Synopsis
Thrombocytopenia in the neonate is most commonly acquired but may in rare cases be due to a congenital disorder. This review will summarize the diagnosis, pathophysiology and management of two congenital inherited platelet disorders that present in the newborn period, congenital amegakaryocytic thrombocytopenia (CAMT) and thrombocytopenia with absent radii (TAR).
Additional keywords: neonatal thrombocytopenia, c-Mpl, inherited thrombocytopenia
Introduction
Thrombocytopenia is a relatively common clinical problem in hospitalized neonates, and it is critical to distinguish infants with rare congenital thrombocytopenias from those with acquired disorders. Two well-described inherited thrombocytopenia syndromes that present in the newborn period include congenital amegakaryocytic thrombocytopenia (CAMT) and thrombocytopenia with absent radii (TAR). Although both are characterized by severe (<50,000/μl) thrombocytopenia at birth, the molecular mechanisms underlying these disorders as well as their clinical presentations and courses are distinct. CAMT is an autosomal recessive disorder due to mutations in the thrombopoietin (TPO) receptor c-Mpl. TAR is a syndrome of variable inheritance and unclear genetic etiology consisting of thrombocytopenia in association with bilateral absent radii and frequently additional congenital abnormalities. This chapter will summarize our current understanding of the pathophysiology and clinical course of CAMT and TAR.
CAMT: presentation and differential diagnosis
CAMT is an autosomal recessive disorder that presents at birth with severe thrombocytopenia. Mean platelet counts at diagnosis are 21,000/μl, and platelets are of normal size and morphology 1. Importantly, phenotypic findings in CAMT are usually limited to those related to thrombocytopenia, such as cutaneous and intracranial hemorrhages. An increased incidence of psychomotor retardation has been described in patients with CAMT, although some neurologic abnormalities may be sequelae of intracranial bleeding 1. Because no specific congenital malformations are characteristic of CAMT, consideration should be given to an alternative syndrome if such malformations are present.
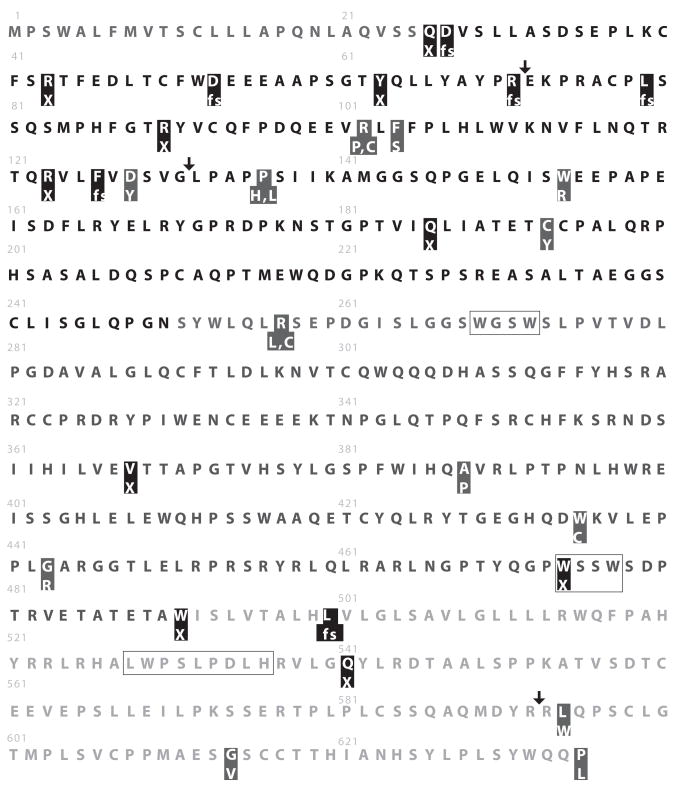
Bone marrow evaluation in newborns with CAMT typically demonstrates normal overall cellularity with an isolated reduction or absence of megakaryocytes 1, although in some cases marrows studied early in the course of the disease can have misleadingly minimal findings and serial marrows may be required to clarify the diagnosis (Fox et al., submitted and 2). Although originally a clinical diagnosis, CAMT can now be molecularly defined by mutations involving the TPO receptor c-Mpl 3, 4. Mutations have been identified throughout c-Mpl and include nonsense, missense and splicing mutations (Fox et al., unpublished data and 2, 4–11), although in severely affected patients mutations are frequently located in exons 2 and 3, which encode the first cytokine receptor homology domain (Figure 1). Some patients with CAMT have inherited two different mutations of c-Mpl, resulting in a compound heterozygous state, whereas in families with consanguinity the inheritance of homozygous mutations is more common. Clinically certified mutation analysis of c-Mpl can now be obtained at GeneDx (Gaithersburg, MD) and Prevention Genetics (Marshfield, Wisconsin).
Figure 1.
Summary of reported c-Mpl mutations in CAMT. Amino acids are represented as single letters. The signal peptide (residues 1–25) is shown in dark gray, the extracellular domain of the receptor (residues 26–491) in black and the intracellular domain of the receptor (residues 492–635) in light gray. The WSXW motifs and Box 1 are noted with open boxes. Identified mutations are highlighted and the resulting changes are listed below. Changes resulting in stop codons (X) and frameshifts (fs) are highlighted with black whereas substitutions are highlighted in gray. Arrows indicate the positions of splicing mutations.
