Abstract
Economic recessions, the industrial shift from manufacturing toward service industries, and rising global competition have contributed to uncertainty about job security, with potential consequences for workers’ health. To address limitations of prior research on the health consequences of perceived job insecurity, we use longitudinal data from two nationally-representative samples of the United States population, and examine episodic and persistent perceived job insecurity over periods of about three years to almost a decade. Results show that persistent perceived job insecurity is a significant and substantively important predictor of poorer self-rated health in the American’s Changing Lives (ACL) and Midlife in the United States (MIDUS) samples, and of depressive symptoms among ACL respondents. Job losses or unemployment episodes are associated with perceived job insecurity, but do not account for its association with health. Results are robust to controls for sociodemographic and job characteristics, negative reporting style, and earlier health and health behaviors.
Keywords: USA, perceived job insecurity, self-rated health, depressive symptoms
INTRODUCTION
Dramatic labor market changes have led to a rising sense that long-term relationships between employers and workers are becoming a thing of the past (Cappelli, Bassi, Katz, Knoke, Osterman, and Useem 1997; Hacker 2006). Economic recessions, the industrial shift from manufacturing toward service industries, and rising global competition have led to reductions of permanent employees through layoffs and plant closings, contributing to uncertainty about job security in recent years (Fullerton and Wallace 2007). The consequences of perceived job insecurity have received increasing popular and scholarly attention, and a limited number of studies have shown a negative association with health across a variety of national and organizational contexts (e.g., Cheng, Chen, Chen, and Chiang 2005; McDonough 2000). Existing studies have some important limitations, however. Some use cross-sectional data, leaving open the question of whether insecure workers actually become less healthy, or alternatively, if unhealthy workers are more likely to report that their jobs are insecure (Sverke, Gallagher, and Hellgren 2000). Those that use longitudinal data adjust for measures of prior health and other individual characteristics to address potential reverse causation due to health selection, and continue to find an impact of perceived insecurity on subsequent health (De Witte 1999; Dekker and Schaufeli 1995; Ferrie, Shipley, Marmot, Stansfeld, and Smith 1998; Heaney, Israel, and House 1994; Hellgren and Sverke 2003). But these longitudinal studies generally have used only a single point-in-time measure of perceived job insecurity and have not explored job losses or unemployment as an alternative explanation for a relationship between perceived insecurity and health. Moreover, existing longitudinal studies are based on samples that may not generalize across workers in the United States, where employment contracts have become less secure and worker protections have declined in the past several decades (Price and Burgard 2008).
Macroeconomic changes in the last several decades have generated a sense that no one is immune from instability at work (Elman and O’Rand 2002; Schmidt 2000) though a relatively smaller fraction of the U.S. labor force experiences job loss due to these changes. If perceived job insecurity is associated with health decline net of objective employment disruptions, it could represent an even wider population health threat than job loss or unemployment. A better understanding of the distribution and consequences of perceived job insecurity in the United States is needed to improve scientific understanding that can inform policy and intervention there, with potential implications for other societies as well.
How Does Perceived Job Insecurity affect Health?
An individual worried about losing a job may experience stress due to anticipation about the problems associated with a job loss, mental strain associated with being in a powerless position, and ambiguity about the future (Heaney, Israel, and House 1994; Joelson and Wahlquist 1987). Perceived job insecurity is not a socially-visible event like job loss or unemployment, but an internal experience for which there are no obvious appropriate responses and no institutionalized supports. Also, people experiencing perceived job insecurity cannot employ instrumental strategies of coping because of the persistent uncertainty about whether or not the feared employment instability will actually occur. These circumstances make perceived insecurity potentially as stressful, or perhaps even more stressful, than actual job losses or unemployment episodes (Hartley, Jacobson, Klandermans, and van Vuuren 1991; Lazarus 1966). Workers’ responses to the stress of perceived job insecurity in the shorter term could be emotional (anxiety, tension, dissatisfaction), physiological (elevated heart rate, increased catecholamine secretion) and behavioral (drug use, absenteeism, lack of concentration), while in the longer term, the accumulation of these responses could result in more permanent and manifest adverse consequences for mental and physical health (Gazzaniga and Heatherton 2003; Heaney, Israel, and House 1994).
Measurement and Meaning of Perceived Job Insecurity
While some studies have classified people as experiencing job insecurity if they work at a factory or organization that has announced layoffs or closure (e.g., Ferrie, Shipley, Marmot, Stansfeld, and Smith 1995; Iversen, Sabroe, and Damsgaard 1989; Kasl, Cobb, and Brooks 1968; Mattiasson, Lindgarde, Nilsson, and Theorell 1990), others have asked individuals in broader, population-based samples how likely they think it is that they will lose their job (e.g., Cheng, Chen, Chen, and Chiang 2005; McDonough 2000). The latter strategy more specifically targets “perceived” job insecurity, and is the approach we take in the present study. While there are clear advantages to plant closure studies, most notably that preexisting health problems of individual workers are less likely to be the underlying cause of their job insecurity, there are also limitations. For example, when a plant is scheduled to close all workers are exposed to the same threat of actual job loss, making it nearly impossible to disentangle the contribution of perceived job insecurity – that exists before the plant closes – from the objective employment insecurity that these workers will experience when it does close. Moreover, even given the same objective employment conditions, the perception and consequences of perceived job insecurity may vary across individuals based on their appraisal of the context and their situation (Greenhalgh and Rosenblatt 1984; Hartley, Jacobson, Klandermans, and van Vuuren 1991). For these reasons, and to examine associations across the population of U.S. workers, we use self-reported measures of perceived job insecurity obtained from nationally-representative samples of adults working in a variety of objective employment situations.
Perceived job insecurity is a subjective experience and must be self-reported, so there are challenges to obtaining a reliable assessment of its impact on subsequent health. When using respondents’ self-reports of their health as outcome measures, any association with perceived job insecurity may be spurious if an underlying negative reporting style determines respondents’ reports of both outcome (health) and predictor (insecurity) (Brief, Burke, George, Robinson, and Webster 1988; Watson and Clark 1984). We include a measure of an individual’s level of neuroticism in all multivariate analyses; longitudinal analyses using repeated measures of perceived job insecurity and self-reported health also help to reduce the influence of other stable underlying traits that cause individuals to report in a consistently negative way.
Prior Research and Limitations
There have been a few prospective studies of the association between perceived job insecurity and subsequent health, but most have relied on measurement of perceived job insecurity at a single time point (e.g., Lee, Colditz, Berkman, and Kawachi 2004), such that we know relatively little about whether workers with more persistent exposure are likely to fare worse than their counterparts with briefer exposure. Two prospective studies have shown the poorest health outcomes for those who perceived job insecurity at both of two measurement points, one study with measurements in 1986 and 1987 (Heaney, Israel, and House 1994), and the other with measurements in 1995/6 and 1997/99 (Ferrie, Shipley, Stansfeld, and Marmot 2002). Ferrie and colleagues (2002) also showed that respondents who became insecure after baseline, and those who were insecure at baseline but not at follow-up, generally had worse health than the never insecure, but better health than the persistently insecure.
Even methodologically-rigorous prospective studies generally have not addressed the possibility that the perceived job insecurity–health relationship is spurious, generated by unmeasured objective employment insecurity. Job losses and unemployment experiences have been linked to negative health consequences for workers in the United States in many studies (Burgard, Brand, and House 2007; Gallo, Bradley, Dubin, Jones, Falba, Teng, and Kasl 2006; Gallo, Teng, Falba, Kasl, Krumholz, and Bradley 2006; Kessler, Turner, and House 1989; Turner 1995). A recent job loss could predict both current perceived job insecurity and subsequent health decline, or workers worried about losing their jobs may be predicting an actual spell of unemployment in the near future, which then acts as the true cause of subsequent health decline.
