocal answers on treatment efficacy. In the long term, we should strive to provide our patients with the best designs for clinical trials.11 Additionally, as Collinge and co-workers also note, earlier and improved diagnosis is a crucial advance that will add more power to future trials.
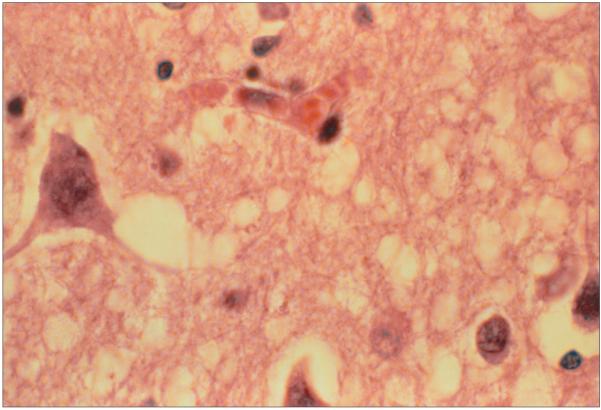
Light micrograph of a section through the brain of a patient with Creutzfeldt-Jakob disease
Acknowledgments
I am an investigator in a related treatment trial of quinacrine for sporadic CJD. My research in CJD is funded by the US National Institutes of Health and the Michael J Homer Fund.
References
- 1.Prusiner SB. Shattuck lecture—neurodegenerative diseases and prions. N Engl J Med. 2001;344:1516–26. doi: 10.1056/NEJM200105173442006. [DOI] [PubMed] [Google Scholar]
- 2.Trevitt CR, Collinge J. A systematic review of prion therapeutics in experimental models. Brain. 2006;129:2241–65. doi: 10.1093/brain/awl150. [DOI] [PubMed] [Google Scholar]
- 3.Bone I. In: Intraventricular pentosan polysulfate in human prion diseases. A study of experience in the United Kingdom. Unit UKCS, editor. Edinburgh, UK: 2006. pp. 1–11. [Google Scholar]
- 4.Korth C, May BCH, Cohen FE, Prusiner SB. Acridine and phenothiazine derivatives as pharmacoptherapeutics for prion disease. Proc Natl Acad Sci USA. 2001;98:9836–41. doi: 10.1073/pnas.161274798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Otto M, Cepek L, Ratzka P, et al. Efficacy of fl upirtine on cognitive function in patients with CJD: a double-blind study. Neurology. 2004;62:714–18. doi: 10.1212/01.wnl.0000113764.35026.ef. [DOI] [PubMed] [Google Scholar]
- 6.Collinge J, Gorham M, Hudson F, et al. Safety and efficacy of quinacrine in human prion disease (PRION-1 study): a patient-preference trial. Lancet Neurol. 2009;8:334–44. doi: 10.1016/S1474-4422(09)70049-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Engel GL. Quinacrine effects on the central nervous system. JAMA. 1966;197:505. [PubMed] [Google Scholar]
- 8.Haik S, Brandel JP, Salomon D, et al. Compassionate use of quinacrine in Creutzfeldt-Jakob disease fails to show significant effects. Neurology. 2004;63:2413–15. doi: 10.1212/01.wnl.0000148596.15681.4d. [DOI] [PubMed] [Google Scholar]
- 9.Nakajima M, Yamada T, Kusuhara T, et al. Results of quinacrine administration to patients with Creutzfeldt-Jakob disease. Dement Geriatr Cogn Disord. 2004;17:158–63. doi: 10.1159/000076350. [DOI] [PubMed] [Google Scholar]
- 10.CJD (Creutzfeldt-Jakob disease) quinacrine study http://clinicaltrials.gov/ct2/show/NCT00183092 (accessed March 4, 2009)
- 11.Kennedy A, Walker S, Thomas D, Rossor M, Darbyshire J, Collinge J. Quinacrine in possible or probable CJD. BMJ. 2002;324:239. [Google Scholar]