Another diagnostic evaluation that is useful in establishing the diagnosis of CAMT is determination of the plasma TPO level. In CAMT, plasma levels of TPO are high, consistent with severely reduced platelet production and absence of c-Mpl 3. The relationship between TPO and thrombopoiesis reflects the normal metabolism of TPO, which is produced at a constant rate by the liver and removed from the circulation by receptor-mediated uptake and destruction 12–14. c-Mpl receptors expressed on megakaryocytes and platelets are responsible for the majority of TPO uptake 15. In CAMT, impaired expression of c-Mpl means that there is little if any receptor-mediated TPO destruction and therefore circulating levels of the cytokine increase to as much as 10-fold above those seen in normal controls. By comparison, in disorders such as immune thrombocytopenia where c-Mpl is normal and thrombocytopenia is caused by platelet destruction TPO levels are normal or only modestly elevated 16, 17. Elevated TPO levels are not specific for CAMT and can be elevated in other conditions in which there is severely impaired production of megakaryocytes and platelets (for example, in acquired aplastic anemia); however, in the appropriate clinical setting a highly elevated TPO level supports a diagnosis of CAMT and justifies further confirmation by specific gene sequencing.
CAMT is a rare cause of thrombocytopenia in the newborn period; much more frequent etiologies include prenatal factors (such as pre-eclampsia, placental insufficiency and intrauterine growth retardation), anoxic insult, infection, or maternal transfer of platelet allo- or autoantibodies. The timing of onset, severity of thrombocytopenia, clinical history and maternal platelet counts are often helpful in identifying underlying factors contributing to neonatal thrombocytopenia 18. Neonatal alloimmune thrombocytopenia (NAIT) is an especially important cause of severe thrombocytopenia that must be differentiated from CAMT. Like CAMT, NAIT typically presents as severe thrombocytopenia in an otherwise normal newborn whose mother’s platelets are normal. NAIT is more common than CAMT (1:1000-1:2000 live births 19, 20), compared to less than 100 reported cases of CAMT. DNA-based platelet phenotyping can establish if there is incompatibility between maternal and paternal platelet antigens that would predispose to alloimmunization, and serologic assays using patient or maternal serum may detect platelet-specific alloantibodies 21–23. Bone marrow aspiration is not usually required to diagnose NAIT but if performed typically shows normal to increased megakaryocytes. Following birth the maternally derived platelet alloantibody diminishes and after the first month of life the expectation is that platelet counts will improve. Even with antigen incompatibility consistent with the possibility of NAIT, if thrombocytopenia does not resolve after 3 months, alternative diagnoses such as CAMT should be explored (Fox et al., submitted).
CAMT: Pathophysiology
Platelets are produced by bone marrow megakaryocytes, which like all blood cells are derived from the hematopoietic stem cell. Although many cytokines and factors contribute to the growth and maturation of megakaryocytes, TPO is required for normal thrombopoiesis 24–27. Consistent with the critical role of TPO signaling in megakaryocyte and platelet development, deletion of TPO or c-Mpl in mouse models results in severe thrombocytopenia with reduction of platelet counts to 10% of normal values 27, 28. However, it was discovered that hematopoietic progenitors and stem cells are also reduced to approximately 10% of normal values in c-Mpl and TPO-null mice 27, 29, 30. Thus, TPO is critical not only for thrombopoiesis but also for maintenance of the hematopoietic stem cell compartment. Clinical confirmation of this experimental finding came in 1999 when mutations in c-Mpl were discovered in children with CAMT 4, a disease characterized not only by thrombocytoptenia but also by the development of bone marrow failure. It is now well established that the lack of TPO signaling in CAMT due to absent or defective c-Mpl expression leads to impaired megakaryocyte and platelet production and ultimately aplastic anemia in affected patients 3, 4.
Further studies of patients with CAMT have described two classes of c-Mpl mutation, type I and type II 1, 5. Type I mutations completely eliminate receptor signaling through disruption of all or most of the intracellular domain, often through creation of a stop codon or frameshift. Type II mutations typically create amino acid substitutions or altered splice sites that result in a small degree of residual receptor signaling. One of the most frequently identified mutations in CAMT involves the substitution of proline for arginine at position 102 in the extracellular domain, a non-conservative change that is predicted to significantly alter change receptor conformation. In contrast, another common amino acid substitution has been described (methionine for valine at residue 114) which is not associated with disease 8. The mechanisms by some substitutions interfere with signaling are not obvious and further study using structural or cell line models may lead to new insights into interactions between c-Mpl and its ligand or other signaling molecules.
Although c-Mpl mutations cause thrombocytopenia in CAMT, other mutations that alter c-Mpl and TPO signaling are associated with thrombocytosis. Constitutional mutations in the transmembrane domain of c-Mpl that lead to persistent receptor activation have been described in familial thrombocytosis 31, and acquired mutations in c-Mpl or its associated kinase Jak2 that promote chronic activation of signaling are found in approximately 50% of patients with essential thrombocythemia and almost all patients with polycythemia vera 32–37. A receptor variant called c-Mpl Baltimore has been described in which a substitution in the extracellular domain of the receptor leads to reduced expression of c-Mpl and paradoxically increased platelet counts 38, possibly due to the relatively increased availability of circulating TPO. Thus, alterations of c-Mpl signaling may contribute not only to thrombocytopenia but also to thrombocytosis.