The few studies that have considered objective employment insecurity have produced mixed results. One population-based prospective study designed to assess the impact of the 1974–75 U.S. recession on the well-being of full-time workers and the potential mediators of that association considered repeated measures of perceived job insecurity and actual unemployment experiences in 1973 and 1977. Rather than creating a categorical indicator of episodic and persistent insecurity as in the studies discussed above, Tausig and Fenwick (1999) used an indicator of perceived job insecurity in 1973 and an indicator of change in perceived insecurity between 1973 and 1977. They found that perceived job insecurity and change in insecurity were not associated with a measure of general distress in 1977. However, a study of state employees in Australia showed that those who perceived job insecurity in 1990 and lost their jobs by 1991 showed a reduction in psychological distress, while those who remained both employed and insecure in 1990 and 1991 showed significantly higher psychological distress (Dekker and Schaufeli 1995).
A final limitation of existing studies is that findings may not generalize across workers in the United States. For example, past studies examining perceived insecurity at multiple time points used samples of employees of a single Michigan automotive factory (Heaney, Israel, and House 1994) and white collar civil servants in Britain (Ferrie, Shipley, Stansfeld, and Marmot 2002), while the sole nationally-representative study of U.S. workers with multiple measures of insecurity used data from the mid-1970s (Tausig and Fenwick 1999). Since then macroeconomic conditions have changed drastically. Studies of perceived job insecurity based on more recently collected nationally-representative data have been conducted in Western Europe (e.g., Rugulies, Bultmann, Aust, and Burr 2006), Canada (McDonough 2000), and Taiwan (Cheng, Chen, Chen, and Chiang 2005), where benefits for displaced workers, unionization, and employer latitude to lay-off and fire workers vary considerably.
Study Design and Hypotheses
Our study includes several innovations that build on the extant literature. We examined episodic and persistent perceived insecurity, comparing our findings across two large, nationally-representative samples of U.S. adults. These studies covered different historical periods and made it possible to examine the robustness of results over follow up periods of three years versus almost ten years. We also examined job losses or unemployment both prior to the first measurement of perceived job insecurity, and over the period of follow-up, to untangle their potential contributions. Based on the prior evidence and gaps therein, we examined several hypotheses:
Hypothesis 1: Perceived job insecurity is associated with subsequent health among U.S. workers;
Hypothesis 2: Persistent exposure to perceived job insecurity is associated with worse health consequences than episodic exposure;
Hypothesis 3: The association between perceived job insecurity and health is not completely explained by job losses or unemployment episodes.
DATA AND METHODS
Data
Two complementary data sources are used to examine the relationship between perceived job insecurity and health over about twenty years of recent history. The American’s Changing Lives (ACL) study is a stratified, multi-stage area probability sample of non-institutionalized adults 25 years and older living in the United States in 1986, with oversampling of adults 60 and older and of African Americans (House, Lantz, and Herd 2005). Face-to-face interviews lasting approximately 90 minutes were conducted at baseline (Wave 1), with response rates of 70 percent for households and 68 percent for individuals, and follow-up face-to-face interviews (Wave 2) were conducted with 83 percent of survivors in 1989. Follow up surveys were also conducted in 1994 and 2001/2, but information on perceived job insecurity was not collected, so these are not used. Sample weights to adjust for oversampling of special populations, sample non-response and non-coverage as of Wave 1, and loss to follow-up due to attrition or death by Wave 2 are used in all descriptive and multivariate analyses. The analytic sample included ACL respondents who were employed at Wave 1 (N = 1,867), who responded to the survey in Wave 2 (N = 1,550) and who had complete information on all covariates (N=1,507). The Midlife in the United States (MIDUS) study is a nationally-representative survey of English-speaking Americans aged 25 to 74, initiated in 1995–96. Thirty minute telephone interviews and two mailed self-administered questionnaires were used at baseline (Wave 1) and in a follow-up interview (Wave 2) in 2005. Response rates in 1995 for the main random digit-dialed sample used here were 70 percent for the phone interview and 87 percent for the self-administered questionnaire (among those who completed a phone interview), for an overall response rate of 61 percent. Follow up phone interviews were conducted in 2005 with 71 percent of known survivors from 1995–96, and 80 percent of these retuned a self-administered questionnaire. Sample weights for Wave 2 have been designed to correct for selection probabilities and non-response, and are used in all descriptive and multivariate analyses. The analytic sample included MIDUS respondents who were employed at Wave 1 (N = 1,712), who responded to the survey in Wave 2 (N = 1,254) and who had complete information on all covariates (N=1,216).
By comparing these two samples, we obtain information about one period of declining unemployment, from about 7 percent in 1986 to about 5 percent in 1989, and a longer period during which unemployment fell but then rose again, so that the rate was about 5.5 percent in both 1995 and 2005. The baseline survey waves for each survey were collected a few years after much higher cyclical peaks in the U.S. unemployment rate, at around 10 percent in 1983 and 7.5 percent in 1992.
Measures
Health Outcomes
We use overall self-rated health and depressive symptoms (ACL)/negative affect (MIDUS) as health outcomes. Self-rated health is measured in both samples with a single item: “How would you rate your health at the present time?” with five response categories ranging from poor (1) to excellent (5). Self-rated health has been shown to be a reliable, valid measure of health, and is predictive of subsequent functional decline and mortality (Idler and Benyamini 1997) and physical health among adults of working age, despite our limited understanding of the complexities of how individuals rate their health (Schnittker 2005).
As a second measure of health we use closely related, but distinct measures of mental well-being: depressive symptoms (ACL) and negative affect (MIDUS). These measures both capture symptoms of poor mental health, rather than diagnosable depression, and may provide a more sensitive indicator of recent changes in well-being. Depressive symptoms are measured in the ACL with an eleven-item version of the Center for Epidemiological Studies Depression Scale or CES-D (Radloff 1977). Responses to each item about how respondents felt in the past week are scored on a three-item Likert scale (1 = hardly ever, 2 = some of the time, 3 = most of the time) and scores of all available items are averaged (α = 0.82). The MIDUS negative affect index is based on a series of questions about negative sentiments drawn from a collection of related measures, including the CES-D. This index contains six items (α = 0.87). Respondents are asked about their feelings in the past 30 days, and responses to items are scored on a five-item Likert scale ranging from 1 = all of the time to 5 = none of the time, with all available items averaged. One identical overlapping item is used in the construction of the ACL and MIDUS indices: “I felt that everything I did was an effort.” Several other items used for each index overlap conceptually across samples, as shown in Appendix A, but these two indices of poor mental health are not interchangeable and results should be interpreted accordingly.
Appendix A.
Items Used in Construction of Indices of Depressive Symptoms (ACL) and Negative Affect (MIDUS)
| ACL Stem Question and Items |
In the past week…
|
| MIDUS Stem Question and Items |
| During the past 30 days, how much of the time did you feel… |
|
Perceived Job Insecurity
Indicators of perceived insecurity at Waves 1 and 2 are used to construct measures of episodic and persistent exposure to perceived job insecurity. ACL respondents employed for pay were asked in 1986 and 1989: “How likely is it that during the next couple of years you will involuntarily lose your main job – not at all likely, not too likely, somewhat likely, or very likely?” For ACL respondents, perceived job insecurity is dichotomized so that 0 = not insecure (not at all or not too likely to lose job) and 1 = insecure (somewhat or very likely to lose job); this dichotomization of job insecurity is consistent with several prior studies using similar measures (Elman and O’Rand 2002; Schmidt 2000). MIDUS respondents employed for pay in 1995 and 2005 were asked a similar question at each wave, though the emphasis was on keeping their job rather than losing it: “If you wanted to stay in your present job, what are the chances you could keep it for the next two years – excellent, very good, good, fair or poor?” For MIDUS respondents, perceived job insecurity is dichotomized so that 0 = not insecure (excellent or very good chance to stay in job) and 1 = insecure (good, fair or poor chance to stay in job). No studies have used the MIDUS item in dichotomized form, so we strove to achieve the greatest similarity in frequency of perceived insecurity between this and the ACL measure. Coded this way, the percentage of MIDUS respondents reporting insecurity in Wave 1 (16 percent) was similar to the percentage of ACL respondents who did so in Wave 1 (18 percent). Using data from the General Social Survey, Fullerton and Wallace (2007) show that the unadjusted percentage of respondents reporting that they were fairly or very likely to lose their job in the next 12 months was very similar in 1986 and 1996, so the stability in unadjusted perceived insecurity in our samples in 1986 and 1995 seems reasonable. We create an indicator of episodic and persistent perceived job insecurity with four categories: 0 = perceived insecurity at neither wave; 1 = Wave 1 only; 2 = Wave 2 only; and 3 = Waves 1 and 2.
Objective Employment Insecurity
We include measures of job loss among ACL respondents and of unemployment experience among MIDUS respondents. At each survey wave, ACL respondents were asked: “In the last three years, have you involuntarily lost a job for reasons other than retirement?” coded so that 0 = no job loss and 1 = job loss. We consider job losses occurring between 1983 and 1986, up to three years prior to Wave 1, and between 1986 and1989, between Waves 1 and 2. Information about recent involuntary job losses was not collected from MIDUS respondents, so we use respondents’ reports of unemployment in the past 12 months, coded so that 0 = no unemployment in the past year and 1 = at least one week of unemployment. Respondents were asked how many weeks they were unemployed, so we explored continuous and categorical specifications; multivariate results were substantively equivalent regardless of specification. We consider unemployment experiences in the 12 months prior to Wave 1 and in the 12 months preceding the Wave 2 interview.
Other Predictor Variables
To address the possibility that health selection influences estimates of the association between perceived job insecurity and health, we pursue two strategies. First, we control for measures of an individuals’ health prior to and concurrent with the Wave 1 measure of perceived job insecurity. For ACL respondents, we use self-reported occurrences and dates of serious or life-threatening illnesses or accidental injuries to construct an indicator of a health shock (0 = no shock, 1 = had shock) between 1983 and 1986. For MIDUS respondents we include a self-reported measure of the respondents’ mental health at age 16, coded so that 1= poor and 5 = excellent. To measure health at Wave 1 for ACL and MIDUS respondents, we include respondents’ self report of experiencing or being treated for hypertension in the past year (0 = no report and 1 = reported hypertension) and current smoking status (0 = nonsmoker and 1 = current smoker). These measures are used as indicators of health status and behavior that could both select workers into particular jobs and influence subsequent health directly. As a second strategy to address potential health selection, we also control for a baseline measure of the focal health outcome, either self-rated health or depressive symptoms/negative affect. This is a relatively strict control, as perceived insecurity measured at baseline may have been a problem for some time beforehand, and controlling for baseline health will thus reduce the apparent association between persistent perceived insecurity and subsequent health.
We also include a measure of neuroticism, a relatively stable underlying personality trait that may mark a negative reporting style. In the ACL we use a neuroticism index based on the four questions from the Eysenck Personality Inventory (Eysenck and Eysenck 1975), such as “Are you a worrier?” The standardized scale has a range from −1.2 (least neurotic) to 2.2 (most neurotic). For MIDUS respondents, a neuroticism index was available based on four items. Respondents were asked to “Please indicate how well each of the following describes you – not at all (1), a little (2), some (3), or a lot (4).” Items included in the index were: moody, worrying, nervous, and calm. Scores across items were averaged for all individuals reporting at least two items and range from 1 (least) to 4 (most neurotic).
Finally, multivariate analyses adjust additively for key sociodemographic characteristics and job characteristics that predict job insecurity and/or health. We include a measure of the respondent’s sex (0 = female, 1 = male) and age at baseline. We mean-center the respondent’s age for regression models to obtain a measure that denotes the difference from the average respondent’s age in that year. Respondent’s race is coded as 0 = non-Black or 1 = Black; there were not enough respondents of other racial/ethnic backgrounds to construct additional categories for the analysis. Marital status is coded so that 0 = married or living with a partner and 1 = unmarried/not living with a partner. We also tested an indicator that distinguished individuals with working spouses from those whose spouses did not work and from the unmarried; results did not differ from those presented. Educational attainment at baseline is coded as 0 = some college or more and 1 = high school graduate or less. We also include a measure of household income, reported in Table 1 in 2007 dollars, but transformed by taking the logarithm for multivariate analysis (a small positive constant of $500 was added before taking the logarithm so that individuals with no income are retained). We also include indicators of self-employment (0 = not self-employed, 1 = self-employed), as self-employed people may have greater control over their employment status, and part-time status (less than 35 hours per week), to indicate extent of involvement in paid work. Additional job characteristics were explored, including blue-collar versus white-collar occupation, major occupational group, occupational status, job strain, and indicators of the psychological salience of the job, but none added substantively to the analysis.
Table 1.
Means or Percentages for Dependent and Independent Variables for Respondents Working at Wave One, ACL and MIDUS Respondents
| ACL 1986–1989 |
MIDUS 1995–2005 |
|||
|---|---|---|---|---|
| Health Outcomes (Wave 2) | Mean / % | S.D | Mean / % | S.D |
| Self-Rated Health (1=Poor, 5=Excellent) | 3.76 | (0.899) | 3.59 | (0.966) |
| Depressive Symptoms/Negative Affect | ||||
| ACL (1=Low, 2.82=High) | 1.33 | (0.316) | -- | -- |
| MIDUS (1=Low, 5=High) | -- | -- | 1.54 | (0.595) |
| Perceived Job Insecurity | ||||
| % Perceived Job Insecurity Wave 1 | 17.9% | 15.9% | ||
| % Perceived Job Insecurity Wave 2a | 14.9% | 13.2% | ||
| Episodic and Persistent Insecurityb | ||||
| % Neither Wave | 74.0% | 76.9% | ||
| % Wave 1 only | 12.6% | 13.2% | ||
| % Wave 2 only | 8.1% | 7.2% | ||
| % Waves 1 and 2 | 5.3% | 2.7% | ||
| Objective Employment Insecurity | ||||
| % Job Loss 1983 – 1986 | 8.7% | -- | ||
| % Job Loss 1986 – 1989 | 8.2% | -- | ||
| % Any Unemployed Weeks 1994 | -- | 6.2% | ||
| % Any Unemployed Weeks 2004 | -- | 5.2% | ||
| Wave One and Earlier Health | ||||
| % Health Shock 1983–1986 | 16.3% | -- | ||
| Mental Health at Age 16 (1 = Poor, 5 = Excellent) | -- | 4.05 | (1.025) | |
| Self-rated Health Wave 1 | 4.00 | (0.881) | 3.61 | (0.888) |
| Depressive Symptoms/Negative Affect Wave 1 | ||||
| ACL (1=Low, 2.91=High) | 1.36 | (0.330) | -- | |
| MIDUS (1=Low, 5=High) | -- | 1.55 | (0.592) | |
| Neuroticism Wave 1 | ||||
| ACL (−1.2 = Low, 2.2 =High) | −0.082 | (0.950) | -- | |
| MIDUS (1 =Low, 4 =High) | -- | 2.27 | (0.667) | |
| % High Blood Pressure | 13.4% | 13.9% | ||
| % Current Smoker | 30.8% | 22.0% | ||
| Sociodemographic Characteristics at Wave 1 | ||||
| % Male | 53.6% | 43.7% | ||
| Age | 41.2 | (11.85) | 43.4 | (11.21) |
| % Black Race | 9.9% | 8.1% | ||
| % Unmarried/Unpartnered | 23.6% | 22.4% | ||
| % <=High School Education | 47.0% | 42.9% | ||
| Household Income in 2007 dollars | 66,958 | (43,690) | 64,660 | (48,688) |
| % Self Employed | 16.7% | 16.1% | ||
| % Part time (<35 hrs/wk) | 18.2% | 21.2% | ||
| Working at Wave 1 & Wave 2 | 91.8% | 74.6% | ||
|
|
||||
| N | 1507 | 1216 | ||
Note : Figures are weighted, column total Ns unweighted. All variables refer to survey wave one except as noted (ACL: 1986, MIDUS: 1995).