Not all children with thrombocytopenia and a clinical picture resembling CAMT can be shown to have c-Mpl mutations, and therefore it is possible that other genetic loci for this disease exist. For example, because TPO is the only known ligand for c-Mpl, mutations that eliminate or severely reduce circulating TPO would be predicted to cause a clinical picture identical to CAMT. In fact, TPO-null mice phenocopy c-Mpl-null mice 30, but mutations leading to the absence of TPO have not been described in humans. Whether there is active selection against TPO mutations in humans or whether they have simply not yet been discovered is not known. Children with CAMT who do not have demonstrable mutations in c-Mpl may have novel mutations affecting c-Mpl transcription or other components of the TPO signaling pathway; further research is needed to understand the etiology of thrombocytopenia in such patients.
CAMT: Clinical course and management
Thrombocytopenia in patients with CAMT can have a variable clinical course 1. Whereas infants with type I receptor mutations generally remain thrombocytopenic and have a rapid progression to trilineage bone marrow failure (mean onset 1yr 11 mo of age), infants with type II mutations may show transient modest improvement of platelet counts during the first year of life and have a delayed onset of marrow failure (mean onset 5 yr of age) 1. Nevertheless, with rare exceptions most patients with CAMT go on to develop bone marrow failure. Importantly, patients with CAMT are also at increased risk for the development of myelodysplasia and acute myeloid leukemia 39. The mechanism by which absence of c-Mpl predisposes to malignancy is not understood, but it is possible that the environment of impaired hematopoiesis selects for the outgrowth of abnormal clones 40.
Supportive care in patients with CAMT consists primarily of platelet transfusion as well as adjunctive therapies such as fibrinolytic inhibitors to manage bleeding symptoms, and red cell transfusions and antibiotics if needed. The use of alternative cytokines to stimulate thrombopoiesis has shown some efficacy in mouse models 41 but clinical use has been limited by toxicity. Given the lack of functional c-Mpl in hematopoietic stem cells and megakaryocytic progenitors it is unlikely that currently available TPO-mimetics will be therapeutically useful in this disease (Fox et al., submitted and 42). Gene therapy, while an attractive strategy for correction of the stem cell defect 43, 44, has not been studied clinically in CAMT and concerns regarding its potential leukemogenicity remain.
Currently, the only definitive treatment for the long-term management of patients with CAMT is hematopoietic stem cell transplantation. HLA typing for the patient and siblings should be obtained at the time of diagnosis to direct management decisions. Transplantation with a matched sibling donor is the treatment of choice 1, 45, 46. Siblings who are heterozygous carriers of the c-Mpl mutation have been used successfully as stem cell donors 9. Outcomes are less favorable for patients without a matched sibling donor, with failures due to delayed engraftment, rejection, GVHD and regimen-related toxicity having been reported 1, 47, 48. Although the numbers of patients are very small, haploidentical donors have been used as an alternative to unrelated donors with some success 1, 45. The optimal timing for transplantation is not known but has been suggested to be before pancytopenia develops, thus limiting transfusion exposures and risk for infections that could compromise transplant outcomes. In the review by King and colleagues, 15 of 20 patients received transplants at a median age of 38 months (range 7–89 months) 1. Further studies are needed to optimize donor selection and conditioning regimens for patients with CAMT, particularly those who lack a matched sibling donor.
TAR: Presentation and diagnosis
TAR is a clinically-defined syndrome characterized by thrombocytopenia and bilateral radial aplasia with thumbs present 49, 50. At birth thrombocytopenia may be of variable severity, with platelet counts ranging from 10–100,000/μl and platelets that are normal in size and granularity. Bone marrow examination typically demonstrates a reduction in the size and number of bone marrow megakaryocytes, and if obtained plasma TPO levels are usually elevated 51, 52. Although bilateral radial aplasia is the defining skeletal feature in TAR, additional skeletal abnormalities are frequently observed, including more extensive upper limb malformations, phocomelia, and lower limb malformations in as many as 50% of the patients 53. Non-skeletal abnormalities are also common, including gastroenteritis and cow’s milk intolerance in 47%, renal malformations in 23%, cardiac defects in 15%, facial dysmorphism in 53%, short stature in 95%, macrocephaly in 76% and capillary hemangiomata in 24% 53. Thus, when a child is born with absent radii, a multi-system evaluation with genetics and orthopedics consultations should be initiated to detect and manage associated congenital malformations.
Although TAR is distinctive, several syndromes have interesting phenotypic similarities to TAR. Amegakaryocytic thrombocytopenia with radioulnar synostosis (ATRUS) is a rare disorder characterized by neonatal thrombocytopenia in association with proximal fusion of the radius and ulna 54. This skeletal finding may be discovered by demonstration of limited supination of the wrist or detected by radiographic evaluation. In two unrelated families with autosomal dominant transmission of ATRUS, genetic analysis revealed heterozygous inheritance of a point mutation in the homeobox gene HoxA11 which leads to truncation of this transcription factor within its DNA binding domain 55. Studies using a cell line model demonstrated that over-expression of this truncated HoxA11 impairs megakaryocytic differentiation 56, whereas in mouse models deletion of HoxA11 is associated with forelimb abnormalities 57. Further studies are needed to define the role of HoxA11 in hematopoiesis. Despite their association with ATRUS, Hox gene mutations have not been identified in TAR 58. Radial abnormalities and thrombocytopenia may also be found in Fanconi’s Anemia (FA), a chromosomal instability syndrome with a constellation of findings that may include bone marrow failure, predisposition to malignancy, skeletal malformations, abnormal pigmentation and growth failure 59. Although FA may present with thrombocytopenia, hematopoietic findings are not usually present at birth and therefore the timing of onset of thrombocytopenia should distinguish between FA and TAR or ATRUS; additionally, upper limb abnormalities in FA patients often involve the thumbs, whereas in TAR thumbs are characteristically normal. The diagnosis of FA can be confirmed by examining peripheral blood lymphocytes for the increased chromosomal breakage in the presence of clastogenic agents such as diepoxybutane or mitomycin C.