Values for respondents working in wave 2 (ACL N = 1,302; MIDUS N = 893).
Values presented for respondents working in wave 1 or waves 1 and 2, though only those working in both waves are eligible for latter two categories.
Data Analysis
All analyses are conducted using Stata software version 10.0 SE. For multivariate analyses we estimate ordinary least squares (OLS) regression models with robust standard errors. We found no evidence for significant problems of multicollinearity; the variance inflation factor ranges from 1.04 to 1.45 for all independent variables. We also tested an ordinal logistic regression specification for models of self-rated health, but results were consistent with those presented here, so we present the more easily interpretable and parsimonious OLS estimates. OLS approaches rely on the strong assumption that unmeasured factors are uncorrelated with included covariates, so fixed effects specifications are preferred in causal modeling, where the outcome is specified as the difference between the post- and pre-treatment measures (Allison 1994; Halaby 2004). While preferring the fixed effects approach, however, Allison argues that both this and the “regressor variable” method used here (i.e., a baseline measure of the health outcome of interest is included as a predictor) account for empirical patterns in observational studies and that each has strengths. We pursue the regressor variable method because the conventional fixed effects approach drops all participants whose exposure does not change over time, eliminating respondents with persistent exposure to perceived job insecurity, a group of particular interest in our analysis.
In all regression models we use Wave 2 survey weights to adjust for loss to follow up. In addition, we estimate models using all respondents working at Wave 1 and responding to the survey in Wave 2, even those who had left paid employment by Wave 2. Retaining only those working at both Wave 1 and 2 may introduce selectivity into the analytic sample, particularly for the MIDUS sample with its much longer follow up period. Results presented here are consistent with those obtained from a more restricted sample of respondents working at both survey waves.
RESULTS
Means and standard deviations or percentages of dependent and independent variables are presented in Table 1, separately for ACL and MIDUS respondents. Variables measured differently across samples are presented on separate rows.
Table 1 shows that average self-rated health at Wave 2 is similar for ACL and MIDUS respondents at 3.6 to 3.8, reflecting scores close to “very good.” Average levels of depressive symptoms/negative affect fall in the lower end of the possible ranges for both ACL respondents (mean: 1.3, range: 1.0 – 2.8) and MIDUS respondents (mean: 1.5, range: 1.0–5.0). About 18 percent of ACL respondents perceived job insecurity in 1986 and 15 percent perceived insecurity in 1989, compared with about 16 percent of MIDUS respondents in 1995 and 13 percent in 2005. While about three-quarters of each sample did not perceive job insecurity, about 13 percent reported it in Wave 1 only, about 7–8 percent in Wave 2 only, and 3–5 percent in both waves. Episodic and persistence measures are presented for all respondents working at Wave 1 (though some have left paid work by Wave 2 and thus are ineligible to report perceived insecurity at Wave 2 only, or in both Waves 1 and 2). In a more restricted sample working at both waves (not shown), the distributions were similar, with 11–12 percent insecure in Wave 1 only, 9–10 percent insecure in Wave 2 only, and 4–6 percent insecure at both waves. About 9 percent of ACL respondents lost a job involuntarily between 1983 and 1986, while about 8 percent did between 1986 and 1989. About 6 percent of MIDUS respondents experienced at least one week of unemployment in 1994, and about 5 percent did in 2004. The two samples show many similarities in the other sociodemographic characteristics, though there are more smokers and a greater share of men in the ACL sample, and a larger fraction of MIDUS respondents left paid work over the longer follow up.
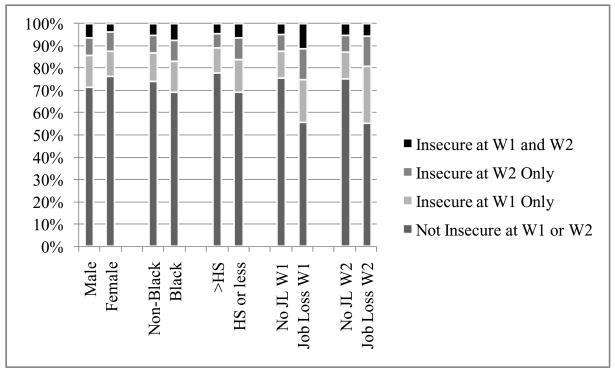
Figure 1 and Figure 2 present bivariate comparisons of episodic and persistent perceived job insecurity by key sociodemographic characteristics and objective employment experiences, with chi-square tests used to assess the significance of differences. Figure 1 shows that among ACL respondents, Blacks report significantly more insecurity than non-Blacks (p < .05), those with high school or less education report significantly more job insecurity than those with more education (p <.01), and those with a job loss in the three years before baseline (p < .001) or over follow-up (p < .001) report considerably more perceived insecurity than those who did not experience a job loss.
Figure 1.
Episodic and Persistent Perceived Job Insecurity by Sociodemographic Characteristics, ACL Respondents.
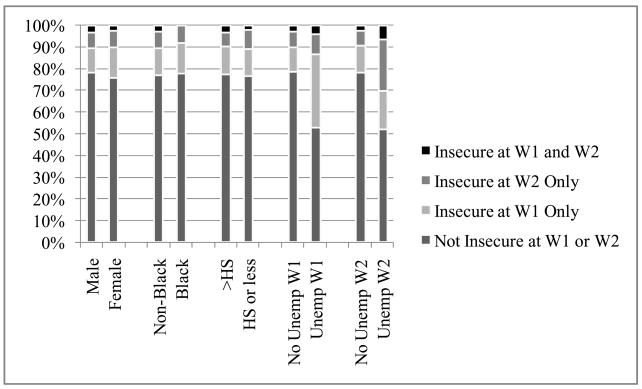
Figure 2.
Episodic and Persistent Perceived Job Insecurity by Sociodemographic Characteristics, MIDUS Respondents.
Figure 2 presents the same comparisons for MIDUS respondents; the only significant differences are between those with unemployment experience in 1994 (p < .001) or in 2004 (p < .001) and those without any unemployment experience. Both figures show that the largest variation in perceived job insecurity is associated with objective employment insecurity experiences, suggesting that people are responding realistically to their experiences in the labor market.
Table 2 (ACL) and Table 3 (MIDUS) present results from OLS regression models of self-rated health and depressive symptoms/negative affect, displaying unstandardized coefficients with robust standard errors in parentheses. Results show that with only basic controls for sex, age, race, and employment status at follow-up in Models 1 and 4, ACL and MIDUS respondents who perceived job insecurity only at Wave 1 have significantly worse depressive symptoms/negative affect at Wave 2 than those who never perceived job insecurity, although the association is only marginally significant (p < .10) among MIDUS respondents. ACL respondents who perceived insecurity only at Wave 1 have significantly poorer self-rated health. Respondents who reported insecurity only at Wave 2 have significantly poorer self-rated health and negative affect at Wave 2 in the MIDUS sample. For ACL and MIDUS respondents alike, however, Models 1 and 4 in Tables 2 and 3 show that persistent exposure to perceived job insecurity is associated with substantively and statistically significantly worse self-rated health and depressive symptoms/negative affect.
Table 2.
Unstandardized Coefficients (and Standard Errors) from OLS Regressions of Self-Rated Health and Depressive Symptoms at Wave 2, ACL Respondents
| Self-Rated Health |
Depressive Symptoms |
|||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
| Coef. (S.E.) | Coef. (S.E.) | Coef. (S.E.) | Coef. (S.E.) | Coef. (S.E.) | Coef. (S.E.) | |
| Insecure Wave 1 Only (N = 208)a | −0.223 (0.098) * | −0.044 (0.086) | −0.032 (0.085) | 0.121 (0.032) ** | 0.035 (0.028) | 0.032 (0.028) |
| Insecure Wave 2 Only (N = 123)a | −0.127 (0.096) | −0.109 (0.080) | −0.101 (0.082) | 0.033 (0.034) | 0.010 (0.027) | 0.008 (0.027) |
| Insecure Waves 1 & 2(N = 85)a | −0.449 (0.115) *** | −0.397 (0.103) *** | −0.396 (0.103) *** | 0.179 (0.048) *** | 0.117 (0.042) ** | 0.117 (0.042) ** |
| Male | 0.059 (0.056) | 0.025 (0.050) | 0.031 (0.050) | −0.043 (0.019) * | −0.009 (0.018) | −0.011 (0.018) |
| Age 1986 | −0.009 (0.002) *** | −0.005 (0.002) * | −0.005 (0.002) ** | −0.002 (0.001) * | 0.000 (0.001) | 0.000 (0.001) |
| Black Race | −0.189 (0.067) ** | −0.080 (0.058) | −0.076 (0.058) | 0.103 (0.022) *** | 0.065 (0.020) ** | 0.064 (0.020) ** |
| Working in 1989 | 0.195 (0.120) | 0.055 (0.091) | 0.044 (0.091) | −0.042 (0.039) | −0.008 (0.031) | −0.005 (0.031) |
| Involuntary job loss 1983–1986 | -- | −0.116 (0.092) | −0.094 (0.094) | -- | 0.047 (0.034) | 0.042 (0.035) |
| Involuntary job loss 1986–1989 | -- | -- | −0.139 (0.093) | -- | -- | 0.035 (0.037) |
| Unmarried/Unpartnered 1986 | -- | 0.038 (0.057) | 0.037 (0.057) | -- | −0.032 (0.020) | −0.032 (0.020) |
| <=High School 1986 | -- | 0.015 (0.051) | 0.015 (0.052) | -- | 0.004 (0.019) | 0.004 (0.019) |
| Self Employed 1986 | -- | 0.106 (0.063)† | 0.103 (0.063) | -- | −0.018 (0.022) | −0.018 (0.022) |
| Part time 1986 | -- | −0.065 (0.065) | −0.062 (0.064) | -- | 0.002 (0.022) | 0.001 (0.022) |
| Household Income1986 | -- | −0.011 (0.036) | −0.014 (0.036) | -- | −0.036 (0.013) ** | −0.036 (0.013) ** |
| Health Shock 1983–1986 | -- | −0.116 (0.070)† | −0.118 (0.069)† | -- | 0.052 (0.028)† | 0.052 (0.028)† |
| Neuroticism 1986 | -- | −0.077 (0.026) ** | −0.076 (0.026) ** | -- | 0.067 (0.012) *** | 0.067 (0.012) *** |
| High Blood Pressure 1986 | -- | −0.177 (0.076) * | −0.175 (0.076) * | -- | 0.045 (0.028) | 0.045 (0.028) |
| Current Smoker 1986 | -- | −0.154 (0.054) ** | −0.150 (0.054) ** | -- | 0.023 (0.019) | 0.022 (0.019) |
| SRH/Depressive Symptoms 1986 | -- | 0.486 (0.029) *** | 0.489 (0.029) *** | -- | 0.316 (0.037) *** | 0.315 (0.037) *** |
| Constant | 3.569 (0.112) *** | 1.949 (0.433) *** | 1.981 (0.434) *** | 1.344 (0.036) *** | 1.275 (0.168) *** | 1.267 (0.169) *** |
|
|
||||||
| R2 | 0.046 | 0.341 | 0.342 | 0.047 | 0.290 | 0.291 |
Note : N = 1507 for all models. Models estimated using wave two weight.
p<.001,
p<.01,
p<.01,
p<.10.
Omitted category is insecure at neither wave.
Table 3.
Unstandardized Coefficients (and Standard Errors) from OLS Regressions of Self-Rated Health and Negative Affect at Wave 2, MIDUS Respondents
| Self-Rated Health |
Negative Affect |
|||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
| Coef. (S.E.) | Coef. (S.E.) | Coef. (S.E.) | Coef. (S.E.) | Coef. (S.E.) | Coef. (S.E.) | |
| Insecure Wave 1 Only (N = 156)a | −0.153 (0.097) | −0.042 (0.074) | −0.039 (0.074) | 0.119 (0.064)† | −0.002 (0.054) | −0.005 (0.054) |
| Insecure Wave 2 Only (N = 83)a | −0.295 (0.107) ** | −0.112 (0.094) | −0.104 (0.094) | 0.225 (0.090) * | 0.170 (0.089)† | 0.158 (0.090)† |
| Insecure Waves 1 & 2 (N = 35)a | −0.422 (0.155) ** | −0.295 (0.140) * | −0.290 (0.141) * | 0.268 (0.121) * | 0.137 (0.084) | 0.130 (0.085) |
| Male | −0.062 (0.061) | −0.117 (0.054)* | −0.116 (0.054) * | −0.080 (0.036) * | −0.024 (0.034) | −0.025 (0.034) |
| Age 1995 | −0.004 (0.003) | −0.006 (0.003)* | −0.006 (0.003) * | −0.010 (0.002)*** | −0.005 (0.002) ** | −0.005 (0.002) ** |
| Black Race | −0.430 (0.139) ** | −0.322 (0.110) ** | −0.321 (0.109) ** | 0.073 (0.120) | 0.072 (0.131) | 0.071 (0.130) |
| Working in 2005 | 0.525 (0.085) *** | 0.329 (0.065) *** | 0.329 (0.065) *** | −0.237 (0.062) *** | −0.161 (0.051) ** | −0.161 (0.050) ** |
| Unemployed in 1994 | -- | 0.054 (0.110) | 0.053 (0.110) | -- | 0.019 (0.126) | 0.020 (0.126) |
| Unemployed in 2004 | -- | -- | −0.072 (0.099) | -- | -- | 0.100 (0.075) |
| Unmarried/Unpartnered 1995 | -- | 0.007 (0.062) | 0.009 (0.062) | -- | −0.079 (0.036)* | −0.081 (0.036)* |
| <=High School 1995 | -- | −0.196 (0.056)*** | −0.196 (0.056) ** | -- | 0.031 (0.036) | 0.031 (0.036) |
| Self Employed 1995 | -- | 0.079 (0.072) | 0.078 (0.072) | -- | −0.067 (0.043) | −0.067 (0.043) |
| Part time 1995 | -- | −0.059 (0.069) | −0.059 (0.069) | -- | 0.051 (0.049) | 0.051 (0.049) |
| Household Income 1995 | -- | 0.091 (0.031) ** | 0.091 (0.031) ** | -- | −0.008 (0.021) | −0.008 (0.021) |
| Self Rated Mental Health Age 16 | -- | 0.046 (0.029) | 0.047 (0.029) | -- | −0.039 (0.017) * | −0.040 (0.017) * |
| Neuroticism 1995 | -- | −0.113 (0.041) ** | −0.113 (0.041) ** | -- | 0.080 (0.030) ** | 0.081 (0.030) ** |
| High Blood Pressure 1995 | -- | −0.116 (0.080) | −0.117 (0.080) | -- | 0.069 (0.052) | 0.069 (0.052) |
| Current Smoker 1995 | -- | −0.240 (0.068) *** | −0.239 (0.069) ** | -- | 0.064 (0.044) | 0.061 (0.044) |
| SRH/Negative Affect 1995 | -- | 0.429 (0.034) *** | 0.428 (0.034) *** | -- | 0.357 (0.050) *** | 0.354 (0.050) *** |
| Constant | 3.275 (0.082) *** | 1.098 (0.378) ** | 1.098 (0.379) ** | 1.693 (0.057) *** | 1.133 (0.268) *** | 1.141 (0.268) *** |
|
|
||||||
| R2 | 0.081 | 0.345 | 0.345 | 0.063 | 0.261 | 0.262 |
Note : N = 1216 for all models. Models estimated using wave two weight.