TAR: Pathophysiology
Despite significant interest, the molecular basis of TAR is not yet known. The inheritance pattern of TAR is complex, and autosomal recessive as well as autosomal dominant with variable penetrance inheritance patterns have been reported. Females are over-represented (27:7) 53. As with CAMT, plasma TPO levels in patients with TAR are elevated, and studies of patients with TAR reveal that megakaryocyte maturation is blocked and signaling in response to TPO is abnormal 60–62; nevertheless, no mutations in c-Mpl or its associated kinase Jak2 have been identified 61, 63 and the underlying reason for this signaling defect is not understood. Recently an interstitial microdeletion involving chromosome 1q was identified in a cohort of 30 individuals with TAR 64. Although all affected patients carried the microdeletion, in approximately 75% of the cases the microdeletion was identified in an unaffected parent, suggesting that co-inheritance of an additional, unknown modifier is required for the expression of the disease. Nevertheless, there are eleven genes within this critical region, including a negative regulator of STAT3, an integrin subunit and a ribosomal binding protein, and these genes now provide novel candidates for proteins that could be involved in the pathogenesis of TAR; in addition, these proteins may have previously unsuspected and important functions in megakaryopoiesis.
Any mechanism proposed for impaired megakaryopoiesis in TAR must account for the observation that platelet counts typically recover spontaneously to near normal levels after the first year of life. This pattern has led some to postulate that the defect underlying TAR is relatively specific for fetal megakaryocytes. Although the differences between fetal and adult megakaryopoiesis remain poorly understood, it is clear that fetal and adult megakaryocytes respond differently to cytokine stimulation and have different potentials for proliferation and maturation 65. Insights into the basis of TAR could have implications for our understanding of megakaryopoiesis during fetal development.
TAR: Clinical course and management
Although CAMT and TAR both involve abnormal TPO signaling, the clinical course of the two disorders is very different. Although patients with CAMT nearly always develop bone marrow failure, in TAR platelet counts generally improve over the first year of life and can eventually approach normal adult levels. Marrow failure is generally not seen. However, as with CAMT, patients with TAR have been reported to develop both acute myeloid and lymphoid leukemias 66–68, suggesting that this disorder is also associated with a predisposition to malignancy. Nevertheless, lymphocytes from patients with TAR do not exhibit abnormal chromosomal instability 53 and an explanation for this tendency to develop cancer will require a better molecular understanding of the disorder.
Because thrombocytopenia tends to remit, the treatment of TAR is largely supportive with platelet transfusions in the first year of life as needed to control bleeding symptoms and facilitate orthopedic or other procedures. Much of the clinical management following the first year of life will be directed towards the non-hematologic manifestations of this disorder. Hematopoietic stem cell transplantation is generally not indicated, although matched related donor transplantation has been successfully performed in a child with TAR and unusually persistent thrombocytopenia 69. The advent of TPO-agonists for the stimulation of platelet production offers an exciting new possibility for a targeted therapy in TAR, but this approach may be of limited efficacy if plasma levels of endogenous TPO are high and megakaryocytes have a downstream signaling defect. There are case reports of patients in whom thrombocytopenia has responded to alternative cytokines such as erythropoietin and IL-6 70, 71. Following resolution of the thrombocytopenia, long-term monitoring of patients for late recurrence of thrombocytopenia or leukemia is recommended.
Summary
Thrombocytopenia in the newborn period can have diverse etiologies but among them it is important to consider congenital disorders such as CAMT and TAR. Making the correct diagnosis is critical for optimal patient management, although not all patients with inherited thrombocytopenia will fulfill criteria for a known disorder. Few physicians outside of large referral centers will encounter more than one or a few patients with these rare diseases, and therefore participation in national or international registries may be helpful in gaining access to specialized testing. Widespread participation in registries will also facilitate additional studies into the molecular basis, long-term outcomes and development of novel therapies for inherited thrombocytoptenias, and the discovery of new mutations may provide insights into TPO signaling and thrombopoiesis.
Acknowledgments
The author would like to thank Norma E. Fox for ongoing essential research contributions, Kenneth Kaushansky for critical review of the manuscript and Monica Gudea for valuable administrative assistance.
The author receives research support from R01DK049858 and Amgen.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Literature cited
- 1.King S, Germeshausen M, Strauss G, Welte K, et al. Congenital amegakaryocytic thrombocytopenia: a retrospective clinical analysis of 20 patients. Br J Haematol. 2005 Dec;131(5):636–644. doi: 10.1111/j.1365-2141.2005.05819.x. [DOI] [PubMed] [Google Scholar]
- 2.Rose MJ, Nicol KK, Skeens MA, Gross TG, et al. Congenital amegakaryocytic thrombocytopenia: The diagnostic importance of combining pathology with molecular genetics. Pediatr Blood Cancer. 2008 Jan 31; doi: 10.1002/pbc.21453. [DOI] [PubMed] [Google Scholar]
- 3.Ballmaier M, Germeshausen M, Schulze H, et al. c-mpl mutations are the cause of congenital amegakaryocytic thrombocytopenia. Blood. 2001 Jan 1;97(1):139–146. doi: 10.1182/blood.v97.1.139. [DOI] [PubMed] [Google Scholar]
- 4.Ihara K, Ishii E, Eguchi M, et al. Identification of mutations in the c-mpl gene in congenital amegakaryocytic thrombocytopenia. Proc Natl Acad Sci U S A. 1999 Mar 16;96(6):3132–3136. doi: 10.1073/pnas.96.6.3132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Germeshausen M, Ballmaier M, Welte K. MPL mutations in 23 patients suffering from congenital amegakaryocytic thrombocytopenia: the type of mutation predicts the course of the disease. Hum Mutat. 2006 Mar;27(3):296. doi: 10.1002/humu.9415. [DOI] [PubMed] [Google Scholar]
- 6.Steinberg O, Gilad G, Dgany O, et al. Congenital amegakaryocytic thrombocytopenia-3 novel c-MPL mutations and their phenotypic correlations. J Pediatr Hematol Oncol. 2007 Dec;29(12):822–825. doi: 10.1097/MPH.0b013e318158152e. [DOI] [PubMed] [Google Scholar]
- 7.Passos-Coelho JL, Sebastiao M, Gameiro P, et al. Congenital amegakaryocytic thrombocytopenia--report of a new c-mpl gene missense mutation. Am J Hematol. 2007 Mar;82(3):240–241. doi: 10.1002/ajh.20756. [DOI] [PubMed] [Google Scholar]
- 8.Gandhi MJ, Pendergrass TW, Cummings CC, et al. Congenital amegakaryocytic thrombocytopenia in three siblings: molecular analysis of atypical clinical presentation. Exp Hematol. 2005 Oct;33(10):1215–1221. doi: 10.1016/j.exphem.2005.06.017. [DOI] [PubMed] [Google Scholar]
- 9.Muraoka K, Ishii E, Ihara K, et al. Successful bone marrow transplantation in a patient with c-mpl-mutated congenital amegakaryocytic thrombocytopenia from a carrier donor. Pediatr Transplant. 2005 Feb;9(1):101–103. doi: 10.1111/j.1399-3046.2005.00247.x. [DOI] [PubMed] [Google Scholar]
- 10.van den Oudenrijn S, Bruin M, Folman CC, et al. Mutations in the thrombopoietin receptor, Mpl, in children with congenital amegakaryocytic thrombocytopenia. Br J Haematol. 2000 Aug;110(2):441–448. doi: 10.1046/j.1365-2141.2000.02175.x. [DOI] [PubMed] [Google Scholar]
- 11.Savoia A, Balduini CL, Savino M, et al. Autosomal dominant macrothrombocytopenia in Italy is most frequently a type of heterozygous Bernard-Soulier syndrome. Blood. 2001 Mar 1;97(5):1330–1335. doi: 10.1182/blood.v97.5.1330. [DOI] [PubMed] [Google Scholar]
- 12.Kuter DJ, Rosenberg RD. The reciprocal relationship of thrombopoietin (c-Mpl ligand) to changes in the platelet mass during busulfan-induced thrombocytopenia in the rabbit. Blood. 1995 May 15;85(10):2720–2730. [PubMed] [Google Scholar]
- 13.Nagata Y, Shozaki Y, Nagahisa H, et al. Serum thrombopoietin level is not regulated by transcription but by the total counts of both megakaryocytes and platelets during thrombocytopenia and thrombocytosis. Thromb Haemost. 1997 May;77(5):808–814. [PubMed] [Google Scholar]
- 14.Yang C, Li YC, Kuter DJ. The physiological response of thrombopoietin (c-Mpl ligand) to thrombocytopenia in the rat. Br J Haematol. 1999 May;105(2):478–485. [PubMed] [Google Scholar]
- 15.Geddis AE, Fox NE, Kaushansky K. The Mpl receptor expressed on endothelial cells does not contribute significantly to the regulation of circulating thrombopoietin levels. Exp Hematol. 2006 Jan;34(1):82–86. doi: 10.1016/j.exphem.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 16.Kunishima S, Tahara T, Kato T, et al. Serum thrombopoietin and plasma glycocalicin concentrations as useful diagnostic markers in thrombocytopenic disorders. Eur J Haematol. 1996 Jul;57(1):68–71. doi: 10.1111/j.1600-0609.1996.tb00492.x. [DOI] [PubMed] [Google Scholar]