p<.001,
p<.01,
p<.01,
p<.10.
Omitted category is insecure at neither wave.
Adding controls for sociodemographic and job characteristics, health prior to wave one, hypertension and smoking status, neuroticism, and objective employment insecurity before Wave 1 (Models 2 and 5) and objective employment insecurity over follow-up (Models 3 and 6) eliminates the association between perceived job insecurity at Wave 1 and health at Wave 2. Negative effects of perceived insecurity do not appear to persist after insecure working conditions, or an individual’s appraisal of them, change for the better, and after we adjust for factors that may select workers into an insecure job at Wave 1. The additional controls also reduce the association between insecurity at Wave 2 and health at Wave 2 among MIDUS respondents, leaving it only marginally significant in models of negative affect and no longer significant for self-rated health. However, respondents who perceived job insecurity at Waves 1 and 2 have significantly worse self-rated health at follow-up in both samples, and significantly more depressive symptoms among ACL respondents. The association between persistent insecurity and negative affect is no longer significant for MIDUS respondents, likely due to the small number of respondents in this exposure category (N = 35). When we reclassified MIDUS respondents with less than an “excellent” chance to stay in their job as insecure (resulting in 14 percent of respondents persistently insecure instead of the 3 percent reported on here), we found that respondents who were persistently insecure showed significantly worse negative affect (results not shown). By contrast, recoding similarly for ACL resulted in a much larger 30 percent of respondents being classified as persistently insecure, and reduced the magnitude of the association with both outcome measures, rendering the association with depressive symptoms non-significant.
To assess the sensitivity of our findings to the specifications used here, we re-estimated models using only respondents working at both waves, using those who were healthiest at wave one, and including unemployed respondents in the exposed category (models not shown). None of these alternative specifications substantially changed the results reported here, except in some cases making them stronger. We also included measures of stress from other social roles in models not shown here, but our results were unchanged. Finally, we explored interactions between perceived job insecurity and several socio-demographic characteristics of workers, but did not find strong or consistent evidence for socially-patterned differentials in the health consequences of perceived job insecurity.
DISCUSSION
Dramatic changes in the U.S. labor market over recent decades – rising global competition, major restructuring of firms and industrial shifts, and waves of job displacements – have weakened bonds between employers and employees and fueled perceptions of job insecurity. This study provides stronger evidence for the link between perceived insecurity and health than has been available heretofore, with measures of episodic and persistent exposure, adjustment for typically unmeasured job losses and unemployment experiences that could create a spurious relationship, and broad coverage of U.S. workers. We also compared results across longitudinal samples that span about three years to almost a decade, and cover different macroeconomic periods over the 1980s through the mid-2000s.
We hypothesized that perceived job insecurity is associated with subsequent health among U.S. workers, that persistent exposure is associated with worse health consequences than episodic exposure, and that the association is not entirely explained by job losses or unemployment episodes. Our results show that even after adjusting for sociodemographic and job characteristics, health prior to baseline, neuroticism, hypertension and smoking status, and objective employment insecurity before baseline or over follow-up, perceived job insecurity remains a significant predictor of subsequent health. The association is largely concentrated among individuals who reported persistent perceived job insecurity; persistently insecure ACL and MIDUS respondents report significantly worse self-rated health at follow-up, and persistently insecure ACL respondents showed significantly worse depressive symptoms at Wave 2 than those who never perceived their jobs were at risk. Moreover, standardized coefficients (not shown) suggest that persistent job insecurity is a substantively meaningful predictor of subsequent health (not shown). Among ACL respondents, for example, persistent job insecurity has a larger association with self-rated health at follow up than hypertension or smoking status at baseline. By contrast, in only one case was episodic exposure associated with health; perceived insecurity at only Wave 2 was associated with negative affect at Wave 2 among MIDUS respondents, though the association was only marginally significant. The lack of a similar finding for depressive symptoms among ACL respondents might be explained by the substantial variation in the length of the follow-up between studies. It is not possible to determine when respondents who felt secure in Wave 1, but insecure by Wave 2, began to worry about their job security. Nonetheless, with almost a decade between exposure measurements for MIDUS respondents, the potential that the job insecurity measured at Wave 2 had been present long enough to exert effects on mental health is greater than for ACL respondents, whose exposure measurements were collected only about three years apart.
These findings are broadly consistent with those obtained in prior studies of Michigan auto workers (Heaney, Israel, and House 1994) and British civil servants (Ferrie, Shipley, Stansfeld, and Marmot 2002), in that persistent insecurity appears to have the strongest association with health. The larger sample used in the study by Ferrie and colleagues may help to explain why they found stronger associations between episodic exposure and subsequent or concurrent health. However, our results differed from another population-based study of U.S. workers, which did not show a significant influence of perceived insecurity in 1973 or change in perceived insecurity between 1973 and 1977 on distress in 1977 (Tausig and Fenwick 1999). When we re-estimated our models using Tausig and Fenwick’s strategy for coding perceived insecurity and added other predictors included in their analysis, however, the results (not shown) were substantively very similar to those presented here. Perceptions of job insecurity and its salience for U.S. workers may have changed since the recession of the mid-1970s, but it is worth noting that our findings may also be tied to the historical periods they cover. Alternatively, the differences between these two U.S. studies may be due to the different measures of health used.
While job losses and unemployment spells predicted reports of perceived insecurity (Figures 1 and 2), controls for objective employment insecurity did not eliminate the association between persistent perceived insecurity and subsequent health. Our results suggest that concerns about job loss are associated with their own negative consequences, net of the effects of actual job separation and unemployment during the same period of the career. In fact, the estimated impact of perceived insecurity is greater than the estimated effects of job losses or unemployment episodes, based on standardized coefficients (not shown). That objective employment insecurity does not exercise a stronger negative effect on health may appear unexpected, but there are a number of reasons why chronically-high perceived job insecurity may be more strongly associated with health decline than actual job loss or unemployment. These include the ongoing ambiguity about the future, inability to take action unless the feared event actually happens, and the lack of institutionalized supports associated with perceived insecurity. Moreover, there is considerable heterogeneity across workers who lose jobs. For example, a job loss for health-related reasons is relatively rare, but is associated with worse health trajectories than losses for other reasons (Burgard, Brand, and House 2007).
Some limitations of this study remain. We are unable to fully control for unobserved heterogeneity across individuals in the models used here. Unmeasured characteristics of individuals, such as their true underlying health status, could account for both perceived insecurity and health decline. Still, we have included multiple measures of health and health behavior at and before baseline, providing control for time-invariant unobserved characteristics of individuals that may bias association between job insecurity and health, and further tested the sensitivity of our findings in several ways detailed above. A second important limitation is the difficulty of assessing the causal ordering of changes in exposure and outcome. Using prospective measurements of perceived job insecurity improves upon most prior studies, but the actual sequence of events that occurs between survey waves remains unclear. Further attention to these difficulties is warranted, possibly by collecting data with more measurement points and detailed assessment of the timing of changes in perceived job security and health. Finally, as is the case in many studies of job insecurity, we rely on self-reports gathered in survey data. This means that unmeasured characteristics of respondents could determine their responses to questions about their perceived insecurity and their depressive symptoms, for example, creating a spurious association between the two. We have made efforts to address this problem by using longitudinal data, because stable individual characteristics that affect self-reports should be eliminated when we examine changes in health over time. We have also included a measure of neuroticism to tap underlying negative reporting styles, and indicators of objective job losses or unemployment spells. Nonetheless, future studies should include more objective measures of health outcomes where possible.
Our findings have potential implications for policy and intervention. Persistently insecure workers appear to be at risk of negative health consequences, and identification and monitoring are needed so that solutions can be tailored to their experiences. Programs designed for displaced or unemployed workers are unlikely to solve problems faced by many workers who perceive job insecurity, because only a subset of them experiences job loss or unemployment. Different intervention strategies are likely needed to address the damaging aspects of persistent perceived job insecurity. It would also be useful to know more about the conditions that generate or change workers’ perceptions of their job security. Could organizations intervene to reduce perceptions of insecurity and/or their deleterious consequences? Or are broader governmental policies needed that would cushion the adverse effects of job loss, and hence also mitigate the degree of stress associated with perceived job insecurity? Moreover, additional acute and chronic strains in the work domain and other life domains could compound the strain of perceived job insecurity. Future work should also examine the actions undertaken by individuals who perceive their jobs to be insecure (Thoits 1994); do insecure workers who voluntarily change jobs fare better than those who remain in insecure jobs? In addition, the context surrounding the perceived job insecurity–health relationship deserves more attention. Aggregate-level conditions, such as the vibrancy of the national and local labor market, may influence the perception or consequences of job insecurity (Catalano, Rook, and Dooley 1986; Tausig and Fenwick 1999).
Job insecurity is not a new phenomenon, and social commentators have been concerned with its consequences at least since Marx described a “reserve army of labor” whose low wages and unstable employment opportunities instilled fear of job loss in other workers (McDonough 2000). However, as increased “flexibility” in the labor market and the current economic downturn leaves workers at all levels of the occupational hierarchy with concerns about the future of their positions, and consequences of job loss continue to be substantial, perceived job insecurity persists as a potential threat to population health.
Acknowledgments
Author Comments:
Burgard and Brand were supported by the Robert Wood Johnson Health & Society Scholars Program. Brand was supported by the Carolina Population Center NICHD training grant. This research uses data from the Americans’ Changing Lives Study, which has been supported by grants from the National Institute on Aging (PO1 AG05561 and R01 AG018418) and Robert Wood Johnson Foundation Investigators in Health Policy Research Program (030987), which have also supported House’s involvement with this paper. We also use data from the Midlife in the United State Study (MIDUS), funded by the John D. and Catherine T. MacArthur Foundation and the National Institute on Aging, and publicly available from the Inter-university Consortium for Political and Social Research (ICPSR).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Sarah A. Burgard, University of Michigan Ann Arbor, MI UNITED STATES
Jennie E Brand, University of California, Los Angeles.
James S House, University of Michigan.
References
- Allison Paul. Using Panel Data to Estimate the Effects of Events. Sociological Methods and Research. 1994;23:174–199. [Google Scholar]
- Brief AP, Burke MJ, George JM, Robinson BS, Webster J. Should Negative Affectivity Remain an Unmeasured Variable in the Study of Job Stress? Journal of Applied Psychology. 1988;73:193–198. doi: 10.1037/0021-9010.73.2.193. [DOI] [PubMed] [Google Scholar]
- Burgard Sarah A, Brand Jennie E, House James S. Toward a Better Estimation of the Effect of Job Loss on Health. Journal of Health and Social Behavior. 2007;48:369–384. doi: 10.1177/002214650704800403. [DOI] [PubMed] [Google Scholar]
- Cappelli P, Bassi L, Katz H, Knoke D, Osterman P, Useem M. Change at Work. New York: Oxford University Press; 1997. [Google Scholar]
- Catalano Ralph, Rook Karen, Dooley David. Labor Markets and Help-Seeking: A Test of the Employment Security Hypothesis. Journal of Health and Social Behavior. 1986;27:277–287. [PubMed] [Google Scholar]
- Cheng Yawen, Chen Chun-Wan, Chen Chiou-Jong, Chiang Tung-Liang. Job Insecurity and Its Association with Health among Employees in the Taiwanese General Population. Social Science and Medicine. 2005;61:41–52. doi: 10.1016/j.socscimed.2004.11.039. [DOI] [PubMed] [Google Scholar]
- De Witte H. Job Insecurity and Psychological Well-Being: Review of the Literature and Exploration of Some Unresolved Issues. European Journal of Work and Organizational Psychology. 1999;8:155–177. [Google Scholar]