- 17.Mukai HY, Kojima H, Todokoro K, et al. Serum thrombopoietin (TPO) levels in patients with amegakaryocytic thrombocytopenia are much higher than those with immune thrombocytopenic purpura. Thromb Haemost. 1996 Nov;76(5):675–678. [PubMed] [Google Scholar]
- 18.Roberts I, Stanworth S, Murray NA. Thrombocytopenia in the neonate. Blood Rev. 2008 Jul;22(4):173–186. doi: 10.1016/j.blre.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 19.Williamson LM, Hackett G, Rennie J, et al. The natural history of fetomaternal alloimmunization to the platelet-specific antigen HPA-1a (PlA1, Zwa) as determined by antenatal screening. Blood. 1998 Oct 1;92(7):2280–2287. [PubMed] [Google Scholar]
- 20.Panzer S, Auerbach L, Cechova E, et al. Maternal alloimmunization against fetal platelet antigens: a prospective study. Br J Haematol. 1995 Jul;90(3):655–660. doi: 10.1111/j.1365-2141.1995.tb05597.x. [DOI] [PubMed] [Google Scholar]
- 21.Bussel JB. Alloimmune thrombocytopenia in the fetus and newborn. Semin Thromb Hemost. 2001 Jun;27(3):245–252. doi: 10.1055/s-2001-15254. [DOI] [PubMed] [Google Scholar]
- 22.McFarland JG. Detection and identification of platelet antibodies in clinical disorders. Transfus Apher Sci. 2003 Jun;28(3):297–305. doi: 10.1016/S1473-0502(03)00049-1. [DOI] [PubMed] [Google Scholar]
- 23.Arnold DM, Smith JW, Kelton JG. Diagnosis and management of neonatal alloimmune thrombocytopenia. Transfus Med Rev. 2008 Oct;22(4):255–267. doi: 10.1016/j.tmrv.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 24.Kaushansky K. The mpl ligand: molecular and cellular biology of the critical regulator of megakaryocyte development. Stem Cells. 1994;12(Suppl 1):91–96. discussion 96–97. [PubMed] [Google Scholar]
- 25.Kaushansky K, Lok S, Holly RD, et al. Promotion of megakaryocyte progenitor expansion and differentiation by the c-Mpl ligand thrombopoietin. Nature. 1994 Jun 16;369(6481):568–571. doi: 10.1038/369568a0. [DOI] [PubMed] [Google Scholar]
- 26.Bartley TD, Bogenberger J, Hunt P, et al. Identification and cloning of a megakaryocyte growth and development factor that is a ligand for the cytokine receptor Mpl. Cell. 1994 Jul 1;77(7):1117–1124. doi: 10.1016/0092-8674(94)90450-2. [DOI] [PubMed] [Google Scholar]
- 27.Alexander WS, Roberts AW, Maurer AB, et al. Studies of the c-Mpl thrombopoietin receptor through gene disruption and activation. Stem Cells. 1996;14 (Suppl 1):124–132. doi: 10.1002/stem.5530140716. [DOI] [PubMed] [Google Scholar]
- 28.Gurney AL, Carver-Moore K, de Sauvage FJ, et al. Thrombocytopenia in c-mpl-deficient mice. Science. 1994 Sep 2;265(5177):1445–1447. doi: 10.1126/science.8073287. [DOI] [PubMed] [Google Scholar]
- 29.Alexander WS, Roberts AW, Nicola NA, et al. Deficiencies in progenitor cells of multiple hematopoietic lineages and defective megakaryocytopoiesis in mice lacking the thrombopoietic receptor c-Mpl. Blood. 1996 Mar 15;87(6):2162–2170. [PubMed] [Google Scholar]
- 30.Carver-Moore K, Broxmeyer HE, Luoh SM, et al. Low levels of erythroid and myeloid progenitors in thrombopoietin-and c-mpl-deficient mice. Blood. 1996 Aug 1;88(3):803–808. [PubMed] [Google Scholar]
- 31.Ding J, Komatsu H, Wakita A, et al. Familial essential thrombocythemia associated with a dominant-positive activating mutation of the c-MPL gene, which encodes for the receptor for thrombopoietin. Blood. 2004 Jun 1;103(11):4198–4200. doi: 10.1182/blood-2003-10-3471. [DOI] [PubMed] [Google Scholar]
- 32.Levine RL, Wadleigh M, Cools J, et al. Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell. 2005 Apr;7(4):387–397. doi: 10.1016/j.ccr.2005.03.023. [DOI] [PubMed] [Google Scholar]
- 33.Vainchenker W, Constantinescu SN. A Unique Activating Mutation in JAK2 (V617F) Is at the Origin of Polycythemia Vera and Allows a New Classification of Myeloproliferative Diseases. Hematology (Am Soc Hematol Educ Program) 2005:195–200. doi: 10.1182/asheducation-2005.1.195. [DOI] [PubMed] [Google Scholar]
- 34.Baxter EJ, Scott LM, Campbell PJ, et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet. 2005 Mar 19–25;365(9464):1054–1061. doi: 10.1016/S0140-6736(05)71142-9. [DOI] [PubMed] [Google Scholar]
- 35.James C, Ugo V, Le Couedic JP, et al. A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature. 2005 Apr 28;434(7037):1144–1148. doi: 10.1038/nature03546. [DOI] [PubMed] [Google Scholar]
- 36.Kralovics R, Passamonti F, Buser AS, et al. A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med. 2005 Apr 28;352(17):1779–1790. doi: 10.1056/NEJMoa051113. [DOI] [PubMed] [Google Scholar]