- Dekker SWA, Schaufeli WB. The Effects of Job Insecurity on Psychological Health and Withdrawal: A Longitudinal Study. Australian Psychologist. 1995;30:57–63. [Google Scholar]
- Elman Cheryl, O’Rand Angela M. Perceived Job Insecurity and Entry Into Work-Related Education and Training among Adult Workers. Social Science Research. 2002;31:49–76. [Google Scholar]
- Eysenck HJ, Eysenck SBG. Manual of the Eysenck Personality Questionnaire. London: Hodder & Stoughton; 1975. [Google Scholar]
- Ferrie Jane Elizabeth, Shipley Martin John, Marmot Michael Gideon, Stansfeld Stephen Alfred, Smith George Davey. Health Effects of Anticipation of Job Change and Non-employment: Longitudinal Data from the Whitehall II Study. British Medical Journal. 1995;311:1264–1269. doi: 10.1136/bmj.311.7015.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrie Jane Elizabeth, Shipley Martin John, Marmot Michael Gideon, Stansfeld Stephen Alfred, Smith George Davey. An Uncertain Future: The Health Effects of Threats to Employment Security in White-Collar Men and Women. American Journal of Public Health. 1998;88:1030–1036. doi: 10.2105/ajph.88.7.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrie Jane Elizabeth, Shipley Martin John, Stansfeld Stephen Alfred, Marmot Michael Gideon. Effects of Chronic Job Insecurity and Change in Job Security on Self Reported Health, Minor Psychiatric Morbidity, Physiological Measures, and Health Related Behaviors in British Civil Servants: The Whitehall II Study. Journal of Epidemiology and Community Health. 2002;56:450–454. doi: 10.1136/jech.56.6.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fullerton Andrew S, Wallace Michael. Traversing the flexible turn: US workers’ perceptions of job security, 1977–2002. Social Science Research. 2007;36:201–221. [Google Scholar]
- Gallo WT, Bradley EH, Dubin JA, Jones RN, Falba TA, Teng HM, Kasl SV. The persistence of depressive symptoms in older workers who experience involuntary job loss: results from the health and retirement survey. J Gerontol B Psychol Sci Soc Sci. 2006;61:S221–S228. doi: 10.1093/geronb/61.4.s221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo WT, Teng HM, Falba TA, Kasl SV, Krumholz HM, Bradley EH. The impact of late career job loss on myocardial infarction and stroke: a 10 year follow up using the health and retirement survey. Occupational and Environmental Medicine. 2006;63:683–687. doi: 10.1136/oem.2006.026823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazzaniga MS, Heatherton TF. Psychological Science: Mind, Brain, and Behavior. New York: W.W. Norton Company; 2003. [Google Scholar]
- Greenhalgh L, Rosenblatt Z. Job Insecurity: Toward Conceptual Clarity. Academy of Management Review. 1984;3:438–448. [Google Scholar]
- Hacker Jacob S. The Great Risk Shift: The Assault on American Jobs, Families, Health Care, and Retirement--And How You Can Fight Back. New York: Oxford University Press; 2006. [Google Scholar]
- Halaby Charles N. Panel Models in Sociological Research: Theory into Practice. Annual Review of Sociology. 2004;30:507–544. [Google Scholar]
- Hartley J, Jacobson D, Klandermans B, van Vuuren T. Job Insecurity: Coping with Jobs at Risk. London: Sage; 1991. [Google Scholar]
- Heaney Catherine A, Israel Barbara A, House James S. Chronic Job Insecurity Among Automobile Workers: Effects on Job Satisfaction and Health. Social Science and Medicine. 1994;38:1431–1437. doi: 10.1016/0277-9536(94)90281-x. [DOI] [PubMed] [Google Scholar]
- Hellgren Johnny, Sverke Magnus. Does Job Insecurity Lead to Impaired Well-Being or Vice Versa? Estimation of Cross-Lagged Effects Using Latent Variable Modelling. Journal of Organizational Behavior. 2003;24:215–236. [Google Scholar]
- House James S, Lantz Paula M, Herd Pamela. Continuity and Change in the Social Stratification of Aging and Health Over the Life Course: Evidence from a Nationally Representative Longitudinal Study from 1986 to 2001/2 (Americans’ Changing Lives Study) Journal of Gerontology: Series B. 2005;60 B:S15–26. doi: 10.1093/geronb/60.special_issue_2.s15. [DOI] [PubMed] [Google Scholar]
- Idler Ellen L, Benyamini Yael. Self-Rated Health and Mortality: A Review of Twenty-Seven Community Studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Iversen L, Sabroe S, Damsgaard MT. Hospital Admissions Before and After Shipyard Closure. British Medical Journal. 1989;299:1073–1076. doi: 10.1136/bmj.299.6707.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joelson L, Wahlquist L. The Psychological Meaning of Job Insecurity and Job Loss: Results of a Longitudinal Study. Social Science and Medicine. 1987;25:179–182. doi: 10.1016/0277-9536(87)90386-8. [DOI] [PubMed] [Google Scholar]
- Kasl SV, Cobb S, Brooks GW. Changes in Serum Uric Acid and Cholesterol Levels among Men Undergoing Job Loss. Journal of the American Medical Association. 1968;206:1500–1507. [PubMed] [Google Scholar]
- Kessler Ronald C, Turner JB, House James S. Unemployment, Reemployment and Emotional Functioning in a Community Sample. American Sociological Review. 1989;54:648–657. [Google Scholar]
- Lazarus RS. Psychological Stress and the Coping Process. New York: McGraw-Hill; 1966. [Google Scholar]
- Lee Submin, Colditz Graham A, Berkman Lisa F, Kawachi Ichiro. Prospective Study of Job Insecurity and Coronary Heart Disease in US Women. Annals of Epidemiology. 2004;14:24–30. doi: 10.1016/s1047-2797(03)00074-7. [DOI] [PubMed] [Google Scholar]
- Mattiasson I, Lindgarde F, Nilsson JA, Theorell T. Threat of Unemployment and Cardiovascular Risk Factors: Longitudinal Study of Quality of Sleep and Serum Cholesterol Concentrations in Men Threatened with Redundancy. British Medical Journal. 1990;301:461–466. doi: 10.1136/bmj.301.6750.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonough Peggy. Job Insecurity and Health. International Journal of Health Services. 2000;30:453–476. doi: 10.2190/BPFG-X3ME-LHTA-6RPV. [DOI] [PubMed] [Google Scholar]
- Price Richard H, Burgard Sarah A. The New Employment Contract and Worker Health in the United States. In: Schoeni RF, House JS, Kaplan GA, Pollack H, editors. Social and Economic Policy as Health Policy: Rethinking America’s Approach to Improving Health. New York: Russell Sage; 2008. pp. 201–227 . [Google Scholar]
- Radloff Lenore S. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rugulies Reiner, Bultmann Ute, Aust Birgit, Burr Hermann. Psychosocial Work Environment and Incidence of Severe Depressive Symptoms: Prospective Findings from a 5-Year Follow-Up of the Danish Work Environment Cohort Study. American Journal of Epidemiology. 2006;163:877–887. doi: 10.1093/aje/kwj119. [DOI] [PubMed] [Google Scholar]
- Schmidt Stefanie R. Job Security Beliefs in the General Social Survey: Evidence on Long-Run Trends and Comparability with Other Surveys. In: Neumark D, editor. On the Job: Is Long-Term Employment a Thing of the Past? New York: Russell Sage Foundation; 2000. pp. 300–334. [Google Scholar]
- Schnittker Jason. When Mental Health Becomes Health: Age and the Shifting Meaning of Self-Evaluations of General Health. The Milbank Quarterly. 2005;83:397–423. doi: 10.1111/j.1468-0009.2005.00407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sverke Magnus, Gallagher DG, Johnny Hellgren. Job Stress, Well-being, and Work Attitudes Among Employees with Different Employment Contracts. In: Isaksson K, Hogstedt C, Eriksson C, Theorell T, editors. Health Effects of the New Labour Market. New York: Kluwer Academic/Plenum Publishers; 2000. pp. 145–167. [Google Scholar]
- Tausig Mark, Fenwick Rudy. Recession and Well-Being. Journal of Health and Social Behavior. 1999;40:1–16. [PubMed] [Google Scholar]
- Thoits Peggy A. Stressors and Problem-Solving: The Individual as Psychological Activist. Journal of Health and Social Behavior. 1994;35:143–159. [PubMed] [Google Scholar]
- Turner J Blake. Economic Context and the Health Effects of Unemployment. Journal of Health and Social Behavior. 1995;36:213–229. [PubMed] [Google Scholar]
- Watson D, Clark LA. Negative Affectivity: The Disposition to Experience Aversive Emotional States. Psychological Bulletin. 1984;96:465–490. [PubMed] [Google Scholar]