- 37.Pikman Y, Lee BH, Mercher T, et al. MPLW515L is a novel somatic activating mutation in myelofibrosis with myeloid metaplasia. PLoS Med. 2006 Jul;3(7):e270. doi: 10.1371/journal.pmed.0030270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moliterno AR, Williams DM, Gutierrez-Alamillo LI, et al. Mpl Baltimore: a thrombopoietin receptor polymorphism associated with thrombocytosis. Proc Natl Acad Sci U S A. 2004 Aug 3;101(31):11444–11447. doi: 10.1073/pnas.0404241101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alter BP. Bone marrow failure syndromes in children. Pediatr Clin North Am. 2002 Oct;49(5):973–988. doi: 10.1016/s0031-3955(02)00031-7. [DOI] [PubMed] [Google Scholar]
- 40.Bagby GC, Meyers G. Bone marrow failure as a risk factor for clonal evolution: prospects for leukemia prevention. Hematology Am Soc Hematol Educ Program. 2007;2007:40–46. doi: 10.1182/asheducation-2007.1.40. [DOI] [PubMed] [Google Scholar]
- 41.Gainsford T, Roberts AW, Kimura S, et al. Cytokine production and function in c-mpl-deficient mice: no physiologic role for interleukin-3 in residual megakaryocyte and platelet production. Blood. 1998 Apr 15;91(8):2745–2752. [PubMed] [Google Scholar]
- 42.Tijssen MR, di Summa F, van den Oudenrijn S, et al. Functional analysis of single amino-acid mutations in the thrombopoietin-receptor Mpl underlying congenital amegakaryocytic thrombocytopenia. Br J Haematol. 2008 Jun;141(6):808–813. doi: 10.1111/j.1365-2141.2008.07139.x. [DOI] [PubMed] [Google Scholar]
- 43.Jin L, Siritanaratkul N, Emery DW, et al. Targeted expansion of genetically modified bone marrow cells. Proc Natl Acad Sci U S A. 1998 Jul 7;95(14):8093–8097. doi: 10.1073/pnas.95.14.8093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Richard RE, Blau CA. Small-molecule-directed mpl signaling can complement growth factors to selectively expand genetically modified cord blood cells. Stem Cells. 2003;21(1):71–78. doi: 10.1634/stemcells.21-1-71. [DOI] [PubMed] [Google Scholar]
- 45.Lackner A, Basu O, Bierings M, et al. Haematopoietic stem cell transplantation for amegakaryocytic thrombocytopenia. Br J Haematol. 2000 Jun;109(4):773–775. doi: 10.1046/j.1365-2141.2000.02099.x. [DOI] [PubMed] [Google Scholar]
- 46.Al-Ahmari A, Ayas M, Al-Jefri A, et al. Allogeneic stem cell transplantation for patients with congenital amegakaryocytic thrombocytopenia (CAT) Bone Marrow Transplant. 2004 Apr;33(8):829–831. doi: 10.1038/sj.bmt.1704445. [DOI] [PubMed] [Google Scholar]
- 47.MacMillan ML, Davies SM, Wagner JE, et al. Engraftment of unrelated donor stem cells in children with familial amegakaryocytic thrombocytopenia. Bone Marrow Transplant. 1998 Apr;21(7):735–737. doi: 10.1038/sj.bmt.1701147. [DOI] [PubMed] [Google Scholar]
- 48.Gluckman E, Wagner JE. Hematopoietic stem cell transplantation in childhood inherited bone marrow failure syndrome. Bone Marrow Transplant. 2008 Jan;41(2):127–132. doi: 10.1038/sj.bmt.1705960. [DOI] [PubMed] [Google Scholar]
- 49.Hall JG, Levin J, Kuhn JP, et al. Thrombocytopenia with absent radius (TAR) Medicine (Baltimore) 1969 Nov;48(6):411–439. doi: 10.1097/00005792-196948060-00001. [DOI] [PubMed] [Google Scholar]
- 50.Hedberg VA, Lipton JM. Thrombocytopenia with absent radii. A review of 100 cases. Am J Pediatr Hematol Oncol. 1988 Spring;10(1):51–64. doi: 10.1097/00043426-198821000-00010. [DOI] [PubMed] [Google Scholar]
- 51.Ballmaier M, Schulze H, Strauss G, et al. Thrombopoietin in patients with congenital thrombocytopenia and absent radii: elevated serum levels, normal receptor expression, but defective reactivity to thrombopoietin. Blood. 1997 Jul 15;90(2):612–619. [PubMed] [Google Scholar]
- 52.Homans AC, Cohen JL, Mazur EM. Defective megakaryocytopoiesis in the syndrome of thrombocytopenia with absent radii. Br J Haematol. 1988 Oct;70(2):205–210. doi: 10.1111/j.1365-2141.1988.tb02465.x. [DOI] [PubMed] [Google Scholar]
- 53.Greenhalgh KL, Howell RT, Bottani A, et al. Thrombocytopenia-absent radius syndrome: a clinical genetic study. J Med Genet. 2002 Dec;39(12):876–881. doi: 10.1136/jmg.39.12.876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Thompson AA, Woodruff K, Feig SA, et al. Congenital thrombocytopenia and radio-ulnar synostosis: a new familial syndrome. Br J Haematol. 2001 Jun;113(4):866–870. doi: 10.1046/j.1365-2141.2001.02834.x. [DOI] [PubMed] [Google Scholar]
- 55.Thompson AA, Nguyen LT. Amegakaryocytic thrombocytopenia and radio-ulnar synostosis are associated with HOXA11 mutation. Nat Genet. 2000 Dec;26(4):397–398. doi: 10.1038/82511. [DOI] [PubMed] [Google Scholar]
- 56.Horvat-Switzer RD, Thompson AA. HOXA11 mutation in amegakaryocytic thrombocytopenia with radio-ulnar synostosis syndrome inhibits megakaryocytic differentiation in vitro. Blood Cells Mol Dis Jul-Aug. 2006;37(1):55–63. doi: 10.1016/j.bcmd.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 57.Boulet AM, Capecchi MR. Multiple roles of Hoxa11 and Hoxd11 in the formation of the mammalian forelimb zeugopod. Development. 2004 Jan;131(2):299–309. doi: 10.1242/dev.00936. [DOI] [PubMed] [Google Scholar]
- 58.Fleischman RA, Letestu R, Mi X, et al. Absence of mutations in the HoxA10, HoxA11 and HoxD11 nucleotide coding sequences in thrombocytopenia with absent radius syndrome. Br J Haematol. 2002 Feb;116(2):367–375. doi: 10.1046/j.1365-2141.2002.03263.x. [DOI] [PubMed] [Google Scholar]
- 59.Alter BP. Bone marrow failure: a child is not just a small adult (but an adult can have a childhood disease) Hematology (Am Soc Hematol Educ Program) 2005:96–103. doi: 10.1182/asheducation-2005.1.96. [DOI] [PubMed] [Google Scholar]
- 60.Letestu R, Vitrat N, Masse A, et al. Existence of a differentiation blockage at the stage of a megakaryocyte precursor in the thrombocytopenia and absent radii (TAR) syndrome. Blood. 2000 Mar 1;95(5):1633–1641. [PubMed] [Google Scholar]
- 61.Ballmaier M, Schulze H, Cremer M, et al. Defective c-Mpl signaling in the syndrome of thrombocytopenia with absent radii. Stem Cells. 1998;16 (Suppl 2):177–184. doi: 10.1002/stem.5530160720. [DOI] [PubMed] [Google Scholar]
- 62.al-Jefri AH, Dror Y, Bussel JB, Freedman MH. Thrombocytopenia with absent radii: frequency of marrow megakaryocyte progenitors, proliferative characteristics, and megakaryocyte growth and development factor responsiveness. Pediatr Hematol Oncol. 2000 Jun;17(4):299–306. doi: 10.1080/088800100276280. [DOI] [PubMed] [Google Scholar]
- 63.Strippoli P, Savoia A, Iolascon A, et al. Mutational screening of thrombopoietin receptor gene (c-mpl) in patients with congenital thrombocytopenia and absent radii (TAR) Br J Haematol. 1998 Nov;103(2):311–314. doi: 10.1046/j.1365-2141.1998.00991.x. [DOI] [PubMed] [Google Scholar]
- 64.Klopocki E, Schulze H, Strauss G, et al. Complex inheritance pattern resembling autosomal recessive inheritance involving a microdeletion in thrombocytopenia-absent radius syndrome. Am J Hum Genet. 2007 Feb;80(2):232–240. doi: 10.1086/510919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pastos KM, Slayton WB, Rimsza LM, et al. Differential effects of recombinant thrombopoietin and bone marrow stromal-conditioned media on neonatal versus adult megakaryocytes. Blood. 2006 Nov 15;108(10):3360–3362. doi: 10.1182/blood-2006-04-018036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fadoo Z, Naqvi SM. Acute myeloid leukemia in a patient with thrombocytopenia with absent radii syndrome. J Pediatr Hematol Oncol. 2002 Feb;24(2):134–135. doi: 10.1097/00043426-200202000-00015. [DOI] [PubMed] [Google Scholar]
- 67.Go RS, Johnston KL. Acute myelogenous leukemia in an adult with thrombocytopenia with absent radii syndrome. Eur J Haematol. 2003 Apr;70(4):246–248. doi: 10.1034/j.1600-0609.2003.00054.x. [DOI] [PubMed] [Google Scholar]
- 68.Camitta BM, Rock A. Acute lymphoidic leukemia in a patient with thrombocytopenia/absent radii (Tar) syndrome. Am J Pediatr Hematol Oncol. 1993 Aug;15(3):335–337. [PubMed] [Google Scholar]
- 69.Brochstein JA, Shank B, Kernan NA, et al. Marrow transplantation for thrombocytopenia-absent radii syndrome. J Pediatr. 1992 Oct;121(4):587–589. doi: 10.1016/s0022-3476(05)81152-7. [DOI] [PubMed] [Google Scholar]
- 70.Dempfle CE, Burck C, Grutzmacher T, et al. Increase in platelet count in response to rHuEpo in a patient with thrombocytopenia and absent radii syndrome. Blood. 2001 Apr 1;97(7):2189–2190. doi: 10.1182/blood.v97.7.2189. [DOI] [PubMed] [Google Scholar]
- 71.Aquino VM, Mustafa MM, Vaickus L, et al. Recombinant interleukin-6 in the treatment of congenital thrombocytopenia associated with absent radii. J Pediatr Hematol Oncol. 1998 Sep-Oct;20(5):474–476. doi: 10.1097/00043426-199809000-00013. [DOI] [PubMed] [Google Scholar]